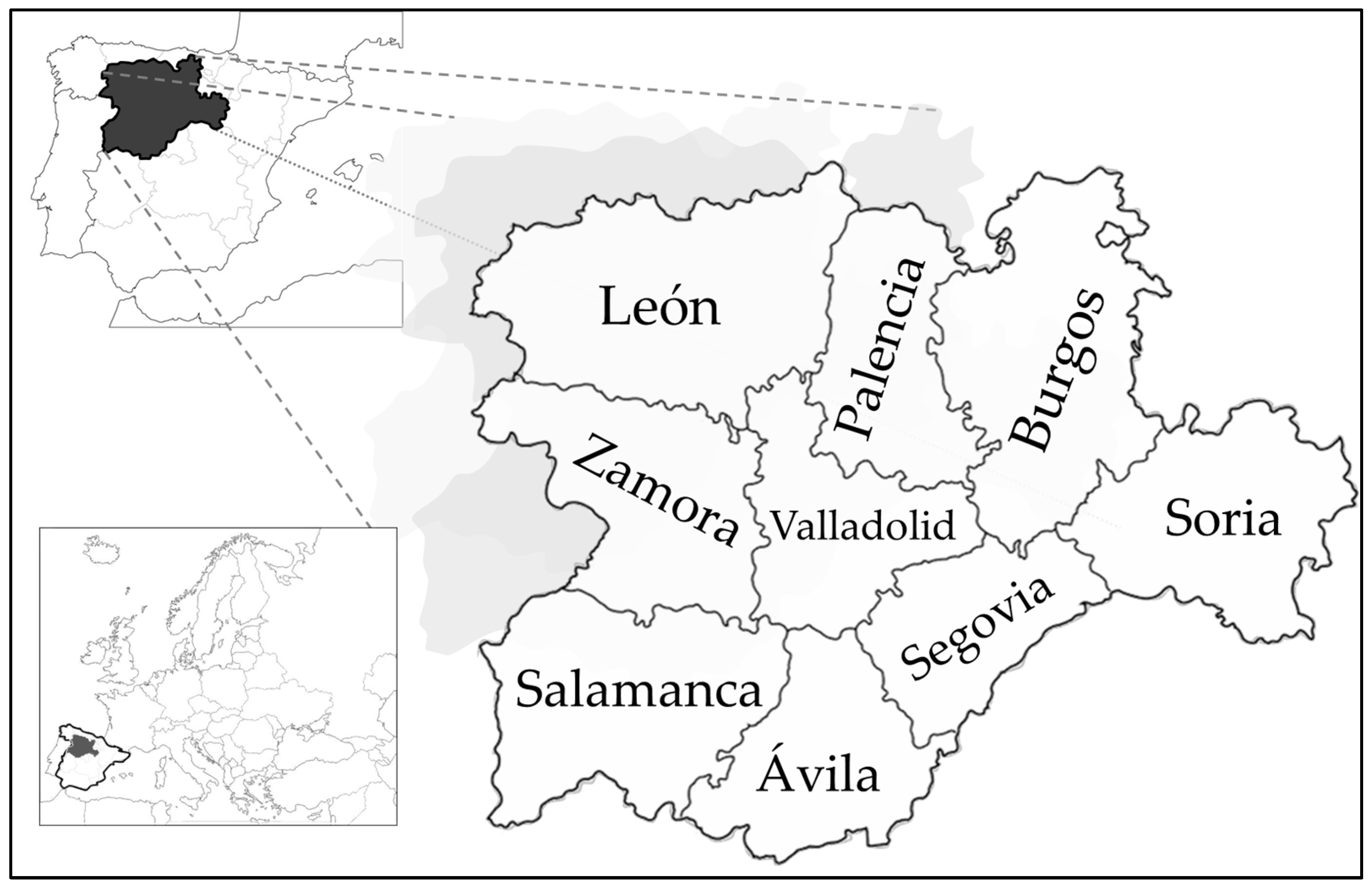
An Analysis of Primary Healthcare Antibiotic Prescription Rates Within Castile and Leon (Spain): 2013–2023
Abstract
1. Introduction
2. Results
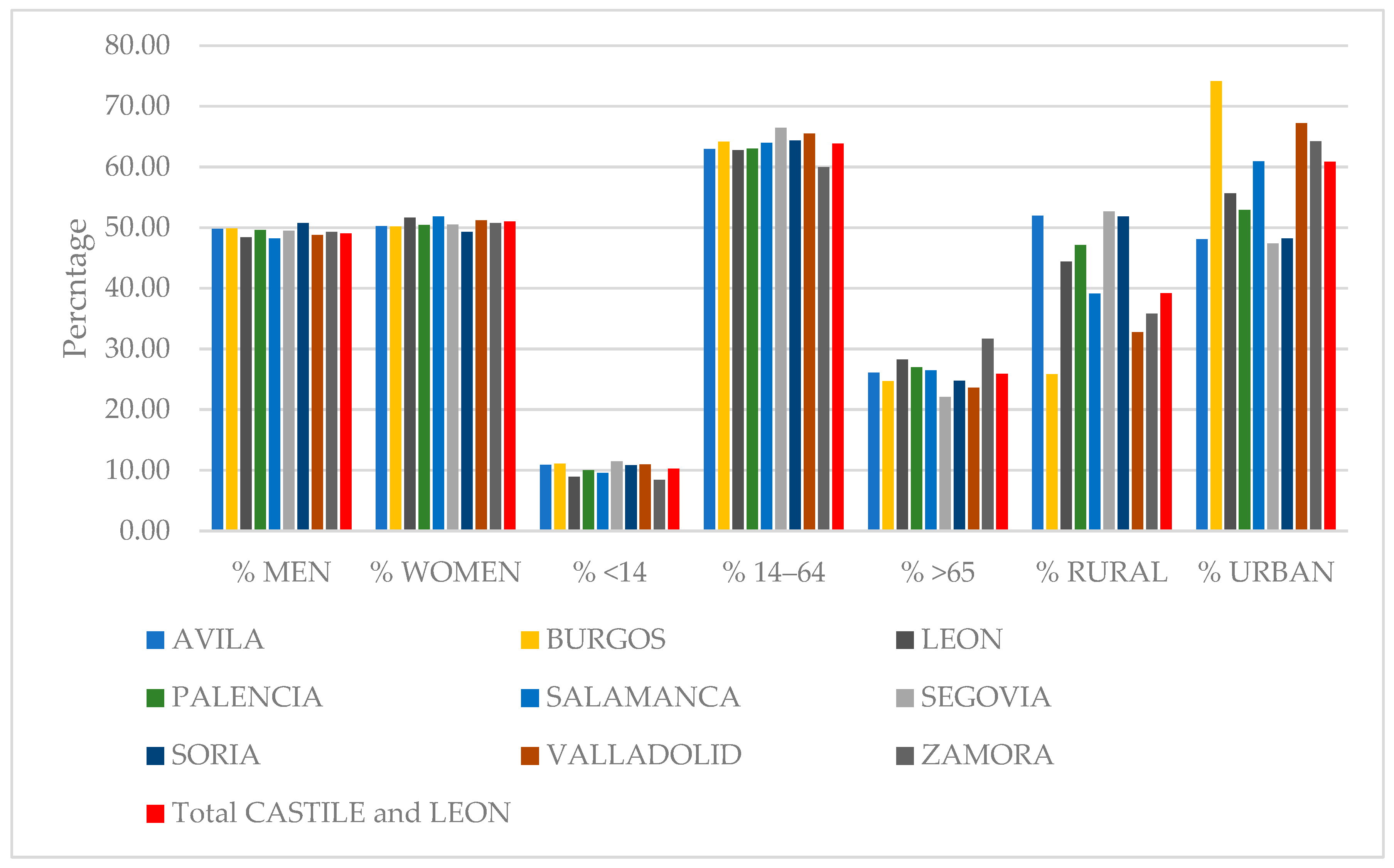
2.1. Descriptive Analysis of the Population Holding a Healthcare Card in Castile and Leon
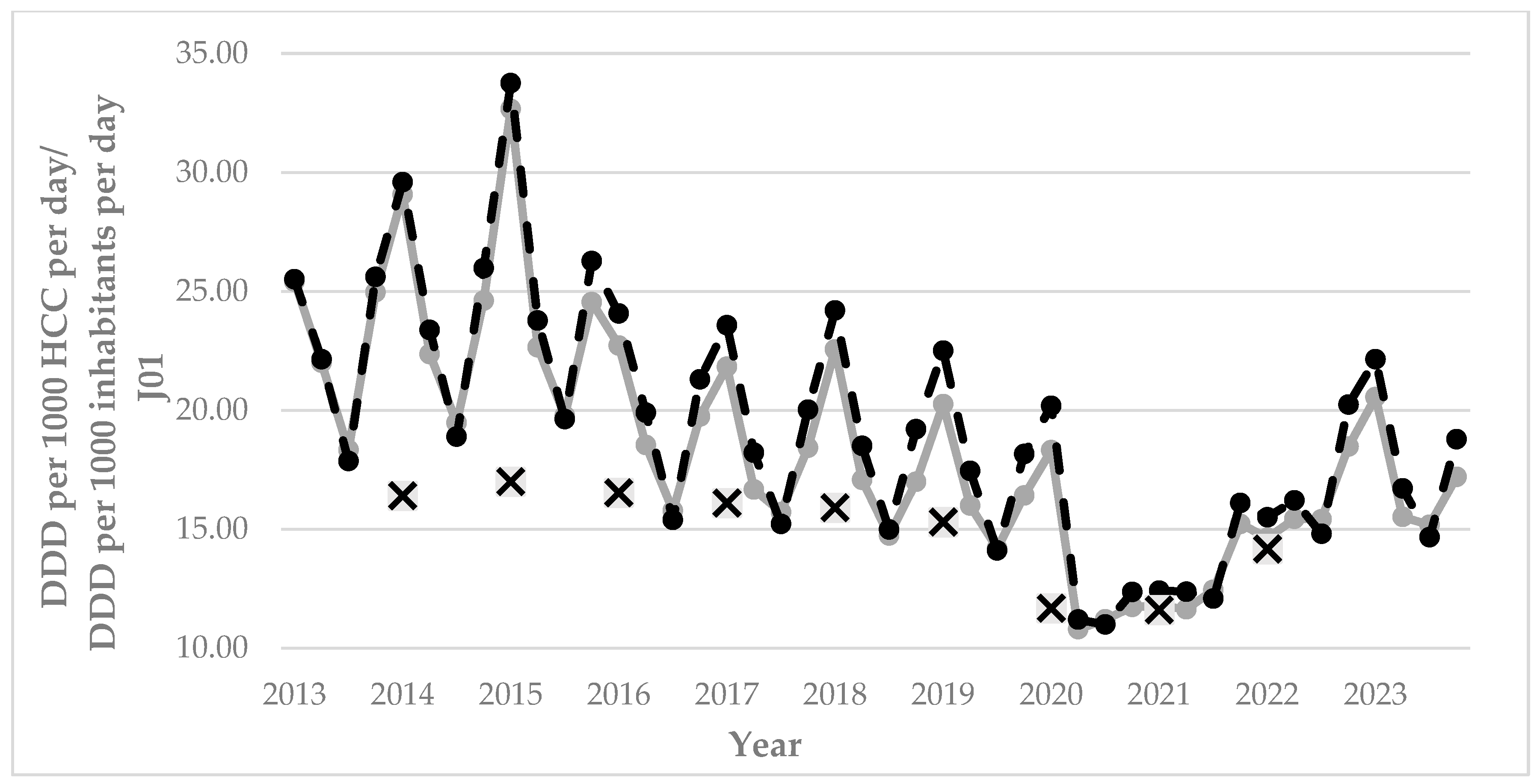
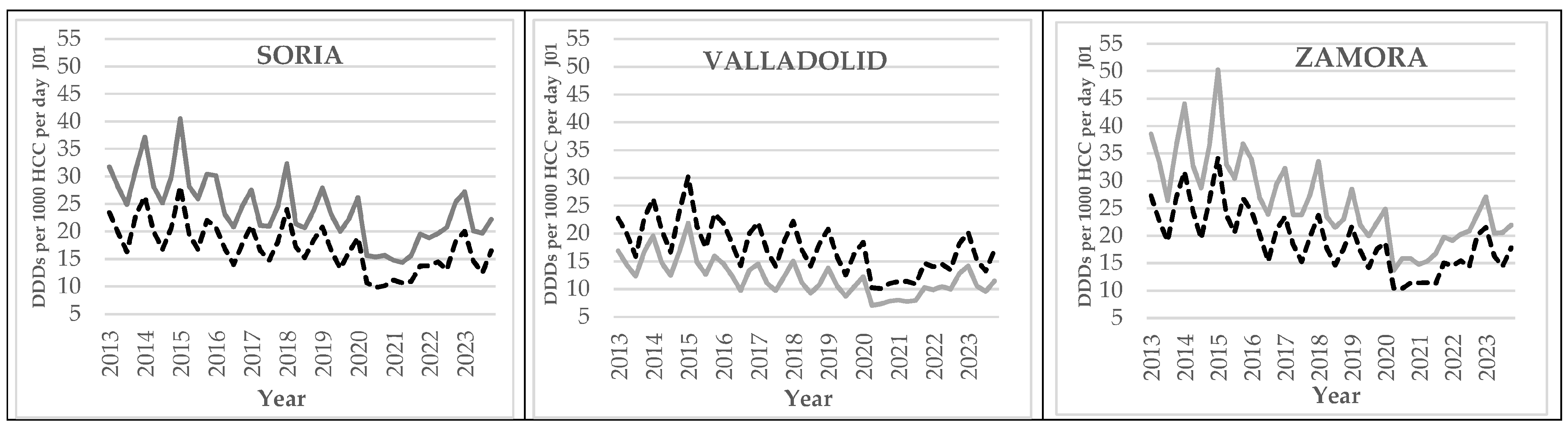
2.2. Prescriptions of Anti-Microbials for Systemic Use (J01): Seasonality, Urban–Rural Differences, and Outlier Provinces
2.3. Differences in Prescription Rates of Pharmacological Therapeutic Subgroups
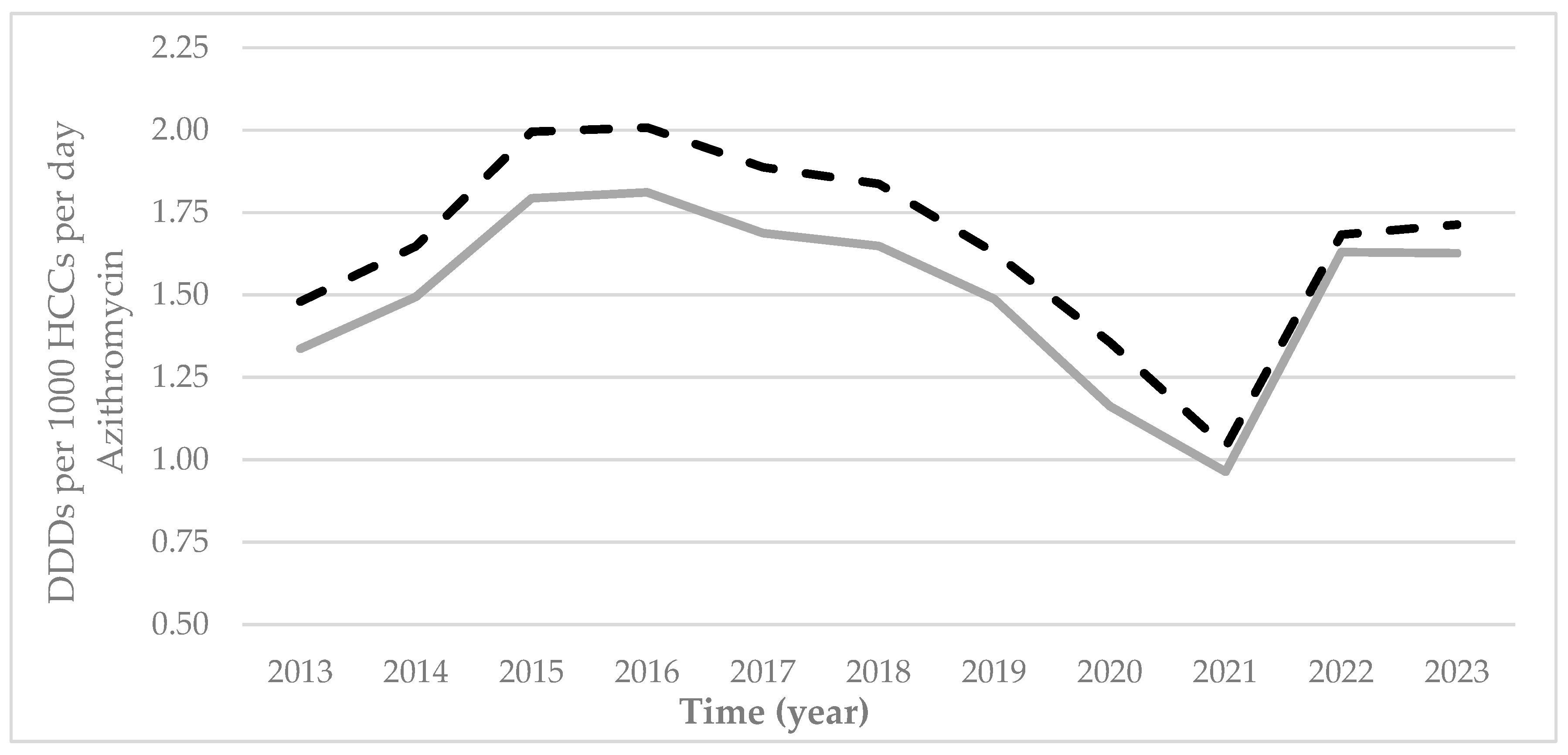
2.4. Prescription Rates of Azithromycin
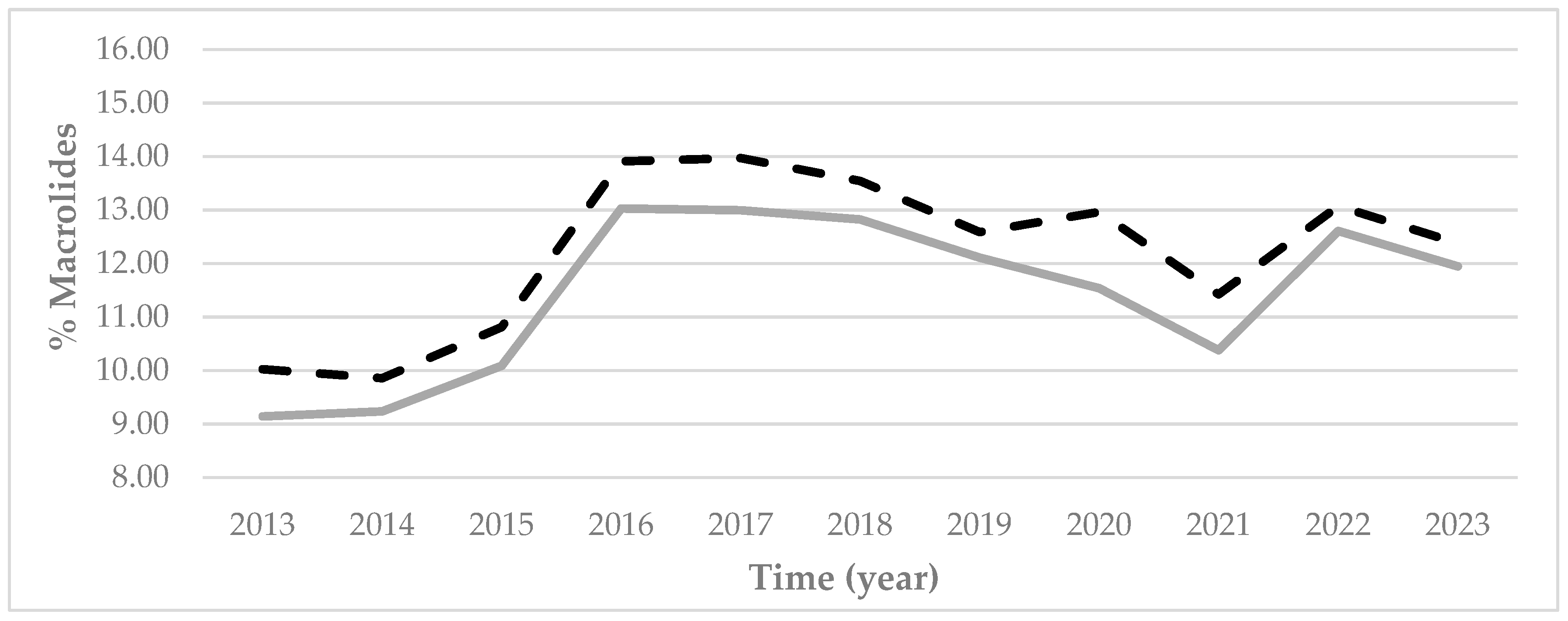
2.5. Qualitative Indicators (Choice of Antibiotic)
3. Discussion
Limitations of the Study and Future Lines of Work
4. Materials and Methods
- (1)
- The average number of HCCs in each province (by rural and urban) was calculated over 2013–2023.
- (2)
- The total was divided by 366 days for the calculations referring to leap years. A total of 91 days were used for the calculations, referring to the first quarter of each leap year.
- -
- -
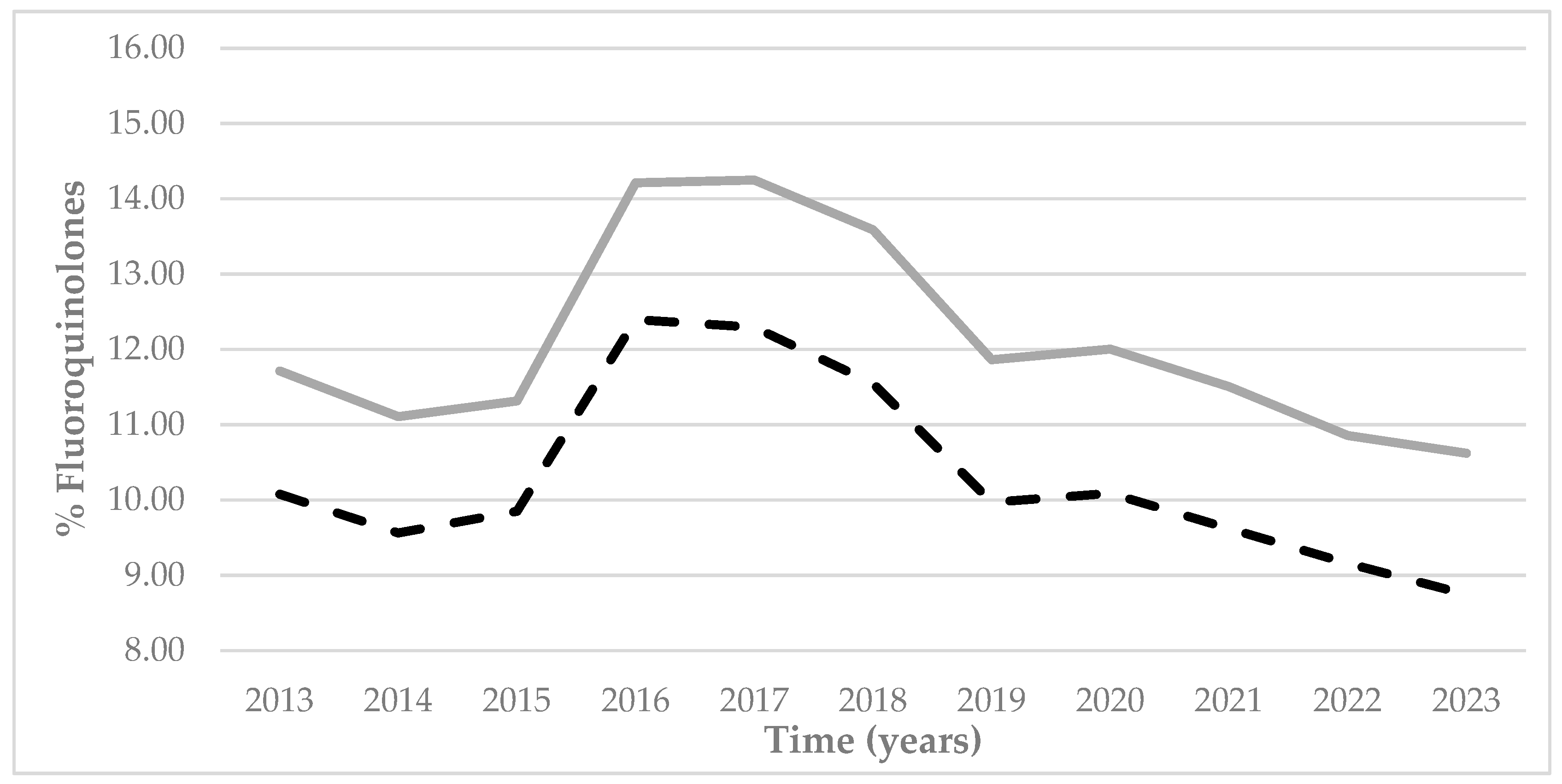
- Percentage DDDs of fluoroquinolones (J01MA). Fluoroquinolones are used to treat respiratory and urinary infections, although they are not included in front-line antibiotic treatment in primary healthcare. In view of the failure of front-line antibiotics, their use must be reduced to very specific cases due to the high levels of antibiotic resistance [25,26]. The following formula was used for its calculation:
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMR | Anti-Microbial Resistance |
| ATC | Anatomic, Therapeutic, Chemical |
| BHCs | Basic Health Centers |
| DDDs | Defined Daily Doses |
| HCC | Healthcare Card |
| J01 | Anti-Microbials for Systemic Use |
| PHC | Primary HealthCare |
| PRAN | Plan Nacional Frente a la Resistencia a los Antibióticos [National Plan to Combat Antibiotic Resistance] |
| WHO | World Health Organization |
References
- Werner, G.; Abu Sin, M. Antimicrobial Resistance Is Invisible. I Am Not. Eurosurveillance 2024, 29, 2400762. [Google Scholar] [CrossRef] [PubMed]
- Camacho-Silvas, L.A. Resistencia Bacteriana, Una Crisis Actual. Rev. Esp. Salud Publica 2023, 97, e202302013. [Google Scholar]
- Aslam, B.; Khurshid, M.; Arshad, M.I.; Muzammil, S.; Rasool, M.; Yasmeen, N.; Shah, T.; Chaudhry, T.H.; Rasool, M.H.; Shahid, A.; et al. Antibiotic Resistance: One Health One World Outlook. Front. Cell Infect. Microbiol. 2021, 11, 771510. [Google Scholar] [CrossRef]
- Naghavi, M.; Vollset, S.E.; Ikuta, K.S.; Swetschinski, L.R.; Gray, A.P.; Wool, E.E.; Robles Aguilar, G.; Mestrovic, T.; Smith, G.; Han, C.; et al. Global Burden of Bacterial Antimicrobial Resistance 1990–2021: A Systematic Analysis with Forecasts to 2050. Lancet 2024, 404, 1199–1226. [Google Scholar] [CrossRef]
- Menting, S.G.P.; Redican, E.; Murphy, J.; Bucholc, M. Primary Care Antibiotic Prescribing and Infection-Related Hospitalisation. Antibiotics 2023, 12, 1685. [Google Scholar] [CrossRef]
- Madden, J.; Outterson, K. Trends in the Global Antibiotics Market. Nat. Rev. Drug Discov. 2023, 22, 174. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control. Antimicrobial Consumption in the EU/EEA (ESAC-Net). Annual Epidemiological Report for 2023; European Centre for Disease Prevention and Control: Estocolmo, Sweden, 2024. [Google Scholar]
- Agencia Española de Medicamentos y Productos Sanitarios. Informe Anual 2024 Plan Nacional Frente a La Resistencia a Los Antibióticos; Agencia Española de Medicamentos y Productos Sanitarios: Madrid, Spain, 2025. [Google Scholar]
- Agencia Española de Medicamentos y Productos Sanitarios. Plan Estratégico 2022–2024 del Plan Nacional Frente a la Resistencia a los Antibióticos (PRAN); Agencia Española de Medicamentos y Productos Sanitarios: Madrid, Spain, 2022. [Google Scholar]
- Sánchez-Herrero, H.; Solaz-García, Á.; Pinilla-González, A.; Martínez-Sánchez, E.V.; Santágueda-Balader, P.; Cernada-Badía, M. Características Epidemiológicas Del Uso de Antimicrobianos En Atención Primaria En España: Un Estudio a Nivel Nacional. Rev. Esp. Quimioter. 2025, 38, 115–125. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística Índice de Envejecimiento. INE. Available online: https://ine.es/jaxiT3/Tabla.htm?t=1418 (accessed on 14 July 2025).
- Álvarez, M.; Eiros, J.M.; Pastor, E.; Sierra, E. Consumo de Antibióticos de Uso Sistémico En La Comunidad de Castilla y León. Med. Fam. SEMERGEN 2011, 37, 534–539. [Google Scholar] [CrossRef]
- Ministerio de Sanidad Consumo y Bienestar Social. Plan Nacional Frente a Las Resistencias Antibióticos (PRAN). Programas de Optimización de Uso de Antibióticos (PROA); Ministerio de Sanidad Consumo y Bienestar Social: Madrid, Spain, 2017. [Google Scholar]
- Llor, C. Uso Prudente de Antibióticos y Propuestas de Mejora Desde La Atención Primaria. Enferm. Infecc. Microbiol. Clin. 2010, 28, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Marcilla-Vázquez, C.; Ríos-Laorden, J.; Lloret-Callejo, Á.; Tejada-Cifuentes, F.; Tirado-Peláez, M.J.; Párraga-Martínez, I. Evolución de Prescripción Antibiótica En Atención Primaria Según Indicadores Del PRAN (Plan Nacional Frente a La Resistencia a Los Antibióticos). An Pediatr (Engl. Ed.) 2025, 102, 503840. [Google Scholar] [CrossRef]
- Fernández-Urrusuno, R.; Flores-Dorado, M.; Vilches-Arenas, A.; Serrano-Martino, C.; Corral-Baena, S.; Montero-Balosa, M.C. Adecuación de La Prescripción de Antibióticos En Un Área de Atención Primaria: Estudio Descriptivo Transversal. Enferm. Infecc. Microbiol. Clin. 2014, 32, 285–292. [Google Scholar] [CrossRef]
- Agencia Española de Medicamentos y Productos Sanitarios Consumos Antibióticos Sector Comunitario Por Comunidades Autónomas | PRAN. Available online: https://www.resistenciaantibioticos.es/es/lineas-de-accion/vigilancia/mapas-de-consumo/consumo-antibioticos-humana/consumos-antibioticos-extrahospitalarios-por-comunidades (accessed on 24 July 2025).
- Gonzalez-Zorn, B. Antibiotic Use in the COVID-19 Crisis in Spain. Clin. Microbiol. Infect. 2021, 27, 646–647. [Google Scholar] [CrossRef]
- Wang, J.; Li, F.; Chen, Z.; Guo, Y.; Liu, N.; Liu, B.; Xiao, S.; Yao, L.; Li, J.; Zhuo, C.; et al. Antibiotic Prescription Patterns for Acute Respiratory Infections in Rural Primary Healthcare Settings in Guangdong, China: Analysis of 162,742 Outpatient Prescriptions. Antibiotics 2023, 12, 297. [Google Scholar] [CrossRef] [PubMed]
- Base de Datos de Usuarios y Tarjeta Sanitaria de Sacyl Población de Tarjeta Sanitaria. Available online: https://www.saludcastillayleon.es/transparencia/es/transparencia/sanidad-cifras/informes-estadisticos/ordenacion-alfabetica/poblacion-tarjeta-sanitaria (accessed on 16 July 2025).
- Agencia Española de Medicamentos y Productos Sanitarios (AEMPS). Plan Estratégico y de Acción Para Reducir el Riesgo de Selección y Diseminación de la Resistencia a los Antibióticos; Agencia Española de Medicamentos y Productos Sanitarios (AEMPS): Madrid, Spain, 2014. [Google Scholar]
- Nicieza-García, M.L.; Pérez-Solís, P.; Gómez-de Oña, C.; Suárez-Gil, P.; Rolle-Sóñora, V.; Suárez-Mier, B. Consumo de Antibióticos En Atención Primaria En Población Adulta de Asturias Durante El Periodo 2014-2020. Aten Primaria 2022, 54, 102261. [Google Scholar] [CrossRef]
- Díaz, A.; Ochoa, C.; Brezmes, M.F.; López-Urrutia, L.; Rivas, N. Correlación Entre La Prescripción de Antibióticos y El Descenso de Las Resistencias a Antimicrobianos En El Área de Salud de Zamora. Enferm. Infecc. Microbiol. Clin. 2009, 27, 153–159. [Google Scholar] [CrossRef]
- Agencia Española de Medicamentos y Productos Sanitarios Plan Nacional Frente a La Resistencia a Los Antibióticos (PRAN) 2025-2027. Available online: https://resistenciaantibioticos.es/es/publicaciones/plan-nacional-frente-la-resistencia-los-antibioticos-pran-2025-2027 (accessed on 15 July 2025).
- Dirección Técnica de Asistencia Farmacéutica Gerencia Regional de Salud. Indicadores de Prescripción de Antibióticos; Agencia Española de Medicamentosy Productos Sanitarios (AEMPS): Madrid, Spain, 2018. [Google Scholar]
- Albañil, R.; Campos, J.; Cots, J.M.; Urrusuno, R.F.; de la Fuente, C.; García, A.; García, I.; Izquierdo, J.M.; Morros, R. Indicadores de Uso de Antibióticos En Atención Primaria; Agencia Española de Medicamentosy Productos Sanitarios (AEMPS): Madrid, Spain, 2017. [Google Scholar]
- García-Ortiz, A. Prescripción de Antibióticos En Atención Primaria. Available online: https://www.saludcastillayleon.es/portalmedicamento/fr/terapeutica/ojo-markov/prescripcion-antibioticos-atencion-primaria (accessed on 16 July 2025).
- World Health Organization. Anatomical Therapeutic Chemical (ATC) Classification. Available online: https://www.who.int/tools/atc-ddd-toolkit/atc-classification (accessed on 11 August 2025).
- Ripoll-Lozano, M.Á.; Jiménez-Arce, J.I.; Pedraza-Dueñas, A. Variabilidad En La Prescripción de Antibióticos En La Provincia de Ávila. Rev. Española Quimioter. 2007, 20, 44–50. [Google Scholar]
- Miguélez-Ferreiro, S.; Moreno-Sánchez, E.; Gutiérrez-de Antonio, M.; Hernando-Real, S. Antibiotic Prescribing and Changes in Antimicrobial Resistances in the Health Area of Segovia (Spain) during the Period between 2007 and 2011. Rev. Española Quimioter. 2014, 27, 28–35. [Google Scholar]
- García, E.P.; Eiros-Bouza, J.M.; Mayo-Iscar, A. Análisis de La Variabilidad Geográfica Del Consumo de Antibióticos de Uso Sistémico En La Provincia de Valladolid. Med. General 2002, 45, 473–480. [Google Scholar]
- Vázquez-Fernández, M.E.; Bachiller-Luque, M.R.; Vázquez-Fernández, M.J.; Pastor-García, E.; Eiros-Bouza, J.M. Variability in Antibiotic Prescription in the Pediatric Population of Castile and Leon (Spain) from 2001 to 2005 in Relation to Urban or Rural Setting. An Pediatr (Engl. Ed.) 2007, 67, 139–144. [Google Scholar] [CrossRef]
- Calle-Miguel, L.; Riaño, G.M.; Carbajo, A.I.I.; Álvarez, M.A.A.; Martínez, C.V.; Sánchez, G.S. Variabilidad Entre Áreas Sanitarias En El Consumo Extrahospitalario de Antibióticos de Uso Sistémico En La Población Pediátrica Del Principado de Asturias, España (2005-2018). Rev. Española Quimioter. 2021, 34, 107. [Google Scholar] [CrossRef]
- Catalina-Serna, M.; Ribes, E.; Real, J.; Galván, L.; Gascó, E.; Godoy, P. Alta Exposición a Antibióticos En La Población y Sus Diferencias Por Género y Edad. Aten. Primaria 2011, 43, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Malo, S.; Rabanaque, M.J.; Feja, C.; Lallana, M.J.; Aguilar, I.; Bjerrum, L. High Antibiotic Consumption: A Characterization of Heavy Users in Spain. Basic Clin. Pharmacol. Toxicol. 2014, 115, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Serna, M.C.; Real, J.; Ribes, E.; Marsal, J.R.; Godoy, P.; Galván, L. Factors Determining Antibiotic Prescription in Primary Care. Enferm. Infecc. Microbiol. Clin. 2011, 29, 193–200. [Google Scholar] [CrossRef]
- Lallana-Alvarez, M.J.; Feja-Solana, C.; Armesto-Gómez, J.; Bjerrum, L.; Rabanaque-Hernández, M.J. Outpatient Antibiotic Prescription in Aragón and the Differences by Gender and Age. Enferm. Infecc. Microbiol. Clin. 2012, 30, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Clark, A.W.; Durkin, M.J.; Olsen, M.A.; Keller, M.; Ma, Y.; O’Neil, C.A.; Butler, A.M. Rural-Urban Differences in Antibiotic Prescribing for Uncomplicated Urinary Tract Infection. Infect. Control Hosp. Epidemiol. 2021, 42, 1437–1444. [Google Scholar] [CrossRef]
- Brown, A.; Wong, J.R.; Kandiah, S.; Moore, J.; Quairoli, K. Inappropriate Fluoroquinolone Use in Academic and Non-Academic Primary Care Clinics. J. Gen. Intern. Med. 2019, 34, 2342–2344. [Google Scholar] [CrossRef]
- Sarría-Santamera, A.; Prado-Galbarro, J.; Ramallo-Farina, Y.; Quintana-Díaz, M.; Martínez-Virto, A.; Serrano-Aguilar, P. Utilización de Los Servicios de Urgencias En Zonas Rurales y Urbanas. Med. Familia. Semer. 2015, 41, 63–69. [Google Scholar] [CrossRef]
- Calle-Miguel, L.; Iglesias Carbajo, A.I.; Modroño Riaño, G.; Pérez Méndez, C.; García García, E.; Rodríguez Nebreda, S.; Solís Sánchez, G. Evolution of Antibiotic Consumption in Pediatric Outpatients of Asturias, Spain (2005–2018). An. Pediatr. (Engl. Ed.) 2021, 95, 438–447. [Google Scholar] [CrossRef]
- Vazquez-Cancela, O.; Souto-Lopez, L.; Vazquez-Lago, J.M.; Lopez, A.; Figueiras, A. Factors Determining Antibiotic Use in the General Population: A Qualitative Study in Spain. PLoS ONE 2021, 16, e0246506. [Google Scholar] [CrossRef]
- Nova, I.P. Enfermería Se Incorpora al Plan Nacional de Resistencia a Antibióticos. Redacción Médica 2020. Available online: https://www.redaccionmedica.com/secciones/ministerio-sanidad/enfermeria-se-incorpora-al-plan-nacional-de-resistencia-a-antibioticos-8330 (accessed on 25 July 2025).
- Ministerio de Sanidad, Seguridad Social e Inmigración. los Sistemas Sanitarios en los Países de la Unión Europea. Características e Indicadores de Salud 2019; Ministerio de Sanidad, Seguridad Social e Inmigración: Madrid, Spain, 2019. [Google Scholar]
- WHO Collaborating Centre for Drug Statistics Methodology ATC Classification Index with DDDs: Structure and Principles. Available online: https://www.whocc.no/atc/structure_and_principles/ (accessed on 12 August 2025).
- García Lobato, E.; Caro-Patón Carmona, T. Evidencia Disponible de Los Fármacos Utilizados En Pacientes Con COVID-19 (II): Hidroxicloroquina y Azitromicina. Available online: https://www.saludcastillayleon.es/portalmedicamento/en/terapeutica/ojo-markov/evidencia-disponible-farmacos-utilizados-pacientes-c-15a028 (accessed on 15 July 2025).
- Echeverría-Esnal, D.; Martin-Ontiyuelo, C.; Navarrete-Rouco, M.E.; De-Antonio Cuscó, M.; Ferrández, O.; Horcajada, J.P.; Grau, S. Azithromycin in the Treatment of COVID-19: A Review. Expert. Rev. Anti-Infect. Ther. 2021, 19, 147–163. [Google Scholar] [CrossRef]
- Consejería de Cultura y Bienestar Social. Decreto 32/1988 de 18 de Febrero, Por el que se Establece la Delimitación Territorial de las Zonas Básicas de Salud en el Territorio de la Comunidad Autónoma de Castilla y León; Consejería de Cultura y Bienestar Social: Valladolid, Spain, 1988. [Google Scholar]
- Elena, S.; Eva, C.L.; Germán, C.O. Changes Experienced in the Nutritional Pattern and in Some Health Habits by the Spanish Young Adult Population According to Place of Residence. J. Public Health 2025, 33, 1565–1574. [Google Scholar] [CrossRef]
- Gerencia Regional de Salud de Castilla y León. Informe Anual Del Sistema Nacional de Salud 2018. Estrategias y Acciones Destacables. Comunidad Autónoma de Castilla y León; Gerencia Regional de Salud de Castilla y León: Valladolid, Spain, 2020. [Google Scholar]
- Consejería de Sanidad. Dirección General de Salud Pública Estudio de Hábitos y Estilos de Vida en la Población Joven de Castilla y León; Consejería de Sanidad: Valladolid, Spain, 2023. [Google Scholar]




| 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spain | 109.9 | 112.6 | 114.7 | 116.3 | 118.4 | 120.6 | 123 | 125.8 | 129.2 | 133.6 | 137.3 | 142.4 |
| Castile and Leon | 179.4 | 182.9 | 185.4 | 188 | 191.2 | 194.5 | 198.3 | 202.3 | 205.7 | 212.9 | 217.2 | 223.9 |
| Year | AV | BU | LE | PA | SA | SE | SO | VA | ZA | C&L | C&L PRAN | ES |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2013 | 26.28 | 23.43 | 23.91 | 26.73 | 21.68 | 19.09 | 24.87 | 18.55 | 27.31 | 22.66 | ||
| 2014 | 28.24 | 25.47 | 25.12 | 28.16 | 23.11 | 20.50 | 25.60 | 19.80 | 29.00 | 24.13 | 18.94 | 16.42 |
| 2015 | 29.31 | 26.13 | 27.18 | 29.43 | 24.38 | 21.72 | 26.49 | 20.80 | 30.23 | 25.36 | 19.99 | 17.01 |
| 2016 | 22.53 | 20.39 | 21.14 | 21.85 | 19.00 | 16.58 | 21.10 | 16.57 | 23.16 | 19.71 | 19.86 | 16.54 |
| 2017 | 21.16 | 19.60 | 19.60 | 20.80 | 18.17 | 16.22 | 20.62 | 15.89 | 21.86 | 18.75 | 19.18 | 16.10 |
| 2018 | 20.63 | 19.90 | 19.21 | 20.44 | 18.12 | 16.35 | 21.62 | 15.75 | 20.80 | 18.59 | 19.11 | 15.91 |
| 2019 | 18.53 | 18.30 | 18.88 | 18.75 | 17.28 | 15.36 | 20.05 | 14.54 | 19.58 | 17.45 | 18.08 | 15.31 |
| 2020 | 14.27 | 14.32 | 14.27 | 13.87 | 13.47 | 12.18 | 15.31 | 11.13 | 14.40 | 13.36 | 13.80 | 11.68 |
| 2021 | 14.18 | 13.71 | 13.86 | 14.02 | 13.45 | 12.03 | 13.89 | 10.88 | 13.82 | 13.04 | 13.36 | 11.61 |
| 2022 | 17.60 | 17.11 | 17.69 | 17.34 | 16.84 | 14.55 | 18.08 | 13.61 | 17.84 | 16.39 | 16.70 | 14.17 |
| 2023 | 19.24 | 18.24 | 19.07 | 18.70 | 17.90 | 15.94 | 19.13 | 14.71 | 19.21 | 17.62 | n.a. | 15.26 |
| J01A | J01C | J01D | J01E | J01F | J01G | J01M | J01X | ||
|---|---|---|---|---|---|---|---|---|---|
| AVILA | R | 0.71 (±0.07) | 12.60 (±4.10) | 2.07 (±0.27) | 0.61 (±0.07) | 2.05 (±0.38) | 0.017 (±0.003) | 2.91 (±0.78) | 0.49 (±0.05) |
| U | 0.95 (±0.09) | 12.80 (±4.10) | 1.86 (±0.31) | 0.51 (±0.04) | 1.91 (±0.40) | 0.014 (±0.008) | 2.06 (±0.53) | 0.48 (±0.02) | |
| % DIF R-U | −25.76 | −1.57 | 11.10 | 20.26 | 7.17 | 28.13 | 41.03 | 3.42 | |
| BURGOS | R | 0.53(±0.05) | 11.84 (±3.80) | 2.24 (±0.31) | 0.40 (±0.09) | 2.55 (±0.32) | 0.004 (±0.003) | 2.41 (±0.63) | 0.59 (±0.06) |
| U | 0.73(±0.05) | 11.21 (±3.60) | 2.08 (±0.24) | 0.36 (±0.06) | 2.67 (±0.28) | 0.002 (±0.001) | 1.78 (±0.45) | 0.53 (±0.03) | |
| % DIF R-U | −27.24 | 5.57 | 7.52 | 11.69 | −4.56 | 82.15 | 35.00 | 12.81 | |
| LEON | R | 0.58 (±0.02) | 8.72 (±2.84) | 1.80 (±0.32) | 0.46 (±0.04) | 2.50 (±0.58) | 0.004 (±0.003) | 2.34 (±0.41) | 0.45 (±0.33) |
| U | 0.79 (±0.06) | 12.40 (±3.86) | 2.47 (±0.49) | 0.52 (±0.06) | 3.05 (±0.68) | 0.004 (±0.002) | 2.65 (±0.51) | 0.62 (±0.05) | |
| % DIF R-U | −38.95 | −29.59 | −26.90 | −10.50 | −18.18 | −9.52 | −12.04 | −26.57 | |
| PALENCIA | R | 0.68 (±0.06) | 12.11 (±4.48) | 1.49 (±0.32) | 0.33 (±0.03) | 1.86 (±0.32) | 0.003 (±0.001) | 1.95 (±0.44) | 0.54 (±0.06) |
| U | 0.85 (±0.07) | 14.31 (±5.10) | 1.77 (±0.33) | 0.40 (±0.06) | 2.53 (±0.37) | 0.005 (±0.002) | 2.09 (±0.42) | 0.64 (±0.07) | |
| % DIF R-U | −19.29 | −15.39 | −15.64 | −16.93 | −26.29 | −36.29 | −6.51 | −16.09 | |
| SALAMANCA | R | 0.48 (±0.05) | 10.73 (±3.38) | 2.47 (±0.46) | 0.51 (±0.10) | 2.39 (±0.44) | 0.007 (±0.001) | 2.40 (±0.56) | 0.52 (±0.09) |
| U | 0.59 (±0.07) | 9.73 (±2.92) | 2.27 (±0.33) | 0.61 (±0.09) | 2.26 (±0.41) | 0.006 (±0.002) | 1.81 (±0.47) | 0.59 (±0.06) | |
| % DIF R-U | −17.94 | 10.25 | 9.14 | −15.75 | 6.06 | 18.59 | 32.46 | −11.76 | |
| SEGOVIA | R | 0.77 (±0.05) | 10.95 (±3.15) | 1.90 (±0.16) | 0.34 (±0.06) | 1.57 (±0.26) | 0.004 (±0.002) | 1.94 (±0.45) | 0.42 (±0.05) |
| U | 0.78 (±0.10) | 8.90 (±2.49) | 1.56 (±0.12) | 0.28 (±0.06) | 1.42 (±0.22) | 0.002 (±0.002) | 1.39 (±0.34) | 0.36 (±0.03) | |
| % DIF R-U | −1.03 | 23.04 | 21.69 | 21.92 | 10.97 | 94.96 | 39.81 | 15.53 | |
| SORIA | R | 0.62 (±0.06) | 13.24 (±4.07) | 4.14 (±0.48) | 0.40 (±0.08) | 2.62 (±0.35) | 0.018 (±0.004) | 2.14 (±0.51) | 0.72 (±0.03) |
| U | 0.69 (±0.05) | 8.87 (±2.66) | 3.14 (±0.53) | 0.36 (±0.07) | 1.88 (±0.30) | 0.015 (±0.003) | 1.54 (±0.44) | 0.55 (±0.05) | |
| % DIF R-U | −10.22 | 49.24 | 31.94 | 11.50 | 39.60 | 21.34 | 39.05 | 31.06 | |
| VALLADOLID | R | 0.49 (±0.08) | 7.06 (±2.26) | 1.05 (±0.19) | 0.26 (±0.04) | 1.41 (±0.29) | 0.003 (±0.001) | 1.44 (±0.36) | 0.36 (±0.05) |
| U | 1.02 (±0.08) | 9.73 (±2.96) | 1.59 (±0.29) | 0.41 (±0.06) | 2.21 (±0.49) | 0.003 (±0.001) | 1.87 (±0.49) | 0.52 (±0.05) | |
| % DIF R-U | −52.08 | −27.40 | −33.94 | −37.76 | −36.40 | 11.27 | −23.28 | −30.61 | |
| ZAMORA | R | 0.70 (±0.07) | 14.86 (±5.72) | 3.31 (±0.43) | 0.70 (±0.17) | 2.67 (±0.49) | 0.008 (±0.004) | 3.24 (±0.94) | 0.59 (±0.05) |
| U | 0.74 (±0.07) | 10.81 (±3.92) | 2.18 (±0.23) | 0.47 (±0.07) | 2.28 (±0.42) | 0.010 (±0.007) | 2.01 (±0.59) | 0.48 (±0.02) | |
| % DIF R-U | −5.81 | 37.46 | 51.68 | 47.10 | 16.85 | −22.28 | 61.13 | 22.60 | |
| CASTILE & LEON | R | 0.57 (±0.03) | 10.41 (±3.40) | 2.02 (±0.26) | 0.43 (±0.05) | 2.14 (±0.37) | 0.006 (±0.001) | 2.22 (±0.51) | 0.49 (±0.04) |
| U | 0.81 (±0.05) | 10.90 (±3.44) | 2.04 (±0.28) | 0.45 (±0.06) | 2.41 (±0.40) | 0.005 (±0.002) | 1.98 (±0.48) | 0.54 (±0.03) | |
| % DIF R-U | −29.87 | −4.45 | −0.96 | −4.23 | −11.24 | 27.69 | 11.99 | −9.99 | |
| DDDs Per 1000 HCCs Per Day RURAL | DDDs Per 1000 HCCs Per Day URBAN | % DIF R-U | |
|---|---|---|---|
| ÁVILA | 1.419 (±0.295) | 1.194 (±0.280) | 18.768 |
| BURGOS | 1.934 (±0.263) | 1.961 (±0.251) | −1.371 |
| LEÓN | 1.942 (±0.425) | 2.354 (±0.499) | −17.502 |
| PALENCIA | 1.149 (±0.239) | 1.432 (±0.268) | −19.782 |
| SALAMANCA | 1.757 (±0.342) | 1.508 (±0.294) | 16.485 |
| SEGOVIA | 0.879 (±0.176) | 0.714 (±0.141) | 23.135 |
| SORIA | 1.801 (±0.275) | 1.235 (±0.222) | 45.823 |
| VALLADOLID | 0.909 (±0.181) | 1.439 (±0.320) | −36.823 |
| ZAMORA | 1.830 (±0.334) | 1.618 (±0.359) | 13.040 |
| CASTILE and LEON | 1.513 (±0.264) | 1.661 (±0.289) | −8.937 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salvador Martín, R.; Sierra-Medina, M.J.; Sánchez-Gutiérrez, M.E.; Rodríguez Vázquez, B.; Gallego-Ausín, N.; Azofra Casado, L.; Machín Morón, M.Á.; Serrano-Gómez, D. An Analysis of Primary Healthcare Antibiotic Prescription Rates Within Castile and Leon (Spain): 2013–2023. Antibiotics 2025, 14, 1070. https://doi.org/10.3390/antibiotics14111070
Salvador Martín R, Sierra-Medina MJ, Sánchez-Gutiérrez ME, Rodríguez Vázquez B, Gallego-Ausín N, Azofra Casado L, Machín Morón MÁ, Serrano-Gómez D. An Analysis of Primary Healthcare Antibiotic Prescription Rates Within Castile and Leon (Spain): 2013–2023. Antibiotics. 2025; 14(11):1070. https://doi.org/10.3390/antibiotics14111070
Chicago/Turabian StyleSalvador Martín, Rocío, María José Sierra-Medina, María Elena Sánchez-Gutiérrez, Bárbara Rodríguez Vázquez, Noelia Gallego-Ausín, Laura Azofra Casado, Mª Ángeles Machín Morón, and Diego Serrano-Gómez. 2025. "An Analysis of Primary Healthcare Antibiotic Prescription Rates Within Castile and Leon (Spain): 2013–2023" Antibiotics 14, no. 11: 1070. https://doi.org/10.3390/antibiotics14111070
APA StyleSalvador Martín, R., Sierra-Medina, M. J., Sánchez-Gutiérrez, M. E., Rodríguez Vázquez, B., Gallego-Ausín, N., Azofra Casado, L., Machín Morón, M. Á., & Serrano-Gómez, D. (2025). An Analysis of Primary Healthcare Antibiotic Prescription Rates Within Castile and Leon (Spain): 2013–2023. Antibiotics, 14(11), 1070. https://doi.org/10.3390/antibiotics14111070






