Effect of Tocilizumab on Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta or Omicron Variants: A Propensity-Matched Analysis in Nimes University Hospital, France
Abstract
1. Introduction
2. Results
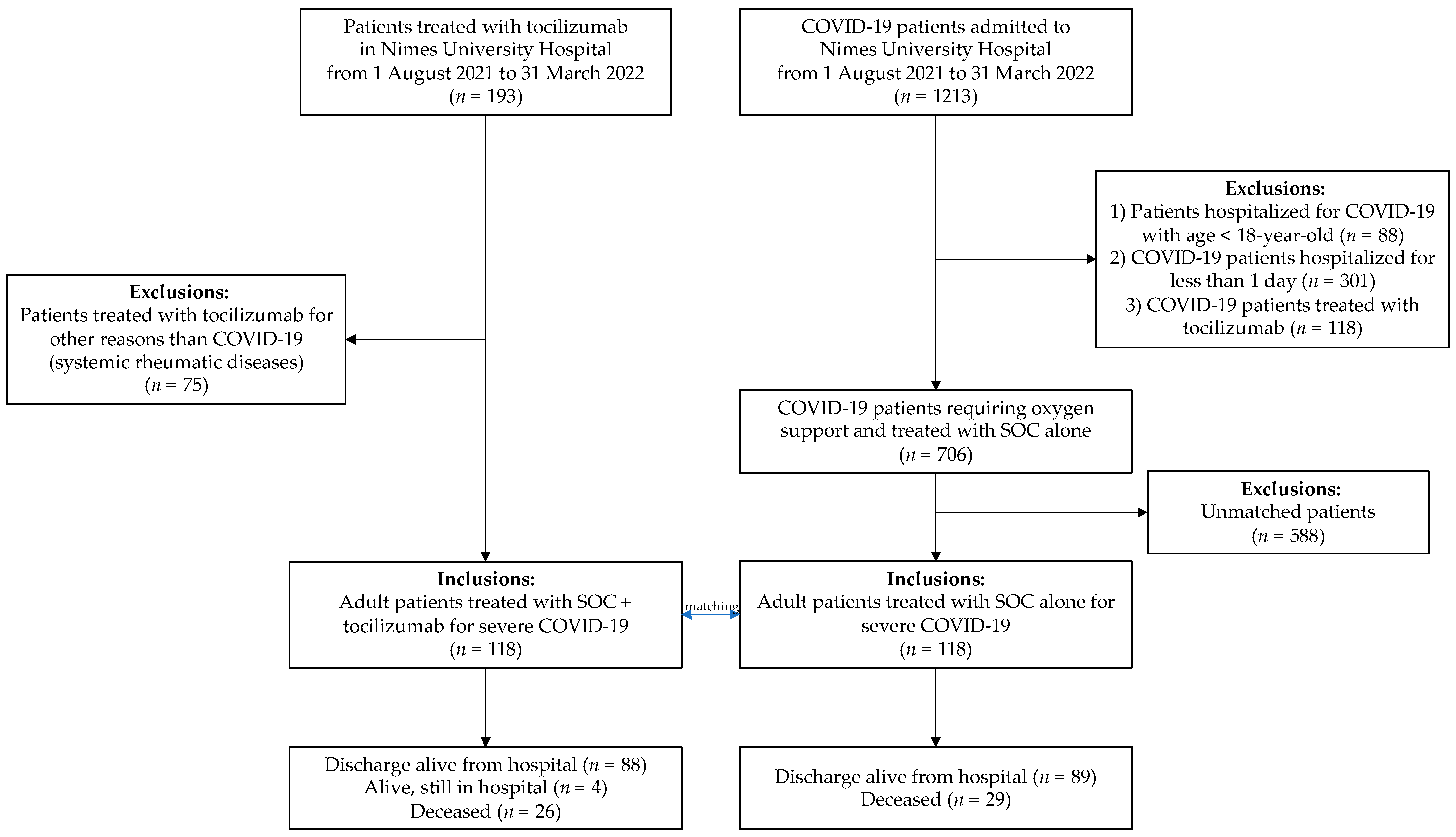
2.1. Population
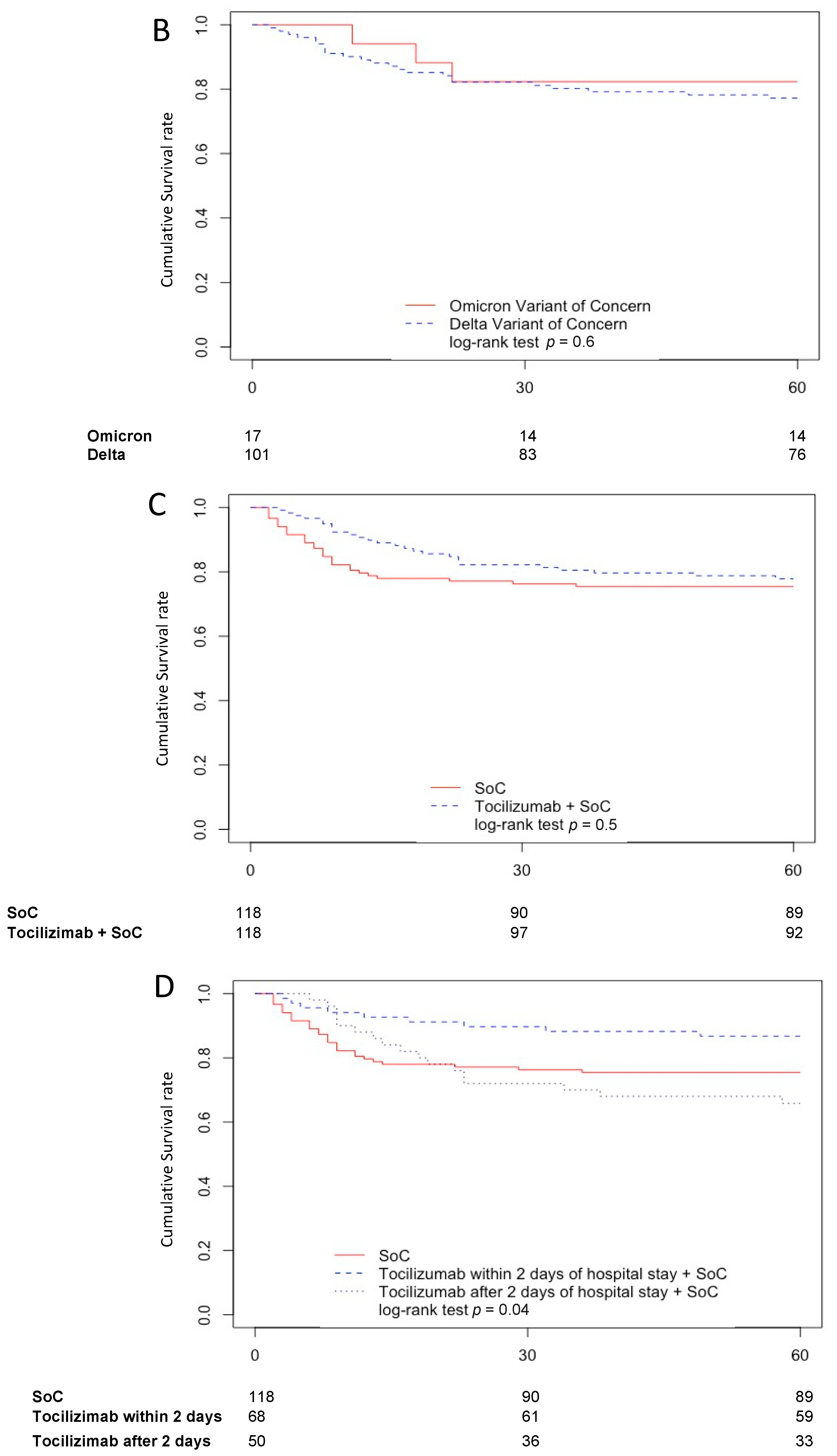
2.2. Outcomes
2.3. Factors Associated with Mortality
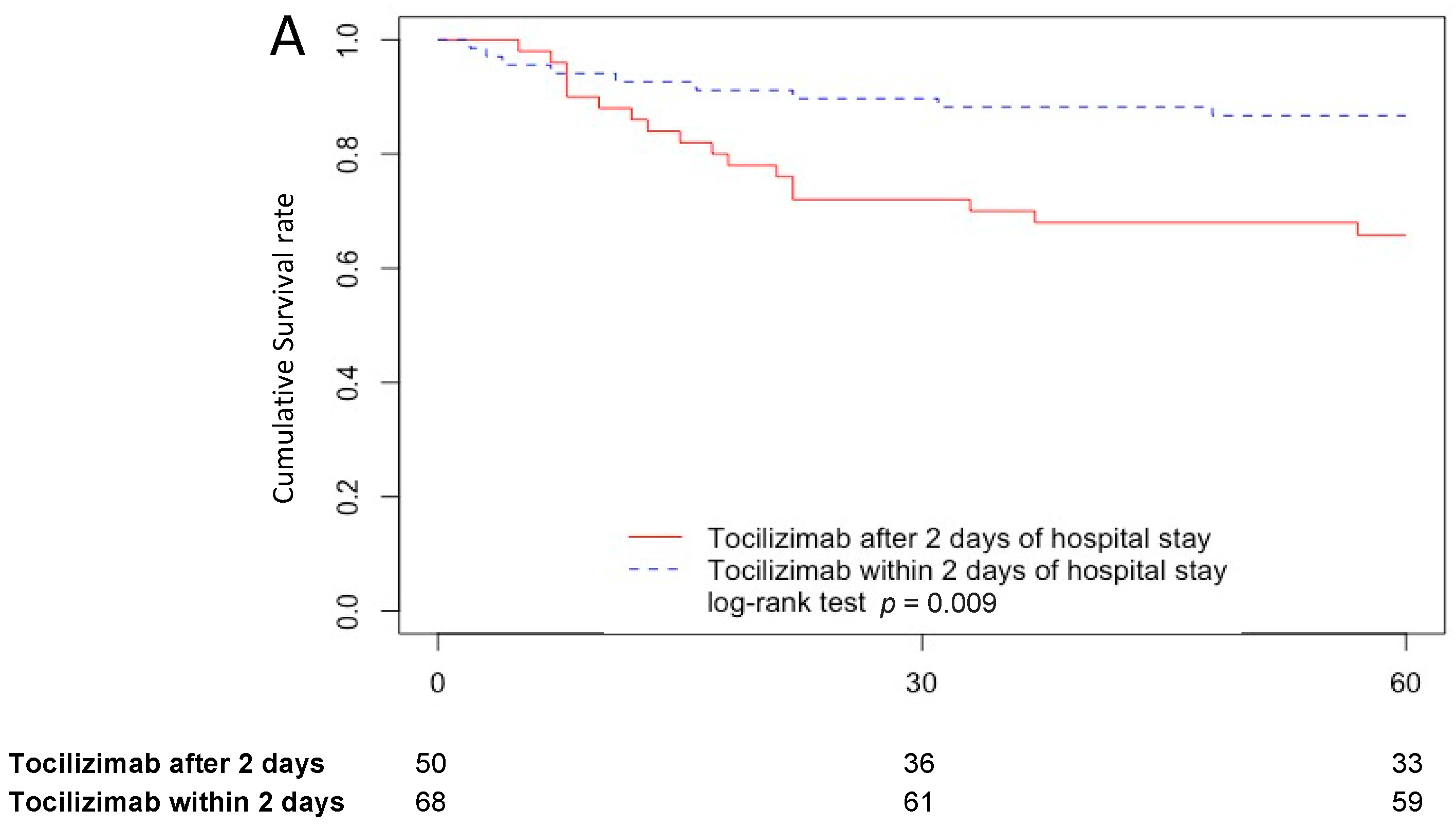
2.4. Tocilizumab Treatment Effect on Mortality
3. Discussion
4. Materials and Methods
4.1. Study Design and Settings
4.2. Tocilizumab Treatment
4.3. Patients
4.4. Data Collection
4.5. Outcomes
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Moore, J.B.; June, C.H. Cytokine Release Syndrome in Severe COVID-19. Science 2020, 368, 473–474. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Zhao, B.; Qu, Y.; Chen, Y.; Xiong, J.; Feng, Y.; Men, D.; Huang, Q.; Liu, Y.; Yang, B.; et al. Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated With Drastically Elevated Interleukin 6 Level in Critically Ill Patients with Coronavirus Disease 2019. Clin. Infect. Dis. 2020, 71, 1937–1942. [Google Scholar] [CrossRef] [PubMed]
- The RECOVERY Collaborative Group Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [CrossRef]
- Zhang, S.; Li, L.; Shen, A.; Chen, Y.; Qi, Z. Rational Use of Tocilizumab in the Treatment of Novel Coronavirus Pneumonia. Clin. Drug. Investig. 2020, 40, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Abani, O.; Abbas, A.; Abbas, F.; Abbas, M.; Abbasi, S.; Abbass, H.; Abbott, A.; Abdallah, N.; Abdelaziz, A.; Abdelfattah, M.; et al. Tocilizumab in Patients Admitted to Hospital with COVID-19 (RECOVERY): A Randomised, Controlled, Open-Label, Platform Trial. Lancet 2021, 397, 1637–1645. [Google Scholar] [CrossRef]
- The REMAP-CAP Investigators Interleukin-6 Receptor Antagonists in Critically Ill Patients with COVID-19. N. Engl. J. Med. 2021, 384, 1491–1502. [CrossRef]
- Cassone, G.; Dolci, G.; Besutti, G.; Braglia, L.; Pavone, P.; Corsini, R.; Sampaolesi, F.; Iotti, V.; Teopompi, E.; Massari, M.; et al. Predictive Factors of Clinical Outcomes in Patients with COVID-19 Treated with Tocilizumab: A Monocentric Retrospective Analysis. PLoS ONE 2022, 17, e0262908. [Google Scholar] [CrossRef]
- Radulescu, A.; Istrate, A.; Muntean, M. Treatment with Tocilizumab in Adult Patients with Moderate to Critical COVID-19 Pneumonia: A Single-Center Retrospective Study. Int. J. Infect. Dis. 2022, 117, 1–7. [Google Scholar] [CrossRef]
- Hafez, W.; Abdelrahman, A. Factors Influencing Disease Stability and Response to Tocilizumab Therapy in Severe COVID-19: A Retrospective Cohort Study. Antibiotics 2022, 11, 1078. [Google Scholar] [CrossRef]
- San-Juan, R.; Fernández-Ruiz, M.; López-Medrano, F.; Carretero, O.; Lalueza, A.; Maestro de la Calle, G.; Pérez-Jacoiste Asín, M.A.; Bueno, H.; Caro-Teller, J.M.; Catalán, M.; et al. Analysis of the Factors Predicting Clinical Response to Tocilizumab Therapy in Patients with Severe COVID-19. Int. J. Infect. Dis. 2022, 117, 56–64. [Google Scholar] [CrossRef]
- Nigo, M.; Rasmy, L.; May, S.B.; Rao, A.; Karimaghaei, S.; Kannadath, B.S.; De la Hoz, A.; Arias, C.A.; Li, L.; Zhi, D. Real World Long-Term Assessment of The Efficacy of Tocilizumab in Patients with COVID-19: Results from A Large De-Identified Multicenter Electronic Health Record Dataset in the United States. Int. J. Infect. Dis. 2021, 113, 148–154. [Google Scholar] [CrossRef] [PubMed]
- Writing Committee for the REMAP-CAP Investigators; Florescu, S.; Stanciu, D.; Zaharia, M.; Kosa, A.; Codreanu, D.; Kidwai, A.; Masood, S.; Kaye, C.; Coutts, A.; et al. Long-Term (180-Day) Outcomes in Critically Ill Patients With COVID-19 in the REMAP-CAP Randomized Clinical Trial. JAMA 2022. [Google Scholar] [CrossRef] [PubMed]
- Rezaei Tolzali, M.M.; Noori, M.; Shokri, P.; Rahmani, S.; Khanzadeh, S.; Nejadghaderi, S.A.; Fazlollahi, A.; Sullman, M.J.M.; Singh, K.; Kolahi, A.-A.; et al. Efficacy of Tocilizumab in the Treatment of COVID-19: An Umbrella Review. Rev. Med. Virol. 2022, 32, e2388. [Google Scholar] [CrossRef] [PubMed]
- Oliynyk, O.; Barg, W.; Oliynyk, Y.; Dubrov, S.; Gurianov, V.; Rorat, M. Lack of Difference in Tocilizumab Efficacy in the Treatment of Severe COVID-19 Caused by Different SARS-CoV-2 Variants. J. Pers. Med. 2022, 12, 1103. [Google Scholar] [CrossRef] [PubMed]
- Ullah, S.; Abid, R.; Haider, S.; Khuda, F.; Albadrani, G.M.; Abdulhakim, J.A.; Altyar, A.E.; Abdel-Daim, M.M.; Halimi, S.M.A.; Khalil, A.A.K. Assessment of Tocilizumab (Humanized Monoclonal Antibody) for Therapeutic Efficacy and Clinical Safety in Patients with Coronavirus Disease (COVID-19). Medicina 2022, 58, 1076. [Google Scholar] [CrossRef]
- Wolter, N.; Jassat, W.; Walaza, S.; Welch, R.; Moultrie, H.; Groome, M.; Amoako, D.G.; Everatt, J.; Bhiman, J.N.; Scheepers, C.; et al. Early Assessment of the Clinical Severity of the SARS-CoV-2 Omicron Variant in South Africa: A Data Linkage Study. Lancet 2022, 399, 437–446. [Google Scholar] [CrossRef]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors Associated with COVID-19-Related Death Using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef]
- Lv, F.; Gao, X.; Huang, A.H.; Zu, J.; He, X.; Sun, X.; Liu, J.; Gao, N.; Jiao, Y.; Keane, M.G.; et al. Excess Diabetes Mellitus-Related Deaths during the COVID-19 Pandemic in the United States. eClinicalMedicine 2022, 54, 100387. [Google Scholar] [CrossRef]
- Katz, A.; Altshuler, D.; Papadopoulos, J.; Amoroso, N.; Goldenberg, R.; Tarras, E.; Krolikowski, K.; Hagedorn, J.; Fridman, D.; Chen, X.J.C.; et al. The Use of High-Dose Corticosteroids Versus Low-Dose Corticosteroids with and without Tocilizumab in COVID-19 Acute Respiratory Distress Syndrome. Ann. Pharm. 2023, 57, 5–15. [Google Scholar] [CrossRef]
- Twohig, K.A.; Nyberg, T.; Zaidi, A.; Thelwall, S.; Sinnathamby, M.A.; Aliabadi, S.; Seaman, S.R.; Harris, R.J.; Hope, R.; Lopez-Bernal, J.; et al. Hospital Admission and Emergency Care Attendance Risk for SARS-CoV-2 Delta (B.1.617.2) Compared with Alpha (B.1.1.7) Variants of Concern: A Cohort Study. Lancet Infect. Dis. 2022, 22, 35–42. [Google Scholar] [CrossRef]
- Nyberg, T.; Ferguson, N.M.; Nash, S.G.; Webster, H.H.; Flaxman, S.; Andrews, N.; Hinsley, W.; Bernal, J.L.; Kall, M.; Bhatt, S.; et al. Comparative Analysis of the Risks of Hospitalisation and Death Associated with SARS-CoV-2 Omicron (B.1.1.529) and Delta (B.1.617.2) Variants in England: A Cohort Study. Lancet 2022, 399, 1303–1312. [Google Scholar] [CrossRef] [PubMed]
- Korobova, Z.R.; Arsentieva, N.A.; Liubimova, N.E.; Batsunov, O.K.; Dedkov, V.G.; Gladkikh, A.S.; Sharova, A.A.; Adish, Z.; Chernykh, E.I.; Kaschenko, V.A.; et al. Cytokine Profiling in Different SARS-CoV-2 Genetic Variants. Int. J. Mol. Sci. 2022, 23, 14146. [Google Scholar] [CrossRef] [PubMed]
- Richier, Q.; Jachiet, V.; Bonnemains, V.; Plaçais, L.; Abisror, N.; Garnier, M.; Pacanowski, J.; Dhote, R.; Hinchschberger, O.; Michel, M.; et al. Tocilizumab and COVID-19: Timing of Administration Assessment. Infect. Dis. Now 2022, 52, 31–34. [Google Scholar] [CrossRef]
- Stone, J.H.; Frigault, M.J.; Serling-Boyd, N.J.; Fernandes, A.D.; Harvey, L.; Foulkes, A.S.; Horick, N.K.; Healy, B.C.; Shah, R.; Bensaci, A.M.; et al. Efficacy of Tocilizumab in Patients Hospitalized with COVID-19. N. Engl. J. Med. 2020, 383, 2333–2344. [Google Scholar] [CrossRef] [PubMed]
- Rosas, I.O.; Bräu, N.; Waters, M.; Go, R.C.; Hunter, B.D.; Bhagani, S.; Skiest, D.; Aziz, M.S.; Cooper, N.; Douglas, I.S.; et al. Tocilizumab in Hospitalized Patients with Severe COVID-19 Pneumonia. N. Engl. J. Med. 2021, 384, 1503–1516. [Google Scholar] [CrossRef]
- Salama, C.; Han, J.; Yau, L.; Reiss, W.G.; Kramer, B.; Neidhart, J.D.; Criner, G.J.; Kaplan-Lewis, E.; Baden, R.; Pandit, L.; et al. Tocilizumab in Patients Hospitalized with COVID-19 Pneumonia. N. Engl. J. Med. 2021, 384, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, G.; Piraino, S.T.; Piticaru, J. Secondary Infection Risk in Patients with Severe COVID-19 Pneumonia Treated with Tocilizumab. Am. J. Ther. 2022, 29, e275–e278. [Google Scholar] [CrossRef]
- Prattes, J.; Wauters, J.; Giacobbe, D.R.; Salmanton-García, J.; Maertens, J.; Bourgeois, M.; Reynders, M.; Rutsaert, L.; Van Regenmortel, N.; Lormans, P.; et al. Risk Factors and Outcome of Pulmonary Aspergillosis in Critically Ill Coronavirus Disease 2019 Patients—A Multinational Observational Study by the European Confederation of Medical Mycology. Clin. Microbiol. Infect. 2021, 28, 580–587. [Google Scholar] [CrossRef]
- Ripa, M.; Galli, L.; Poli, A.; Oltolini, C.; Spagnuolo, V.; Mastrangelo, A.; Muccini, C.; Monti, G.; De Luca, G.; Landoni, G.; et al. Secondary Infections in Patients Hospitalized with COVID-19: Incidence and Predictive Factors. Clin. Microbiol. Infect. 2021, 27, 451–457. [Google Scholar] [CrossRef]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Westwood, D.; MacFadden, D.R.; Soucy, J.-P.R.; Daneman, N. Bacterial Co-Infection and Secondary Infection in Patients with COVID-19: A Living Rapid Review and Meta-Analysis. Clin. Microbiol. Infect. 2020, 26, 1622–1629. [Google Scholar] [CrossRef]
- Koehler, P.; Bassetti, M.; Chakrabarti, A.; Chen, S.C.A.; Colombo, A.L.; Hoenigl, M.; Klimko, N.; Lass-Flörl, C.; Oladele, R.O.; Vinh, D.C.; et al. Defining and Managing COVID-19-Associated Pulmonary Aspergillosis: The 2020 ECMM/ISHAM Consensus Criteria for Research and Clinical Guidance. Lancet Infect. Dis. 2021, 21, e149–e162. [Google Scholar] [CrossRef] [PubMed]
- Khurshid, S.; Rehman, N.; Ahmed, S.; Ahmad, B.; Khurshid, M.; Muhammad, A.; Siddiqi, F.A.; Nayab, D.; Saleem, H.; Saleem, Z. Early Fall in C-Reactive Protein (CRP) Level Predicts Response to Tocilizumab in Rapidly Progressing COVID-19: Experience in a Single-Arm Pakistani Center. Cureus 2021, 13, e20031. [Google Scholar] [CrossRef] [PubMed]
- Therapeutics and COVID-19: Living Guideline, 22 April 2022; World Health Organization: Geneva, Switzerland, 2022.
- Albuquerque, A.M.; Tramujas, L.; Sewanan, L.R.; Williams, D.R.; Brophy, J.M. Mortality Rates among Hospitalized Patients with COVID-19 Infection Treated with Tocilizumab and Corticosteroids: A Bayesian Reanalysis of a Previous Meta-Analysis. JAMA Netw. Open 2022, 5, e220548. [Google Scholar] [CrossRef] [PubMed]
- The WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group Association between Administration of IL-6 Antagonists and Mortality among Patients Hospitalized for COVID-19: A Meta-Analysis. JAMA 2021, 326, 499–518. [CrossRef]
- COVID-19 Treatment Guidelines Panel Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. Available online: https://www.covid19treatmentguidelines.nih.gov (accessed on 23 November 2022).
- European Centre for Disease Prevention and Control Strategies for the Surveillance of COVID-19 2020. Available online: https://www.ecdc.europa.eu/en/publications-data/strategies-surveillance-covid-19 (accessed on 23 November 2022).
- Ojha, V.; Mani, A.; Pandey, N.N.; Sharma, S.; Kumar, S. CT in Coronavirus Disease 2019 (COVID-19): A Systematic Review of Chest CT Findings in 4410 Adult Patients. Eur. Radiol. 2020, 30, 6129–6138. [Google Scholar] [CrossRef]
- International Classification of Diseases (ICD). Available online: https://www.who.int/standards/classifications/classification-of-diseases (accessed on 6 June 2022).
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Tawab, M.; Basha, M.A.A.; Mohamed, I.A.I.; Ibrahim, H.M. A Simple Chest CT Score for Assessing the Severity of Pulmonary Involvement in COVID-19. Egypt. J. Radiol. Nucl. Med. 2021, 52, 149. [Google Scholar] [CrossRef]
- Marshall, J.C.; Murthy, S.; Diaz, J.; Adhikari, N.K.; Angus, D.C.; Arabi, Y.M.; Baillie, K.; Bauer, M.; Berry, S.; Blackwood, B.; et al. A Minimal Common Outcome Measure Set for COVID-19 Clinical Research. Lancet Infect. Dis. 2020, 20, e192–e197. [Google Scholar] [CrossRef]

| Characteristics | Total (N = 118) | Survivor (N = 92) | Non-Survivor (N = 26) | p-Value |
|---|---|---|---|---|
| Age, years | 69 (56–77) | 64 (54–72) | 78 (71–84) | <0.001 * |
| Male | 79 (67%) | 61 (66%) | 18 (69%) | 0.78 |
| BMI, kg/m2 a | 28 (25–31) | 28 (25–31) | 27 (24–31) | 0.20 |
| Main comorbidities | ||||
| Diabetes | 36 (31%) | 24 (26%) | 12 (46%) | 0.05 |
| Myocardial ischemia | 18 (15%) | 9 (10%) | 9 (35%) | 0.003 * |
| Chronic heart failure | 5 (4%) | 2 (2%) | 3 (12%) | 0.06 |
| Chronic lung disease | 18 (15%) | 12 (13%) | 6 (23%) | 0.22 |
| Chronic kidney disease | 7 (6%) | 4 (4%) | 3 (12%) | 0.19 |
| Dementia | 5 (4%) | 1 (1%) | 4 (15%) | 0.01 * |
| Cancer | 19 (16%) | 11 (12%) | 8 (31%) | 0.03 * |
| Hemopathy b | 8 (7%) | 4 (4%) | 4 (15%) | 0.06 |
| Charlson index | 1 (0–2) | 1 (0–2) | 2.5 (1–5) | <0.001 * |
| Chest CT-Scan c | ||||
| Mild | 13 (11%) | 8 (9%) | 5 (19%) | 0.14 |
| Moderate | 72 (61%) | 59 (64%) | 13 (50%) | 0.2 |
| Severe | 24 (20%) | 18 (20%) | 6 (23%) | 0.7 |
| Critical | 8 (7%) | 6 (7%) | 2 (8%) | 0.83 |
| Variant of concern | ||||
| Delta | 101 (86%) | 78 (85%) | 23 (88%) | 0.64 |
| Omicron | 17 (14%) | 14 (15%) | 3 (12%) | 0.64 |
| Oxygen requirement | ||||
| Conventional oxygen therapy | 43 (36%) | 41 (45%) | 2 (8%) | 0.003 * |
| High-flow nasal canula | 57 (48%) | 39 (42%) | 18 (69%) | 0.02 * |
| Mechanical ventilation | 18 (15%) | 12 (13%) | 6 (23%) | 0.22 |
| ECMO d | 6 (5%) | 5 (5%) | 1 (4%) | 0.75 |
| WHO-CPS e at admission | 5 (5–6) | 5 (5–6) | 5 (5–6) | 0.66 |
| WHO-CPS at tocilizumab administration | 6 (5–6) | 5 (5–6) | 6 (5–6) | 0.047 * |
| Tocilizumab treatment | ||||
| Administration timing, days | 2 (2–4) | 2 (2–3) | 3.5 (2–5) | 0.002 * |
| Administration within 2 days | 68 (58%) | 59 (64%) | 9 (35%) | 0.009 * |
| Inflammation biomarker | ||||
| CRP pre-tocilizumab, mg/L | 124 (89–165) | 128 (91–166) | 103 (77–162) | 0.45 |
| CRP post-tocilizumab, mg/L | 47 (23–89) | 47 (23–81) | 54 (24–95) | 0.25 |
| Outcomes | ||||
| Death at day 60 | 26 (22%) | - | - | |
| ICU f admission | 56 (47%) | 39 (42%) | 17 (65%) | 0.04 * |
| Limitation of life support | 20 (17%) | 20 (77%) | ||
| CAPA g | 3 (3%) | 1 (<1%) | 2 (8%) | 0.1 |
| Univariable Analysis | Multivariable Analysis | |||||
|---|---|---|---|---|---|---|
| Characteristics | HR | 95% CI | p-Value | HR | 95% CI | p-Value |
| Male | 1.2 | 0.5–2.7 | 0.73 | |||
| Age | 1.1 | 1–1.1 | <0.001 * | 1.06 | 1.02–1.11 | 0.002 * |
| BMI | 0.95 | 0.88–1 | 0.2 * | 0.99 | 0.91–1.08 | 0.83 |
| Charlson index | 1.5 | 1.3–1.7 | <0.001 * | 1.33 | 1.11–1.6 | 0.002 * |
| Chest CT-Scan a | ||||||
| Mild | 2.1 | 0.78–5.5 | 0.14 * | 0.99 | 0.31–3.12 | 0.98 |
| Moderate | 0.61 | 0.28–1.3 | 0.21 | |||
| Severe | 1.2 | 0.47–2.9 | 0.74 | |||
| Critical | 1.3 | 0.3–5.3 | 0.76 | |||
| Variant of concern | ||||||
| Delta | 1.3 | 0.4–4.4 | 0.65 | |||
| Omicron | 0.76 | 0.23–2.5 | 0.65 | |||
| WHO-CPS b | ||||||
| At admission | 1.2 | 0.54–2.5 | 0.69 | |||
| At tocilizumab administration | 2.3 | 0.98–5.2 | 0.055 * | 2.58 | 1.07–6.22 | 0.03 * |
| Inflammation biomarkers | ||||||
| CRP pre-tocilizumab | 1 | 0.99–1 | 0.49 | |||
| CRP post-tocilizumab | 1 | 1–1 | 0.16 * | 1 | 1–1.01 | 0.27 |
| Tocilizumab treatment | ||||||
| Administration within 2 days | 0.35 | 0.16–0.73 | 0.012 * | 0.37 | 0.14–0.97 | 0.04 * |
| Dose | 1 | 0.99–1 | 0.16 * | 1 | 0.99–1 | 0.57 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laffont-Lozes, P.; Laureillard, D.; Loubet, P.; Stephan, R.; Chiaruzzi, M.; Clemmer, E.; Martin, A.; Roger, C.; Muller, L.; Claret, P.-G.; et al. Effect of Tocilizumab on Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta or Omicron Variants: A Propensity-Matched Analysis in Nimes University Hospital, France. Antibiotics 2023, 12, 88. https://doi.org/10.3390/antibiotics12010088
Laffont-Lozes P, Laureillard D, Loubet P, Stephan R, Chiaruzzi M, Clemmer E, Martin A, Roger C, Muller L, Claret P-G, et al. Effect of Tocilizumab on Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta or Omicron Variants: A Propensity-Matched Analysis in Nimes University Hospital, France. Antibiotics. 2023; 12(1):88. https://doi.org/10.3390/antibiotics12010088
Chicago/Turabian StyleLaffont-Lozes, Paul, Didier Laureillard, Paul Loubet, Robin Stephan, Myriam Chiaruzzi, Edouard Clemmer, Aurelie Martin, Claire Roger, Laurent Muller, Pierre-Géraud Claret, and et al. 2023. "Effect of Tocilizumab on Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta or Omicron Variants: A Propensity-Matched Analysis in Nimes University Hospital, France" Antibiotics 12, no. 1: 88. https://doi.org/10.3390/antibiotics12010088
APA StyleLaffont-Lozes, P., Laureillard, D., Loubet, P., Stephan, R., Chiaruzzi, M., Clemmer, E., Martin, A., Roger, C., Muller, L., Claret, P.-G., Goulabchand, R., Roux, C., Lavigne, J.-P., Sotto, A., & Larcher, R. (2023). Effect of Tocilizumab on Mortality in Patients with SARS-CoV-2 Pneumonia Caused by Delta or Omicron Variants: A Propensity-Matched Analysis in Nimes University Hospital, France. Antibiotics, 12(1), 88. https://doi.org/10.3390/antibiotics12010088






