Virulence Factors and Pathogenicity Mechanisms of Acinetobacter baumannii in Respiratory Infectious Diseases
Abstract
:1. Introduction
2. Antibiotic Resistance of A. baumannii
3. Virulence Factors
3.1. Outer Membrane Proteins (Omps)
3.1.1. OmpA
3.1.2. CarO
3.1.3. Omp33
3.1.4. OprD/OccAB1
3.1.5. OmpW
3.2. Lipopolysaccharides (LPS)
3.3. Capsular Polysaccharides (CPS)
3.4. Phospholipase
3.5. Pili and Motility
3.5.1. Type IV Pili
3.5.2. The Chaperone–Usher Pilus System
3.6. Iron Acquisition
3.7. Secretion Systems
3.7.1. T1SS
3.7.2. T2SS
3.7.3. T4SS
3.7.4. T5SS
3.7.5. T6SS
3.8. GigA, GigB, and GigC
3.9. Thioredoxin A (TrxA)
3.10. Polyphosphate Kinase (PPK)
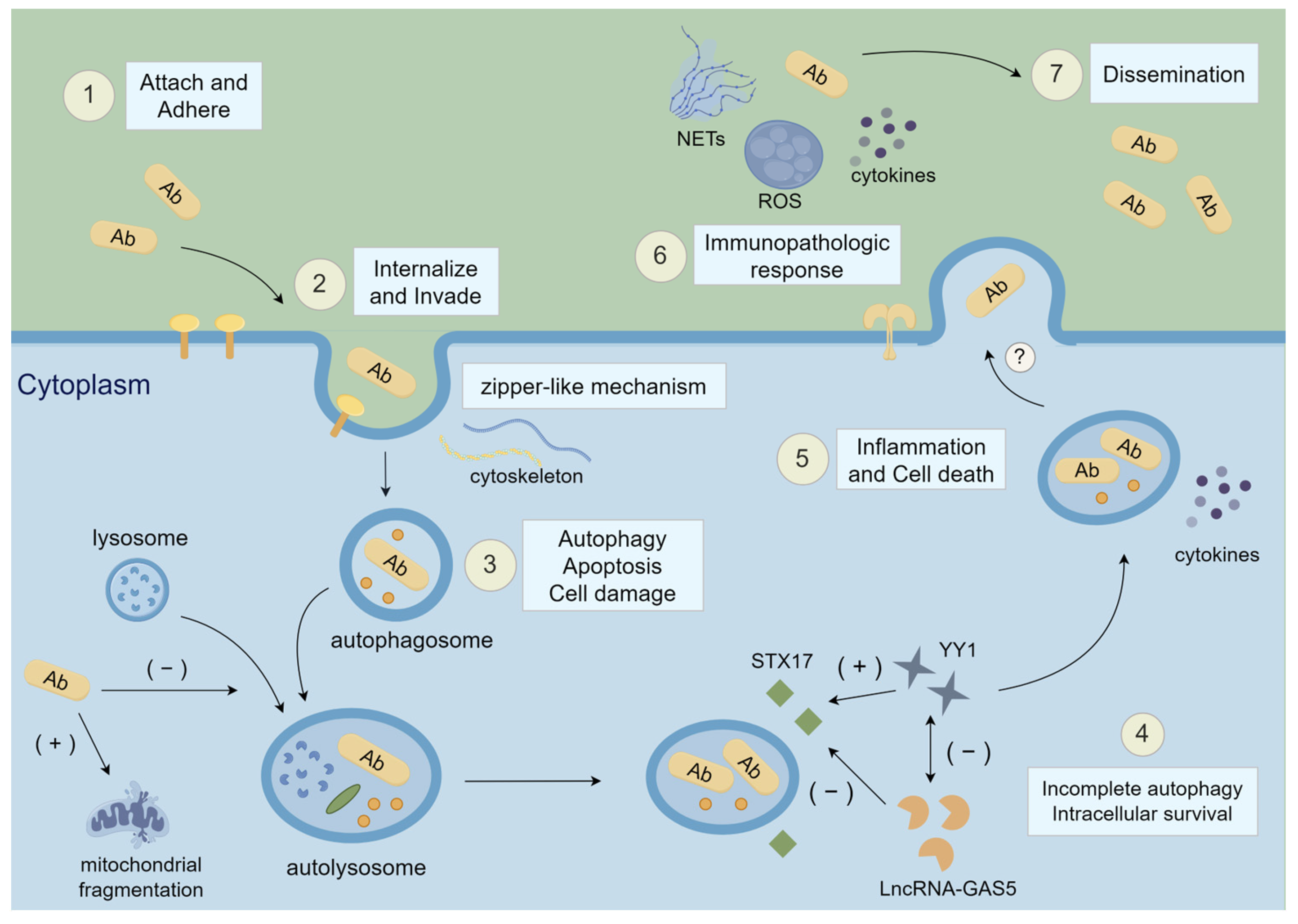
4. Pathogenic Mechanisms in Respiratory Infectious Diseases
4.1. Attach and Adhere
4.1.1. Omps
4.1.2. Protein Secretion Systems
4.1.3. Type IV Pili and CsuA/BABCDE-Mediated Pilus
4.1.4. Biofilm-Associated Protein (Bap), Bap-like Protein (Blp), and PstS
4.2. Internalize and Invade
4.3. Autophagy, Apoptosis, and Cell Damage
4.4. Incomplete Autophagy
4.5. Inflammatory Response and Cell Death
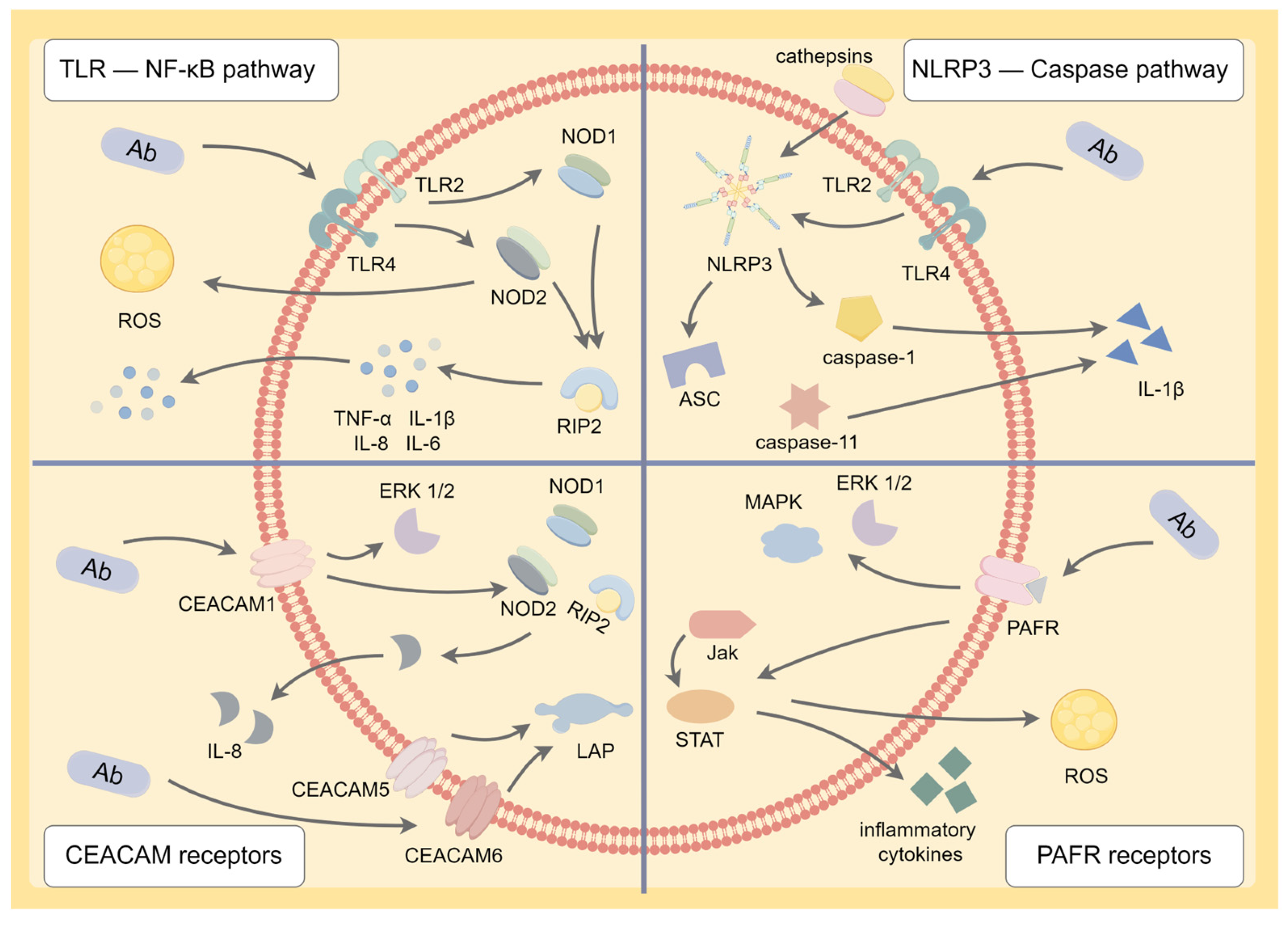
4.5.1. TLR-Nuclear Factor-Kappa B (NF-κB) Signaling Pathway
4.5.2. NLRP3 Inflammasome-Caspase Pathway
4.5.3. CEACAM and PAFR
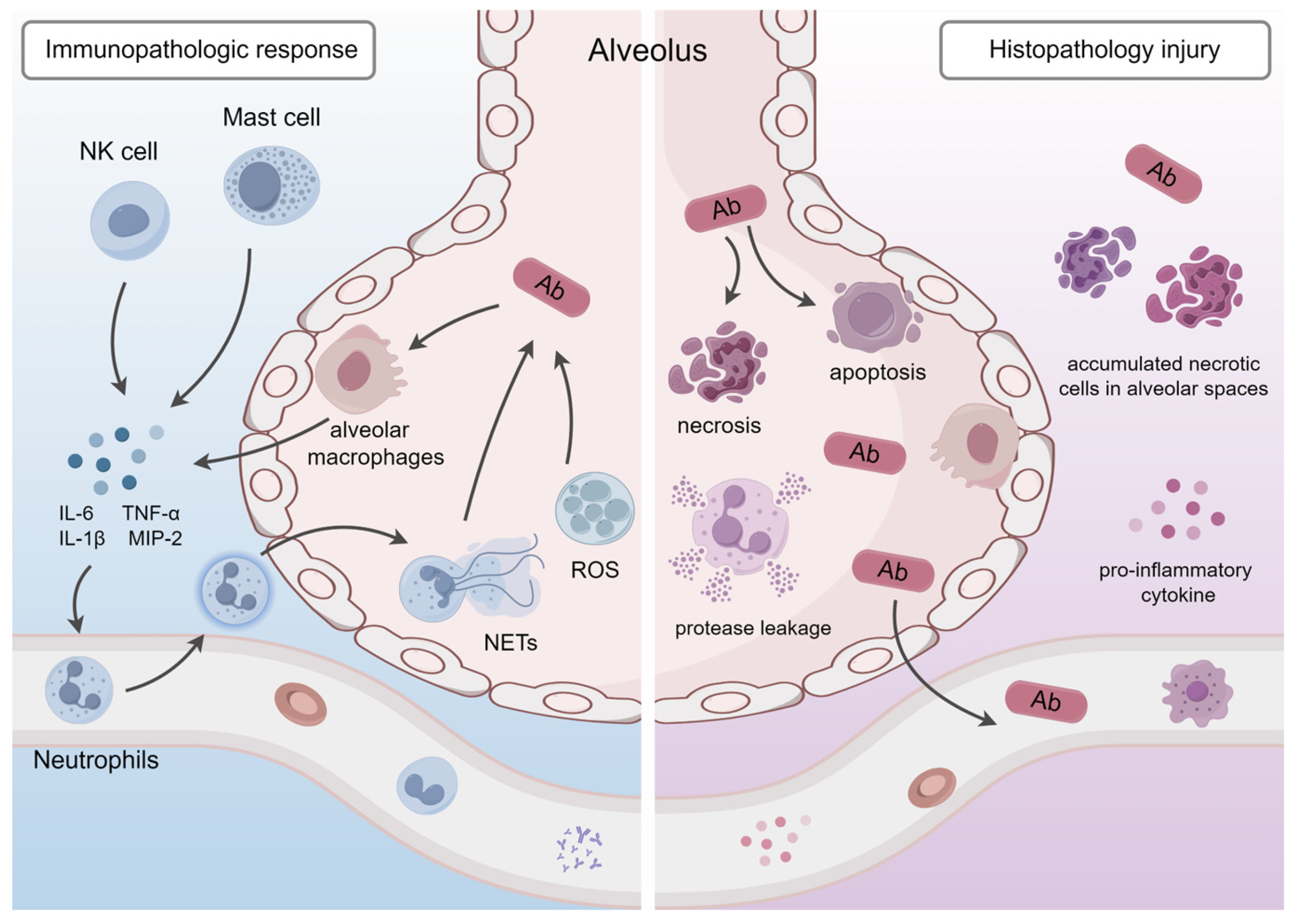
4.6. Immunopathologic Response and Histopathology
4.6.1. Interactions with the Immune System
4.6.2. Histopathological Changes and Lung Injury
4.7. Systemic Dissemination
5. Conclusions and Perspective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sarshar, M.; Behzadi, P.; Scribano, D.; Palamara, A.T.; Ambrosi, C. Acinetobacter baumannii: An Ancient Commensal with Weapons of a Pathogen. Pathogens 2021, 10, 387. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; KuoLee, R.; Harris, G.; Van Rooijen, N.; Patel, G.B.; Chen, W. Role of macrophages in early host resistance to respiratory Acinetobacter baumannii infection. PLoS ONE 2012, 7, e40019. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Zhou, H.; Jiang, Y.; He, J.; Yao, Y.; Wang, J.; Liu, X.; Leptihn, S.; Hua, X.; Yu, Y. Acinetobacter baumannii Outer Membrane Protein A Induces Pulmonary Epithelial Barrier Dysfunction and Bacterial Translocation Through The TLR2/IQGAP1 Axis. Front. Immunol. 2022, 13, 927955. [Google Scholar] [CrossRef] [PubMed]
- Uppalapati, S.R.; Sett, A.; Pathania, R. The Outer Membrane Proteins OmpA, CarO, and OprD of Acinetobacter baumannii Confer a Two-Pronged Defense in Facilitating Its Success as a Potent Human Pathogen. Front. Microbiol. 2020, 11, 589234. [Google Scholar] [CrossRef] [PubMed]
- Rumbo, C.; Tomas, M.; Fernandez Moreira, E.; Soares, N.C.; Carvajal, M.; Santillana, E.; Beceiro, A.; Romero, A.; Bou, G. The Acinetobacter baumannii Omp33-36 porin is a virulence factor that induces apoptosis and modulates autophagy in human cells. Infect. Immun. 2014, 82, 4666–4680. [Google Scholar] [CrossRef] [PubMed]
- Harding, C.M.; Hennon, S.W.; Feldman, M.F. Uncovering the mechanisms of Acinetobacter baumannii virulence. Nat. Rev. Microbiol. 2018, 16, 91–102. [Google Scholar] [CrossRef] [PubMed]
- Towner, K.J. Acinetobacter: An old friend, but a new enemy. J. Hosp. Infect. 2009, 73, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Chai, D.; Wang, R.; Liang, B.; Bai, N. Colistin resistance of Acinetobacter baumannii: Clinical reports, mechanisms and antimicrobial strategies. J. Antimicrob. Chemother. 2012, 67, 1607–1615. [Google Scholar] [CrossRef]
- Al-Kadmy, I.M.S.; Ali, A.N.M.; Salman, I.M.A.; Khazaal, S.S. Molecular characterization of Acinetobacter baumannii isolated from Iraqi hospital environment. New Microbes New Infect. 2018, 21, 51–57. [Google Scholar] [CrossRef]
- Kareem, S.M.; Al-Kadmy, I.M.S.; Al-Kaabi, M.H.; Aziz, S.N.; Ahmad, M. Acinetobacter baumannii virulence is enhanced by the combined presence of virulence factors genes phospholipase C (plcN) and elastase (lasB). Microb. Pathog. 2017, 110, 568–572. [Google Scholar] [CrossRef]
- Giammanco, A.; Cala, C.; Fasciana, T.; Dowzicky, M.J. Global Assessment of the Activity of Tigecycline against Multidrug-Resistant Gram-Negative Pathogens between 2004 and 2014 as Part of the Tigecycline Evaluation and Surveillance Trial. mSphere 2017, 2, e00310-16. [Google Scholar] [CrossRef] [PubMed]
- Rizk, S.S.; Elwakil, W.H.; Attia, A.S. Antibiotic-Resistant Acinetobacter baumannii in Low-Income Countries (2000–2020): Twenty-One Years and Still below the Radar, Is It Not There or Can They Not Afford to Look for It? Antibiotics 2021, 10, 764. [Google Scholar] [CrossRef] [PubMed]
- Ke, X.; Shen, L. Molecular targeted therapy of cancer: The progress and future prospect. Front. Lab. Med. 2017, 1, 69–75. [Google Scholar] [CrossRef]
- Al-Kadmy, I.M.S.; Ibrahim, S.A.; Al-Saryi, N.; Aziz, S.N.; Besinis, A.; Hetta, H.F. Prevalence of Genes Involved in Colistin Resistance in Acinetobacter baumannii: First Report from Iraq. Microb. Drug Resist. 2020, 26, 616–622. [Google Scholar] [CrossRef] [PubMed]
- Hussein, N.H.; Al-Kadmy, I.M.S.; Taha, B.M.; Hussein, J.D. Mobilized colistin resistance (mcr) genes from 1 to 10: A comprehensive review. Mol. Biol. Rep. 2021, 48, 2897–2907. [Google Scholar] [CrossRef] [PubMed]
- Hujer, A.M.; Higgins, P.G.; Rudin, S.D.; Buser, G.L.; Marshall, S.H.; Xanthopoulou, K.; Seifert, H.; Rojas, L.J.; Domitrovic, T.N.; Cassidy, P.M.; et al. Nosocomial Outbreak of Extensively Drug-Resistant Acinetobacter baumannii Isolates Containing bla(OXA-237) Carried on a Plasmid. Antimicrob. Agents Chemother. 2017, 61, e00797-17. [Google Scholar] [CrossRef] [PubMed]
- Morris, F.C.; Dexter, C.; Kostoulias, X.; Uddin, M.I.; Peleg, A.Y. The Mechanisms of Disease Caused by Acinetobacter baumannii. Front. Microbiol. 2019, 10, 1601. [Google Scholar] [CrossRef]
- Mea, H.J.; Yong, P.V.C.; Wong, E.H. An overview of Acinetobacter baumannii pathogenesis: Motility, adherence and biofilm formation. Microbiol. Res. 2021, 247, 126722. [Google Scholar] [CrossRef]
- Gaddy, J.A.; Tomaras, A.P.; Actis, L.A. The Acinetobacter baumannii 19606 OmpA protein plays a role in biofilm formation on abiotic surfaces and in the interaction of this pathogen with eukaryotic cells. Infect. Immun. 2009, 77, 3150–3160. [Google Scholar] [CrossRef]
- Iyer, R.; Moussa, S.H.; Durand-Reville, T.F.; Tommasi, R.; Miller, A. Acinetobacter baumannii OmpA Is a Selective Antibiotic Permeant Porin. ACS Infect. Dis. 2018, 4, 373–381. [Google Scholar] [CrossRef]
- An, Z.; Huang, X.; Zheng, C.; Ding, W. Acinetobacter baumannii outer membrane protein A induces HeLa cell autophagy via MAPK/JNK signaling pathway. Int. J. Med. Microbiol. 2019, 309, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Li, Y.; Peng, C.; Lin, J.; Yu, F.; Zhao, Y.; Zhang, X.; Zhao, D. Outer membrane protein a in Acinetobacter baumannii induces autophagy through mTOR signalling pathways in the lung of SD rats. Biomed. Pharmacother. 2021, 135, 111034. [Google Scholar] [CrossRef] [PubMed]
- Tiku, V.; Kofoed, E.M.; Yan, D.; Kang, J.; Xu, M.; Reichelt, M.; Dikic, I.; Tan, M.W. Outer membrane vesicles containing OmpA induce mitochondrial fragmentation to promote pathogenesis of Acinetobacter baumannii. Sci. Rep. 2021, 11, 618. [Google Scholar] [CrossRef] [PubMed]
- Geisinger, E.; Huo, W.; Hernandez-Bird, J.; Isberg, R.R. Acinetobacter baumannii: Envelope Determinants That Control Drug Resistance, Virulence, and Surface Variability. Annu. Rev. Microbiol. 2019, 73, 481–506. [Google Scholar] [CrossRef] [PubMed]
- Labrador-Herrera, G.; Perez-Pulido, A.J.; Alvarez-Marin, R.; Casimiro-Soriguer, C.S.; Cebrero-Cangueiro, T.; Moran-Barrio, J.; Pachon, J.; Viale, A.M.; Pachon-Ibanez, M.E. Virulence role of the outer membrane protein CarO in carbapenem-resistant Acinetobacter baumannii. Virulence 2020, 11, 1727–1737. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Unno, Y.; Kawakami, S.; Ubagai, T.; Ono, Y. Virulence characteristics of Acinetobacter baumannii clinical isolates vary with the expression levels of omps. J. Med. Microbiol. 2017, 66, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Zahn, M.; Bhamidimarri, S.P.; Basle, A.; Winterhalter, M.; van den Berg, B. Structural Insights into Outer Membrane Permeability of Acinetobacter baumannii. Structure 2016, 24, 221–231. [Google Scholar] [CrossRef]
- Hua, M.; Liu, J.; Du, P.; Liu, X.; Li, M.; Wang, H.; Chen, C.; Xu, X.; Jiang, Y.; Wang, Y.; et al. The novel outer membrane protein from OprD/Occ family is associated with hypervirulence of carbapenem resistant Acinetobacter baumannii ST2/KL22. Virulence 2021, 12, 1–11. [Google Scholar] [CrossRef]
- Catel-Ferreira, M.; Marti, S.; Guillon, L.; Jara, L.; Coadou, G.; Molle, V.; Bouffartigues, E.; Bou, G.; Shalk, I.; Jouenne, T.; et al. The outer membrane porin OmpW of Acinetobacter baumannii is involved in iron uptake and colistin binding. FEBS Lett. 2016, 590, 224–231. [Google Scholar] [CrossRef]
- Gil-Marques, M.L.; Pachon, J.; Smani, Y. iTRAQ-Based Quantitative Proteomic Analysis of Acinetobacter baumannii under Hypoxia and Normoxia Reveals the Role of OmpW as a Virulence Factor. Microbiol. Spectr. 2022, 10, e0232821. [Google Scholar] [CrossRef]
- Rossi, E.; Longo, F.; Barbagallo, M.; Peano, C.; Consolandi, C.; Pietrelli, A.; Jaillon, S.; Garlanda, C.; Landini, P. Glucose availability enhances lipopolysaccharide production and immunogenicity in the opportunistic pathogen Acinetobacter baumannii. Future Microbiol. 2016, 11, 335–349. [Google Scholar] [CrossRef] [PubMed]
- Knapp, S.; Wieland, C.W.; Florquin, S.; Pantophlet, R.; Dijkshoorn, L.; Tshimbalanga, N.; Akira, S.; van der Poll, T. Differential roles of CD14 and toll-like receptors 4 and 2 in murine Acinetobacter pneumonia. Am. J. Respir. Crit. Care Med. 2006, 173, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Russo, T.A.; Manohar, A.; Beanan, J.M.; Olson, R.; MacDonald, U.; Graham, J.; Umland, T.C. The Response Regulator BfmR Is a Potential Drug Target for Acinetobacter baumannii. mSphere 2016, 1, e00082-16. [Google Scholar] [CrossRef] [PubMed]
- Pires, S.; Parker, D. Innate Immune Responses to Acinetobacter baumannii in the Airway. J. Interferon Cytokine Res. 2019, 39, 441–449. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.K.; Adams, F.G.; Brown, M.H. Diversity and Function of Capsular Polysaccharide in Acinetobacter baumannii. Front. Microbiol. 2018, 9, 3301. [Google Scholar] [CrossRef] [PubMed]
- Tipton, K.A.; Chin, C.Y.; Farokhyfar, M.; Weiss, D.S.; Rather, P.N. Role of Capsule in Resistance to Disinfectants, Host Antimicrobials, and Desiccation in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2018, 62, e01188-18. [Google Scholar] [CrossRef] [PubMed]
- Xu, Q.; Chen, T.; Yan, B.; Zhang, L.; Pi, B.; Yang, Y.; Zhang, L.; Zhou, Z.; Ji, S.; Leptihn, S.; et al. Dual Role of gnaA in Antibiotic Resistance and Virulence in Acinetobacter baumannii. Antimicrob. Agents Chemother. 2019, 63, e00694-19. [Google Scholar] [CrossRef] [PubMed]
- Geisinger, E.; Isberg, R.R. Antibiotic modulation of capsular exopolysaccharide and virulence in Acinetobacter baumannii. PLoS Pathog. 2015, 11, e1004691. [Google Scholar] [CrossRef]
- Shan, W.; Kan, J.; Cai, X.; Yin, M. Insights into mucoid Acinetobacter baumannii: A review of microbiological characteristics, virulence, and pathogenic mechanisms in a threatening nosocomial pathogen. Microbiol. Res. 2022, 261, 127057. [Google Scholar] [CrossRef]
- Fiester, S.E.; Arivett, B.A.; Schmidt, R.E.; Beckett, A.C.; Ticak, T.; Carrier, M.V.; Ghosh, R.; Ohneck, E.J.; Metz, M.L.; Sellin Jeffries, M.K.; et al. Iron-Regulated Phospholipase C Activity Contributes to the Cytolytic Activity and Virulence of Acinetobacter baumannii. PLoS ONE 2016, 11, e0167068. [Google Scholar] [CrossRef]
- Stahl, J.; Bergmann, H.; Gottig, S.; Ebersberger, I.; Averhoff, B. Acinetobacter baumannii Virulence Is Mediated by the Concerted Action of Three Phospholipases D. PLoS ONE 2015, 10, e0138360. [Google Scholar] [CrossRef] [PubMed]
- Corral, J.; Perez-Varela, M.; Sanchez-Osuna, M.; Cortes, P.; Barbe, J.; Aranda, J. Importance of twitching and surface-associated motility in the virulence of Acinetobacter baumannii. Virulence 2021, 12, 2201–2213. [Google Scholar] [CrossRef] [PubMed]
- Behzadi, P. Classical chaperone-usher (CU) adhesive fimbriome: Uropathogenic Escherichia coli (UPEC) and urinary tract infections (UTIs). Folia Microbiol. 2020, 65, 45–65. [Google Scholar] [CrossRef] [PubMed]
- Ronish, L.A.; Lillehoj, E.; Fields, J.K.; Sundberg, E.J.; Piepenbrink, K.H. The structure of PilA from Acinetobacter baumannii AB5075 suggests a mechanism for functional specialization in Acinetobacter type IV pili. J. Biol. Chem. 2019, 294, 218–230. [Google Scholar] [CrossRef]
- Ayoub Moubareck, C.; Hammoudi Halat, D. Insights into Acinetobacter baumannii: A Review of Microbiological, Virulence, and Resistance Traits in a Threatening Nosocomial Pathogen. Antibiotics 2020, 9, 119. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, I.; Nygren, E.; Khalid, F.; Myint, S.L.; Uhlin, B.E. A Cyclic-di-GMP signalling network regulates biofilm formation and surface associated motility of Acinetobacter baumannii 17978. Sci. Rep. 2020, 10, 1991. [Google Scholar] [CrossRef]
- Corral, J.; Perez-Varela, M.; Barbe, J.; Aranda, J. Direct interaction between RecA and a CheW-like protein is required for surface-associated motility, chemotaxis and the full virulence of Acinetobacter baumannii strain ATCC 17978. Virulence 2020, 11, 315–326. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.L.; Dudek, A.; Liang, Y.H.; Janapatla, R.P.; Lee, H.Y.; Hsu, L.; Kuo, H.Y.; Chiu, C.H. d-mannose-sensitive pilus of Acinetobacter baumannii is linked to biofilm formation and adherence onto respiratory tract epithelial cells. J. Microbiol. Immunol. Infect. 2022, 55, 69–79. [Google Scholar] [CrossRef]
- Wood, C.R.; Ohneck, E.J.; Edelmann, R.E.; Actis, L.A. A Light-Regulated Type I Pilus Contributes to Acinetobacter baumannii Biofilm, Motility, and Virulence Functions. Infect. Immun. 2018, 86, e00442-18. [Google Scholar] [CrossRef]
- Noto, M.J.; Boyd, K.L.; Burns, W.J.; Varga, M.G.; Peek, R.M., Jr.; Skaar, E.P. Toll-like Receptor 9 Contributes to Defense against Acinetobacter baumannii Infection. Infect. Immun. 2015, 83, 4134–4141. [Google Scholar] [CrossRef]
- Sheldon, J.R.; Skaar, E.P. Acinetobacter baumannii can use multiple siderophores for iron acquisition, but only acinetobactin is required for virulence. PLoS Pathog. 2020, 16, e1008995. [Google Scholar] [CrossRef]
- Song, W.Y.; Kim, H.J. Current biochemical understanding regarding the metabolism of acinetobactin, the major siderophore of the human pathogen Acinetobacter baumannii, and outlook for discovery of novel anti-infectious agents based thereon. Nat. Prod. Rep. 2020, 37, 477–487. [Google Scholar] [CrossRef] [PubMed]
- Runci, F.; Gentile, V.; Frangipani, E.; Rampioni, G.; Leoni, L.; Lucidi, M.; Visaggio, D.; Harris, G.; Chen, W.; Stahl, J.; et al. Contribution of Active Iron Uptake to Acinetobacter baumannii Pathogenicity. Infect. Immun. 2019, 87, e00755-18. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Cao, C.Y.; Qiu, F.L.; Huang, H.N.; Xie, H.; Dong, R.; Shi, Y.Z.; Hu, X.N. Iron-Rich Conditions Induce OmpA and Virulence Changes of Acinetobacter baumannii. Front. Microbiol. 2021, 12, 725194. [Google Scholar] [CrossRef] [PubMed]
- Eijkelkamp, B.A.; Hassan, K.A.; Paulsen, I.T.; Brown, M.H. Investigation of the human pathogen Acinetobacter baumannii under iron limiting conditions. BMC Genom. 2011, 12, 126. [Google Scholar] [CrossRef] [PubMed]
- Skerniskyte, J.; Karazijaite, E.; Deschamps, J.; Krasauskas, R.; Armalyte, J.; Briandet, R.; Suziedeliene, E. Blp1 protein shows virulence-associated features and elicits protective immunity to Acinetobacter baumannii infection. BMC Microbiol. 2019, 19, 259. [Google Scholar] [CrossRef] [PubMed]
- Harding, C.M.; Pulido, M.R.; Di Venanzio, G.; Kinsella, R.L.; Webb, A.I.; Scott, N.E.; Pachon, J.; Feldman, M.F. Pathogenic Acinetobacter species have a functional type I secretion system and contact-dependent inhibition systems. J. Biol. Chem. 2017, 292, 9075–9087. [Google Scholar] [CrossRef] [PubMed]
- Sycz, G.; Di Venanzio, G.; Distel, J.S.; Sartorio, M.G.; Le, N.H.; Scott, N.E.; Beatty, W.L.; Feldman, M.F. Modern Acinetobacter baumannii clinical isolates replicate inside spacious vacuoles and egress from macrophages. PLoS Pathog. 2021, 17, e1009802. [Google Scholar] [CrossRef]
- Elhosseiny, N.M.; Attia, A.S. Acinetobacter: An emerging pathogen with a versatile secretome. Emerg. Microbes Infect. 2018, 7, 33. [Google Scholar] [CrossRef]
- Elhosseiny, N.M.; Elhezawy, N.B.; Attia, A.S. Comparative proteomics analyses of Acinetobacter baumannii strains ATCC 17978 and AB5075 reveal the differential role of type II secretion system secretomes in lung colonization and ciprofloxacin resistance. Microb. Pathog. 2019, 128, 20–27. [Google Scholar] [CrossRef]
- Elhosseiny, N.M.; Elhezawy, N.B.; Sayed, R.M.; Khattab, M.S.; El Far, M.Y.; Attia, A.S. gamma-Glutamyltransferase as a Novel Virulence Factor of Acinetobacter baumannii Inducing Alveolar Wall Destruction and Renal Damage in Systemic Disease. J. Infect. Dis. 2020, 222, 871–879. [Google Scholar] [CrossRef] [PubMed]
- Jackson-Litteken, C.D.; Di Venanzio, G.; Le, N.H.; Scott, N.E.; Djahanschiri, B.; Distel, J.S.; Pardue, E.J.; Ebersberger, I.; Feldman, M.F. InvL, an Invasin-Like Adhesin, Is a Type II Secretion System Substrate Required for Acinetobacter baumannii Uropathogenesis. mBio 2022, 13, e0025822. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.C.; Kuo, H.Y.; Tang, C.Y.; Chang, K.C.; Liou, M.L. Prevalence and mapping of a plasmid encoding a type IV secretion system in Acinetobacter baumannii. Genomics 2014, 104, 215–223. [Google Scholar] [CrossRef] [PubMed]
- Smith, C.A.; Antunes, N.T.; Stewart, N.K.; Toth, M.; Kumarasiri, M.; Chang, M.; Mobashery, S.; Vakulenko, S.B. Structural basis for carbapenemase activity of the OXA-23 beta-lactamase from Acinetobacter baumannii. Chem. Biol. 2013, 20, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- Perez, A.; Merino, M.; Rumbo-Feal, S.; Alvarez-Fraga, L.; Vallejo, J.A.; Beceiro, A.; Ohneck, E.J.; Mateos, J.; Fernandez-Puente, P.; Actis, L.A.; et al. The FhaB/FhaC two-partner secretion system is involved in adhesion of Acinetobacter baumannii AbH12O-A2 strain. Virulence 2017, 8, 959–974. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Iyer, L.M.; Aravind, L. A novel immunity system for bacterial nucleic acid degrading toxins and its recruitment in various eukaryotic and DNA viral systems. Nucleic Acids Res. 2011, 39, 4532–4552. [Google Scholar] [CrossRef] [PubMed]
- Weidensdorfer, M.; Ishikawa, M.; Hori, K.; Linke, D.; Djahanschiri, B.; Iruegas, R.; Ebersberger, I.; Riedel-Christ, S.; Enders, G.; Leukert, L.; et al. The Acinetobacter trimeric autotransporter adhesin Ata controls key virulence traits of Acinetobacter baumannii. Virulence 2019, 10, 68–81. [Google Scholar] [CrossRef]
- Weidensdorfer, M.; Chae, J.I.; Makobe, C.; Stahl, J.; Averhoff, B.; Muller, V.; Schurmann, C.; Brandes, R.P.; Wilharm, G.; Ballhorn, W.; et al. Analysis of Endothelial Adherence of Bartonella henselae and Acinetobacter baumannii Using a Dynamic Human Ex Vivo Infection Model. Infect. Immun. 2015, 84, 711–722. [Google Scholar] [CrossRef]
- Rahbar, M.R.; Zarei, M.; Jahangiri, A.; Khalili, S.; Nezafat, N.; Negahdaripour, M.; Fattahian, Y.; Ghasemi, Y. Trimeric autotransporter adhesins in Acinetobacter baumannii, coincidental evolution at work. Infect. Genet. Evol. 2019, 71, 116–127. [Google Scholar] [CrossRef]
- Hood, R.D.; Peterson, S.B.; Mougous, J.D. From Striking Out to Striking Gold: Discovering that Type VI Secretion Targets Bacteria. Cell Host Microbe 2017, 21, 286–289. [Google Scholar] [CrossRef]
- Lewis, J.M.; Deveson Lucas, D.; Harper, M.; Boyce, J.D. Systematic Identification and Analysis of Acinetobacter baumannii Type VI Secretion System Effector and Immunity Components. Front. Microbiol. 2019, 10, 2440. [Google Scholar] [CrossRef] [PubMed]
- Cianfanelli, F.R.; Monlezun, L.; Coulthurst, S.J. Aim, Load, Fire: The Type VI Secretion System, a Bacterial Nanoweapon. Trends Microbiol. 2016, 24, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zhou, Z.; He, F.; Ruan, Z.; Jiang, Y.; Hua, X.; Yu, Y. The role of the type VI secretion system vgrG gene in the virulence and antimicrobial resistance of Acinetobacter baumannii ATCC 19606. PLoS ONE 2018, 13, e0192288. [Google Scholar] [CrossRef]
- Lopez, J.; Ly, P.M.; Feldman, M.F. The Tip of the VgrG Spike Is Essential to Functional Type VI Secretion System Assembly in Acinetobacter baumannii. mBio 2020, 11, e02761-19. [Google Scholar] [CrossRef]
- Gebhardt, M.J.; Shuman, H.A. GigA and GigB are Master Regulators of Antibiotic Resistance, Stress Responses, and Virulence in Acinetobacter baumannii. J. Bacteriol. 2017, 199, e00066-17. [Google Scholar] [CrossRef] [PubMed]
- Zhou, H.; Gebhardt, M.J.; Czyz, D.M.; Yao, Y.; Shuman, H.A. The gigA/gigB Genes Regulate the Growth, Stress Response, and Virulence of Acinetobacter baumannii ATCC 17978 Strain. Front. Microbiol. 2021, 12, 723949. [Google Scholar] [CrossRef] [PubMed]
- Gebhardt, M.J.; Czyz, D.M.; Singh, S.; Zurawski, D.V.; Becker, L.; Shuman, H.A. GigC, a LysR Family Transcription Regulator, Is Required for Cysteine Metabolism and Virulence in Acinetobacter baumannii. Infect. Immun. 2020, 89, e00180-20. [Google Scholar] [CrossRef]
- Ketter, P.M.; Yu, J.J.; Guentzel, M.N.; May, H.C.; Gupta, R.; Eppinger, M.; Klose, K.E.; Seshu, J.; Chambers, J.P.; Cap, A.P.; et al. Acinetobacter baumannii Gastrointestinal Colonization Is Facilitated by Secretory IgA Which Is Reductively Dissociated by Bacterial Thioredoxin A. mBio 2018, 9, e01298-18. [Google Scholar] [CrossRef]
- Shrihari, S.; May, H.C.; Yu, J.J.; Papp, S.B.; Chambers, J.P.; Guentzel, M.N.; Arulanandam, B.P. Thioredoxin-mediated alteration of protein content and cytotoxicity of Acinetobacter baumannii outer membrane vesicles. Exp. Biol. Med. 2022, 247, 282–288. [Google Scholar] [CrossRef]
- May, H.C.; Yu, J.J.; Shrihari, S.; Seshu, J.; Klose, K.E.; Cap, A.P.; Chambers, J.P.; Guentzel, M.N.; Arulanandam, B.P. Thioredoxin Modulates Cell Surface Hydrophobicity in Acinetobacter baumannii. Front. Microbiol. 2019, 10, 2849. [Google Scholar] [CrossRef]
- May, H.C.; Yu, J.J.; Zhang, H.; Wang, Y.; Cap, A.P.; Chambers, J.P.; Guentzel, M.N.; Arulanandam, B.P. Thioredoxin-A is a virulence factor and mediator of the type IV pilus system in Acinetobacter baumannii. PLoS ONE 2019, 14, e0218505. [Google Scholar] [CrossRef] [PubMed]
- Neville, N.; Roberge, N.; Jia, Z. Polyphosphate Kinase 2 (PPK2) Enzymes: Structure, Function, and Roles in Bacterial Physiology and Virulence. Int. J. Mol. Sci. 2022, 23, 670. [Google Scholar] [CrossRef]
- Lv, H.; Zhou, Y.; Liu, B.; Guan, J.; Zhang, P.; Deng, X.; Li, D.; Wang, J. Polyphosphate Kinase Is Required for the Processes of Virulence and Persistence in Acinetobacter baumannii. Microbiol. Spectr. 2022, 10, e0123022. [Google Scholar] [CrossRef] [PubMed]
- Choi, C.H.; Lee, J.S.; Lee, Y.C.; Park, T.I.; Lee, J.C. Acinetobacter baumannii invades epithelial cells and outer membrane protein A mediates interactions with epithelial cells. BMC Microbiol. 2008, 8, 216. [Google Scholar] [CrossRef] [PubMed]
- Parra-Millan, R.; Guerrero-Gomez, D.; Ayerbe-Algaba, R.; Pachon-Ibanez, M.E.; Miranda-Vizuete, A.; Pachon, J.; Smani, Y. Intracellular Trafficking and Persistence of Acinetobacter baumannii Requires Transcription Factor EB. mSphere 2018, 3, e00106-18. [Google Scholar] [CrossRef] [PubMed]
- Jacob-Dubuisson, F.; Villeret, V.; Clantin, B.; Delattre, A.S.; Saint, N. First structural insights into the TpsB/Omp85 superfamily. Biol. Chem. 2009, 390, 675–684. [Google Scholar] [CrossRef] [PubMed]
- Piepenbrink, K.H.; Lillehoj, E.; Harding, C.M.; Labonte, J.W.; Zuo, X.; Rapp, C.A.; Munson, R.S., Jr.; Goldblum, S.E.; Feldman, M.F.; Gray, J.J.; et al. Structural Diversity in the Type IV Pili of Multidrug-resistant Acinetobacter. J. Biol. Chem. 2016, 291, 22924–22935. [Google Scholar] [CrossRef] [PubMed]
- Crepin, S.; Ottosen, E.N.; Peters, K.; Smith, S.N.; Himpsl, S.D.; Vollmer, W.; Mobley, H.L.T. The lytic transglycosylase MltB connects membrane homeostasis and in vivo fitness of Acinetobacter baumannii. Mol. Microbiol. 2018, 109, 745–762. [Google Scholar] [CrossRef]
- De Gregorio, E.; Del Franco, M.; Martinucci, M.; Roscetto, E.; Zarrilli, R.; Di Nocera, P.P. Biofilm-associated proteins: News from Acinetobacter. BMC Genom. 2015, 16, 933. [Google Scholar] [CrossRef]
- Gil-Marques, M.L.; Labrador Herrera, G.; Miro Canturri, A.; Pachon, J.; Smani, Y.; Pachon-Ibanez, M.E. Role of PstS in the Pathogenesis of Acinetobacter baumannii under Microaerobiosis and Normoxia. J. Infect. Dis. 2020, 222, 1204–1212. [Google Scholar] [CrossRef]
- Radin, J.N.; Orihuela, C.J.; Murti, G.; Guglielmo, C.; Murray, P.J.; Tuomanen, E.I. β-Arrestin 1 participates in platelet-activating factor receptor-mediated endocytosis of Streptococcus pneumoniae. Infect. Immun. 2005, 73, 7827–7835. [Google Scholar] [CrossRef] [PubMed]
- Smani, Y.; Docobo-Perez, F.; Lopez-Rojas, R.; Dominguez-Herrera, J.; Ibanez-Martinez, J.; Pachon, J. Platelet-activating factor receptor initiates contact of Acinetobacter baumannii expressing phosphorylcholine with host cells. J. Biol. Chem. 2012, 287, 26901–26910. [Google Scholar] [CrossRef] [PubMed]
- Hauck, C.R. Cell adhesion receptors—Signaling capacity and exploitation by bacterial pathogens. Med. Microbiol. Immunol. 2002, 191, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Kc, R.; Shukla, S.D.; Walters, E.H.; O’Toole, R.F. Temporal upregulation of host surface receptors provides a window of opportunity for bacterial adhesion and disease. Microbiology 2017, 163, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Ambrosi, C.; Scribano, D.; Sarshar, M.; Zagaglia, C.; Singer, B.B.; Palamara, A.T. Acinetobacter baumannii Targets Human Carcinoembryonic Antigen-Related Cell Adhesion Molecules (CEACAMs) for Invasion of Pneumocytes. mSystems 2020, 5, e00604-20. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Brumell, J.H. Bacteria-autophagy interplay: A battle for survival. Nat. Rev. Microbiol. 2014, 12, 101–114. [Google Scholar] [CrossRef] [PubMed]
- An, Z.; Ding, W. Acinetobacter baumannii up-regulates LncRNA-GAS5 and promotes the degradation of STX17 by blocking the activation of YY1. Virulence 2021, 12, 1965–1979. [Google Scholar] [CrossRef]
- Du, J.; Ren, W.; Yao, F.; Wang, H.; Zhang, K.; Luo, M.; Shang, Y.; O’Connell, D.; Bei, Z.; Wang, H.; et al. YY1 cooperates with TFEB to regulate autophagy and lysosomal biogenesis in melanoma. Mol. Carcinog. 2019, 58, 2149–2160. [Google Scholar] [CrossRef]
- Peng, C.; Han, J.; Ye, X.; Zhang, X. IL-33 Treatment Attenuates the Systemic Inflammation Reaction in Acinetobacter baumannii Pneumonia by Suppressing TLR4/NF-kappaB Signaling. Inflammation 2018, 41, 870–877. [Google Scholar] [CrossRef]
- Kikuchi-Ueda, T.; Ubagai, T.; Kamoshida, G.; Nakano, R.; Nakano, A.; Ono, Y. Acinetobacter baumannii LOS Regulate the Expression of Inflammatory Cytokine Genes and Proteins in Human Mast Cells. Pathogens 2021, 10, 290. [Google Scholar] [CrossRef]
- Diep, J.K.; Russo, T.A.; Rao, G.G. Mechanism-Based Disease Progression Model Describing Host-Pathogen Interactions during the Pathogenesis of Acinetobacter baumannii Pneumonia. CPT Pharmacomet. Syst. Pharmacol. 2018, 7, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Kale, S.D.; Dikshit, N.; Kumar, P.; Balamuralidhar, V.; Khameneh, H.J.; Bin Abdul Malik, N.; Koh, T.H.; Tan, G.G.Y.; Tan, T.T.; Mortellaro, A.; et al. Nod2 is required for the early innate immune clearance of Acinetobacter baumannii from the lungs. Sci. Rep. 2017, 7, 17429. [Google Scholar] [CrossRef] [PubMed]
- Tiku, V.; Kew, C.; Kofoed, E.M.; Peng, Y.; Dikic, I.; Tan, M.W. Acinetobacter baumannii Secretes a Bioactive Lipid That Triggers Inflammatory Signaling and Cell Death. Front. Microbiol. 2022, 13, 870101. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Shao, Y.; Li, S.; Xin, N.; Ma, T.; Zhao, C.; Song, M. Caspase-11 Plays a Protective Role in Pulmonary Acinetobacter baumannii Infection. Infect. Immun. 2017, 85, e00350-17. [Google Scholar] [CrossRef] [PubMed]
- Dikshit, N.; Kale, S.D.; Khameneh, H.J.; Balamuralidhar, V.; Tang, C.Y.; Kumar, P.; Lim, T.P.; Tan, T.T.; Kwa, A.L.; Mortellaro, A.; et al. NLRP3 inflammasome pathway has a critical role in the host immunity against clinically relevant Acinetobacter baumannii pulmonary infection. Mucosal Immunol. 2018, 11, 257–272. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.; Nielsen, T.B.; Bonomo, R.A.; Pantapalangkoor, P.; Luna, B.; Spellberg, B. Clinical and Pathophysiological Overview of Acinetobacter Infections: A Century of Challenges. Clin. Microbiol. Rev. 2017, 30, 409–447. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Peng, C.; Zhao, D.; Liu, L.; Guo, B.; Shi, M.; Xiao, Y.; Yu, Z.; Yu, Y.; Sun, B.; et al. Outer membrane protein A inhibits the degradation of caspase-1 to regulate NLRP3 inflammasome activation and exacerbate the Acinetobacter baumannii pulmonary inflammation. Microb. Pathog. 2021, 153, 104788. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Ren, W.; Jiang, Z.; Zhu, L. Regulation of the NLRP3 inflammasome and macrophage pyroptosis by the p38 MAPK signaling pathway in a mouse model of acute lung injury. Mol. Med. Rep. 2018, 18, 4399–4409. [Google Scholar] [CrossRef]
- March, C.; Regueiro, V.; Llobet, E.; Moranta, D.; Morey, P.; Garmendia, J.; Bengoechea, J.A. Dissection of host cell signal transduction during Acinetobacter baumannii-triggered inflammatory response. PLoS ONE 2010, 5, e10033. [Google Scholar] [CrossRef]
- Skariyachan, S.; Taskeen, N.; Ganta, M.; Venkata Krishna, B. Recent perspectives on the virulent factors and treatment options for multidrug-resistant Acinetobacter baumannii. Crit. Rev. Microbiol. 2019, 45, 315–333. [Google Scholar] [CrossRef]
- Marion, C.R.; Lee, J.; Sharma, L.; Park, K.S.; Lee, C.; Liu, W.; Liu, P.; Feng, J.; Gho, Y.S.; Dela Cruz, C.S. Toll-Like Receptors 2 and 4 Modulate Pulmonary Inflammation and Host Factors Mediated by Outer Membrane Vesicles Derived from Acinetobacter baumannii. Infect. Immun. 2019, 87, e00243-19. [Google Scholar] [CrossRef] [PubMed]
- Gu, H.; Zeng, X.; Peng, L.; Xiang, C.; Zhou, Y.; Zhang, X.; Zhang, J.; Wang, N.; Guo, G.; Li, Y.; et al. Vaccination induces rapid protection against bacterial pneumonia via training alveolar macrophage in mice. eLife 2021, 10, e69951. [Google Scholar] [CrossRef] [PubMed]
- Chen, W. Host Innate Immune Responses to Acinetobacter baumannii Infection. Front. Cell. Infect. Microbiol. 2020, 10, 486. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Crowell, S.A.; Harding, C.M.; De Silva, P.M.; Harrison, A.; Fernando, D.M.; Mason, K.M.; Santana, E.; Loewen, P.C.; Kumar, A.; et al. KatG and KatE confer Acinetobacter resistance to hydrogen peroxide but sensitize bacteria to killing by phagocytic respiratory burst. Life Sci. 2016, 148, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Kamoshida, G.; Kikuchi-Ueda, T.; Nishida, S.; Tansho-Nagakawa, S.; Ubagai, T.; Ono, Y. Pathogenic Bacterium Acinetobacter baumannii Inhibits the Formation of Neutrophil Extracellular Traps by Suppressing Neutrophil Adhesion. Front. Immunol. 2018, 9, 178. [Google Scholar] [CrossRef] [PubMed]
- Rosales-Reyes, R.; Gayosso-Vazquez, C.; Fernandez-Vazquez, J.L.; Jarillo-Quijada, M.D.; Rivera-Benitez, C.; Santos-Preciado, J.I.; Alcantar-Curiel, M.D. Virulence profiles and innate immune responses against highly lethal, multidrug-resistant nosocomial isolates of Acinetobacter baumannii from a tertiary care hospital in Mexico. PLoS ONE 2017, 12, e0182899. [Google Scholar] [CrossRef] [PubMed]
- Martinez, J.; Fernandez, J.S.; Liu, C.; Hoard, A.; Mendoza, A.; Nakanouchi, J.; Rodman, N.; Courville, R.; Tuttobene, M.R.; Lopez, C.; et al. Human pleural fluid triggers global changes in the transcriptional landscape of Acinetobacter baumannii as an adaptive response to stress. Sci. Rep. 2019, 9, 17251. [Google Scholar] [CrossRef] [PubMed]
- Rodman, N.; Martinez, J.; Fung, S.; Nakanouchi, J.; Myers, A.L.; Harris, C.M.; Dang, E.; Fernandez, J.S.; Liu, C.; Mendoza, A.M.; et al. Human Pleural Fluid Elicits Pyruvate and Phenylalanine Metabolism in Acinetobacter baumannii to Enhance Cytotoxicity and Immune Evasion. Front. Microbiol. 2019, 10, 1581. [Google Scholar] [CrossRef]
- Tansho-Nagakawa, S.; Sato, Y.; Ubagai, T.; Kikuchi-Ueda, T.; Kamoshida, G.O.; Nishida, S.; Ono, Y. Histopathological Analysis of Acinetobacter baumannii Lung Infection in a Mouse Model. Pol. J. Microbiol. 2021, 70, 469–477. [Google Scholar] [CrossRef]
- Lee, H.H.; Aslanyan, L.; Vidyasagar, A.; Brennan, M.B.; Tauber, M.S.; Carrillo-Sepulveda, M.A.; Dores, M.R.; Rigel, N.W.; Martinez, L.R. Depletion of Alveolar Macrophages Increases Pulmonary Neutrophil Infiltration, Tissue Damage, and Sepsis in a Murine Model of Acinetobacter baumannii Pneumonia. Infect. Immun. 2020, 88, e00128-20. [Google Scholar] [CrossRef]
- Xiong, S.; Hong, Z.; Huang, L.S.; Tsukasaki, Y.; Nepal, S.; Di, A.; Zhong, M.; Wu, W.; Ye, Z.; Gao, X.; et al. IL-1beta suppression of VE-cadherin transcription underlies sepsis-induced inflammatory lung injury. J. Clin. Investig. 2020, 130, 3684–3698. [Google Scholar] [CrossRef]
- Waack, U.; Warnock, M.; Yee, A.; Huttinger, Z.; Smith, S.; Kumar, A.; Deroux, A.; Ginsburg, D.; Mobley, H.L.T.; Lawrence, D.A.; et al. CpaA Is a Glycan-Specific Adamalysin-like Protease Secreted by Acinetobacter baumannii That Inactivates Coagulation Factor XII. mBio 2018, 9, e01606-18. [Google Scholar] [CrossRef]
- Smiline Girija, A.S.; Ganesh, P.S. Virulence of Acinetobacter baumannii in proteins moonlighting. Arch. Microbiol. 2021, 204, 96. [Google Scholar] [CrossRef]
- Koenigs, A.; Zipfel, P.F.; Kraiczy, P. Translation Elongation Factor Tuf of Acinetobacter baumannii Is a Plasminogen-Binding Protein. PLoS ONE 2015, 10, e0134418. [Google Scholar] [CrossRef]
- Zhang, W.; Yao, Y.; Zhou, H.; He, J.; Wang, J.; Li, L.; Gao, M.; Liu, X.; Shi, Y.; Lin, J.; et al. Interactions between host epithelial cells and Acinetobacter baumannii promote the emergence of highly antibiotic resistant and highly mucoid strains. Emerg. Microbes Infect. 2022, 11, 2556–2569. [Google Scholar] [CrossRef] [PubMed]
| Category | Virulence Factor(s) | Function(s) | References |
|---|---|---|---|
| Outer membrane proteins (Omps) | OmpA | Adhesion, invasion, autophagy induction, cellular injury, host–pathogen interactions, biofilm formation, antibiotics resistance | [19,21] |
| CarO | Adhesion, invasion, host–pathogen interactions, antibiotic resistance | [4,24,25] | |
| Omp33 | Adhesion, invasion, apoptosis induction | [5] | |
| OprD/OccAB1 | Nutrient intake | [27,28,29] | |
| OmpW | Iron assimilation, adhesion, invasion, cytotoxicity, biofilm formation | [29,30] | |
| Lipopolysaccharides | LPS | Pro-inflammatory effect, serum resistance | [22,31,32] |
| Capsular polysaccharides | CPS | Stress resistance, persistence, antibiotic resistance | [33,34,36,37,38,39] |
| Phospholipase | Phospholipase C/D | Invasion, serum resistance, iron assimilation | [17,40,41] |
| Pili and motility | Type IV pili | Motility, biofilm formation | [43,44] |
| Csu pilus | Biofilm formation | [48] | |
| Photo-regulated type I chaperone–usher pilus | Biofilm formation, adhesion, virulence | [49] | |
| Iron acquisition | Acinetobactin | Iron assimilation | [50,51,52,53,54,55,56,57,58] |
| Secretion systems | T1SS | Intracellular survival, adhesion, biofilm formation | [56,57,58] |
| T2SS | Adhesion, serum resistance, host–pathogen interactions | [59,60,61,62] | |
| T4SS | Antibiotic resistance, host–pathogen interactions | [63,64] | |
| T5SS | Adhesion, invasion, apoptosis induction, biofilm formation | [65,67,68,69] | |
| T6SS | Stress resistance, killing of bacterial competitors, biofilm formation | [70,71,72,73,74] | |
| Gig (Growth in Galleria) | GigA/B/C | Stress resistance, antibiotic resistance | [75,76,77] |
| Thioredoxin A | TrxA | Stress resistance, adhesion, host–pathogen interactions, biofilm formation | [79,80,81] |
| Polyphosphate kinase | PPK | Motility, stress resistance, biofilm formation | [82,83] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yao, Y.; Chen, Q.; Zhou, H. Virulence Factors and Pathogenicity Mechanisms of Acinetobacter baumannii in Respiratory Infectious Diseases. Antibiotics 2023, 12, 1749. https://doi.org/10.3390/antibiotics12121749
Yao Y, Chen Q, Zhou H. Virulence Factors and Pathogenicity Mechanisms of Acinetobacter baumannii in Respiratory Infectious Diseases. Antibiotics. 2023; 12(12):1749. https://doi.org/10.3390/antibiotics12121749
Chicago/Turabian StyleYao, Yake, Qi Chen, and Hua Zhou. 2023. "Virulence Factors and Pathogenicity Mechanisms of Acinetobacter baumannii in Respiratory Infectious Diseases" Antibiotics 12, no. 12: 1749. https://doi.org/10.3390/antibiotics12121749
APA StyleYao, Y., Chen, Q., & Zhou, H. (2023). Virulence Factors and Pathogenicity Mechanisms of Acinetobacter baumannii in Respiratory Infectious Diseases. Antibiotics, 12(12), 1749. https://doi.org/10.3390/antibiotics12121749







