Genetic and Phenotypic Characterization of Subclinical Mastitis-Causing Multidrug-Resistant Staphylococcus aureus
Abstract
1. Introduction
2. Results
2.1. Cow Variables and S. aureus Isolates
2.2. Antibiotic Resistance Profile of S. aureus Isolates
2.3. Frequency of Multidrug-Resistant S. aureus (MDRSA) Isolates
2.4. Beta-Lactam Resistance, Efflux Pump, and Biofilm Formation
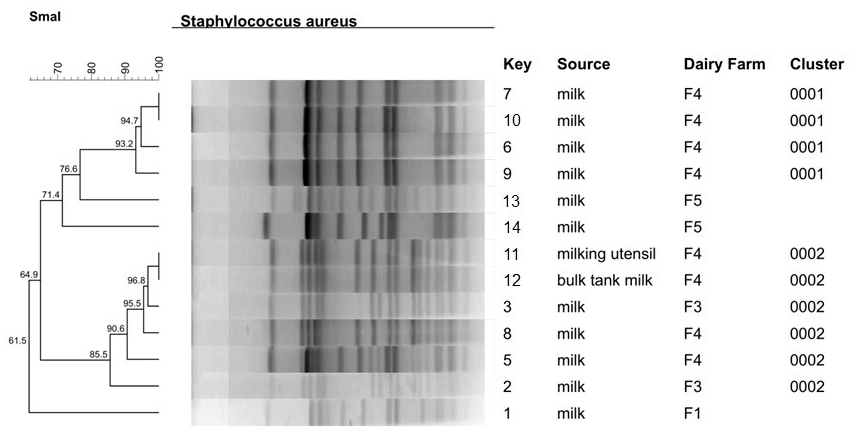
2.5. Molecular Fingerprinting of MDRSA Isolates by PFGE
2.6. Molecular Characterization of Five Cefoxitin-Resistant MDRSA Isolates by MLST
2.7. Risk Factors
3. Discussion
4. Materials and Methods
4.1. Selection of Farms and Cows
4.2. S. aureus Identification by Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI-TOF MS)
4.3. Antimicrobial Susceptibility Test
4.4. Identification of Multidrug-Resistant S. aureus (MDRSA) and Multiple Antimicrobial Resistance (MAR) Index Calculation
4.5. Biofilm Formation Assay
4.6. Detection of Genes Associated with Beta-Lactam Resistance, Efflux Pump, and Biofilm Formation
4.7. Pulsed-Field Gel Electrophoresis (PFGE)
4.8. Multi-Locus Sequence Typing (MLST)
4.9. Statistical Analyses
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Busanello, M.; Rossi, R.S.; Cassoli, L.D.; Pantoja, J.C.F.; Machado, P.F. Estimation of Prevalence and Incidence of Subclinical Mastitis in a Large Population of Brazilian Dairy Herds. J. Dairy Sci. 2017, 100, 6545–6553. [Google Scholar] [CrossRef] [PubMed]
- Silva, A.C.; Laven, R.; Benites, N.R. Risk Factors Associated with Mastitis in Smallholder Dairy Farms in Southeast Brazil. Animals 2021, 11, 2089. [Google Scholar] [CrossRef] [PubMed]
- Dittmann, K.K.; Chaul, L.T.; Lee, S.H.I.; Corassin, C.H.; de Oliveira, C.A.F.; De Martinis, E.C.P.; Alves, V.F.; Gram, L.; Oxaran, V. Staphylococcus Aureus in Some Brazilian Dairy Industries: Changes of Contamination and Diversity. Front. Microbiol. 2017, 8, 2049. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Cha, J.; Liu, K.; Deng, J.; Yang, B.; Xu, H.; Wang, J.; Zhang, L.; Gu, X.; Huang, C.; et al. The Prevalence of Bovine Mastitis-Associated Staphylococcus Aureus in China and Its Antimicrobial Resistance Rate: A Meta-Analysis. Front. Vet. Sci. 2022, 9, 1006676. [Google Scholar] [CrossRef]
- Naushad, S.; Nobrega, D.B.; Naqvi, S.A.; Barkema, H.W.; De Buck, J. Genomic Analysis of Bovine Staphylococcus Aureus Isolates from Milk To Elucidate Diversity and Determine the Distributions of Antimicrobial and Virulence Genes and Their Association with Mastitis. mSystems 2020, 5, 10-1128. [Google Scholar] [CrossRef]
- Alav, I.; Sutton, J.M.; Rahman, K.M. Role of Bacterial Efflux Pumps in Biofilm Formation. J. Antimicrob. Chemother. 2018, 73, 2003–2020. [Google Scholar] [CrossRef]
- Webber, M.A.; Piddock, L.J.V. The Importance of Efflux Pumps in Bacterial Antibiotic Resistance. J. Antimicrob. Chemother. 2003, 51, 9–11. [Google Scholar] [CrossRef]
- Bonsaglia, E.C.R.; Latosinski, G.S.; Rossi, R.S.; Rossi, B.F.; Possebon, F.S.; Pantoja, J.C.F.; Fernandes Júnior, A.; Rall, V.L.M. Biofilm Production under Different Atmospheres and Growth Media by Streptococcus Agalactiae Isolated from Milk of Cows with Subclinical Mastitis. Arch. Microbiol. 2020, 202, 209–212. [Google Scholar] [CrossRef]
- Blanco, P.; Hernando-Amado, S.; Reales-Calderon, J.A.; Corona, F.; Lira, F.; Alcalde-Rico, M.; Bernardini, A.; Sanchez, M.B.; Martinez, J.L. Bacterial Multidrug Efflux Pumps: Much More than Antibiotic Resistance Determinants. Microorganisms 2016, 4, 14. [Google Scholar] [CrossRef]
- Campos, B.; Pickering, A.C.; Rocha, L.S.; Aguilar, A.P.; Fabres-Klein, M.H.; de Oliveira Mendes, T.A.; Fitzgerald, J.R.; de Oliveira Barros Ribon, A. Diversity and Pathogenesis of Staphylococcus Aureus from Bovine Mastitis: Current Understanding and Future Perspectives. BMC Vet. Res. 2022, 18, 115. [Google Scholar] [CrossRef]
- Silva, V.; Araújo, S.; Monteiro, A.; Eira, J.; Pereira, J.E.; Maltez, L.; Igrejas, G.; Lemsaddek, T.S.; Poeta, P. Staphylococcus Aureus and MRSA in Livestock: Antimicrobial Resistance and Genetic Lineages. Microorganisms 2023, 11, 124. [Google Scholar] [CrossRef] [PubMed]
- Rainard, P.; Foucras, G.; Fitzgerald, J.R.; Watts, J.L.; Koop, G.; Middleton, J.R. Knowledge Gaps and Research Priorities in Staphylococcus Aureus Mastitis Control. Transbound. Emerg. Dis. 2018, 65, 149–165. [Google Scholar] [CrossRef] [PubMed]
- Feltrin, F.; Alba, P.; Kraushaar, B.; Ianzano, A.; Argudín, A.; Matteo, D. Staphylococcus Aureus Clonal Complex 97 Lineage Spreading in Dairy Cattle and Pigs in Italy. Appl. Environ. Microbiol. 2016, 82, 816–821. [Google Scholar] [CrossRef] [PubMed]
- Alves, B.G.; Gonçalves, J.L.; Freu, G.; Rossi, B.F.; Rall, V.L.M.; Dos Santos, M.V. Pulsed-Field Gel Electrophoresis Genotyping and Antimicrobial Resistance Profiles of Staphylococcus Aureus Isolated from Subclinical Mastitis in Dairy Cattle in Brazil. Genet. Mol. Res. 2022, 21, 11. [Google Scholar] [CrossRef]
- Gonçalves, M.S.; Dorneles, E.M.S.; Heinemann, M.B.; E Brito, M.A.V.P.; de Sá Guimarães, A. Genetic Diversity and Antimicrobial Susceptibility of Staphylococcus Aureus Isolated from Bovine Mastitis in Minas Gerais, Brazil. Cienc. Rural. 2023, 53, e20210643. [Google Scholar] [CrossRef]
- Hoekstra, J.; Zomer, A.L.; Rutten, V.P.M.G.; Benedictus, L.; Stegeman, A.; Spaninks, M.P.; Bennedsgaard, T.W.; Biggs, A.; De Vliegher, S.; Mateo, D.H.; et al. Genomic Analysis of European Bovine Staphylococcus Aureus from Clinical versus Subclinical Mastitis. Sci. Rep. 2020, 10, 18172. [Google Scholar] [CrossRef] [PubMed]
- Sivakumar, R.; Pranav, P.S.; Annamanedi, M.; Chandrapriya, S.; Isloor, S.; Rajendhran, J.; Hegde, N.R. Genome Sequencing and Comparative Genomic Analysis of Bovine Mastitis-Associated Staphylococcus Aureus Strains from India. BMC Genom. 2023, 24, 44. [Google Scholar] [CrossRef]
- Krewer, C.C.; Izabela, I.P.; Amanso, E.S.; Cavalcante, N.B.; de M. Peixoto, R.; Pinheiro, J.W.; da Costa, M.M.; Mota, R.A. Etiology, Antimicrobial Susceptibility Profile of Staphylococcus Spp. and Risk Factors Associated with Bovine Mastitis in the States of Bahia and Pernambuco. Pesqui. Vet. Bras. 2013, 33, 601–606. [Google Scholar] [CrossRef]
- Beuron, D.C.; Cortinhas, C.S.; Botaro, B.G.; Macedo, S.N.; Gonçalves, J.L.; Brito, M.A.V.P.; Santos, M.V. Risk Factors Associated with the Antimicrobial Resistance of Staphylococcus Aureus Isolated from Bovine Mastitis. Pesqui. Vet. Bras. 2014, 34, 947–952. [Google Scholar] [CrossRef][Green Version]
- Ferreira, L.B.; De Freitas Santiago Israel, L.; Rabello, R.F.; De Souza, G.N.; Peruquetti, R.C.; Dos Santos Medeiros, L. Risk Factors Associated with the Occurrence of Multiresistant Staphylococcus Spp. Isolated from Bovine Subclinical Mastitis in Northern Brazil. Semin. Cienc. Agrar. 2022, 43, 901–910. [Google Scholar] [CrossRef]
- Silva, J.G.; Araujo, W.J.; Leite, E.L.; Dias, L.M.; Vasconcelos, P.C.; Silva, N.M.V.; Oliveira, R.P.; Sena, M.J.; Oliveira, C.J.B.; Mota, R.A. First Report of a Livestock-Associated Methicillin-Resistant Staphylococcus Aureus ST126 Harbouring the MecC Variant in Brazil. Transbound. Emerg. Dis. 2021, 68, 1019–1025. [Google Scholar] [CrossRef] [PubMed]
- Garcia, S.N.; Osburn, B.I.; Cullor, J.S. A One Health Perspective on Dairy Production and Dairy Food Safety. One Health 2019, 7, 100086. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.; Brown, P.D. Multiple Antibiotic Resistance Index, Fitness and Virulence Potential in Respiratory Pseudomonas Aeruginosa from Jamaica. J. Med. Microbiol. 2016, 65, 261–271. [Google Scholar] [CrossRef] [PubMed]
- Marques, V.F.; da Motta, C.C.; da Silva Soares, B.; de Melo, D.A.; de Oliveira Coelho, S.d.M.; da Silva Coelho, I.; Barbosa, H.S.; de Souza, M.M.S. Biofilm Production and Beta-Lactamic Resistance in Brazilian Staphylococcus Aureus Isolates from Bovine Mastitis. Braz. J. Microbiol. 2017, 48, 118–124. [Google Scholar] [CrossRef] [PubMed]
- CLSI. Performance Standards for Antimicrobial Disk and Dilution Susceptiblity Tests for Bacteria Isolated from Animals, 5th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018; Available online: https://clsi.org/media/2321/vet08ed4_sample.pdf (accessed on 19 July 2023).
- Munive Nuñez, K.V.; da Silva Abreu, A.C.; Gonçalves, J.L.; dos Santos, M.V.; de Oliveira Rocha, L.; Cirone Silva, N.C. Virulence and Antimicrobial Resistance Genes Profiles of Spa Type T605 Methicillin-Susceptible Staphylococcus Aureus Isolated from Subclinical Bovine Mastitis. J. Appl. Microbiol. 2023, 134, lxad057. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, J.G.; De Barros, M.; Santos, N.D.D.L.; Paiva, P.M.G.; Napoleão, T.H.; De Sena, M.J.; Da Costa, M.M.; De Oliveira, H.P.; Moreira, M.A.S.; Mota, R.A. Antimicrobial Activity of Polypyrrole Nanoparticles and Aqueous Extract of Moringa Oleifera against Staphylococcus Spp. Carriers of Multi-Drug Efflux System Genes Isolated from Dairy Farms. J. Dairy Res. 2020, 87, 309–314. [Google Scholar] [CrossRef]
- He, X.; Ahn, J. Differential Gene Expression in Planktonic and Biofilm Cells of Multiple Antibiotic-Resistant Salmonella Typhimurium and Staphylococcus Aureus. FEMS Microbiol. Lett. 2011, 325, 180–188. [Google Scholar] [CrossRef]
- Bowler, P.; Murphy, C.; Wolcott, R. Biofilm Exacerbates Antibiotic Resistance: Is This a Current Oversight in Antimicrobial Stewardship? Antimicrob. Resist. Infect. Control 2020, 9, 162. [Google Scholar] [CrossRef]
- Valle, J.; Fang, X.; Lasa, I. Revisiting Bap Multidomain Protein: More Than Sticking Bacteria Together. Front. Microbiol. 2020, 11, 613581. [Google Scholar] [CrossRef]
- Peng, Q.; Tang, X.; Dong, W.; Sun, N.; Yuan, W. A Review of Biofilm Formation of Staphylococcus Aureus and Its Regulation Mechanism. Antibiotics 2023, 12, 12. [Google Scholar] [CrossRef]
- Liu, K.; Tao, L.; Li, J.; Fang, L.; Cui, L.; Li, J.; Meng, X.; Zhu, G.; Bi, C.; Wang, H. Characterization of Staphylococcus Aureus Isolates From Cases of Clinical Bovine Mastitis on Large-Scale Chinese Dairy Farms. Front. Vet. Sci. 2020, 7, 580129. [Google Scholar] [CrossRef]
- Silva, A.T.F.; da Silva, J.G.; Aragão, B.B.; Peixoto, R.M.; Mota, R.A. Occurrence of β-Lactam-Resistant Staphylococcus Aureus in Milk from Primiparous Dairy Cows in the Northeastern Region of Brazil. Trop. Anim. Health Prod. 2020, 52, 2303–2307. [Google Scholar] [CrossRef] [PubMed]
- da Silva Soares, B.; da Motta, C.C.; Barbieri, N.L.; de Melo, D.A.; Gomez, M.A.; de Alencar, T.A.; da Silva Coelho, I.; de Mattos de Oliveira Coelho, S.; Logue, C.M.; de Souza, M.M.S. Molecular Characterization and Genetic Diversity of Staphylococcus Aureus Isolates of Dairy Production Farms in Rio de Janeiro, Brazil. Braz. J. Vet. Med. 2021, 43, e001120. [Google Scholar] [CrossRef]
- Ben Said, M.; Abbassi, M.S.; Bianchini, V.; Sghaier, S.; Cremonesi, P.; Romanò, A.; Gualdi, V.; Hassen, A.; Luini, M. V Genetic Characterization and Antimicrobial Resistance of Staphylococcus Aureus Isolated from Bovine Milk in Tunisia. Lett. Appl. Microbiol. 2016, 63, 473–481. [Google Scholar] [CrossRef]
- Dabul, A.N.G.; Camargo, I.L.B.C. Clonal Complexes of Staphylococcus Aureus: All Mixed and Together. FEMS Microbiol. Lett. 2014, 351, 7–8. [Google Scholar] [CrossRef]
- Silva, N.C.C.; Guimarães, F.F.; Manzi, M.P.; Budri, P.E.; Gómez-Sanz, E.; Benito, D.; Langoni, H.; Rall, V.L.M.; Torres, C. Molecular Characterization and Clonal Diversity of Methicillin-Susceptible Staphylococcus Aureus in Milk of Cows with Mastitis in Brazil. J. Dairy Sci. 2013, 96, 6856–6862. [Google Scholar] [CrossRef] [PubMed]
- Boss, R.; Cosandey, A.; Luini, M.; Artursson, K.; Bardiau, M.; Breitenwieser, F.; Hehenberger, E.; Lam, T.; Mansfeld, M.; Michel, A.; et al. Bovine Staphylococcus Aureus: Subtyping, Evolution, and Zoonotic Transfer. J. Dairy Sci. 2016, 99, 515–528. [Google Scholar] [CrossRef] [PubMed]
- Badua, A.T.; Boonyayatra, S.; Awaiwanont, N.; Gaban, P.B.V.; Mingala, C.N. Methicillin-Resistant Staphylococcus Aureus (MRSA) Associated with Mastitis among Water Buffaloes in the Philippines. Heliyon 2020, 6, e05663. [Google Scholar] [CrossRef]
- Rabello, R.F.; Moreira, B.M.; Lopes, R.M.M.; Teixeira, L.M.; Riley, L.W.; Castro, A.C.D. Multilocus Sequence Typing of Staphylococcus Aureus Isolates Recovered from Cows with Mastitis in Brazilian Dairy Herds. J. Med. Microbiol. 2007, 56, 1505–1511. [Google Scholar] [CrossRef]
- Alves, M.d.F.N.F.; Penna, B.; Pereira, R.F.A.; Geraldo, R.B.; Folly, E.; Castro, H.C.; Aguiar-Alves, F. First Report of Meticillin-Resistant Staphylococcus Aureus Harboring MecC Gene in Milk Samples from Cows with Mastitis in Southeastern Brazil. Braz. J. Microbiol. 2020, 51, 2175–2179. [Google Scholar] [CrossRef]
- Bonsaglia, E.C.R.; Silva, N.C.C.; Rossi, B.F.; Camargo, C.H.; Dantas, S.T.A.; Langoni, H.; Guimarães, F.F.; Lima, F.S.; Fitzgerald, J.R.; Fernandes, A.J.; et al. Molecular Epidemiology of Methicillin-Susceptible Staphylococcus Aureus (MSSA) Isolated from Milk of Cows with Subclinical Mastitis. Microb. Pathog. 2018, 124, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Ruegg, P.L. Realities, Challenges and Benefits of Antimicrobial Stewardship in Dairy Practice in the United States. Microorganisms 2022, 10, 1626. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, C.S.F.; Hogeveen, H.; Botelho, A.M.; Maia, P.V.; Coelho, S.G.; Haddad, J.P.A. Cow-Specific Risk Factors for Clinical Mastitis in Brazilian Dairy Cattle. Prev. Vet. Med. 2015, 121, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Ryman, V.E.; Nickerson, S.C.; Hurley, D.J.; Berghaus, R.D.; Kautz, F.M. Influence of Horn Flies (Haematobia irritans) on Teat Skin Condition, Intramammary Infection, and Serum Anti-S. Aureus Antibody Titres in Holstein Heifers. Res. Vet. Sci. 2013, 95, 343–346. [Google Scholar] [CrossRef] [PubMed]
- Oliver, S.P.; Gillespie, B.E.; Headrick, S.J.; Lewis, M.J.; Dowlen, H.H. Prevalence, Risk Factors, and Strategies for Controlling Mastitis in Heifers During the Periparturient Period. Int. J. Appl. Res. Vet. Med. 2005, 3, 150–162. [Google Scholar]
- Demil, E.; Teshome, L.; Kerie, Y.; Habtamu, A.; Kumilachew, W.; Andualem, T.; Mekonnen, S.A. Prevalence of Subclinical Mastitis, Associated Risk Factors and Antimicrobial Susceptibility of the Pathogens Isolated from Milk Samples of Dairy Cows in Northwest Ethiopia. Prev. Vet. Med. 2022, 205, 105680. [Google Scholar] [CrossRef]
- Barcelos, M.M.; Martins, L.; Grenfell, R.C.; Juliano, L.; Anderson, K.L.; dos Santos, M.V.; Gonçalves, J.L. Comparison of Standard and On-Plate Extraction Protocols for Identification of Mastitis-Causing Bacteria by MALDI-TOF MS. Braz. J. Microbiol. 2019, 50, 849–857. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Disk and Dilution Susceptiblity Tests for Bacteria Isolated from Animals. In CLSI Supplement VET01S; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018; Available online: https://clsi.org/media/1530/vet01s_sample.pdf (accessed on 19 July 2023).
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-Resistant, Extensively Drug-Resistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef]
- Sweeney, M.T.; Lubbers, B.V.; Schwarz, S.; Watts, J.L. Applying Definitions for Multidrug Resistance, Extensive Drug Resistance and Pandrug Resistance to Clinically Significant Livestock and Companion Animal Bacterial Pathogens—Authors’ Response. J. Antimicrob. Chemother. 2019, 74, 536–537. [Google Scholar] [CrossRef]
- Krumperman, P.H. Multiple Antibiotic Resistance Indexing of Escherichia Coli to Identify High-Risk Sources of Fecal Contamination of Foods. Appl. Environ. Microbiol. 1983, 46, 165–170. [Google Scholar] [CrossRef]
- Stepanović, S.; Vuković, D.; Hola, V.; Di Bonaventura, G.; Djukić, S.; Cirković, I.; Ruzicka, F. Quantification of Biofilm in Microtiter Plates: Overview of Testing Conditions and Practical Recommendations for Assessment of Biofilm Production by Staphylococci. APMIS 2007, 115, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Sawant, A.A.; Gillespie, B.E.; Oliver, S.P. Antimicrobial Susceptibility of Coagulase-Negative Staphylococcus Species Isolated from Bovine Milk. Vet. Microbiol. 2009, 134, 73–81. [Google Scholar] [CrossRef]
- Nakagawa, S.; Taneike, I.; Mimura, D.; Iwakura, N.; Nakayama, T.; Emura, T.; Kitatsuji, M.; Fujimoto, A.; Yamamoto, T. Gene Sequences and Specific Detection for Panton-Valentine Leukocidin. Biochem. Biophys. Res. Commun. 2005, 328, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Paterson, G.K.; Larsen, A.R.; Robb, A.; Edwards, G.E.; Pennycott, T.W.; Foster, G.; Mot, D.; Hermans, K.; Baert, K.; Peacock, S.J.; et al. The Newly Described MecA Homologue, MecALGA251, Is Present in Methicillin-Resistant Staphylococcus Aureus Isolates from a Diverse Range of Host Species. J. Antimicrob. Chemother. 2012, 67, 2809–2813. [Google Scholar] [CrossRef] [PubMed]
- Martineau, F.; Ois Picard, F.J.; Lansac, N.; Mé Nard, C.; Roy, P.H.; Ouellette, M.; Bergeron, M.G. Correlation between the Resistance Genotype Determined by Multiplex PCR Assays and the Antibiotic Susceptibility Patterns of Staphylococcus aureus and Staphylococcus epidermidis. Antimicrob. Agents Chemother. 2000, 44, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Truong-Bolduc, Q.C.; Zhang, X.; Hooper, D.C. Characterization of NorR Protein, a Multifunctional Regulator of NorA Expression in Staphylococcus Aureus. J. Bacteriol. 2003, 185, 3127–3138. [Google Scholar] [CrossRef]
- Truong-Bolduc, Q.C.; Dunman, P.M.; Strahilevitz, J.; Projan, S.J.; Hooper, D.C. MgrA Is a Multiple Regulator of Two New Efflux Pumps in Staphylococcus Aureus. J. Bacteriol. 2005, 187, 2395–2405. [Google Scholar] [CrossRef]
- Truong-Bolduc, Q.C.; Bolduc, G.R.; Medeiros, H.; Vyas, J.M.; Wang, Y.; Hooper, D.C. Role of the Tet38 Efflux Pump in Staphylococcus Aureus Internalization and Survival in Epithelial Cells. Infect. Immun. 2015, 83, 4362–4372. [Google Scholar] [CrossRef]
- Cucarella, C.; Solano, C.; Valle, J.; Amorena, B.; Lasa, I.; Penadés, J.R. Bap, a Staphylococcus Aureus Surface Protein Involved in Biofilm Formation. J. Bacteriol. 2001, 183, 2888–2896. [Google Scholar] [CrossRef]
- Vasudevan, P.; Nair, M.K.M.; Annamalai, T.; Venkitanarayanan, K.S. Phenotypic and Genotypic Characterization of Bovine Mastitis Isolates of Staphylococcus Aureus for Biofilm Formation. Vet. Microbiol. 2003, 92, 179–185. [Google Scholar] [CrossRef]
- McDougal, L.K.; Steward, C.D.; Killgore, G.E.; Chaitram, J.M.; McAllister, S.K.; Tenover, F.C. Pulsed-Field Gel Electrophoresis Typing of Oxacillin-Resistant Staphylococcus Aureus Isolates from the United States: Establishing a National Database. J. Clin. Microbiol. 2003, 41, 5113–5120. [Google Scholar] [CrossRef] [PubMed]
- Souza, R.A.; Pitondo-Silva, A.; Falcão, D.P.; Falcão, J.P. Evaluation of Four Molecular Typing Methodologies as Tools for Determining Taxonomy Relations and for Identifying Species among Yersinia Isolates. J. Microbiol. Methods 2010, 82, 141–150. [Google Scholar] [CrossRef] [PubMed]

| Antibiotic Class | Antibiotic Disks (Concentration) | S. aureus Isolates (n = 191) | |
|---|---|---|---|
| Res 1 | RF (%) 2 | ||
| Beta-lactam | Cefoxitin (30 µg) | 5 | 2.62 |
| Penicillin (10 µg) | 177 | 92.70 | |
| Penicillin/Novobiocin (40 µg) | 2 | 1.05 | |
| Ceftiofur (30 µg) | 2 | 1.05 | |
| Macrolide | Erythromycin (15 µg) | 12 | 6.30 |
| Tetracycline | Tetracycline (30 µg) | 19 | 9.95 |
| Sulfonamide | Trimethoprim/Sulfamethoxazole (25 μg) | 2 | 1.05 |
| Aminoglycoside | Gentamicin (10 μg) | 7 | 3.7 |
| Nitrofuran | Nitrofurantoin (300 µg) | 0 | 0 |
| Fluoroquinolone | Enrofloxacin (5 μg) | 3 | 1.6 |
| Lincosamide | Clindamycin (2 μg) | 10 | 5.23 |
| Fenicol | Chloramphenicol (30 µg) | 2 | 1.05 |
| Id. 1 | No. of Ab 2 | No. of Isolates | Resistance Profile 3 | Resistance to Ab Group | MAR Index |
|---|---|---|---|---|---|
| 1 | 2 | 1 | PEN, PNV | 1 | 0.2 |
| 2 | 2 | 8 | PEN, TET | 2 | 0.2 |
| 3 | 2 | 2 | PEN, ERY | 2 | 0.2 |
| 4 | 2 | 1 | PEN, GEN | 2 | 0.2 |
| 5 | 2 | 2 | PEN, ENO | 2 | 0.2 |
| 6 | 2 | 1 | ERI, CLI | 2 | 0.2 |
| 7 | 3 | 1 | PEN, TET, ENO | 3 | 0.25 |
| 8 | 3 | 1 | PEN, TET, CLO | 3 | 0.25 |
| 9 | 3 | 3 | PEN, ERY, CLI | 3 | 0.25 |
| 10 | 4 | 1 | PEN, ERY, CLI, GEN | 4 | 0.3 |
| 11 | 4 | 1 | PEN, ERY, CLI, TSU | 4 | 0.3 |
| 12 | 4 | 1 | PEN, ERY, CLI, TET | 4 | 0.3 |
| 13 | 4 | 1 | PEN, CFO, CFT, GEN, TSU | 3 | 0.3 |
| 14 | 5 | 1 | PEN, ERY, CLI, TET, GEN | 5 | 0.4 |
| 15 | 5 | 1 | PEN, CFO, ERY, CLI, TET | 4 | 0.4 |
| 16 | 5 | 1 | PEN, PNV, CFO, ERY, CLI | 3 | 0.4 |
| 17 | 6 | 1 | PEN, CFO, ERY, CLI, TET, GEN | 5 | 0.5 |
| 18 | 7 | 1 | PEN, CFO, CFT, ERY, CLI, TET, GEN | 5 | 0.6 |
| Farm | ID | Source | Lactation | Phenotypic Resistance * | Βeta-Lactam Resistance Genes | Efflux Pump Genes | Biofilm Production Genes | Biofilm Formation on Polystyrene (570 nm) | PFGE Cluster |
|---|---|---|---|---|---|---|---|---|---|
| F1 | 1 | Milk | 1 | PEN, CFO, CFT, GEN, TSU | - | - | - | Moderate | - |
| F3 | 2 | Milk | 1 | PEN, ERY, CLI | - | - | icaA, icaD | Weak | 2 |
| F3 | 3 | Milk | 3 | PEN, ERY, CLI | blaZ | norA | icaA, icaD | Weak | 2 |
| F3 | 4 | Milk | 2 | PEN, ERY, CLI | - | norA | icaD | Weak | non-genotypeable |
| F4 | 5 | Milk | 1 | PEN, TET, ENO | - | - | icaD, bap | Moderate | 2 |
| F4 | 6 | Milk | 2 | PEN, CFO, ERY, CLI, TET, GEN | blaZ | - | icaA, icaD, bap | Moderate | 1 |
| F4 | 7 | Milk | 2 | PEN, ERY, CLI, GEN | - | - | icaA, icaD, bap | Moderate | 1 |
| F4 | 8 | Milk | 4 | PEN, CFO, ERY, CLI, TET | blaZ | norA | icaA, icaD | Moderate | 2 |
| F4 | 9 | Milk | 4 | PEN, TET, CLO | blaZ | norA, norC, tet38 | - | Strong | 1 |
| F4 | 10 | Milk | 2 | PEN, CFO, CFT, ERI, CLI, TET, GEN | blaZ | - | icaD | Moderate | 1 |
| F4 | 11 | Milking utensil | N/A | PEN, ERY, CLI, TET | blaZ | norA | icaA, icaD | Moderate | 2 |
| F4 | 12 | Bulk tank milk | N/A | PEN, ERY, CLI, TET, GEN | - | norA | icaD | Moderate | 2 |
| F5 | 13 | Milk | 2 | PEN, PNV, CFO, ERY, CLI | blaZ | norA | icaD, bap | Weak | - |
| F5 | 14 | Milk | 1 | PEN, ERY, CLI, TSU | - | - | icaD | Weak | - |
| Gene | Primer | Sequence (5′–3′) | Amplicon Size (bp) | Reference |
|---|---|---|---|---|
| blaZ | blaZ-F blaZ-R | AAG AGA TTT GCC TAT GCT TC GGC AAT ATG ATC AAG ATA C | 517 | [54] |
| mecA | mecA-F mecA-R | TGG TAT GTG GAA GTT AGA TTG GGA T CTA ATC TCA TAT GTG TTC CTG TAT TGG C | 155 | [55] |
| mecC | mecC-F mecC-R | CAT TAA AAT CAG AGC GAG GC TGG CTG AAC CCA TTT TTG AT | 188 | [56] |
| msrA | msrA-F msrA-R | TCC AAT CAT TGC ACA AAA TC AAT TCC CTC TAT TTG GTG GT | 890 | [57] |
| norA | norA-F norA-R | TGC AAT TTC ATA TGA TCA ATC CC AGATTGCAATTCATGCTAAATATT | 150 | [58] |
| norC | norC-F norC-R | ATA AAT ACC TGA AGC AAC GCC AAC AAA TGG TTC TAA GCG ACC AA | 200 | [59] |
| tet38 | tet38-F tet38-R | TTC AGT TTG GTT ATA GAC AA CGT AGA AAT AAA TCC ACC TG | 200 | [60] |
| bap | bap-F bap-R | CCC TAT ATC GAA GGT GTA GAA TTG GCT GTT GAA GTT AAT ACT GTA CCT GC | 97 | [61] |
| icaA | icaA-F icaA-R | CCT AAC TAA CGA AGG TAG AAG ATA TAG CGA TAA GTG C | 1315 | [62] |
| icaD | icaD-F icaD-R | AAA CGT AAG AGA GGT GG GGC AAT ATG ATC AAG ATA C | 381 | [62] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva, A.T.F.; Gonçalves, J.L.; Dantas, S.T.A.; Rall, V.L.M.; de Oliveira, P.R.F.; dos Santos, M.V.; Peixoto, R.d.M.; Mota, R.A. Genetic and Phenotypic Characterization of Subclinical Mastitis-Causing Multidrug-Resistant Staphylococcus aureus. Antibiotics 2023, 12, 1353. https://doi.org/10.3390/antibiotics12091353
Silva ATF, Gonçalves JL, Dantas STA, Rall VLM, de Oliveira PRF, dos Santos MV, Peixoto RdM, Mota RA. Genetic and Phenotypic Characterization of Subclinical Mastitis-Causing Multidrug-Resistant Staphylococcus aureus. Antibiotics. 2023; 12(9):1353. https://doi.org/10.3390/antibiotics12091353
Chicago/Turabian StyleSilva, Amanda Thaís Ferreira, Juliano Leonel Gonçalves, Stéfani Thais Alves Dantas, Vera Lúcia Mores Rall, Pollyanne Raysa Fernandes de Oliveira, Marcos Veiga dos Santos, Rodolfo de Moraes Peixoto, and Rinaldo Aparecido Mota. 2023. "Genetic and Phenotypic Characterization of Subclinical Mastitis-Causing Multidrug-Resistant Staphylococcus aureus" Antibiotics 12, no. 9: 1353. https://doi.org/10.3390/antibiotics12091353
APA StyleSilva, A. T. F., Gonçalves, J. L., Dantas, S. T. A., Rall, V. L. M., de Oliveira, P. R. F., dos Santos, M. V., Peixoto, R. d. M., & Mota, R. A. (2023). Genetic and Phenotypic Characterization of Subclinical Mastitis-Causing Multidrug-Resistant Staphylococcus aureus. Antibiotics, 12(9), 1353. https://doi.org/10.3390/antibiotics12091353








