Appropriateness of Empirical Prescriptions of Ceftriaxone and Identification of Opportunities for Stewardship Interventions: A Single-Centre Cross-Sectional Study
Abstract
1. Introduction
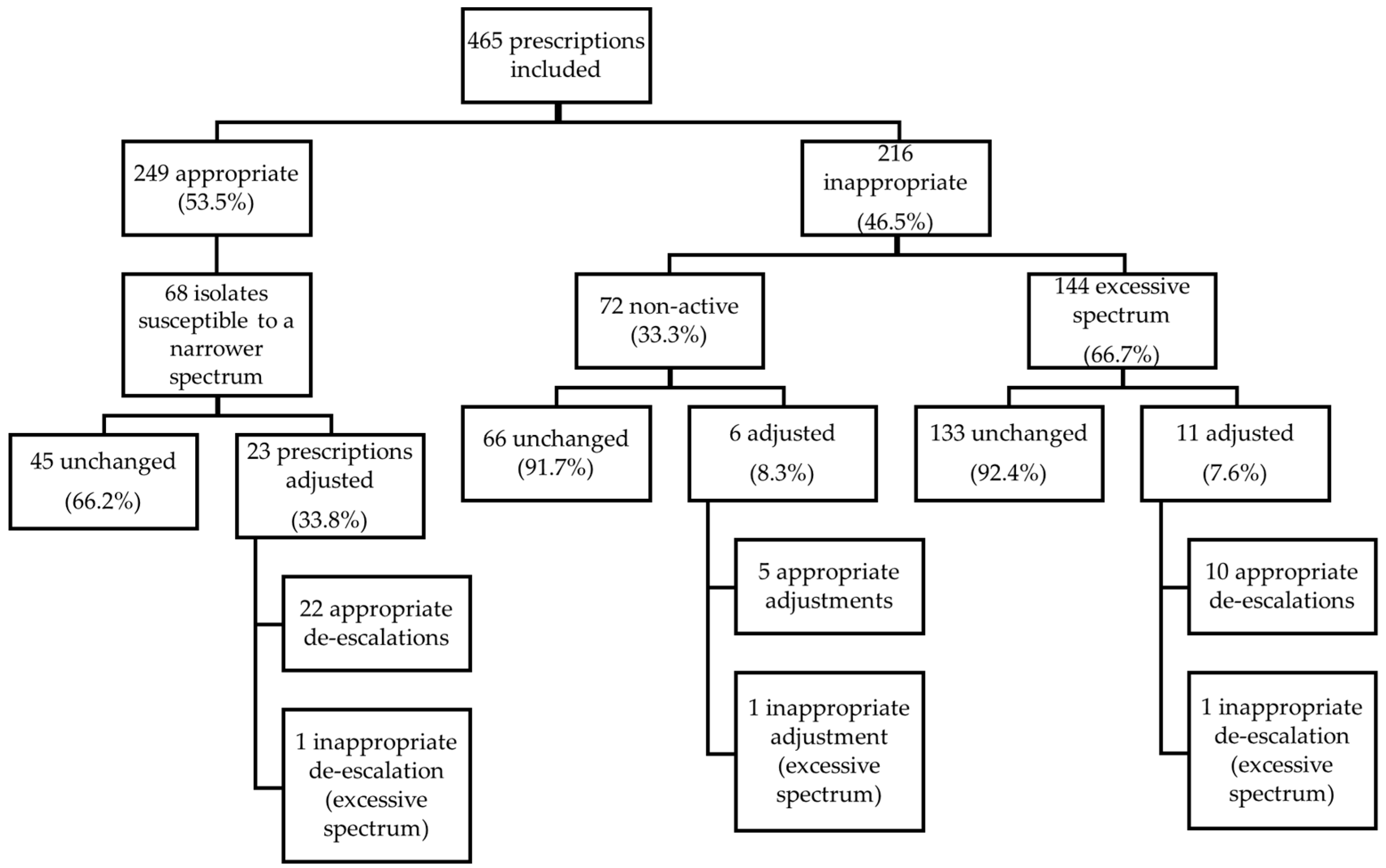
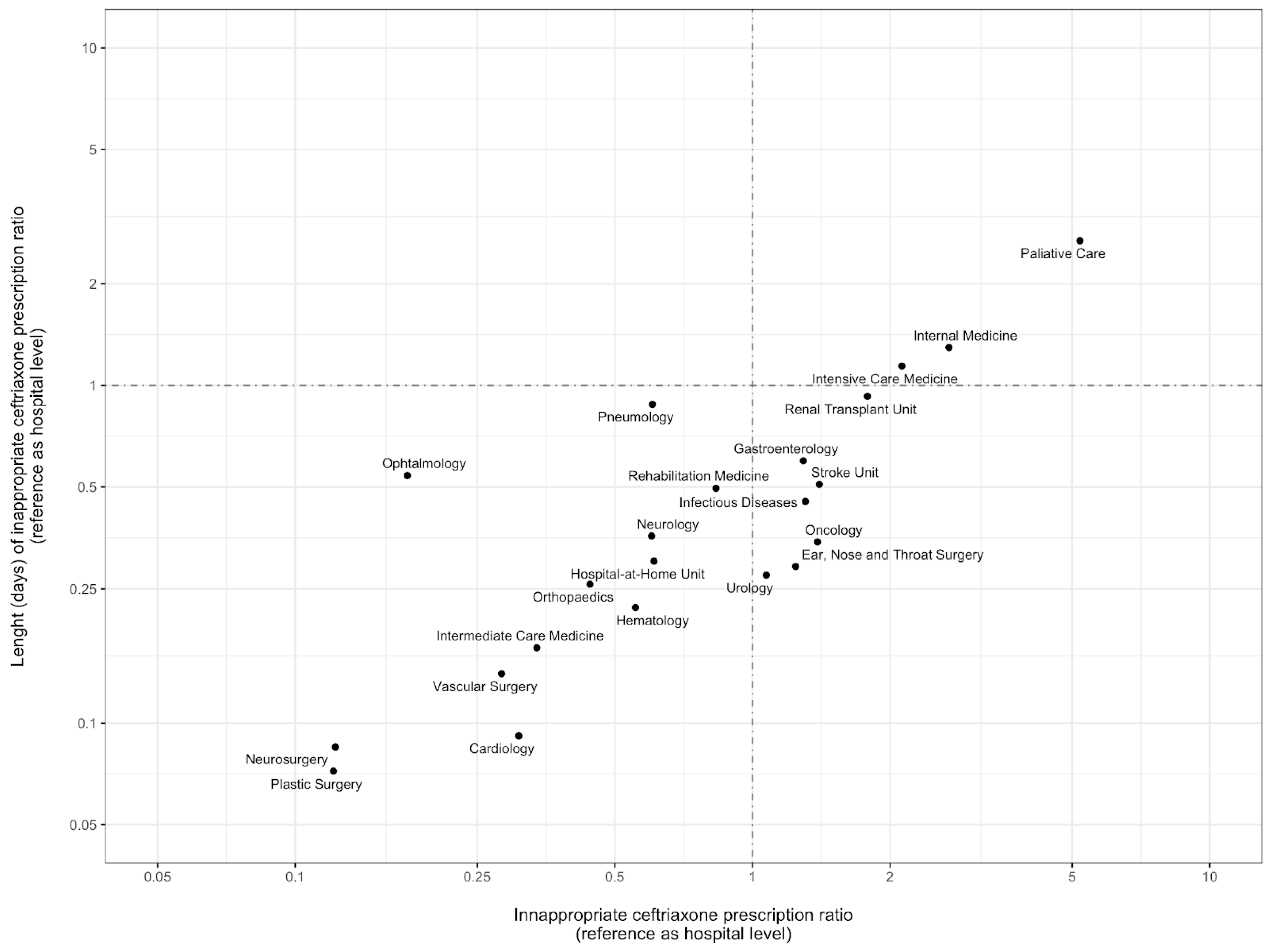
2. Results
3. Discussion
4. Materials and Methods
4.1. Setting and Design
4.2. Inclusion and Exclusion Criteria
4.3. Data Collection
4.4. Outcomes
4.5. Definitions
4.5.1. Empirical Ceftriaxone Prescription Appropriateness
4.5.2. Appropriate Suspension/De-Escalation of Ceftriaxone
4.5.3. Days of Inappropriate Ceftriaxone
4.6. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- European Centre for Disease Prevention and Control (ECDC). Antimicrobial Consumption in the EU/EEA (ESAC-Net). An-nual Epidemiological Report 2021. Published 2021. Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-consumption-europe-2021 (accessed on 27 November 2022).
- Cornaglia, G. Cephalosporins: A microbiological update. Clin. Microbiol. Infect. 2000, 6, 41–45. [Google Scholar] [CrossRef]
- Gomi, H.; Solomkin, J.; Schlossberg, D.; Okamoto, K.; Takada, T.; Strasberg, S.M.; Ukai, T.; Endo, I.; Iwashita, Y.; Hibi, T.; et al. Tokyo Guidelines 2018: Antimicrobial therapy for acute cholangitis and cholecystitis. J. Hepato-Biliary-Pancreatic Sci. 2018, 25, 3–16. [Google Scholar] [CrossRef]
- Bonkat, G.; Bartoletii, R.; Bruyère, F.; Cai, T.; Geerlings, S.E.; Kranz, J.; Koves, B.; Pilatz, A.; Schubert, S.; Veeratterapillay, R.; et al. EAU Guidelines on Urological Infections. Available online: https://uroweb.org/guidelines/urological-infections (accessed on 25 October 2022).
- van de Beek, D.; Cabellos, C.; Dzupova, O.; Esposito, S.; Klein, M.; Kloek, A.; Leib, S.; Mourvillier, B.; Ostergaard, C.; Pagliano, P.; et al. ESCMID guideline: Diagnosis and treatment of acute bacterial meningitis. Clin. Microbiol. Infect. 2016, 22, S37–S62. [Google Scholar] [CrossRef]
- Cyr, S.S.; Barbee, L.; Workowski, K.A.; Bachmann, L.H.; Pham, C.; Schlanger, K.; Torrone, E.; Weinstock, H.; Kersh, E.N.; Thorpe, P. Update to CDC’s Treatment Guidelines for Gonococcal Infection, 2020. MMWR. Morb. Mortal. Wkly. Rep. 2020, 69, 1911–1916. [Google Scholar] [CrossRef]
- Bratzler, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical Practice Guidelines for Antimicrobial Prophylaxis in Surgery. Surg. Infect. 2013, 14, 73–156. [Google Scholar] [CrossRef]
- Metlay, J.P.; Waterer, G.W.; Long, A.C.; Anzueto, A.; Brozek, J.; Crothers, K.; Cooley, L.A.; Dean, N.C.; Fine, M.J.; Flanders, S.A.; et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the american thoracic society and infectious diseases society of America. Am. J. Respir. Crit. Care Med. 2019, 200, e45–e67. [Google Scholar] [CrossRef]
- Tacconelli, E.; Gorska, A.; De Angelis, G.; Lammens, C.; Restuccia, G.; Schrenzel, J.; Huson, D.; Carević, B.; Preoţescu, L.; Carmeli, Y.; et al. Estimating the association between antibiotic exposure and colonization with extended-spectrum β-lactamase-producing Gram-negative bacteria using machine learning methods: A multicentre, prospective cohort study. Clin. Microbiol. Infect. 2020, 26, 87–94. [Google Scholar] [CrossRef]
- Batard, E.; Ollivier, F.; Boutoille, D.; Hardouin, J.-B.; Montassier, E.; Caillon, J.; Ballereau, F. Relationship between hospital antibiotic use and quinolone resistance in Escherichia coli. Int. J. Infect. Dis. 2013, 17, e254–e258. [Google Scholar] [CrossRef]
- Slimings, C.; Riley, T.V. Antibiotics and hospital-acquired Clostridium difficile infection: Update of systematic review and meta-analysis. J. Antimicrob. Chemother. 2013, 69, 881–891. [Google Scholar] [CrossRef]
- Vernaz, N.; Huttner, B.; Muscionico, D.; Salomon, J.-L.; Bonnabry, P.; López-Lozano, J.M.; Beyaert, A.; Schrenzel, J.; Harbarth, S. Modelling the impact of antibiotic use on antibiotic-resistant Escherichia coli using population-based data from a large hospital and its surrounding community. J. Antimicrob. Chemother. 2011, 66, 928–935. [Google Scholar] [CrossRef]
- Wilcox, M.H.; Chalmers, J.D.; Nord, C.E.; Freeman, J.; Bouza, E. Role of cephalosporins in the era of Clostridium difficile infection. J. Antimicrob. Chemother. 2016, 72, 1–18. [Google Scholar] [CrossRef]
- Rodríguez-Baño, J.; Navarro, M.D.; Romero, L.; Muniain, M.A.; de Cueto, M.; Gálvez-Acebal, J.; Perea, E.J.; Pascual, A. Risk-factors for emerging bloodstream infections caused by extended-spectrum β-lactamase-producing Escherichia coli. Clin. Microbiol. Infect. 2008, 14, 180–183. [Google Scholar] [CrossRef]
- WHO. 2021 AWaRe Classification—WHO Access, Watch, Reserve, Classification of Antibiotics for Evaluation and Monitoring of Use. Available online: https://www.who.int/publications/i/item/2021-aware-classification (accessed on 27 November 2022).
- Bantar, C.; Vesco, E.; Heft, C.; Salamone, F.; Krayeski, M.; Gomez, H.; Coassolo, M.A.; Fiorillo, A.; Franco, D.; Arango, C.; et al. Replacement of Broad-Spectrum Cephalosporins by Piperacillin-Tazobactam: Impact on Sustained High Rates of Bacterial Resistance. Antimicrob. Agents Chemother. 2004, 48, 392–395. [Google Scholar] [CrossRef]
- Petrikkos, G.; Markogiannakis, A.; Papapareskevas, J.; Daikos, G.L.; Stefanakos, G.; Zissis, N.P.; Avlamis, A. Differences in the changes in resistance patterns to third- and fourth-generation cephalosporins and piperacillin/tazobactam among Klebsiella pneumoniae and Escherichia coli clinical isolates following a restriction policy in a Greek tertiary care hospital. Int. J. Antimicrob. Agents 2007, 29, 34–38. [Google Scholar] [CrossRef]
- Dancer, S.; Kirkpatrick, P.; Corcoran, D.; Christison, F.; Farmer, D.; Robertson, C. Approaching zero: Temporal effects of a restrictive antibiotic policy on hospital-acquired Clostridium difficile, extended-spectrum β-lactamase-producing coliforms and meticillin-resistant Staphylococcus aureus. Int. J. Antimicrob. Agents 2013, 41, 137–142. [Google Scholar] [CrossRef]
- Peñalva, G.; Högberg, L.D.; Weist, K.; Vlahović-Palčevski, V.; Heuer, O.; Monnet, D.L.; ESAC-Net Study Group. Decreasing and stabilising trends of antimicrobial consumption and resistance in Escherichia coli and Klebsiella pneumoniae in segmented regression analysis, European Union/European Economic Area, 2001 to 2018. Eurosurveillance 2019, 24, 1900656. [Google Scholar] [CrossRef]
- Goulet, H.; Daneluzzi, V.; Dupont, C.; Heym, B.; Page, B.; Almeida, K.; Auvert, B.; Elkharrat, D.; Rouveix, E. Évaluation de la qualité des prescriptions d’antibiotiques dans le service d’accueil des urgences d’un CHU en région parisienne. Med. Mal. Infect. 2009, 39, 48–54. [Google Scholar] [CrossRef]
- Roger, P.M.; Martin, C.; Taurel, M.; Fournier, J.P.; Nicole, I.; Carles, M.; Mondain, V.; Fontas, E.; Bertrand, F.; Pradier, C.; et al. Motives for the prescription of antibiotics in the emergency department of the Universi-ty Hospital Center in Nice. A prospective study. Presse Med. 2002, 31, 58–63. [Google Scholar]
- Tan, B.K.; Vivier, E.; Bouziad, K.A.; Zahar, J.-R.; Pommier, C.; Parmeland, L.; Pariset, C.; Misslin, P.; Haond, C.; Poirié, P.; et al. A hospital-wide intervention replacing ceftriaxone with cefotaxime to reduce rate of healthcare-associated infections caused by extended-spectrum β-lactamase-producing Enterobacteriaceae in the intensive care unit. Intensiv. Care Med. 2018, 44, 672–673. [Google Scholar] [CrossRef]
- Batard, E.; Javaudin, F.; Kervagoret, E.; Caruana, E.; Le Bastard, Q.; Chapelet, G.; Goffinet, N.; Montassier, E. Are third-generation cephalosporins associated with a better prognosis than amoxicillin–clavulanate in patients hospitalized in the medical ward for community-onset pneumonia? Clin. Microbiol. Infect. 2018, 24, 1171–1176. [Google Scholar] [CrossRef]
- Melo-Cristino, J.; Santos, L.; Silva-Costa, C.; Friães, A.; Pinho, M.D.; Ramirez, M. The Viriato Study Update on Antimicrobial Re-sistance of Microbial Pathogens Responsible for Community-Acquired Respiratory Tract Infections in Portugal. Pediatr. Drugs 2010, 12, 11–17. [Google Scholar] [CrossRef]
- Hecker, M.T.; Fox, C.J.; Son, A.H.; Cydulka, R.K.; Siff, J.E.; Emerman, C.L.; Sethi, A.K.; Muganda, C.P.; Donskey, C.J. Effect of a Stewardship Intervention on Adherence to Uncomplicated Cystitis and Pyelonephritis Guidelines in an Emergency Department Setting. PLoS ONE 2014, 9, e87899. [Google Scholar] [CrossRef]
- Girotti, M.; Fodoruk, S.; Irvine-Meek, J.; Rotstein, O. Antibiotic handbook and pre-printed perioperative order forms for surgical antibiotic prophylaxis: Do they work? Can. J. Surg. 1990, 33, 385–388. [Google Scholar]
- Van De Beek, D.; De Gans, J.; Spanjaard, L.; Vermeulen, M.; Dankert, J. Antibiotic guidelines and antibiotic use in adult bacterial meningitis in The Netherlands. J. Antimicrob. Chemother. 2002, 49, 661–666. [Google Scholar] [CrossRef]
- Direção-Geral da Saúde. NORMA CLÍNICA: 031/2013 de 31/12/2013 Atualizada a 17/11/2022: Profilaxia Antibiótica Cirúrgica Na Criança e No Adulto. 2022. Available online: https://www.dgs.pt/normas-orientacoes-e-informacoes/normas-e-circulares-normativas/0312013-de-31122013-atualizada-a-17112022-pdf.aspx (accessed on 19 December 2022).
- Zhang, C.D.; Zeng, Y.J.; Li, Z.; Chen, J.; Li, H.W.; Zhang, J.K.; Dai, D.Q. Extended antimicrobial prophylaxis after gastric cancer surgery: A systematic review and meta-analysis. World J. Gastroenterol. 2013, 19, 2104–2109. [Google Scholar] [CrossRef]
- Albrecht, J.S.; McGregor, J.C.; Fromme, E.K.; Bearden, D.T.; Furuno, J.P. A Nationwide Analysis of Antibiotic Use in Hospice Care in the Final Week of Life. J. Pain Symptom Manag. 2013, 46, 483–490. [Google Scholar] [CrossRef]
- De Bus, L.; Depuydt, P.; Steen, J.; Dhaese, S.; De Smet, K.; Tabah, A.; Akova, M.; Cotta, M.O.; De Pascale, G.; Dimopoulos, G.; et al. Antimicrobial de-escalation in the critically ill patient and assessment of clinical cure: The DIANA study. Intensiv. Care Med. 2020, 46, 1404–1417. [Google Scholar] [CrossRef]
- Pauwels, I.; Versporten, A.; Drapier, N.; Vlieghe, E.; Goossens, H.; Koraqi, A.; Hoxha, I.; Tafaj, S.; Cornistein, W.; Quiros, R.; et al. Hospital antibiotic prescribing patterns in adult patients according to the WHO Access, Watch and Reserve classification (AWaRe): Results from a worldwide point prevalence survey in 69 countries. J. Antimicrob. Chemother. 2021, 76, 1614–1624. [Google Scholar] [CrossRef]
| All Prescriptions n = 465 | |
|---|---|
| Male sex—n (%) | 249 (53.5) |
| Age, years—mean (SD) | 69.7 (17.7) |
| Long-term care facility residency—n (%) | 28 (6.0) |
| Transfer from another hospital—n (%) | 43 (9.2) |
| Known antibiotic allergy—n (%) | 18 (3.9) |
| Hospitalisation in the previous 3 months—n (%) | 63 (13.6) |
| Antibiotic therapy in the previous 3 months—n (%) | 70 (15.1) |
| Presence of sepsis—n (%) | 124 (26.7) |
| Intensive care admission—n (%) | 58 (12.5) |
| Isolated pathogens in the previous 3 months—n (%) | 29 (6.2) |
| Colonisation by MDRO—n (%) | 9 (1.9) |
| Appropriate Prescription n = 249 | Inappropriate Prescription n = 216 | p Value | |
|---|---|---|---|
| Sex—n (%) Male | |||
| 130 (52.2) | 119 (55.1) | 0.597 | |
| Age (mean ± SD), y | 66.5 (18.1) | 73.4 (16.5) | <0.001 |
| Long-term care facility residency—n (%) | 10 (4.0) | 18 (8.3) | 0.079 |
| Transfer from another hospital—n (%) | 25 (10.0) | 18 (8.3) | 0.636 |
| Hospitalisation department during the treatment—n (%) | |||
| Medical | 85 (34.1) | 131 (60.6) | Ref. |
| Surgical | 146 (58.6) | 58 (26.9) | <0.001 |
| Intensive Care | 18 (7.3) | 27 (12.5) | 0.931 |
| Known antibiotic allergy—n (%) | 14 (5.6) | 4 (1.8) | 0.063 |
| Intensive care admission—n (%) | 28 (11.2) | 30 (13.9) | 0.394 |
| Presence of sepsis—n (%) | 77 (30.9) | 47 (21.8) | 0.034 |
| Previous antibiotic therapy—n (%) | 36 (14.5) | 34 (15.7) | 0.798 |
| Hospitalisation in the last 3 months—n (%) | 43 (17.3) | 20 (9.3) | 0.017 |
| Colonisation by MDRO—n (%) | 3 (1.2) | 6 (2.8) | 0.314 |
| Defined hospital guideline—n (%) | 180 (72.3) | 150 (69.4) | 0.424 |
| Previously isolated pathogens—n (%) | 13 (5.2) | 16 (7.4) | 0.435 |
| Microbiological sampling—n (%) | 195 (78.3) | 160 (74.1) | 0.335 |
| Day of antibiotic initiation—n (%) | |||
| Weekday | 167 (67.1) | 164 (75.9) | Ref. |
| Weekend | 82 (32.9) | 52 (24.1) | 0.036 |
| Setting of empirical antibiotic prescription—n (%) | |||
| ED | 143 (57.4) | 83 (38.4) | Ref. |
| Ward | 96 (38.6) | 105 (48.6) | 0.001 |
| ICU | 8 (3.2) | 19 (8.8) | 0.001 |
| OR | 2 (0.8) | 9 (4.2) | 0.004 |
| Aim of antibiotic prescription—n (%) | |||
| Treatment | 249 (100) | 181 (83.8) | Ref. |
| Prophylaxis | 0 (0.0) | 35 (16.2) | <0.001 |
| Ceftriaxone duration (mean ± SD), days | 5.1 (3.6) | 4.4 (4.2) | 0.002 |
| Hospital Protocol | Appropriate Prescription N = 180 | Inappropriate Prescription N= 150 |
|---|---|---|
| Intra-abdominal and biliary infections—n (%) | 48 (100) | 0 (0) |
| LRTI—n (%) | 4 (4.3) | 90 (95.7) |
| UTI—n (%) | 119 (72.1) | 46 (27.9) |
| Osteoarticular infection—n (%) | 6 (85.7) | 1 (14.3) |
| CNS infection—n (%) | 3 (100) | 0 (0) |
| Surgical prophylaxis—n (%) | 0 (0) | 13 (100) |
| Hospitalisation Department | Infectious Syndrome | Appropriate Prescription n (%) | Inappropriate Prescription n (%) |
|---|---|---|---|
| Medical (n = 215) | Abdominal | 10 (100) | 0 (0) |
| Biliary | 1 (100) | 0 (0) | |
| Lower respiratory | 3 (4.3) | 66 (95.7) | |
| Urinary | 55 (59.8) | 37 (40.2) | |
| Central nervous system | 4 (100) | 0 (0) | |
| Osteoarticular | 1 (100) | 0 (0) | |
| Skin and soft tissue | 5 (83.3) | 1 (16.7) | |
| Other | 6 (18.8) | 26 (81.2) | |
| Surgical (n = 170) | Abdominal | 29 (96.7) | 1 (3.3) |
| Biliary | 28 (100) | 0 (0) | |
| Lower respiratory | 1 (14.3) | 6 (85.7) | |
| Urinary | 60 (92.3) | 5 (7.7) | |
| Central nervous system | 1 (100) | 0 (0) | |
| Osteoarticular | 6 (100) | 0 (0) | |
| Skin and soft tissue | 10 (100) | 0 (0) | |
| Other | 11 (47.8) | 12 (52.2) | |
| Intensive Care (n = 45) | Abdominal | 3 (75) | 1 (25) |
| Biliary | 1 (100) | 0 (0) | |
| Lower respiratory | 0 (0) | 18 (100) | |
| Urinary | 8 (61.5) | 5 (38.5) | |
| Central nervous system | 5 (100) | 0 (0) | |
| Osteoarticular | 0 (0) | 1 (100) | |
| Skin and soft tissue | 1 (100) | 0 (0) | |
| Other | 0 (0) | 2 (100) |
| Problem Identified | Potential Stewardship Intervention(s) |
|---|---|
| Inappropriate empirical prescription in lower respiratory and urinary tract infections | Understanding the drivers for excessive spectrum prescription in these syndromes Intensification of feedback regarding local patterns of antimicrobial resistance of the primary pathogens Post-prescription review of ceftriaxone use in the hospital |
| Non-adherence to internal guidelines | Raising awareness for the existence of local guidelines Promoting adherence to local guidelines regarding empirical antibiotic therapy |
| High ratios of inappropriate prescription in palliative care, internal medicine and intensive care departments, regarding both empirical prescription and duration of inappropriate therapy | Identifying drivers for inappropriate empirical prescription in these specific departments Audit and feedback interventions Targeted interventions at the level of these prescribers, such as antimicrobial stewardship ward rounds |
| Ceftriaxone as surgical prophylaxis | Identification of surgical procedures with inappropriate prophylaxis Promoting adherence to local surgical prophylaxis guidelines |
| Missed opportunities for de-escalation | Implementation of electronic alerts for possible narrowing of the antimicrobial spectrum Training of prescribers regarding the importance of frequent re-evaluation of microbiology results and antimicrobial prescription Audit and feedback interventions |
| Lack of microbiological sampling | Assessing potential difficulties to microbiological specimen collection (logistical/infrastructural, lack of training, among others) Training of healthcare workers |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gorgulho, A.; Cunha, F.; Alves Branco, E.; Azevedo, A.; Almeida, F.; Duro, R.; Andrade, P.; Rocha Pereira, N.; Lima Alves, C. Appropriateness of Empirical Prescriptions of Ceftriaxone and Identification of Opportunities for Stewardship Interventions: A Single-Centre Cross-Sectional Study. Antibiotics 2023, 12, 288. https://doi.org/10.3390/antibiotics12020288
Gorgulho A, Cunha F, Alves Branco E, Azevedo A, Almeida F, Duro R, Andrade P, Rocha Pereira N, Lima Alves C. Appropriateness of Empirical Prescriptions of Ceftriaxone and Identification of Opportunities for Stewardship Interventions: A Single-Centre Cross-Sectional Study. Antibiotics. 2023; 12(2):288. https://doi.org/10.3390/antibiotics12020288
Chicago/Turabian StyleGorgulho, Ana, Flávia Cunha, Elsa Alves Branco, Ana Azevedo, Francisco Almeida, Raquel Duro, Paulo Andrade, Nuno Rocha Pereira, and Carlos Lima Alves. 2023. "Appropriateness of Empirical Prescriptions of Ceftriaxone and Identification of Opportunities for Stewardship Interventions: A Single-Centre Cross-Sectional Study" Antibiotics 12, no. 2: 288. https://doi.org/10.3390/antibiotics12020288
APA StyleGorgulho, A., Cunha, F., Alves Branco, E., Azevedo, A., Almeida, F., Duro, R., Andrade, P., Rocha Pereira, N., & Lima Alves, C. (2023). Appropriateness of Empirical Prescriptions of Ceftriaxone and Identification of Opportunities for Stewardship Interventions: A Single-Centre Cross-Sectional Study. Antibiotics, 12(2), 288. https://doi.org/10.3390/antibiotics12020288






