Risk Factors Associated with Community-Onset Infections Due to Multidrug-Resistant Organisms
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Study Population
4.3. Data Collection
4.4. Data Management
4.5. Ethical Considerations
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AMR | Antimicrobial Resistance |
| BSI | Bloodstream Infection |
| CAD | Coronary Artery Disease |
| CDC | Centers for Disease Control and Prevention |
| CHF | Congestive Heart Failure |
| CI | Confidence Interval |
| CKD | Chronic Kidney Disease |
| COPD | Chronic Obstructive Pulmonary Disease |
| CRP | C-Reactive Protein |
| CTD | Connective Tissue Disease |
| CVC | Central Venous Catheter |
| DM | Diabetes Mellitus |
| ECDC | European Centre for Disease Control and Prevention |
| ESBL | Extended-Spectrum β-lactamase |
| ESRD | End-Stage Renal Disease |
| MDRO | Multidrug-Resistant Organism |
| GDPR | General Data Protection Regulation |
| GII | Gastrointestinal Infection |
| HAI | Hospital-Acquired Infection |
| ICU | Intensive Care Unit |
| MRSA | methicillin-resistant Staphylococcus aureus |
| OR | Odds Ratio |
| PAD | Peripheral Artery Disease |
| PCT | Procalcitonin |
| RTI | Respiratory Tract Infection |
| SD | Standard Deviation |
| SOFA | Sequential Organ Failure Assessment |
| SSTI | Skin and Soft Tissue Infection |
| UTI | Urinary Tract Infection |
| VISA | Vancomycin Intermediate Staphylococcus aureus |
| VRE | Vancomycin Resistant Enterococci |
| VRSA | Vancomycin Resistant Staphylococcus aureus |
| WBC | White Blood Cell |
References
- DeLeo, F.R.; Otto, M.; Kreiswirth, B.N.; Chambers, H.F. Community-Associated Meticillin-Resistant Staphylococcus Aureus. Lancet 2010, 375, 1557–1568. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Baño, J.; Pascual, A. Clinical Significance of Extended-Spectrum Beta-Lactamases. Expert. Rev. Anti Infect. Ther. 2008, 6, 671–683. [Google Scholar] [CrossRef]
- Lynch, J.P.; Zhanel, G.G. Streptococcus pneumoniae: Does Antimicrobial Resistance Matter? Semin. Respir. Crit. Care Med. 2009, 30, 210–238. [Google Scholar] [CrossRef]
- Villafuerte, D.; Aliberti, S.; Soni, N.J.; Faverio, P.; Marcos, P.J.; Wunderink, R.G.; Rodriguez, A.; Sibila, O.; Sanz, F.; Martin-Loeches, I.; et al. Prevalence and Risk Factors for Enterobacteriaceae in Patients Hospitalized with Community-Acquired Pneumonia. Respirology 2020, 25, 543–551. [Google Scholar] [CrossRef]
- Cassone, M.; Mody, L. Colonization with Multi-Drug Resistant Organisms in Nursing Homes: Scope, Importance, and Management. Curr. Geriatr. Rep. 2015, 4, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Arancibia, F.; Ruiz, M. Risk Factors for Drug-Resistant Cap in Immunocompetent Patients. Curr. Infect. Dis. Rep. 2017, 19, 11. [Google Scholar] [CrossRef]
- Costelloe, C.; Metcalfe, C.; Lovering, A.; Mant, D.; Hay, A.D. Effect of Antibiotic Prescribing in Primary Care on Antimicrobial Resistance in Individual Patients: Systematic Review and Meta-Analysis. BMJ 2010, 340, c2096. [Google Scholar] [CrossRef]
- Mermel, L.A.; Eells, S.J.; Acharya, M.K.; Cartony, J.M.; Dacus, D.; Fadem, S.; Gay, E.A.; Gordon, S.; Lonks, J.R.; Perl, T.M.; et al. Quantitative Analysis and Molecular Fingerprinting of Methicillin-Resistant Staphylococcus aureus Nasal Colonization in Different Patient Populations: A Prospective, Multicenter Study. Infect. Control Hosp. Epidemiol. 2010, 31, 592–597. [Google Scholar] [CrossRef]
- Parker, M.G.; Doebbeling, B.N. The Challenge of Methicillin-Resistant Staphylococcus aureus Prevention in Hemodialysis Therapy. Semin. Dial. 2012, 25, 42–49. [Google Scholar] [CrossRef]
- Schmid, H.; Romanos, A.; Schiffl, H.; Lederer, S.R. Persistent Nasal Methicillin-Resistant Staphylococcus aureus Carriage in Hemodialysis Outpatients: A Predictor of Worse Outcome. BMC Nephrol. 2013, 14, 93. [Google Scholar] [CrossRef] [PubMed]
- Larson, E. Community Factors in the Development of Antibiotic Resistance. Annu. Rev. Public Health 2007, 28, 435–447. [Google Scholar] [CrossRef]
- Sun, R.; Yao, T.; Zhou, X.; Harbarth, S.; Lin, L. Non-Biomedical Factors Affecting Antibiotic Use in the Community: A Mixed-Methods Systematic Review and Meta-Analysis. Clin. Microbiol. Infect. 2022, 28, 345–354. [Google Scholar] [CrossRef] [PubMed]
- Shutt, A.E.; Ashiru-Oredope, D.; Price, J.; Padoveze, M.C.; Shafiq, N.; Carter, E.; Ghataure, A.; Shariq, S.; Holmes, A.H.; Charani, E. The Intersection of the Social Determinants of Health and Antimicrobial Resistance in Human Populations: A Systematic Review. BMJ Glob. Health 2025, 10, e017389. [Google Scholar] [CrossRef] [PubMed]
- Cooper, L.N.; Beauchamp, A.M.; Ingle, T.A.; Diaz, M.I.; Wakene, A.D.; Katterpalli, C.; Keller, T.; Walker, C.; Blumberg, S.; Kanjilal, S.; et al. Socioeconomic Disparities and the Prevalence of Antimicrobial Resistance. Clin. Infect. Dis. 2024, 79, 1346–1353. [Google Scholar] [CrossRef] [PubMed]
- Barrasa-Villar, J.I.; Aibar-Remón, C.; Prieto-Andrés, P.; Mareca-Doñate, R.; Moliner-Lahoz, J. Impact on Morbidity, Mortality, and Length of Stay of Hospital-Acquired Infections by Resistant Microorganisms. Clin. Infect. Dis. 2017, 65, 644–652. [Google Scholar] [CrossRef]
- Shindo, Y.; Ito, R.; Kobayashi, D.; Ando, M.; Ichikawa, M.; Shiraki, A.; Goto, Y.; Fukui, Y.; Iwaki, M.; Okumura, J.; et al. Risk Factors for Drug-Resistant Pathogens in Community-Acquired and Healthcare-Associated Pneumonia. Am. J. Respir. Crit. Care Med. 2013, 188, 985–995. [Google Scholar] [CrossRef]
- Sulis, G.; Sayood, S.; Katukoori, S.; Bollam, N.; George, I.; Yaeger, L.H.; Chavez, M.A.; Tetteh, E.; Yarrabelli, S.; Pulcini, C.; et al. Exposure to World Health Organization’s AWaRe Antibiotics and Isolation of Multidrug Resistant Bacteria: A Systematic Review and Meta-Analysis. Clin. Microbiol. Infect. 2022, 28, 1193–1202. [Google Scholar] [CrossRef]
- Qureshi, S.; Maria, N.; Zeeshan, M.; Irfan, S.; Qamar, F.N. Prevalence and Risk Factors Associated with Multi-Drug Resistant Organisms (MDRO) Carriage among Pediatric Patients at the Time of Admission in a Tertiary Care Hospital of a Developing Country. A Cross-Sectional Study. BMC Infect. Dis. 2021, 21, 547. [Google Scholar] [CrossRef]
- Ye, Q.; Chen, X.; Zhang, J.; Lin, J. Meta-Analysis of Risk Factors for Infection by Multi-Drug-Resistant Organisms in Intensive Care Unit Patients. J. Hosp. Infect. 2025, 158, 1–10. [Google Scholar] [CrossRef]
- Woodhouse, E.W.; Alsoubani, M.; Roach, D.J.; Flynn, D.B.; LaValley, M.; Sheridan, K.; Hooper, D.C.; Fowler, V.G.; Duffy, E.M.; Grossman, T.H. Infection Risk Associated with Colonization by Multidrug-Resistant Gram-Negative Bacteria: An Umbrella Review and Meta-Analysis. Open Forum Infect. Dis. 2025, 12, ofaf365. [Google Scholar] [CrossRef]
- Tenney, J.; Hudson, N.; Alnifaidy, H.; Li, J.T.C.; Fung, K.H. Risk Factors for Aquiring Multidrug-Resistant Organisms in Urinary Tract Infections: A Systematic Literature Review. Saudi Pharm. J. 2018, 26, 678–684. [Google Scholar] [CrossRef]
- Capsoni, N.; Bellone, P.; Aliberti, S.; Sotgiu, G.; Pavanello, D.; Visintin, B.; Callisto, E.; Saderi, L.; Soldini, D.; Lardera, L.; et al. Prevalence, Risk Factors and Outcomes of Patients Coming from the Community with Sepsis Due to Multidrug Resistant Bacteria. Multidiscip. Respir. Med. 2019, 14, 23. [Google Scholar] [CrossRef] [PubMed]
- Dadi, N.C.T.; Radochová, B.; Vargová, J.; Bujdáková, H. Impact of Healthcare-Associated Infections Connected to Medical Devices—An Update. Microorganisms 2021, 9, 2332. [Google Scholar] [CrossRef] [PubMed]
- Papanikolopoulou, A.; Maltezou, H.C.; Stoupis, A.; Kalimeri, D.; Pavli, A.; Boufidou, F.; Karalexi, M.; Pantazis, N.; Pantos, C.; Tountas, Y.; et al. Catheter-Associated Urinary Tract Infections, Bacteremia, and Infection Control Interventions in a Hospital: A Six-Year Time-Series Study. JCM 2022, 11, 5418. [Google Scholar] [CrossRef]
- Bouhrour, N.; Nibbering, P.H.; Bendali, F. Medical Device-Associated Biofilm Infections and Multidrug-Resistant Pathogens. Pathogens 2024, 13, 393. [Google Scholar] [CrossRef] [PubMed]
- Laudisio, A.; Marinosci, F.; Gemma, A.; Bartoli, I.R.; Montenegro, N.; Incalzi, R.A. The Burden of Comorbidity Is Associated with Antibiotic Resistance Among Institutionalized Elderly with Urinary Infection: A Retrospective Cohort Study in a Single Italian Nursing Home Between 2009 and 2014. Microb. Drug Resist. 2017, 23, 500–506. [Google Scholar] [CrossRef]
- Itani, R.; Khojah, H.M.J.; Kibrit, R.; Raychouni, H.; Shuhaiber, P.; Dib, C.; Hassan, M.; Mukattash, T.L.; El-Lakany, A. Risk Factors Associated with Multidrug-Resistant Klebsiella Pneumoniae Infections: A Multicenter Observational Study in Lebanese Hospitals. BMC Public. Health 2024, 24, 2958. [Google Scholar] [CrossRef]
- Nakai, H.; Hagihara, M.; Kato, H.; Hirai, J.; Nishiyama, N.; Koizumi, Y.; Sakanashi, D.; Suematsu, H.; Yamagishi, Y.; Mikamo, H. Prevalence and Risk Factors of Infections Caused by Extended-Spectrum β-Lactamase (ESBL)-Producing Enterobacteriaceae. J. Infect. Chemother. 2016, 22, 319–326. [Google Scholar] [CrossRef]
- Ng, R.W.Y.; Yang, L.; Lau, S.H.; Hawkey, P.; Ip, M. Global Prevalence of Human Intestinal Carriage of ESBL-Producing E. Coli during and after the COVID-19 Pandemic. JAC-Antimicrob. Resist. 2024, 7, dlaf001. [Google Scholar] [CrossRef]
- Al-Mayahie, S.; Al Kuriashy, J.J. Distribution of ESBLs among Escherichia coli Isolates from Outpatients with Recurrent UTIs and Their Antimicrobial Resistance. J. Infect. Dev. Ctries. 2016, 10, 575–583. [Google Scholar] [CrossRef]
- Doi, Y.; Park, Y.S.; Rivera, J.I.; Adams-Haduch, J.M.; Hingwe, A.; Sordillo, E.M.; Lewis, J.S.; Howard, W.J.; Johnson, L.E.; Polsky, B.; et al. Community-Associated Extended-Spectrum β-Lactamase–Producing Escherichia coli Infection in the United States. Clin. Infect. Dis. 2013, 56, 641–648. [Google Scholar] [CrossRef]
- Zhang, J.; Zhou, K.; Zheng, B.; Zhao, L.; Shen, P.; Ji, J.; Wei, Z.; Li, L.; Zhou, J.; Xiao, Y. High Prevalence of ESBL-Producing Klebsiella pneumoniae Causing Community-Onset Infections in China. Front. Microbiol. 2016, 7, 1830. [Google Scholar] [CrossRef]
- Azzam, A.; Khaled, H.; Samer, D.; Nageeb, W.M. Prevalence and Molecular Characterization of ESBL-Producing Enterobacteriaceae in Egypt: A Systematic Review and Meta-Analysis of Hospital and Community-Acquired Infections. Antimicrob. Resist. Infect. Control 2024, 13, 145. [Google Scholar] [CrossRef] [PubMed]
- Naushad, V.A.; Purayil, N.K.; Wilson, G.J.; Chandra, P.; Joseph, P.; Khalil, Z.; Zahid, M.; Kayakkool, M.K.; Shaik, N.; Ayari, B.; et al. Epidemiology of Urinary Tract Infection in Adults Caused by Extended-Spectrum Beta-Lactamase (ESBL)-Producing Enterobacteriaceae—A Case-Control Study from Qatar. IJID Reg. 2022, 3, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Kung, C.-H.; Ku, W.-W.; Lee, C.-H.; Fung, C.-P.; Kuo, S.-C.; Chen, T.-L.; Lee, Y.-T. Epidemiology and Risk Factors of Community-Onset Urinary Tract Infection Caused by Extended-Spectrum β-Lactamase-Producing Enterobacteriaceae in a Medical Center in Taiwan: A Prospective Cohort Study. J. Microbiol. Immunol. Infect. 2015, 48, 168–174. [Google Scholar] [CrossRef][Green Version]
- Bezabih, Y.M.; Bezabih, A.; Dion, M.; Batard, E.; Teka, S.; Obole, A.; Dessalegn, N.; Enyew, A.; Roujeinikova, A.; Alamneh, E.; et al. Comparison of the Global Prevalence and Trend of Human Intestinal Carriage of ESBL-Producing Escherichia coli between Healthcare and Community Settings: A Systematic Review and Meta-Analysis. JAC-Antimicrob. Resist. 2022, 4, dlac048. [Google Scholar] [CrossRef] [PubMed]
- Sule, I.O.; Mendelsohn, A.; Panas, R.M. The Causes and Control Measures of Extended Spectrum Beta-Lactamase Producing Enterobacteriaceae in Long-Term Care Facilities: A Systematic Review and Meta-Analysis. Health Serv. Res. Manag. Epidemiol. 2022, 9, 23333928221131709. [Google Scholar] [CrossRef]
- Freeman, J.T.; McBride, S.J.; Nisbet, M.S.; Gamble, G.D.; Williamson, D.A.; Taylor, S.L.; Holland, D.J. Bloodstream Infection with Extended-Spectrum Beta-Lactamase-Producing Enterobacteriaceae at a Tertiary Care Hospital in New Zealand: Risk Factors and Outcomes. Int. J. Infect. Dis. 2012, 16, e371–e374. [Google Scholar] [CrossRef]
- Kohler, P.; Wolfensberger, A.; Stampf, S.; Brönnimann, A.; Boggian, K.; Van Delden, C.; Favre, M.; Hirzel, C.; Khanna, N.; Kuster, S.P.; et al. Temporal Trends, Risk Factors and Outcomes of Infections Due to Extended-Spectrum β-Lactamase Producing Enterobacterales in Swiss Solid Organ Transplant Recipients between 2012 and 2018. Antimicrob. Resist. Infect. Control 2021, 10, 50. [Google Scholar] [CrossRef]
- Larramendy, S.; Deglaire, V.; Dusollier, P.; Fournier, J.-P.; Caillon, J.; Beaudeau, F.; Moret, L. Risk Factors of Extended-Spectrum Beta-Lactamases-Producing Escherichia coli Community Acquired Urinary Tract Infections: A Systematic Review. IDR 2020, 13, 3945–3955. [Google Scholar] [CrossRef]
- Barlam, T.F.; Cosgrove, S.E.; Abbo, L.M.; MacDougall, C.; Schuetz, A.N.; Septimus, E.J.; Srinivasan, A.; Dellit, T.H.; Falck-Ytter, Y.T.; Fishman, N.O.; et al. Implementing an Antibiotic Stewardship Program: Guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin. Infect. Dis. 2016, 62, e51–e77. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-Resistant, Extensively Drug-Resistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
| Variable | Mean (SD) or N (%) |
|---|---|
| Demographics | |
| Age (years) | 77.9 (N = 125, SD: 16.9) |
| Sex | |
| Female | 73/125 (58.4%) |
| Male | 52/125 (41.6%) |
| Residence before hospital admission | |
| Home | 93/124 (75%) * |
| Healthcare facility | 31/124 (25%) * |
| Clinical Characteristics | |
| Previous MDRO infections within 12 months | 9/119 (7.6%) * |
| Known colonization with an MDRO | 7/117 (6%) * |
| Previous antibiotic use within 3 months | 46/123 (37.4%) * |
| Previous hospitalizations within 12 months | 54/118 (45.8%) * |
| History of invasive procedure within 1 month (surgery or biopsy) | 3/119 (2.5%) * |
| History of non-invasive procedure within 1 month (colonoscopy or cystoscopy) | 8/118 (6.8%) * |
| CVC | 1/119 (0.8%) * |
| Permanent urinary catheter | 26/120 (21.7%) * |
| Presence of foreign bodies (pacemaker, graft, or joint prostheses) | 18/118 (15.3%) * |
| History of CKD into renal replacement | 1/119 (0.8%) * |
| History of IV infusion therapy at home | 5/119 (4.2%) * |
| Presence of gastrostomy | 2/120 (1.7%) * |
| Variable | N (%) |
|---|---|
| Dementia | 51/125 (40.8%) |
| Hypertension | 65/125 (52%) |
| DM | 29/125 (23.2%) |
| CHF | 23/125 (18.4%) |
| Stroke | 19/125 (15.2%) |
| CAD | 8/124 (6.5%) * |
| PAD | 4/125 (3.2%) |
| CKD | 14/125 (11.2%) |
| Asthma or COPD | 19/125 (15.2%) |
| Immunosuppression | 15/125 (12%) |
| Active malignancy | 9/125 (7.2%) |
| Connective tissue disease | 6/125 (4.8%) |
| Chronic Liver Disease | 5/125 (4%) |
| History of transplantation | 1/125 (0.8%) |
| Trauma | 2/120 (1.7%) * |
| Chronic ulcers or other skin lesions (i.e., decubitus ulcer, diabetic foot, postoperative wound) | 10/125 (8%) |
| Variable | Mean (SD) or N (%) |
|---|---|
| Duration of antibiotics | 11.3 days (N = 119, SD: 7.3) * |
| MDRO | 39/125 (31.7%) |
| ESBL | 28/125 (22.4%) |
| MRSA | 3/125 (2.4%) |
| VRE | 0/125 (0%) |
| VRSA | 0/125 (0%) |
| VISA | 1/125 (0.8%) |
| Resistance to carbapenems | 9/124 (7.3%) * |
| Resistance to colistin | 5/124 (4%) * |
| Length of hospital stay | 10.9 (N = 120, SD: 8.6) * |
| Sepsis | 54/121 (44.6%) * |
| Septic shock | 29/121 (24%) * |
| ICU admission | 1/120 (0.8%) * |
| Death | 30/121 (24.8%) * |
| WBCs (cells/μL) | 12,974 (N = 125, SD: 6490) |
| PCT (ng/mL) | 7.1 (N = 54, SD: 20.9) * |
| CRP (mg/L) | 106.4 (N = 124, SD: 93.8) * |
| Lactic Acid (mmol/L) | 1.85 (N = 119, SD: 1.4) * |
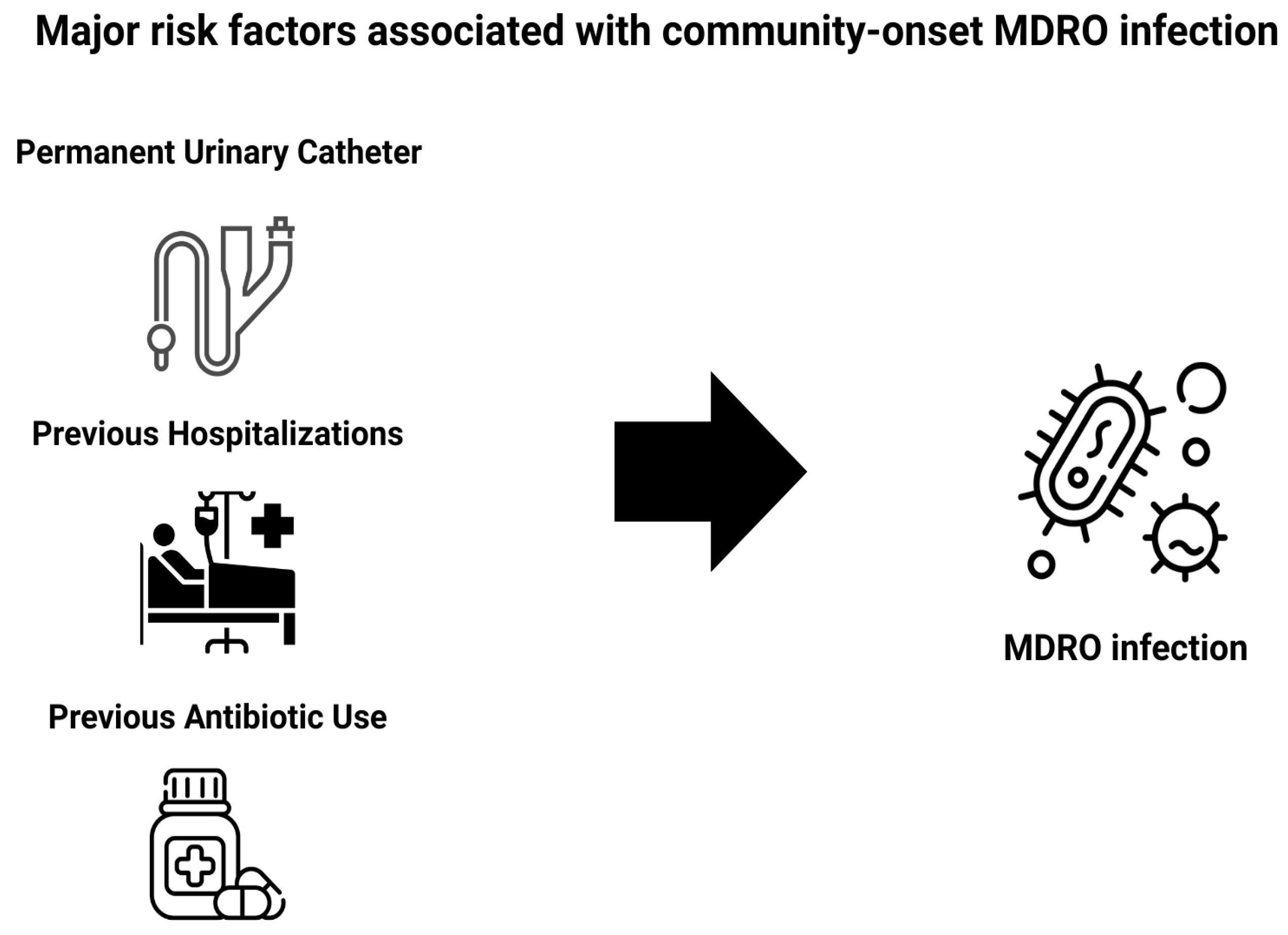
| Variable | OR | p-Value | 95% CI |
|---|---|---|---|
| Healthcare facility residence (vs home) | 1.87 | 0.171 | 0.76–4.59 |
| Recent antibiotic use within 3 months | 2.18 | 0.057 | 0.98–4.84 |
| Previous hospitalizations within 12 months | 3.33 | 0.004 | 1.48–7.51 |
| Permanent urinary catheter | 3.69 | 0.011 | 1.35–10.05 |
| Presence of foreign body (pacemaker, graft, or joint prostheses) | 1.59 | 0.383 | 0.56–4.52 |
| Charlson index score | 3.08 | 0.033 | 1.1–8.68 |
| DM | 1.67 | 0.263 | 0.68–4.07 |
| Hypertension | 1.27 | 0.530 | 0.60–2.72 |
| Chronic liver disease | 0.84 | 0.859 | 0.13–5.63 |
| CKD | 0.81 | 0.737 | 0.24–2.78 |
| CHF | 0.81 | 0.684 | 0.30–2.19 |
| CAD | 1.18 | 0.833 | 0.26–5.24 |
| COPD | 1.83 | 0.258 | 0.64–5.21 |
| Stroke | 2.06 | 0.182 | 0.71–5.94 |
| Dementia | 2.07 | 0.065 | 0.96–4.5 |
| CTD | 2.03 | 0.440 | 0.34–12.17 |
| PAD | 0.309 | 0.323 | 0.03–3.17 |
| Chronic ulcers or other skin lesions (i.e., decubitus ulcer, diabetic foot) | 1.89 | 0.365 | 0.48–7.47 |
| Active malignancy | 1.4 | 0.636 | 0.35–5.69 |
| Immunodeficiency | 0.455 | 0.192 | 0.14–1.48 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matzaras, R.; Biros, D.; Sakkou, S.F.; Lymperatou, D.; Filippas-Ntekouan, S.; Prokopidou, A.; Konstantopoulou, R.; Samanidou, V.; Athanasiou, L.; Christou, A.; et al. Risk Factors Associated with Community-Onset Infections Due to Multidrug-Resistant Organisms. Antibiotics 2025, 14, 1073. https://doi.org/10.3390/antibiotics14111073
Matzaras R, Biros D, Sakkou SF, Lymperatou D, Filippas-Ntekouan S, Prokopidou A, Konstantopoulou R, Samanidou V, Athanasiou L, Christou A, et al. Risk Factors Associated with Community-Onset Infections Due to Multidrug-Resistant Organisms. Antibiotics. 2025; 14(11):1073. https://doi.org/10.3390/antibiotics14111073
Chicago/Turabian StyleMatzaras, Rafail, Dimitrios Biros, Sissy Foteini Sakkou, Diamantina Lymperatou, Sempastian Filippas-Ntekouan, Anastasia Prokopidou, Revekka Konstantopoulou, Valentini Samanidou, Lazaros Athanasiou, Anastasia Christou, and et al. 2025. "Risk Factors Associated with Community-Onset Infections Due to Multidrug-Resistant Organisms" Antibiotics 14, no. 11: 1073. https://doi.org/10.3390/antibiotics14111073
APA StyleMatzaras, R., Biros, D., Sakkou, S. F., Lymperatou, D., Filippas-Ntekouan, S., Prokopidou, A., Konstantopoulou, R., Samanidou, V., Athanasiou, L., Christou, A., Adamidis, P.-S., Koutsogianni, A. D., Liamis, G., Milionis, H., Florentin, M., & Christaki, E. (2025). Risk Factors Associated with Community-Onset Infections Due to Multidrug-Resistant Organisms. Antibiotics, 14(11), 1073. https://doi.org/10.3390/antibiotics14111073








