Successful Integration of Clinical Pharmacists in an OPAT Program: A Real-Life Multidisciplinary Circuit
Abstract
1. Introduction
Main Barriers for Efficient OPAT Implementation
2. Effectiveness, Safety, and Cost-Effectiveness
2.1. Clinical Effectiveness of OPAT
2.2. OPAT Safety
2.2.1. Catheter-Related Complications
2.2.2. ADRs and Drug Interactions
2.3. Cost-Effectiveness of OPAT
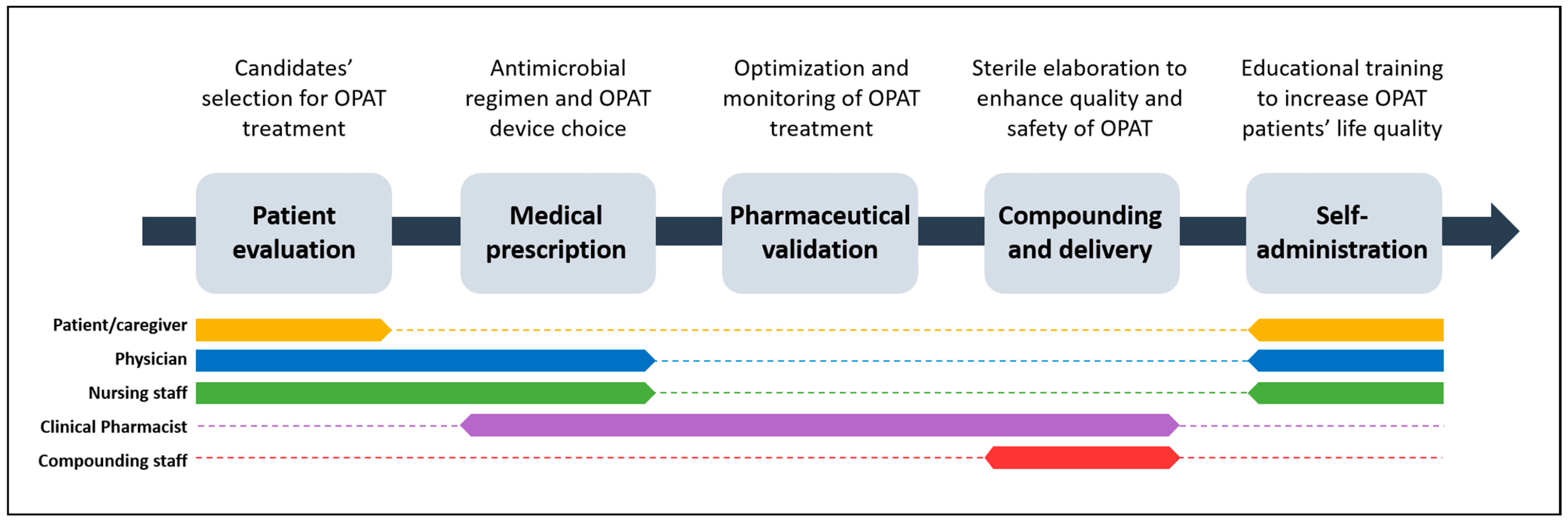
3. Implementation of an OPAT Multidisciplinary Circuit
3.1. Patient Evaluation
3.2. Medical Prescription
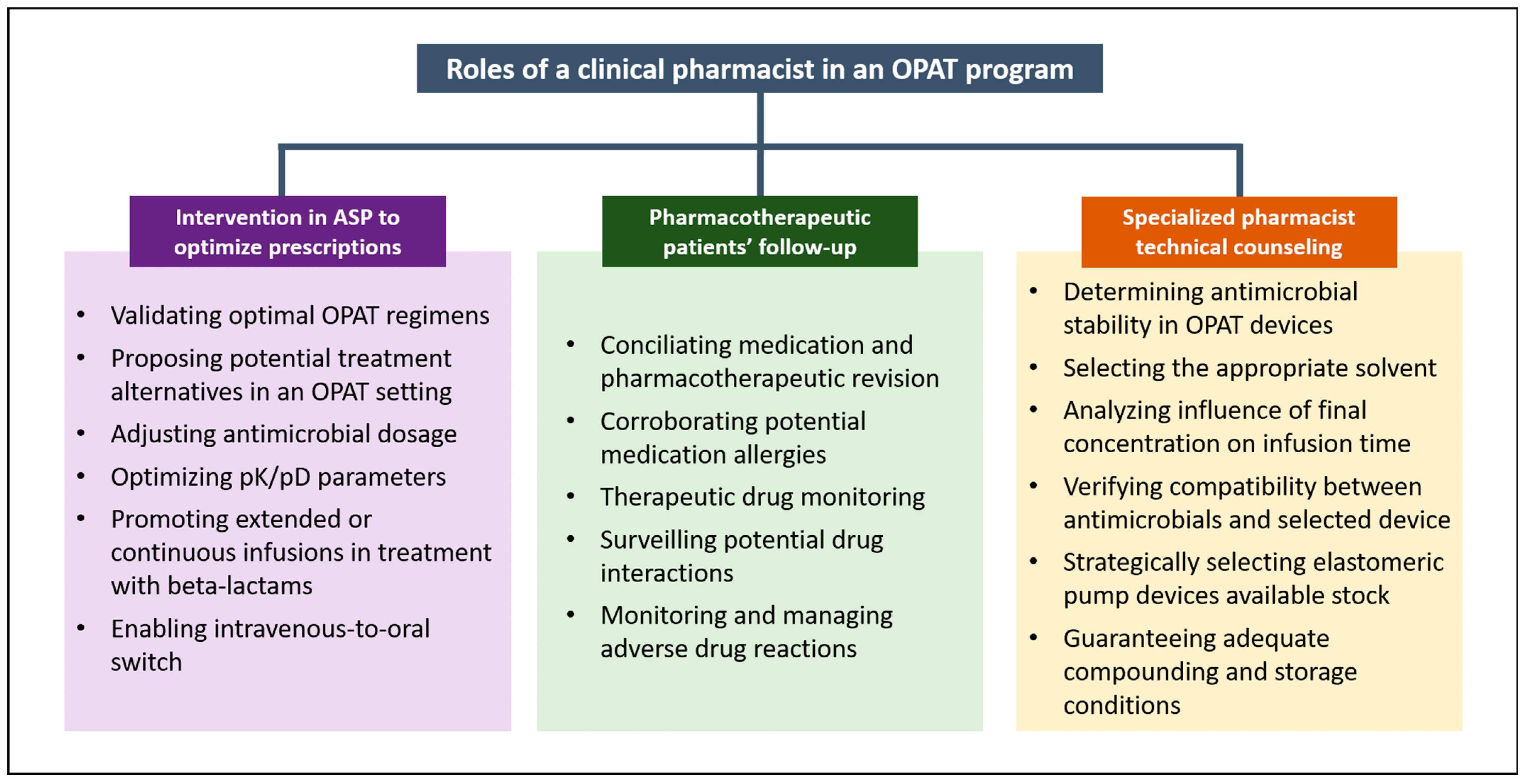
3.3. Clinical Pharmaceutical Validation: Involvement of Pharmacists in an OPAT Program
3.3.1. Intervention in ASP to Optimize OPAT Prescriptions
3.3.2. Pharmacotherapeutic Patient Follow-Up
3.3.3. OPAT-Specialized Pharmacist Technical Counselling
3.4. OPAT Technical Compounding and Delivery
Compounding and Delivery Procedure in our OPAT Program
3.5. Self-Administration
3.5.1. Selection of Vascular Catheter and Catheter Care
- PICC: Used for long-term OPAT (>3–4 weeks) and allows multidose daily administration as well as bitherapy.
- Midline catheters: Employed for mid-term OPAT (between 2 and 3 weeks). Mainly used for once- or twice-daily OPAT administration. Our team has also successfully employed midline catheters for OPAT regimens with frequencies of every 6–8 h.
- Peripheral venous catheter: Used for short-term OPAT (less than 10 days of treatment) and only recommended in once-daily regimens.
3.5.2. Counselling on OPAT Storage Conditions
4. Managing Pharmacy Department in an OPAT Multidisciplinary Circuit
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tice, A.D.; Rehm, S.J.; Dalovisio, J.R.; Bradley, J.S.; Martinelli, L.P.; Graham, D.R.; Gainer, R.B.; Kunkel, M.J.; Yancey, R.W.; Williams, D.N.; et al. Practice Guidelines for Outpatient Parenteral Antimicrobial Therapy. IDSA Guidelines. Clin. Infect. Dis. 2004, 38, 1651–1672. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.N. Home Intravenous Antibiotic Therapy (HIVAT): Indications, Patients and Antimicrobial Agents. Int. J. Antimicrob. Agents 1995, 5, 3–8. [Google Scholar] [CrossRef]
- Mujal Martínez, A.; Solá Aznar, J.; Hernández Ávila, M.; Aragüás Flores, C.; Machado Sicilia, M.L.; Oristrell Salvá, J. Safety and Efficacy of Home Intravenous Antibiotic Therapy for Patients Referred by the Hospital Emergency Department. Emergencias 2013, 25, 31–36. [Google Scholar]
- Garde, C.; Goenaga, M.A. Tratamiento Antibiótico Parenteral En El Paciente Ambulatorio. Enferm. Infecc. Microbiol. Clin. 2005, 23, 393–395. [Google Scholar] [CrossRef] [PubMed]
- González Ramallo, V.J.; Valdivieso Martínez, B.; Ruiz García, V. Hospital at Home. Med. Clin. 2002, 118, 659–664. [Google Scholar] [CrossRef]
- Montalto, M.; Portelli, R.; Collopy, B. Measuring the Quality of Hospital in the Home Care: A Clinical Indicator Approach. Int. J. Qual. Health Care 1999, 11, 413–418. [Google Scholar] [CrossRef]
- Bentur, N. Hospital at Home: What Is Its Place in the Health System? Health Policy 2001, 55, 71–79. [Google Scholar] [CrossRef]
- Mujal Martínez, A.; Mirón-Rubio, M. Decálogo Sobre el TADE; Sociedad Española de Hospitalización a Domicilio (SEHAD): Madrid, Spain, 2021. [Google Scholar]
- Seaton, R.A.; Ritchie, N.D.; Robb, F.; Stewart, L.; White, B.; Vallance, C. From “OPAT” to “COpAT”: Implications of the OVIVA Study for Ambulatory Management of Bone and Joint Infection. J. Antimicrob. Chemother. 2019, 74, 2119–2121. [Google Scholar] [CrossRef]
- López Cortés, L.E.; Mujal Martínez, A.; Fernández Martínez de Mandojana, M.; Martín, N.; Gil Bermejo, M.; Solà Aznar, J.; Villegas Bruguera, E.; Peláez Cantero, M.J.; Retamar Gentil, P.; Delgado Vicente, M.; et al. Executive Summary of Outpatient Parenteral Antimicrobial Therapy: Guidelines of the Spanish Society of Clinical Microbiology and Infectious Diseases and the Spanish Domiciliary Hospitalisation Society. Enferm. Infecc. Microbiol. Clin. 2019, 37, 405–409. [Google Scholar] [CrossRef]
- García-Lamberechts, E.J.; González-Del Castillo, J.; Hormigo-Sánchez, A.I.; Núñez-Orantos, M.J.; Candel, F.J.; Martín-Sánchez, F.J. Factors Predicting Failure in Empirical Antibiotic Treatment. An. Sist. Sanit. Navar. 2017, 40, 119–130. [Google Scholar] [CrossRef]
- Mirón Rubio, M.; Estrada Cuxart, O.; González Ramallo, V.J. Protocolos Tratamiento Antimicrobiano Domiciliario Endovenoso (TADE), 1st ed.; Sociedad Española de Medicina Interna and Elsevier España: Madrid, Spain, 2008; ISBN 978-84-691-3742-0. [Google Scholar]
- Hale, C.M.; Steele, J.M.; Seabury, R.W.; Miller, C.D. Characterization of Drug-Related Problems Occurring in Patients Receiving Outpatient Antimicrobial Therapy. J. Pharm. Pract. 2017, 30, 600–605. [Google Scholar] [CrossRef] [PubMed]
- Keller, S.C.; Cosgrove, S.E.; Arbaje, A.I.; Chang, R.H.; Krosche, A.; Williams, D.; Gurses, A.P. It’s Complicated: Patient and Informal Caregiver Performance of Outpatient Parenteral Antimicrobial Therapy-Related Tasks. Am. J. Med. Qual. 2020, 35, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Hamad, Y.; Lane, M.A.; Beekmann, S.E.; Polgreen, P.M.; Keller, S.C. Perspectives of United States-Based Infectious Diseases Physicians on Outpatient Parenteral Antimicrobial Therapy Practice. Open Forum Infect. Dis. 2019, 6, ofz363. [Google Scholar] [CrossRef] [PubMed]
- Marks, M.; Bell, L.C.K.; Jones, I.; Rampling, T.; Kranzer, K.; Morris-Jones, S.; Logan, S.; Pollara, G. Clinical and Economic Impact of Implementing OVIVA Criteria on Patients With Bone and Joint Infections in Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2020, 71, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Hamad, Y.; Dodda, S.; Frank, A.; Beggs, J.; Sleckman, C.; Kleinschmidt, G.; Lane, M.A.; Burnett, Y. Perspectives of Patients on Outpatient Parenteral Antimicrobial Therapy: Experiences and Adherence. Open Forum Infect. Dis. 2020, 7, ofaa205. [Google Scholar] [CrossRef]
- Ruh, C.A.; Parameswaran, G.I.; Wojciechowski, A.L.; Mergenhagen, K.A. Outcomes and Pharmacoeconomic Analysis of a Home Intravenous Antibiotic Infusion Program in Veterans. Clin. Ther. 2015, 37, 2527–2535. [Google Scholar] [CrossRef]
- Berrevoets, M.A.H.; ten Oever, J.; Oerlemans, A.J.M.; Kullberg, B.J.; Hulscher, M.E.; Schouten, J.A. Quality Indicators for Appropriate Outpatient Parenteral Antimicrobial Therapy in Adults: A Systematic Review and RAND-Modified Delphi Procedure. Clin. Infect. Dis. 2020, 70, 1075–1082. [Google Scholar] [CrossRef]
- Le Maréchal, M.; Tebano, G.; Monnier, A.A.; Adriaenssens, N.; Gyssens, I.C.; Huttner, B.; Milanic, R.; Schouten, J.; Stanic Benic, M.; Versporten, A.; et al. Quality Indicators Assessing Antibiotic Use in the Outpatient Setting: A Systematic Review Followed by an International Multidisciplinary Consensus Procedure. J. Antimicrob. Chemother. 2018, 73, vi40–vi49. [Google Scholar] [CrossRef]
- Sadler, E.D.; Avdic, E.; Cosgrove, S.E.; Hohl, D.; Grimes, M.; Swarthout, M.; Dzintars, K.; Lippincott, C.K.; Keller, S.C. Failure Modes and Effects Analysis to Improve Transitions of Care in Patients Discharged on Outpatient Parenteral Antimicrobial Therapy. Am. J. Health Syst. Pharm. 2021, 78, 1223–1232. [Google Scholar] [CrossRef]
- Bugeja, S.J.; Stewart, D.; Strath, A.; Vosper, H. Human Factors Approaches to Evaluating Outpatient Parenteral Antimicrobial Therapy Services: A Systematic Review. Res. Soc. Adm. Pharm. 2020, 16, 614–627. [Google Scholar] [CrossRef]
- Mirón-Rubio, M.; González-Ramallo, V.; Estrada-Cuxart, O.; Sanroma-Mendizábal, P.; Segado-Soriano, A.; Mujal-Martínez, A.; del Río-Vizoso, M.; García-Lezcano, M.; Martín-Blanco, N.; Florit-Serra, L.; et al. Intravenous Antimicrobial Therapy in the Hospital-at-Home Setting: Data from the Spanish Outpatient Parenteral Antimicrobial Therapy Registry. Future Microbiol. 2016, 11, 375–390. [Google Scholar] [CrossRef] [PubMed]
- Quintens, C.; Steffens, E.; Jacobs, K.; Schuermans, A.; van Eldere, J.; Lagrou, K.; de Munter, P.; Derdelinckx, I.; Peetermans, W.E.; Spriet, I. Efficacy and Safety of a Belgian Tertiary Care Outpatient Parenteral Antimicrobial Therapy (OPAT) Program. Infection 2020, 48, 357–366. [Google Scholar] [CrossRef]
- al Shareef, H.J.; al Harbi, A.; Alatawi, Y.; Aljabri, A.; Al-Ghanmi, M.A.; Alzahrani, M.S.; Algarni, M.A.; Khobrani, A.; Haseeb, A.; AlSenani, F.; et al. Evaluate the Effectiveness of Outpatient Parenteral Antimicrobial Therapy (OPAT) Program in Saudi Arabia: A Retrospective Study. Antibiotics 2022, 11, 441. [Google Scholar] [CrossRef] [PubMed]
- Sanroma, P.; Muñoz, P.; Mirón-Rubio, M.; Aguilera, A.; Estrada, O.; García, D.; González-Ramallo, V.J.; Pajarón, M.; Sgaramella, G.A.; González, C.R.; et al. Effectiveness and Safety of Ertapenem Used in Hospital-at-Home Units: Data from Spanish Outpatient Parenteral Antimicrobial Therapy Registry. Future Microbiol. 2018, 13, 1363–1373. [Google Scholar] [CrossRef] [PubMed]
- Voumard, R.; Gardiol, C.; André, P.; Arensdorff, L.; Cochet, C.; Boillat-Blanco, N.; Decosterd, L.; Buclin, T.; de Vallière, S. Efficacy and Safety of Continuous Infusions with Elastomeric Pumps for Outpatient Parenteral Antimicrobial Therapy (OPAT): An Observational Study. J. Antimicrob. Chemother. 2018, 73, 2540–2545. [Google Scholar] [CrossRef] [PubMed]
- Nathwani, D. The Management of Skin and Soft Tissue Infections: Outpatient Parenteral Antibiotic Therapy in the United Kingdom. Chemotherapy 2001, 47 (Suppl. 1), 17–23. [Google Scholar] [CrossRef]
- Pérez-López, J.; San José Laporte, A.; Pardos-Gea, J.; Tapia Melenchón, E.; Lozano Ortín, E.; Barrio Guirado, A.; Vilardell Tarrés, M. Safety and Efficacy of Home Intravenous Antimicrobial Infusion Therapy in Older Patients: A Comparative Study with Younger Patients. Int. J. Clin. Pract. 2008, 62, 1188–1192. [Google Scholar] [CrossRef]
- Pérez López, J.; San José Laporte, A.; Alemán Mansó, C.; Pardos-Gea, J.; Vilardell Tarrés, M. Intravenous Antibiotic Treatment in a Hospital Based Home Care Unit. Predictors of Hospital Readmission. Med. Clin. 2008, 131, 290–292. [Google Scholar] [CrossRef]
- Chapman, A.L.N.; Dixon, S.; Andrews, D.; Lillie, P.J.; Bazaz, R.; Patchett, J.D. Clinical Efficacy and Cost-Effectiveness of Outpatient Parenteral Antibiotic Therapy (OPAT): A UK Perspective. J. Antimicrob. Chemother. 2009, 64, 1316–1324. [Google Scholar] [CrossRef]
- Mackintosh, C.L.; White, H.A.; Seaton, R.A. Outpatient Parenteral Antibiotic Therapy (OPAT) for Bone and Joint Infections: Experience from a UK Teaching Hospital-Based Service. J. Antimicrob. Chemother. 2011, 66, 408–415. [Google Scholar] [CrossRef]
- Saini, E.; Ali, M.; Du, P.; Crook, T.; Zurlo, J. Early Infectious Disease Outpatient Follow-up of Outpatient Parenteral Antimicrobial Therapy Patients Reduces 30-Day Readmission. Clin. Infect. Dis. 2019, 69, 865–868. [Google Scholar] [CrossRef] [PubMed]
- Otu, A.A.; Bongomin, F.; Bazaz, R.; Harris, C.; Denning, D.W.; Kosmidis, C. Micafungin May Be Safely Administered as Outpatient Parenteral Antimicrobial Therapy for Chronic Pulmonary Aspergillosis. Mycoses 2019, 62, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Mujal, A.; Sola, J.; Hernandez, M.; Villarino, M.-A.; Baylina, M.; Tajan, J.; Oristrell, J. Safety and Effectiveness of Outpatient Parenteral Antimicrobial Therapy in Older People. J. Antimicrob. Chemother. 2016, 71, 1402–1407. [Google Scholar] [CrossRef] [PubMed]
- van Anglen, L.J.; Mandel, R.M.; Nathan, R.V.; Krinsky, A.H.; Luu, Q.; Bacon, A.E.; Baker, H.B.; Schroeder, C.P.; Couch, K.A. Safety and Effectiveness of Outpatient Parenteral Antimicrobial Therapy (OPAT) in the Aged Population. Open Forum Infect. Dis. 2017, 4, S331–S332. [Google Scholar] [CrossRef][Green Version]
- Subedi, S.; Looke, D.F.M.; McDougall, D.A.; Sehu, M.M.; Playford, E.G. Supervised Self-Administration of Outpatient Parenteral Antibiotic Therapy: A Report from a Large Tertiary Hospital in Australia. Int. J. Infect. Dis. 2015, 30, 161–165. [Google Scholar] [CrossRef]
- Williams, D.N.; Baker, C.A.; Kind, A.C.; Sannes, M.R. The History and Evolution of Outpatient Parenteral Antibiotic Therapy (OPAT). Int. J. Antimicrob. Agents 2015, 46, 307–312. [Google Scholar] [CrossRef]
- Browning, S.; Loewenthal, M.R.; Freelander, I.; Dobson, P.M.; Schneider, K.; Davis, J.S. Safety of Prolonged Outpatient Courses of Intravenous Antibiotics: A Prospective Cohort Study. Clin. Microbiol. Infect. 2022, 28, 832–837. [Google Scholar] [CrossRef]
- Krein, S.L.; Saint, S.; Trautner, B.W.; Kuhn, L.; Colozzi, J.; Ratz, D.; Lescinskas, E.; Chopra, V. Patient-Reported Complications Related to Peripherally Inserted Central Catheters: A Multicentre Prospective Cohort Study. BMJ Qual. Saf. 2019, 28, 574–581. [Google Scholar] [CrossRef]
- Grau, D.; Clarivet, B.; Lotthé, A.; Bommart, S.; Parer, S. Complications with Peripherally Inserted Central Catheters (PICCs) Used in Hospitalized Patients and Outpatients: A Prospective Cohort Study. Antimicrob. Resist. Infect. Control. 2017, 6, 18. [Google Scholar] [CrossRef]
- Schneider, L.V.; Duron, S.; Arnaud, F.-X.; Bousquet, A.; Kervella, Y.; Bouzad, C.; Baccialone, J.; A’Teriitehau, C.; Potet, J. Evaluation of PICC Complications in Orthopedic Inpatients with Bone Infection for Long-Term Intravenous Antibiotics Therapy. J. Vasc. Access 2015, 16, 299–308. [Google Scholar] [CrossRef]
- Bertoglio, S.; Faccini, B.; Lalli, L.; Cafiero, F.; Bruzzi, P. Peripherally Inserted Central Catheters (PICCs) in Cancer Patients under Chemotherapy: A Prospective Study on the Incidence of Complications and Overall Failures. J. Surg. Oncol. 2016, 113, 708–714. [Google Scholar] [CrossRef] [PubMed]
- Cotogni, P.; Barbero, C.; Garrino, C.; Degiorgis, C.; Mussa, B.; de Francesco, A.; Pittiruti, M. Peripherally Inserted Central Catheters in Non-Hospitalized Cancer Patients: 5-Year Results of a Prospective Study. Support. Care Cancer 2015, 23, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Szeinbach, S.L.; Pauline, J.; Villa, K.F.; Commerford, S.R.; Collins, A.; Seoane-Vazquez, E. Evaluating Catheter Complications and Outcomes in Patients Receiving Home Parenteral Nutrition. J. Eval. Clin. Pract. 2015, 21, 153–159. [Google Scholar] [CrossRef]
- Underwood, J.; Marks, M.; Collins, S.; Logan, S.; Pollara, G. Intravenous Catheter-Related Adverse Events Exceed Drug-Related Adverse Events in Outpatient Parenteral Antimicrobial Therapy. J. Antimicrob. Chemother. 2019, 74, 787–790. [Google Scholar] [CrossRef]
- Seo, H.; Altshuler, D.; Dubrovskaya, Y.; Nunnally, M.E.; Nunn, C.; Ello, N.; Papadopoulos, J.; Chen, X.J. The Safety of Midline Catheters for Intravenous Therapy at a Large Academic Medical Center. Ann. Pharmacother. 2020, 54, 232–238. [Google Scholar] [CrossRef]
- Keller, S.C.; Williams, D.; Gavgani, M.; Hirsch, D.; Adamovich, J.; Hohl, D.; Gurses, A.P.; Cosgrove, S.E. Rates of and Risk Factors for Adverse Drug Events in Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2018, 66, 11–19. [Google Scholar] [CrossRef]
- Allison, G.M.; Muldoon, E.G.; Kent, D.M.; Paulus, J.K.; Ruthazer, R.; Ren, A.; Snydman, D.R. Prediction Model for 30-Day Hospital Readmissions among Patients Discharged Receiving Outpatient Parenteral Antibiotic Therapy. Clin. Infect. Dis. 2014, 58, 812–819. [Google Scholar] [CrossRef]
- Seetoh, T.; Lye, D.C.; Cook, A.R.; Archuleta, S.; Chan, M.; Sulaiman, Z.; Zhong, L.; Llorin, R.M.; Balm, M.; Fisher, D. An Outcomes Analysis of Outpatient Parenteral Antibiotic Therapy (OPAT) in a Large Asian Cohort. Int. J. Antimicrob. Agents 2013, 41, 569–573. [Google Scholar] [CrossRef] [PubMed]
- Grau, S.; de Antonio-Cuscó, M.; Ortonobes-Roig, S.; Los-Arcos, I.; Jiménez, M.J.; Soy, D. Personalized Antimicrobial Therapy in Critical and Elderly Patients. Farm. Hosp. 2021, 45, 64–76. [Google Scholar]
- Barr, D.A.; Semple, L.; Seaton, R.A. Outpatient Parenteral Antimicrobial Therapy (OPAT) in a Teaching Hospital-Based Practice: A Retrospective Cohort Study Describing Experience and Evolution over 10 Years. Int. J. Antimicrob. Agents 2012, 39, 407–413. [Google Scholar] [CrossRef]
- Hitchcock, J.; Jepson, A.P.; Main, J.; Wickens, H.J. Establishment of an Outpatient and Home Parenteral Antimicrobial Therapy Service at a London Teaching Hospital: A Case Series. J. Antimicrob. Chemother. 2009, 64, 630–634. [Google Scholar] [CrossRef] [PubMed]
- Paladino, J.A.; Poretz, D. Outpatient Parenteral Antimicrobial Therapy Today. Clin. Infect. Dis. 2010, 51 (Suppl. 2), S198–S208. [Google Scholar] [CrossRef] [PubMed]
- Dimitrova, M.; Gilchrist, M.; Seaton, R.A. Outpatient Parenteral Antimicrobial Therapy (OPAT) versus Inpatient Care in the UK: A Health Economic Assessment for Six Key Diagnoses. BMJ Open 2021, 11, e049733. [Google Scholar] [CrossRef]
- González-Ramallo, V.J.; Mirón-Rubio, M.; Mujal, A.; Estrada, O.; Forné, C.; Aragón, B.; Rivera, A.J. Costs of Outpatient Parenteral Antimicrobial Therapy (OPAT) Administered by Hospital at Home Units in Spain. Int. J. Antimicrob. Agents 2017, 50, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Polo, A.; Ramon-Cortes, S.; Plaja-Dorca, J.; Bartolomé-Comas, R.; Vidal-Valdivia, L.; Soler-Palacín, P. Impacto del Tratamiento Antimicrobiano Domiciliario Endovenoso (TADE) Como Parte de un Programa de Optimización del uso de Antimicrobianos (PROA) Específico Para Pediatría. Enferm. Infecc. Microbiol. Clin. 2021. [Google Scholar] [CrossRef]
- Yong, C.; Fisher, D.A.; Sklar, G.E.; Li, S.-C. A Cost Analysis of Outpatient Parenteral Antibiotic Therapy (OPAT): An Asian Perspective. Int. J. Antimicrob. Agents 2009, 33, 46–51. [Google Scholar] [CrossRef]
- Sanromá Mendizábal, P.; Sanpedro García, I.; González Fernández, C.R.; Baños Canales, M.T. Recomendaciones Clínicas y Procedimientos. Hospitalización Domiciliaria, 1st ed.; Fundación Marqués de Valdecilla: Santander, Spain, 2011; ISBN 978-84-693-5969-3. [Google Scholar]
- Candel, F.J.; Julián-Jiménez, A.; González-Del Castillo, J. Current Status in Outpatient Parenteral Antimicrobial Therapy: A Practical View. Rev. Esp. Quimioter. 2016, 29, 55–68. [Google Scholar]
- Halilovic, J.; Christensen, C.L.; Nguyen, H.H. Managing an Outpatient Parenteral Antibiotic Therapy Team: Challenges and Solutions. Ther. Clin. Risk Manag. 2014, 10, 459–465. [Google Scholar] [CrossRef]
- Nolet, B.R. Patient Selection in Outpatient Parenteral Antimicrobial Therapy. Infect. Dis. Clin. N. Am. 1998, 12, 835–847. [Google Scholar] [CrossRef]
- High, K.P. Outpatient Parenteral Antimicrobial Therapy: A Long-Overdue Option for Older Adults. J. Am. Geriatr. Soc. 2007, 55, 792–793. [Google Scholar] [CrossRef]
- Diamantis, S.; Dawudi, Y.; Cassard, B.; Longuet, P.; Lesprit, P.; Gauzit, R. Home Intravenous Antibiotherapy and the Proper Use of Elastomeric Pumps: Systematic Review of the Literature and Proposals for Improved Use. Infect. Dis. Now 2021, 51, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Norris, A.H.; Shrestha, N.K.; Allison, G.M.; Keller, S.C.; Bhavan, K.P.; Zurlo, J.J.; Hersh, A.L.; Gorski, L.A.; Bosso, J.A.; Rathore, M.H.; et al. 2018 Infectious Diseases Society of America Clinical Practice Guideline for the Management of Outpatient Parenteral Antimicrobial Therapy. Clin. Infect. Dis. 2019, 68, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Chapman, A.L.N.; Seaton, R.A.; Cooper, M.A.; Hedderwick, S.; Goodall, V.; Reed, C.; Sanderson, F.; Nathwani, D.; BSAC/BIA OPAT Project Good Practice Recommendations Working Group. Good Practice Recommendations for Outpatient Parenteral Antimicrobial Therapy (OPAT) in Adults in the UK: A Consensus Statement. J. Antimicrob. Chemother. 2012, 67, 1053–1062. [Google Scholar] [CrossRef]
- Heintz, B.H.; Halilovic, J.; Christensen, C.L. Impact of a Multidisciplinary Team Review of Potential Outpatient Parenteral Antimicrobial Therapy Prior to Discharge from an Academic Medical Center. Ann. Pharmacother. 2011, 45, 1329–1337. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.J.; Bergman, S.J.; Graham, D.R.; Glenn, S. Monitoring of Outpatient Parenteral Antimicrobial Therapy and Implementation of Clinical Pharmacy Services at a Community Hospital Infusion Unit. J. Pharm. Pract. 2015, 28, 462–468. [Google Scholar] [CrossRef] [PubMed]
- Chung, E.K.; Beeler, C.B.; Muloma, E.W.; Osterholzer, D.; Damer, K.M.; Erdman, S.M. Development and Implementation of a Pharmacist-Managed Outpatient Parenteral Antimicrobial Therapy Program. Am. J. Health Syst. Pharm. 2016, 73, e24–e33. [Google Scholar] [CrossRef]
- Docherty, T.; Schneider, J.J.; Cooper, J. Clinic- and Hospital-Based Home Care, Outpatient Parenteral Antimicrobial Therapy (OPAT) and the Evolving Clinical Responsibilities of the Pharmacist. Pharmacy 2020, 8, 233. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, M.V.; Childs-Kean, L.M.; Khan, P.; Rivera, C.G.; Stevens, R.W.; Ryan, K.L. Recent Updates in Antimicrobial Stewardship in Outpatient Parenteral Antimicrobial Therapy. Curr. Infect. Dis. Rep. 2021, 23, 24. [Google Scholar] [CrossRef]
- Petroff, B.J.; Filibeck, D.; Nowobilski-Vasilios, A.; Olsen, R.S.; Rollins, C.J.; Johnson, C. ASHP Guidelines on Home Infusion Pharmacy Services. Am. J. Health Syst. Pharm. 2014, 71, 325–341. [Google Scholar] [CrossRef]
- Oliveira, P.R.; Carvalho, V.C.; Cimerman, S.; Lima, A.L.M. Recommendations for Outpatient Parenteral Antimicrobial Therapy in Brazil. Braz. J. Infect. Dis. 2017, 21, 648–655. [Google Scholar] [CrossRef]
- Papic, I.; Vrca, V.B.; Marinović, I.; Samardžić, I.; Galešić, K. 4CPS-220 Clinical Pharmacist Interventions in Hospitalised Patients with Renal Impairment. Eur. J. Hosp. Pharm. 2018, 25, A144. [Google Scholar]
- Owens, R.C.; Shorr, A.F. Rational Dosing of Antimicrobial Agents: Pharmacokinetic and Pharmacodynamic Strategies. Am. J. Health Syst. Pharm. 2009, 66, S23–S30. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Hidalgo, L.; de Alarcón, A.; López-Cortes, L.E.; Luque-Márquez, R.; López-Cortes, L.F.; Gutiérrez-Valencia, A.; Gil-Navarro, M.V. Is Once-Daily High-Dose Ceftriaxone plus Ampicillin an Alternative for Enterococcus Faecalis Infective Endocarditis in Outpatient Parenteral Antibiotic Therapy Programs? Antimicrob. Agents Chemother. 2020, 65, e02099-20. [Google Scholar] [CrossRef] [PubMed]
- Vardakas, K.Z.; Voulgaris, G.L.; Maliaros, A.; Samonis, G.; Falagas, M.E. Prolonged versus Short-Term Intravenous Infusion of Antipseudomonal β-Lactams for Patients with Sepsis: A Systematic Review and Meta-Analysis of Randomised Trials. Lancet Infect. Dis. 2018, 18, 108–120. [Google Scholar] [CrossRef]
- Jones, B.M.; Huelfer, K.; Bland, C.M. Clinical and Safety Evaluation of Continuously Infused Ceftolozane/Tazobactam in the Outpatient Setting. Open Forum Infect. Dis. 2020, 7, ofaa014. [Google Scholar] [CrossRef] [PubMed]
- García-Queiruga, M.; Feal Cortizas, B.; Lamelo Alfonsín, F.; Pertega Diaz, S.; Martín-Herranz, I. Continuous Infusion of Antibiotics Using Elastomeric Pumps in the Hospital at Home Setting. Rev. Esp. Quimioter. 2021, 34, 200–206. [Google Scholar] [CrossRef]
- Farmer, E.C.W.; Seaton, R.A. Recent Innovations and New Applications of Outpatient Parenteral Antimicrobial Therapy. Expert. Rev. Anti. Infect. Ther. 2021, 19, 55–64. [Google Scholar] [CrossRef]
- Dryden, M.; Saeed, K.; Townsend, R.; Winnard, C.; Bourne, S.; Parker, N.; Coia, J.; Jones, B.; Lawson, W.; Wade, P.; et al. Antibiotic Stewardship and Early Discharge from Hospital: Impact of a Structured Approach to Antimicrobial Management. J. Antimicrob. Chemother. 2012, 67, 2289–2296. [Google Scholar] [CrossRef]
- Li, H.-K.; Rombach, I.; Zambellas, R.; Walker, A.S.; McNally, M.A.; Atkins, B.L.; Lipsky, B.A.; Hughes, H.C.; Bose, D.; Kümin, M.; et al. Oral versus Intravenous Antibiotics for Bone and Joint Infection. N. Engl. J. Med. 2019, 380, 425–436. [Google Scholar] [CrossRef]
- Iversen, K.; Ihlemann, N.; Gill, S.U.; Madsen, T.; Elming, H.; Jensen, K.T.; Bruun, N.E.; Høfsten, D.E.; Fursted, K.; Christensen, J.J.; et al. Partial Oral versus Intravenous Antibiotic Treatment of Endocarditis. N. Engl. J. Med. 2019, 380, 415–424. [Google Scholar] [CrossRef]
- Wen, W.; Li, H.; Wang, C.; Chen, C.; Tang, J.; Zhou, M.; Hong, X.; Cheng, Y.; Wu, Q.; Zhang, X.; et al. Efficacy and Safety of Outpatient Parenteral Antibiotic Therapy in Patients with Infective Endocarditis: A Meta-Analysis. Rev. Esp. Quimioter. 2022, 35, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Baré, M.; Lleal, M.; Ortonobes, S.; Gorgas, M.Q.; Sevilla-Sánchez, D.; Carballo, N.; de Jaime, E.; Herranz, S. Factors Associated to Potentially Inappropriate Prescribing in Older Patients According to STOPP/START Criteria: MoPIM Multicentre Cohort Study. BMC Geriatrics 2022, 22, 44. [Google Scholar] [CrossRef] [PubMed]
- Su, T.; Broekhuizen, B.D.L.; Verheij, T.J.M.; Rockmann, H. The Impact of Penicillin Allergy Labels on Antibiotic and Health Care Use in Primary Care: A Retrospective Cohort Study. Clin. Transl. Allergy 2017, 7, 18. [Google Scholar] [CrossRef]
- Blumenthal, K.G.; Peter, J.G.; Trubiano, J.A.; Phillips, E.J. Antibiotic Allergy. Lancet 2019, 393, 183–198. [Google Scholar] [CrossRef]
- Wijnakker, R.; Visser, L.E.; Schippers, E.F.; Visser, L.G.; van Burgel, N.D.; van Nieuwkoop, C. The Impact of an Infectious Disease Expert Team on Outpatient Parenteral Antimicrobial Treatment in the Netherlands. Int. J. Clin. Pharm. 2019, 41, 49–55. [Google Scholar] [CrossRef]
- Douiyeb, S.; de la Court, J.R.; Tuinte, B.; Sombogaard, F.; Schade, R.P.; Kuijvenhoven, M.; Minderhoud, T.; Sigaloff, K.C.E. Risk Factors for Readmission among Patients Receiving Outpatient Parenteral Antimicrobial Therapy: A Retrospective Cohort Study. Int. J. Clin. Pharm. 2022, 44, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Abdul–Aziz, M.H.; Brady, K.; Cotta, M.O.; Roberts, J.A. Therapeutic Drug Monitoring of Antibiotics: Defining the Therapeutic Range. Ther. Drug Monit. 2022, 44, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Shrestha, N.K.; Blaskewicz, C.; Gordon, S.M.; Everett, A.; Rehm, S.J. Safety of Outpatient Parenteral Antimicrobial Therapy in Nonagenarians. Open Forum Infect. Dis. 2020, 7, ofaa398. [Google Scholar] [CrossRef]
- Downes, K.J.; Goldman, J.L. Too Much of a Good Thing: Defining Antimicrobial Therapeutic Targets to Minimize Toxicity. Clin. Pharmacol. Ther. 2021, 109, 905–917. [Google Scholar] [CrossRef]
- Samura, M.; Takada, K.; Hirose, N.; Kurata, T.; Nagumo, F.; Koshioka, S.; Ishii, J.; Uchida, M.; Inoue, J.; Enoki, Y.; et al. Incidence of Elevated Creatine Phosphokinase between Daptomycin Alone and Concomitant Daptomycin and Statins: A Systematic Review and Meta-analysis. Br. J. Clin. Pharmacol. 2022, 88, 1985–1998. [Google Scholar] [CrossRef]
- Diamantis, S.; Longuet, P.; Lesprit, P.; Gauzit, R. Terms of Use of Outpatient Parenteral Antibiotic Therapy. Infect. Dis. Now 2021, 51, 14–38. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Rubio, B.; del Valle-Moreno, P.; Herrera-Hidalgo, L.; Gutiérrez-Valencia, A.; Luque-Márquez, R.; López-Cortés, L.E.; Gutiérrez-Urbón, J.M.; Luque-Pardos, S.; Fernández-Polo, A.; Gil-Navarro, M.V. Stability of Antimicrobials in Elastomeric Pumps: A Systematic Review. Antibiotics 2021, 11, 45. [Google Scholar] [CrossRef]
- Jenkins, A.; Shanu, S.; Jamieson, C.; Santillo, M. Widening the Net: A Literature Review of Antimicrobial Agents with Potential Suitability for Outpatient Parenteral Antimicrobial Therapy Services-the Importance of Storage and Stability. Eur. J. Hosp. Pharm. 2021. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, C.; Drummond, F.; Hills, T.; Ozolina, L.; Gilchrist, M.; Seaton, R.A.; Santillo, M.; Wilkinson, A.-S.; Allwood, M.C. Assessment of Ceftolozane/Tazobactam Stability in Elastomeric Devices and Suitability for Continuous Infusion via Outpatient Parenteral Antimicrobial Therapy. JAC Antimicrob. Resist. 2021, 3, dlab141. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.H.; Martin, E.K.; Nicolau, D.P.; Kuti, J.L. Assessment of Meropenem and Vaborbactam Room Temperature and Refrigerated Stability in Polyvinyl Chloride Bags and Elastomeric Devices. Clin. Ther. 2020, 42, 606–613. [Google Scholar] [CrossRef]
- Perks, S.J.; Lanskey, C.; Robinson, N.; Pain, T.; Franklin, R. Systematic Review of Stability Data Pertaining to Selected Antibiotics Used for Extended Infusions in Outpatient Parenteral Antimicrobial Therapy (OPAT) at Standard Room Temperature and in Warmer Climates. Eur. J. Hosp. Pharm. 2020, 27, 65–72. [Google Scholar] [CrossRef]
- Raby, E.; Naicker, S.; Sime, F.B.; Manning, L.; Wallis, S.C.; Pandey, S.; Roberts, J.A. Ceftolozane-Tazobactam in an Elastomeric Infusion Device for Ambulatory Care: An in Vitro Stability Study. Eur. J. Hosp. Pharm. 2020, 27, e84–e86. [Google Scholar] [CrossRef]
- Viaene, E.; Chanteux, H.; Servais, H.; Mingeot-Leclercq, M.-P.; Tulkens, P.M. Comparative Stability Studies of Antipseudomonal Beta-Lactams for Potential Administration through Portable Elastomeric Pumps (Home Therapy for Cystic Fibrosis Patients) and Motor-Operated Syringes (Intensive Care Units). Antimicrob. Agents Chemother. 2002, 46, 2327–2332. [Google Scholar] [CrossRef]
- Gaspar Carreño, M.; Torrico Martín, F.; Novajarque Sala, L.; Batista Cruz, M.; Ribeiro Gonçalves, P.; Porta Oltra, B.; Sánchez Santos, J.C. Parenteral Administration Medicines: Recommendations of Preparation, Administration and Stability. Farm. Hosp. 2014, 38, 461–467. [Google Scholar] [CrossRef]
- Medicine Online Information Center of Spanish Agency of Medicines and Health Products. Summary of Product Characteristics. AmBisome Liposomal 50 Mg Polvo Para Dispersión Para Perfusión. Available online: https://cima.aemps.es/cima/dochtml/ft/61117/FT_61117.html (accessed on 21 July 2022).
- Medicine Online Information Center of Spanish Agency of Medicines and Health Products. Summary of Product Characteristics. Cubicin 500 Mg Polvo Para Solución Inyectable y Para Perfusión. Available online: https://cima.aemps.es/cima/dochtml/ft/05328002/FT_05328002.html (accessed on 21 July 2022).
- Manning, L.; Wright, C.; Ingram, P.R.; Whitmore, T.J.; Heath, C.H.; Manson, I.; Page-Sharp, M.; Salman, S.; Dyer, J.; Davis, T.M.E. Continuous Infusions of Meropenem in Ambulatory Care: Clinical Efficacy, Safety and Stability. PLoS ONE 2014, 9, e102023. [Google Scholar] [CrossRef]
- Foy, F.; Luna, G.; Martinez, J.; Nizich, Z.; Seet, J.; Lie, K.; Sunderland, B.; Czarniak, P. An Investigation of the Stability of Meropenem in Elastomeric Infusion Devices. Drug Des. Devel. Ther. 2019, 13, 2655–2665. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, C.; Allwood, M.C.; Stonkute, D.; Wallace, A.; Wilkinson, A.-S.; Hills, T. BSAC Drug Stability Working Party Investigation of Meropenem Stability after Reconstitution: The Influence of Buffering and Challenges to Meet the NHS Yellow Cover Document Compliance for Continuous Infusions in an Outpatient Setting. Eur. J. Hosp. Pharm. 2020, 27, e53–e57. [Google Scholar] [CrossRef] [PubMed]
- Manrique-Rodríguez, S.; Heras-Hidalgo, I.; Pernia-López, M.S.; Herranz-Alonso, A.; del Río Pisabarro, M.C.; Suárez-Mier, M.B.; Cubero-Pérez, M.A.; Viera-Rodríguez, V.; Cortés-Rey, N.; Lafuente-Cabrero, E.; et al. Standardization and Chemical Characterization of Intravenous Therapy in Adult Patients: A Step Further in Medication Safety. Drugs R D 2021, 21, 39–64. [Google Scholar] [CrossRef]
- Quintens, C.; Spriet, I. 4CPS-049 Underdosing with High Dose Piperacillin/Tazobactam Administered via Continuous Infusion in Outpatient Parenteral Antimicrobial Therapy: A Stability or Viscosity Problem? Eur. J. Hosp. Pharm. 2020, 27, A70. [Google Scholar]
- Herrera-Hidalgo, L.; López-Cortes, L.E.; Luque-Márquez, R.; Gálvez-Acebal, J.; de Alarcón, A.; López-Cortes, L.F.; Gutiérrez-Valencia, A.; Gil-Navarro, M.V. Ampicillin and Ceftriaxone Solution Stability at Different Temperatures in Outpatient Parenteral Antimicrobial Therapy. Antimicrob. Agents Chemother. 2020, 64, e00309-20. [Google Scholar] [CrossRef]
- Medicine Online Information Center of Spanish Agency of Medicines and Health Products. Summary of Product Characteristics. Zerbaxa 1 g/0.5 g Polvo Para Concentrado Para Solución Para Perfusión. Available online: https://cima.aemps.es/cima/dochtml/ft/1151032001/FT_1151032001.html (accessed on 21 July 2022).
- Voumard, R.; van Neyghem, N.; Cochet, C.; Gardiol, C.; Decosterd, L.; Buclin, T.; de Valliere, S. Antibiotic Stability Related to Temperature Variations in Elastomeric Pumps Used for Outpatient Parenteral Antimicrobial Therapy (OPAT). J. Antimicrob. Chemother. 2017, 72, 1462–1465. [Google Scholar] [CrossRef] [PubMed]
- March-López, P.; Freixa, I.A.; Gil, M.M.; Espinoza, G.A.; Polonio, L.O.; Paredes, E.C.; Sanchez, M.C.; Sangrador, C.; Pardo, J.; Nicolás, J.; et al. Applicability of Quality Indicators for Appropriate Antibiotic Use in Outpatient Parenteral Antimicrobial Therapy (OPAT): A Point Prevalence Survey. Front. Pharmacol. 2021, 12, 713882. [Google Scholar] [CrossRef]
- Inaraja, M.T.; Castro, I.; Martínez, M.J. Formas Farmacéuticas Estériles: Mezclas Intravenosas, Citostáticos, Nutrición Parenteral; Sociedad Española de Farmacia Hospitalaria: Madrid, Spain, 2002; pp. 487–506. [Google Scholar]
- Spanish Ministry of Health Social Services and Equality. Guía de Buenas Prácticas de Preparación de Medicamentos En Servicios de Farmacia Hospitalaria. Available online: https://www.sanidad.gob.es/profesionales/farmacia/documentacion.htm (accessed on 21 July 2022).
- Okeke, C.C.; Newton, D.W.; Kastango, E.S.; Allen, L.V., Jr. Basics of Compounding: United States Pharmacapeia General Chapter 797 Pharmaceutical Compounding-Sterile Preparations, Part 10: First Revision: The Main Changes, Events, and Rationale. Int. J. Pharm. Compd. 2008, 12, 530–536. [Google Scholar]
- Larmené-Beld, K.H.M.; Frijlink, H.W.; Taxis, K. A Systematic Review and Meta-Analysis of Microbial Contamination of Parenteral Medication Prepared in a Clinical versus Pharmacy Environment. Eur. J. Clin. Pharmacol. 2019, 75, 609–617. [Google Scholar] [CrossRef]
- Cousins, D.H.; Otero, M.J.; Schmitt, É. Time to Review How Injectable Medicines Are Prepared and Administered in European Hospitals. Farm. Hosp. 2021, 45, 204–209. [Google Scholar] [CrossRef]
- Martín de Rosales Cabrera, A.M.; López Cabezas, C.; Pernía López, M.S.; Dávila Pousa, C.; Vila Clérigues, M.N.; Alonso Herreros, J.M.; García Salom, P.; Lozano Blázquez, A. Recommendations for the Safety Preparation of Sterile Medicines in Medical Wards. Farm. Hosp. 2014, 38, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Herranz, A.; Pernia, S. Centralized Drug Compounding Units: An Essential Driver of Patient Safety. Farm. Hosp. 2021, 45, 163–164. [Google Scholar] [CrossRef] [PubMed]
- Mansour, O.; Heslin, J.; Townsend, J.L. Impact of the Implementation of a Nurse-Managed Outpatient Parenteral Antibiotic Therapy (OPAT) System in Baltimore: A Case Study Demonstrating Cost Savings and Reduction in Re-Admission Rates. J. Antimicrob. Chemother. 2018, 73, 3181–3188. [Google Scholar] [CrossRef]
- Pallejà Gutiérrez, E.; López Carranza, M.; Jiménez Vilches, P.L. Catéteres Venosos de Inserción Periférica (PICC): Un Avance En Las Terapias Intravenosas de Larga Permanencia. Nutr. Clin. Med. 2017, 11, 114–127. [Google Scholar]
- Meyer, B.M.; Berndt, D.; Biscossi, M.; Eld, M.; Gillette-Kent, G.; Malone, A.; Wuerz, L. Vascular Access Device Care and Management. J. Infus. Nurs. 2020, 43, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Keller, S.C.; Cosgrove, S.E.; Kohut, M.; Krosche, A.; Chang, H.-E.; Williams, D.; Gurses, A.P. Hazards from Physical Attributes of the Home Environment among Patients on Outpatient Parenteral Antimicrobial Therapy. Am. J. Infect. Control. 2019, 47, 425–430. [Google Scholar] [CrossRef] [PubMed]
- Ferry, T.; Lodise, T.P.; Gallagher, J.C.; Forestier, E.; Goutelle, S.; Tam, V.H.; Mohr, J.F.; Roubaud-Baudron, C. Outpatient Subcutaneous Antimicrobial Therapy (OSCAT) as a Measure to Improve the Quality and Efficiency of Healthcare Delivery for Patients With Serious Bacterial Infections. Front. Med. 2020, 7, 585658. [Google Scholar] [CrossRef]
- Oteo Ochoa, L.A.; Repullo Labrador, J.R. La Innovación En Los Servicios Sanitarios; Consideraciones Desde La Perspectiva Del Sistema Nacional de Salud Español. Rev. Adm. Sanit. 2003, 1, 307–332. [Google Scholar]
- Myers, C.E. History of Sterile Compounding in U.S. Hospitals: Learning from the Tragic Lessons of the Past. Am. J. Health Syst. Pharm. 2013, 70, 1414–1427. [Google Scholar] [CrossRef]
- Chaker, A.; Omair, I.; Mohamed, W.H.; Mahomed, S.H.; Siddiqui, M.A. Workforce Planning and Safe Workload in Sterile Compounding Hospital Pharmacy Services. Am. J. Health Syst. Pharm. 2022, 79, 187–192. [Google Scholar] [CrossRef]
- Rivera, C.; Mara, K.; Mahoney, M.; Ryan, K. Survey of pharmacists on their roles and perceptions of outpatient parenteral antimicrobial therapy in the United States. Antimicrob. Steward. Healthc. Epidemiol. 2022, 2, E69. [Google Scholar] [CrossRef]
- Fisher, D.; Michaels, J.; Hase, R.; Zhang, J.; Kataria, S.; Sim, B.; Tsang, J.K.; Pollard, J.; Chan, M.; Swaminathan, S. Outpatient parenteral antibiotic therapy (OPAT) in Asia: Missing an opportunity. J. Antimicrob. Chemother. 2017, 72, 1221–1226. [Google Scholar] [CrossRef] [PubMed]
- Catalan Department of Health. Model Organitzatiu D’hospitalització a Domicili de Catalunya. Alternativa a L’hospitalització Convencional. Available online: https://catsalut.gencat.cat/ca/detalls/articles/model-organitzatiu-hospitalitzacio-domicili (accessed on 21 July 2022).
- Gilchrist, M.; Seaton, R.A. Outpatient Parenteral Antimicrobial Therapy and Antimicrobial Stewardship: Challenges and Checklists. J. Antimicrob. Chemother. 2015, 70, 965–970. [Google Scholar] [CrossRef] [PubMed]
| Spanish Society of Hospital at Home OPAT Decalogue |
|---|
|
| General Criteria for Patient Admission in an HaH Unit |
|
| Specific Admission Criteria for OPAT Programs |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortonobes, S.; Mujal-Martínez, A.; de Castro Julve, M.; González-Sánchez, A.; Jiménez-Pérez, R.; Hernández-Ávila, M.; De Alfonso, N.; Maye-Pérez, I.; Valle-Delmás, T.; Rodríguez-Sánchez, A.; et al. Successful Integration of Clinical Pharmacists in an OPAT Program: A Real-Life Multidisciplinary Circuit. Antibiotics 2022, 11, 1124. https://doi.org/10.3390/antibiotics11081124
Ortonobes S, Mujal-Martínez A, de Castro Julve M, González-Sánchez A, Jiménez-Pérez R, Hernández-Ávila M, De Alfonso N, Maye-Pérez I, Valle-Delmás T, Rodríguez-Sánchez A, et al. Successful Integration of Clinical Pharmacists in an OPAT Program: A Real-Life Multidisciplinary Circuit. Antibiotics. 2022; 11(8):1124. https://doi.org/10.3390/antibiotics11081124
Chicago/Turabian StyleOrtonobes, Sara, Abel Mujal-Martínez, María de Castro Julve, Alba González-Sánchez, Rafael Jiménez-Pérez, Manuel Hernández-Ávila, Natalia De Alfonso, Ingrid Maye-Pérez, Teresa Valle-Delmás, Alba Rodríguez-Sánchez, and et al. 2022. "Successful Integration of Clinical Pharmacists in an OPAT Program: A Real-Life Multidisciplinary Circuit" Antibiotics 11, no. 8: 1124. https://doi.org/10.3390/antibiotics11081124
APA StyleOrtonobes, S., Mujal-Martínez, A., de Castro Julve, M., González-Sánchez, A., Jiménez-Pérez, R., Hernández-Ávila, M., De Alfonso, N., Maye-Pérez, I., Valle-Delmás, T., Rodríguez-Sánchez, A., Pino-García, J., & Gómez-Valent, M. (2022). Successful Integration of Clinical Pharmacists in an OPAT Program: A Real-Life Multidisciplinary Circuit. Antibiotics, 11(8), 1124. https://doi.org/10.3390/antibiotics11081124





