Abstract
Antibiotic resistance is a global health crisis. New classes of antibiotics that can treat drug-resistant infections are urgently needed. To communicate this message, researchers have used antibiotic development timelines, but these are often contradictory or imprecise. We conducted a systematic literature review to produce an antibiotic timeline that incorporates the dates of discovery, first use, and initial reports of the emergence of resistance for the 38 classes of clinically used antibiotics. From our timeline, we derive lessons for identifying new antibiotics that are less prone to resistance. These include a required focus on molecules that exhibit multiple modes of action, possess unusually long ‘resistance windows’, or those that engage cellular targets whose molecular architectures are at least in part decoupled from evolutionary pressures. Our analysis also further highlights the importance of safeguarding antibiotics as a mechanism for mitigating the development of resistance. We have made our data and sources freely available so that the research community can adapt them to their own needs.
1. Introduction
Antibiotic resistance—bacterial infections that no longer respond to the drugs used to treat them—is a global health crisis of growing concern [1,2]. The demand for existing antibiotics is too high, which drives the evolution of resistance in pathogens [2,3,4]. The supply of new classes of antibiotics that can treat drug-resistant infections is too low, which leaves us with few treatment options for the most serious infections [5,6,7]. To communicate the scale of the problem, researchers have used graphical timelines that show how the rate of antibiotic discovery has slowed in recent times. These timelines are valuable tools for science communication, but often disagree with one another and lack clarity.
In previous reviews, the definitions used for the date of the discovery of an antibiotic, its first clinical use, and the emergence of resistance to it, either are not disclosed or lack internal consistency. Examples include the non-disclosure of methods used to generate a timeline for antibiotic discovery [5]; inconsistency in the definition of when an antibiotic was introduced into the clinic [8]; not defining the “year of discovery” or “year of introduction” categories and employing a scale with a resolution of decades [9]; and the CDC’s 2013 Antibiotic Threats Report, which includes an antibiotic resistance timeline “based on early reports in the literature”, but with a lack of clarity as to whether this refers to in vitro, in vivo, or clinical data [10].
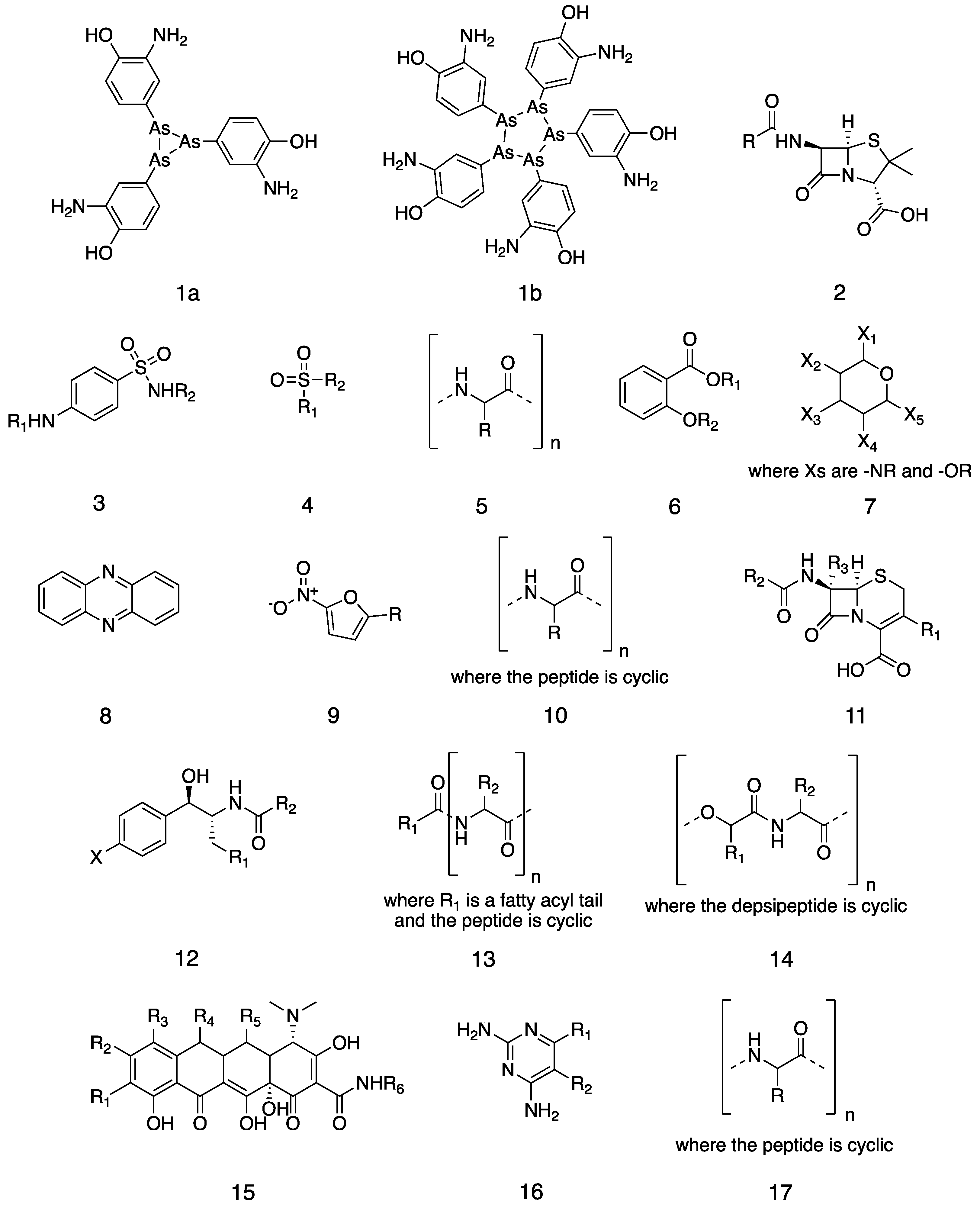
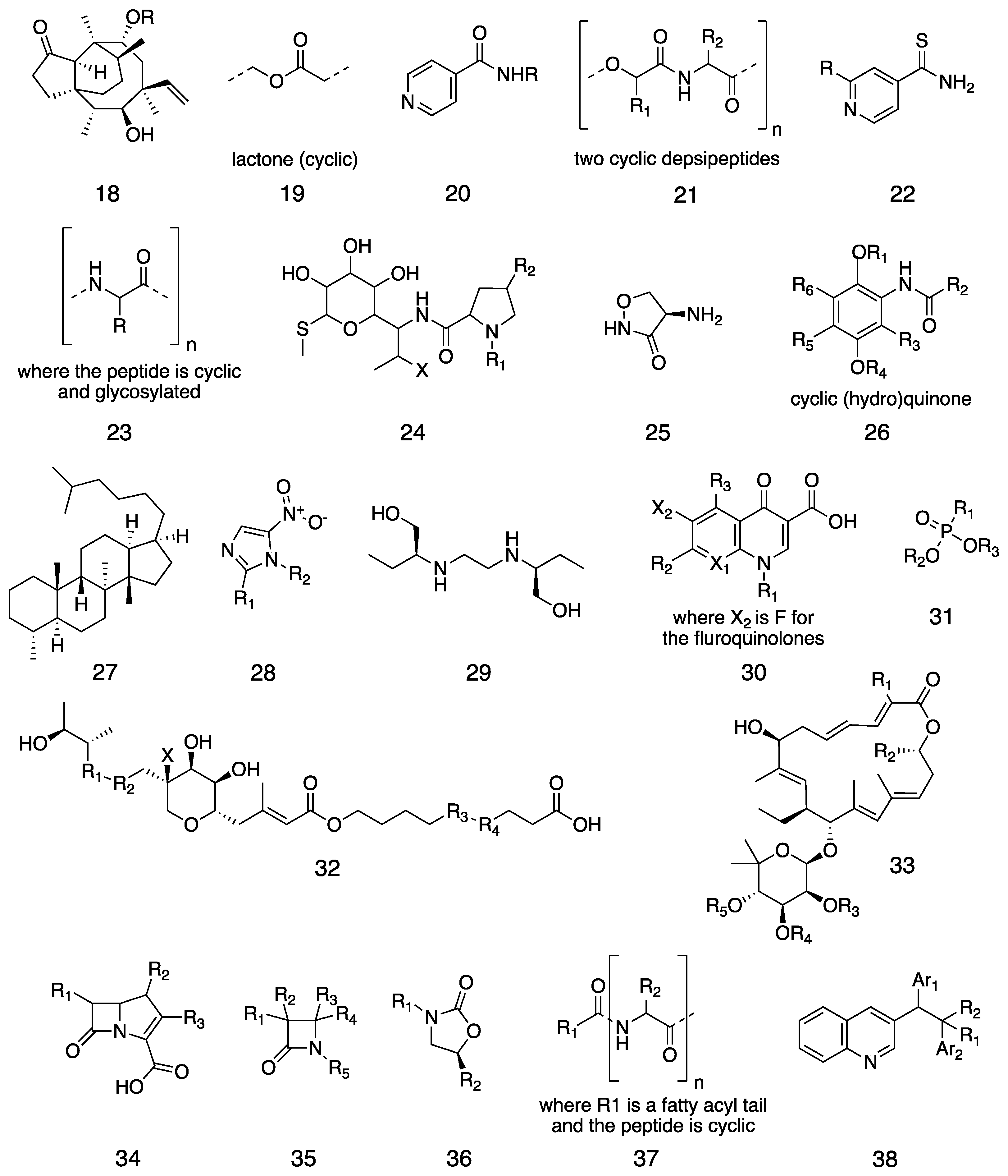
We conducted a systematic literature review to produce a more precise timeline for antibiotic discovery, introduction, and resistance. Antibiotics can be classified by their origins, structures, and mechanisms of action. We took the 38 classes of antibiotics in clinical use (Figure 1), as defined by Hutchings et al. [8], and consistently applied the following definitions to them:
- Discovery: when a compound or extract—not merely an organism—was first reported to have antibiotic activity. In some cases, this was decades after the compound was first discovered or synthesized.
- First clinical use: the first use of the antibiotic to treat a bacterial infection: in modern terms, a phase II trial. Clinical studies of tolerance and toxicity are not included. The approval of an antibiotic for human use is not used because several of these drugs predate regulatory bodies.
- Resistance: the first report of clinically isolated bacteria resistant to the antibiotic.
We hope that our timeline will be a useful resource to the antibiotic research and public health communities. We have included our data and sources so that the timeline can be verified, updated, and modified.
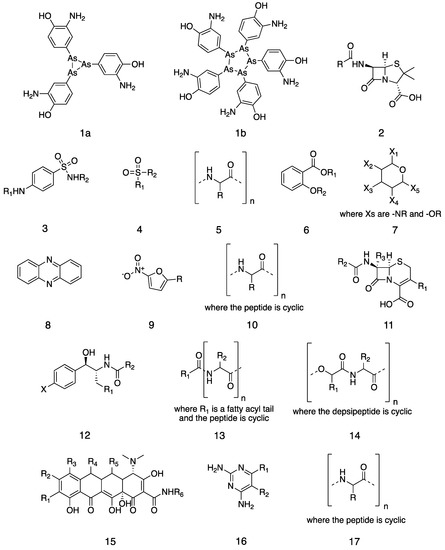
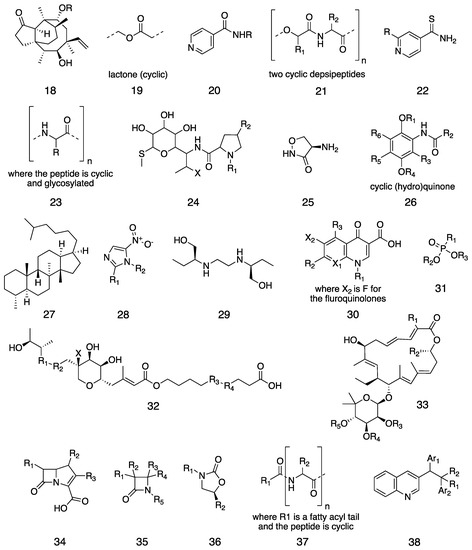
Figure 1.
Chemical structures of the 38 classes of antibiotics. (1) Arsphenamine in its (1a) trivalent and (1b) pentavalent forms. General chemical structures of (2) a penicillin, (3) a sulfonamide, (4) a sulphone, (5) a polypeptide, (6) a salicylate, (7) an aminoglycoside, (8) a phenazine, (9) a nitrofuran, (10) a cyclic peptide, (11) a cephalosporin, (12) an amphenicol, (13) a polymyxin, (14) an enniatin, (15) a tetracycline, (16) a diaminopyrimidine, (17) a tuberactinomycin, (18) a pleuromutilin, (19) a macrolide, (20) a nicotinamide, (21) a streptogramin, (22) a thioisonicotinamide, (23) a glycopeptide, (24) a lincosamide, (25) a cycloserine, (26) an ansamycin, (27) a fusidane, (28) a nitroimidazole, (29) ethambutol, (30) a quinolone, (31) a phosphonate, (32) a mupirocin, (33) a lipiarmycin, (34) a carbapenem, (35) a monobactam, (36) an oxazolidinone, (37) a lipopeptide, and (38) a diarylquinoline.
Figure 1.
Chemical structures of the 38 classes of antibiotics. (1) Arsphenamine in its (1a) trivalent and (1b) pentavalent forms. General chemical structures of (2) a penicillin, (3) a sulfonamide, (4) a sulphone, (5) a polypeptide, (6) a salicylate, (7) an aminoglycoside, (8) a phenazine, (9) a nitrofuran, (10) a cyclic peptide, (11) a cephalosporin, (12) an amphenicol, (13) a polymyxin, (14) an enniatin, (15) a tetracycline, (16) a diaminopyrimidine, (17) a tuberactinomycin, (18) a pleuromutilin, (19) a macrolide, (20) a nicotinamide, (21) a streptogramin, (22) a thioisonicotinamide, (23) a glycopeptide, (24) a lincosamide, (25) a cycloserine, (26) an ansamycin, (27) a fusidane, (28) a nitroimidazole, (29) ethambutol, (30) a quinolone, (31) a phosphonate, (32) a mupirocin, (33) a lipiarmycin, (34) a carbapenem, (35) a monobactam, (36) an oxazolidinone, (37) a lipopeptide, and (38) a diarylquinoline.
2. Results
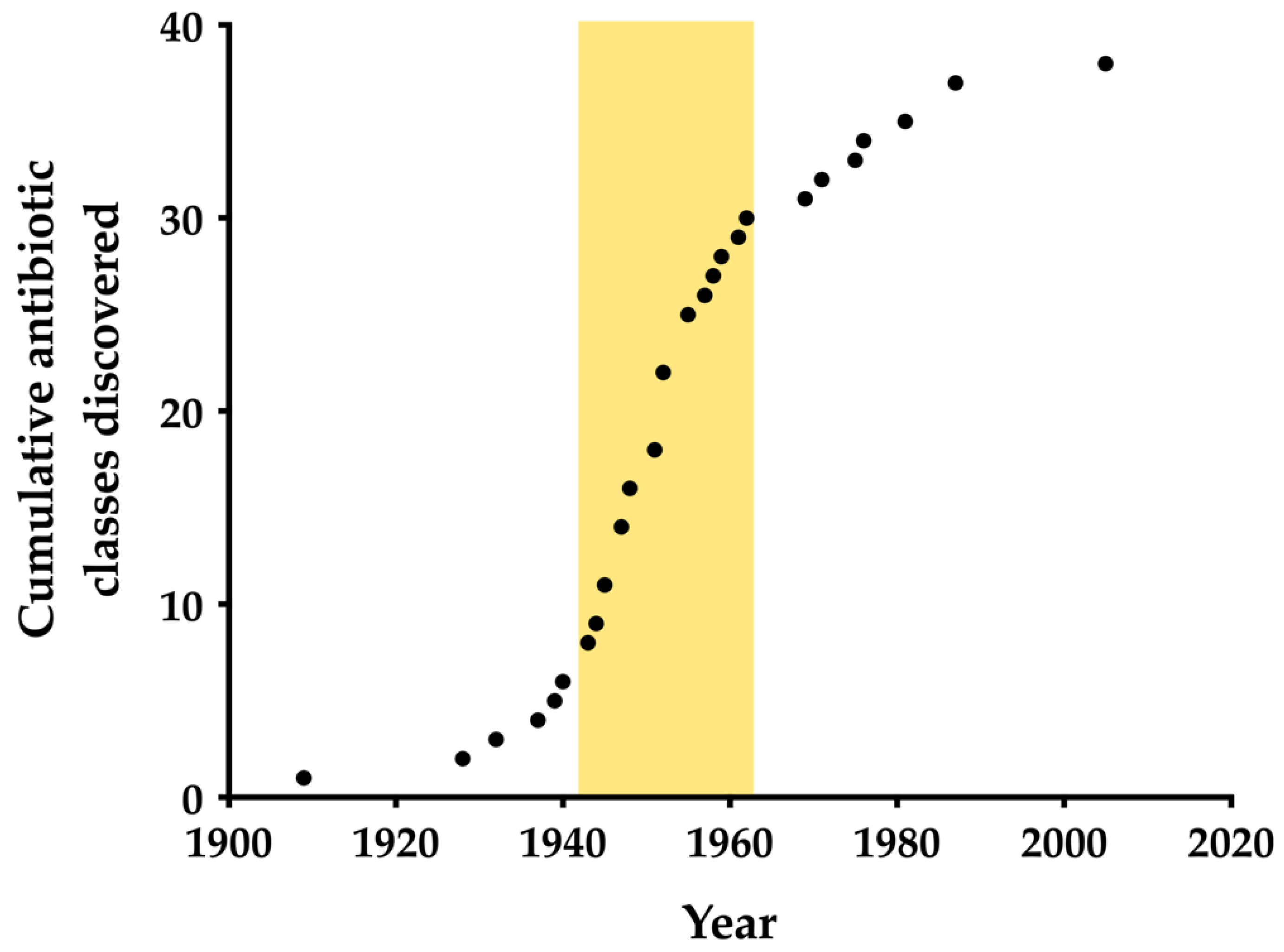
Figure 2 emphasizes the stark reduction in the antibiotic discovery rate after the “Golden Age”, the most prolific period of antibiotic research [11,12]. In fact, the rate of discovery is now at its lowest since the first antibiotic, arsphenamine, was discovered in 1909. The Golden Age is usually roughly defined as 1940–1960, beginning with the discovery of streptomycin [8]. Extending the linear part of the sigmoidal discovery curve in Figure 1 allows us to better define the Golden Age as 1943–1962, when streptomycin and the quinolones were discovered, respectively. A 2011 review in Clinical Microbiology Reviews defined the “discovery void”, during which no new antibiotic classes have been discovered, as starting from 1987, and several sources have repeated this claim [5,13,14,15]. However, the diarylquinolines were FDA-approved the year after this review, and thus this definition requires revision [16].
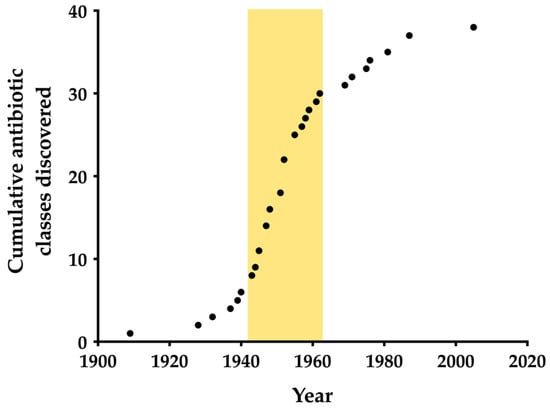
Figure 2.
The cumulative discovery of the 38 classes of clinically used antibiotics. The Golden Age of discovery is highlighted in yellow.
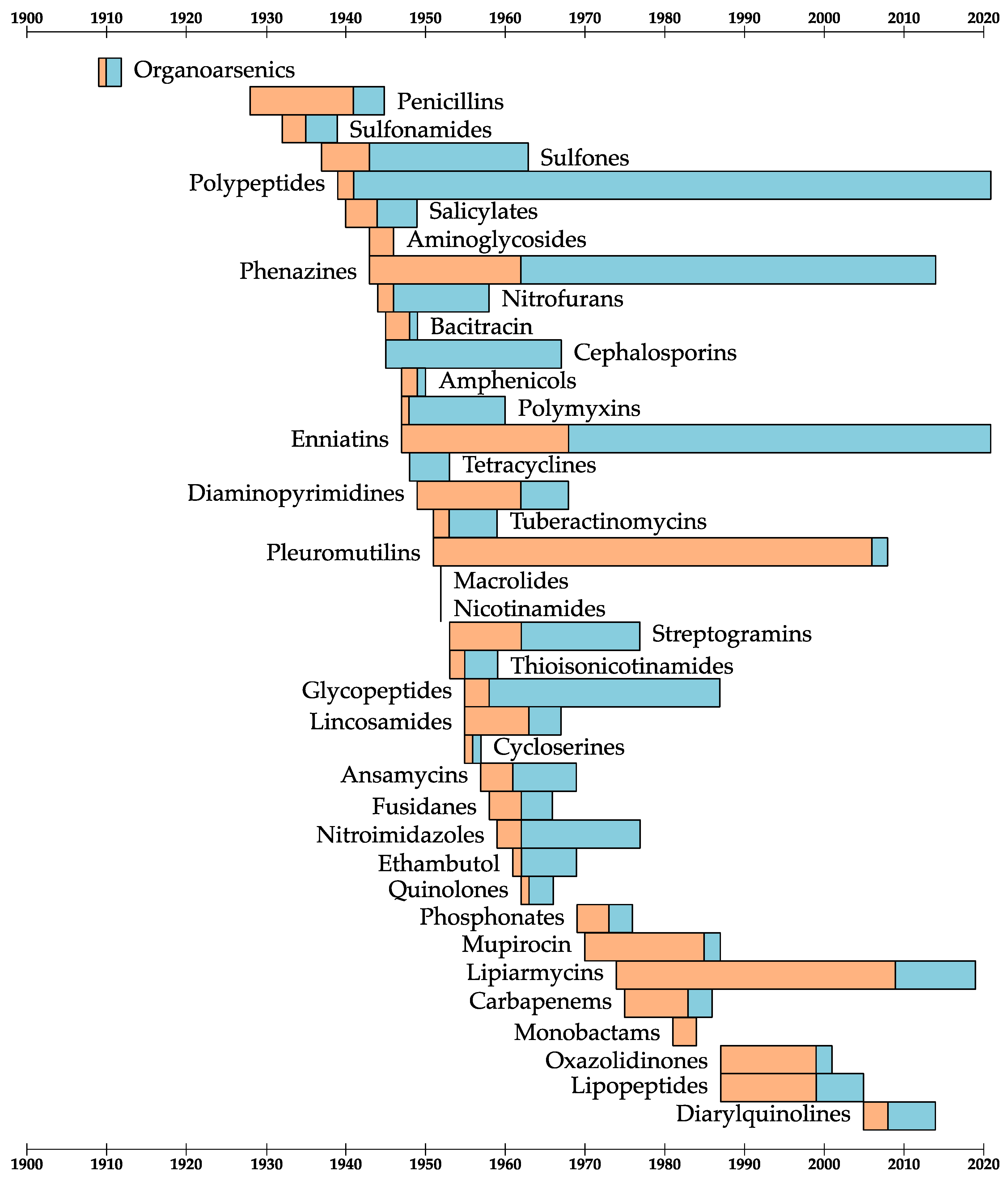
Figure 3 shows the discovery, first clinical use, and resistance dates for the 38 antibiotic classes. From these dates, we can define two periods of time:
- The development window: how long after its discovery the antibiotic was first used in the clinic.
- The resistance window: how long after its first use clinical resistance was reported.
There are some obvious outliers in this analysis. The antibiotics with long development windows were either technically challenging to optimize or shelved because they were not considered to be promising drugs until the antibiotic resistance crisis worsened [17,18,19,20]. Five new antibiotic classes have been approved for human use by the FDA in this century: oxazolidinones (2000), lipopeptides (2003), pleuromutilins (2007), diarylquinolones (2007), and lipiarmycins (2011). Three of these were abandoned early in their development because of adverse side effects [16,17,21]. The diarylquinolones carry a black box warning—the strongest warning that the FDA requires—because of their significant life-threatening side effects [16]. The lipiarmycins and pleuromutilins were first approved for human use long after their discovery: 36 and 56 years, respectively [17,22].
More promisingly, there are a few examples of antibiotics with unusually long resistance windows, from which we can derive some lessons for designing or identifying “resistance-proof” antibiotics [23,24].
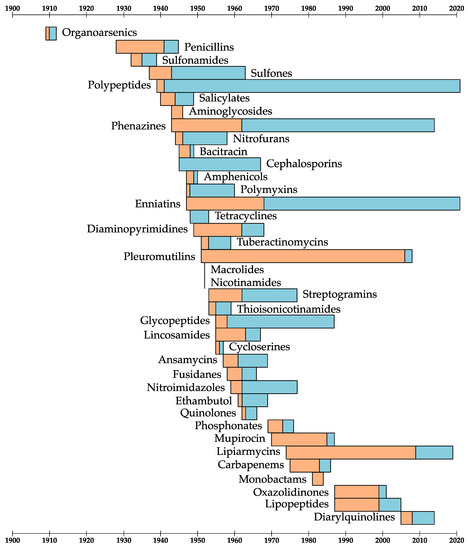
Figure 3.
A timeline for the discovery, first clinical use of, and first report of clinical resistance to the 38 classes of antibiotics. For each antibiotic class, the orange bars are the “development windows” and the blue bars are the “resistance windows”.
Figure 3.
A timeline for the discovery, first clinical use of, and first report of clinical resistance to the 38 classes of antibiotics. For each antibiotic class, the orange bars are the “development windows” and the blue bars are the “resistance windows”.
2.1. Multiple Targets
The polypeptide antibiotic tyrothricin has only been used topically, which is likely part of the reason for its long resistance window [25]. However, even after decades of use, no clinical resistance to the antibiotic has been seen and significant resistance cannot be induced in vitro [25,26]. Wenzel et al. interrogated the antibiotic mechanism of tyrothricin and found that even though its component peptides are highly similar in sequence, they have different mechanisms of action [27]. Their combined effects are to damage DNA, increase membrane permeability, decrease membrane fluidity, and delocalize membrane proteins [27]. This attack on multiple fronts is difficult for bacteria to defend against and makes tyrothricin a natural combination therapy [28]. Clinical phenazine resistance is also extremely rare, although it has been induced in vitro [29,30]. Like tyrothricin, these antibiotics likely have multiple mechanisms of action, which makes resistance more difficult to evolve [31,32]. Identifying new antibiotics with multiple mechanisms of action, or using multiple antibiotics as combination therapies, is likely to slow the development of resistance [28].
2.2. “Resistance-Proof” Targets
Glycopeptides such as vancomycin bind D-Ala-D-Ala residues at the ends of glycan chains, preventing the binding of peptidoglycan biosynthetic enzymes [33]. This mode of action targets a structural component of the cell that is not directly genetically encoded, so it is difficult to evolve resistance by mutating the target [34]. Furthermore, glycopeptides do not have to enter the cell to act, which means that resistance cannot evolve by reduced permeability to or modification of the antibiotics [34]. Resistance to glycopeptides did not arise in pathogens directly: the self-resistance genes were transferred from the producing microorganisms to pathogens [34]. New antibiotics with similar targets are likely to be “resistance-proof” [23].
2.3. Low Use
The long resistance window for sulfones is probably due to their main indication as drugs for leprosy [35]. Leprosy is a neglected tropical disease and there are many gaps in our understanding of it [36]. Furthermore, sulfones are only weakly antibacterial against Mycobacterium leprae, which made resistance to these antibiotics more difficult to definitively prove [37]. Enniatins are thought to act as ionophores, collapsing ion gradients across membranes in general [38]. In vivo resistance to ionophores has been recorded and can occur by enzymatic degradation or exclusion of the compounds from the cell [39]. Presumably, such mechanisms are also possible for the enniatins, and their limited use due to their cytotoxicity has delayed the onset of resistance [40,41]. The most important lesson for safeguarding antibiotics is that reducing their use will slow the development of resistance [4].
3. Discussion
This work represents the first comprehensive and consistent timeline for antibiotic discovery, development, and resistance. It should prove useful for communicating the alarmingly low number of new antibiotic classes that are reaching the clinic, and we have also shown how the data can be used to identify antibiotic classes for which resistance is more difficult to evolve. Our findings reveal a correlation between pharmacophore novelty and a reduced ‘development window’, and also serve to highlight the importance of prioritizing molecules with expanded ‘resistance windows’ to ensure the long-term safeguarding of antibiotics. By making our data fully available, and our methods transparent, we hope that future researchers can use and adapt our timeline for their own science communication.
4. Materials and Methods
We conducted a systematic literature review by searching the Web of Science Core Collection and PubMed databases for the names of antibiotic classes or their first members, and found the earliest dates of discovery, use, and resistance, defined in Section 1. Table 1 shows the data used to make these timelines, with sources for each data point.
Author Contributions
Conceptualization, H.L.S., C.R.B. and P.R.R.; investigation, H.L.S.; writing—original draft preparation, H.L.S.; writing—review and editing, C.R.B. and P.R.R.; visualization, H.L.S.; supervision, P.R.R.; funding acquisition, P.R.R. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by BBSRC grants BB/T001968/1 and BB/L01386X/1, MRF grant MRF-131-0005-RG-RACE-C0853, and through the award of a PhD studentship to H.L.S. from the EPSRC Centre for Doctoral Training in Synthetic Biology (EP/L016494/1) and Dstl.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Martens, E.; Demain, A.L. The antibiotic resistance crisis, with a focus on the United States. J. Antibiot. 2017, 70, 520–526. [Google Scholar] [CrossRef]
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Ther. 2015, 40, 277–283. [Google Scholar]
- Klein, E.Y.; van Boeckel, T.P.; Martinez, E.M.; Pant, S.; Gandra, S.; Levin, S.A.; Goossens, H.; Laxminarayan, R. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc. Natl. Acad. Sci. USA 2018, 115, E3463–E3470. [Google Scholar] [CrossRef] [PubMed]
- zur Wiesch, P.A.; Kouyos, R.; Engelstadter, J.; Regoes, R.R.; Bonhoeffer, S. Population biological principles of drug-resistance evolution in infectious diseases. Lancet Infect. Dis. 2011, 11, 236–247. [Google Scholar] [CrossRef]
- Silver, L.L. Challenges of antibacterial discovery. Clin. Microbiol. Rev. 2011, 24, 71–109. [Google Scholar] [CrossRef] [PubMed]
- Boucher, H.W.; Talbot, G.H.; Bradley, J.S.; Edwards, J.E.; Gilbert, D.; Rice, L.B.; Scheld, M.; Spellberg, B.; Bartlett, J. Bad bugs, no drugs: No ESKAPE! An update from the Infectious Diseases Society of America. Clin. Infect. Dis. 2009, 48, 1–12. [Google Scholar] [CrossRef]
- Theuretzbacher, U.; Outterson, K.; Engel, A.; Karlén, A. The global preclinical antibacterial pipeline. Nat. Rev. Microbiol. 2019, 18, 275–285. [Google Scholar] [CrossRef]
- Hutchings, M.I.; Truman, A.W.; Wilkinson, B. Antibiotics: Past, present and future. Curr. Opin. Microbiol. 2019, 51, 72–80. [Google Scholar] [CrossRef]
- Lewis, K. The science of antibiotic discovery. Cell 2020, 181, 29–45. [Google Scholar] [CrossRef]
- CDC. Antibiotic Resistance Threats in the United States; U.S. Department for Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2013.
- Shen, B. A new golden age of natural products drug discovery. Cell 2015, 163, 1300. [Google Scholar] [CrossRef]
- Wright, G.D. Unlocking the potential of natural products in drug discovery. Microb. Biotechnol. 2019, 12, 55–57. [Google Scholar] [CrossRef] [PubMed]
- Few Antibiotics under Development—How Did We End up Here?—ReAct. Available online: https://www.reactgroup.org/toolbox/understand/how-did-we-end-up-here/few-antibiotics-under-development (accessed on 29 October 2021).
- Plackett, B. Why big pharma has abandoned antibiotics. Nature 2020, 586, S50–S52. [Google Scholar] [CrossRef]
- Nelson, D.W.; Moore, J.E.; Rao, J.R. Antimicrobial resistance (AMR): Significance to food quality and safety. Food Qual. Saf. 2019, 3, 15–22. [Google Scholar] [CrossRef]
- Mahajan, R. Bedaquiline: First FDA-approved tuberculosis drug in 40 years. Int. J. Appl. Basic Med. Res. 2013, 3, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Novak, R. Are pleuromutilin antibiotics finally fit for human use? Ann. N. Y. Acad. Sci. 2011, 1241, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Nation, R.L.; Li, J. Colistin in the 21st Century. Curr. Opin. Infect. Dis. 2009, 22, 535. [Google Scholar] [CrossRef]
- Theuretzbacher, U.; van Bambeke, F.; Cantón, R.; Giske, C.G.; Mouton, J.W.; Nation, R.L.; Paul, M.; Turnidge, J.D.; Kahlmeter, G. Reviving old antibiotics. J. Antimicrob. Chemother. 2015, 70, 2177–2181. [Google Scholar] [CrossRef]
- Bergen, P.J.; Landersdorfer, C.B.; Lee, H.J.; Li, J.; Nation, R.L. ‘Old’ antibiotics for emerging multidrug-resistant bacteria. Curr. Opin. Infect. Dis. 2012, 25, 626–633. [Google Scholar] [CrossRef]
- Tally, F.P.; DeBruin, M.F. Development of daptomycin for Gram-positive infections. J. Antimicrob. Chemother. 2000, 46, 523–526. [Google Scholar] [CrossRef]
- McAlpine, J.B. The ups and downs of drug discovery: The early history of Fidaxomicin. J. Antibiot. 2017, 70, 492–494. [Google Scholar] [CrossRef]
- Wu, Z.C.; Boger, D.L. Maxamycins: Durable antibiotics derived by rational redesign of vancomycin. Acc. Chem. Res. 2020, 53, 2587–2599. [Google Scholar] [CrossRef] [PubMed]
- Oldfield, E.; Feng, X. Resistance-resistant antibiotics. Trends Pharmacol. Sci. 2014, 35, 664–674. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.; Staiger, C. Tyrothricin—An underrated agent for the treatment of bacterial skin infections and superficial wounds? Pharmazie 2016, 71, 299–305. [Google Scholar] [PubMed]
- Stauss-Grabo, M.; Atiye, S.; Kretschmar, M. Decade-long use of the antimicrobial peptide combination tyrothricin does not pose a major risk of acquired resistance with Gram-positive bacteria and Candida spp. Pharmazie 2014, 69, 838–841. [Google Scholar] [PubMed]
- Wenzel, M.; Rautenbach, M.; Voslo, J.A.; Siersma, T.; Aisenbrey, C.H.M.; Zaitseva, E.; Laubscher, W.E.; van Rensburg, W.; Behrends, J.C.; Bechinger, B.; et al. The Multifaceted Antibacterial Mechanisms of the Pioneering Peptide Antibiotics Tyrocidine and Gramicidin S. mBio 2018, 9, e00802–e00818. [Google Scholar] [CrossRef] [PubMed]
- Coates, A.R.M.; Hu, Y.; Holt, J.; Yeh, P. Antibiotic combination therapy against resistant bacterial infections: Synergy, rejuvenation and resistance reduction. Expert Rev. Anti-Infect. Ther. 2020, 18, 5–15. [Google Scholar] [CrossRef]
- Hartkoorn, R.C.; Uplekar, S.; Cole, S.T. Cross-resistance between clofazimine and bedaquiline through upregulation of MmpL5 in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 2014, 58, 2979–2981. [Google Scholar] [CrossRef]
- Fu, T.; Cai, Z.; Yue, Z.; Yang, H.; Fang, B.; Zhang, X.; Fan, Z.; Pan, X.; Yang, F.; Jin, Y.; et al. Evolution of resistance to phenazine antibiotics in Staphylococcus aureus and its role during coinfection with Pseudomonas aeruginosa. ACS Infect. Dis. 2021, 7, 636–649. [Google Scholar] [CrossRef]
- Cholo, M.C.; Steel, H.C.; Fourie, P.B.; Germishuizen, W.A.; Anderson, R. Clofazimine: Current status and future prospects. J. Antimicrob. Chemother. 2012, 67, 290–298. [Google Scholar] [CrossRef]
- Guttenberger, N.; Blankenfeldt, W.; Breinbauer, R. Recent developments in the isolation, biological function, biosynthesis, and synthesis of phenazine natural products. Bioorg. Med. Chem. 2017, 25, 6149–6166. [Google Scholar] [CrossRef]
- Barna, J.C.; Williams, D.H. The structure and mode of action of glycopeptide antibiotics of the vancomycin group. Annu. Rev. Microbiol. 1984, 38, 339–357. [Google Scholar] [CrossRef]
- Kahne, D.; Leimkuhler, C.; Lu, W.; Walsh, C. Glycopeptide and lipoglycopeptide antibiotics. Chem. Rev. 2005, 105, 425–448. [Google Scholar] [CrossRef] [PubMed]
- Pearson, J.M.; Rees, R.J.; Waters, M.F. Sulphone resistance in leprosy. A review of one hundred proven clinical cases. Lancet 1975, 2, 69–72. [Google Scholar] [CrossRef]
- Molyneux, D. Neglected tropical diseases. Community Eye Health 2013, 26, 21–24. [Google Scholar] [PubMed]
- Prasad, P.V.S.; Kaviarasan, P.K. Leprosy therapy, past and present: Can we hope to eliminate it? Indian J. Dermatol. 2010, 55, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Bakker, E.P. Ionophore Antibiotics. In Mechanism of Action of Antibacterial Agents, 2nd ed.; Hahn, F.E., Ed.; Springer: Berlin/Heidelberg, Germany, 1979; Volume 5, pp. 67–97. [Google Scholar]
- Russell, J.B.; Houlihan, A.J. Ionophore resistance of ruminal bacteria and its potential impact on human health. FEMS Microbiol. Rev. 2003, 27, 65–74. [Google Scholar] [CrossRef]
- Olleik, H.; Nicoletti, C.; Lafond, M.; Courvoisier-Dezord, E.; Xue, P.; Hijazi, A.; Baydoun, E.; Perrier, J.; Maresca, M. Comparative structure-activity analysis of the antimicrobial activity, cytotoxicity, and mechanism of action of the fungal cyclohexadepsipeptides enniatins and beauvericin. Toxins 2019, 11, 514. [Google Scholar] [CrossRef]
- German-Fattal, M. Fusafungine, an antimicrobial with anti-inflammatory properties in respiratory tract infections. Clin. Drug Investig. 2001, 21, 653–670. [Google Scholar] [CrossRef]
- Rubin, R.P. A brief history of great discoveries in pharmacology: In celebration of the centennial anniversary of the founding of the American Society of Pharmacology and Experimental Therapeutics. Pharmacol. Rev. 2007, 59, 289–359. [Google Scholar] [CrossRef]
- Williams, K. The introduction of ‘chemotherapy’ using arsphenamine—The first magic bullet. J. R. Soc. Med. 2009, 102, 343. [Google Scholar] [CrossRef]
- Tan, S.Y.; Tatsumura, Y. Alexander Fleming (1881–1955): Discoverer of penicillin. Singap. Med. J. 2015, 56, 366. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, C. First clinical use of penicillin. Br. Med. J. 1984, 289, 1721. [Google Scholar] [CrossRef] [PubMed]
- Plough, H.H. Penicillin resistance of Staphylococcus aureus and its clinical implications. Am. J. Clin. Pathol. 1945, 15, 446–451. [Google Scholar] [CrossRef]
- Domagk, G. Chemotherapie der bakteriellen infektionen. Angew. Chem. 1935, 48, 657–667. [Google Scholar] [CrossRef]
- Maclean, I.; Rogers, K.; Fleming, A. M. & B. 693 and pneumococci. Lancet 1939, 233, 562–568. [Google Scholar]
- Wozel, G. The story of sulfones in tropical medicine and dermatology. Int. J. Dermatol. 1989, 28, 17–21. [Google Scholar] [CrossRef]
- Faget, G.H.; Pogge, R.C.; Johansen, F.A.; Dinan, J.F.; Prejean, B.M.; Eccles, C.G. The promin treatment of leprosy. A progress report. Public Health Rep. 1943, 58, 1729. [Google Scholar] [CrossRef]
- Dubos, R.J. Studies on a bactericidal agent extracted from a soil Bacillus: I. Preparation of the agent. Its activity in vitro. J. Exp. Med. 1939, 70, 1–10. [Google Scholar] [CrossRef]
- Herrell, W.E.; Heilman, D. Experimental and clinical studies on gramicidin. J. Clin. Investig. 1941, 20, 583. [Google Scholar] [CrossRef]
- Bernheim, F. The effect of salicylate on the oxygen uptake of the tubercle bacillus. Science 1940, 92, 204. [Google Scholar] [CrossRef]
- Lehmann, J. Para-aminosalicylic acid in the treatment of tuberculosis. Lancet 1946, 1, 15–16. [Google Scholar] [CrossRef]
- A Medical Research Council Investigation. Treatment of pulmonary tuberculosis with streptomycin and para-amino-salicylic acid. Br. Med. J. 1950, 2, 1073–1085. [Google Scholar] [CrossRef]
- Rawlins, M. The disputed discovery of streptomycin. Lancet 2012, 380, 207. [Google Scholar] [CrossRef]
- Crofton, J. The MRC randomized trial of streptomycin and its legacy: A view from the clinical front line. J. R. Soc. Med. 2006, 99, 531. [Google Scholar] [CrossRef] [PubMed]
- Finland, M.; Murray, R. Development of streptomycin resistance during treatment. J. Am. Med. Assoc. 1946, 132, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Carr, C.J.; Vivian, D.L.; Krantz, J.C. A contribution to the pharmacology of phenazine and certain of its derivatives. J. Pharmacol. Exp. Ther. 1943, 77, 215–219. [Google Scholar]
- Browne, S.G.; Hogerzeil, L.M. “B 663” in the treatment of leprosy. Preliminary report of a pilot trial. Lepr. Rev. 1962, 33, 6–10. [Google Scholar] [CrossRef]
- Andries, K.; Villellas, C.; Coeck, N.; Thys, K.; Gevers, T.; Vranckx, L.; Lounis, N.; de Jong, B.C.; Koul, A. Acquired Resistance of Mycobacterium tuberculosis to bedaquiline. PLoS ONE 2014, 9, e102135. [Google Scholar] [CrossRef]
- Dodd, M.C.; Stillman, W.B.; Roys, M.; Crosby, C. The in vitro bacteriostatic action of some simple furan derivatives. J. Pharmacol. Exp. Ther. 1944, 82, 11–18. [Google Scholar]
- Dodd, M.C.; Hartmann, F.W.; Ward, W.C. The local application of nitrofuran compounds with special reference to use on wounds. Surg. Gynecol. Obstet. 1946, 83, 73–82. [Google Scholar]
- Lutz, A.; Witz, M.; Schaeffer, A. Recherches sur l’évolution de la résistance de germes du genre proteus aux antibiotiques usuels de 1950 à 1958; l’action in vitro de la novobiocine, de la kanamycine, de la nitrofurantoine, et des sulfamides. Ann. Inst. Pasteur 1958, 95, 413–423. [Google Scholar]
- Johnson, B.A.; Anker, H.; Meleney, F.L. Bacitracin: A new antibiotic produced by a member of the B. subtilis group. Science 1945, 102, 376–377. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, R.; Khanna, N.R.; Safadi, A.O.; Sun, Y. Bacitracin Topical. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Stone, J.L. Induced resistance to bacitracin in cultures of Staphylococcus aureus. J. Infect. Dis. 1949, 85, 91–96. [Google Scholar] [CrossRef]
- Abraham, E.P. A glimpse of the early history of the cephalosporins. Rev. Infect. Dis. 1979, 1, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Bastin, R.; Worms, R.; Acar, J.F. Clinical incidence of heterogenous resistance of Staphylococcus to penicillin and cephalosporin. Pathol. Biol. 1967, 15, 1205–1211. [Google Scholar] [PubMed]
- Ehrlich, J.; Bartz, Q.R.; Smith, R.M.; Joslyn, D.A.; Burkholder, P.R. Chloromycetin, a new antibiotic from a soil actinomycete. Science 1947, 106, 417. [Google Scholar] [CrossRef]
- Smadel, J.E. Clinical use of the antibiotic chloramphenicol (chloromycetin®). J. Am. Med. Assoc. 1950, 142, 315–318. [Google Scholar] [CrossRef]
- Colquhoun, J.; Weetch, R.S. Resistance to chloramphenicol developing during treatment of typhoid fever. Lancet 1950, 256, 621–623. [Google Scholar] [CrossRef]
- Ainsworth, G.C.; Brown, A.M.; Brownlee, G. ‘Aerosporin’, an antibiotic produced by Bacillus aerosporus Greer. Nature 1947, 160, 263. [Google Scholar] [CrossRef]
- Schoenbach, E.B.; Bryer, M.S. Polymyxin; A note on experimental and clinical investigations. J. Am. Med. Assoc. 1948, 136, 1096–1098. [Google Scholar] [CrossRef]
- Hirsch, H.A.; McCarthy, C.G.; Finland, M. Polymyxin B and colistin: Activity, resistance and crossresistance in vitro. Proc. Soc. Exp. Biol. Med. 1960, 103, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Gaumann, E.; Roth, S. Enniatin, a new antibiotic that works against mycobacteria. Experientia 1947, 3, 202–203. [Google Scholar] [PubMed]
- Piquet, J.J.; Hequet, B.; Decroix, G. Value of the use of locabiotal pressurise in rhinosinus pathology in children. Lille Méd. 1968, 14, S497–S499. [Google Scholar]
- German-Fattal, M. Fusafungine. An antimicrobial agent for the local treatment of respiratory tract infections. Clin. Drug Investig. 1996, 12, 308–317. [Google Scholar] [CrossRef]
- Duggar, B.M. Aureomycin: A product of the continuing search for new antibiotics. Ann. N. Y. Acad. Sci. 1948, 51, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.; Burke, F.G. Aureomycin; preliminary report of a clinical trial. Clin. Proc. Child. Hosp. Dist. Columbia 1948, 4, 315–331. [Google Scholar]
- Chopra, I.; Roberts, M. Tetracycline antibiotics: Mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol. Mol. Biol. Rev. 2001, 65, 232. [Google Scholar] [CrossRef]
- Hitchings, G.H.; Elion, G.B. Pyrimidine derivatives as antagonists of pteroylglutamic acid. J. Biol. Chem. 1948, 174, 765. [Google Scholar] [CrossRef]
- Noall, E.W.P.; Sewards, H.F.G.; Waterworth, P.M. Successful treatment of a case of Proteus septicaemia. Br. Med. J. 1962, 2, 1101. [Google Scholar] [CrossRef]
- Darrell, J.H.; Garrod, L.P.; Waterworth, P.M. Trimethoprim: Laboratory and clinical studies. J. Clin. Pathol. 1968, 21, 202. [Google Scholar] [CrossRef]
- Finlay, A.C.; Hobby, G.L.; Hochstein, F.; Lees, T.M.; Lenert, T.F.; Means, J.A.; P’an, S.Y.; Regna, P.P.; Routien, J.B.; Sobin, B.A.; et al. Viomycin, a new antibiotic active against mycobacteria. Am. Rev. Tuberc. 1951, 63, 1–3. [Google Scholar] [PubMed]
- Hackney, R.; King, E.; Marshall, E.; Harden, A.; Payne, H. Clinical observations on viomycin sulphate in the treatment of tuberculosis. Dis. Chest 1953, 24, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Tsukamura, M. Drug-resistance test for kanamycin and cross resistance problem in Mycobacterium tuberculosis with special reference to kanamycin, streptomycin, and viomycin. J. Antibiot. 1959, 12, 189–191. [Google Scholar]
- Kavanagh, F.; Hervey, A.; Robbins, W.J. Antibiotic Substances from Basidiomycetes: VIII. Pleurotus Multilus (Fr.) Sacc. and Pleurotus Passeckerianus Pilat. Proc. Natl. Acad. Sci. USA 1951, 37, 570–574. [Google Scholar] [CrossRef]
- Parish, L.C.; Jorizzo, J.L.; Breton, J.J.; Hirman, J.W.; Scangarella, N.E.; Shawar, R.M.; White, S.M.; SB275833/032 Study Team. Topical retapamulin ointment (1%, wt./wt.) twice daily for 5 days versus oral cephalexin twice daily for 10 days in the treatment of secondarily infected dermatitis: Results of a randomized controlled trial. J. Am. Acad. Dermatol. 2006, 55, 1003–1013. [Google Scholar] [CrossRef] [PubMed]
- Gentry, D.R.; McCloskey, L.; Gwynn, M.N.; Rittenhouse, S.F.; Scangarella, N.; Shawar, R.; Holmes, D.J. Genetic characterization of VgaABC proteins conferring reduced susceptibility to pleuromutilins in Staphylococcus aureus. Antimicrob. Agents Chemother. 2008, 52, 4507–4509. [Google Scholar] [CrossRef]
- Erythromycin. Br. Med. J. 1952, 2, 1085–1086. [CrossRef]
- Haight, T.H.; Finland, M. Laboratory and clinical studies on erythromycin. N. Engl. J. Med. 1952, 247, 227–232. [Google Scholar] [CrossRef]
- Haight, T.H.; Finland, M. Resistance of bacteria to erythromycin. Exp. Biol. Med. 1952, 81, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Fox, H.H. The chemical attack on tuberculosis. Trans. N. Y. Acad. Sci. 1953, 15, 234–242. [Google Scholar] [CrossRef]
- Bernstein, J.; Lott, W.A.; Steinberg, B.A.; Yale, H.L. Chemotherapy of experimental tuberculosis. V. Isonicotinic acid hydrazide (nydrazid) and related compounds. Am. Rev. Tuberc. 1952, 65, 357–364. [Google Scholar] [PubMed]
- Clark, C.M.; Elmendorf, D.F.; Cawthon, W.U.; Muschenheim, C.; McDermott, W. Isoniazid (isonicotinic acid hydrazide) in the treatment of miliary and meningeal tuberculosis. Am. Rev. Tuberc. 1952, 66, 391–415. [Google Scholar] [PubMed]
- Nash, J.C.; Grosfeld, W. Isoniazid and iproniazid resistance in pulmonary tuberculosis. J. Am. Med. Assoc. 1952, 150, 813. [Google Scholar]
- Mast, Y.; Wohlleben, W. Streptogramins—Two are better than one! Int. J. Med. Microbiol. 2014, 304, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Jolles, G.; Terlain, B.; Thomas, J.P. Metabolic investigations on pristinamycin. Nature 1965, 207, 199–200. [Google Scholar] [CrossRef]
- Dublanchet, A.; Soussy, C.J.; Squinazi, F.; Duval, J. Resistance to streptogramin antibiotics in Staphylococcus aureus. Ann. Microbiol. 1977, 128A, 277–287. [Google Scholar]
- Rist, N.; Grumbach, F.; Libermann, D. Experiments on the antituberculous activity of alpha-ethylthioisonicotinamide. Am. Rev. Tuberc. 1959, 79, 1–5. [Google Scholar]
- Robson, J.M.; Sullivan, F.M. Antituberculosis drugs. Pharmacol. Rev. 1963, 15, 169–223. [Google Scholar]
- Fairbrother, R.W.; Williams, B.L. Two new antibiotics: Antibacterial activity of novobiocin and vancomycin. Lancet 1956, 268, 1177–1179. [Google Scholar] [CrossRef]
- Geraci, J.E.; Heilman, F.R.; Nichols, D.R.; Wellman, W.E. Antibiotic therapy of bacterial endocarditis. VII. Vancomycin for acute micrococcal endocarditis; preliminary report. Proc. Staff Meet. Mayo Clin. 1958, 33, 172–181. [Google Scholar]
- Courvalin, P. Vancomycin resistance in Gram-positive cocci. Clin. Infect. Dis. 2006, 42, S25–S34. [Google Scholar] [CrossRef] [PubMed]
- De Boer, C.; Dietz, A.; Wilkins, J.R.; Lewis, C.N.; Savage, G.M. Celesticetin—A new, crystalline antibiotic. I. Biologic studies of celesticetin. In Antibiotics Annual, 6th ed.; Welch, H., Marti-Ibanez, F., Eds.; Interscience Publishers: Chichester, UK, 1955; pp. 831–836. [Google Scholar]
- Schaffer, L.; Finkelstein, J.; Hohn, A.; Lees, T.M.; Lenert, T.F.; Means, J.A.; P’an, S.Y.; Regna, P.P.; Routien, J.B.; Sobin, B.A.; et al. Lincomycin—A new antibiotic: Studies in children carrying β-hemolytic streptococci in association with acute pharyngitis, tonsillitis, or both. Clin. Pediatrics 1963, 2, 642–645. [Google Scholar] [CrossRef] [PubMed]
- Desmyter, J. Lincomycin resistance of erythromycin-resistant cocci. N. Engl. J. Med. 1968, 278, 967. [Google Scholar]
- Epstein, I.G.; Nair, K.G.; Boyd, L.J. Cycloserine, a new antibiotic, in the treatment of human pulmonary tuberculosis: A preliminary report. Antibiot. Med. Clin. Ther. 1955, 1, 80–93. [Google Scholar]
- Epstein, I.G.; Nair, K.G.; Boyd, L.J. The treatment of human pulmonary tuberculosis with cycloserine: Progress report. Dis. Chest 1956, 29, 241–257. [Google Scholar] [CrossRef]
- Storey, P.B.; Mclean, R.L. A current appraisal of cycloserine. Antibiot. Med. Clin. Ther. 1957, 4, 223–232. [Google Scholar]
- Sensi, P. History of the development of rifampin. Rev. Infect. Dis. 1983, 5, S402–S406. [Google Scholar] [CrossRef]
- Kontomichalou, P.; Papadakis, Z.; Daikos, G. Rifamycin SV: Clinical and laboratory experience. Chemotherapy 1963, 7, 357–364. [Google Scholar] [CrossRef]
- Manten, A.; van Wijngaarden, L.J. Development of drug resistance to rifampicin. Chemotherapy 1969, 14, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Van Dijck, P.J.; De Somer, P. Ramycin: A new antibiotic. J. Gen. Microbiol. 1958, 18, 377–381. [Google Scholar] [CrossRef]
- Godtfredsen, W.O.; Jahnsen, S.; Lorck, H.; Roholt, K.; Tybring, L. Fusidic acid: A new antibiotic. Nature 1962, 193, 987. [Google Scholar] [CrossRef] [PubMed]
- Vanderhaeghe, H.; van Dijck, P.; De Somer, P. Identity of ramycin with fusidic acid. Nature 1965, 205, 710–711. [Google Scholar] [CrossRef] [PubMed]
- Newman, R.L.; Bhat, K.M.; Hackney, R.; Robinson, C.; Stewart, G.T. Fusidic acid: Laboratory and clinical assessment. Br. Med. J. 1962, 2, 1645. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Evans, R.J.; Waterworth, P.M. Naturally-occurring fusidic acid resistance in staphylococci and its linkage to other resistances. J. Clin. Pathol. 1966, 19, 555. [Google Scholar] [CrossRef] [PubMed]
- Cosar, C.; Julou, L. The activity of 1-(2-hydroxyethyl)-2-methyl-5-nitroimidazole (R. P. 8823) against experimental Trichomonas vaginalis infections. Ann. Inst. Pasteur 1959, 96, 238–241. [Google Scholar]
- Shinn, D.L.S. Metronidazole in acute ulcerative gingivitis. Lancet 1962, 279, 1191. [Google Scholar] [CrossRef]
- Ingham, H.R.; Eaton, S.; Venables, C.W.; Adams, P.C. Bacteroides fragilis resistant to metronidazole after long-term therapy. Lancet 1978, 1, 214. [Google Scholar] [CrossRef]
- Thomas, J.P.; Baughn, C.O.; Wilkinson, R.G.; Shepherd, R.G. A new synthetic compound with antituberculous activity in mice: Ethambutol (dextro-2,2′-(ethylenediimino)-di-l-butanol). Am. Rev. Respir. Dis. 1961, 83, 891–893. [Google Scholar]
- Carr, R.E.; Henkind, P. Ocular manifestations of ethambutol, toxic amblyopia after administration of an experimental antituberculous drug. Arch. Ophthalmol. 1962, 67, 566–571. [Google Scholar] [CrossRef]
- Hobby, G.L.; Johnson, P.M.; Boytar-Papirnyik, V.; Wilber, J. Primary drug resistance: A continuing study of tubercle bacilli in a veteran population within the United States. VI. Initial observations on the incidence of resistance to rifampin and ethambutol. Am. Rev. Respir. Dis. 1969, 99, 777–779. [Google Scholar]
- Lesher, G.Y.; Froelich, E.J.; Gruett, M.D.; Bailey, J.H.; Brundage, R.P. 1,8-naphthyridine derivatives. A new class of chemotherapeutic agents. J. Med. Pharm. Chem. 1962, 91, 1063–1065. [Google Scholar] [CrossRef] [PubMed]
- Barlow, A.M. Nalidixic acid in infections of urinary tract. Br. Med. J. 1963, 2, 1308. [Google Scholar] [CrossRef] [PubMed]
- Ronald, A.R.; Turck, M.; Petersdorf, R.G. A critical evaluation of nalidixic acid in urinary-tract infections. N. Engl. J. Med. 1966, 275, 1081–1089. [Google Scholar] [CrossRef]
- Hendlin, D.; Stapley, E.O.; Jackson, M.; Wallick, H.; Miller, A.K.; Wolf, F.J.; Miller, T.W.; Chaiet, L.; Kahan, F.M.; Foltz, E.L.; et al. Phosphonomycin, a new antibiotic produced by strains of streptomyces. Science 1969, 166, 122–123. [Google Scholar] [CrossRef] [PubMed]
- Lagunero, R.L.; Menéndez, M.L. Urinary tract infections treated with phosphonomycin (author’s translation). Folia Clin. Int. 1974, 24, 130–148. [Google Scholar]
- Courtieu, A.L.; Drugeon, H.; Billaudel, S. Susceptibility to fosfomycin of hospital strains isolated in Nantes (France). Frequency of mutation to resistance. Chemotherapy 1977, 23, 25–36. [Google Scholar] [CrossRef]
- Fuller, A.T.; Mellows, G.; Woolford, M.; Banks, G.T.; Barrow, K.D.; Chain, E.B. Pseudomonic acid: An antibiotic produced by Pseudomonas fluorescens. Nature 1971, 234, 416–417. [Google Scholar] [CrossRef] [PubMed]
- Lever, L.R.; Leigh, D.A.; Wilkinson, J.D. A double-blind study to assess the effectiveness of mupirocin in the treatment of infected eczema. Br. J. Dermatol. 1985, 113, 35–36. [Google Scholar] [CrossRef]
- Rahman, M.; Noble, W.C.; Cookson, B.; Baird, D.; Coia, J. Mupirocin-resistant Staphylococcus aureus. Lancet 1987, 330, 387–388. [Google Scholar] [CrossRef]
- Coronelli, C.; White, R.J.; Lancini, G.C.; Parenti, F. Lipiarmycin, a new antibiotic from Actinoplanes. II. Isolation, chemical, biological and biochemical characterization. J. Antibiot. 1975, 28, 253–259. [Google Scholar] [CrossRef]
- Citron, D.M.; Babakhani, F.; Goldstein, E.J.C.; Nagaro, K.; Sambol, S.; Sears, P.; Shue, Y.-K.; Gerding, D.N. Typing and susceptibility of bacterial isolates from the fidaxomicin (OPT-80) phase II study for C. difficile infection. Anaerobe 2009, 15, 234–236. [Google Scholar] [CrossRef] [PubMed]
- Schwanbeck, J.; Riedel, T.; Laukien, F.; Schober, I.; Oehmig, I.; Zimmermann, O.; Overmann, J.; Groß, U.; Zautner, A.E.; Bohne, W. Characterization of a clinical Clostridioides difficile isolate with markedly reduced fidaxomicin susceptibility and a V1143D mutation in rpoB. J. Antimicrob. Chemother. 2019, 74, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Baker, F.; Cama, L.D.; Christensen, B.G.; Leanza, W.J.; Shih, D.H.; Wildonger, K.J. Thienamycin, imipenem and new members of the carbapenem class of β-lactam antibiotics. In IUPHAR 9th International Congress of Pharmacology London 1984; Paton, W., Mitchell, J., Turner, P., Eds.; Palgrave Macmillan: London, UK, 1984; pp. 105–109. [Google Scholar]
- Eron, L.J.; Hixon, D.L.; Park, C.H.; Goldenberg, R.I.; Poretz, D.M. Imipenem versus moxalactam in the treatment of serious infections. Antimicrob. Agents Chemother. 1983, 24, 841. [Google Scholar] [CrossRef]
- Quinn, J.P.; Dudek, E.J.; DiVincenzo, C.A.; Lucks, D.A.; Lerner, S.A. Emergence of resistance to imipenem during therapy for Pseudomonas aeruginosa infections. J. Infect. Dis. 1986, 154, 289–294. [Google Scholar] [CrossRef]
- Percival, A.; Thomas, E.; Hart, C.A.; Karayiannis, P. In-vitro activity of monobactam, SQ 26,776, against Gram-negative bacteria. J. Antimicrob. Chemother. 1981, 8, 49–55. [Google Scholar] [CrossRef]
- Giamarellou, H.; Galanakis, N.; Douzinas, E.; Petrikkos, G.; El Messidi, M.; Papoulias, G.; Daikos, G.K. Evaluation of aztreonam in difficult-to-treat infections with prolonged posttreatment follow-up. Antimicrob. Agents Chemother. 1984, 26, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Dworzack, D.L.; Bartelt, M.A.; Bailey, R.T.; Fitzgibbons, R.J.; Reich, J.W.; Picetti, G.D. Emergence of resistance to aztreonam. Clin. Pharm. 1984, 3, 467–470. [Google Scholar]
- Slee, A.M.; Wuonola, M.A.; McRipley, R.J.; Zajac, I.; Zawada, M.J.; Bartholomew, P.T.; Gregory, W.A.; Forbes, M. Oxazolidinones, a new class of synthetic antibacterial agents: In vitro and in vivo activities of DuP 105 and DuP 721. Antimicrob. Agents Chemother. 1987, 31, 1791–1797. [Google Scholar] [CrossRef]
- Riedl, B.; Endermann, R. Recent developments with oxazolidinone antibiotics. Expert Opin. Ther. Pat. 1999, 9, 625–633. [Google Scholar] [CrossRef]
- Tsiodras, S.; Gold, H.S.; Sakoulas, G.; Eliopoulos, G.M.; Wennersten, C.; Venkataraman, L.; Moellering, R.C.; Ferraro, M.J. Linezolid resistance in a clinical isolate of Staphylococcus aureus. Lancet 2001, 358, 207–208. [Google Scholar] [CrossRef]
- Ehlert, F.; Neu, H.C. In vitro activity of LY146032 (daptomycin), a new peptolide. Eur. J. Clin. Microbiol. 1987, 6, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Tally, F.P.; Zeckel, M.; Wasilewski, M.M.; Carini, C.; Berman, C.L.; Drusano, G.L.; Oleson, F.B. Daptomycin: A novel agent for Gram-positive infections. Expert Opin. Investig. Drugs 1999, 8, 1223–1238. [Google Scholar] [CrossRef]
- Lewis, J.S.; Owens, A.; Cadena, J.; Sabol, K.; Patterson, J.E.; Jorgensen, J.H. Emergence of daptomycin resistance in Enterococcus faecium during daptomycin therapy. Antimicrob. Agents Chemother. 2005, 49, 1664–1665. [Google Scholar]
- Andries, K.; Verhasselt, P.; Guillemont, J.; Göhlmann, H.W.H.; Neefs, J.-M.; Winkler, H.; van Gestel, F.; Timmerman, P.; Zhu, M.; Lee, E.; et al. A diarylquinoline drug active on the ATP synthase of Mycobacterium tuberculosis. Science 2005, 307, 223–227. [Google Scholar] [CrossRef] [PubMed]
- Rustomjee, R.; Diacon, A.H.; Allen, J.; Venter, A.; Reddy, C.; Patientia, R.F.; Mthiyane, T.C.P.; de Marez, T.; van Heeswijk, R.; Kerstens, R.; et al. Early bactericidal activity and pharmacokinetics of the diarylquinoline TMC207 in treatment of pulmonary tuberculosis. Antimicrob. Agents Chemother. 2008, 52, 2831. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).