Efficacy of Chlorhexidine after Oral Surgery Procedures on Wound Healing: Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Study Selection Process
2.5. Data Extraction
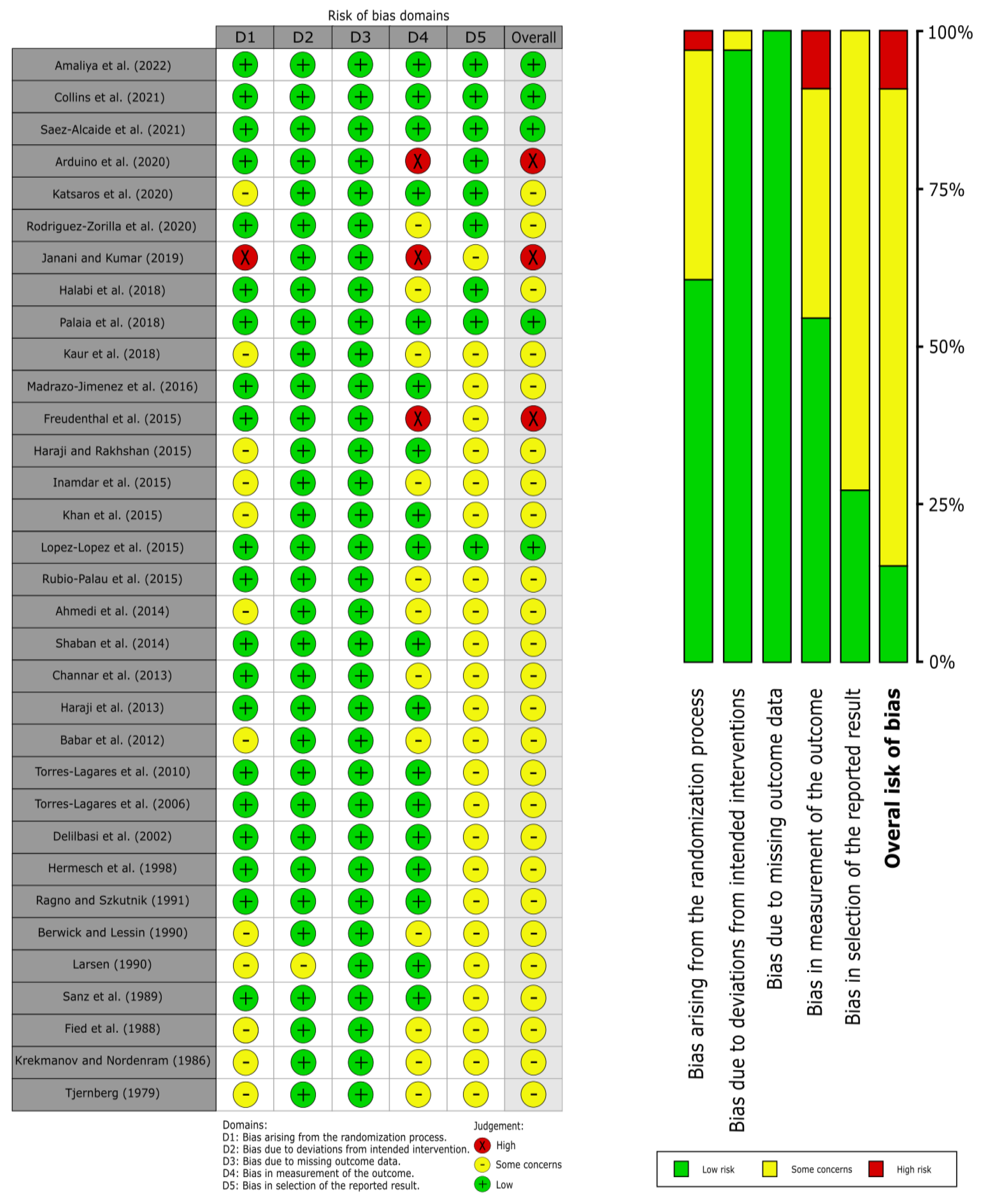
2.6. Evaluation of Quality and Risk of Bias
2.7. Statistical Analysis
3. Results
3.1. Results of the Literature Search
3.2. Study Characteristics
3.3. Qualitative Evaluation
3.4. Quantitative Evaluation
3.4.1. Meta-Analysis on Wound Healing
3.4.2. Meta-Analysis on Alveolar Osteitis
3.4.3. Meta-Analysis on Erythema
3.4.4. Meta-Analysis on Epithelization
3.4.5. Meta-Analysis on Pain during Wound Healing
3.4.6. Small-Study Effects Analysis
| Pooled Data | Heterogeneity | |||||||
|---|---|---|---|---|---|---|---|---|
| Meta-Analyses | No. of Studies * | No. of Cases * | Stat. Model | Wt | ES (95% CI) | p-Value | phet | I2 (%) |
| Wound healing | ||||||||
| all (poor vs. better wound healing) a | 8 | 771 | FEM | M-H | RR = 0.66 (0.55 to 0.80) | <0.001 | <0.001 | 85.9 |
| Subgroup analysis by type of intervention b | <0.001 c | |||||||
| CHX single | 4 | 527 | FEM | M-H | RR = 1.10 (0.87 to 1.40) | 0.43 | 0.02 | 71.3 |
| CHX + chitosan | 4 | 244 | FEM | M-H | RR = 0.25 (0.17 to 0.37) | <0.001 | 0.02 | 70.8 |
| Subgroup analysis by type of vehicle b | <0.001 c | |||||||
| CHX gel | 5 | 272 | FEM | M-H | RR = 0.26 (0.18 to 0.37) | <0.001 | 0.04 | 60.1 |
| CHX rinse | 3 | 499 | FEM | M-H | RR = 1.14 (0.90 to 1.45) | 0.28 | 0.01 | 77 |
| Subgroup analysis by type of concentration b | <0.001 c | |||||||
| CHX 0.12% | 1 | 239 | — | — | RR = 1.59 (1.16 to 2.19) | 0.004 | — | — |
| CHX 0.20% | 7 | 532 | FEM | M-H | RR = 0.41 (0.32 to 0.53) | <0.001 | 0.007 | 66.0 |
| Subgroup analysis by type of oral surgery | <0.001 c | |||||||
| biopsy | 2 | 474 | FEM | M-H | RR = 1.18 (0.92 to 1.51) | 0.20 | 0.005 | 87.0 |
| third molar | 6 | 297 | FEM | M-H | RR = 0.29 (0.21 to 0.41) | <0.001 | 0.02 | 62.2 |
| Subgroup analysis by study design | 0.09 c | |||||||
| Parallel-group design | 6 | 696 | FEM | M-H | RR = 0.70 (0.57 to 0.86) | 0.001 | <0.001 | 88.4 |
| Split-mouth design | 2 | 75 | FEM | M-H | RR = 0.41 (0.23 to 0.74) | 0.003 | 0.08 | 67.3 |
| Subgroup analysis by overall RoB | <0.001 c | |||||||
| Low | 2 | 166 | FEM | M-H | RR = 0.26 (0.17 to 0.40) | <0.001 | 0.002 | 89.3 |
| Some concerns | 3 | 106 | FEM | M-H | RR = 0.24 (0.11 to 0.53) | <0.001 | 0.83 | 0.0 |
| High | 3 | 166 | FEM | M-H | RR = 1.14 (0.90 to 1.45) | 0.28 | 0.01 | 77.0 |
| Alveolar osteitis | ||||||||
| All (alveolar osteitis vs. healing) a | 26 | 4205 | FEM | M-H | RR = 0.46 (0.39 to 0.53) | <0.001 | 0.36 | 7.1 |
| Subgroup analysis by type of intervention b | 0.17 c | |||||||
| CHX single | 21 | 3504 | FEM | M-H | RR = 0.49 (0.41 to 0.57) | <0.001 | 0.32 | 10.7 |
| CHX + antibiotics | 4 | 629 | FEM | M-H | RR = 0.35 (0.23 to 0.54) | <0.001 | 0.84 | 0.0 |
| CHX + chitosan | 1 | 72 | — | — | RR = 0.09 (0.01 to 1.59) | <0.001 | — | — |
| Subgroup analysis by type of vehicle b | <0.14 c | |||||||
| CHX gel | 13 | 1523 | FEM | M-H | RR = 0.40 (0.31 to 0.51) | <0.001 | 0.17 | 27.5 |
| CHX rinse | 13 | 2682 | FEM | M-H | RR = 0.50 (0.41 to 0.62) | <0.001 | 0.71 | 0.0 |
| Subgroup analysis by type of concentration b | 0.52 c | |||||||
| CHX 0.12% | 7 | 1936 | FEM | M-H | RR = 0.47 (0.37 to 0.59) | <0.001 | 0.78 | 0.0 |
| CHX 0.20% | 18 | 2219 | FEM | M-H | RR = 0.46 (0.37 to 0.57) | <0.001 | 0.18 | 23.6 |
| CHX 1% | 1 | 50 | — | — | RR = 0.14 (0.02 to 1.08) | 0.06 | — | — |
| Subgroup analysis by type of oral surgery b | 0.17 c | |||||||
| Third molar | 23 | 2992 | FEM | M-H | RR = 0.48 (0.40 to 0.56) | <0.001 | 0.33 | 9.4 |
| Simple extraction | 3 | 1213 | FEM | M-H | RR = 0.34 (0.21 to 0.54) | <0.001 | 0.92 | 0.0 |
| Subgroup analysis by study design | 0.051 c | |||||||
| Parallel-group design | 20 | 3363 | FEM | M-H | RR = 0.50 (0.42 to 0.60) | <0.001 | 0.39 | 5.4 |
| Split-mouth design | 6 | 842 | FEM | M-H | RR = 0.35 (0.25 to 0.48) | <0.001 | 0.75 | 0.0 |
| Subgroup analysis by overall RoB b | — | |||||||
| Low | 1 | 72 | — | — | RR = 0.09 (0.01 to 1.59) | 0.99 | — | — |
| Some concerns | 24 | 4038 | FEM | M-H | RR = 0.47 (0.38 to 0.52) | <0.001 | 0.64 | 0.0 |
| High | 1 | 95 | — | — | RR = 1.20 (0.55 to 2.62) | 0.65 | — | — |
| Erythema | ||||||||
| All (erythematous vs. better healing) a | 3 | 88 | FEM | M-H | RR = 0.60 (0.39 to 0.93) | 0.02 | 0.02 | 76.3 |
| Epithelization | ||||||||
| All (not-epithelized vs. epithelized) a | 5 | 140 | FEM | M-H | RR = 1.05 (0.77 to 1.42) | 0.76 | 0.06 | 55.6 |
| Dehiscence | ||||||||
| All (open vs. closed) | 1 | 25 | — | — | RR = 0.77 (0.33 to 1.79) | 0.55 | — | — |
| Pain | ||||||||
| All (absolute difference) a | 9 | 919 | REM | D-L | MD = −0.35 (−0.88 to 0.17) | 0.19 | <0.001 | 80.5 |
| Subgroup analysis by type of intervention b | 0.52 c | |||||||
| CHX single | 7 | 819 | REM | D-L | MD = −0.33 (−0.95 to 0.28) | 0.29 | <0.001 | 84.9 |
| CHX + chitosan | 2 | 100 | REM | D-L | MD = −0.63 (−1.26 to 0.01) | 0.052 | 0.40 | 0.0 |
| Subgroup analysis by type of vehicle b | <0.001 c | |||||||
| CHX gel | 5 | 378 | REM | D-L | MD = −0.97 (−1.26 to−0.68) | <0.001 | 0.72 | 0.0 |
| CHX rinse | 4 | 541 | REM | D-L | MD = 0.18 (−0.25 to 0.60) | 0.41 | 0.13 | 46.8 |
| Subgroup analysis by type of concentration b | 0.71 c | |||||||
| CHX 0.12% | 3 | 436 | REM | D-L | MD = −0.19 (−1.48 to 1.10) | 0.77 | <0.001 | 93.3 |
| CHX 0.20% | 6 | 483 | REM | D-L | MD = −0.45 (−0.95 to 0.05) | 0.08 | 0.05 | 56.0 |
| Subgroup analysis by type of oral surgery b | <0.001 c | |||||||
| Biopsy | 3 | 504 | REM | D-L | MD = 0.21 (−0.29 to 0.70) | 0.41 | 0.07 | 61.9 |
| Periodontal | 1 | 37 | — | — | MD = −0.14 (−1.35 to 1.07) | 0.82 | — | — |
| Third molar | 5 | 378 | REM | D-L | MD = −0.97 (−1.26 to −0.68) | <0.001 | 0.72 | 0.0 |
| Subgroup analysis by study design b | <0.001 c | |||||||
| Parallel-group design | 7 | 669 | REM | D-L | MD = −0.03 (−0.48 to 0.42) | 0.90 | 0.05 | 53.4 |
| Split-mouth design | 2 | 250 | REM | D-L | MD = −1.06 (−1.39 to −0.73) | <0.001 | 0.99 | 0.0 |
| Subgroup analysis by overall RoB b | <0.001 c | |||||||
| Low | 3 | 138 | REM | D-L | MD = −0.45 (−0.90 to −0.003) | 0.05 | 0.60 | 0.0 |
| Some concerns | 4 | 306 | REM | D-L | MD = −1.04 (−1.36 to −0.71) | <0.001 | 0.75 | 0.0 |
| High | 2 | 475 | REM | D-L | MD = 0.37 (−0.17 to 0.91) | 0.18 | 0.10 | 64.1 |
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Broughton, G.; Janis, J.E.; Attinger, C.E. Wound Healing: An Overview. Plast. Reconstr. Surg. 2006, 117, 1e-S–32e-S. [Google Scholar] [CrossRef] [PubMed]
- Politis, C.; Schoenaers, J.; Jacobs, R.; Agbaje, J.O. Wound Healing Problems in the Mouth. Front. Physiol. 2016, 7, 507. [Google Scholar] [CrossRef] [PubMed]
- Bielefeld, K.A.; Amini-Nik, S.; Alman, B.A. Cutaneous wound healing: Recruiting developmental pathways for regeneration. Cell. Mol. Life Sci. 2013, 70, 2059–2081. [Google Scholar] [CrossRef] [PubMed]
- Eming, S.A.; Martin, P.; Tomic-Canic, M. Wound repair and regeneration: Mechanisms, signaling, and translation. Sci. Transl. Med. 2014, 6, 265sr6. [Google Scholar] [CrossRef] [PubMed]
- González-Moles, M.Á.; Ramos-García, P. State of Evidence on Oral Health Problems in Diabetic Patients: A Critical Review of the Literature. J. Clin. Med. 2021, 10, 5383. [Google Scholar] [CrossRef] [PubMed]
- Loftus, M.J.; Peterson, L.J. Delayed healing of mandibular fracture in idiopathic myxedema. Oral Surg. Oral Med. Oral Pathol. 1979, 47, 233–237. [Google Scholar] [CrossRef] [PubMed]
- Aghaloo, T.; Pi-Anfruns, J.; Moshaverinia, A.; Sim, D.; Grogan, T.; Hadaya, D. The Effects of Systemic Diseases and Medications on Implant Osseointegration: A Systematic Review. Int. J. Oral Maxillofac. Implants 2019, 34, S35–S49. [Google Scholar] [CrossRef] [PubMed]
- Gál, P.; Brábek, J.; Holub, M.; Jakubek, M.; Šedo, A.; Lacina, L.; Strnadová, K.; Dubový, P.; Hornychová, H.; Ryška, A.; et al. Autoimmunity, cancer and COVID-19 abnormally activate wound healing pathways: Critical role of inflammation. Histochem. Cell Biol. 2022, 158, 415–434. [Google Scholar] [CrossRef]
- Kalyan, S.; Wang, J.; Quabius, E.S.; Huck, J.; Wiltfang, J.; Baines, J.F.; Kabelitz, D. Systemic immunity shapes the oral microbiome and susceptibility to bisphosphonate-associated osteonecrosis of the jaw. J. Transl. Med. 2015, 13, 212. [Google Scholar] [CrossRef]
- Vellappally, S.; Fiala, Z.; Smejkalová, J.; Jacob, V.; Somanathan, R. Smoking related systemic and oral diseases. Acta Medica-Hradec Kral. 2007, 50, 161–166. [Google Scholar] [CrossRef][Green Version]
- Hampton, S. Bacteria and wound healing. J. Community Nurs. 2007, 21, 32–40. [Google Scholar]
- Jones, S.G.; Edwards, R.; Thomas, D.W. Inflammation and Wound Healing: The Role of Bacteria in the Immuno-Regulation of Wound Healing. Int. J. Low. Extrem. Wounds 2004, 3, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Robson, M.C. Wound infection. Surg. Clin. N. Am. 1997, 77, 637–650. [Google Scholar] [CrossRef]
- Bolton, L.L.; van Rijswijk, L.; Shaffer, F.A. Quality wound care equals cost-effective wound care: A clinical model. Adv. Wound Care 1997, 10, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Steed, D.L.; Attinger, C.; Colaizzi, T.; Crossland, M.; Franz, M.; Harkless, L.; Johnson, A.; Moosa, H.; Robson, M.; Serena, T.; et al. Guidelines for the treatment of diabetic ulcers. Wound Repair Regen. 2006, 14, 680–692. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Drada, J.A.; García-Perdomo, H.A. Effectiveness of Antimicrobial Prophylaxis in Preventing the Spread of Infection as a Result of Oral Procedures: A Systematic Review and Meta-Analysis. J. Oral Maxillofac. Surg. 2016, 74, 1313–1321. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; Aggarwal, V.R.; Moore, R. Aetiology, Prevention and Management of Alveolar Osteitis—A Scoping Review. J. Oral Rehabil. 2022, 49, 103–113. [Google Scholar] [CrossRef] [PubMed]
- Au, A.H.Y.; Choi, S.W.; Cheung, C.W.; Leung, Y.Y. The Efficacy and Clinical Safety of Various Analgesic Combinations for Post-Operative Pain after Third Molar Surgery: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0127611. [Google Scholar] [CrossRef]
- Bouloux, G.F.; Steed, M.B.; Perciaccante, V.J. Complications of Third Molar Surgery. Oral Maxillofac. Surg. Clin. N. Am. 2007, 19, 117–128. [Google Scholar] [CrossRef]
- Belusic-Gobic, M.; Car, M.; Juretic, M.; Cerovic, R.; Gobic, D.; Golubovic, V. Risk factors for wound infection after oral cancer surgery. Oral Oncol. 2007, 43, 77–81. [Google Scholar] [CrossRef]
- Cho, H.; Lynham, A.J.; Hsu, E. Postoperative interventions to reduce inflammatory complications after third molar surgery: Review of the current evidence. Aust. Dent. J. 2017, 62, 412–419. [Google Scholar] [CrossRef]
- Zhu, J.; Zhang, S.; Yuan, X.; He, T.; Liu, H.; Wang, J.; Xu, B. Effect of platelet-rich fibrin on the control of alveolar osteitis, pain, trismus, soft tissue healing, and swelling following mandibular third molar surgery: An updated systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2021, 50, 398–406. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L. Chlorhexidine Gel Use in the Oral District: A Systematic Review. Gels 2019, 5, 31. [Google Scholar] [CrossRef] [PubMed]
- Fine, D.H. Mouthrinses as adjuncts for plaque and gingivitis management. A status report for the American Journal of Dentistry. Am. J. Dent. 1988, 1, 259–263. [Google Scholar] [PubMed]
- Hugo, W.B.; Longworth, A.R. The effect of chlorhexidine on the electrophoretic mobility, cytoplasmic constituents, dehydrogenase activity and cell walls of Escherichia coli and Staphylococcus aureus. J. Pharm. Pharmacol. 1966, 18, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Pérez, M.; Bravo-Pérez, M.; Sánchez-López, J.-D.; Muñoz-Soto, E.; Romero-Olid, M.-N.; Baca-García, P. Effectiveness of 1% versus 0.2% chlorhexidine gels in reducing alveolar osteitis from mandibular third molar surgery: A randomized, double-blind clinical trial. Med. Oral Patol. Oral Cir. Bucal 2013, 18, e693–e700. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series; Wiley and Sons: Hoboken, NJ, USA, 2008; pp. 1–649. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. PRISMA-P Group Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Torres-Lagares, D.; Gutierrez-Perez, J.L.; Infante-Cossio, P.; Garcia-Calderon, M.; Romero-Ruiz, M.M.; Serrera-Figallo, M.A. Randomized, double-blind study on effectiveness of intra-alveolar chlorhexidine gel in reducing the incidence of alveolar osteitis in mandibular third molar surgery. Int. J. Oral Maxillofac. Surg. 2006, 35, 348–351. [Google Scholar] [CrossRef] [PubMed]
- Berwick, J.E.; Lessin, M.E. Effects of a chlorhexidine gluconate oral rinse on the incidence of alveolar osteitis in mandibular third molar surgery. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1990, 48, 444–448. [Google Scholar] [CrossRef] [PubMed]
- Freudenthal, N.; Sternudd, M.; Jansson, L.; Wannfors, K. A double-blind randomized study evaluating the effect of intra-alveolar chlorhexidine gel on alveolar osteitis after removal of mandibular third molars. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2015, 73, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Tjernberg, A. Influence of oral hygiene measures on the development of alveolitis sicca dolorosa after surgical removal of mandibular third molars. Int. J. Oral Surg. 1979, 8, 430–434. [Google Scholar] [CrossRef]
- Sáez-Alcaide, L.; Molinero-Mourelle, P.; González-Serrano, J.; Rubio-Alonso, L.; Bornstein, M.; López-Quiles, J. Efficacy of a topical gel containing chitosan, chlorhexidine, allantoin and dexpanthenol for pain and inflammation control after third molar surgery: A randomized and placebo-controlled clinical trial. Med. Oral Patol. Oral Cir. Bucal 2020, 25, e644–e651. [Google Scholar] [CrossRef]
- Rodríguez Zorrilla, S.; Blanco Carrión, A.; García García, A.; Galindo Moreno, P.; Marichalar Mendía, X.; Seoane Prado, R.; Pérez Estévez, A.J.; Pérez-Sayáns, M. Effect of antiseptic gels in the microbiologic colonization of the suture threads after oral surgery. Sci. Rep. 2020, 10, 8360. [Google Scholar] [CrossRef] [PubMed]
- Lope-Lopez, J.; Jan-Palli, E.; Gonzalez-Navarro, B.; Jane-Salas, E.; Estrugo-Devesa, A.; Milani, M.; Lopez-Lopez, J.; Jan-Pallí, E.; lez-Navarro, B.G.; Jané-Salas, E.; et al. Efficacy of chlorhexidine, dexpanthenol, allantoin and chitosan gel in comparison with bicarbonate oral rinse in controlling post-interventional inflammation, pain and cicatrization in subjects undergoing dental surgery. Curr. Med. Res. Opin. 2015, 31, 2179–2183. [Google Scholar] [CrossRef] [PubMed]
- Amaliya, A.; Ramadhanti, R.; Hadikrishna, I.; Maulina, T. The Effectiveness of 0.2% Chlorhexidine Gel on Early Wound Healing after Tooth Extraction: A Randomized Controlled Trial. Eur. J. Dent. 2022, 16, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Haraji, A.; Rakhshan, V.; Khamverdi, N.; Alishahi, H.K. Effects of intra-alveolar placement of 0.2% chlorhexidine bioadhesive gel on dry socket incidence and postsurgical pain: A double-blind split-mouth randomized controlled clinical trial. J. Orofac. Pain 2013, 27, 256–262. [Google Scholar] [CrossRef] [PubMed]
- Delilbasi, C.; Saracoglu, U.; Keskin, A. Effects of 0.2% chlorhexidine gluconate and amoxicillin plus clavulanic acid on the prevention of alveolar osteitis following mandibular third molar extractions. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2002, 94, 301–304. [Google Scholar] [CrossRef] [PubMed]
- Halabi, D.; Escobar, J.; Alvarado, C.; Martinez, N.; Muñoz, C. Chlorhexidine for prevention of alveolar osteitis: A randomised clinical trial. J. Appl. Oral Sci. 2018, 26, e20170245. [Google Scholar] [CrossRef] [PubMed]
- Palaia, G.; Tenore, G.; Tribolati, L.; Russo, C.; Gaimari, G.; Del Vecchio, A.; Romeo, U. Evaluation of wound healing and postoperative pain after oral mucosa laser biopsy with the aid of compound with chlorhexidine and sodium hyaluronate: A randomized double blind clinical trial. Clin. Oral Investig. 2019, 23, 3141–3151. [Google Scholar] [CrossRef] [PubMed]
- Ahmedi, J.; Ahmedi, E.; Agani, Z.; Hamiti, V.; Reçica, B.; Tmava-Dragusha, A. The Efficacy of 1% Chlorhexidine Gel on the Reduction of Dry Socket Occurence Following Surgical Third Molar Extraction—Pilot Study. Open J. Stomatol. 2014, 4, 152–160. [Google Scholar] [CrossRef]
- Kaur, J.; Raval, R.; Bansal, A.; Kumawat, V. Repercussions of intraalveolar placement of combination of 0.2% chlorhexidine & 10 Mg metronidazole gel on the occurrence of dry sockets—A randomized control trial. J. Clin. Exp. Dent. 2017, 9, e284–e288. [Google Scholar] [CrossRef]
- Katsaros, T.; Mayer, E.; Palaiologou, A.; Romero-Bustillos, M.; Evans, G.H.; Lallier, T.E.; Maney, P. Effect of different concentrations of commercially available mouthwashes on wound healing following periodontal surgery: A randomized controlled clinical trial. Clin. Oral Investig. 2020, 24, 3587–3595. [Google Scholar] [CrossRef]
- Larsen, P.E. The effect of a chlorhexidine rinse on the incidence of alveolar osteitis following the surgical removal of impacted mandibular third molars. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 1991, 49, 932–937. [Google Scholar] [CrossRef] [PubMed]
- Ragno, J.R.J.; Szkutnik, A.J. Evaluation of 0.12% chlorhexidine rinse on the prevention of alveolar osteitis. Oral Surg. Oral Med. Oral Pathol. 1991, 72, 524–526. [Google Scholar] [CrossRef] [PubMed]
- Babar, A.; Ibrahim, M.W.; Baig, N.J.; Shah, I.; Amin, E. Efficacy of intra-alveolar chlorhexidine gel in reducing frequency of alveolar osteitis in mandibular third molar surgery. J. Coll. Physicians Surg. Pak. 2012, 22, 91–94. [Google Scholar]
- Arduino, P.G.; Gambino, A.; Cabras, M.; Sciannameo, V.; Nimot, Y.; Karimi, D.; Ricceri, F.; Broccoletti, R. Effect of two different alcohol-free chlorhexidine formulations in mouthrinses on the immediate postoperative period for oral mucosal biopsies. J. Oral Sci. 2020, 62, 202–205. [Google Scholar] [CrossRef] [PubMed]
- Madrazo-Jimenez, M.; Rodriguez-Caballero, A.; Serrera-Figallo, M.A.; Garrido-Serrano, R.; Gutierrez-Corrales, A.; Gutierrez-Perez, J.L.; Torres-Lagares, D. The effects of a topical gel containing chitosan, 0,2% chlorhexidine, allantoin and despanthenol on the wound healing process subsequent to impacted lower third molar extraction. Med. Oral Patol. Oral Cir. Bucal 2016, 21, e696–e702. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Khan, M.A.; Bashir, S.; Khan, F.R.; Umer, F.; Haider, S.M.; Hasan, T. Clinical efficacy of single dose chlorhexidine gel application in molars extractions-a randomized clinical trial. J. Pakistan Dent. Assoc. 2015, 24, 175–181. [Google Scholar]
- Inamdar, M.N.; Chauhan, R.; Mapare, S.A.; Goswami, R.P.; Goswami, Y.; Khadri, S.F. Prevention of Dry Socket using Chlorhexidine Gel and Ornidazole Gel in Impacted Mandibular Third Molar: A Comparative Randomized Prospective Study on 30 Patients. J. Int. Oral Health 2015, 7, 41–46. [Google Scholar]
- Hermesch, C.B.; Hilton, T.J.; Biesbrock, A.R.; Baker, R.A.; Cain-Hamlin, J.; McClanahan, S.F.; Gerlach, R.W. Perioperative use of 0.12% chlorhexidine gluconate for the prevention of alveolar osteitis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 1998, 85, 381–387. [Google Scholar] [CrossRef]
- Torres-Lagares, D.; Gutierrez-Perez, J.L.; Hita-Iglesias, P.; Magallanes-Abad, N.; Flores-Ruiz, R.; Basallote-Garcia, M.; Gonzalez-Martin, M. Randomized, double-blind study of effectiveness of intra-alveolar application of chlorhexidine gel in reducing incidence of alveolar osteitis and bleeding complications in mandibular third molar surgery in patients with bleeding disorders. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2010, 68, 1322–1326. [Google Scholar] [CrossRef]
- Sanz, M.; Newman, M.G.; Anderson, L.; Matoska, W.; Otomo—Corgel, J.; Saltini, C. Clinical Enhancement of Post-Periodontal Surgical Therapy by a 0.12% Chlorhexidine Gluconate Mouthrinse. J. Periodontol. 1989, 60, 570–576. [Google Scholar] [CrossRef]
- Krekmanov, L.; Nordenram, Å. Postoperative complications after surgical removal of mandibular third molars. Int. J. Oral Maxillofac. Surg. 1986, 15, 25–29. [Google Scholar] [CrossRef]
- Shaban, B.; Azimi, H.R.; Naderi, H.; Janani, A.; Zarrabi, M.J.; Nejat, A.H. Effect of 0.2% Chlorhexidine Gel on Frequency of Dry Socket Following Mandibular Third Molar Surgery: A Double-Blind Clinical Trial. J. Dent. Mater. Tech. 2014, 3, 175–184. [Google Scholar]
- Collins, J.R.; Veras, K.; Hernández, M.; Hou, W.; Hong, H.; Romanos, G.E. Anti-inflammatory effect of salt water and chlorhexidine 0.12% mouthrinse after periodontal surgery: A randomized prospective clinical study. Clin. Oral Investig. 2021, 25, 4349–4357. [Google Scholar] [CrossRef] [PubMed]
- Channar, K.; Dall, A.; Memon, A.; Lal, R. Prevention of alveolar osteitis in surgical removal of lower third molar. Pak. Oral Dent. J. 2013, 3, 244–248. [Google Scholar]
- Rubio-Palau, J.; Garcia-Linares, J.; Hueto-Madrid, J.-A.; González-Lagunas, J.; Raspall-Martin, G.; Mareque-Bueno, J. Effect of intra-alveolar placement of 0.2% chlorhexidine bioadhesive gel on the incidence of alveolar osteitis following the extraction of mandibular third molars. A double-blind randomized clinical trial. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e117. [Google Scholar] [CrossRef]
- Janani, K.; Kumar, M.P.S. Effectiveness of chlorhexidine and warm saline mouthrinses against bacterial colonization on silk suture material in third molar surgery—A clinico-microbiological study. Int. J. Clin. Dent. 2019, 12, 137–145. [Google Scholar]
- Haraji, A.; Rakhshan, V. Chlorhexidine gel and less difficult surgeries might reduce post-operative pain, controlling for dry socket, infection and analgesic consumption: A split-mouth controlled randomised clinical trial. J. Oral Rehabil. 2015, 42, 209–219. [Google Scholar] [CrossRef]
- Field, E.A.; Nind, D.; Varga, E.; Martin, M. V The effect of chlorhexidine irrigation on the incidence of dry socket: A pilot study. Br. J. Oral Maxillofac. Surg. 1988, 26, 395–401. [Google Scholar] [CrossRef]
- Canullo, L.; Laino, L.; Longo, F.; Filetici, P.; D’Onofrio, I.; Troiano, G. Does Chlorhexidine Prevent Complications in Extractive, Periodontal, and Implant Surgery? A Systematic Review and Meta-analysis with Trial Sequential Analysis. Int. J. Oral Maxillofac. Implants 2020, 35, 1149–1158. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, M.P.; Espiga, A.; Silva, D.; Baptista, P.; Henriques, J.; Ferreira, C.; Silva, J.C.; Borges, J.P.; Pires, E.; Chaves, P.; et al. Development of a new chitosan hydrogel for wound dressing. Wound Repair Regen. 2009, 17, 817–824. [Google Scholar] [CrossRef]
- Chatelet, C.; Damour, O.; Domard, A. Influence of the degree of acetylation on some biological properties of chitosan films. Biomaterials 2001, 22, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, M.; Ono, K.; Sato, M.; Nakanishi, K.; Saito, Y.; Yura, H.; Matsui, T.; Hattori, H.; Fujita, M.; Kikuchi, M.; et al. Acceleration of wound contraction and healing with a photocrosslinkable chitosan hydrogel. Wound Repair Regen. 2001, 9, 513–521. [Google Scholar] [CrossRef] [PubMed]
- Kratz, G.; Back, M.; Arnander, C.; Larm, O. Immobilised heparin accelerates the healing of human wounds in vivo. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1998, 32, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, M.; Nakanishi, K.; Ono, K.; Sato, M.; Kikuchi, M.; Saito, Y.; Yura, H.; Matsui, T.; Hattori, H.; Uenoyama, M.; et al. Photocrosslinkable chitosan as a dressing for wound occlusion and accelerator in healing process. Biomaterials 2002, 23, 833–840. [Google Scholar] [CrossRef] [PubMed]
- Hoemann, C.D.; Sun, J.; Légaré, A.; McKee, M.D.; Buschmann, M.D. Tissue engineering of cartilage using an injectable and adhesive chitosan-based cell-delivery vehicle. Osteoarthr. Cartil. 2005, 13, 318–329. [Google Scholar] [CrossRef] [PubMed]
- Vescovali, C.; Damour, O.; Shahabedin, L.; David, M. Epidermalization of an artificial dermis made of collagen. Ann. Mediterrian Burn. Club 1989, 2, 137139. [Google Scholar]
- Damour, O.; Gueugniaud, P.Y.; Berthin-Maghit, M.; Rousselle, P.; Berthod, F.; Sahuc, F.; Collombel, C. A dermal substrate made of collagen-GAG-chitosan for deep burn coverage: First clinical uses. Clin. Mater. 1994, 15, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Azad, A.K.; Sermsintham, N.; Chandrkrachang, S.; Stevens, W.F. Chitosan membrane as a wound-healing dressing: Characterization and clinical application. J. Biomed. Mater. Res. B Appl. Biomater. 2004, 69, 216–222. [Google Scholar] [CrossRef]
- Stone, C.A.; Wright, H.; Clarke, T.; Powell, R.; Devaraj, V.S. Healing at skin graft donor sites dressed with chitosan. Br. J. Plast. Surg. 2000, 53, 601–606. [Google Scholar] [CrossRef]
- Yengopal, V.; Mickenautsch, S. Chlorhexidine for the prevention of alveolar osteitis. Int. J. Oral Maxillofac. Surg. 2012, 41, 1253–1264. [Google Scholar] [CrossRef]
- Teshome, A. The efficacy of chlorhexidine gel in the prevention of alveolar osteitis after mandibular third molar extraction: A systematic review and meta-analysis. BMC Oral Health 2017, 17, 82. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Hu, B.; Liu, Y.; Yang, Z.; Song, J. The efficacy of intra-alveolar 0.2% chlorhexidine gel on alveolar osteitis: A meta-analysis. Oral Dis. 2017, 23, 598–608. [Google Scholar] [CrossRef]
- Taberner-Vallverdú, M.; Sánchez-Garcés, M.-Á.; Gay-Escoda, C. Efficacy of different methods used for dry socket prevention and risk factor analysis: A systematic review. Med. Oral Patol. Oral Cir. Bucal 2017, 22, e750–e758. [Google Scholar] [CrossRef]
- Wang, C.-H.; Yang, S.-H.; Jen, H.-J.; Tsai, J.-C.; Lin, H.-K.; Loh, E.-W. Preventing Alveolar Osteitis After Molar Extraction Using Chlorhexidine Rinse and Gel: A Meta-Analysis of Randomized Controlled Trials. J. Nurs. Res. 2020, 29, e137. [Google Scholar] [CrossRef]
- Kolokythas, A.; Olech, E.; Miloro, M. Alveolar Osteitis: A Comprehensive Review of Concepts and Controversies. Int. J. Dent. 2010, 2010, 249073. [Google Scholar] [CrossRef]
- Blum, I.R. Contemporary views on dry socket (alveolar osteitis): A clinical appraisal of standardization, aetiopathogenesis and management: A critical review. Int. J. Oral Maxillofac. Surg. 2002, 31, 309–317. [Google Scholar] [CrossRef] [PubMed]


| Total | 33 Studies |
|---|---|
| Year of publication | 1979–2022 |
| Number of cases | |
| Total | 4766 cases |
| Intervention group | 2525 cases |
| Control group | 2241 cases |
| Sample size, range | 20 to 744 cases |
| Type of interventions * | |
| CHX | 31 studies |
| CHX + chitosan | 4 studies |
| CHX + antibiotics | 4 studies |
| Type of CHX vehicles * | |
| Gel | 18 studies |
| Rinse | 21 studies |
| Type of CHX concentrations * | |
| 1% | 1 study |
| 0.20% | 26 studies |
| 0.12% | 11 studies |
| 0.006% | 1 study |
| Type of oral surgery procedures * | |
| Third molar surgery | 28 studies |
| Simple tooth extraction | 4 studies |
| Periodontal surgery | 4 studies |
| Oral biopsy | 3 studies |
| Type of study design * | |
| Parallel group design | 31 studies |
| Split-mouth design | 8 studies |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero-Olid, M.d.N.; Bucataru, E.; Ramos-García, P.; González-Moles, M.Á. Efficacy of Chlorhexidine after Oral Surgery Procedures on Wound Healing: Systematic Review and Meta-Analysis. Antibiotics 2023, 12, 1552. https://doi.org/10.3390/antibiotics12101552
Romero-Olid MdN, Bucataru E, Ramos-García P, González-Moles MÁ. Efficacy of Chlorhexidine after Oral Surgery Procedures on Wound Healing: Systematic Review and Meta-Analysis. Antibiotics. 2023; 12(10):1552. https://doi.org/10.3390/antibiotics12101552
Chicago/Turabian StyleRomero-Olid, María de Nuria, Elena Bucataru, Pablo Ramos-García, and Miguel Ángel González-Moles. 2023. "Efficacy of Chlorhexidine after Oral Surgery Procedures on Wound Healing: Systematic Review and Meta-Analysis" Antibiotics 12, no. 10: 1552. https://doi.org/10.3390/antibiotics12101552
APA StyleRomero-Olid, M. d. N., Bucataru, E., Ramos-García, P., & González-Moles, M. Á. (2023). Efficacy of Chlorhexidine after Oral Surgery Procedures on Wound Healing: Systematic Review and Meta-Analysis. Antibiotics, 12(10), 1552. https://doi.org/10.3390/antibiotics12101552








