Abstract
This review explores the potential of antimicrobial metabolites derived from Caucasian medicinal plants as alternatives to conventional antibiotics. With the rise of antibiotic resistance posing a global health threat, there is a pressing need to investigate alternative sources of antimicrobial agents. Caucasian medicinal plants have traditionally been used for their therapeutic properties, and recent research has highlighted their potential as sources of antimicrobial compounds. Representatives of 15 families of Caucasian medicinal plant extracts (24 species) have been explored for their efficacy against these pathogens. The effect of these plants on Gram-positive and Gram-negative bacteria and fungi is discussed in this paper. By harnessing the bioactive metabolites present in these plants, this study aims to contribute to the development of new antimicrobial treatments that can effectively combat bacterial infections while minimizing the risk of resistance emergence. Herein we discuss the following classes of bioactive compounds exhibiting antimicrobial activity: phenolic compounds, flavonoids, tannins, terpenes, saponins, alkaloids, and sulfur-containing compounds of Allium species. The review discusses the pharmacological properties of selected Caucasian medicinal plants, the extraction and characterization of these antimicrobial metabolites, the mechanisms of action of antibacterial and antifungal plant compounds, and their potential applications in clinical settings. Additionally, challenges and future directions in the research of antimicrobial metabolites from Caucasian medicinal plants are addressed.
1. Introduction
A reduction in the number of infection-related deaths is a crucial worldwide public health objective, with the World Health Organization (WHO) ranking antibiotic resistance as one of the top 10 dangers to global public health [1]. In 2019, out of 13.7 million infection-related deaths, 7.7 million deaths were associated with 33 bacterial pathogens [2]. Antibiotic resistance [3,4] has led to a decreased effectiveness or even the complete ineffectiveness of current antibacterial medications [5]. Consequently, there is a growing demand to create novel antimicrobial drugs that can combat the emergence of resistance and reduce the need for antibiotics [1]. Various bioactive chemicals can be obtained from medicinal plants [6,7,8,9,10], and numerous techniques have been employed to investigate their potential as antimicrobial agents [11]. These bioactive compounds are secondary plant metabolites, representing one of the unexplored sources of antimicrobial agents in nature [12]. The results of phytochemical studies demonstrated that plant extracts may inhibit the growth of bacteria, fungi, viruses, and protozoa by mechanisms different from antibiotics and therefore may have significant clinical value in the treatment of resistant microbial strains [13]. Information regarding the traditional use of medicinal plants can be a useful basis for the identification of plants exhibiting pharmacological activity [14]. This is particularly true for biodiversity-rich regions of the world such as the Caucasus, with a history of long-time traditional (ethnobotanical) use of medicinal plants [15].
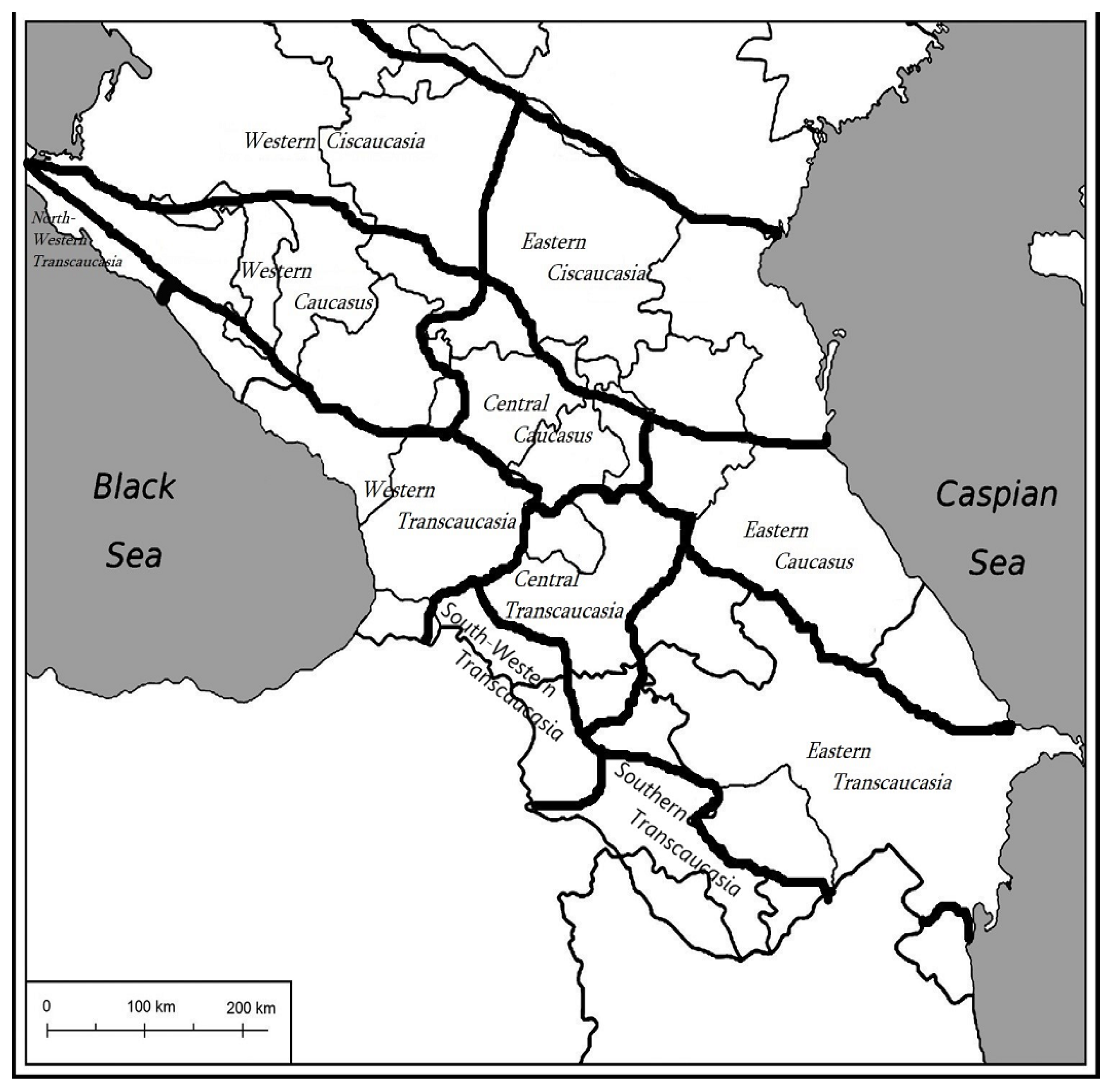
As a geographic, historical, and cultural phenomenon, the Caucasus covers a vast area between the Black Sea to the west and the Caspian Sea to the east [16]. In this study, we determined the floristic boundaries of the Caucasus following the guidelines outlined in [17]. The demarcation of primary natural zones within the Caucasus territory is established through floristic zoning, employing the “sectoral” principle as developed by A. A. Grossheim [18] and A. L. Takhtajan [19] (Figure 1). According to this principle, the territory of the Caucasus is divided into zones associated with the division of territory by Greater Caucasus and Lesser Caucasus mountain ranges [19]. These mountain systems and long-term climate changes, specifically the gradual decline in temperature and humidity, have contributed to the development of the Caucasus biodiversity hotspot [20,21]. In total, 6350 vascular plant species occur in the Caucasus, including more than 2900 endemic species [21]. Among these plant materials, 1000 species have therapeutic uses in traditional folk medicine and approximately 180 species are used in modern medicine [22]. The distribution of the Caucasian medicinal plant species in Table 1 is shown according to the floristic zones.

Figure 1.
The borders and floristic districts of the Caucasus according to [19].

Table 1.
Antimicrobial screening of Caucasian medicinal plants.
In this review, we conducted a systematic classification of Caucasian plants, focusing on their revealed antimicrobial properties, while also outlining their species range following the sectoral principle as described previously. Our literature search adhered to the Prisma guidelines for systematic reviews [67]. The literature search was carried out in PubMed, Scopus, ScienceDirect, and Google Scholar databases. A total of 207 publications were collected and assessed. The following search criteria were used: (1) “Antimicrobial”; (2) “Caucasian plants”; (3) “Caucasian Medicinal Plants”; (4) the name of each Caucasian medicinal plant, for which antimicrobial activity was demonstrated, was also used for the further search aimed at the identification of bioactive compounds, described for the particular species. All reported plant names were cross-checked following The Plant List (http://www.theplantlist.org/, accessed on 9 May 2024) and the International Plant Names Index (https://www.ipni.org/, accessed on 9 May 2024). Plant families were assigned using the Angiosperm Phylogeny Group IV guidance [68]. The names of all bacterial species discussed in the review were cross-checked with the LPSN (List of Prokaryotic Names) at https://www.bacterio.net/ (accessed on 9 May 2024); the names of fungi were cross-checked at https://www.indexfungorum.org/names/Names.asp (accessed on 9 May 2024).
2. Antimicrobial and Antifungal Activity of Caucasian Medicinal Plants
Throughout human history, different plant parts of medicinal plants such as leaves, stems, bark, roots, seeds, and fruits have been used for the treatment and prevention of all main types of diseases [69]. Biologically active compounds isolated from plant material still serve as the major sources of new drug molecules today. However, the revision of the published articles devoted to the antimicrobial effect of these biologically active compounds revealed that a comparison between results is often difficult due to the use of different non-standardized approaches. Various laboratory methods can be used for the in vitro assessment of the antimicrobial activity of a given extract or a pure compound [70]. These methods include diffusion methods (such as the agar disk diffusion method, the antimicrobial gradient method, the agar well diffusion method, the agar plug diffusion method, and the cross streak method), thin-layer chromatography (TLC)–bioautography methods (agar diffusion, direct bioautography), and dilution methods (broth dilution method, agar dilution method, time-kill test) [70]. The most common indicators of antimicrobial activity, measured by various methods, are the minimum inhibitory concentration (MIC) and zone of inhibition (IZ). The MIC is the lowest concentration of an antibacterial agent expressed in mg/L which, under strictly controlled in vitro conditions, completely prevents visible growth of the test strain of an organism [71]. Another indicator used in the study of antimicrobial activity is the zone of inhibition (IZ), expressed in mm and defined as a circular area around the spot of the antibiotic or bioactive compound where the bacteria colonies do not grow [72]. The higher susceptibility of bacteria or fungi is associated with higher values of IZ and lower MIC values. These indicators were used in this study to compare the antibacterial and antifungal activity of Caucasian medicinal plants. In particular, the anticancer, anti-inflammatory, antibacterial, and antifungal properties of Caucasian medicinal plants were demonstrated [73]. The WHO has identified the discovery of novel antibacterial drugs to combat multidrug-resistant ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species) as a top priority. These pathogens, known for their ability to “escape” the effects of antimicrobial agents, are responsible for a significant portion of nosocomial infections [74]. Representatives of 15 families of Caucasian medicinal plant extracts have been explored for their efficacy against these pathogens (Table 1; the floristic regions are indicated in accordance with Figure 1). The most significant antimicrobial activity, based on MIC values, against resistant ESKAPE pathogens was revealed for the essential oil obtained from Artemisia fragrans Willd. stems [33], while acetone extract of Hypericum alpestre Steven. aerial part [36], aqueous extracts of Juglans regia L. green husks [41], acetone extract of Sanguisorba officinalis L. aerial part [36], methanol extract of Peganum harmala L. plant [66], and methanol [35] and ethanol extracts of Agrimonia eupatoria L. plants [36] showed significant activity against S. aureus. Ethanol extracts from Peganum harmala L. seeds and Mentha pulegium L. leaves demonstrated high activity against K. pneumoniae [45], whereas methanol extracts of Acer cappadocicum Gled. branches exhibited activity against A. baumannii [65].
The antimicrobial activity of Caucasian medicinal plants against P. aeruginosa was also investigated in many studies [28,30,33,34,36,41,49,50,54]. In particular, significant activity against P. aeruginosa was revealed for the essential oil obtained from A. fragrans flowers [33], the acetone extracts of H. alpestre aerial part [36] and Lilium monadelphum subsp. armenum (Miscz. ex Grossh.) Kudrjasch. bulb [36], as well as for the methanol extract of Cyclamen coum Mill. aerial parts [54], the acetone extracts of A. eupatoria plants [36], the ethanol extract of Rosa canina L. fruits [62], and the acetone extract of S. officinalis aerial parts [36]. In addition to their antimicrobial properties, medicinal plants have long been regarded as a traditional source of antifungal remedies [75]. Many studies demonstrated antifungal activities of Caucasian medicinal plants against different fungal species, including Candida [25,29,36,39,41,46,47,49,50,54,56,63,66]. Significant activity against the Candida species was revealed for the essential oil obtained from the aerial parts of Clinopodium nepeta (L.) Kuntze [43] and the acetone extracts of A. eupatoria plants [36], as well as the methanol extracts of P. harmala [66] and the essential oil obtained from the flowering aerial parts of M. pulegium [46]. Antifungal activities were also observed against Aspergillus sp., Microsporum sp., and T. mentagrophytes for the essential oil obtained from the aerial parts of C. nepeta [43]. Interestingly, essential oils obtained from the flowering aerial part of M. pulegium possessed activity against A. niger [46]. Remarkably, the growth of Fusarium and Bipolaris sp. was inhibited by an essential oil obtained from Laurus nobilis L. leaves [52]. Antifungal activity against Penicillium sp. was also revealed for acetone extracts of A. eupatoria aerial part [58]. Methanol extracts of the aerial parts and roots of Filipendula ulmaria (L.) Maxim. exhibited antifungal activity against a variety of species such as A. alternata, C. albicans, T. longibrachiatum, P. cyclopium, P. canescens, F. oxysporum, A. niger, A. glaucus, T. harzianum, D. stemonitis, and P. fastigiate [61].
In vivo studies of the antibacterial activity of Caucasian medicinal plants are very limited. Thus, in vivo studies demonstrated that a 3% Laurus nobilis L. leaf-supplemented diet in ulcerative colitis rat models increased the population of Bifidobacteria and Lactobacillus and significantly inhibited the growth of Clostridium and sulfate-reducing bacteria [76]. A total alkaloid extract of P. harmala at a concentration of 300 μg/mL decreased brown rot symptoms on potato tubers caused by aerobic, Gram-negative R. solanacearum in vivo [77]. It also was shown that a mixture of Carum copticum (L.) Benth. & Hook.f. ex Hiern essential oil and P. harmala extract encapsulated in chitosan nanoparticles is a superior treatment for the inhibition of fungi A. alternata in both in vitro and in vivo conditions [78]. The healing of infected wounds was promoted by gels prepared from M. pulegium essential oil loaded into nanostructured lipid carriers by increasing antibacterial properties [79]. The efficiency of Allium sativum L. extract against S. flexneri [26] and P. aeruginosa [80] was demonstrated in in vivo studies.
3. Major Groups of Antimicrobial Compounds of Caucasian Medicinal Plants
3.1. Phenolic Compounds
Phenolic compounds are secondary metabolites widely found in all higher plants, which play crucial roles in defense against plant diseases and herbivorous animal aggression [81]. Phenolic compounds are usually divided into simple phenolic compounds, polyphenols, and other phenolic compounds [82]. Simple phenolic compounds include simple phenolics (hydroxyphenols or dihydroxybenzenes) and phenolic acids (hydroxybenzoic and hydroxycinnamic acids, coumarins). Polyphenols include flavonoids, tannins, and stilbenes. Lignans and lignins are classified as other phenolic compounds [82]. Antibacterial, antitoxin, antiviral, and antifungal properties of phenolic compounds were described [83], with the best investigated antibacterial mechanism of polyphenols consisting of their direct binding to the bacterial cell membranes with consequent damage to them. Since Gram-positive bacteria do not possess outer membranes and have peptidoglycans on their surface, they seem to be the most susceptible to phenolic chemicals [84]. Phenolic compounds also have an impact on bacterial DNA structure, morphology, synthesis, and regulation [85]. They can transform pro-oxidants, and the oxidation of polyphenolic substances can lead to the production of hydrogen peroxide, causing DNA breaks [86]. Another mechanism underlying the antibacterial action of phenolic compounds is the inhibition of enzymatic activity [87]. This inhibition occurs through interactions between polyphenols and protein SH groups, as well as through non-specific interactions, contributing to the mechanism of enzyme inhibition [88].
3.1.1. Phenolic Acids
Several representatives of different families of Caucasian medicinal plants considered in this study contained phenolic acids (Table 2). Gallic acid (Scheme 1) was the most commonly detected phenolic acid, found in the bulbs, flowers, and shoots of G. transcaucasicus [28], the bark of J. regia [41], aerial part and roots of F. ulmaria [61], and S. officinalis roots [89]. Gallic acid was the dominant phenolic acid in bulbs of G. transcaucasicus [28], as well as flowers and middle stems of F. ulmaria [60] (Table 2).
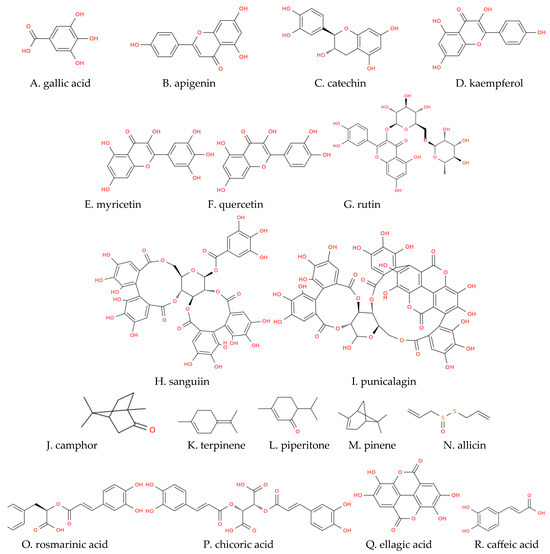
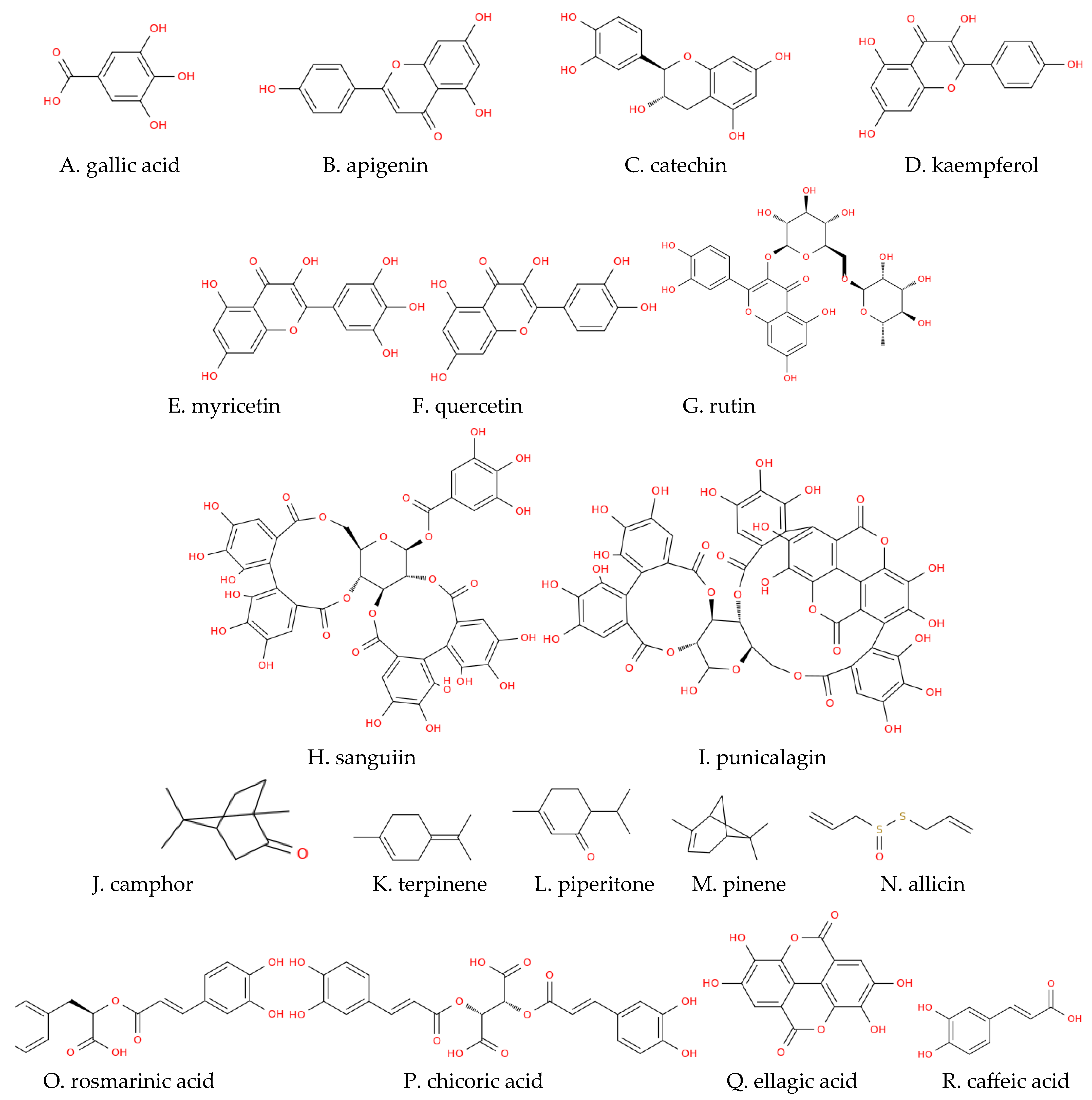
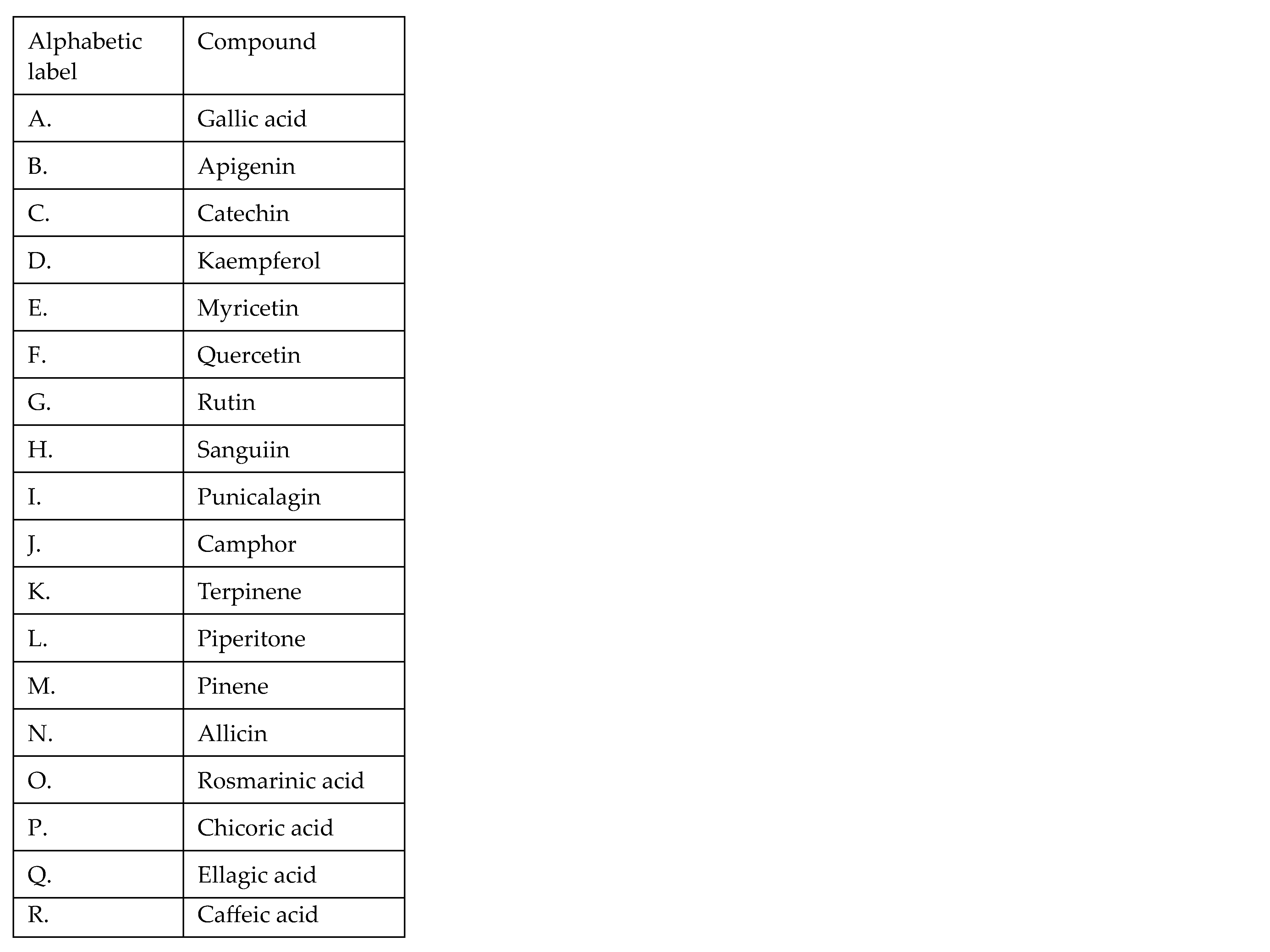
Scheme 1.
Molecular representation of some of the phytochemicals detected in Georgian flora in the order they are mentioned within this work. A list of compound names with their corresponding alphabetic labels is also provided.
The proposed mechanism for the action of phenolic acids involves hyperacidification, affecting cell membrane potential and the operation of the sodium–potassium pump. Gram-positive bacteria are particularly susceptible to this antibacterial mechanism due to the absence of an outer membrane [84]. Additionally, phenolic acids such as gallic acid may disrupt the membrane of Gram-negative bacteria by chelating divalent cations [90]. In their undissociated form, phenolic acids can penetrate the cell membrane through passive diffusion, leading to cytosolic acidification and subsequent protein denaturation [84]. The antibacterial activity of ferulic and gallic acids was tested on E. coli, P. aeruginosa, S. aureus, and L. monocytogenes. For the studied bacteria, an MIC ranging from 100 to 1250 µg/mL was established for ferulic acid, whereas gallic acid acted with an MIC ranging from 500 to 2000 µg/mL [91]. It was concluded that gallic and ferulic acid reduce the negative surface charge, leading to local membrane rupture or pore formation and consequent leakage of essential intracellular constituents [91]. p-Coumaric acid was found in various parts of several Caucasian medicinal plants, including the bulbs of A. sativum and A. ursinum [25], leaves of J. regia [92], L. nobilis [49], leaves, flowers, and fruits of F. ulmaria [60], and the aerial part of S. officinalis [89]. Investigations into the antibacterial activity mechanism of p-coumaric acid unveiled a dual mechanism: it disrupts bacterial cell membranes and can bind to the phosphate anion in the DNA double helix, thereby intercalating into the DNA groove and affecting replication, transcription, and expression [93]. Phenolic acids have demonstrated in vitro and in vivo activity against Candida species [94], suggesting that, akin to the antibacterial effect, the antifungal effect may be linked to the impairment of cell surface hydrophobicity and charge [94]. Additionally, the impact of caffeic acid derivatives on 1,3-β-glucan synthase has been observed in the cell wall of C. albicans [95].
3.1.2. Flavonoids
Different subclasses of flavonoids were detected in extracts of Caucasian medicinal plants (Table 2). Flavonoids exhibit multiple targets within bacterial cells, with their interaction with the cell membrane being the most extensively investigated mechanism [84]. Flavonoids with higher hydrophobicity can partition into the hydrophobic core of membranes. At the same time, those with greater hydrophilicity interact via hydrogen bonding with the polar head groups at the lipid–water interface, altering the physical and chemical properties of the membrane [96]. For instance, naringenin and sophoraflavanone were shown to reduce the fluidity of both the outer and inner membrane layers of bacterial cells [97]. The predominant group of flavonoids identified in Caucasian medicinal plants was flavanols (flavan-3-ols), encompassing apigenin, catechin and its derivatives, kaempferol, myricetin, quercetin, and rutin [98] (Scheme 1). The presence of apigenin was demonstrated in G. transcaucasicus flowers [28], L. nobilis leaves [49], and in A. eupatoria plants [99]. Catechin and its derivatives were detected in F. ulmaria leaves and roots [60], as well as in leaves, roots, and flowers of S. officinalis [64] and the fruits of R. canina [100]. Catechin and its derivatives compose the major fraction of flavonoids in flowers of S. officinalis [64]. Kaempferol was found in bulbs and was a major flavonoid in shoots of G. transcaucasicus [28] and L. nobilis leaves [49]; a derivative of kaempferol was found in S. officinalis leaves [64]. Quercetin and its derivatives were detected in G. transcaucasicus flowers and shoots [28], L. nobilis leaves [49], the aerial part of F. ulmaria [61], R. canina fruits [100], and in leaves and roots of S. officinalis [64]. Quercetin was the major flavonoid in G. transcaucasicus flowers [28]. On the other hand, rutin was revealed in G. transcaucasicus bulbs [28], F. ulmaria leaves, flowers, roots, and fruits [60], and R. canina fruits [100], whereas L. nobilis leaves contained myricetin [49], and it was also present in R. canina fruits [100]. Significant antibacterial activity of catechins against both Gram-positive and Gram-negative bacteria has been demonstrated, attributed to their ability to impair membrane integrity or induce membrane fusion [101,102,103]. This ability is associated with a high amount of phenolic hydroxyl groups, determining the high affinity of catechins for lipids, proteins, and nucleic acids [104]. Quercetin, apigenin, and sakuranetin were shown to possess a competitive inhibitory effect against bacterial enzymes involved in the type II fatty acid biosynthesis pathway: β-hydroxyacyl-acyl carrier protein dehydratase and β hydroxyacyl-ACP dehydrase [105]. It was suggested that inhibiting these enzymes impairs the lipid homeostasis of bacteria during both growth and stationary phases [106]. Myricetin inhibited the growth of Gram-positive and Gram-negative bacterial species via the inhibition of DNA helicase RepA and ATPase activities [107]. Rutin eradicated P. aeruginosa via a reduction in the production of protease, pyocyanin, rhamnolipid, and elastase and the disruption of membrane integrity [108]. Similarly, the bacteriostatic effect of kaempferol was mainly associated with the disruption of cellular integrity and leakage of cell contents [109]. The high antifungal activity of flavonoids against a wide range of pathogenic organisms was reviewed in [110]. In general, the antifungal action of flavonoids was associated with different mechanisms. Similarly to the case of their antibacterial action, these mechanisms involved plasma membrane disruption [111] and the effect of flavonoids on RNA and proteins [110]. However, it was demonstrated that flavonoids also induce mitochondrial dysfunction. Thus, the treatment with the flavone wogonin induced the accumulation of reactive oxygen species (ROS) in mitochondria and caused decreased membrane potential, as well as a reduction in ATP synthesis, and eventually, the contraction or cracking of fungal filaments [112]. Honey flavonoid extracts also inhibited cell division, preventing the proliferation of C. albicans phenotypes [113]. The inhibition of efflux-mediated pumps by many flavones (apigenin, chrysin, baicalein, luteolin, 6-hydroxyflavone, etc.), leading to fungi cell death, was demonstrated [114,115].
3.1.3. Tannins
Tannins were detected in many species of Caucasian plants including J. regia leaves [92], A. rosea plants [53], R. obtusifolius seeds [99], A. eupatoria plants [99], the aerial part of S. officinalis [99], and the leaves, roots, and flowers of S. officinalis [64] (Table 2). A. rosea plants also contained phlobatannins [53], another class of ring-isomerized condensed tannins [116]. In studies where tannins were identified, mainly hydrolyzed tannins such as sanguiin and punicalagin gallate (Scheme 1) were revealed in Caucasian plants (Table 2). Hydrolyzable tannins have a polyhydric alcohol at their core, with the hydroxyl groups partially, or fully, esterified with either gallic or hexahydroxydiphenic acid [117]. The number of hydroxyl groups in tannins was used as a marker for assessing the antibacterial properties, positively associated with antioxidant characteristics [118]. Tannins inhibit the growth of diverse microbes, such as Gram-positive and Gram-negative bacteria, fungi, and yeasts [119]. For the majority of tannins, a bacteriostatic effect rather than bactericidal activity was revealed [120]. Tannins inhibited bacterial growth using different action mechanisms including iron chelation [119] and the inhibition of cell wall synthesis via inactivation of enzymes involved in cell wall synthesis or by binding to the cell wall [121]. Tannins also alter the structure of the bacterial membranes in S. aureus, increasing fluidity and disrupting the formation of virulent membrane vesicles, thus acting as potential enhancers of antibiotics [122]. Moreover, tannins affect the integrity and permeability of the cell wall and membrane by raising intracellular Ca2+ concentrations and affecting the activities of alkaline phosphatase and Na+/K+-ATPase [123], and tannin-loaded nanoparticles and hydrogels have demonstrated profound antibacterial effects [124]. Additionally, the antifungal effects of hydrolysable tannins were demonstrated against filamentous fungi and opportunistic yeasts [125], with the proposed mechanism of action involving the disruption of the cell wall and the plasma membrane, inducing leakage of the intracellular contents, such as sugars, as was demonstrated for the cell wall of P. digitatum [126].
3.2. Terpenes
Terpenes represent a large group of hydrocarbons consisting of five-carbon isoprene (C5H8) units as their basic building block. The modified family of terpenes are terpenoids, synthesized by the addition/removal of functional groups to/from terpenes [127] and comprising 40,000 compounds including terpenoid-derived indole alkaloids [128]. Terpenes and terpenoids were detected in the aerial part and the roots of E. caucasicum [30,31], A. fragrans aerial parts [32], roots [34] and flowers [33], and P. fraxinifolia stems [42], as well as in aerial parts of C. nepeta [43,44], M. pulegium [46,47], and T. caucasicus [48] and the leaves of L. nobilis [50]. In these Caucasian medicinal plants, camphor, terpinene, piperitone, pinene (Scheme 1), and their derivatives were the most frequently detected terpenes (Table 2). The antimicrobial and antifungal activity of terpenes and terpenoids was demonstrated and many studies were reviewed in [129]. Thus, a nanogel containing camphor and thymol provided complete growth suppression against P. aeruginosa and S. aureus [130]. Additionally, antibacterial properties of terpinen-4-ol against E. faecalis, P. gingivalis, P. intermedia, and F. nucleatum were demonstrated [131]. Piperitenone epoxide exhibited high antimicrobial efficiency against 28 strains of S. aureus and 10 strains of E. coli [132]. Antimicrobial and antifungal effects of α- and β-pinene were reported in many studies and reviewed in [133]. The proposed mechanism of antibacterial action of this class of compounds is the disruption of the bacterial membrane via the induction of oxidative stress and the impairment of several pathways involved in the bacterial membrane repair system, as was demonstrated in the study on K. pneumoniae [134]. The antifungal activity of terpenes against C. albicans, S. aureus, and P. aeruginosa was also demonstrated [135,136], with the proposed antifungal mechanism being the activation of specific downstream signaling pathways, which leads to the activation of genes involved in alternate metabolic and energy pathways. Moreover, drug efflux was prominently upregulated by terpenes which also caused the repression of genes mediating ribosome biogenesis and RNA metabolism [137].
3.3. Saponins
Saponins are natural compounds containing one or more sugar (glycon) and non-sugar parts (aglycon) connected via glycosidic bonds [138]. Due to the glycosylation of the hydrophobic aglycones, they can act as biological detergents and, when agitated in water, form foams (like in soap), which gave rise to the name of this group of compounds [139]. Saponins were found in aerial parts of H. alpestre [99], C. coum [55], A. rosea [53], A. eupatoria [99], A. cappadocicum [65], P. harmala plants [140], and R. obtusifolius seeds [99]. The biological properties such as antibacterial, anti-inflammatory, antifungal, and antiviral activities of various saponins were demonstrated [141,142], with the antibacterial and antifungal properties of saponins being associated with their detergent-like properties, providing increased permeability of bacterial cell membranes [138].
3.4. Alkaloids
Alkaloids are a large and structurally diverse group of natural products, detected in about 300 plant families [143]. Based on their chemical structure, alkaloids can be divided into three different types: true alkaloids (heterocyclics), protoalkaloids (non-heterocyclics), and pseudoalkaloids [144]. Among the investigated Caucasian plants, bioactive alkaloids were revealed in bulbs of G. transcaucasicus (native to Armenia, Azerbaijan, and Georgia) [29], A. rosea [53], A. cappadocicum [65], and P. harmala [66] plants. However, the specific types of alkaloids were not identified. Alkaloids inhibit bacterial growth through a variety of mechanisms; the most well-studied mechanism involves the inhibition of bacterial nucleic acid and protein synthesis [145]. Thus, the inhibitory action of berberine on DNA replication, RNA transcription, and protein biosynthesis in bacteria was shown [145]. Remarkably, sanguinarine inhibited the assembly of filamentous temperature-sensitive protein Z (FtsZ), essential in the process of bacterial cell division [146]. Moreover, alkaloids affect cell membrane permeability, causing damage to the cell membrane and cell wall [145,147]. Another mechanism of the antibacterial action of alkaloids is the inhibition of the efflux pump. This mechanism was demonstrated in the study of the effect of alkaloids extracted from Callistemon citrinus Skeels on P. aeruginosa [148]. Alkaloids are also capable of inhibiting various pathways of the bacterial metabolism. Thus, berberine increased the conversion and uptake of carbohydrates and decreased carbohydrate consumption by S. pyogenes [149]. A biological alkaline solution of Aconitum carmichaeli var. carmichaeli inhibited the metabolism of S. aureus [145]. At least 70 different plant-derived alkaloids were reviewed in [150] and were shown to possess significant antifungal activity in vitro. Similarly to the mechanism of antibacterial action, the antifungal action of alkaloids was related to membrane permeabilization, as well as to the inhibition of DNA, RNA, and protein synthesis [151].
3.5. Sulfur-Containing Compounds of Allium Species
Extracts of medicinal plants of the Alliaceae family found in the Caucasus area (including A. atroviolaceum and A. ursinum) were characterized by a high content of sulfur-containing compounds with proven antimicrobial, antioxidant, or antitumor activity [23,25,152]. Amongst the sulfur-containing compounds revealed in various Allium species discussed here, the most well-known and well-investigated compound is allicin (diallyl thiosulphate, Scheme 1), the major sulfur-containing compound in bulbs of A. sativum bulbs [153]. Antifungal and antimicrobial activities of allicin have been well known for a long time [153,154]. The antimicrobial and antifungal activity of allicin has been associated with its action as the inhibitor of sulfhydryl-dependent enzymes. This suggestion was supported by the finding that inhibition was alleviated or reduced by cysteine and glutathione [152,155]. The sulfur-containing compound ajoene from A. sativum caused a significant clearing of P. aeruginosa in a pulmonary infection model in mice in vivo [156]. Diallyl sulfide and diallyl disulfide isolated from A. sativum inhibited methicillin-resistant S. aureus infection in diabetic mice [157].
In summary, the investigation into major groups of antimicrobial compounds derived from Caucasian medicinal plants reveals a rich diversity of bioactive substances with significant potential for therapeutic applications. Phenolic compounds, including phenolic acids, flavonoids, and tannins, were prominently identified and exhibited multifaceted mechanisms of antimicrobial action. Phenolic acids, such as gallic acid and p-coumaric acid, exhibited antibacterial effects through membrane disruption and enzyme inhibition. Flavonoids, such as quercetin and rutin, showed antibacterial and antifungal properties by altering membrane integrity and interfering with bacterial enzymes. Tannins, particularly hydrolyzable tannins like sanguiin and punicalagin, exerted bacteriostatic effects and disrupted bacterial membranes and cell walls. Terpenes and terpenoids, abundant in many Caucasian medicinal plants, displayed antimicrobial and antifungal activities by disrupting bacterial membranes and inducing oxidative stress. Saponins, another group of natural compounds found in several plants, exhibited antibacterial properties attributed to their detergent-like effects, increasing bacterial cell membrane permeability. Alkaloids, identified in various plant species, inhibited bacterial nucleic acid and protein synthesis, damaged cell membranes, and inhibited efflux pumps, thereby exerting antimicrobial effects. Sulfur-containing compounds, particularly allicin from Allium species, demonstrated potent antimicrobial and antifungal activities by inhibiting sulfhydryl-dependent enzymes. Overall, the diverse array of antimicrobial compounds present in Caucasian medicinal plants offers promising avenues for the development of novel antimicrobial agents to combat infectious diseases. In conclusion, while Section 3 provides a comprehensive overview of the major groups of antimicrobial compounds found in Caucasian medicinal plants, it is essential to acknowledge some limitations and areas for further exploration. One notable gap is the need for more extensive studies elucidating the specific mechanisms of action of these compounds against various pathogens. While many studies have demonstrated the antimicrobial efficacy of phenolic compounds, terpenes, saponins, alkaloids, and sulfur-containing compounds, there remains a lack of clarity regarding their precise modes of action and potential synergistic effects. Additionally, further research is needed to optimize extraction methods to maximize the yield of bioactive compounds from medicinal plants while minimizing environmental impact. Moreover, the pharmacokinetics and bioavailability of these compounds in vivo warrant investigation to assess their potential as therapeutic agents for treating infectious diseases. Overall, continued interdisciplinary research efforts are necessary to unlock the full therapeutic potential of antimicrobial compounds derived from Caucasian medicinal plants and address the pressing global challenge of antibiotic resistance.

Table 2.
Bioactive compounds with antimicrobial and antifungal activity revealed in Caucasian medicinal plants (susceptible microorganisms are shown in Table 1). Quantitative data on compound contents are shown when available.
Table 2.
Bioactive compounds with antimicrobial and antifungal activity revealed in Caucasian medicinal plants (susceptible microorganisms are shown in Table 1). Quantitative data on compound contents are shown when available.
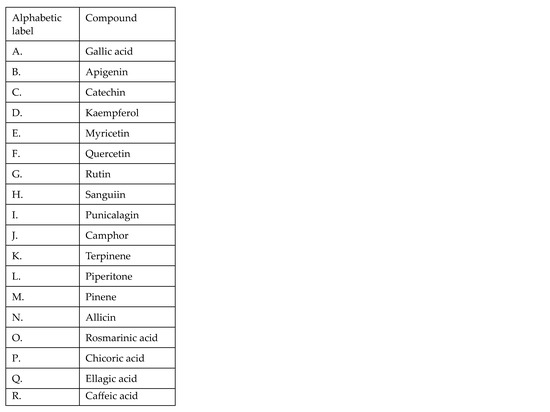
| Family | Plant Species | Plant Part | Extract Type | Class of Bioactive Compound | Bioactive Compound | Susceptible Microorganisms | References |
|---|---|---|---|---|---|---|---|
| Alliaceae | A. atroviolaceum | Bulb | essential oil | Sulfur-containing compounds | methyl methyl thiomethyl disulfide (61%) dimethyl trisulfide (15%) methyl allyl disulfide (4%) | Gram-positive | [158] |
| A. sativum | aqueous extract | Simple phenolic compounds (phenolic acids) | gentisic acid 38 μg/g FW chlorogenic acid 36 μg/g FW 4-hydroxybenzoic acid 16 μg/g FW p-coumaric acid 26 μg/g FW | Gram-positive, Gram-negative, fungi | [25,156,157] | ||
| Sulfur-containing compounds | alliin 1580 38 μg/g FW allicin 280 μg/g FW ajoene diallyl sulfide diallyl disulfide | ||||||
| A. ursinum | aqueous extract | Simple phenolic compounds (phenolic acids) | chlorogenic acid 40 μg/g FW p-coumaric acid 102 μg/g FW | Gram-positive, Gram-negative, fungi | [25] | ||
| Sulfur-containing compounds | alliin 260 μg/g FW allicin 130 μg/g FW | ||||||
| Amaryllidaceae | G. transcaucasicus | Bulb | 99% methanol extract | Polyphenols (flavonoids) | naringin kaempferol rutin | Gram-positive, Gram-negative, fungi | [28] |
| Simple phenolic compounds (phenolic acids) | gallic acid 439.5 μg/g DW syringic acid 117.7 μg/g DW ferulic acid 244.2 μg/g DW | ||||||
| Bulb | 96% ethanol extract | Alkaloids Sterols Cardiac glycosides | Gram-positive, Gram-negative, fungi | [29] | |||
| Flower | 99% methanol extract | Polyphenols (flavonoids) | naringin 72.6 μg/g DW quercetin 915.5 μg/g DW apigenin 67.1 μg/g DW genistein 131.5 μg/g DW | Gram-positive, Gram-negative | [28] | ||
| Simple phenolic compounds (phenolic acids) | gallic acid 112.1 μg/g DW syringic acid 926.2 μg/g DW | ||||||
| Shoot | 99% methanol extract | Polyphenols (flavonoids) | naringin 112.9 μg/g DW quercetin 259.3 μg/g DW kaempferol 411.5 μg/g DW genistein 202 μg/g DW | Gram-positive, Gram-negative | [28] | ||
| Simple phenolic compounds (phenolic acids) | gallic acid 345.8 μg/g DW syringic acid 705.5 μg/g DW ferulic acid 412 μg/g DW | ||||||
| Apiaceae | E. caucasicum | Roots | essential oil | Fatty Acid Esters | hexyl isovalerate hexyl valerate | Gram-positive, Gram-negative | [30] |
| Terpenes | trans-pinocarvyl acetate | ||||||
| Aerial part | Fatty Acid Esters | hexyl isovalerate | [31] | ||||
| Terpenes | trans-pinocarvyl acetate caryophyllene oxide | ||||||
| Shoots | 80% methanol extract | Simple phenolic compounds (phenolic acids) | rosmarinic acid chicoric acid (Scheme 1) | [159] | |||
| Asteraceae | A. fragrans | Aerial part | essential oil | Terpenes | α-thujone β-thujone 1,8-cineole davanone d camphor cadinol verbenene ortho-oci-men | Gram-positive, Gram-negative | [32] |
| Leaves | essential oil | Terpenes | Chrysanthenon 23.8% 1,8-cineole 23.7% β-caryophyllene 9.6% p-cymene 7.7% filifolide-A 5.7% filifolone 5.7% camphor terpinene-4-ol artemisyl acetate camphene | Gram-positive, Gram-negative | [33,34] | ||
| Roots | essential oil | Terpenes | camphor 67% camphene 16.9% | Gram-positive, Gram-negative | [34] | ||
| Stem | essential oil | Terpenes | camphor 1,8-cineole borneol artedouglasia oxide a chrysanthenyl acetate | Gram-positive, Gram-negative | [33] | ||
| Flowers | essential oil | Terpenes | camphor 1,8-cineole terpinene-4-ol borneol carvacrol | Gram-positive, Gram-negative | [33] | ||
| Hypericaceae | H. alpestre | Aerial part | 99% methanol extract | Saponins Steroids Polyphenols | Flavonoids Coumarins | Gram-positive, Gram-negative, fungi | [99] |
| Juglandaceae | J. regia | Leaves | 80% methanol extract | Polyphenols (flavonoids) | - | Gram-positive, Gram-negative | [38] |
| 99% methanol extract | Polyphenols (tannins) Antioxidants | alpha-tocopherol | Gram-positive, Gram-negative | [92] | |||
| Simple phenolic compounds (phenolic acids) | caffeic acid p-coumaric acid ellagic acid malic acid chlorogenic acid | ||||||
| Bark | 99% methanol extract | Simple phenolic compounds (phenolic acids) | chlorogenic acid caffeic acid ferulic acid sinapic acid gallic acid ellagic acid vanillic acid | Gram-positive, Gram-negative, fungi | [41] | ||
| Green husks | 99% methanol extract | Simple phenolic compounds (phenolic acids) | coumaric acid ellagic acid chlorogenic acid | Gram-positive, Gram-negative, fungi | [41] | ||
| P. fraxinifolia | Stem | essential oil | Terpenes Fatty Acids | 2,4-heptadienal hexanol 2-pyrrolidinone menthone menthol thymol vinylguajacol hexadecanoic acid | Gram-positive, Gram-negative, fungi | [42] | |
| Lamiaceae | C. nepeta | Aerial part | essential oil | Terpenes | piperitenone oxide 47.8% limonene 18.6% piperitone oxide 13.6% 6-hydroxycarvotanacetone 5.1% | Gram-positive, Gram-negative, fungi | [43,44] |
| M. pulegium | Flowering aerial part | essential oil | Terpenes | piperitone 38% piperitenone 33% α-terpineol 4.7% 1,8-cineole menthone 4% borneol 3% pulegone 0.6% | Gram-positive, Gram-negative, fungi | [46,47] | |
| T. caucasicus | Aerial part | essential oil | Terpenes | 1,8-cineol 21.5% thymol 12.6% β-fenchyl alcohol 8.7% nerolidol 7.8% terpinolene 7.2% α-pinene 7% myrcene 6.8% | Gram-positive, Gram-negative, fungi | [48] | |
| Lauraceae | L. nobilis | Leaves | essential oil | Simple phenolic compounds (phenolic acids) | chlorogenic acid 48.1 μg/g DW caffeic acid 789.3 μg/g DW p-coumaric acid 375. 9 μg/g DW sinapic acid 1513.9 μg/g DW ferulic acid 70.4 μg/g DW cinnamic acid 513.4 μg/g DW | Gram-positive, Gram-negative, fungi | [49,50] |
| Simple phenolic compounds (phenolic acids) | protocatechuic acid 68.6 μg/g DW salicylic acid 29. 4 μg/g DW syringic acid 789.1 μg/g DW | ||||||
| Polyphenols (flavonoids) | myricetin 47.2 μg/g DW quercetin 44.9 μg/g DW kaempferol 688.1 μg/g DW luteolin 839.1 μg/g DW apigenin 262.7 μg/g DW hesperetin 31.2 μg/g DW | ||||||
| Terpenes | 1,8-cineole 31.9% a-terpinyl acetate 5.9% β-pinene 2.5% sabinene 8.8% β-linalool 4.9% piperitenone isomenthone pulegone | [50,52,160] | |||||
| Malvaceae | A. rosea | Whole plant | 98% ethyl acetate extract | Saponins Phenolic compounds (tannins and phlobtannins) Terpenoids Alkaloids Cardiac glycosides | - | Gram-positive, Gram-negative | [53] |
| Polygonaceae | R. obtusifolius | Seeds | 99% methanol extract | Saponins Terpenoids Phenolic compounds Coumarins | - | Gram-positive, Gram-negative, fungi | [99] |
| 99.8% acetone extract | Polyphenols (tannins and flavonoids) | - | |||||
| Primulacea | C. coum | Aerial part | 99% methanol extract | Proteins Phenolic compounds Saponins Cardiac glycosides Steroids | - | Gram-positive, fungi | [55] |
| P. macrocalyx | Whole plant | 99% methanol extract | Polyphenols (flavonoids) | 3′-methoxyflavone 2′-methoxyflavone 2′,5′-dimethoxyflavone 2′-methoxy-5′-hydroxyflavone 3′-hydroxy-4′,5′-dimethoxyflavone 5,6,2′,6′-tetramethoxyflavone 5,6,2′,3′,6′-pentamethoxyflavone 3′-hydroxyflavone 2′-hydroxyflavone 5,6,8,2′,6′-pentamethoxyflavone 5,6,2′-trimethoxyflavone | Fungi | [56] | |
| Rosaceae | A. eupatoria | Whole plant | 99% methanol extract | Saponins Steroids Polyphenols (tannins) | luteolin apigenin | Gram-positive, Gram-negative, fungi | [99] |
| 99.8% acetone extract | Steroids Phenolic compounds | - | |||||
| F. ulmaria | Middle leaves | 60% ethanol extract | Simple phenolic compounds (phenolic acids Polyphenols (flavonoids) | gallic acid 0.8 mg/g extract caftaric acid 0.6 mg/g extract chlorogenic acid 1.3 mg/g extract p-coumaric acid 0.2 mg/g extract catechin 4.1 mg/g extract rutin 4.8 mg/g extract isoquercitrin 2.6 mg/g extract ellagic acid 0.4 mg/g extract | Gram-positive, Gram-negative | [60] | |
| Middle stem | 60% ethanol extract | Simple phenolic compounds (phenolic acids) Polyphenols (flavonoids) | gallic acid 1.3 mg/g extract caftaric acid 0.05 mg/g extract chlorogenic acid 0.2 mg/g extract ellagic acid 0.4 mg/g extract isoquercitrin 0.07 mg/g extract | Gram-positive, Gram-negative | [60] | ||
| Flowers | 60% ethanol extract | Simple phenolic compounds (phenolic acids) Polyphenols (flavonoids) | gallic acid 5.8 mg/g extract caftaric acid 2.9 mg/g extract chlorogenic acid 0.3 mg/g extract caffeic acid 0.1 mg/g extract p-coumaric acid 0.04 mg/g extract ellagic acid 5.8 mg/g extract rutin 4.2 mg/g extract isoquercitrin 2.4 mg/g extract spiraeoside 20.4 mg/g extract cymaroside 0.09 mg/g extract | Gram-positive, Gram-negative | [60] | ||
| Fruits | 60% ethanol extract | Simple phenolic compounds (phenolic acids) Polyphenols (flavonoids) | gallic acid 4.3 mg/g extract caftaric acid 1.5 mg/g extract chlorogenic acid 0.6 mg/g extract p-coumaric acid 0.7 mg/g extract caffeic acid 0.07 mg/g extract ellagic acid 3.4 mg/g extract rutin 2.1 mg/g extract spiaeoside 2.4 mg/g extract isoquercitrin 0.5 mg/g extract | Gram-positive, Gram-negative | [60] | ||
| Aerial part | 99% methanol extract | Simple phenolic compounds (phenolic acids) Polyphenols (flavonoids) | gallic acid 7.02 mg/g extract ellagic acid 8.9 mg/g extract rutin 6.2 mg/g extract quercetin 15. 5 mg/g extract catechin 11.3 mg/g extract | Gram-positive, Gram-negative, fungi | [61] | ||
| Roots | 60% ethanol extract | Simple phenolic compounds (phenolic acids) Polyphenols (flavonoids) | gallic acid 0.1 mg/g extract salicylic acid 0.6 mg/g extract ellagic acid 1.2 mg/g extract catechin 8.0 mg/g extract rutin 0.7 mg/g extract isoquercitrin 0.05 mg/g extract | Gram-positive, Gram-negative, fungi | [60] | ||
| Roots | 99% methanol extract | Polyphenols (flavonoids) | catechin 17.2 mg/g extract epicatechin 3.1 mg/g extract | Gram-positive, Gram-negative, fungi | [61] | ||
| R. canina | Fruits | hexane/acetone/ethanol (2:1:1), and 0.05% (w/v) butylated hydroxytoluene extract | Carotenes | carotene lycopene | Gram-positive, Gram-negative, fungi | [63] | |
| Acetone/water (80:20 v/v) extract | Simple phenolic compounds (phenolic acids) Polyphenols (flavonoids) | vanilic acid 260 μg/kg DW cafeic acid 2 μg/kg DW syringic acid 110 μg/kg DW gallic 298 μg/kg DW ellagic acid 80 μg/kg DW procatechuic acid 210 μg/kg DW myricetin 5.4 μg/kg DW rutin 22 μg/kg DW catechin 11.9 μg/kg DW quercetin 1.5 μg/kg DW | [100] | ||||
| S. officinalis | Aerial part | 99% methanol extract | Phenolic compounds (tannins, flavonoids and coumarins) Steroids Glycosides Quinones | - | Gram-positive, Gram-negative, fungi | [99] | |
| petroleum ether extract, followed by extraction with 80% methanol | Simple phenolic compounds (phenolic acids) | caffeic acid p-coumaric acid syringic acid vannilic acid ferulic acid | [89] | ||||
| Roots | 70% ethanol extract | Polyphenols (tannins) | 2,3-hexahydroxydiphenoyl-glucose 15.3 mg/g DW sanguiin H-10 derivative 9 mg/g DW punicalagin gallate 3.8 mg/g DW sanguiin H-1 7.7 mg/g DW galoyl-bis-hexahydroxydiphenyl-glucoside, isomer 2.8 mg/g DW ellagic acid 2.3 mg/g DW | Gram-positive, Gram-negative, fungi | [64] | ||
| Polyphenols (flavonoids) | c-type (epi)catechin trimer 10.5 mg/g DW b-type (epi)catechin dimer catechin 17.2 mg/g DW | ||||||
| Simple phenolic compounds (phenolic acids) | 3-caffeoylquinic acid caffeic acid-glucoside chlorogenic acid p-coumaroylquinic acid ellagic acid | ||||||
| petroleum ether extract, followed by extraction with 80% methanol | Simple phenolic compounds (phenolic acids) | gallic acid protocatechuic acid | [89] | ||||
| Leaves | 70% ethanol extract | Polyphenols (tannins) Polyphenols (flavonoids) Simple phenolic compounds (phenolic acids) | 2,3-hexahydroxydiphenoyl-glucose 6.9 mg/g DW sanguiin H-10 derivative 1.9 mg/g DW punicalagin gallate 9.9 mg/g DW sanguiin H-1 8.3 mg/g DW b-type (epi)catechin dimer 6.1 mg/g DW catechin 7.4 mg/g DW quercetin-galloyl-glucoside 2.9 mg/g DW quercetin-glucoside 18.6 mg/g DW kaempferol-glucuronide 7.6 mg/g DW 3-caffeoylquinic acid 1 mg/g DW caffeic acid-glucoside 2.4 mg/g DW chlorogenic acid 1.6 mg/g DW p-coumaroylquinic acid 2.8 mg/g DW | Gram-positive, Gram-negative | [64] | ||
| Flowers | 70% ethanol extract | Polyphenols (tannins) Polyphenols (flavonoids) Simple phenolic compounds (phenolic acids) | 2,3-hexahydroxydiphenoyl-glucose 12.6 mg/g DW sanguiin H-10 derivative 8.3 mg/g DW punicalagin gallate 11.1 mg/g DW sanguiin 19.7 mg/g DW ellagic acid pentoside 2.6 mg/g DW cyanidin-glucoside 0.5 mg/g DW b-type (epi)catechin dimer 5 mg/g DW catechin 2.3 mg/g DW 3-caffeoylquinic acid 2.1 mg/g DW caffeic acid-glucoside 5.4 mg/g DW chlorogenic acid 2.2 mg/g DW p-coumaroylquinic acid 3.1 mg/g DW | Gram-positive, Gram-negative | [64] | ||
| Sapindaceae | A. cappadocicum | Whole plant | 99% methanol extract | Alkaloids Saponins Flavone glycosides Quinones | Gram-positive, Gram-negative, fungi | [65] | |
| Zygophyllaceae | P. harmala | Whole plant | 99% methanol extract | Alkaloids Saponins Flavone glycosides | peganine harmaline | Gram-positive, Gram-negative, fungi | [66,140] |
4. Mechanisms of Action of Antibacterial and Antifungal Plant Compounds
Bacterial infections pose an escalating threat to human health worldwide. While antibiotics have historically provided an effective means of treating such infections, the widespread and often excessive use of these drugs has led to the emergence and spread of antibiotic-resistant bacteria. As a consequence, antimicrobial resistance has become a pressing global concern, resulting in the loss of efficacy of many antibiotics, and, tragically, this phenomenon contributes to the deaths of at least 700,000 people annually across the globe [161]. The first reports of antibiotic resistance date back to the 1950s with Salmonella, Shigella, and E. coli species [162]. However, the comprehension of the mechanisms providing bacterial resistance took several decades [163]. In contrast, research into resistance against antifungal agents has progressed more slowly, likely due to the recognition of mycoses as a significant threat in the mid-1970s (as reviewed in [164]).
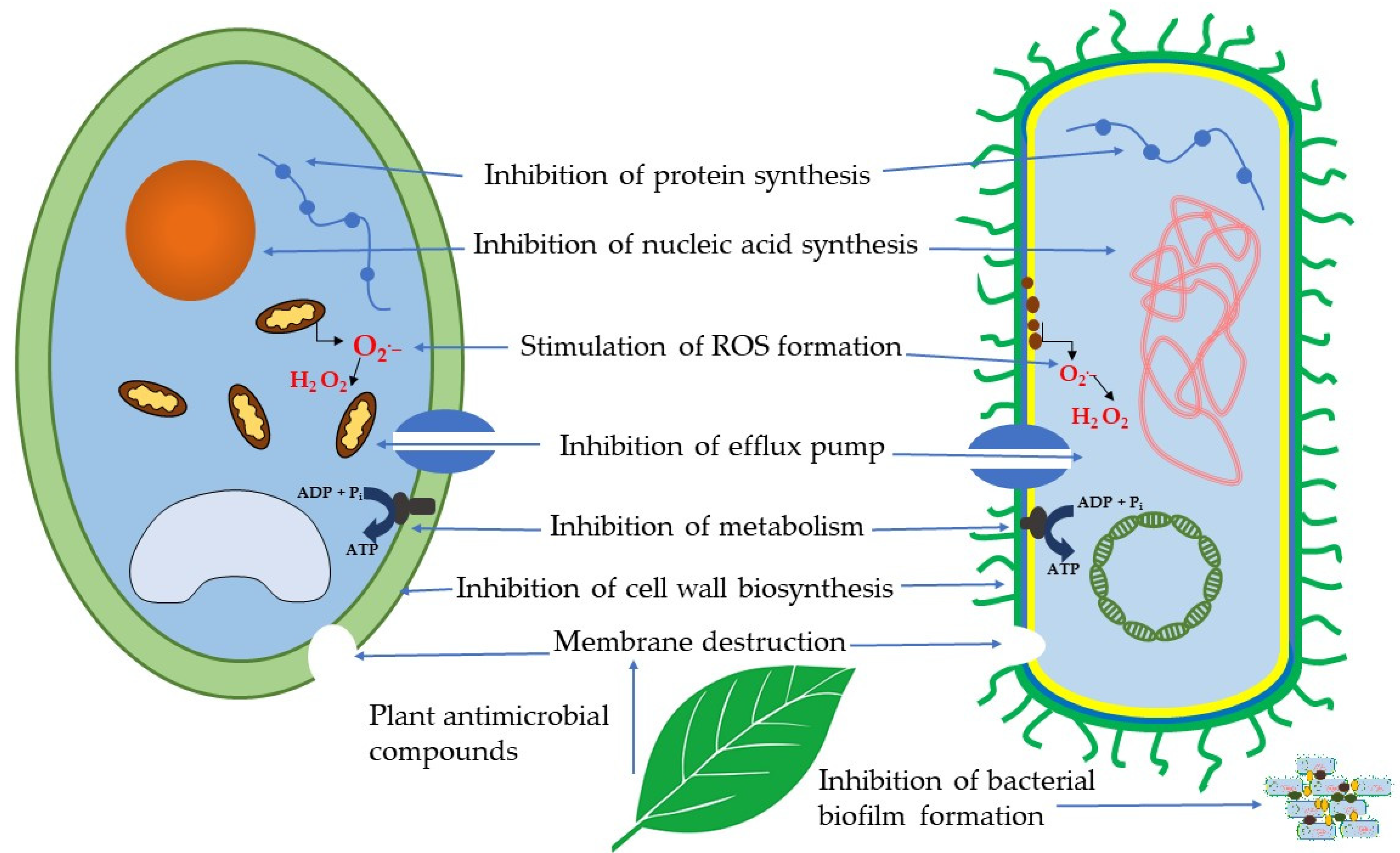
As was discussed above, plants produce a variety of secondary metabolites, such as phenolic compounds, terpenes, saponins, alkaloids, and sulfur-containing compounds. These compounds have been used since ancient times in folk medicine for the treatment of various diseases [73]. Since phytochemicals can act via different mechanisms or target sites different from those of antibiotics, their use either alone or in combination with antibiotics can be efficient for the suppression of bacterial resistance [11]. The current elucidated mechanisms of action of antibacterial and antifungal secondary metabolites as antimicrobial agents are related to a variety of targets in bacterial and fungal cells (Figure 2).
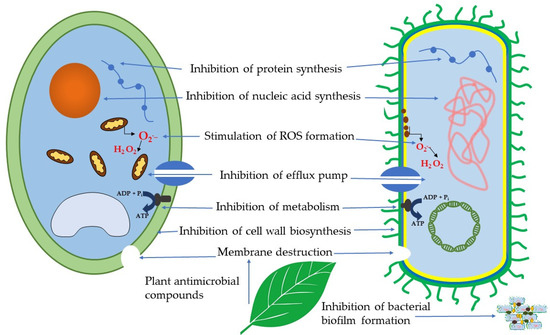
Figure 2.
Mechanisms of action of antibacterial and antifungal plant compounds.
4.1. Membrane Destruction
Similar to certain antibiotics, like polymyxins, which induce structural alterations in bacterial membranes [165], plant-derived bioactive compounds are capable of causing the destruction of bacterial cell membranes. This ability has been reported for various classes of phenolic compounds [166]. For example, quinones bind to the adhesin complex on the cell wall, eventually leading to its lysis [167]. Experimental studies on the interaction between flavonoids and biomembranes have shown that flavonoids with a planar configuration, such as quercetin, rutin, and tiliroside, reduce the thickness and fluidity of lipid bilayers, thereby increasing membrane permeability [168]. Tannins have been shown to deactivate microbial adhesins, enzymes, and membrane transporter systems [169]. Terpenes, on the other hand, break down the outer membrane of various Gram-negative bacteria, causing the release of lipopolysaccharides [170]. Alkaloids derived from Dicranostigma leptopodum (Maxim.) Fedde altered the cell permeability of K. pneumoniae, exerting a significant antibacterial effect on its growth [145]. Terpenes, owing to their lipophilic properties, can traverse the phospholipid bilayer of bacteria, demonstrating antibacterial or bactericidal effects [171]. The efficacy of several terpenes (carvacrol, thymol, eugenol) against S. typhimurium, E. coli, P. fluorescens, B. thermosphacta, and S. aureus was examined, revealing membrane damage [172]. Flavonoids modified the cell membrane of Candida spp., enhancing cell permeability and inhibiting the function of plasma membrane proteins [173]. The alkaloid tomatidine, isolated from Solanum tuberosum L., inhibited two enzymes involved in ergosterol biosynthesis in C. albicans, C. krusei, and S. cerevisiae [174].
4.2. Inhibition of Cell Wall Biosynthesis
The bacterial cell wall, composed of a network of peptide and glycan strands that are covalently cross-linked, serves as a crucial target for antibacterial medications due to its ability to provide high mechanical strength and prevent osmotic lysis [175]. Inhibiting enzymes involved in fatty acid biosynthesis is a promising strategy for antimicrobial agents to impede bacterial growth. In this regard, various steps of fatty acid biosynthesis have been shown to be inhibited by flavonoids. For instance, quercetin, apigenin, and sakuranetin have been found to inhibit 3-hydroxyacyl-ACP dehydrase from H. pylori [176]. Additionally, different subclasses of flavonoids have been shown to inhibit 3-ketoacyl-ACP synthase and malonyl CoA-acyl carrier protein [177,178]. Quercetin and apigenin have also demonstrated inhibitory effects on peptidoglycan synthesis, an essential constituent of the bacterial cell wall [179]. Acidic terpenoids such as enfumafungin, ascosteroside, arundifungin, and ergokonin A, which exhibit antifungal activity against Aspergillus and Candida, are proposed to inhibit β(1,3)-D-glucan synthase, an enzyme involved in glucan synthesis, the primary polysaccharide in the fungal cell wall (reviewed in [180]). Studies have shown that these compounds selectively target β(1,3)-D-glucan synthases in a non-competitive manner [181]. Remarkably, glabridin, a flavonoid, exerts its antifungal mechanism through cell wall deformation [110].
4.3. Inhibition of Biofilm Formation
Biofilms represent well-organized communities of microbes entrenched within a self-produced extracellular matrix [182]. Within these biofilms, bacteria can endure harsh conditions and secrete various polymers such as polysaccharides, extracellular DNA (e-DNA), and amyloidogenic proteins [183]. Bacterial biofilm infections, whether stemming from pre-existing conditions, hospital-acquired infections, or the use of different medical devices, pose significant threats to public health [184]. In this respect, numerous studies have showcased the ability of flavonoids to inhibit bacterial biofilm formation [184]. For example, phloretin, a flavonoid belonging to the dihydrochalcone class, hindered the formation of fimbriae—elongated filamentous polymeric protein structures located on the surface of bacterial cells in E. coli—by reducing the expression of curli genes (csgA, csgB), ultimately impeding biofilm formation [182]. Flavonoids have also been observed to induce pseudo-multicellular aggregation of S. aureus, thereby inhibiting biofilm formation [185,186]. The alkaloid anguinarine significantly suppressed biofilm formation by P. rettgeri through the blockade of expression and formation of biofilm substances [187]. Similarly, the alkaloid berberine exhibited inhibition of biofilm formation in drug-resistant E. coli strains [188].
Flavonoids such as quercetin and apigenin were found to inhibit biofilm formation by C. albicans, while ellagic and caffeic acid from propolis were effective against the biofilms of C. auris (reviewed in [151]). Prenylflavanone 8PP demonstrated inhibition of C. albicans biofilms by increasing the production of ROS and reactive nitrogen intermediates [189].
4.4. Inhibition of Nucleic Acid and Protein Synthesis
The crucial bacterial enzyme responsible for catalyzing the ATP-dependent negative supercoiling of double-stranded closed-circular DNA is DNA gyrase [190]. In a study assessing the antibacterial activity of flavonoids against E. coli, the inhibitory effects of these compounds on DNA gyrase were evaluated through DNA supercoiling assays. Among the compounds investigated, kaempferol exhibited the most potent inhibitory activity [191]. A docking study aimed at identifying potential DNA gyrase B inhibitors from C. difficile suggested that several flavonoids have significantly higher binding affinity compared to the known inhibitor novobiocin [192]. Additionally, flavonoids such as luteolin and myricetin were found to inhibit DNA gyrase, a crucial replicative enzyme responsible for separating and/or rearranging DNA double strands in E. coli [193]. Various flavonoids have been proposed as potent inhibitors of several DNA and RNA polymerases, as well as viral reverse transcriptase [194]. The already mentioned alkaloid berberine demonstrated inhibition of DNA replication, RNA transcription, and protein biosynthesis in bacteria [145]. It was also observed to inhibit the assembly of FtsZ protein, crucial for bacterial cell cycle and division [146], and to inhibit the synthesis of proteins related to cell growth [145]. Catechin inhibited nucleic acid synthesis in C. albicans, reducing the expression of hypha-specific genes in the mitogen-activated protein kinase cascade and the cyclic adenosine 3,5-monophosphate pathway [195]. Similarly, several flavonoids inhibited the growth of C. lunatus by inhibiting nucleic acid synthesis [196]. Gallic acid extracted from Paeonia rockii (S. G. Haw & Lauener) T. Hong & J. J. Li ex D.Y. Hong inhibited protein synthesis in C. albicans, leading to a reduction in the number of hyphal cells and germ tubes [197].
4.5. Inhibition of Metabolism
Numerous studies have demonstrated the inhibition of various pathways of bacterial metabolism by bioactive plant compounds. For instance, the inhibitory effect of 17 bioflavonoid compounds on purified F1 or membrane-bound F1Fo of E. coli was evidenced [198]. Catechin and epigallocatechin gallate were shown to inhibit the enzymatic activity of F1Fo-ATPase and lactate dehydrogenase in S. mutans [199]. Flavonoids were found to hinder the growth of P. aeruginosa and S. aureus by affecting the enzymatic activity of ATPase [169]. The alkaloid berberine impacted the carbohydrate metabolism of S. pyogenes by upregulating ATP-binding cassette transporter and phosphotransferase systems involved in carbohydrate uptake and increasing carbohydrate conversion [149]. Additionally, various terpenes isolated from vegetal sources were tested on eleven fungi species, revealing their antifungal effect through the inhibition of respiration, succinate dehydrogenase, and NADH oxidase activities [200].
4.6. Stimulation of ROS Generation
The induction of high levels of reactive oxygen species through various methods has been extensively explored for the treatment of infections [201]. Numerous plant compounds have been demonstrated to augment ROS production. The inhibitory mechanism of catechin on the growth of both Gram-positive and Gram-negative bacteria has been linked to the induction of ROS production via membrane permeabilization, a phenomenon confirmed through the formation and treatment of bacterial liposomes [202]. For example, berberine has been shown to stimulate excessive ROS production in S. pyogenes [149]. The flavonoid bacalein has been found to induce ROS accumulation and subsequent cell apoptosis in Candida species [115]. Flavonoids found in honey [113] and quercetin have been observed to inhibit the growth of C. albicans by increasing intracellular ROS levels [203].
4.7. Inhibition of Efflux Pumps
Efflux pumps, found in most living cells, are transport proteins responsible for moving substrates from the cell to the external environment. They play a crucial role in detoxifying bacterial or fungal cells by removing accumulated drugs, and their high expression is often associated with drug resistance [204]. Consequently, inhibiting efflux pumps is essential for combating drug resistance. One of the earliest discovered efflux inhibitors of plant origin is the alkaloid reserpine, which has been demonstrated to effectively inhibit the Bmr (Bacillus multidrug resistance) efflux pump of B. subtilis [66]. Plant alkaloids such as ellagic and tannic acids have also shown inhibitory effects on efflux activities in A. baumannii [30]. Flavonoids from various subclasses have exhibited activity as bacterial efflux pump inhibitors (as reviewed in [205]). Numerous studies have demonstrated the inhibition of bacterial efflux pumps by terpenes [206], with S. aureus being the most commonly studied bacterium and carvacrol being the most investigated terpene. Importantly, efflux pumps of Gram-positive bacteria have been found to be more susceptible to the action of terpenes, which may involve either inhibition of gene expression or interaction with the binding site of membrane-associated efflux proteins [206]. The polyphenol curcumin has been shown to modulate efflux pump activity in S. cerevisiae [207]. Additionally, various flavonoids (such as apigenin, chrysin, baicalein, luteolin, tangeritin, scutellarein, 6-hydroxyflavone, and sedonan A) have been found to inhibit efflux-mediated pumps, leading to cell death in fungi (reviewed in [110]). In summary, a myriad of mechanisms of action for antibacterial and antifungal compounds derived from plants, including those found in Caucasus plants, have been uncovered, offering promising avenues for combating antimicrobial resistance. These mechanisms are multifaceted, involving various targets within bacterial and fungal cells, and encompass membrane destruction, inhibition of cell wall biosynthesis, inhibition of biofilm formation, inhibition of nucleic acid and protein synthesis, inhibition of metabolism, stimulation of ROS generation, and inhibition of efflux pumps. Plant-derived secondary metabolites, such as phenolic compounds, terpenes, saponins, alkaloids, and sulfur-containing compounds, have long been utilized in folk medicine for treating various ailments. Their diverse mechanisms of action or target sites, distinct from those of antibiotics, offer potential for combating bacterial resistance either alone or in combination with antibiotics. However, gaps persist in fully elucidating the mechanisms of action of antibacterial and antifungal secondary metabolites. Understanding these diverse mechanisms is crucial for developing effective strategies to combat antimicrobial resistance. Further research into the therapeutic potential of plant-derived antimicrobial compounds holds promise for addressing the growing threat of antimicrobial resistance and improving global public health outcomes.
5. Conclusions and Future Perspectives
In conclusion, this study underscores the significant antimicrobial potential of Caucasian medicinal plants, many of which are endemic species, such as Eryngium caucasicum and Thymus caucasicum. These plants have long been valued for their therapeutic properties, offering promising avenues for drug discovery against a wide range of pathogens. The diverse array of bioactive compounds present in these endemic species underscores their value as sources of novel therapeutic agents in the fight against infectious diseases, particularly in the face of rising antimicrobial resistance. Moreover, this study underscores the critical role of traditional knowledge in guiding modern drug discovery efforts. Indigenous communities have long recognized the medicinal properties of endemic plants and their sustainable use, providing valuable insights that can inform scientific research and conservation initiatives. However, it is crucial to address the challenges associated with standardizing methodologies for assessing antimicrobial activity, particularly when comparing results across different studies. Standardization efforts can facilitate more accurate comparisons and reliable data interpretation in future research. Looking ahead, the identified antimicrobial compounds from Caucasian medicinal plants, including endemic species, hold great promise for further investigation and development into novel therapeutic agents. Given the urgent global need for effective treatments against multidrug-resistant pathogens, these natural sources represent valuable reservoirs for drug discovery efforts. Continued research efforts should focus on elucidating the mechanisms of action of these bioactive compounds, optimizing extraction techniques, and conducting preclinical and clinical trials. Moreover, it is essential to prioritize conservation efforts aimed at protecting endemic species and their habitats, ensuring their availability for future generations and supporting ongoing research endeavors in natural-product-based drug discovery. By combining scientific innovation with the preservation of biodiversity and traditional knowledge associated with endemic plants, we can unlock the full therapeutic potential of Caucasian medicinal flora and contribute to addressing the global challenge of antimicrobial resistance.
Author Contributions
M.F.-J., V.M., C.M., M.V., C.V. and G.N.R. have contributed equally to the preparation of this work. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
| DW | dry weight |
| FW | fresh weight |
| Bacterial species | |
| A. alternata | Alternaria alternata |
| A. baumannii | Acinetobacter baumannii |
| A. flavus | Aspergillus flavus |
| A. niger | Aspergillus niger |
| A. terreus | Aspergillus terreus |
| A. viscosus | Actinomyces viscosus |
| A. versicolor | Aspergillus versicolor |
| B. anthracis | Bacillus anthracis |
| B. cereus | Bacillus cereus |
| B. subtilis | Bacillus subtilis |
| B.thermosphacta | Brochothrix thermosphacta |
| C. albicans | Candida albicans |
| C. auris | Candida auris |
| C. difficile | Clostridium difficile |
| C. dubliniensis | Candida dubliniensis |
| C. glabrata | Candida glabrata |
| C. guilliermondii | Candida guilliermondii |
| C. krusei | Candida krusei |
| C. lunatus | Cochliobolus lunatus |
| C. neoformans | Cryptococcus neoformans |
| C. parapsilosis | Candida parapsilosis |
| C. perfringens | Clostridium perfringens |
| C. rugosa | Candida rugosa |
| C. tropicalis | Candida tropicalis |
| D.stemonitis | Doratomycesstemonitis |
| E. aerogenes | Enterobacter aerogenes |
| E. coli | Escherichia coli |
| E. faecalis | Enterococcus faecalis |
| E. faecium | Enterococcus faecium |
| F. fujikuroi | Fusarium fujikuroi |
| F. nucleatum | Fusobacterium nucleatum |
| F. oxysporum | Fusarium oxysporum |
| F. solani | Fusarium solani |
| H. pylori | Helicobacter pylori |
| K. oxytoca | Klebsiella oxytoca |
| K. pneumoniae | Klebsiella pneumoniae |
| L. monocytogenes | Listeria monocytogenes |
| M. canis | Microsporum canis |
| M. gypseum | Microsporum gypseum |
| M. haemolytica | Mannheimia haemolytica |
| P. aeruginosa | Pseudomonas aeruginosa |
| P.canescens | Penicilliumcanescens |
| P. chrysogenum | Penicillium chrysogenum |
| P. citrinum | Penicillium citrinum |
| P.cyclopium | Penicilliumcyclopium |
| P. digitatum | Penicillium digitatum |
| P. expansum | Penicillium expansum |
| P. fastigiate | Phialophora fastigiate |
| P. fluorescens | Pseudomonas fluorescens |
| P. gingivalis | Porphyromonas gingivalis |
| P. guilliermondii | Pichia guilliermondii |
| P. italicum | Penicillium italicum |
| P. intermedia | Prevotella intermedia |
| P. mirabilis | Proteus mirabilis |
| P. multocida | Pasteurella multocida |
| P. rettgeri | Providencia rettgeri |
| P. ultimum | Pythium ultimum |
| P. vulgaris | Proteus vulgaris |
| R. solanacearum | Ralstonia solanacearum |
| R. oryzae | Rhizopus oryzae |
| S. abony | Salmonella abony |
| S. aureus | Staphylococcus aureus |
| S. cerevisiae | Saccharomyces cerevisiae |
| S. dysenteriae | Shigella dysenteriae |
| S. enterica | Salmonella enterica |
| S. enteritidis | Salmonella enteritidis |
| S. epidermidis | Staphylococcus epidermidis |
| S. flexneri | Shigella flexneri |
| S. mitis | Streptococcus mitis |
| S. mutans | Streptococcus mutans |
| S. paratyphi | Salmonella paratyphi |
| S. pneumoniae | Streptococcus pneumoniae |
| S. pyogenes | Streptococcus pyogenes |
| S. salivarius | Streptococcus salivarius |
| S. sanguinis | Streptococcus sanguinis |
| S. saprophyticus | Staphylococcus saprophyticus |
| S. typhi | Salmonella typhi |
| S. typhimurium | Salmonella typhimurium |
| T.harzianum | Trichodermaharzianum |
| T.longibrachiatum | Trichodermalongibrachiatum |
| V. cholera | Vibrio cholera |
| Plant species | |
| Agrimonia eupatoria L. | A. eupatoria |
| Acer cappadocicum Gled. | A. cappadocicum |
| Aconitum carmichaeli var. carmichaeli | A. carmichaeli |
| Alcea rosea L. | A. rosea |
| Allium atroviolaceum Hornem. Ex Steud. | A. atroviolaceum |
| Allium sativum L. | A. sativum |
| Allium ursinum L. | A. ursinum |
| Artemisia fragrans Willd. | A. fragrans |
| Carum copticum (L.) Benth. & Hook.f. ex Hiern | C. copticum |
| Clinopodium nepeta (L.) Kuntze | C. nepeta |
| Cyclamen coum Mill. | C. coum |
| Eryngium caucasicum Trautv. | E. caucasicum |
| Filipendula ulmaria (L.) Maxim. | F. ulmaria |
| Galanthus transcaucasicus Fomin | G. transcaucasicus |
| Hypericum alpestre Steven. | H. alpestre |
| Juglans regia L. | J. regia |
| Laurus nobilis L. | L. nobilis |
| Lilium monadelphum subsp. armenum (Miscz. ex Grossh.) Kudrjasch. | L. armenum |
| Mentha pulegium L. | M. pulegium |
| Peganum harmala L. | P. harmala |
| Primula macrocalyx Bunge | P. macrocalyx |
| Pterocarya fraxinifolia (Poir.) Spach | P. fraxinifolia |
| Rosa canina L. | R. canina |
| Rumex obtusifolius L. | R. obtusifolius |
| Sanguisorba officinalis L. | S. officinalis |
| Thymus caucasicus Willd. ex Benth. | T. caucasicus |
References
- Vaou, N.; Stavropoulou, E.; Voidarou, C.; Tsigalou, C.; Bezirtzoglou, E. Towards advances in medicinal plant antimicrobial activity: A review study on challenges and future perspectives. Microorganisms 2021, 9, 2041. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Antimicrobial resistance collaborators. Global mortality associated with 33 bacterial pathogens in 2019: A systematic analysis for the global burden of disease study 2019. Lancet Lond. Engl. 2022, 400, 2221–2248. [Google Scholar] [CrossRef] [PubMed]
- Costanzo, V.; Roviello, G.N. The potential role of vaccines in preventing antimicrobial resistance (amr): An update and future perspectives. Vaccines 2023, 11, 333. [Google Scholar] [CrossRef] [PubMed]
- Frieri, M.; Kumar, K.; Boutin, A. Antibiotic resistance. J. Infect. Public Health 2017, 10, 369–378. [Google Scholar] [CrossRef] [PubMed]
- Baym, M.; Stone, L.K.; Kishony, R. Multidrug evolutionary strategies to reverse antibiotic resistance. Science 2016, 351, aad3292. [Google Scholar] [CrossRef]
- Autiero, I.; Roviello, G.N. Interaction of Laurusides 1 and 2 with the 3C-like protease (Mpro) from wild-type and omicron variant of SARS-CoV-2: A Molecular Dynamics Study. Int. J. Mol. Sci. 2023, 24, 5511. [Google Scholar] [CrossRef] [PubMed]
- Vicidomini, C.; Roviello, V.; Roviello, G.N. Molecular basis of the therapeutical potential of clove (Syzygium aromaticum L.) and clues to its anti-COVID-19 utility. Molecules 2021, 26, 1880. [Google Scholar] [CrossRef] [PubMed]
- Vicidomini, C.; Roviello, V.; Roviello, G.N. In Silico Investigation on the interaction of chiral phytochemicals from opuntia ficus-indica with SARS-CoV-2 Mpro. Symmetry 2021, 13, 1041. [Google Scholar] [CrossRef]
- Baker, S.; Gilhen-Baker, M.; Roviello, G.N. The Role of nutrition and forest-bathing in the physical rehabilitation of physically inactive patients: From the molecular aspects to new nature-inspired techniques. Int. J. Environ. Res. Public. Health 2022, 20, 793. [Google Scholar] [CrossRef]
- Ricci, A.; Roviello, G.N. Exploring the Protective effect of food drugs against viral diseases: Interaction of functional food ingredients and SARS-CoV-2, influenza virus, and HSV. Life 2023, 13, 402. [Google Scholar] [CrossRef]
- Álvarez-Martínez, F.J.; Barrajón-Catalán, E.; Herranz-López, M.; Micol, V. Antibacterial plant compounds, extracts and essential oils: An updated review on their effects and putative mechanisms of action. Phytomedicine 2021, 90, 153626. [Google Scholar] [CrossRef]
- Keita, K.; Darkoh, C.; Okafor, F. Secondary plant metabolites as potent drug candidates against antimicrobial-resistant pathogens. SN Appl. Sci. 2022, 4, 209. [Google Scholar] [CrossRef] [PubMed]
- Shankar, S.R.; Rangarajan, R.; Sarada, D.V.L.; Kumar, C.S. Evaluation of antibacterial activity and phytochemical screening of Wrightia tinctoria L. Pharmacogn. J. 2010, 2, 19–22. [Google Scholar] [CrossRef]
- Manukyan, A.; Lumlerdkij, N.; Heinrich, M. Caucasian endemic medicinal and nutraceutical plants: In-vitro antioxidant and cytotoxic activities and bioactive compounds. J. Pharm. Pharmacol. 2019, 71, 1152–1161. [Google Scholar] [CrossRef] [PubMed]
- Miller, N.F. Plants and humans in the near east and the Caucasus: Ancient and traditional uses of plants as food and medicine, a diachronic ethnobotanical review. Ethnobiol. Lett. 2014, 5, 22–23. [Google Scholar] [CrossRef]
- Price, M.F. Cooperation in the European Mountains. 2: The Caucasus; Environmental research series; IUCN: Gland, Switzerland, 2000; ISBN 978-2-8317-0534-7. [Google Scholar]
- Takhtadzhian, A.L.; Crovello, T.J.; Cronquist, A. Floristic Regions of the World; University of California Press: Berkeley, CA, USA, 1986; ISBN 978-0-520-04027-4. [Google Scholar]
- Grossheim, A.A. Analysis of the Flora of the Caucasus: Proceedings of the Botanical Institute of Azerbaijan; FAN USSR: Baku, Azerbaijan, 1936. [Google Scholar]
- Takhtajan, A.L. Konspekt Florii Kavkaz; Sankt Peterburg University Press: Sankt Peterburg, Russia, 2003; Volume 1, 204p. [Google Scholar]
- Tarkhnishvili, D. Historical Biogeography of the Caucasus; Nova Publ.: New York, NY, USA, 2014; 234p, ISBN 978-1-63321-910-6. [Google Scholar]
- Plant Diversity in the Central Great Caucasus: A Quantitative Assessment; Nakhutsrishvili, G.S., Abdaladze, O., Batsatsashvili, K., Spehn, E.M., Körner, C., Eds.; Springer International Publishing: Cham, Switzerland, 2017; 170p, ISBN 978-3-319-55777-9. [Google Scholar]
- Mamedov, N.; Mehdiyeva, N.P.; Craker Lyle, E. Medicinal plants used in traditional medicine of the Caucasus and North America. J. Med. Act. Plants 2015, 4, 42–66. [Google Scholar] [CrossRef]
- Eynanlou Yaghmerlou, S.; Malekzadeh, H.; Ghaznavi, D.; Zeighami, H.; Tavakolizadeh, M. Anti-bacterial effects of Allium atroviolaceum hydroalcoholic extract on oral bacteria of Streptococcus viridans groups. Jundishapur J. Nat. Pharm. Prod. 2024, 19. [Google Scholar] [CrossRef]
- Chehregani, A.; Azimishad, F.; Alizade, H.H. Study on antibacterial effect of some Allium species from Hamedan-Iran. IJAB 2007, 9, 873–876. [Google Scholar]
- Barbu, I.A.; Ciorîță, A.; Carpa, R.; Moț, A.C.; Butiuc-Keul, A.; Pârvu, M. Phytochemical characterization and antimicrobial activity of several Allium extracts. Molecules 2023, 28, 3980. [Google Scholar] [CrossRef]
- Chowdhury, A.K.; Ahsan, M.; Islam, S.N.; Ahmed, Z.U. Efficacy of aqueous extract of garlic & allicin in experimental shigellosis in rabbits. Indian J. Med. Res. 1991, 93, 33–36. [Google Scholar]
- Saha, S.K.; Saha, S.; Hossain, M.A.; Paul, S.K. In vitro assessment of antibacterial eEffect of garlic (Allium Sativum) extracts on Pseudomonas aeruginosa. Mymensingh Med. J. MMJ 2015, 24, 222–232. [Google Scholar] [PubMed]
- Karimi, E.; Mehrabanjoubani, P.; Homayouni-Tabrizi, M.; Abdolzadeh, A.; Soltani, M. Phytochemical evaluation, antioxidant properties and antibacterial activity of Iranian medicinal herb Galanthus transcaucasicus Fomin. J. Food Meas. Charact. 2018, 12, 433–440. [Google Scholar] [CrossRef]
- Sharifzadeh, M.; Yousefbeyk, F.; Amin, G.; Salehi Sormaghi, M.; Azadi, B.; Samadi, N.; Amini Moghadam Farouj, N.; Amin, M. Investigation on pharmacological and antimicrobial activities of Galanthus transcaucasicus Fomin growing in Iran. Planta Med. 2010, 76, P474. [Google Scholar] [CrossRef]
- Hamedi, A.; Pasdaran, A.; Pasdaran, A. Antimicrobial activity and analysis of the essential oils of selected endemic edible Apiaceae plants root from Caspian Hyrcanian region (North of Iran). Pharm. Sci. 2019, 25, 138–144. [Google Scholar] [CrossRef]
- Mohamadipour, S.; Hatamzadeh, A.; Bakhshi, D.; Pasdaran, A. Antimicrobial activities of Caucalis platycarpos L. and Eryngium caucasicum Trautv. essential oils. Aust. J. Crop Sci. 2018, 12, 1357–1362. [Google Scholar] [CrossRef]
- Younessi-Hamzekhanlu, M.; Sanjari, S.; Dejahang, A.; Karkaj, E.S.; Nojadeh, M.S.; Gönenç, T.M.; Ozturk, M. Evaluation of essential oil from different Artemisia fragrans Willd. populations: Chemical composition, antioxidant, and antibacterial activity. J. Essent. Oil Bear. Plants 2020, 23, 1218–1236. [Google Scholar] [CrossRef]
- Aminkhani, A.; Sharifi, S.; Hosseinzadeh, P. Chemical constituent, antimicrobial activity, and synergistic effect of the stem, leaf, and flower essential oil of the Artemisia fragrans Willd. from Khoy. Chem. Biodivers. 2021, 18, e2100241. [Google Scholar] [CrossRef] [PubMed]
- Shafaghat, A.; Noormohammadi, Y.; Zaifizadeh, M. Composition and antibacterial activity of essential oils of Artemisia fragrans Willd. leaves and roots from Iran. Nat. Prod. Commun. 2009, 4, 279–282. [Google Scholar] [CrossRef] [PubMed]
- Ginovyan, M.; Trchounian, A. Novel approach to combat antibiotic resistance: Evaluation of some Armenian herb crude extracts for their antibiotic modulatory and antiviral properties. J. Appl. Microbiol. 2019, 127, 472–480. [Google Scholar] [CrossRef]
- Ginovyan, M.; Petrosyan, M.; Trchounian, A. Antimicrobial activity of some plant materials used in Armenian traditional medicine. BMC Complement. Altern. Med. 2017, 17, 50. [Google Scholar] [CrossRef]
- Fathi, H.; Ebrahimzadeh, M.; Ahanjan, M. Comparison of the antimicrobial activity of Caucasian wingnut leaf extract (Pterocarya fraxinifolia) and walnut (Juglans regia L.) plants. Acta Biol. Indica 2015, 4, 67–74. [Google Scholar]
- Chaleshtori, R.S.; Chaleshtori, F.S.; Rafieian, M. Biological characterization of Iranian walnut (Juglans regia) leaves. Turk. J. Biol. 2011, 35, 635–639. [Google Scholar] [CrossRef]
- Noumi, E.; Snoussi, M.; Hajlaoui, H.; Valentin, E.; Bakhrouf, A. Antifungal properties of Salvadora persica and Juglans regia L. extracts against oral Candida strains. Eur. J. Clin. Microbiol. Infect. Dis. 2010, 29, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Moori Bakhtiari, N.; Khalafi, E. Antibacterial activity of the hydro-alcoholic extract of Juglans regia L. stem bark on human bacterial infection. Int. Arch. Health Sci. 2015, 2, 139–143. [Google Scholar]
- Oliveira, I.; Sousa, A.; Ferreira, I.C.F.R.; Bento, A.; Estevinho, L.; Pereira, J.A. Total phenols, antioxidant potential and antimicrobial activity of walnut (Juglans regia L.) green husks. Food Chem. Toxicol. 2008, 46, 2326–2331. [Google Scholar] [CrossRef] [PubMed]
- Azirian, M.; Hadjiakhoondi, A.; Vatankhah, E.; Hosseinizadeh, S.; Tavakoli, S.; Akhbari, M. Variation in chemical components and biological activity of Pterocarya fraxinifolia Lam. stems at different developmental stages. Res. J. Pharmacogn. 2017, 4, 41–50. [Google Scholar]
- Debbabi, H.; El Mokni, R.; Chaieb, I.; Nardoni, S.; Maggi, F.; Caprioli, G.; Hammami, S. Chemical composition, antifungal and insecticidal activities of the essential oils from Tunisian Clinopodium nepeta subsp. nepeta and Clinopodium nepeta subsp. glandulosum. Molecules 2020, 25, 2137. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, G.; Yilmaz, G.; Ekşi, G.; DemiRci, B. Chemical composition and antibacterial activity of Clinopodium nepeta subsp. glandulosum (Req.) Govaerts essential oil. Nat. Volatiles Essent. Oils 2021, 8, 75–80. [Google Scholar] [CrossRef]
- Atakishiyeva, Y.; Ghasemi, M. Investigation of the antibacterial effect of native Peganum harmala, Mentha pulegium and Alcea rosea hydro-alcoholic extracts on antibiotic resistant Streptococcus pneumoniae and Klebsiella pneumonia isolated from Baku, Azerbaijan. IEM 2016, 2, 12–14. [Google Scholar]
- Mahboubi, M.; Haghi, G. Antimicrobial activity and chemical composition of Mentha pulegium L. essential oil. J. Ethnopharmacol. 2008, 119, 325–327. [Google Scholar] [CrossRef]
- Luís, Â.; Domingues, F. Screening of the potential bioactivities of pennyroyal (Mentha pulegium L.) essential oil. Antibiotics 2021, 10, 1266. [Google Scholar] [CrossRef] [PubMed]
- Asbaghian, S.; Shafaghat, A.; Zarea, K.; Kasimov, F.; Salimi, F. Comparison of volatile constituents, and antioxidant and antibacterial activities of the essential oils of Thymus caucasicus, T. kotschyanus and T. vulgaris. Nat. Prod. Commun. 2011, 6, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Stefanova, G.; Girova, T.; Gochev, V.; Stoyanova, M.; Petkova, Z.; Stoyanova, A.; Zheljazkov, V.D. Comparative study on the chemical composition of laurel (Laurus nobilis L.) leaves from Greece and Georgia and the antibacterial activity of their essential oil. Heliyon 2020, 6, e05491. [Google Scholar] [CrossRef] [PubMed]
- Caputo, L.; Nazzaro, F.; Souza, L.; Aliberti, L.; De Martino, L.; Fratianni, F.; Coppola, R.; De Feo, V. Laurus nobilis: Composition of essential oil and its biological activities. Molecules 2017, 22, 930. [Google Scholar] [CrossRef] [PubMed]
- Sakran, K.A.; Raharjo, D.; Mertaniasih, N.M. Antimicrobial activities of Laurus nobilis leaves ethanol extract on Staphylococcus aureus, Salmonellae typhi, and Escherichia coli. Indones. J. Trop. Infect. Dis. 2021, 9, 119. [Google Scholar] [CrossRef]
- Rizwana, H.; Kubaisi, N.A.; Al-Meghailaith, N.N.; Moubayed, N.M.; Albasher, G. Evaluation of chemical composition, antibacterial, antifungal, and cytotoxic activity of Laurus nobilis L. grown in Saudi Arabia. J. Pure Appl. Microbiol. 2019, 13, 2073–2085. [Google Scholar] [CrossRef]
- Nazir, S.; Ahmad, M.K.; Ali, F.; Ganie, S.A.; Nazir, Z.U. Phytochemical analysis and antibacterial potential of Onosma hispidium and Alcea rosea. Biomedicine 2022, 42, 47–52. [Google Scholar] [CrossRef]
- Özcan, F.; Semerci, A.B.; Tunç, K. A study on antimicrobial and antioxidant activities of Cyclamen coum, Colchicum turcicum and Colchicum bornmuelleri species. Curr. Pers. MAPs 2020, 3, 121–127. [Google Scholar]
- Amin Jaradat, N.; Al-Masri, M.; Hussen, F.; Zaid, A.N.; Ali, I.; Tammam, A.; Mostafa Odeh, D.; Hussein Shakarneh, O.; Rajabi, A. Preliminary Phytochemical and biological screening of Cyclamen coum a member of Palestinian flora. Pharm. Sci. 2017, 23, 231–237. [Google Scholar] [CrossRef]
- Li, X.; Wang, X.; Li, C.; Khutsishvili, M.; Fayvush, G.; Atha, D.; Zhang, Y.; Borris, R.P. Unusual flavones from Primula macrocalyx as inhibitors of OAT1 and OAT3 and as antifungal agents against Candida rugosa. Sci. Rep. 2019, 9, 9230. [Google Scholar] [CrossRef]
- Copland, A.; Nahar, L.; Tomlinson, C.T.M.; Hamilton, V.; Middleton, M.; Kumarasamy, Y.; Sarker, S.D. Antibacterial and free radical scavenging activity of the seeds of Agrimonia eupatoria. Fitoterapia 2003, 74, 133–135. [Google Scholar] [CrossRef] [PubMed]
- Muruzović, M.Ž.; Mladenović, K.G.; Stefanović, O.D.; Vasić, S.M.; Čomić, L.R. Extracts of Agrimonia eupatoria L. as sources of biologically active compounds and evaluation of their antioxidant, antimicrobial, and antibiofilm activities. J. Food Drug Anal. 2016, 24, 539–547. [Google Scholar] [CrossRef] [PubMed]
- Watkins, F.; Pendry, B.; Sanchez-Medina, A.; Corcoran, O. Antimicrobial assays of three native British plants used in Anglo-Saxon medicine for wound healing formulations in 10th century England. J. Ethnopharmacol. 2012, 144, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Savina, T.; Lisun, V.; Feduraev, P.; Skrypnik, L. Variation in phenolic compounds, antioxidant and antibacterial activities of extracts from different plant organs of meadowsweet (Filipendula ulmaria (L.) Maxim.). Molecules 2023, 28, 3512. [Google Scholar] [CrossRef] [PubMed]
- Katanić, J.; Boroja, T.; Stanković, N.; Mihailović, V.; Mladenović, M.; Kreft, S.; Vrvić, M.M. Bioactivity, stability and phenolic characterization of Filipendula ulmaria (L.) Maxim. Food Funct. 2015, 6, 1164–1175. [Google Scholar] [CrossRef] [PubMed]
- Rovná, K.; Ivanišová, E.; Žiarovská, J.; Ferus, P.; Terentjeva, M.; Kowalczewski, P.Ł.; Kačániová, M. Characterization of Rosa canina fruits collected in urban areas of Slovakia. Genome size, iPBS profiles and antioxidant and antimicrobial activities. Molecules 2020, 25, 1888. [Google Scholar] [CrossRef] [PubMed]
- Miljković, V.M.; Nikolić, L.; Mrmošanin, J.; Gajić, I.; Mihajilov-Krstev, T.; Zvezdanović, J.; Miljković, M. Chemical profile and antioxidant and antimicrobial activity of Rosa canina L. dried fruit commercially available in Serbia. Int. J. Mol. Sci. 2024, 25, 2518. [Google Scholar] [CrossRef] [PubMed]
- Tocai (Moţoc), A.-C.; Ranga, F.; Teodorescu, A.G.; Pallag, A.; Vlad, A.M.; Bandici, L.; Vicas, S.I. Evaluation of polyphenolic composition and antimicrobial properties of Sanguisorba officinalis L. and Sanguisorba minor Scop. Plants 2022, 11, 3561. [Google Scholar] [CrossRef] [PubMed]
- Kausar, F.; Farooqi, M.-A.; Farooqi, H.-M.-U.; Salih, A.-R.-C.; Khalil, A.-A.-K.; Kang, C.-W.; Mahmoud, M.H.; Batiha, G.-E.-S.; Choi, K.-H.; Mumtaz, A.-S. Phytochemical investigation, antimicrobial, antioxidant and anticancer activities of Acer cappadocicum Gled. Life Basel Switz. 2021, 11, 656. [Google Scholar] [CrossRef] [PubMed]
- Iranshahi, M.; Fazli Bazaz, S.; Haririzadeh, G.; Abootorabi, B.Z.; Mohamadi, A.M.; Khashyarmanesh, Z. Chemical composition and antibacterial properties of Peganum harmala L. Avicenna J. Phytomedicine 2019, 9, 530. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA group preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- The Angiosperm Phylogeny Group. An update of the angiosperm phylogeny group classification for the orders and families of flowering plants: APG III: APG III. Bot. J. Linn. Soc. 2009, 161, 105–121. [Google Scholar] [CrossRef]
- Oteng Mintah, S.; Asafo-Agyei, T.; Archer, M.-A.; Atta-Adjei Junior, P.; Boamah, D.; Kumadoh, D.; Appiah, A.; Ocloo, A.; Duah Boakye, Y.; Agyare, C. Medicinal plants for treatment of prevalent diseases. In Pharmacognosy—Medicinal Plants; Perveen, S., Al-Taweel, A., Eds.; IntechOpen: London, UK, 2019; ISBN 978-1-83880-610-1. [Google Scholar]
- Balouiri, M.; Sadiki, M.; Ibnsouda, S.K. Methods for in vitro evaluating antimicrobial activity: A review. J. Pharm. Anal. 2016, 6, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Methods for the determination of susceptibility of bacteria to antimicrobial agents. Terminology. Clin. Microbiol. Infect. 1998, 4, 291–296. [CrossRef]
- Bhargav, H.S.; Shastri, S.D.; Poornav, S.P.; Darshan, K.M.; Nayak, M.M. Measurement of the zone of inhibition of an antibiotic. In Proceedings of the 2016 6th International Conference on Advanced Computing (IACC), Bhimavaram, India, 27–28 February 2016; pp. 409–414. [Google Scholar]
- Pirtskhalava, M.; Mittova, V.; Tsetskhladze, Z.R.; Palumbo, R.; Pastore, R.; Roviello, G.N. Georgian medicinal plants as rich natural sources of antioxidant derivatives: A review on the current knowledge and future perspectives. Curr. Med. Chem. 2024, 31. [Google Scholar] [CrossRef] [PubMed]
- Mulani, M.S.; Kamble, E.E.; Kumkar, S.N.; Tawre, M.S.; Pardesi, K.R. Emerging strategies to combat ESKAPE Pathogens in the era of antimicrobial resistance: A review. Front. Microbiol. 2019, 10, 539. [Google Scholar] [CrossRef] [PubMed]
- Kumar Mishra, K.; Deep Kaur, C.; Kumar Sahu, A.; Panik, R.; Kashyap, P.; Prasad Mishra, S.; Dutta, S. Medicinal plants having antifungal properties. In Medicinal Plants—Use in Prevention and Treatment of Diseases; Abdul Rasool Hassan, B., Ed.; IntechOpen: London, UK, 2020; ISBN 978-1-78985-887-7. [Google Scholar]
- Khalil, N.A.; ALFaris, N.A.; ALTamimi, J.Z.; Mohamed Ahmed, I.A. Anti-inflammatory effects of bay laurel (Laurus nobilis L.) towards the Gut microbiome in dextran sodium sulfate induced colitis animal models. Food Sci. Nutr. 2024, 12, 2650–2660. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, H.A.; Issa, M.Y. In vitro and in vivo activity of Peganum harmala L. alkaloids against phytopathogenic bacteria. Sci. Hortic. 2020, 264, 108940. [Google Scholar] [CrossRef]
- Izadi, M.; Moosawi Jorf, S.A.; Nikkhah, M.; Moradi, S. Antifungal activity of hydrocolloid nano encapsulated Carum copticum essential oil and Peganum harmala extract on the pathogenic fungi Alternaria alternata. Physiol. Mol. Plant Pathol. 2021, 116, 101714. [Google Scholar] [CrossRef]
- Khezri, K.; Farahpour, M.R.; Mounesi Rad, S. Efficacy of Mentha pulegium essential oil encapsulated into nanostructured lipid carriers as an in vitro antibacterial and infected wound healing agent. Colloids Surf. Physicochem. Eng. Asp. 2020, 589, 124414. [Google Scholar] [CrossRef]
- Rasmussen, T.B.; Bjarnsholt, T.; Skindersoe, M.E.; Hentzer, M.; Kristoffersen, P.; Köte, M.; Nielsen, J.; Eberl, L.; Givskov, M. Screening for quorum-sensing inhibitors (QSI) by use of a novel genetic system, the QSI selector. J. Bacteriol. 2005, 187, 1799–1814. [Google Scholar] [CrossRef] [PubMed]
- Daglia, M. Polyphenols as antimicrobial agents. Curr. Opin. Biotechnol. 2012, 23, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Mamari, H.H. Phenolic compounds: Classification, chemistry, and updated techniques of analysis and synthesis. In Biochemistry; Badria, F.A., Ed.; IntechOpen: London, UK, 2022; Volume 26, ISBN 978-1-83969-346-5. [Google Scholar]
- Manso, T.; Lores, M.; De Miguel, T. Antimicrobial activity of polyphenols and natural polyphenolic extracts on clinical isolates. Antibiotics 2021, 11, 46. [Google Scholar] [CrossRef] [PubMed]
- Lobiuc, A.; Pavăl, N.-E.; Mangalagiu, I.I.; Gheorghiță, R.; Teliban, G.-C.; Amăriucăi-Mantu, D.; Stoleru, V. Future antimicrobials: Natural and functionalized phenolics. Molecules 2023, 28, 1114. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Sun, Q.; Gong, S.; Bi, X.; Jiang, W.; Xue, W.; Fei, P. Antimicrobial activity and action approach of the olive oil polyphenol extract against Listeria monocytogenes. Front. Microbiol. 2019, 10, 1586. [Google Scholar] [CrossRef]
- Piekarska-Radzik, L.; Klewicka, E. Mutual influence of polyphenols and Lactobacillus spp. bacteria in food: A Review. Eur. Food Res. Technol. 2021, 247, 9–24. [Google Scholar] [CrossRef]
- Lin, S.; Wang, Z.; Lam, K.-L.; Zeng, S.; Tan, B.K.; Hu, J. Role of intestinal microecology in the regulation of energy metabolism by dietary polyphenols and their metabolites. Food Nutr. Res. 2019, 63. [Google Scholar] [CrossRef] [PubMed]
- Othman, L.; Sleiman, A.; Abdel-Massih, R.M. Antimicrobial activity of polyphenols and alkaloids in middle eastern plants. Front. Microbiol. 2019, 10, 911. [Google Scholar] [CrossRef]
- Biernasiuk, A.; Wozniak, M.; Bogucka-Kocka, A. Determination of free and bounded phenolic acids in the rhizomes and herb of Sanguisorba officinalis L. Curr. Issues Pharm. Med. Sci. 2015, 28, 254–256. [Google Scholar] [CrossRef]
- Kahkeshani, N.; Farzaei, F.; Fotouhi, M.; Alavi, S.S.; Bahramsoltani, R.; Naseri, R.; Momtaz, S.; Abbasabadi, Z.; Rahimi, R.; Farzaei, M.H.; et al. Pharmacological effects of gallic acid in health and disease: A mechanistic review. Iran. J. Basic Med. Sci. 2019, 22, 225–237. [Google Scholar] [CrossRef]
- Borges, A.; Ferreira, C.; Saavedra, M.J.; Simões, M. Antibacterial activity and mode of action of ferulic and gallic acids against pathogenic bacteria. Microb. Drug Resist. 2013, 19, 256–265. [Google Scholar] [CrossRef]
- Croitoru, A.; Ficai, D.; Craciun, L.; Ficai, A.; Andronescu, E. Evaluation and exploitation of bioactive compounds of walnut, Juglans regia. Curr. Pharm. Des. 2019, 25, 119–131. [Google Scholar] [CrossRef]
- Lou, Z.; Wang, H.; Rao, S.; Sun, J.; Ma, C.; Li, J. P-Coumaric acid kills bacteria through dual damage mechanisms. Food Control 2012, 25, 550–554. [Google Scholar] [CrossRef]
- Teodoro, G.R.; Ellepola, K.; Seneviratne, C.J.; Koga-Ito, C.Y. Potential use of phenolic acids as anti-Candida agents: A review. Front. Microbiol. 2015, 6, 1420. [Google Scholar] [CrossRef]
- Ma, C.-M.; Abe, T.; Komiyama, T.; Wang, W.; Hattori, M.; Daneshtalab, M. Synthesis, anti-fungal and 1,3-β-d-glucan synthase inhibitory activities of caffeic and quinic acid derivatives. Bioorg. Med. Chem. 2010, 18, 7009–7014. [Google Scholar] [CrossRef] [PubMed]
- Oteiza, P.I.; Erlejman, A.G.; Verstraeten, S.V.; Keen, C.L.; Fraga, C.G. Flavonoid-membrane interactions: A protective role of flavonoids at the membrane surface? Clin. Dev. Immunol. 2005, 12, 19–25. [Google Scholar] [CrossRef]
- Kumar, S.; Pandey, A.K. Chemistry and biological activities of flavonoids: An overview. Sci. World J. 2013, 2013, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Mahmud, A.R.; Ema, T.I.; Siddiquee, M.F.-R.; Shahriar, A.; Ahmed, H.; Mosfeq-Ul-Hasan, M.; Rahman, N.; Islam, R.; Uddin, M.R.; Mizan, M.F.R. Natural flavonols: Actions, mechanisms, and potential therapeutic utility for various diseases. Beni-Suef Univ. J. Basic Appl. Sci. 2023, 12, 47. [Google Scholar] [CrossRef]
- Ginovyan, M.; Ayvazyan, A.; Nikoyan, A.; Tumanyan, L.; Trchounian, A. Phytochemical screening and detection of antibacterial components from crude extracts of some Armenian herbs using TLC-bioautographic technique. Curr. Microbiol. 2020, 77, 1223–1232. [Google Scholar] [CrossRef]
- Jiménez, S.; Gascón, S.; Luquin, A.; Laguna, M.; Ancin-Azpilicueta, C.; Rodríguez-Yoldi, M.J. Rosa canina extracts have antiproliferative and antioxidant effects on Caco-2 human colon cancer. PLoS ONE 2016, 11, e0159136. [Google Scholar] [CrossRef]
- Ignasimuthu, K.; Prakash, R.; Murthy, P.S.; Subban, N. Enhanced bioaccessibility of green tea polyphenols and lipophilic activity of EGCG octaacetate on Gram-negative bacteria. LWT 2019, 105, 103–109. [Google Scholar] [CrossRef]
- Renzetti, A.; Betts, J.W.; Fukumoto, K.; Rutherford, R.N. Antibacterial green tea catechins from a molecular perspective: Mechanisms of action and structure–activity relationships. Food Funct. 2020, 11, 9370–9396. [Google Scholar] [CrossRef]
- Liu, S.; Zhang, Q.; Li, H.; Qiu, Z.; Yu, Y. Comparative assessment of the antibacterial efficacies and mechanisms of different tea extracts. Foods 2022, 11, 620. [Google Scholar] [CrossRef] [PubMed]
- Xie, Y.; Yang, W.; Tang, F.; Chen, X.; Ren, L. Antibacterial activities of flavonoids: Structure-activity relationship and mechanism. Curr. Med. Chem. 2014, 22, 132–149. [Google Scholar] [CrossRef]
- Biharee, A.; Sharma, A.; Kumar, A.; Jaitak, V. Antimicrobial flavonoids as a potential substitute for overcoming antimicrobial resistance. Fitoterapia 2020, 146, 104720. [Google Scholar] [CrossRef]
- McGillick, B.E.; Kumaran, D.; Vieni, C.; Swaminathan, S. β-hydroxyacyl-acyl carrier protein dehydratase (FabZ) from Francisella tularensis and Yersinia pestis: Structure determination, enzymatic characterization, and cross-inhibition studies. Biochemistry 2016, 55, 1091–1099. [Google Scholar] [CrossRef] [PubMed]
- Xu, H. Flavones inhibit the hexameric replicative helicase RepA. Nucleic Acids Res. 2001, 29, 5058–5066. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, M.; Novović, K.; Malešević, M.; Dinić, M.; Stojković, D.; Jovčić, B.; Soković, M. Polyphenols as inhibitors of antibiotic resistant bacteria—Mechanisms underlying rutin interference with bacterial virulence. Pharmaceuticals 2022, 15, 385. [Google Scholar] [CrossRef] [PubMed]
- Li, A.-P.; He, Y.-H.; Zhang, S.-Y.; Shi, Y.-P. Antibacterial activity and action mechanism of flavonoids against phytopathogenic bacteria. Pestic. Biochem. Physiol. 2022, 188, 105221. [Google Scholar] [CrossRef]
- Al Aboody, M.S.; Mickymaray, S. Anti-fungal efficacy and mechanisms of flavonoids. Antibiotics 2020, 9, 45. [Google Scholar] [CrossRef]
- Yun, D.G.; Lee, D.G. Silymarin exerts antifungal effects via membrane-targeted mode of action by increasing permeability and inducing oxidative stress. Biochim. Biophys. Acta BBA Biomembr. 2017, 1859, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Da, X.; Nishiyama, Y.; Tie, D.; Hein, K.Z.; Yamamoto, O.; Morita, E. Antifungal activity and mechanism of action of Ou-gon (Scutellaria root extract) components against pathogenic fungi. Sci. Rep. 2019, 9, 1683. [Google Scholar] [CrossRef] [PubMed]
- Canonico, B.; Candiracci, M.; Citterio, B.; Curci, R.; Squarzoni, S.; Mazzoni, A.; Papa, S.; Piatti, E. Honey flavonoids inhibit Candida albicans morphogenesis by affecting DNA behavior and mitochondrial function. Future Microbiol. 2014, 9, 445–456. [Google Scholar] [CrossRef] [PubMed]
- Yiğit, D.; Yiğit, N.; Mavi, A. Antioxidant and antimicrobial activities of bitter and sweet apricot (Prunus armeniaca L.) Kernels. Braz. J. Med. Biol. Res. 2009, 42, 346–352. [Google Scholar] [CrossRef]
- Serpa, R.; França, E.J.G.; Furlaneto-Maia, L.; Andrade, C.G.T.J.; Diniz, A.; Furlaneto, M.C. In vitro antifungal activity of the flavonoid baicalein against Candida species. J. Med. Microbiol. 2012, 61, 1704–1708. [Google Scholar] [CrossRef] [PubMed]
- Steenkamp, J.A.; Steynberg, J.P.; Brandt, E.V.; Ferreira, D.; Roux, D.G. Phlobatannins, a novel class of ring-isomerized condensed tannins. J. Chem. Soc. Chem. Commun. 1985, 23, 1678. [Google Scholar] [CrossRef]
- Hill, G.D. Plant antinutritional factors|Characteristics. In Encyclopedia of Food Sciences and Nutrition; Elsevier: Amsterdam, The Netherlands, 2003; pp. 4578–4587. ISBN 978-0-12-227055-0. [Google Scholar]
- Tong, Z.; He, W.; Fan, X.; Guo, A. Biological function of plant tannin and its application in animal health. Front. Vet. Sci. 2022, 8, 803657. [Google Scholar] [CrossRef]
- Scalbert, A. Antimicrobial properties of tannins. Phytochemistry 1991, 30, 3875–3883. [Google Scholar] [CrossRef]
- Boakye, Y.D. Anti-infective properties and time-kill kinetics of Phyllanthus muellerianus and its major constituent, geraniin. Med. Chem. 2016, 6, 95–104. [Google Scholar] [CrossRef]
- Trentin, D.S.; Silva, D.B.; Amaral, M.W.; Zimmer, K.R.; Silva, M.V.; Lopes, N.P.; Giordani, R.B.; Macedo, A.J. Tannins possessing bacteriostatic effect impair Pseudomonas aeruginosa adhesion and biofilm formation. PLoS ONE 2013, 8, e66257. [Google Scholar] [CrossRef]
- Olchowik-Grabarek, E.; Sękowski, S.; Kwiatek, A.; Płaczkiewicz, J.; Abdulladjanova, N.; Shlyonsky, V.; Swiecicka, I.; Zamaraeva, M. The structural changes in the membranes of Staphylococcus aureus caused by hydrolysable tannins witness their antibacterial activity. Membranes 2022, 12, 1124. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; He, C.; Song, L.; Li, T.; Cui, S.; Zhang, L.; Jia, Y. Antimicrobial activity and mechanism of larch bark procyanidins against Staphylococcus aureus. Acta Biochim. Biophys. Sin. 2017, 49, 1058–1066. [Google Scholar] [CrossRef]
- Farha, A.K.; Yang, Q.-Q.; Kim, G.; Li, H.-B.; Zhu, F.; Liu, H.-Y.; Gan, R.-Y.; Corke, H. Tannins as an alternative to antibiotics. Food Biosci. 2020, 38, 100751. [Google Scholar] [CrossRef]
- Latté, K.P.; Kolodziej, H. Antifungal effects of hydrolysable tannins and related compounds on dermatophytes, mould fungi and yeasts. Z. Für Naturforschung C 2000, 55, 467–472. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Lei, M.; Andargie, M.; Zeng, J.; Li, J. Antifungal activity and mechanism of action of tannic acid against Penicillium digitatum. Physiol. Mol. Plant Pathol. 2019, 107, 46–50. [Google Scholar] [CrossRef]
- Barbieri, R.; Coppo, E.; Marchese, A.; Daglia, M.; Sobarzo-Sánchez, E.; Nabavi, S.F.; Nabavi, S.M. Phytochemicals for human disease: An update on plant-derived compounds antibacterial activity. Microbiol. Res. 2017, 196, 44–68. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.C. Production and engineering of terpenoids in plant cell culture. Nat. Chem. Biol. 2007, 3, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Mahizan, N.A.; Yang, S.-K.; Moo, C.-L.; Song, A.A.-L.; Chong, C.-M.; Chong, C.-W.; Abushelaibi, A.; Lim, S.-H.E.; Lai, K.-S. Terpene derivatives as a potential agent against antimicrobial resistance (AMR) pathogens. Molecules 2019, 24, 2631. [Google Scholar] [CrossRef] [PubMed]
- Abdollahi, A.; Fereydouni, N.; Moradi, H.; Karimivaselabadi, A.; Zarenezhad, E.; Osanloo, M. Nanoformulated herbal compounds: Enhanced antibacterial efficacy of camphor and thymol-loaded nanogels. BMC Complement. Med. Ther. 2024, 24, 138. [Google Scholar] [CrossRef] [PubMed]
- Kamiya, H.; Haraguchi, A.; Mitarai, H.; Yuda, A.; Wada, H.; Shuxin, W.; Ziqing, R.; Weihao, S.; Wada, N. In vitro evaluation of the antimicrobial properties of terpinen-4-ol on apical periodontitis-associated bacteria. J. Infect. Chemother. 2024, 30, 306–314. [Google Scholar] [CrossRef]
- Alexopoulos, A.; Kimbaris, A.C.; Plessas, S.; Mantzourani, I.; Voidarou, C.; Pagonopoulou, O.; Tsigalou, C.; Fournomiti, M.; Bontsidis, C.; Stavropoulou, E.; et al. Combined action of piperitenone epoxide and antibiotics against clinical isolates of Staphylococcus aureus and Escherichia coli. Front. Microbiol. 2019, 10, 2607. [Google Scholar] [CrossRef] [PubMed]
- Salehi, B.; Upadhyay, S.; Erdogan Orhan, I.; Kumar Jugran, A.; Jayaweera, L.D.S.; Dias, A.D.; Sharopov, F.; Taheri, Y.; Martins, N.; Baghalpour, N.; et al. Therapeutic potential of α- and β-pinene: A miracle gift of nature. Biomolecules 2019, 9, 738. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.-K.; Yusoff, K.; Ajat, M.; Thomas, W.; Abushelaibi, A.; Akseer, R.; Lim, S.-H.E.; Lai, K.-S. Disruption of KPC-producing Klebsiella pneumoniae membrane via induction of oxidative stress by cinnamon bark (Cinnamomum verum J. Presl) essential oil. PLoS ONE 2019, 14, e0214326. [Google Scholar] [CrossRef] [PubMed]
- Ben Arfa, A.; Combes, S.; Preziosi-Belloy, L.; Gontard, N.; Chalier, P. Antimicrobial activity of carvacrol related to its chemical structure. Lett. Appl. Microbiol. 2006, 43, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Pinto, E.; Vale-Silva, L.; Cavaleiro, C.; Salgueiro, L. Antifungal activity of the clove essential oil from Syzygium aromaticum on Candida, Aspergillus and dermatophyte species. J. Med. Microbiol. 2009, 58, 1454–1462. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.; Zhang, Y.; Muend, S.; Rao, R. Mechanism of antifungal activity of terpenoid phenols resembles calcium stress and inhibition of the TOR pathway. Antimicrob. Agents Chemother. 2010, 54, 5062–5069. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.I.; Karima, G.; Khan, M.Z.; Shin, J.H.; Kim, J.D. Therapeutic Effects of saponins for the prevention and treatment of cancer by ameliorating inflammation and angiogenesis and inducing antioxidant and apoptotic effects in human cells. Int. J. Mol. Sci. 2022, 23, 10665. [Google Scholar] [CrossRef] [PubMed]
- Boysen, R.I.; Hearn, M.T.W. High Performance liquid chromatographic separation methods. In Comprehensive Natural Products II; Elsevier: Amsterdam, The Netherlands, 2010; pp. 5–49. ISBN 978-0-08-045382-8. [Google Scholar]
- Gökkaya, İ.; Renda, G.; Subaş, T.; Özgen, U. Phytochemical, pharmacological, and toxicological studies on Peganum harmala L.: An overview of the last decade. Clin. Exp. Health Sci. 2023, 13, 664–678. [Google Scholar] [CrossRef]
- Sen, S.; Makkar, H.P.S.; Becker, K. Alfalfa saponins and their implication in animal nutrition. J. Agric. Food Chem. 1998, 46, 131–140. [Google Scholar] [CrossRef]
- Bachran, C.; Sutherland, M.; Heisler, I.; Hebestreit, P.; Melzig, M.F.; Fuchs, H. The saponin-mediated enhanced uptake of targeted saporin-based drugs is strongly dependent on the saponin structure. Exp. Biol. Med. 2006, 231, 412–420. [Google Scholar] [CrossRef]
- Cushnie, T.P.T.; Cushnie, B.; Lamb, A.J. Alkaloids: An overview of their antibacterial, antibiotic-enhancing and antivirulence activities. Int. J. Antimicrob. Agents 2014, 44, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Grijalva, E.P.; López-Martínez, L.X.; Contreras-Angulo, L.A.; Elizalde-Romero, C.A.; Heredia, J.B. Plant alkaloids: Structures and bioactive properties. In Plant-Derived Bioactives; Swamy, M.K., Ed.; Springer: Singapore, 2020; pp. 85–117. ISBN 9789811523601. [Google Scholar]
- Yan, Y.; Li, X.; Zhang, C.; Lv, L.; Gao, B.; Li, M. Research progress on antibacterial activities and mechanisms of natural alkaloids: A review. Antibiotics 2021, 10, 318. [Google Scholar] [CrossRef] [PubMed]
- Beuria, T.K.; Santra, M.K.; Panda, D. Sanguinarine blocks cytokinesis in bacteria by inhibiting FtsZ assembly and bundling. Biochemistry 2005, 44, 16584–16593. [Google Scholar] [CrossRef] [PubMed]
- Lei, Q.; Liu, H.; Peng, Y.; Xiao, P. In Silico target fishing and pharmacological profiling for the isoquinoline alkaloids of Macleaya cordata (Bo Luo Hui). Chin. Med. 2015, 10, 37. [Google Scholar] [CrossRef] [PubMed]
- Mabhiza, D.; Chitemerere, T.; Mukanganyama, S. Antibacterial properties of alkaloid extracts from Callistemon citrinus and Vernonia adoensis against Staphylococcus aureus and Pseudomonas aeruginosa. Int. J. Med. Chem. 2016, 2016, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Du, G.-F.; Le, Y.-J.; Sun, X.; Yang, X.-Y.; He, Q.-Y. Proteomic investigation into the action mechanism of berberine against Streptococcus pyogenes. J. Proteom. 2020, 215, 103666. [Google Scholar] [CrossRef] [PubMed]
- Khan, H.; Mubarak, M.S.; Amin, S. Antifungal potential of alkaloids as an emerging therapeutic target. Curr. Drug Targets 2017, 18, 1825–1835. [Google Scholar] [CrossRef] [PubMed]
- Silva-Beltrán, N.P.; Boon, S.A.; Ijaz, M.K.; McKinney, J.; Gerba, C.P. Antifungal activity and mechanism of action of natural product derivates as potential environmental disinfectants. J. Ind. Microbiol. Biotechnol. 2023, 50, kuad036. [Google Scholar] [CrossRef] [PubMed]
- Lanzotti, V.; Scala, F.; Bonanomi, G. Compounds from Allium species with cytotoxic and antimicrobial activity. Phytochem. Rev. 2014, 13, 769–791. [Google Scholar] [CrossRef]
- Cavallito, C.J.; Bailey, J.H. Allicin, the Antibacterial principle of Allium sativum. I. Isolation, physical properties and antibacterial action. J. Am. Chem. Soc. 1944, 66, 1950–1951. [Google Scholar] [CrossRef]
- Yamada, Y.; Azuma, K. Evaluation of the in vitro antifungal activity of allicin. Antimicrob. Agents Chemother. 1977, 11, 743–749. [Google Scholar] [CrossRef] [PubMed]
- Leontiev, R.; Hohaus, N.; Jacob, C.; Gruhlke, M.C.H.; Slusarenko, A.J. A Comparison of the antibacterial and antifungal activities of thiosulfinate analogues of allicin. Sci. Rep. 2018, 8, 6763. [Google Scholar] [CrossRef] [PubMed]
- Jakobsen, T.H.; Van Gennip, M.; Phipps, R.K.; Shanmugham, M.S.; Christensen, L.D.; Alhede, M.; Skindersoe, M.E.; Rasmussen, T.B.; Friedrich, K.; Uthe, F.; et al. Ajoene, a sulfur-rich molecule from garlic, inhibits genes controlled by quorum sensing. Antimicrob. Agents Chemother. 2012, 56, 2314–2325. [Google Scholar] [CrossRef] [PubMed]
- Tsao, S.-M.; Liu, W.-H.; Yin, M.-C. Two Diallyl sulphides derived from garlic inhibit meticillin-resistant Staphylococcus aureus infection in diabetic mice. J. Med. Microbiol. 2007, 56, 803–808. [Google Scholar] [CrossRef] [PubMed]
- Sebtosheikh, P.; Qomi, M.; Ghadami, S.; Mojab, F. Analysis of essential oil from leaves and bulb of Allium atroviolaceum. Int. Pharm. Acta 2020, 3, 3e8. [Google Scholar] [CrossRef]
- Hatami, M.; Karimi, M.; Aghaee, A.; Bovand, F.; Ghorbanpour, M. Morphological Diversity, Phenolic acids, and antioxidant properties in eryngo (Eryngium caucasicum Trautv): Selection of superior populations for agri-food industry. Food Sci. Nutr. 2022, 10, 3905–3919. [Google Scholar] [CrossRef] [PubMed]
- Fidan, H.; Stefanova, G.; Kostova, I.; Stankov, S.; Damyanova, S.; Stoyanova, A.; Zheljazkov, V.D. Chemical composition and antimicrobial activity of Laurus nobilis L. essential oils from Bulgaria. Molecules 2019, 24, 804. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, G.; Midiri, A.; Gerace, E.; Biondo, C. Bacterial antibiotic resistance: The most critical pathogens. Pathogens 2021, 10, 1310. [Google Scholar] [CrossRef] [PubMed]
- Rossolini, G.M.; Arena, F.; Pecile, P.; Pollini, S. Update on the antibiotic resistance crisis. Curr. Opin. Pharmacol. 2014, 18, 56–60. [Google Scholar] [CrossRef]
- Jubair, N.; Rajagopal, M.; Chinnappan, S.; Abdullah, N.B.; Fatima, A. Review on the antibacterial mechanism of plant-derived compounds against multidrug-resistant bacteria (MDR). Evid. Based Complement. Alternat. Med. 2021, 2021, 1–30. [Google Scholar] [CrossRef]
- Ghannoum, M.A.; Rice, L.B. Antifungal Agents: Mode of action, mechanisms of resistance, and correlation of these mechanisms with bacterial resistance. Clin. Microbiol. Rev. 1999, 12, 501–517. [Google Scholar] [CrossRef] [PubMed]
- Tenover, F.C. Mechanisms of antimicrobial resistance in bacteria. Am. J. Infect. Control 2006, 34, S3–S10. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, K.; Xu, B. A Critical Review on Phytochemical profile and health promoting effects of mung bean (Vigna radiata). Food Sci. Hum. Wellness 2018, 7, 11–33. [Google Scholar] [CrossRef]
- Dahlem Junior, M.A.; Nguema Edzang, R.W.; Catto, A.L.; Raimundo, J.-M. Quinones as an efficient molecular scaffold in the antibacterial/antifungal or antitumoral arsenal. Int. J. Mol. Sci. 2022, 23, 14108. [Google Scholar] [CrossRef] [PubMed]
- Sanver, D.; Murray, B.S.; Sadeghpour, A.; Rappolt, M.; Nelson, A.L. Experimental modeling of flavonoid–biomembrane interactions. Langmuir 2016, 32, 13234–13243. [Google Scholar] [CrossRef] [PubMed]
- Mickymaray, S. Efficacy and Mechanism of traditional medicinal plants and bioactive compounds against clinically important pathogens. Antibiotics 2019, 8, 257. [Google Scholar] [CrossRef] [PubMed]
- Ultee, A.; Bennik, M.H.J.; Moezelaar, R. The phenolic hydroxyl group of carvacrol is essential for action against the food-borne pathogen Bacillus cereus. Appl. Environ. Microbiol. 2002, 68, 1561–1568. [Google Scholar] [CrossRef]
- Huang, W.; Wang, Y.; Tian, W.; Cui, X.; Tu, P.; Li, J.; Shi, S.; Liu, X. Biosynthesis investigations of terpenoid, alkaloid, and flavonoid antimicrobial agents derived from medicinal plants. Antibiotics 2022, 11, 1380. [Google Scholar] [CrossRef]
- Di Pasqua, R.; Betts, G.; Hoskins, N.; Edwards, M.; Ercolini, D.; Mauriello, G. Membrane toxicity of antimicrobial compounds from essential oils. J. Agric. Food Chem. 2007, 55, 4863–4870. [Google Scholar] [CrossRef]
- Lee, H.; Woo, E.-R.; Lee, D.G. Apigenin induces cell shrinkage in Candida albicans by membrane perturbation. FEMS Yeast Res. 2018, 18, foy003. [Google Scholar] [CrossRef]
- Dorsaz, S.; Snäkä, T.; Favre-Godal, Q.; Maudens, P.; Boulens, N.; Furrer, P.; Ebrahimi, S.N.; Hamburger, M.; Allémann, E.; Gindro, K.; et al. Identification and mode of action of a plant natural product targeting human fungal pathogens. Antimicrob. Agents Chemother. 2017, 61, e00829-17. [Google Scholar] [CrossRef] [PubMed]
- Khameneh, B.; Iranshahy, M.; Soheili, V.; Fazly Bazzaz, B.S. Review on plant antimicrobials: A mechanistic viewpoint. Antimicrob. Resist. Infect. Control 2019, 8, 118. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Kong, Y.; Wu, D.; Zhang, H.; Wu, J.; Chen, J.; Ding, J.; Hu, L.; Jiang, H.; Shen, X. Three flavonoids targeting the β-hydroxyacyl-acyl carrier protein dehydratase from Helicobacter Pylori: Crystal structure characterization with enzymatic inhibition assay. Protein Sci. 2008, 17, 1971–1978. [Google Scholar] [CrossRef] [PubMed]
- Jeong, K.-W.; Lee, J.-Y.; Kang, D.-I.; Lee, J.-U.; Shin, S.Y.; Kim, Y. Screening of flavonoids as candidate antibiotics against Enterococcus faecalis. J. Nat. Prod. 2009, 72, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Elmasri, W.A.; Zhu, R.; Peng, W.; Al-Hariri, M.; Kobeissy, F.; Tran, P.; Hamood, A.N.; Hegazy, M.F.; Paré, P.W.; Mechref, Y. Multitargeted flavonoid inhibition of the pathogenic bacterium Staphylococcus aureus: A proteomic characterization. J. Proteome Res. 2017, 16, 2579–2586. [Google Scholar] [CrossRef] [PubMed]
- Eumkeb, G.; Siriwong, S.; Phitaktim, S.; Rojtinnakorn, N.; Sakdarat, S. Synergistic activity and mode of action of flavonoids isolated from smaller galangal and amoxicillin combinations against amoxicillin-resistant Escherichia coli: Synergistic of flavonoid on E. coli. J. Appl. Microbiol. 2012, 112, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Curto, M.Á.; Butassi, E.; Ribas, J.C.; Svetaz, L.A.; Cortés, J.C.G. Natural products targeting the synthesis of β(1,3)-d-glucan and chitin of the fungal cell wall. existing drugs and recent findings. Phytomedicine 2021, 88, 153556. [Google Scholar] [CrossRef] [PubMed]
- Douglas, C.M. Fungal ß(1,3)-D-Glucan Synthesis. Med. Mycol. 2001, 39, 55–66. [Google Scholar] [CrossRef] [PubMed]
- Arita-Morioka, K.; Yamanaka, K.; Mizunoe, Y.; Tanaka, Y.; Ogura, T.; Sugimoto, S. Inhibitory effects of myricetin derivatives on curli-dependent biofilm formation in Escherichia coli. Sci. Rep. 2018, 8, 8452. [Google Scholar] [CrossRef]
- Sharma, D.; Misba, L.; Khan, A.U. Antibiotics versus biofilm: An emerging battleground in microbial communities. Antimicrob. Resist. Infect. Control 2019, 8, 76. [Google Scholar] [CrossRef]
- Srinivasan, R.; Santhakumari, S.; Poonguzhali, P.; Geetha, M.; Dyavaiah, M.; Xiangmin, L. Bacterial biofilm inhibition: A focused review on recent therapeutic strategies for combating the biofilm mediated infections. Front. Microbiol. 2021, 12, 676458. [Google Scholar] [CrossRef] [PubMed]
- Awolola, G.; Koorbanally, N.; Chenia, H.; Shode, F.; Baijnath, H. Antibacterial and anti-biofilm activity of flavonoids and triterpenes isolated from the extracts of Ficus sansibarica Warb. subsp. sansibarica (Moraceae) extracts. Afr. J. Tradit. Complement. Altern. Med. 2014, 11, 124. [Google Scholar] [CrossRef] [PubMed]
- Cushnie, T.P.T.; Hamilton, V.E.S.; Chapman, D.G.; Taylor, P.W.; Lamb, A.J. Aggregation of Staphylococcus aureus following treatment with the antibacterial flavonol galangin: Aggregation of S. aureus by galangin. J. Appl. Microbiol. 2007, 103, 1562–1567. [Google Scholar] [CrossRef]
- Zhang, Q.; Lyu, Y.; Huang, J.; Zhang, X.; Yu, N.; Wen, Z.; Chen, S. Antibacterial activity and mechanism of sanguinarine against Providencia rettgeri in vitro. PeerJ 2020, 8, e9543. [Google Scholar] [CrossRef] [PubMed]
- Sun, T.; Li, X.-D.; Hong, J.; Liu, C.; Zhang, X.-L.; Zheng, J.-P.; Xu, Y.-J.; Ou, Z.-Y.; Zheng, J.-L.; Yu, D.-J. Inhibitory effect of two traditional Chinese medicine monomers, berberine and matrine, on the quorum sensing system of antimicrobial-resistant Escherichia coli. Front. Microbiol. 2019, 10, 2584. [Google Scholar] [CrossRef] [PubMed]
- Peralta, M.A.; Da Silva, M.A.; Ortega, M.G.; Cabrera, J.L.; Paraje, M.G. Antifungal activity of a prenylated flavonoid from Dalea elegans against Candida albicans biofilms. Phytomedicine 2015, 22, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Reece, R.J.; Maxwell, A. DNA Gyrase: Structure and function. Crit. Rev. Biochem. Mol. Biol. 1991, 26, 335–375. [Google Scholar] [CrossRef]
- Wu, T.; Zang, X.; He, M.; Pan, S.; Xu, X. Structure–activity relationship of flavonoids on their anti-Escherichia coli activity and inhibition of DNA gyrase. J. Agric. Food Chem. 2013, 61, 8185–8190. [Google Scholar] [CrossRef] [PubMed]
- Verma, K.; Mahalapbutr, P.; Suriya, U.; Somboon, T.; Aiebchun, T.; Shi, L.; Maitarad, P.; Rungrotmongkol, T. In silico screening of DNA gyrase B potent flavonoids for the treatment of Clostridium difficile infection from PhytoHub database. Braz. Arch. Biol. Technol. 2021, 64, e21200402. [Google Scholar] [CrossRef]
- Shadrick, W.R.; Ndjomou, J.; Kolli, R.; Mukherjee, S.; Hanson, A.M.; Frick, D.N. Discovering new medicines targeting helicases: Challenges and recent progress. SLAS Discov. 2013, 18, 761–781. [Google Scholar] [CrossRef]
- Bhosle, A.; Chandra, N. Structural Analysis of dihydrofolate reductases enables rationalization of antifolate binding affinities and suggests repurposing possibilities. FEBS J. 2016, 283, 1139–1167. [Google Scholar] [CrossRef] [PubMed]
- Saito, H.; Tamura, M.; Imai, K.; Ishigami, T.; Ochiai, K. Catechin inhibits Candida albicans dimorphism by disrupting Cek1 phosphorylation and cAMP synthesis. Microb. Pathog. 2013, 56, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Cassetta, A.; Stojan, J.; Krastanova, I.; Kristan, K.; Brunskole Švegelj, M.; Lamba, D.; Lanišnik Rižner, T. Structural basis for inhibition of 17β-hydroxysteroid dehydrogenases by phytoestrogens: The case of fungal 17β-HSDcl. J. Steroid Biochem. Mol. Biol. 2017, 171, 80–93. [Google Scholar] [CrossRef] [PubMed]
- Picerno, P.; Mencherini, T.; Sansone, F.; Del Gaudio, P.; Granata, I.; Porta, A.; Aquino, R.P. Screening of a polar extract of Paeonia rockii: Composition and antioxidant and antifungal activities. J. Ethnopharmacol. 2011, 138, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Chinnam, N.; Dadi, P.K.; Sabri, S.A.; Ahmad, M.; Kabir, M.A.; Ahmad, Z. Dietary bioflavonoids inhibit Escherichia coli ATP synthase in a differential manner. Int. J. Biol. Macromol. 2010, 46, 478–486. [Google Scholar] [CrossRef]
- Xu, X.; Zhou, X.D.; Wu, C.D. The Tea catechin epigallocatechin gallate suppresses cariogenic virulence factors of Streptococcus mutans. Antimicrob. Agents Chemother. 2011, 55, 1229–1236. [Google Scholar] [CrossRef]
- Chen, C.; Long, L.; Zhang, F.; Chen, Q.; Chen, C.; Yu, X.; Liu, Q.; Bao, J.; Long, Z. Antifungal activity, main active components and mechanism of Curcuma longa extract against Fusarium graminearum. PLoS ONE 2018, 13, e0194284. [Google Scholar] [CrossRef] [PubMed]
- Memar, M.Y.; Ghotaslou, R.; Samiei, M.; Adibkia, K. Antimicrobial use of reactive oxygen therapy: Current insights. Infect. Drug Resist. 2018, 11, 567–576. [Google Scholar] [CrossRef] [PubMed]
- Fathima, A.; Rao, J.R. Selective toxicity of catechin—A natural flavonoid towards bacteria. Appl. Microbiol. Biotechnol. 2016, 100, 6395–6402. [Google Scholar] [CrossRef]
- Kwun, M.S.; Lee, D.G. Quercetin-induced yeast apoptosis through mitochondrial dysfunction under the accumulation of magnesium in Candida albicans. Fungal Biol. 2020, 124, 83–90. [Google Scholar] [CrossRef]
- Kang, K.; Fong, W.-P.; Tsang, P.W.-K. Novel Antifungal activity of purpurin against Candida species in vitro. Med. Mycol. 2010, 48, 904–911. [Google Scholar] [CrossRef] [PubMed]
- Waditzer, M.; Bucar, F. Flavonoids as inhibitors of bacterial efflux pumps. Molecules 2021, 26, 6904. [Google Scholar] [CrossRef] [PubMed]
- Dias, K.J.S.D.O.; Miranda, G.M.; Bessa, J.R.; Araújo, A.C.J.D.; Freitas, P.R.; Almeida, R.S.D.; Paulo, C.L.R.; Neto, J.B.D.A.; Coutinho, H.D.M.; Ribeiro-Filho, J. Terpenes as bacterial efflux pump inhibitors: A systematic review. Front. Pharmacol. 2022, 13, 953982. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Manoharlal, R.; Shukla, S.; Puri, N.; Prasad, T.; Ambudkar, S.V.; Prasad, R. Curcumin modulates efflux mediated by yeast ABC multidrug transporters and is synergistic with antifungals. Antimicrob. Agents Chemother. 2009, 53, 3256–3265. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).