Antimicrobial Resistance Profile, Whole-Genome Sequencing and Core Genome Multilocus Sequence Typing of B. anthracis Isolates in Croatia from 2001 to 2022
Abstract
1. Introduction
2. Results
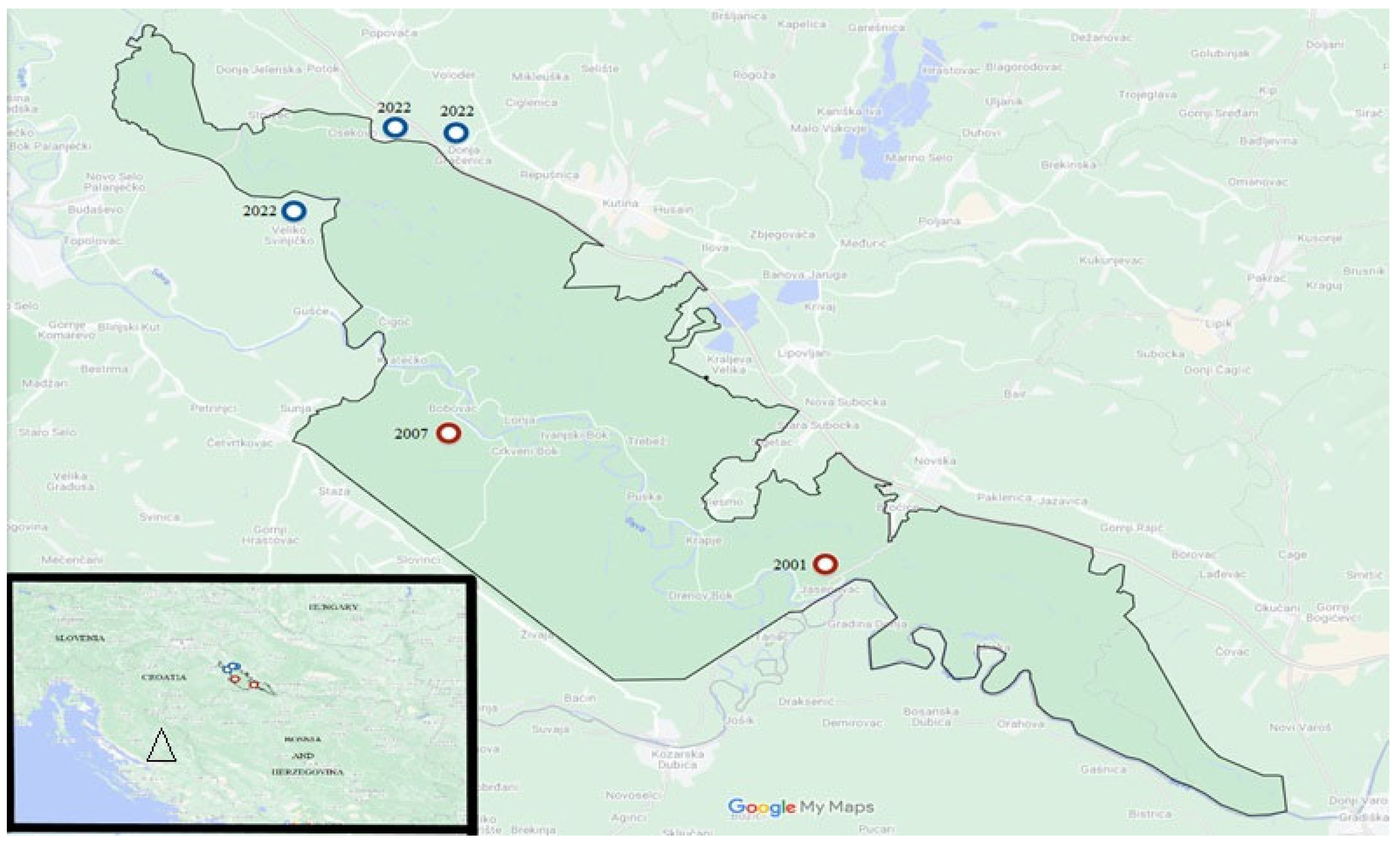
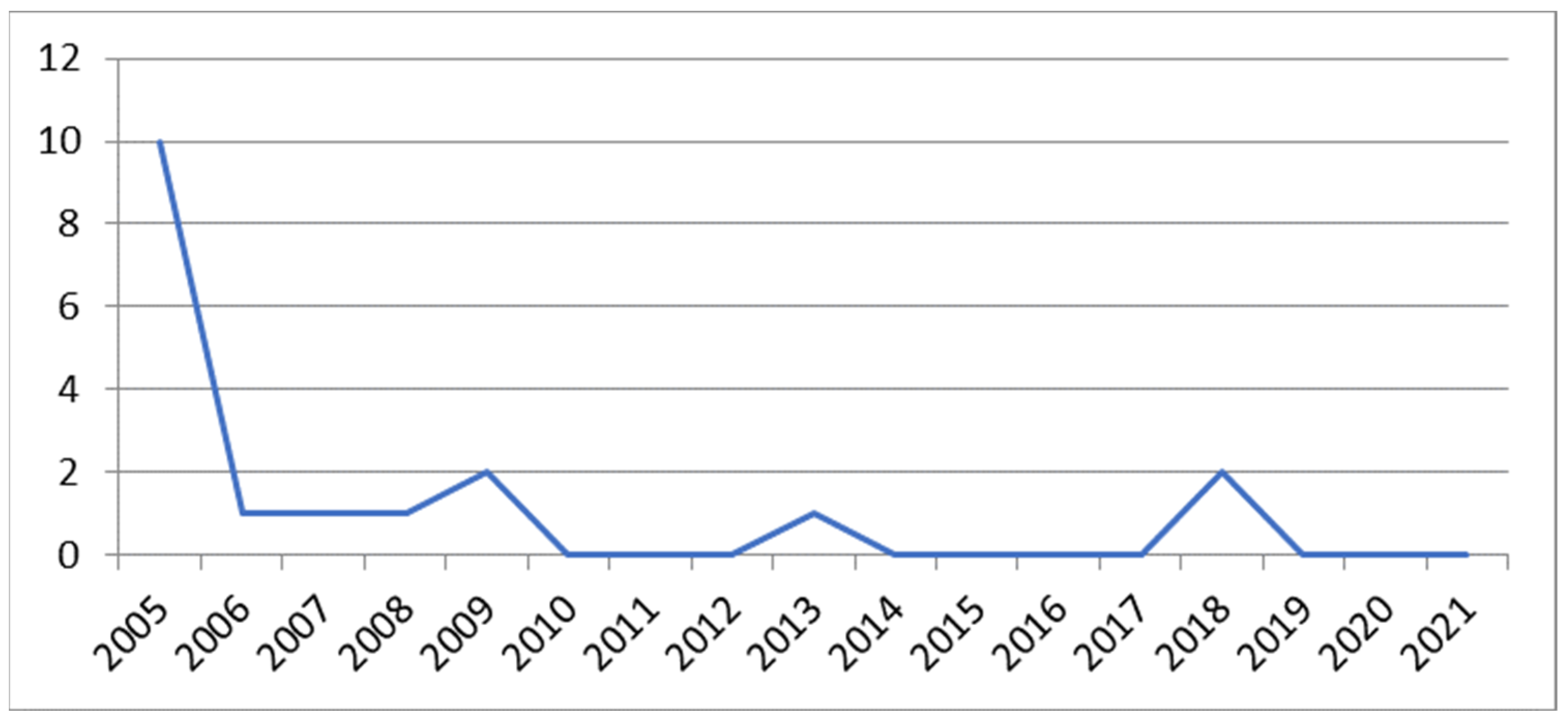
2.1. Isolates
2.2. Antimicrobial Susceptibility
2.3. WGS and Bioinformatic Analysis
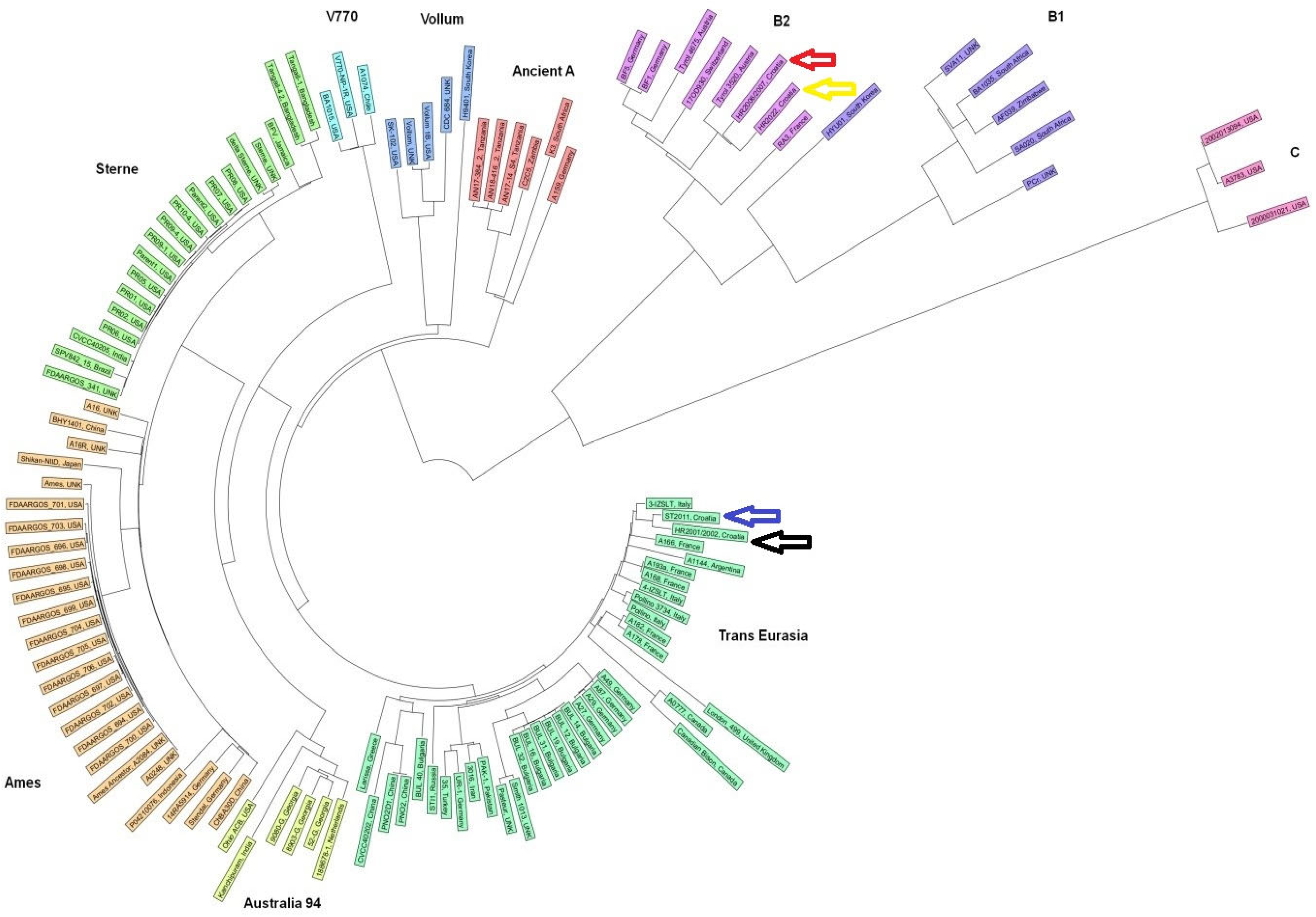
2.4. Core-Genome-Based Multilocus Sequence Typing (cgMLST)
3. Discussion
4. Materials and Methods
4.1. Epidemiological Investigation
4.2. Laboratory Diagnosis
4.3. Isolates Used in This Study
4.4. Antimicrobial Susceptibility Testing
4.5. Whole-Genome Sequencing (WGS) and De Novo Assembly
4.6. Bioinformatic Analysis of Antimicrobial Resistance and Virulence Genes
4.7. Core-Genome-Based Multilocus Sequence Typing (cgMLST)
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Liu, Y.; Lai, Q.; Göker, M.; Meier-Kolthoff, J.P.; Wang, M.; Sun, Y.; Wang, L.; Shao, Z. Genomic insights into the taxonomic status of the Bacillus cereus group. Sci. Rep. 2015, 5, 14082. [Google Scholar] [CrossRef] [PubMed]
- Swartz, M.N. Recognition and management of anthrax—An update. N. Engl. J. Med. 2001, 345, 1621–1626. [Google Scholar] [CrossRef] [PubMed]
- McKendrick, D.R. Anthrax and its transmission to humans. Cent. Afr. J. Med. 1980, 26, 126–129. [Google Scholar] [PubMed]
- Kiple, K.F. The Cambridge World History of Human Disease; Cambridge University Press: Cambridge, UK, 1993. [Google Scholar]
- Ringertz, S.H.; Høiby, E.A.; Jensenius, M.; Maehlen, J.; Caugant, D.A.; Myklebust, A.; Fossum, K. Injectional anthrax in a heroin skin-popper. Lancet 2000, 356, 1574–1575. [Google Scholar] [CrossRef] [PubMed]
- Jernigan, J.A.; Stephens, D.S.; Ashford, D.A.; Omenaca, C.; Topiel, M.S.; Galbraith, M.; Tapper, M.; Fisk, T.L.; Zaki, S.; Popovic, T.; et al. Anthrax Bioterrorism Investigation Team. Bioterrorism-related inhalational anthrax: The first 10 cases reported in the United States. Emerg. Infect Dis. 2001, 7, 933–944. [Google Scholar] [CrossRef] [PubMed]
- Fowler, R.A.; Shafazand, S. Anthrax Bioterrorism: Prevention, Diagnosis and Management Strategies. J. Bioterr. Biodef. 2011, 2, 107. [Google Scholar] [CrossRef]
- World Health Organization; Food and Agriculture Organization of the United Nations; World Organisation for Animal Health. Anthrax in Humans and Animals; WHO: Geneva, Switzerland, 2008; Available online: https://apps.who.int/iris/handle/10665/97503 (accessed on 20 March 2024).
- Jacotot, H.; Virat, B. Long duration of viability of spores of Bacillus anthracis. Ann. Inst. Pasteur 1954, 87, 215–217. [Google Scholar]
- Wilson, J.B.; Russell, K.E. Isolation of Bacillus anthracis from soil stored 60 years. J. Bacteriol. 1964, 87, 237–238. [Google Scholar] [CrossRef] [PubMed]
- De Vos, V. The ecology of anthrax in the Kruger National Park, South Africa. Salisbury Med. Bull. 1990, 68S, 19–23. [Google Scholar]
- Sterne, M. The effects of different carbon dioxide concentrations on the growth of virulent anthrax strains. Pathogenicity and immunity tests on guinea pigs and sheep with anthrax variants derived from virulent strains. Onderstepoort J. Vet. Sci. Anim. Ind. 1937, 9, 49–67. [Google Scholar]
- Sterne, M. The use of anthrax vaccines prepared from avirulent (uncapsulated) variants of Bacillus anthracis. Onderstepoort J. Vet. Sci. Anim. Ind. 1939, 13, 307–312. [Google Scholar]
- Mikesell, P.; Ivins, B.E.; Ristroph, J.D.; Dreier, T.M. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect. Immun. 1983, 39, 371–376. [Google Scholar] [CrossRef]
- Okinaka, R.; Cloud, K.; Hampton, O.; Hoffmaster, A.; Hill, K.; Keim, P.; Koehler, T.; Lamke, G.; Kumano, S.; Manter, D.; et al. Sequence, assembly and analysis of pX01 and pX02. J. Appl. Microbiol. 1999, 87, 261–262. [Google Scholar] [CrossRef] [PubMed]
- Young, J.A.; Collier, R.J. Anthrax toxin: Receptor binding, internalization, pore formation, and translocation. Annu. Rev. Biochem. 2007, 76, 243–265. [Google Scholar] [CrossRef]
- Candela, T.; Fouet, A. Poly-gamma-glutamate in bacteria. Mol. Microbiol. 2006, 60, 1091–1098. [Google Scholar] [CrossRef]
- Green, B.D.; Battisti, L.; Koehler, T.M.; Thorne, C.B.; Ivins, B.E. Demonstration of a capsule plasmid in Bacillus anthracis. Infect. Immun. 1985, 49, 291–297. [Google Scholar] [CrossRef]
- Henderson, I.; Duggleby, C.J.; Turnbull, P.C. Differentiation of Bacillus anthracis from other Bacillus cereus group bacteria with the PCR. Int. J. Syst. Bacteriol. 1994, 44, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Klee, S.R.; Ozel, M.; Appel, B.; Boesch, C.; Ellerbrok, H.; Jacob, D.; Holland, G.; Leendertz, F.H.; Pauli, G.; Grunow, R.; et al. Characterization of Bacillus anthracis-like bacteria isolated from wild great apes from Cote d’Ivoire and Cameroon. J. Bacteriol. 2006, 188, 5333–5344. [Google Scholar] [CrossRef] [PubMed]
- Rasko, D.A.; Rosovitz, M.J.; Økstad, O.A.; Fouts, D.E.; Jiang, L.; Cer, R.Z.; Kolstø, A.B.; Gill, S.R.; Ravel, J. Complete sequence analysis of novel plasmids from emetic and periodontal Bacillus cereus isolates reveals a common evolutionary history among the B. cereus-group plasmids, including Bacillus anthracis pXO1. J. Bacteriol. 2007, 189, 52–64. [Google Scholar] [CrossRef]
- Van der Auwera, G.A.; Andrup, L.; Mahillon, J. Conjugative plasmid pAW63 brings new insights into the genesis of the Bacillus anthracis virulence plasmid pXO2 and of the Bacillus thuringiensis plasmid pBT9727. BMC Genom. 2005, 6, 103. [Google Scholar] [CrossRef]
- Keim, P.; Price, L.B.; Klevytska, A.M.; Smith, K.L.; Schupp, J.M.; Okinaka, R.; Jackson, P.J.; Hugh-Jones, M.E. Multiple-locus variable-number tandem repeat analysis reveals genetic relationships within Bacillus anthracis. J. Bacteriol. 2000, 182, 2928–2936. [Google Scholar] [CrossRef] [PubMed]
- Keim, P.; Gruendike, J.M.; Klevytska, A.M.; Schupp, J.M.; Challacombe, J.; Okinaka, R. The genome and variation of Bacillus anthracis. Mol. Aspects Med. 2009, 30, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Kolstø, A.B.; Tourasse, N.J.; Økstad, O.A. What sets Bacillus anthracis apart from other Bacillus species? Annu. Rev. Microbiol. 2009, 63, 451–476. [Google Scholar] [CrossRef] [PubMed]
- Andersen, G.L.; Simchock, J.M.; Wilson, K.H. Identification of a region of genetic variability among Bacillus anthracis strains and related species. J. Bacteriol. 1996, 178, 377–384. [Google Scholar] [CrossRef]
- Van Ert, M.N.; Easterday, W.R.; Huynh, L.Y.; Okinaka, R.T.; Hugh-Jones, M.E.; Ravel, J.; Zanecki, S.R.; Pearson, T.; Simonson, T.S.; U’Ren, J.M.; et al. Global genetic population structure of Bacillus anthracis. PLoS ONE 2007, 2, e461. [Google Scholar] [CrossRef] [PubMed]
- Thierry, S.; Tourterel, C.; Le Flèche, P.; Derzelle, S.; Dekhil, N.; Mendy, C.; Colaneri, C.; Vergnaud, G.; Madani, N. Genotyping of French Bacillus anthracis strains based on 31-loci multi locus VNTR analysis: Epidemiology, marker evaluation, and update of the internet genotype database. PLoS ONE 2014, 9, e95131. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Glil, M.Y.; Chiaverini, A.; Garofolo, G.; Fasanella, A.; Parisi, A.; Harmsen, D.; Jolley, K.A.; Elschner, M.C.; Tomaso, H.; Linde, J.; et al. A Whole-Genome-Based Gene-by-Gene Typing System for Standardized High-Resolution Strain Typing of Bacillus anthracis. J. Clin. Microbiol. 2021, 59, e0288920. [Google Scholar] [CrossRef] [PubMed]
- Sahl, J.W.; Pearson, T.; Okinaka, R.; Schupp, J.M.; Gillece, J.D.; Heaton, H.; Birdsell, D.; Hepp, C.; Fofanov, V.; Noseda, R.; et al. A Bacillus anthracis Genome Sequence from the Sverdlovsk 1979 Autopsy Specimens. mBio 2016, 7, e01501-16. [Google Scholar] [CrossRef] [PubMed]
- Habrun, B.; Račić, I.; Kompes, G.; Špičić, S.; Benić, M.; Mihaljević, Ž.; Cvetnić, Ž. The antimicrobial susceptibility and virulence factors of Bacillus anthracis strains isolated in Croatia. Vet. Med. 2011, 56, 22–27. [Google Scholar] [CrossRef]
- Ministry of Agriculture of the Republic of Croatia. Available online: http://www.veterinarstvo.hr/default.aspx?id=185 (accessed on 7 July 2024).
- Šoštarić, B.; Habrun, B.; Lipej, Z.; Vicković, I. Prikaz Epizootije Bedrenice u Stadu Ovaca i Koza. Veterinarski Dani, Zagreb, Hrvatska, 17.10.2002–20.10.2002; Hrvatska veterinarska komora: Zagreb, Croatia, 2002; pp. 31–32. [Google Scholar]
- Habrun, B.; Kompes, G.; Šeol, B. Anthrax—Epizootic case in Bobovac (Sunja). Vet. Stanica 2009, 40, 381–388. [Google Scholar]
- Miškić, T.; Lohman Janković, I. Epizootiološke Značajke Bedrenice na Području Parka Prirode Lonjsko Polje 2022. Sažetci, BEDRENICA I AFRIČKA SVINJSKA KUGA U HRVATSKOJ, Zagreb, Hrvatska, 13.10.2023; Hrvatska Akademija Znanosti i Umjetnosti: Zagreb, Croatia, 2023; ISBN 978-953-347-371-0. Available online: https://www.info.hazu.hr/wp-content/uploads/2023/10/2023-HAZU-Zbornik-sazetaka-Bedrenica-i-africka-svinjska-kuga.pdf (accessed on 20 March 2024).
- Schmid, G.; Kaufmann, A. Anthrax in Europe: Its epidemiology, clinical characteristics, and role in bioterrorism. Clin. Microbiol. Infect. 2002, 8, 479–488. [Google Scholar] [CrossRef] [PubMed]
- Nicastri, E.; Vairo, F.; Mencarini, P.; Battisti, A.; Agrati, C.; Cimini, E.; Carrara, S.; D’Arezzo, S.; Adone, R.; Vulcano, A.; et al. Unexpected human cases of cutaneous anthrax in Latium region, Italy, August 2017: Integrated human-animal investigation of epidemiological, clinical, microbiological and ecological factors. Euro Surveill. 2019, 24, 1800685. [Google Scholar] [CrossRef] [PubMed]
- Hodnik, J.J.; Knific, T.; Starič, J.; Toplak, I.; Ocepek, M.; Hostnik, P.; Ježek, J. Overview of Slovenian Control Programmes for Cattle Diseases Not Regulated by the European Union. Front. Vet. Sci. 2021, 8, 674515, Erratum in Front. Vet. Sci. 2022, 8, 835395. [Google Scholar] [CrossRef] [PubMed]
- Orlos, Z.; Rakoczi, E.; Misak, O.; Lenart, B.; Ocsai, G.; Kovacs, I.; Gorzsas, S.; Kardos, L.; Lampe, Z.; Szilvassy, Z.; et al. Outbreak of anthrax in adults and adolescents: A review of nine cases in a regional teaching hospital in East Hungary. Clin. Microbiol. Infect. 2017, 23, 52–54. [Google Scholar] [CrossRef] [PubMed]
- Arapović, J.; Skočibusić, S.; Jelavić, B.; Ivanković, H.B.; Jurić, M.; Mamić, D.; Grgić, S.; Lesko, J.; Leventić, M.; Soldo, I.; et al. Two cases of human cutaneous anthrax in Bosnia and Herzegovina, September 2014. Euro Surveill. 2015, 20, 2–4. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bower, W.A.; Yu, Y.; Person, M.K.; Parker, C.M.; Kennedy, J.L.; Sue, D.; Hesse, E.M.; Cook, R.; Bradley, J.; Bulitta, J.B.; et al. CDC Guidelines for the Prevention and Treatment of Anthrax 2023. MMWR Recomm Rep. 2023, 72, 1–47. [Google Scholar] [CrossRef]
- Severn, M. A fatal case of pulmonary anthrax. Br. Med. J. 1976, 27, 748. [Google Scholar] [CrossRef]
- Cavallo, J.D.; Ramisse, F.; Girardet, M.; Vaissaire, J.; Mock, M.; Hernandez, E. Antibiotic susceptibilities of 96 isolates of Bacillus anthracis isolated in France between 1994 and 2000. Antimicrob. Agents Chemother. 2002, 46, 2307–2309. [Google Scholar] [CrossRef]
- Maxson, T.; Kongphet-Tran, T.; Mongkolrattanothai, T.; Travis, T.; Hendricks, K.; Parker, C.; McLaughlin, H.P.; Bugrysheva, J.; Ambrosio, F.; Michel, P.; et al. Systematic Review of In Vitro Antimicrobial Susceptibility Testing for Bacillus anthracis, 1947–2019. Clin. Infect. Dis. 2022, 75, S373–S378. [Google Scholar] [CrossRef]
- Manzulli, V.; Fasanella, A.; Parisi, A.; Serrecchia, L.; Donatiello, A.; Rondinone, V.; Caruso, M.; Zange, S.; Tscherne, A.; Decaro, N.; et al. Evaluation of in vitro antimicrobial susceptibility of Bacillus anthracis strains isolated during anthrax outbreaks in Italy from 1984 to 2017. J. Vet. Sci. 2019, 20, 58–62. [Google Scholar] [CrossRef]
- Chen, Y.; Succi, J.; Tenover, F.C.; Koehler, T.M. Beta-lactamase genes of the penicillin-susceptible Bacillus anthracis Sterne strain. J. Bacteriol. 2003, 185, 823–830. [Google Scholar] [CrossRef] [PubMed]
- Materon, I.C.; Queenan, A.M.; Koehler, T.M.; Bush, K.; Palzkill, T. Biochemical characterization of beta-lactamases Bla1 and Bla2 from Bacillus anthracis. Antimicrob. Agents Chemother. 2003, 47, 2040–2042. [Google Scholar] [CrossRef] [PubMed]
- Read, T.D.; Peterson, S.N.; Tourasse, N.; Baillie, L.W.; Paulsen, I.T.; Nelson, K.E.; Tettelin, H.; Fouts, D.E.; Eisen, J.A.; Gill, S.R.; et al. The genome sequence of Bacillus anthracis Ames and comparison to closely related bacteria. Nature 2003, 423, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Slamti, L.; Perchat, S.; Gominet, M.; Vilas-Bôas, G.; Fouet, A.; Mock, M.; Sanchis, V.; Chaufaux, J.; Gohar, M.; Lereclus, D. Distinct mutations in PlcR explain why some strains of the Bacillus cereus group are nonhemolytic. J. Bacteriol. 2004, 186, 3531–3538. [Google Scholar] [CrossRef] [PubMed]
- Gohar, M.; Økstad, O.A.; Gilois, N.; Sanchis, V.; Kolstø, A.B.; Lereclus, D. Two-dimensional electrophoresis analysis of the extracellular proteome of Bacillus cereus reveals the importance of the PlcR regulon. Proteomics 2002, 2, 784–791. [Google Scholar] [CrossRef] [PubMed]
- Agaisse, H.; Gominet, M.; Okstad, O.A.; Kolstø, A.B.; Lereclus, D. PlcR is a pleiotropic regulator of extracellular virulence factor gene expression in Bacillus thuringiensis. Mol. Microbiol. 1999, 32, 1043–1053. [Google Scholar] [CrossRef] [PubMed]
- Sastalla, I.; Maltese, L.M.; Pomerantseva, O.M.; Pomerantsev, A.P.; Keane-Myers, A.; Leppla, S.H. Activation of the latent PlcR regulon in Bacillus anthracis. Microbiology 2010, 156, 2982–2993. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.L.; Thomason, K.S.; Koehler, T.M. An extracytoplasmic function sigma factor controls beta-lactamase gene expression in Bacillus anthracis and other Bacillus cereus group species. J. Bacteriol. 2009, 191, 6683–6693. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.D.; Nauta, K.M.; Müh, U.; Ellermeier, C.D. Activation of the Extracytoplasmic Function σ Factor σP by β-Lactams in Bacillus thuringiensis Requires the Site-2 Protease RasP. mSphere 2019, 4, e00511-19. [Google Scholar] [CrossRef]
- Jones, M.E.; Goguen, J.; Critchley, I.A.; Draghi, D.C.; Karlowsky, J.A.; Sahm, D.F.; Porschen, R.; Patra, G.; DelVecchio, V.G. Antibiotic susceptibility of isolates of Bacillus anthracis, a bacterial pathogen with the potential to be used in biowarfare. Clin. Microbiol. Infect. 2003, 9, 984–986. [Google Scholar] [CrossRef]
- Luna, V.A.; King, D.S.; Gulledge, J.; Cannons, A.C.; Amuso, P.T.; Cattani, J. Susceptibility of Bacillus anthracis, Bacillus cereus, Bacillus mycoides, Bacillus pseudomycoides and Bacillus thuringiensis to 24 antimicrobials using Sensititre automated microbroth dilution and Etest agar gradient diffusion methods. J. Antimicrob. Chemother. 2007, 60, 555–567. [Google Scholar] [CrossRef]
- Maho, A.; Rossano, A.; Hächler, H.; Holzer, A.; Schelling, E.; Zinsstag, J.; Hassane, M.H.; Toguebaye, B.S.; Akakpo, A.J.; Van Ert, M.; et al. Antibiotic susceptibility and molecular diversity of Bacillus anthracis strains in Chad: Detection of a new phylogenetic subgroup. J. Clin. Microbiol. 2006, 44, 3422–3425. [Google Scholar] [CrossRef]
- Swaney, S.M.; Aoki, H.; Ganoza, M.C.; Shinabarger, D.L. The oxazolidinone linezolid inhibits initiation of protein synthesis in bacteria. Antimicrob. Agents Chemother. 1998, 42, 3251–3255. [Google Scholar] [CrossRef]
- Pomerantsev, A.P.; Sukovatova, L.V.; Marinin, L.I. Izuchenie svoĭstv Rif-R-populiatsii sibireiazvennogo mikroba [Characterization of a Rif-R population of Bacillus anthracis]. Antibiot. I Khimioterapiia Antibiot. Chemoter. 1993, 38, 34–38. [Google Scholar]
- Kim, H.S.; Choi, E.C.; Kim, B.K. A macrolide-lincosamide-streptogramin B resistance determinant from Bacillus anthracis 590: Cloning and expression of ermJ. J. Gen. Microbiol. 1993, 139, 601–607. [Google Scholar] [CrossRef]
- Sejvar, J.J.; Tenover, F.C.; Stephens, D.S. Management of anthrax meningitis. Lancet Infect. Dis. 2005, 5, 287–295. [Google Scholar] [CrossRef]
- Athamna, A.; Massalha, M.; Athamna, M.; Nura, A.; Medlej, B.; Ofek, I.; Bast, D.; Rubinstein, E. In vitro susceptibility of Bacillus anthracis to various antibacterial agents and their time-kill activity. J. Antimicrob. Chemother. 2004, 53, 247–251. [Google Scholar] [CrossRef]
- Odendaal, M.W.; Pieterson, P.M.; de Vos, V.; Botha, A.D. The antibiotic sensitivity patterns of Bacillus anthracis isolated from the Kruger National Park. Onderstepoort J. Vet. Res. 1991, 58, 17–19. [Google Scholar]
- Heine, H.S.; Bassett, J.; Miller, L.; Purcell, B.K.; Byrne, W.R. Efficacy of Daptomycin against Bacillus anthracis in a murine model of anthrax spore inhalation. Antimicrob. Agents Chemother. 2010, 54, 4471–4473. [Google Scholar] [CrossRef][Green Version]
- Burckhardt, R.M.; Escalante-Semerena, J.C. Insights into the Function of the N-Acetyltransferase SatA That Detoxifies Streptothricin in Bacillus subtilis and Bacillus anthracis. Appl. Environ. Microbiol. 2019, 85, e03029-18. [Google Scholar] [CrossRef]
- Bruce, S.A.; Huang, Y.H.; Kamath, P.L.; van Heerden, H.; Turner, W.C. The roles of antimicrobial resistance, phage diversity, isolation source and selection in shaping the genomic architecture of Bacillus anthracis. Microb. Genom. 2021, 7, 000616. [Google Scholar] [CrossRef] [PubMed]
- Chiaverini, A.; Abdel-Glil, M.Y.; Linde, J.; Galante, D.; Rondinone, V.; Fasanella, A.; Cammà, C.; D’Alterio, N.; Garofolo, G.; Tomaso, H. Whole Genome Sequencing for Studying Bacillus anthracis from an Outbreak in the Abruzzo Region of Italy. Microorganisms 2020, 8, 87. [Google Scholar] [CrossRef] [PubMed]
- Uchida, I.; Hornung, J.M.; Thorne, C.B.; Klimpel, K.R.; Leppla, S.H. Cloning and characterization of a gene whose product is a trans-activator of anthrax toxin synthesis. J. Bacteriol. 1993, 175, 5329–5338. [Google Scholar] [CrossRef] [PubMed]
- Koehler, T.M.; Dai, Z.; Kaufman-Yarbray, M. Regulation of the Bacillus anthracis protective antigen gene: CO2 and a trans-acting element activate transcription from one of two promoters. J. Bacteriol. 1994, 176, 586–595. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.C.; Popova, T.G.; Millis, B.A.; Mukherjee, D.V.; Zhou, W.; Liotta, L.A.; Petricoin, E.F.; Chandhoke, V.; Bailey, C.; Popov, S.G. Secreted neutral metalloproteases of Bacillus anthracis as candidate pathogenic factors. J. Biol. Chem. 2006, 281, 31408–31418. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.C.; Jorgensen, S.C.; Popova, T.G.; Tonry, J.H.; Bailey, C.L.; Popov, S.G. Activation of plasminogen activator inhibitor implicates protease InhA in the acute-phase response to Bacillus anthracis infection. J. Med. Microbiol. 2009, 58, 737–744. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tonry, J.H.; McNichol, B.A.; Ramarao, N.; Chertow, D.S.; Kim, K.S.; Stibitz, S.; Schneewind, O.; Kashanchi, F.; Bailey, C.L.; Popov, S.; et al. Bacillus anthracis protease InhA regulates BslA-mediated adhesion in human endothelial cells. Cell Microbiol. 2012, 14, 1219–1230. [Google Scholar] [CrossRef] [PubMed]
- Gomis-Rüth, F.X. Catalytic domain architecture of metzincin metalloproteases. J. Biol. Chem. 2009, 284, 15353–15357. [Google Scholar] [CrossRef]
- Ramarao, N.; Lereclus, D. The InhA1 metalloprotease allows spores of the B. cereus group to escape macrophages. Cell Microbiol. 2005, 7, 1357–1364. [Google Scholar] [CrossRef]
- Oda, M.; Hashimoto, M.; Takahashi, M.; Ohmae, Y.; Seike, S.; Kato, R.; Fujita, A.; Tsuge, H.; Nagahama, M.; Ochi, S.; et al. Role of sphingomyelinase in infectious diseases caused by Bacillus cereus. PLoS ONE 2012, 7, e38054. [Google Scholar] [CrossRef]
- Cai, Y.; Huang, T.; Xu, Y.; Zhou, G.; Zou, P.; Zeng, G.; Liu, X. Genetic and genomic diversity of NheABC locus from Bacillus strains. Arch. Microbiol. 2017, 199, 775–785. [Google Scholar] [CrossRef] [PubMed]
- Asano, S.I.; Nukumizu, Y.; Bando, H.; Iizuka, T.; Yamamoto, T. Cloning of novel enterotoxin genes from Bacillus cereus and Bacillus thuringiensis. Appl. Environ. Microbiol. 1997, 63, 1054–1057. [Google Scholar] [CrossRef] [PubMed]
- Boonchai, N.; Asano, S.I.; Bando, H.; Wiwat, C. Study on cytotoxicity and nucleotide sequences of enterotoxin FM of Bacillus cereus isolated from various food sources. J. Med. Assoc. Thai. 2008, 91, 1425–1432. [Google Scholar]
- Castiaux, V.; Laloux, L.; Schneider, Y.J.; Mahillon, J. Screening of Cytotoxic B. cereus on Differentiated Caco-2 Cells and in Co-Culture with Mucus-Secreting (HT29-MTX) Cells. Toxins 2016, 8, 320. [Google Scholar] [CrossRef] [PubMed]
- Tourasse, N.J.; Jolley, K.A.; Kolstø, A.B.; Økstad, O.A. Core genome multilocus sequence typing scheme for Bacillus cereus group bacteria. Res. Microbiol. 2023, 174, 104050. [Google Scholar] [CrossRef] [PubMed]
- Simonson, T.S.; Okinaka, R.T.; Wang, B.; Easterday, W.R.; Huynh, L.; U’Ren, J.M.; Dukerich, M.; Zanecki, S.R.; Kenefic, L.J.; Beaudry, J.; et al. Bacillus anthracis in China and its relationship to worldwide lineages. BMC Microbiol. 2009, 9, 71. [Google Scholar] [CrossRef] [PubMed]
- Antwerpen, M.; Ilin, D.; Georgieva, E.; Meyer, H.; Savov, E.; Frangoulidis, D. MLVA and SNP analysis identified a unique genetic cluster in Bulgarian Bacillus anthracis strains. Eur. J. Clin. Microbiol. Infect. Dis. 2011, 30, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Rondinone, V.; Serrecchia, L.; Parisi, A.; Fasanella, A.; Manzulli, V.; Cipolletta, D.; Galante, D. Genetic characterization of Bacillus anthracis strains circulating in Italy from 1972 to 2018. PLoS ONE 2020, 15, e0227875. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.L.; DeVos, V.; Bryden, H.; Price, L.B.; Hugh-Jones, M.E.; Keim, P. Bacillus anthracis diversity in Kruger National Park. J. Clin. Microbiol. 2000, 38, 3780–3784. [Google Scholar] [CrossRef]
- Fouet, A.; Smith, K.L.; Keys, C.; Vaissaire, J.; Le Doujet, C.; Lévy, M.; Mock, M.; Keim, P. Diversity among French Bacillus anthracis isolates. J. Clin. Microbiol. 2002, 40, 4732–4734. [Google Scholar] [CrossRef][Green Version]
- Gierczyński, R.; Kałuzewski, S.; Rakin, A.; Jagielski, M.; Zasada, A.; Jakubczak, A.; Borkowska-Opacka, B.; Rastawicki, W. Intriguing diversity of Bacillus anthracis in eastern Poland--the molecular echoes of the past outbreaks. FEMS Microbiol. Lett. 2004, 239, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Derzelle, S.; Laroche, S.; Le Flèche, P.; Hauck, Y.; Thierry, S.; Vergnaud, G.; Madani, N. Characterization of genetic diversity of Bacillus anthracis in France by using high-resolution melting assays and multilocus variable-number tandem-repeat analysis. J. Clin. Microbiol. 2011, 49, 4286–4292. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garofolo, G.; Serrecchia, L.; Corrò, M.; Fasanella, A. Anthrax phylogenetic structure in Northern Italy. BMC Res. Notes 2011, 4, 273. [Google Scholar] [CrossRef] [PubMed]
- Girault, G.; Blouin, Y.; Vergnaud, G.; Derzelle, S. High-throughput sequencing of Bacillus anthracis in France: Investigating genome diversity and population structure using whole-genome SNP discovery. BMC Genom. 2014, 15, 288. [Google Scholar] [CrossRef] [PubMed]
- Derzelle, S.; Thierry, S. Genetic diversity of Bacillus anthracis in Europe: Genotyping methods in forensic and epidemiologic investigations. Biosecur. Bioterror. 2013, 1, S166–S176. [Google Scholar] [CrossRef]
- Croatian Food Agency. Available online: https://www.hzjz.hr/wp-content/uploads/2017/11/Godi%C5%A1nje-izvje%C5%A1%C4%87e-o-zoonozama-2015_16.pdf (accessed on 7 July 2024).
- Croatian Institute for Public Health. Croatian Health Statistics Yearbook. 2022. Available online: https://www.hzjz.hr/wp-content/uploads/2024/05/HZSLj_2022_12-2023.pdf (accessed on 7 July 2024).
- Pajtlar, S.; Ančić-Birač, S.; Starčević, M. Epidemija Antraksa u Parku Prirode Lonjsko Polje 2022, Sažetci, BEDRENICA I AFRIČKA SVINJSKA KUGA U HRVATSKOJ, Zagreb, Hrvatska, 13.10.2023; Hrvatska Akademija Znanosti I Umjetnosti: Zagreb, Croatia, 2023; ISBN 978-953-347-371-0. Available online: https://www.info.hazu.hr/wp-content/uploads/2023/10/2023-HAZU-Zbornik-sazetaka-Bedrenica-i-africka-svinjska-kuga.pdf (accessed on 20 March 2024).
- Beyer, W.; Glöckner, P.; Otto, J.; Böhm, R. A nested PCR method for the detection of Bacillus anthracis in environmental samples collected from former tannery sites. Microbiol. Res. 1995, 150, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Hutson, R.A.; Duggleby, C.J.; Lowe, J.R.; Manchee, R.J.; Turnbull, P.C. The development and assessment of DNA and oligonucleotide probes for the specific detection of Bacillus anthracis. J. Appl. Bacteriol. 1993, 75, 463–472. [Google Scholar] [CrossRef]
- Clinical and Laboratory Standards Institute (CLSI). Methods for Antimicrobial Dilution and Disk Susceptibility Testing of Infrequently Isolated or Fastidious Bacteria M45, 3rd ed.; CLSI: Wayne, PA, USA, 2016. [Google Scholar]
- Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing, M100, 32nd ed.; CLSI: Wayne, PA, USA, 2022. [Google Scholar]
- Bolger, A.M.; Lohse, M.; Usadel, B. Trimmomatic: A flexible trimmer for Illumina sequence data. Bioinformatics 2014, 30, 2114–2120. [Google Scholar] [CrossRef] [PubMed]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A.D.; et al. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef]
- Gurevich, A.; Saveliev, V.; Vyahhi, N.; Tesler, G. QUAST: Quality assessment tool for genome assemblies. Bioinformatics 2013, 29, 1072–1075. [Google Scholar] [CrossRef]
- Chen, L.; Zheng, D.; Liu, B.; Yang, J.; Jin, Q. VFDB 2016: Hierarchical and refined dataset for big data analysis—10 years on. Nucleic Acids Res. 2016, 44, D694–D697. [Google Scholar] [CrossRef] [PubMed]
- Feldgarden, M.; Brover, V.; Haft, D.H.; Prasad, A.B.; Slotta, D.J.; Tolstoy, I.; Tyson, G.H.; Zhao, S.; Hsu, C.H.; McDermott, P.F.; et al. Validating the AMRFinder Tool and Resistance Gene Database by Using Antimicrobial Resistance Genotype-Phenotype Correlations in a Collection of Isolates. Antimicrob. Agents Chemother. 2019, 63, e00483-19, Erratum in Antimicrob. Agents Chemother. 2020, 64, e00361-20. [Google Scholar] [CrossRef] [PubMed]
- Johansson, M.H.K.; Bortolaia, V.; Tansirichaiya, S.; Aarestrup, F.M.; Roberts, A.P.; Petersen, T.N. Detection of mobile genetic elements associated with antibiotic resistance in Salmonella enterica using a newly developed web tool: MobileElementFinder. J. Antimicrob. Chemother. 2021, 76, 101–109. [Google Scholar] [CrossRef] [PubMed]
- Jünemann, S.; Sedlazeck, F.J.; Prior, K.; Albersmeier, A.; John, U.; Kalinowski, J.; Mellmann, A.; Goesmann, A.; von Haeseler, A.; Stoye, J.; et al. Updating benchtop sequencing performance comparison. Nat. Biotechnol. 2013, 31, 294–296. [Google Scholar] [CrossRef] [PubMed]
- Maestro, M. Bedrenica Domaćih Životinja u BIVŠOJ SAVSKOJ BANOVINI od 1931–1940 Godine. Ph.D. Thesis, Veterinarski fakultet Hrvatskog sveučilišta u Zagrebu, Zagreb, Croatia, 1946. [Google Scholar]
- Anon. Zakona o uređenju veterinarstva u Kraljevinah Hrvatskoj i Slavoniji. Nar. Nov. (Tisk. Zavod Zagreb) 1888, 27. kolovoza. [Google Scholar]
- Mlinac, F. Pojavljivanje Bedrenice na Području Bivše Hrvatske i Slavonije. Ph.D. Thesis, Veterinarski fakultet Kraljevine Jugoslavije, Sveučiliše u Zagrebu, Zagreb, Croatia, 1930. [Google Scholar]
- Zaharija, I. Zarazne Bolesti Domaćih Životinja; Školska knjiga: Zagreb, Croatia, 1978; pp. 111–112. [Google Scholar]
- Fališevac, J.; Hellenbach, H. Antraks kao profesionalno oboljenje sa specijalnim osvrtom na prilike u Jugoslaviji. Arh. Hig. Rada Toksikol. 1951, 2, 428–464. Available online: https://hrcak.srce.hr/clanak/277177 (accessed on 15 September 2019).

| Isolates | Number of Isolates | pXO1 | pXO2 |
|---|---|---|---|
| 2001/2002 | 5 | + | + |
| 2006/2007 | 6 | + | + |
| 2022 | 25 | + | + |
| ST | 4 | + | + |
| Sterne 34F2 | 1 | + | - |
| Antibiotic | MIC50 | MIC90 | Range (mg/L) | Breakpoint | % S/I/R a | |
|---|---|---|---|---|---|---|
| S (≤) | R (≥) | |||||
| Erythromycin ** | 0.5 | 0.5 | 0.25–4 | 0.5 | 8 | 95/5/0 |
| Quinupristin/dalfopristin *** | 1 | 1 | 0.12–4 | 1 | 4 | 100/0/0 |
| Vancomycin ** | 2 | 2 | 1–128 | 4 | 100/0/0 | |
| Ampicillin * | ≤0.12 | ≤0.12 | 0.12–16 | 0.12 | 0.25 | 100/0/0 |
| Rifampin ** | ≤0.5 | ≤0.5 | 0.5–4 | 1 | 4 | 100/0/0 |
| Levofloxacin * | ≤0.25 | ≤0.25 | 0.25–0.5 | 0.25 | 100/0/0 | |
| Penicillin * | ≤0.06 | ≤0.06 | 0.06–8 | 0.5 | 1 | 100/0/0 |
| Trimethoprim/sulfamethoxazole ** | >4/76 | >4/76 | 0.5/9.5–4/76 | 2/38 | 4/76 | 0/0/100 |
| Oxacillin + 2%NaCl *** | ≤0.25 | ≤0.25 | 0.5–8 | 0.5 | 1 | 100/0/0 |
| Ceftriaxone ** | ≤8 | 16 | 8–64 | 8 | 64 | 60/40/0 |
| Clindamycin ** | 0.25 | 0.25 | 0.12–2 | 0.5 | 4 | 100/0/0 |
| Daptomycin *** | 4 | 4 | 0.25–8 | 1 | 0/0/100 | |
| Linezolid *** | 1 | 1 | 0.5–8 | 4 | 8 | 100/0/0 |
| Tetracycline * | ≤2 | ≤2 | 2–16 | 1 | 100/0/0 | |
| Gentamicin ** | ≤2 | ≤2 | 2–16 | 4 | 16 | 100/0/0 |
| Gatifloxacin *** | ≤1 | ≤1 | 1–8 | 0.5 | 2 | 100/0/0 |
| Ciprofloxacin * | ≤0.5 | ≤0.5 | 0.5–2 | 0.25 | 100/0/0 | |
| Streptomycin | ≤1000 | ≤1000 | 1000 | |||
| Gene | Name | Type | Aligned Overlap 100%/Identity ≥ 97% | |||
|---|---|---|---|---|---|---|
| 2001/2002 N = 5 | 2006/2007 N = 6 | ST N = 4 | 2022 N = 25 | |||
| bla | Class A beta-lactamase Bla1 | AMR | + | + | + | + |
| blaII | BcII family subclass B1 metallo-beta-lactamase | AMR | + | + | + | + |
| fosB | fosB/fosD family fosfomycin resistance bacillithiol transferase | AMR | + | - | + | - |
| satA | Streptothricin N- acetyltransferase SatA | AMR | + | + | + | + |
| pagA | anthrax toxin protective antigen | VIR | + | + | + | + |
| lef | anthrax toxin lethal factor | VIR | + | + | + | + |
| cya | anthrax toxin edema factor | VIR | + | + | + | + |
| capA | capsular polyglutamate synthetase CapA | VIR | + | + | + | + |
| capB | capsule biosynthesis protein CapB | VIR | + | + | + | + |
| capC | capsular polyglutamate amide ligase/translocase CapC | VIR | + | + | + | + |
| capD | capsule biosynthesis gamma-glutamyltransferase CapD | VIR | + | + | + | + |
| capE | capsule biosynthesis protein CapE | VIR | + | + | + | + |
| atxA | anthrax toxin expression trans-acting transcriptional regulator AtxA | VIR | + | + | + | + |
| inhA1 | M6 family metalloprotease immune inhibitor InhA1 | VIR | + | + | + | + |
| inhA2 | M6 family metalloprotease immune inhibitor InhA2 | VIR | + | + | + | + |
| entFM | enterotoxin EntFM | VIR | + | + | + | + |
| nheA | non-hemolytic enterotoxin NHE subunit A | VIR | + | + | + | + |
| nheB | non-hemolytic enterotoxin NHE subunit B | VIR | + | + | + | + |
| nheC | non-hemolytic enterotoxin NHE subunit C | VIR | + | + | + | + |
| plcR | transcriptional regulator PlcR | VIR | + | + | + | + |
| sph | sphingomyelinase C | VIR | + | + | + | + |
| hlyIIR | hemolysin II regulator HlyIIR | VIR | + | + | + | + |
| cerA | phospholipase CerA | VIR | + | + | + | + |
| plcA | phosphatidylinositol diacylglycerol-lyase | VIR | + | + | + | + |
| alo | anthrolysin O/cereolysin O family cholesterol-dependent cytolysin Alo | VIR | + | + | + | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kompes, G.; Duvnjak, S.; Reil, I.; Mihaljević, Ž.; Habrun, B.; Benić, M.; Cvetnić, L.; Špičić, S.; Bagarić, A. Antimicrobial Resistance Profile, Whole-Genome Sequencing and Core Genome Multilocus Sequence Typing of B. anthracis Isolates in Croatia from 2001 to 2022. Antibiotics 2024, 13, 639. https://doi.org/10.3390/antibiotics13070639
Kompes G, Duvnjak S, Reil I, Mihaljević Ž, Habrun B, Benić M, Cvetnić L, Špičić S, Bagarić A. Antimicrobial Resistance Profile, Whole-Genome Sequencing and Core Genome Multilocus Sequence Typing of B. anthracis Isolates in Croatia from 2001 to 2022. Antibiotics. 2024; 13(7):639. https://doi.org/10.3390/antibiotics13070639
Chicago/Turabian StyleKompes, Gordan, Sanja Duvnjak, Irena Reil, Željko Mihaljević, Boris Habrun, Miroslav Benić, Luka Cvetnić, Silvio Špičić, and Antonela Bagarić. 2024. "Antimicrobial Resistance Profile, Whole-Genome Sequencing and Core Genome Multilocus Sequence Typing of B. anthracis Isolates in Croatia from 2001 to 2022" Antibiotics 13, no. 7: 639. https://doi.org/10.3390/antibiotics13070639
APA StyleKompes, G., Duvnjak, S., Reil, I., Mihaljević, Ž., Habrun, B., Benić, M., Cvetnić, L., Špičić, S., & Bagarić, A. (2024). Antimicrobial Resistance Profile, Whole-Genome Sequencing and Core Genome Multilocus Sequence Typing of B. anthracis Isolates in Croatia from 2001 to 2022. Antibiotics, 13(7), 639. https://doi.org/10.3390/antibiotics13070639






