The Evolving Challenge of Appropriate Antibiotics Use in Hospitalized COVID-19 Patients: A Systematic Literature Review
Abstract
1. Introduction
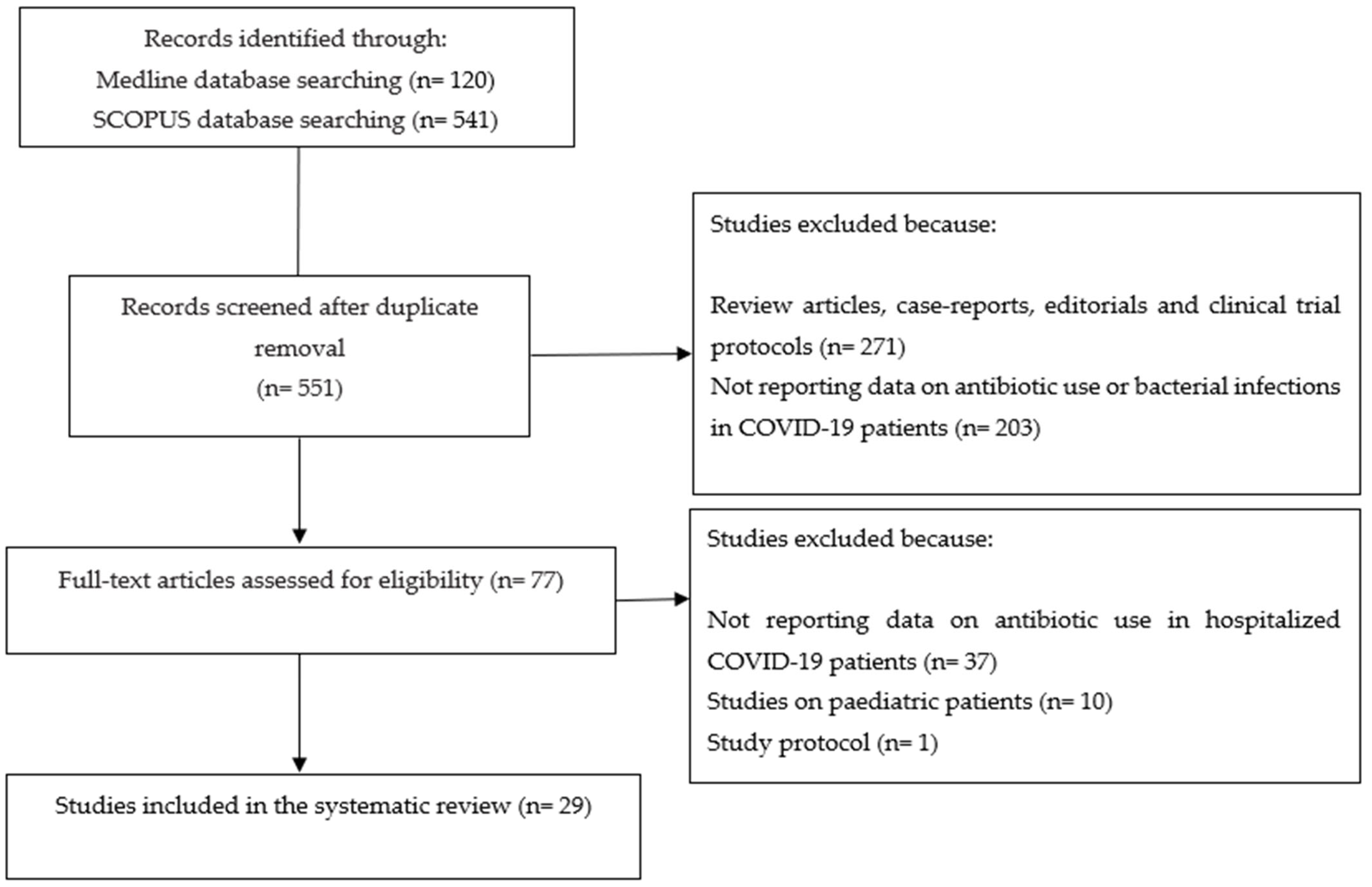
2. Materials and Methods
2.1. Search Strategy and Article Identification
2.2. Eligibility Criteria
2.3. Study Selection, Data Extraction, and Quality Appraisal
2.4. Data Synthesis
3. Results
3.1. Study Descriptions
3.2. Bacterial Infections and Antibiotic Use among COVID-19 Patients
3.2.1. The Prevalence of Bacterial Infection and Antibiotic Use among Hospitalized COVID-19 Patients
3.2.2. The Prevalence of Bacterial Infection and Antibiotic Use among Hospitalized COVID-19 Patients in the Intensive Care Unit
3.2.3. The Efficacy of Early Antibiotic Administration in COVID-19
3.2.4. Studies on the Use of Sepsis Biomarkers for Antibiotic Prescribing in COVID-19-Hospitalized Patients
3.2.5. Studies on the Efficacy of Antimicrobial Stewardship Programs
4. Discussion
Supplementary Materials
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Granata, G.; Schiavone, F.; Pipitone, G.; Taglietti, F.; Petrosillo, N. Antibiotics Use in COVID-19 Patients: A Systematic Literature Review. J. Clin. Med. 2022, 11, 7207. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Torres, V.; de Mendoza, C.; de la Fuente, S.; Sánchez, E.; Martínez-Urbistondo, M.; Herráiz, J.; Gutiérrez, A.; Gutiérrez, Á.; Hernández, C.; Callejas, A.; et al. Bacterial infections in patients hospitalized with COVID-19. Intern Emerg Med. 2022, 17, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Rawson, T.M.; Moore, L.S.P.; Zhu, N.; Ranganathan, N.; Skolimowska, K.; Gilchrist, M.; Satta, G.; Cooke, G.; Holmes, A. Bacterial and Fungal Coinfection in Individuals with Coronavirus: A Rapid Review to Support COVID-19 Antimicrobial Prescribing. Clin Infect Dis. 2020, 71, 2459–2468. [Google Scholar] [CrossRef] [PubMed]
- Sugden, R.; Kelly, R.; Davies, S. Combatting antimicrobial resistance globally. Nat. Microbiol. 2016, 1, 16187. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Moola, S.; Lisy, K.; Riitano, D.; Tufanaru, C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based Healthc. 2015, 13, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Savoldi, A.; Carrara, E.; Graham, D.Y.; Conti, M.; Tacconelli, E. Prevalence of antibiotic resistance in helicobacter pylori: A systematic review and meta-analysis in world health organization regions. Gastroenterology 2018, 155, 1372–1382.e1317. [Google Scholar] [CrossRef] [PubMed]
- Ng, T.M.; Ong, S.W.X.; Loo, A.Y.X.; Tan, S.H.; Tay, H.L.; Yap, M.Y.; Lye, D.C.; Lee, T.H.; Young, B.E. Antibiotic Therapy in the Treatment of COVID-19 Pneumonia: Who and When? Antibiotics 2022, 11, 184. [Google Scholar] [CrossRef] [PubMed]
- Milas, S.; Poncelet, A.; Buttafuoco, F.; Pardo, A.; Lali, S.E.; Cherifi, S. Antibiotic use in patients with Coronavirus disease 2019 (COVID-19): Outcomes and associated factors. Acta Clin. Belg. Int. J. Clin. Lab. Med. 2022, 77, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Rebold, N.; Alosaimy, S.; Morrisette, T.; Holger, D.; Lagnf, A.M.; Ansari, I.; Belza, A.C.; Cheaney, L.; Hussain, H.; Herbin, S.R.; et al. Clinical Characteristics Associated with Bacterial Bloodstream Coinfection in COVID-19. Infect. Dis. Ther. 2022, 11, 1281–1296. [Google Scholar] [CrossRef]
- Ahava, M.J.; Kortela, E.; Forsblom, E.; Pätäri-Sampo, A.; Friberg, N.; Meretoja, A.; Kivivuori, S.-M.; Lappalainen, M.; Kurkela, S.; Järvinen, A.; et al. Low incidence of severe bacterial infections in hospitalised patients with COVID-19: A population-based registry study. Infect. Dis. 2023, 55, 132–141. [Google Scholar] [CrossRef]
- Gajic, I.; Jovicevic, M.; Popadic, V.; Trudic, A.; Kabic, J.; Kekic, D.; Ilic, A.; Klasnja, S.; Hadnadjev, M.; Popadic, D.J.; et al. The emergence of multi-drug-resistant bacteria causing healthcare-associated infections in COVID-19 patients: A retrospective multi-centre study. J. Hosp. Infect. 2023, 137, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Martin, A.J.; Shulder, S.; Dobrzynski, D.; Quartuccio, K.; Pillinger, K.E. Antibiotic Use and Associated Risk Factors for Antibiotic Prescribing in COVID-19 Hospitalized Patients. J. Pharm. Pract. 2023, 36, 256–263. [Google Scholar] [CrossRef] [PubMed]
- Desai, K.; Arora, P.; Ghanekar, S.; Johnson, K.; Harris, I. Antibiotic prescribing trends in the US during the first 11 months of the COVID-19 pandemic. Res. Social Adm. Pharm. 2022, 18, 3855–3859. [Google Scholar] [CrossRef] [PubMed]
- Di Lorenzo, A.; Campogiani, L.; Iannetta, M.; Iannazzo, R.; Imeneo, A.; Alessio, G.; D’Aquila, V.; Massa, B.; Fato, I.; Rindi, L.V.; et al. The Impact of Viral and Bacterial Co-Infections and Home Antibiotic Treatment in SARS-CoV-2 Hospitalized Patients at the Policlinico Tor Vergata Hospital, Rome, Italy. Antibiotics 2023, 12, 1348. [Google Scholar] [CrossRef] [PubMed]
- Habib, G.; Mahmood, K.; Gul, H.; Tariq, M.; Ain, Q.U.; Hayat, A.; Rehman, M.U. Pathophysiology of Methicillin-Resistant Staphylococcus aureus Superinfection in COVID-19 Patients. Pathophysiology 2022, 29, 405–413. [Google Scholar] [CrossRef]
- Widere, J.C.; Davis, C.L.; Loomba, J.J.; Bell, T.D.; Enfield, K.B.; Barros, A.J.; N3C Consortium. Early Empiric Antibiotic Use in Patients Hospitalized With COVID-19: A Retrospective Cohort Study. Crit. Care Med. 2023, 51, 1168–1176. [Google Scholar] [CrossRef] [PubMed]
- Subagdja, M.F.M.; Sugianli, A.K.; Prodjosoewojo, S.; Hartantri, Y.; Parwati, I. Antibiotic Resistance in COVID-19 with Bacterial Infection: Laboratory-Based Surveillance Study at Single Tertiary Hospital in Indonesia. Infect. Drug Resist. 2022, 15, 5849–5856. [Google Scholar] [CrossRef] [PubMed]
- Bilan, J.; Aggrey, K.; Quinn, T.J.; Lumsden, J.; Colquhoun, K. Occurrence and outcomes of possible superadded infections in older adults with COVID-19—Cohort study. Eur. Geriatr. Med. 2022, 13, 1161–1167. [Google Scholar] [CrossRef] [PubMed]
- Maki, K.R.; Steiger, S.N.; Su, Y.; Boumiza, A.; Tan, C.A.; Kerpelev, M.; Seo, S.K.; Cohen, N. Bacterial infections and antibiotic utilization varies by coronavirus disease 19 (COVID-19) severity in hospitalized cancer patients: Analysis from the first phase of the pandemic. Infect Control. Hosp. Epidemiol. 2023, 44, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Gragueb-Chatti, I.; Hyvernat, H.; Leone, M.; Agard, G.; Peres, N.; Guervilly, C.; Boucekine, M.; Hamidi, D.; Papazian, L.; Dellamonica, J.; et al. Incidence, Outcomes and Risk Factors of Recurrent Ventilator Associated Pneumonia in COVID-19 Patients: A Retrospective Multicenter Study. J. Clin. Med. 2022, 11, 7097. [Google Scholar] [CrossRef] [PubMed]
- Aissaoui, Y.; Ennassimi, Y.; Myatt, I.; El Bouhiaoui, M.; Nabil, M.; Bahi, M.; Arsalane, L.; Miloudi, M.; Belhadj, A. What happened during COVID-19 in African ICUs? An observational study of pulmonary co-infections, superinfections, and mortality in Morocco. PLoS ONE 2022, 17, e0278175. [Google Scholar] [CrossRef] [PubMed]
- Sysiak-Sławecka, J.; Wichowska, O.; Piwowarczyk, P.; Borys, M. The impact of bacterial superinfections on the outcome of critically ill patients with COVID-19 associated acute respiratory distress syndrome (ARDS)—a single-centre, observational cohort study. Anaesthesiol. Intensiv. Ther. 2023, 55, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Russo, A.; Bruni, A.; Gullì, S.; Borrazzo, C.; Quirino, A.; Lionello, R.; Serapide, F.; Garofalo, E.; Serraino, R.; Romeo, F.; et al. Efficacy of cefiderocol- vs colistin-containing regimen for treatment of bacteraemic ventilator-associated pneumonia caused by carbapenem-resistant Acinetobacter baumannii in patients with COVID-19. Int. J. Antimicrob. Agents 2023, 62, 106825. [Google Scholar] [CrossRef] [PubMed]
- Petrakis, V.; Panopoulou, M.; Rafailidis, P.; Lemonakis, N.; Lazaridis, G.; Terzi, I.; Papazoglou, D.; Panagopoulos, P. The Impact of the COVID-19 Pandemic on Antimicrobial Resistance and Management of Bloodstream Infections. Pathogens 2023, 12, 780. [Google Scholar] [CrossRef] [PubMed]
- Dhar, R.; Kirkpatrick, J.; Gilbert, L.; Khanna, A.; Modi, M.M.; Chawla, R.K.; Dalal, S.; Maturu, V.N.; Stern, M.; Keppler, O.T.; et al. Doxycycline for the prevention of progression of COVID-19 to severe disease requiring intensive care unit (ICU) admission: A randomized, controlled, open-label, parallel group trial (DOXPREVENT.ICU). PLoS ONE 2023, 18, e0280745. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Xu, X.; Li, H.; Jiang, N.; Wang, J.; Lu, Z.; Xiong, N.; Gong, Y. Evaluation of early antibiotic use in patients with non-severe COVID-19 without bacterial infection. Int. J. Antimicrob. Agents. 2022, 59, 106462. [Google Scholar] [CrossRef] [PubMed]
- Bergami, M.; Manfrini, O.; Nava, S.; Caramori, G.; Yoon, J.; Badimon, L.; Cenko, E.; David, A.; Demiri, I.; Dorobantu, M.; et al. Relationship Between Azithromycin and Cardiovascular Outcomes in Unvaccinated Patients With COVID-19 and Preexisting Cardiovascular Disease. J. Am. Heart Assoc. 2023, 12, e028939. [Google Scholar] [CrossRef] [PubMed]
- Biagioni, E.; Ferrari, E.; Gatto, I.; Serio, L.; Farinelli, C.; Coloretti, I.; Talamonti, M.; Tosi, M.; Meschiari, M.; Tonelli, R.; et al. Role of Selective Digestive Decontamination in the Prevention of Ventilator-Associated Pneumonia in COVID-19 Patients: A Pre-Post Observational Study. J. Clin. Med. 2023, 12, 1432. [Google Scholar] [CrossRef]
- Conlon, A.S.C.; Chopra, Z.; Cahalan, S.; Cinti, S.; Rao, K. Effects of procalcitonin on antimicrobial treatment decisions in patients with coronavirus disease 2019 (COVID-19). Infect. Control. Hosp. Epidemiol. 2023, 44, 1314–1320. [Google Scholar] [CrossRef]
- Hessels, L.M.; Speksnijder, E.; Paternotte, N.; van Huisstede, A.; Thijs, W.; Scheer, M.; van der Steen-Dieperink, M.; Knarren, L.; van Den Bergh, J.P.; Winckers, K.; et al. Procalcitonin-Guided Antibiotic Prescription in Patients With COVID-19: A Multicenter Observational Cohort Study. Chest 2023, 164, 596–605. [Google Scholar] [CrossRef] [PubMed]
- Fartoukh, M.; Nseir, S.; Mégarbane, B.; Cohen, Y.; Lafarge, A.; Contou, D.; Thille, A.W.; Galerneau, L.M.; Reizine, F.; Cour, M.; et al. Respiratory multiplex PCR and procalcitonin to reduce antibiotic exposure in severe SARS-CoV-2 pneumonia: A multicentre randomized controlled trial. Clin. Microbiol. Infect. 2023, 29, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Sathitakorn, O.; Chansirikarnjana, S.; Jantarathaneewat, K.; Weber, D.J.; Warren, D.K.; Apisarnthanarak, P.; Tantiyavarong, P.; Apisarnthanarak, A. The role of procalcitonin and Clinical Pulmonary for Infection Score (CPIS) score to reduce inappropriate antibiotics use among moderate to severe coronavirus disease 2019 (COVID-19) pneumonia: A quasi-experimental multicenter study. Infect. Control. Hosp. Epidemiol. 2023, 44, 1199–1203. [Google Scholar] [CrossRef]
- Sibani, M.; Canziani, L.M.; Tonolli, C.; Armellini, M.; Carrara, E.; Mazzaferri, F.; Conti, M.; SAVE Working Group; Mazzariol, A.; Micheletto, C.; et al. Antimicrobial Stewardship in COVID-19 Patients: Those Who Sow Will Reap Even through Hard Times. Antibiotics 2023, 12, 1009. [Google Scholar] [CrossRef] [PubMed]
- Spernovasilis, N.; Kritsotakis, E.I.; Mathioudaki, A.; Vouidaski, A.; Spanias, C.; Petrodaskalaki, M.; Ioannou, P.; Chamilos, G.; Kofteridis, D.P. A carbapenem-focused antimicrobial stewardship programme implemented during the COVID-19 pandemic in a setting of high endemicity for multidrug-resistant Gram-negative bacteria. J. Antimicrob. Chemother. 2023, 78, 1000–1008. [Google Scholar] [CrossRef] [PubMed]
- Giannella, M.; Rinaldi, M.; Tesini, G.; Gallo, M.; Cipriani, V.; Vatamanu, O.; Campoli, C.; Toschi, A.; Ferraro, G.; Horna, C.S.; et al. Predictive model for bacterial co-infection in patients hospitalized for COVID-19: A multicenter observational cohort study. Infection 2022, 50, 1243–1253. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Clinical Management of COVID-19: Living Guidance. 25 January 2021. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1 (accessed on 10 February 2024).
- COVID-19 Treatment Guidelines Panel Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Available online: https://www.covid19treatmentguidelines.nih.gov (accessed on 10 February 2024).
| Main Issue Evaluated by the Included Studies | Number of Included Studies | Main Findings | Comments |
|---|---|---|---|
| The prevalence of bacterial infection and antibiotic use in hospitalized COVID-19 patients | 18 | Antibiotic administration ranged between 12% and 83%, despite only a small percentage of the patients receiving antibiotics had a documented bacterial infection. Rates of hospital-acquired infections range between 7.5% and 37.7%. Hospital-acquired bacterial pneumonia ranges between 4.2% and 25.6% High rates of MDR Gram-negative bacteria and high in-hospital mortality rate of COVID-19 patients with infection due to MDR bacteria, up to 51.6% | High antibiotic resistance rate has been described among COVID-19 patients developing hospital-acquired infections, with carbapenem-resistance in more than 69.1% of the Gram-negative isolates. In intensive care units, high levels of bacterial superinfections, in particular, MDR Gram-negative bacteria burdened with high mortality rates. Higher bacterial infection rate in specific patients’ groups, i.e., 67% of cancer patients and 43% of elderly patients with COVID-19 |
| The efficacy of early antibiotic use | 4 | Azithromycin does not improve disease progression and length of stay in COVID-19 patients | Early antibiotic use does not improve disease progression and length of stay |
| The use of sepsis biomarkers to improve antibiotic use | 4 | The included studies evaluating procalcitonin-guided antibiotic prescription to reduce antibiotic prescription rates in hospitalized COVID-19 patients gave conflicting results | Considering that COVID-19 can raise the procalcitonin level in the absence of bacterial coinfection, procalcitonin threshold may need to be increased to >0.25 ng/mL when assessing the probability of bacterial coinfection with COVID-19. A combined approach using procalcitonin and clinical score sounds promising |
| The efficacy of antimicrobial stewardship programs | 3 | Decreased amount of total antibiotic consumption and lower in-hospital mortality after the implementation of multi-faceted antimicrobial stewardship interventions in COVID-19 wards | Predictive models to stratify the risk of bacterial coinfection in hospitalized COVID-19 patients may be implemented into antimicrobial stewardship interventions |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Granata, G.; Cicalini, S. The Evolving Challenge of Appropriate Antibiotics Use in Hospitalized COVID-19 Patients: A Systematic Literature Review. Antibiotics 2024, 13, 545. https://doi.org/10.3390/antibiotics13060545
Granata G, Cicalini S. The Evolving Challenge of Appropriate Antibiotics Use in Hospitalized COVID-19 Patients: A Systematic Literature Review. Antibiotics. 2024; 13(6):545. https://doi.org/10.3390/antibiotics13060545
Chicago/Turabian StyleGranata, Guido, and Stefania Cicalini. 2024. "The Evolving Challenge of Appropriate Antibiotics Use in Hospitalized COVID-19 Patients: A Systematic Literature Review" Antibiotics 13, no. 6: 545. https://doi.org/10.3390/antibiotics13060545
APA StyleGranata, G., & Cicalini, S. (2024). The Evolving Challenge of Appropriate Antibiotics Use in Hospitalized COVID-19 Patients: A Systematic Literature Review. Antibiotics, 13(6), 545. https://doi.org/10.3390/antibiotics13060545







