Vancomycin Elution Kinetics of Four Antibiotic Carriers Used in Orthopaedic Surgery: In Vitro Study over 42 Days
Abstract
:1. Introduction
2. Results
2.1. Mean Concentration Differences between Antibiotic Carriers
2.2. Time-Dependent Change in Individual Antibiotic Carriers
- (a)
- Carrier A: A statistically significant difference in mean antibiotic concentrations over time was present (p < 0.001; Table 1). Although an overall steady decrease in antibiotic concentration was observed during the study period, there was no difference between any nearest time points (all p > 0.05).
- (b)
- Carrier B: Neither a significant difference in mean vancomycin concentration over time (p = 0.921) nor between nearest time points was observed (all p > 0.5; Table 1). Notably, a very shallow decrease in vancomycin concentration over time was present, starting from 4.5 mg/mL at 48 h and reaching 2.6 mg/mL at 42 days.
- (c)
- Carrier C: There was a significant mean difference in antibiotic concentration over the study period (p < 0.001; Table 1). However, apart from a significant drop in vancomycin concentration from day 7 to day 14 by 5.9 mg/mL (p < 0.001), no difference between the nearest time points was observed (p > 0.05).
- (d)
- Carrier D: Significant mean differences in vancomycin concentrations over time were observed (p < 0.001; Table 1). Assessing nearest time points, a significant decrease in vancomycin concentration between 8 and 24 h (−1.5 mg/mL; p = 0.001); a significant increase between 8 and 24 h (+5.6 mg/mL; p < 0.001); and subsequently significant decreases between 24 and 48 h (−2.1 mg/mL; p < 0.001), 48 h and 7 days (−3.9 mg/mL; p < 0.001), 7 and 14 days (−3.0; p < 0.001), as well as 14 and 21 days (−1.3; p = 0.003) were observed (Table 1).
3. Discussion
4. Materials and Methods
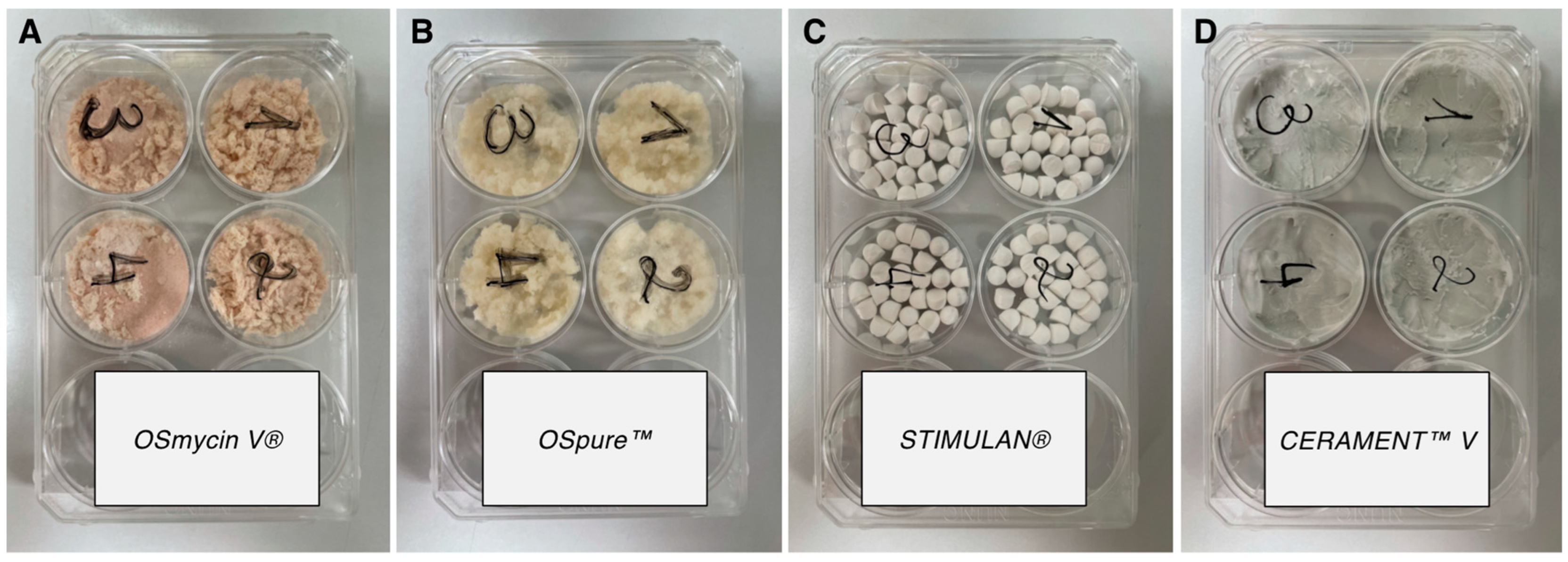
4.1. Description of Antibiotic Carriers
- (a)
- Carrier A (OSmycin V® (European Cell and Tissue Bank, Wels, Austria)) consists of decellularized and delipidated human allograft bone chips, sized 1.5–10 mm, that have been impregnated with 0.56 g vancomycin per 1 g of bone chips.
- (b)
- Carrier B (Ospure™ (European Cell and Tissue Bank, Wels, Austria)) likewise contains delipidated and decellularized human allograft bone chips without any additional substances.
- (c)
- Carrier C (STIMULAN® (Biocomposites, Keele, UK)) is a calcium-sulphate matrix that can be mixed with tobramycin, gentamycin, and vancomycin. Prior to implantation into bone, the carrier is shaped into small beads, which promptly solidify. For the current study, 10 mL of carrier C was mixed with 1 g of vancomycin, as suggested by the manufacturer.
- (d)
- Carrier D (CERAMENT™V (Bone Support, Lund, Sweden)) constitutes a vancomycin-loaded hydroxyapatite/calcium-sulphate composite that can either be injected directly into the bone or formed into beads prior to implantation [26]. It contains 0.66 g vancomycin per 10 mL of carrier.
4.2. Preparation of Antibiotic Carriers
- (a)
- For the preparation of carrier A, four wells of a six-well plate were each filled with 5 mL of the carrier as provided by the manufacturer (equivalent to 2 g, containing 1.1 g of vancomycin each) and pressed with a 35 lb-calibrated indenter (Figure 2).
- (b)
- Firstly, 4 wells of a 6-well plate (Figure 2) were filled with 5 mL of carrier B and subsequently impregnated with a physiological saline solution-dissolved vancomycin (Vancomycin Hikma, Hikma Pharmaceuticals, Sintra, Portugal) for 15 min at room temperature. This allowed the bone chips to absorb the vancomycin solution. The resulting samples were equivalent to 1.5 g containing 0.83 g of vancomycin each and were ultimately pressed with a 35 lb-calibrated indenter.
- (c)
- For carrier C, 1 g of vancomycin powder was first mixed with 10 mL of the solid phase of the carrier. Thereafter, 6 mL of the mixing solution provided by the manufacturer was added and thoroughly mixed for 30 s. Within 1–2 min of combining the liquid and solid phases, the mixture was transferred to the bead mat provided by the manufacturer, with a bead size of 6 mm. The mat was gently tapped on the table to remove any potential air bubbles. After another 8 min of setting time, the beads were released from the bead mat by bending it back and forth. Again, four wells of a 6-well plate were each filled with 5 mL of beads (containing 0.305 g of vancomycin) and pressed with the indenter calibrated to 35 lbs (Figure 2).
- (d)
- Carrier D was prepared according to the package insert. First, 1 g of vancomycin powder was dissolved in an iodine-based liquid phase (iohexol, provided by the manufacturer in a syringe). The mixture was subsequently transferred to the mixing device containing hydroxyapatite and calcium sulphate hemihydrate powders. The liquid and solid phase were subsequently combined for 30s using the manufacturer’s mixing device, equivalent to one complete turn per second. Thereafter, 5 mL of the prepared carrier was inserted into 4 wells of a 6-well plate each (containing 0.247 g of vancomycin) and allowed to settle for 3 min. Afterwards, probes were pressed with a 35 lb-calibrated indenter (Figure 2).
4.3. In Vitro Elution Assay
4.4. Kinetic Microparticle Immunoassay
4.5. Statistical Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Harris, M.; Ahmed, H.; Pace, L.; Minter, J.; Neel, M.; Jennings, J. Evaluation of Antibiotic-Releasing Triphasic Bone Void Filler In-Vitro. J. Funct. Biomater. 2018, 9, 55. [Google Scholar] [CrossRef]
- Behairy, Y.; Jasty, M. Bone grafts and bone substitutes in hip and knee surgery. Orthop. Clin. N. Am. 1999, 30, 661–671. [Google Scholar] [CrossRef]
- Blitch, E.L.; Ricotta, P.J. Introduction to bone grafting. J. Foot Ankle Surg. 1996, 35, 458–462. [Google Scholar] [CrossRef]
- Bajammal, S.S.; Zlowodzki, M.; Lelwica, A.; Tornetta, P., 3rd; Einhorn, T.A.; Buckley, R.; Leighton, R.; Russell, T.A.; Larsson, S.; Bhandari, M. The use of calcium phosphate bone cement in fracture treatment. A meta-analysis of randomized trials. J. Bone Jt. Surg. Am. 2008, 90, 1186–1196. [Google Scholar] [CrossRef]
- Campana, V.; Milano, G.; Pagano, E.; Barba, M.; Cicione, C.; Salonna, G.; Lattanzi, W.; Logroscino, G. Bone substitutes in orthopaedic surgery: From basic science to clinical practice. J. Mater. Sci. Mater. Med. 2014, 25, 2445–2461. [Google Scholar] [CrossRef]
- Kurien, T.; Pearson, R.G.; Scammell, B.E. Bone graft substitutes currently available in orthopaedic practice: The evidence for their use. Bone Jt. J. 2013, 95-B, 583–597. [Google Scholar] [CrossRef]
- Winkler, H.; Haiden, P. Allograft Bone as Antibiotic Carrier. J. Bone Jt. Infect. 2017, 2, 52–62. [Google Scholar] [CrossRef]
- Pruss, A.; Hansen, A.; Kao, M.; Gurtler, L.; Pauli, G.; Benedix, F.; Von Versen, R. Comparison of the efficacy of virus inactivation methods in allogeneic avital bone tissue transplants. Cell Tissue Bank. 2001, 2, 201–215. [Google Scholar] [CrossRef]
- Fages, J.; Poirier, B.; Barbier, Y.; Frayssinet, P.; Joffret, M.L.; Majewski, W.; Bonel, G.; Larzul, D. Viral inactivation of human bone tissue using supercritical fluid extraction. ASAIO J. 1998, 44, 289–293. [Google Scholar] [CrossRef]
- Guo, H.; Wei, J.; Liu, C.S. Development of a degradable cement of calcium phosphate and calcium sulfate composite for bone reconstruction. Biomed. Mater. 2006, 1, 193–197. [Google Scholar] [CrossRef]
- Nilsson, M.; Zheng, M.H.; Tagil, M. The composite of hydroxyapatite and calcium sulphate: A review of preclinical evaluation and clinical applications. Expert Rev. Med. Devices 2013, 10, 675–684. [Google Scholar] [CrossRef]
- Jiranek, W.A.; Hanssen, A.D.; Greenwald, A.S. Antibiotic-loaded bone cement for infection prophylaxis in total joint replacement. J. Bone Jt. Surg. Am. 2006, 88, 2487–2500. [Google Scholar] [CrossRef]
- Chai, F.; Hornez, J.C.; Blanchemain, N.; Neut, C.; Descamps, M.; Hildebrand, H.F. Antibacterial activation of hydroxyapatite (HA) with controlled porosity by different antibiotics. Biomol. Eng. 2007, 24, 510–514. [Google Scholar] [CrossRef]
- Ferrell, Z.; Grainger, D.W.; Sinclair, K.D. Antibiotic-eluting resorbable bone-void filler evaluated in a large animal infection prevention model. Eur. Cells Mater. 2019, 37, 265–276. [Google Scholar] [CrossRef]
- Laycock, P.A.; Cooper, J.J.; Howlin, R.P.; Delury, C.; Aiken, S.; Stoodley, P. In Vitro Efficacy of Antibiotics Released from Calcium Sulfate Bone Void Filler Beads. Materials 2018, 11, 2265. [Google Scholar] [CrossRef]
- McNally, M.A.; Ferguson, J.Y.; Lau, A.C.; Diefenbeck, M.; Scarborough, M.; Ramsden, A.J.; Atkins, B.L. Single-stage treatment of chronic osteomyelitis with a new absorbable, gentamicin-loaded, calcium sulphate/hydroxyapatite biocomposite: A prospective series of 100 cases. Bone Jt. J. 2016, 98-B, 1289–1296. [Google Scholar] [CrossRef]
- Scharer, B.M.; Sanicola, S.M. The in vitro elution characteristics of vancomycin from calcium phosphate-calcium sulfate beads. J. Foot Ankle Surg. 2009, 48, 540–542. [Google Scholar] [CrossRef]
- Askew, M.J.; Kufel, M.F.; Fleissner, P.R., Jr.; Gradisar, I.A., Jr.; Salstrom, S.J.; Tan, J.S. Effect of vacuum mixing on the mechanical properties of antibiotic-impregnated polymethylmethacrylate bone cement. J. Biomed. Mater. Res. 1990, 24, 573–580. [Google Scholar] [CrossRef]
- Trippel, S.B. Antibiotic-impregnated cement in total joint arthroplasty. J. Bone Jt. Surg. Am. 1986, 68, 1297–1302. [Google Scholar] [CrossRef]
- Liu, S.J.; Ueng, S.W.; Chan, E.C.; Lin, S.S.; Tsai, C.H.; Wei, F.C.; Shih, C.H. In vitro elution of vancomycin from biodegradable beads. J. Biomed. Mater. Res. 1999, 48, 613–620. [Google Scholar] [CrossRef]
- Kluin, O.S.; van der Mei, H.C.; Busscher, H.J.; Neut, D. Biodegradable vs. non-biodegradable antibiotic delivery devices in the treatment of osteomyelitis. Expert Opin. Drug Deliv. 2013, 10, 341–351. [Google Scholar] [CrossRef]
- Zilberman, M.; Elsner, J.J. Antibiotic-eluting medical devices for various applications. J. Control. Release 2008, 130, 202–215. [Google Scholar] [CrossRef]
- ter Boo, G.J.; Grijpma, D.W.; Moriarty, T.F.; Richards, R.G.; Eglin, D. Antimicrobial delivery systems for local infection prophylaxis in orthopedic- and trauma surgery. Biomaterials 2015, 52, 113–125. [Google Scholar] [CrossRef]
- Kucera, T.; Ryskova, L.; Soukup, T.; Malakova, J.; Cermakova, E.; Mericka, P.; Suchanek, J.; Sponer, P. Elution kinetics of vancomycin and gentamicin from carriers and their effects on mesenchymal stem cell proliferation: An in vitro study. BMC Musculoskelet. Disord. 2017, 18, 381. [Google Scholar] [CrossRef]
- Makarov, C.; Cohen, V.; Raz-Pasteur, A.; Gotman, I. In vitro elution of vancomycin from biodegradable osteoconductive calcium phosphate-polycaprolactone composite beads for treatment of osteomyelitis. Eur. J. Pharm. Sci. 2014, 62, 49–56. [Google Scholar] [CrossRef]
- Nien, Y.H.; Lin, S.W.; Hsu, Y.N. Preparation and characterization of acrylic bone cement with high drug release. Mater. Sci. Eng. C Mater. Biol. Appl. 2013, 33, 974–978. [Google Scholar] [CrossRef]
- Dorozhkin, S.V. Calcium orthophosphate cements for biomedical application. J. Mater. Sci. 2008, 43, 3028–3057. [Google Scholar] [CrossRef]
- Ogose, A.; Hotta, T.; Kawashima, H.; Kondo, N.; Gu, W.; Kamura, T.; Endo, N. Comparison of hydroxyapatite and beta tricalcium phosphate as bone substitutes after excision of bone tumors. J. Biomed. Mater. Res. B Appl. Biomater. 2005, 72, 94–101. [Google Scholar] [CrossRef]
- Walsh, W.R.; Vizesi, F.; Michael, D.; Auld, J.; Langdown, A.; Oliver, R.; Yu, Y.; Irie, H.; Bruce, W. Beta-TCP bone graft substitutes in a bilateral rabbit tibial defect model. Biomaterials 2008, 29, 266–271. [Google Scholar] [CrossRef]
- Proussaefs, P.; Lozada, J.; Valencia, G.; Rohrer, M.D. Histologic evaluation of a hydroxyapatite onlay bone graft retrieved after 9 years: A clinical report. J. Prosthet. Dent. 2002, 87, 481–484. [Google Scholar] [CrossRef]
- Van der Stok, J.; Van Lieshout, E.M.; El-Massoudi, Y.; Van Kralingen, G.H.; Patka, P. Bone substitutes in the Netherlands—A systematic literature review. Acta Biomater. 2011, 7, 739–750. [Google Scholar] [CrossRef]
- Thomas, M.V.; Puleo, D.A. Calcium sulfate: Properties and clinical applications. J. Biomed. Mater. Res. B Appl. Biomater. 2009, 88, 597–610. [Google Scholar] [CrossRef]
- Hing, K.A.; Wilson, L.F.; Buckland, T. Comparative performance of three ceramic bone graft substitutes. Spine J. 2007, 7, 475–490. [Google Scholar] [CrossRef]
- Frayssinet, P.; Rouquet, N.; Mathon, D.; Autefage, A.; Fages, J. Histological integration of allogeneic cancellous bone tissue treated by supercritical CO2 implanted in sheep bones. Biomaterials 1998, 19, 2247–2253. [Google Scholar] [CrossRef]
- Thorén, K.; Aspenberg, P. Increased bone ingrowth distance into lipid-extracted bank bone at 6 weeks. A titanium chamber study in allogeneic and syngeneic rats. Arch. Orthop. Trauma Surg. 1995, 114, 167–171. [Google Scholar] [CrossRef]
- Khan, S.N.; Cammisa, F.P., Jr.; Sandhu, H.S.; Diwan, A.D.; Girardi, F.P.; Lane, J.M. The biology of bone grafting. J. Am. Acad. Orthop. Surg. 2005, 13, 77–86. [Google Scholar] [CrossRef]
- Winkler, H.; Janata, O.; Berger, C.; Wein, W.; Georgopoulos, A. In vitro release of vancomycin and tobramycin from impregnated human and bovine bone grafts. J. Antimicrob. Chemother. 2000, 46, 423–428. [Google Scholar] [CrossRef]
- Bormann, N.; Schwabe, P.; Smith, M.D.; Wildemann, B. Analysis of parameters influencing the release of antibiotics mixed with bone grafting material using a reliable mixing procedure. Bone 2014, 59, 162–172. [Google Scholar] [CrossRef]
- Rathbone, C.R.; Cross, J.D.; Brown, K.V.; Murray, C.K.; Wenke, J.C. Effect of various concentrations of antibiotics on osteogenic cell viability and activity. J. Orthop. Res. 2011, 29, 1070–1074. [Google Scholar] [CrossRef]
- Amerstorfer, F.; Fischerauer, S.; Sadoghi, P.; Schwantzer, G.; Kuehn, K.D.; Leithner, A.; Glehr, M. Superficial Vancomycin Coating of Bone Cement in Orthopedic Revision Surgery: A Safe Technique to Enhance Local Antibiotic Concentrations. J. Arthroplast. 2017, 32, 1618–1624. [Google Scholar] [CrossRef]
- Bishop, A.R.; Kim, S.; Squire, M.W.; Rose, W.E.; Ploeg, H.L. Vancomycin elution, activity and impact on mechanical properties when added to orthopedic bone cement. J. Mech. Behav. Biomed. Mater. 2018, 87, 80–86. [Google Scholar] [CrossRef]
- Aquaclean—Antimicrobial Additive for Water Soluble Heating Bath Fluids; WAK—Chemie Medical GmbH: Steinbach, Germany.

| Time | 4 h | 8 h | 24 h | 48 h | 7 d | 14 d | 21 d | 35 d | 42 d | Overall Difference (ANOVA) |
|---|---|---|---|---|---|---|---|---|---|---|
| Carrier A (OSmycin V®) | 37.5 ± 8.5 | 29.5 ± 4.3 | 28.8 ± 7.3 | 23.8 ± 8.1 | 16.4 ± 7.5 | 10.6 ± 5.7 | 4.5 ± 1.6 | 2.5 ± 0.6 | 1.5 ± 0.4 | F(8, 24) = 54.0 p < 0.001 |
| Carrier B (OSpure™) | 5.5 ± 6.1 | 5.5 ± 6.8 | 5.8 ± 4.8 | 4.5 ± 2.1 | 4.4 ± 0.7 | 3.7 ± 0.2 | 3.7 ± 0.7 | 3.3 ± 0.8 | 2.6 ± 0.8 | F(8, 24) = 0.55 p = 0.921 |
| Carrier C (STIMULAN) | 6.4 ± 0.3 | 5.1 ± 0.2 | 7.1 ± 4.0 | 10.0 ± 0.5 | 10.0 ± 0.5 | 4.1 ± 0.2 | 1.6 ± 0.1 | 0.5 ± 0.1 | 0.1 ± 0.05 | F(8, 24) = 29.8 p < 0.001 |
| Carrier D (CERAMENT™V) | 7.3 ± 0.3 | 5.8 ± 0.4 | 11.5 ± 0.8 | 9.3 ± 0.6 | 5.4 ± 0.4 | 2.4 ± 0.2 | 1.1 ± 0.1 | 0.4 ± 0.05 | 0.1 ± 0.01 | F(8, 24) = 521.8 p < 0.001 |
| Carrier A | Carrier B | Carrier C | Carrier D | |
|---|---|---|---|---|
| Product | OSmycin V® | OSpure™ | STIMULAN® | CERAMENT™V |
| Volume per sample | 5 mL | 5 mL | 5 mL | 5 mL |
| Weight per sample | 2.0 g | 1.5 g | 5.0 g | 5.5 g |
| Vancomycin per sample | 1.1 g | 0.83 g | 0.305 g | 0.247 g |
| Vancomycin per 1 g carrier | 0.55 g | 0.55 g | 0.06 g | 0.045 g |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smolle, M.A.; Murtezai, H.; Niedrist, T.; Amerstorfer, F.; Hörlesberger, N.; Leitner, L.; Klim, S.M.; Glehr, R.; Ahluwalia, R.; Leithner, A.; et al. Vancomycin Elution Kinetics of Four Antibiotic Carriers Used in Orthopaedic Surgery: In Vitro Study over 42 Days. Antibiotics 2023, 12, 1636. https://doi.org/10.3390/antibiotics12111636
Smolle MA, Murtezai H, Niedrist T, Amerstorfer F, Hörlesberger N, Leitner L, Klim SM, Glehr R, Ahluwalia R, Leithner A, et al. Vancomycin Elution Kinetics of Four Antibiotic Carriers Used in Orthopaedic Surgery: In Vitro Study over 42 Days. Antibiotics. 2023; 12(11):1636. https://doi.org/10.3390/antibiotics12111636
Chicago/Turabian StyleSmolle, Maria Anna, Hana Murtezai, Tobias Niedrist, Florian Amerstorfer, Nina Hörlesberger, Lukas Leitner, Sebastian Martin Klim, Reingard Glehr, Raju Ahluwalia, Andreas Leithner, and et al. 2023. "Vancomycin Elution Kinetics of Four Antibiotic Carriers Used in Orthopaedic Surgery: In Vitro Study over 42 Days" Antibiotics 12, no. 11: 1636. https://doi.org/10.3390/antibiotics12111636
APA StyleSmolle, M. A., Murtezai, H., Niedrist, T., Amerstorfer, F., Hörlesberger, N., Leitner, L., Klim, S. M., Glehr, R., Ahluwalia, R., Leithner, A., & Glehr, M. (2023). Vancomycin Elution Kinetics of Four Antibiotic Carriers Used in Orthopaedic Surgery: In Vitro Study over 42 Days. Antibiotics, 12(11), 1636. https://doi.org/10.3390/antibiotics12111636








