Genetic Determinants of Clarithromycin and Fluoroquinolones Resistance in Helicobacter pylori in Serbia
Abstract
1. Introduction
2. Results
2.1. Detection of Helicobacter pylori
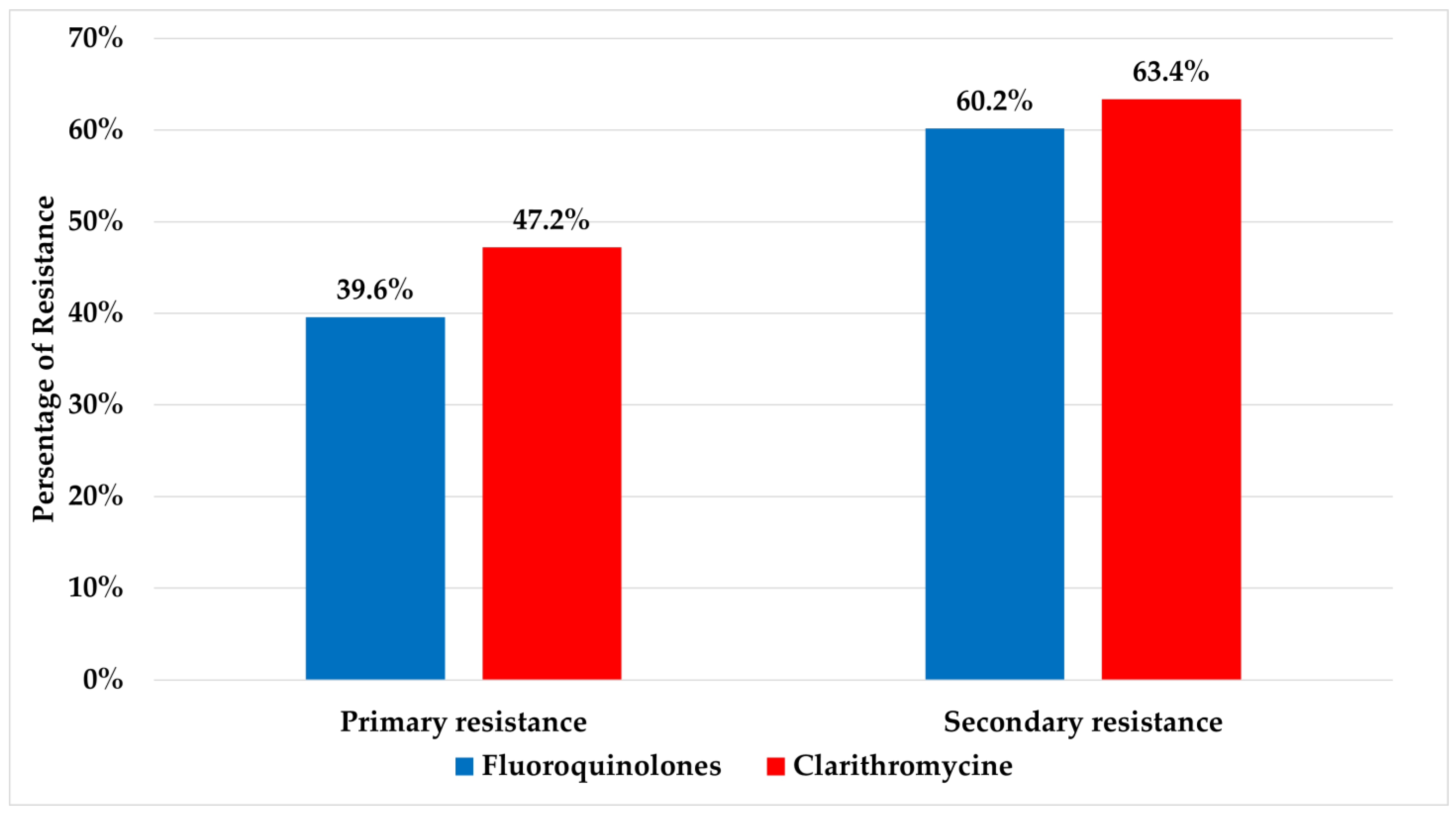
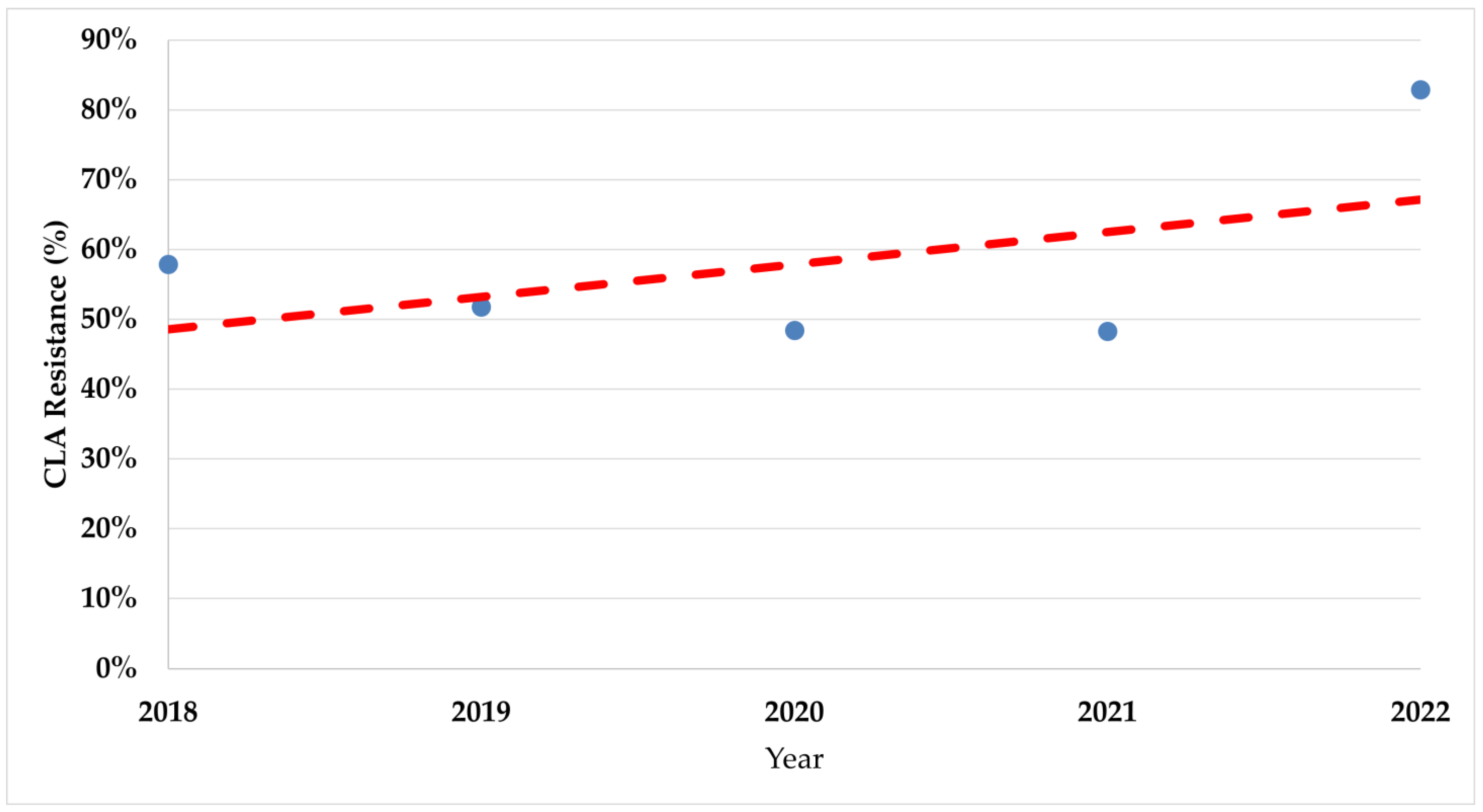
2.2. Detection of Antibiotic Resistance Genes
3. Discussion
4. Materials and Methods
4.1. Patients
4.2. DNA Extraction and Molecular Testing by GenoType Helico DR Kit
4.3. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Peleteiro, B.; Bastos, A.; Ferro, A.; Lunet, N. Prevalence of Helicobacter pylori infection worldwide: A systematic review of studies with national coverage. Dig. Dis. Sci. 2014, 59, 1698–1709. [Google Scholar] [CrossRef] [PubMed]
- Milivojevic, V.; Rankovic, I.; Krstic, M.N.; Milosavljevic, T. Dyspepsia challenge in primary care gastroenterology. Dig. Dis. 2022, 40, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Zamani, M.; Ebrahimtabar, F.; Zamani, V.; Miller, W.H.; Alizadeh-Navaei, R.; Shokri-Shirvani, J.; Derakhshan, M.H. Systematic review with meta-analysis: The Worldwide prevalence of Helicobacter pylori infection. Aliment. Pharmacol. Ther. 2018, 47, 868–876. [Google Scholar] [CrossRef] [PubMed]
- Malfertheiner, P.; Megraud, F.; Rokkas, T.; Gisbert, J.P.; Liou, J.-M.; Schulz, C.; Gasbarrini, A.; Hunt, R.H.; Leja, M.; O’Morain, C.; et al. Management of Helicobacter pylori infection: The Maastricht VI/Florence Consensus Report. Gut 2022, 71, 1724–1762. [Google Scholar] [CrossRef] [PubMed]
- Malfertheiner, P.; Megraud, F.; O’Morain, C.A.; Gisbert, J.P.; Kuipers, E.J.; Axon, A.T.; Bazzoli, F.; Gasbarrini, A.; Atherton, J.; Graham, D.Y.; et al. Management of Helicobacter pylori infection—The Maastricht V/Florence Consensus Report. Gut 2017, 66, 6–30. [Google Scholar] [CrossRef]
- Nyssen, O.P.; Martínez, B.; Mégraud, F.; Savarino, V.; Fallone, C.A.; Bazzoli, F.; Gisbert, J.P. Sequential versus standard triple therapy for first-line Helicobacter pylori eradication: An update. Antibiotics 2024, 13, 136. [Google Scholar] [CrossRef]
- Thung, I.; Aramin, H.; Vavinskaya, V.; Gupta, S.; Park, J.Y.; Crowe, S.E.; Valasek, M.A. Review Article: The global emergence of Helicobacter pylori antibiotic resistance. Aliment. Pharmacol. Ther. 2016, 43, 514–533. [Google Scholar] [CrossRef]
- Dang, B.N.; Graham, D.Y. Helicobacter pylori infection and antibiotic resistance: A WHO High Priority? Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 383–384. [Google Scholar] [CrossRef]
- WHO. Bacterial Priority Pathogens List, 2024: Bacterial Pathogens of Public Health Importance to Guide Research, Development and Strategies to Prevent and Control Antimicrobial Resistance; WHO: Geneva, Switzerland, 2024. [Google Scholar]
- Megraud, F.; Bruyndonckx, R.; Coenen, S.; Wittkop, L.; Huang, T.-D.; Hoebeke, M.; Bénéjat, L.; Lehours, P.; Goossens, H.; Glupczynski, Y. Helicobacter pylori resistance to antibiotics in Europe in 2018 and its relationship to antibiotic consumption in the community. Gut 2021, 70, 1815–1822. [Google Scholar] [CrossRef]
- Savoldi, A.; Carrara, E.; Graham, D.Y.; Conti, M.; Tacconelli, E. Prevalence of antibiotic resistance in Helicobacter pylori: A systematic review and meta-analysis in World Health Organization Regions. Gastroenterology 2018, 155, 1372–1382.e17. [Google Scholar] [CrossRef]
- Fekadu, S.; Engiso, H.; Seyfe, S.; Iizasa, H.; Godebo, A.; Deyno, S.; Yoshiyama, H. Effectiveness of eradication therapy for Helicobacter pylori infection in Africa: A systematic review and meta-analysis. BMC Gastroenterol. 2023, 23, 55. [Google Scholar] [CrossRef] [PubMed]
- Saracino, I.M.; Pavoni, M.; Zullo, A.; Fiorini, G.; Saccomanno, L.; Lazzarotto, T.; Cavallo, R.; Antonelli, G.; Vaira, D. Antibiotic resistance and therapy outcome in H. pylori eradication failure patients. Antibiotics 2020, 9, 121. [Google Scholar] [CrossRef] [PubMed]
- Kocsmár, É.; Buzás, G.M.; Szirtes, I.; Kocsmár, I.; Kramer, Z.; Szijártó, A.; Fadgyas-Freyler, P.; Szénás, K.; Rugge, M.; Fassan, M.; et al. Primary and secondary clarithromycin resistance in Helicobacter pylori and mathematical modeling of the role of macrolides. Nat. Commun. 2021, 12, 2255. [Google Scholar] [CrossRef] [PubMed]
- Zerbetto De Palma, G.; Mendiondo, N.; Wonaga, A.; Viola, L.; Ibarra, D.; Campitelli, E.; Salim, N.; Corti, R.; Goldman, C.; Catalano, M. Occurrence of mutations in the antimicrobial target genes related to levofloxacin, clarithromycin, and amoxicillin resistance in Helicobacter pylori isolates from Buenos Aires city. Microb. Drug Resist. 2017, 23, 351–358. [Google Scholar] [CrossRef]
- Cambau, E.; Allerheiligen, V.; Coulon, C.; Corbel, C.; Lascols, C.; Deforges, L.; Soussy, C.-J.; Delchier, J.-C.; Megraud, F. Evaluation of a new test, GenoType HelicoDR, for molecular detection of antibiotic resistance in Helicobacter pylori. J. Clin. Microbiol. 2009, 47, 3600–3607. [Google Scholar] [CrossRef]
- De Francesco, V.; Zullo, A.; Giorgio, F.; Saracino, I.; Zaccaro, C.; Hassan, C.; Ierardi, E.; Di Leo, A.; Fiorini, G.; Castelli, V.; et al. Change of point mutations in Helicobacter pylori rRNA associated with clarithromycin resistance in Italy. J. Med. Microbiol. 2014, 63, 453–457. [Google Scholar] [CrossRef]
- Marques, A.T.; Vítor, J.M.B.; Santos, A.; Oleastro, M.; Vale, F.F. Trends in Helicobacter pylori resistance to clarithromycin: From phenotypic to genomic approaches. Microb. Genomics 2020, 6, e000344. [Google Scholar] [CrossRef]
- Hashemi, S.J.; Farajzadeh Sheikh, A.; Goodarzi, H.; Yadyad, M.J.; Seyedian, S.S.; Aslani, S.; Assarehzadegan, M.-A. Genetic basis for metronidazole and clarithromycin resistance in Helicobacter pylori strains isolated from patients with gastroduodenal disorders. Infect. Drug Resist. 2019, 12, 535–543. [Google Scholar] [CrossRef]
- Camorlinga-Ponce, M.; Gómez-Delgado, A.; Aguilar-Zamora, E.; Torres, R.C.; Giono-Cerezo, S.; Escobar-Ogaz, A.; Torres, J. Phenotypic and genotypic antibiotic resistance patterns in Helicobacter pylori strains from ethnically diverse population in México. Front. Cell. Infect. Microbiol. 2021, 10, 539115. [Google Scholar] [CrossRef]
- Francesco, V. De Mechanisms of Helicobacter pylori antibiotic resistance: An updated appraisal. World J. Gastrointest. Pathophysiol. 2011, 2, 35. [Google Scholar] [CrossRef]
- Gong, E.J.; Ahn, J.Y.; Kim, J.M.; Lee, S.M.; Na, H.K.; Lee, J.H.; Jung, K.W.; Choi, K.D.; Kim, D.H.; Song, H.J.; et al. Genotypic and phenotypic resistance to clarithromycin in Helicobacter pylori strains. J. Clin. Med. 2020, 9, 1930. [Google Scholar] [CrossRef] [PubMed]
- Milivojevic, V.; Babic, I.; Kekic, D.; Rankovic, I.; Sagdati, S.; Panic, N.; Spasic, I.S.; Krstic, M.; Milosavljevic, T.; Moreira, L.; et al. Current trends in the management of Helicobacter pylori infection in Serbia: Preliminary results from the European Registry on H. pylori Management. Dig. Dis. 2023, 41, 377–386. [Google Scholar] [CrossRef] [PubMed]
- Malfertheiner, P.; Camargo, M.C.; El-Omar, E.; Liou, J.-M.; Peek, R.; Schulz, C.; Smith, S.I.; Suerbaum, S. Helicobacter pylori Infection. Nat. Rev. Dis. Prim. 2023, 9, 19. [Google Scholar] [CrossRef] [PubMed]
- Binyamin, D.; Pastukh, N.; On, A.; Paritsky, M.; Peretz, A. Phenotypic and genotypic correlation as expressed in Helicobacter pylori resistance to clarithromycin and fluoroquinolones. Gut Pathog. 2017, 9, 48. [Google Scholar] [CrossRef]
- Fernandez-Caso, B.; Miqueleiz, A.; Valdez, V.B.; Alarcón, T. Are molecular methods helpful for the Diagnosis of Helicobacter pylori infection and for the prediction of its antimicrobial resistance? Front. Microbiol. 2022, 13, 962063. [Google Scholar] [CrossRef]
- Tepes, B.; Kastelic, M.; Vujasinovic, M.; Lampic, P.; Seruga, M.; Jurecic, N.B.; Nyssen, O.P.; Donday, M.G.; O’Morain, C.; Megraud, F.; et al. Helicobacter pylori treatment results in Slovenia in the period 2013–2015 as a part of European Registry on Helicobacter pylori Management. Radiol. Oncol. 2017, 52, 1–6. [Google Scholar] [CrossRef]
- Graham, D.Y.; Lee, Y.; Wu, M. Rational Helicobacter pylori Therapy: Evidence-based medicine rather than medicine-based evidence. Clin. Gastroenterol. Hepatol. 2014, 12, 177–186.e3. [Google Scholar] [CrossRef]
- Dang, N.Q.H.; Ha, T.M.T.; Nguyen, S.-T.; Le, N.D.K.; Nguyen, T.M.T.; Nguyen, T.H.; Pham, T.T.H.; Tran, V.H. High rates of clarithromycin and levofloxacin resistance of Helicobacter pylori in patients with chronic gastritis in the South East Area of Vietnam. J. Glob. Antimicrob. Resist. 2020, 22, 620–624. [Google Scholar] [CrossRef]
- Bujanda, L.; Nyssen, O.P.; Vaira, D.; Saracino, I.M.; Fiorini, G.; Lerang, F.; Georgopoulos, S.; Tepes, B.; Heluwaert, F.; Gasbarrini, A.; et al. Antibiotic Resistance Prevalence and Trends in Patients Infected with Helicobacter pylori in the Period 2013–2020: Results of the European Registry on H. pylori Management (Hp-EuReg). Antibiotics 2021, 10, 1058. [Google Scholar] [CrossRef]
- Van Boeckel, T.P.; Gandra, S.; Ashok, A.; Caudron, Q.; Grenfell, B.T.; Levin, S.A.; Laxminarayan, R. Global antibiotic consumption 2000 to 2010: An analysis of National Pharmaceutical Sales Data. Lancet Infect. Dis. 2014, 14, 742–750. [Google Scholar] [CrossRef]
- Chen, P.-Y.; Wu, M.-S.; Chen, C.-Y.; Bair, M.-J.; Chou, C.-K.; Lin, J.-T.; Liou, J.-M. Systematic review with meta-analysis: The efficacy of levofloxacin triple therapy as the first- or second-line treatments of Helicobacter pylori infection. Aliment. Pharmacol. Ther. 2016, 44, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Papastergiou, V. Seven-Day genotypic resistance-guided triple Helicobacter pylori eradication therapy can be highly effective. Ann. Gastroenterol. 2017, 31, 198. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, F.; Gong, X.; Yan, L.; Zhao, Q.; Song, Y.; Zhao, R.; He, Y.; Zhou, L.; Liu, D.; et al. Genotype profiles of Helicobacter pylori from gastric biopsies and strains with antimicrobial-induced resistance. Therap. Adv. Gastroenterol. 2020, 13, 175628482095259. [Google Scholar] [CrossRef] [PubMed]
- Lauener, F.; Imkamp, F.; Lehours, P.; Buissonnière, A.; Benejat, L.; Zbinden, R.; Keller, P.; Wagner, K. genetic determinants and prediction of antibiotic resistance phenotypes in Helicobacter pylori. J. Clin. Med. 2019, 8, 53. [Google Scholar] [CrossRef] [PubMed]
- Buran, T.; Sürücüoğlu, S.; Kurutepe, S.; Gazi, H. Recent trends in the antibiotic resistance of Helicobacter Pylori in patient with dyspepsia. Medicine 2022, 101, e29801. [Google Scholar] [CrossRef]
- Martins, G.M.; Sanches, B.S.F.; Moretzsohn, L.D.; Lima, K.S.; Cota, B.D.C.V.; Coelho, L.G.V. Molecular detection of clarithromycin and fluoroquinolones resistance in Helicobacter pylori infection, directly applied to gastric biopsies, in an urban brazilian population. Arq. Gastroenterol. 2016, 53, 113–117. [Google Scholar] [CrossRef]
- Lee, J.H.; Shin, J.-H.; Roe, I.H.; Sohn, S.G.; Lee, J.H.; Kang, G.H.; Lee, H.-K.; Jeong, B.C.; Lee, S.H. Impact of clarithromycin resistance on eradication of Helicobacter pylori in infected adults. Antimicrob. Agents Chemother. 2005, 49, 1600–1603. [Google Scholar] [CrossRef]
- Noguchi, N.; Rimbara, E.; Kato, A.; Tanaka, A.; Tokunaga, K.; Kawai, T.; Takahashi, S.; Sasatsu, M. Detection of mixed clarithromycin-resistant and -susceptible Helicobacter pylori using nested pcr and direct sequencing of dna extracted from faeces. J. Med. Microbiol. 2007, 56, 1174–1180. [Google Scholar] [CrossRef]
- Sheu, S.-M.; Sheu, B.-S.; Lu, C.-C.; Yang, H.-B.; Wu, J.-J. Mixed infections of Helicobacter pylori: Tissue tropism and histological significance. Clin. Microbiol. Infect. 2009, 15, 253–259. [Google Scholar] [CrossRef][Green Version]
- Islam, J.M.; Yano, Y.; Okamoto, A.; Matsuda, R.; Shiraishi, M.; Hashimoto, Y.; Morita, N.; Takeuchi, H.; Suganuma, N.; Takeuchi, H. Evidence of Helicobacter pylori heterogeneity in human stomachs by susceptibility testing and characterization of mutations in drug-resistant isolates. Sci. Rep. 2024, 14, 12066. [Google Scholar] [CrossRef]
- Bačić, A.; Milivojević, V.; Petković, I.; Kekić, D.; Gajić, I.; Medić Brkić, B.; Popadić, D.; Milosavljević, T.; Rajilić-Stojanović, M. In Search for Reasons behind Helicobacter pylori Eradication failure–assessment of the antibiotics resistance rate and co-existence of Helicobacter pylori with Candida species. J. Fungi 2023, 9, 328. [Google Scholar] [CrossRef] [PubMed]
- Nishizawa, T.; Suzuki, H. Mechanisms of Helicobacter pylori antibiotic resistance and molecular testing. Front. Mol. Biosci. 2014, 1, e00019. [Google Scholar] [CrossRef] [PubMed]
- Egli, K.; Wagner, K.; Keller, P.M.; Risch, L.; Risch, M.; Bodmer, T. Comparison of the diagnostic performance of qpcr, sanger sequencing, and whole-genome sequencing in determining clarithromycin and levofloxacin resistance in Helicobacter pylori. Front. Cell. Infect. Microbiol. 2020, 10, 596371. [Google Scholar] [CrossRef] [PubMed]
- Dixon, M.F.; Genta, R.M.; Yardley, J.H.; Correa, P. Classification and Grading of Gastritis. Am. J. Surg. Pathol. 1996, 20, 1161–1181. [Google Scholar] [CrossRef]

| Variables | Clarithromycin Resistant (n = 103) | Fluoroquinolone Resistance (n = 95) | ||||
|---|---|---|---|---|---|---|
| % (n) | OR (95% CI) | p | % (n) | OR (95% CI) | p | |
| Age | ||||||
| ≤50 (n = 72) | 52.8 (38) | 0.681 (0.366–1.268) | 0.226 | 55.6 (40) | 1.127 (0.615–2.066) | 0.698 |
| >50 (n = 104) | 62.5 (65) | Ref | 52.9 (55) | Ref | ||
| Gender | ||||||
| Male (n = 67) | 46.3 (31) | 0.446 (0.239–0.833) | 0.011 * | 49.3 (33) | 0.732 (0.397–1.350) | 0.318 |
| Female (n = 109) | 66.1 (72) | Ref | 56.9 (62) | Ref | ||
| Antibiotic | Fluoroquinolones | Clarithromycin | |||||
|---|---|---|---|---|---|---|---|
| Gene | gyrA 87 | gyrA 91 | rrl | ||||
| Genotype | N87K (MUT) | D91N (MUT1) | D91G (MUT2) | D91Y (MUT3) | A2146G (MUT1) | A2146C (MUT2) | A2147G (MUT3) |
| Exchange | Asparagine/Lysine | Aspartate/Asparagine | Aspartate/Glycine | Aspartate/Tyrosine | AA/GA | AA/CA | AA/AG |
| ∑(N/%) | 26/27.4 | 23/24.2 | 19/20.0 | 14/14.7 | 25/24.3 | 5/4.8 | 81/78.6 |
| Fluoroquinolones Resistant | Clarithromycin Resistant | ||||
|---|---|---|---|---|---|
| Genotype | % of All Samples | % of Resistant Samples | Genotype | % of All Samples | % of Resistant Samples |
| WT 87 + MUT 87 | 6.3 | 3.4 | WT + MUT (1–3) | 9.1 | 15.5 |
| WT 91 + MUT 91 (1–3) | 7.4 | 4.0 | >1 MUT | 4.5 | 7.7 |
| >1 MUT 91 (1–3) | 22.1 | 11.9 | |||
| MUT 87 + MUT 91 (1–3) | 8.4 | 4.5 | |||
| WT 87 + WT 91 + MUT 87 + MUT 91 (1–3) | 2.1 | 1.1 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kekic, D.; Jovicevic, M.; Kabic, J.; Lolic, I.; Gajic, I.; Stojkovic, S.; Ranin, L.; Milosavljevic, T.; Opavski, N.; Rankovic, I.; et al. Genetic Determinants of Clarithromycin and Fluoroquinolones Resistance in Helicobacter pylori in Serbia. Antibiotics 2024, 13, 933. https://doi.org/10.3390/antibiotics13100933
Kekic D, Jovicevic M, Kabic J, Lolic I, Gajic I, Stojkovic S, Ranin L, Milosavljevic T, Opavski N, Rankovic I, et al. Genetic Determinants of Clarithromycin and Fluoroquinolones Resistance in Helicobacter pylori in Serbia. Antibiotics. 2024; 13(10):933. https://doi.org/10.3390/antibiotics13100933
Chicago/Turabian StyleKekic, Dusan, Milos Jovicevic, Jovana Kabic, Iva Lolic, Ina Gajic, Stefan Stojkovic, Lazar Ranin, Tomica Milosavljevic, Natasa Opavski, Ivan Rankovic, and et al. 2024. "Genetic Determinants of Clarithromycin and Fluoroquinolones Resistance in Helicobacter pylori in Serbia" Antibiotics 13, no. 10: 933. https://doi.org/10.3390/antibiotics13100933
APA StyleKekic, D., Jovicevic, M., Kabic, J., Lolic, I., Gajic, I., Stojkovic, S., Ranin, L., Milosavljevic, T., Opavski, N., Rankovic, I., & Milivojevic, V. (2024). Genetic Determinants of Clarithromycin and Fluoroquinolones Resistance in Helicobacter pylori in Serbia. Antibiotics, 13(10), 933. https://doi.org/10.3390/antibiotics13100933







