Abstract
Background: Infection by SARS-CoV-2 has unquestionably had an impact on the health of patients with chronic respiratory airway diseases, such as COPD and asthma, but little information is available about its impact on patients with bronchiectasis. The objective of the present study was to analyze the effect of the SARS-CoV-2 pandemic on the state of health, characteristics, and clinical severity (including the number and severity of exacerbations) of patients with non-cystic fibrosis bronchiectasis. Methods: This study was multicenter, observational, and ambispective (with data collected before and during the SARS-CoV-2 pandemic), and included 150 patients diagnosed with non-cystic fibrosis bronchiectasis. Results: A significant drop was observed in the number and severity of the exacerbations (57% in all exacerbations and 50% in severe exacerbations) in the E-FACED and BSI multidimensional scores, in the pandemic, compared with the pre-pandemic period. There was also a drop in the percentage of sputum samples positive for pathogenic microorganisms in general (from 58% to 44.7%) and, more specifically, Pseudomonas aeruginosa (from 23.3% to 13.3%) and Haemophilus influenzae (from 21.3% to 14%). Conclusions: During the SARS-CoV-2 period, a significant reduction was observed in the exacerbations, severity, and isolations of pathogenic microorganisms in patients with bronchiectasis.
1. Introduction
Since the appearance of the first cases of pneumonia due to SARS-CoV-2 in December 2019, millions of people from all over the world have been infected, many of them with severe cases [1,2,3] and significant consequences [4,5] or death [6,7,8] as a result. On 30 January 2020, the World Health Organization (OMS) declared the disease now known as the novel coronavirus 2019 (COVID-19) a worldwide public health emergency [9]. Since then, some countries have experienced a varying number of waves of greater or lesser severity, depending on the protective measures adopted, the infectiousness, the characteristics of the individuals affected [10,11,12], and the aggressiveness of the various strains of the virus that have appeared, as well as the vaccination coverage achieved [13]. Various social and preventive protection measures were imposed according to the geographical region (mask wearing, social distancing, and even—in periods of high infection—lockdown) while the various vaccines currently on the market were still being developed. This situation led to changes in the healthcare of patients with chronic respiratory diseases [14,15,16,17,18,19,20], with delays in both diagnosis and therapy [21], as well as difficulties in accessing health centers, due not only to the restrictions imposed but also to the fear of being infected among the population [22].
Furthermore, the number of infectious exacerbations produced by respiratory viruses (found in more than 50% of cases) [23,24] also reduced in both healthy individuals and, above all, patients with chronic airway diseases, as reported in patients with chronic obstructive pulmonary disease (COPD) [25,26]. One obvious illustration of this trend was the virtual disappearance of the seasonal influenza virus [27] during the first waves of the pandemic, which has been primarily attributed to respiratory protection measures and social distancing.
In this context, it is necessary to analyze how the pandemic has influenced patients with bronchiectasis, considering that it represents the third most frequent chronic inflammatory disease of the airway (after asthma and COPD), with a high social and economic impact and an important implication upon the quality of life of these patients [28,29]. However, the data on the relationship between the pandemic caused by SARS-CoV-2 and the control of, and impact on, bronchiectasis (BE) patients are scarce. In this respect, only one single-center study comparing the pre-pandemic period and the pandemic itself [30], initially designed for the validation of a questionnaire on the quality of life in BE, has found a decrease of up to 50% in the number of exacerbations; the authors mainly attributed this reduction to favorable environmental factors (less environmental pollution and widespread respiratory protection) during the pandemic. Nevertheless, this development did not translate into changes in the symptoms or quality of life of patients in a stable phase. Since BE is acquiring ever greater epidemiological significance [31] and exacerbations are crucially linked to the severity, quality of life, prognosis, and even costs associated with this disease [28], the results obtained by Crichton et al. [30] are hugely important.
Our working hypothesis was that of a possible decrease in the number and severity of exacerbations, as well as a variable impact on other circumstances affecting these patients. Our objective was thus to analyze the impact of infection by SARS-CoV-2 during the pandemic, compared with the pre-pandemic period, on the number and severity of exacerbations and on other variables of interest, such as clinical, microbiological, therapeutic, lung-function, and analytical aspects.
2. Materials and Methods
2.1. Study Design
The study was observational, ambispective, and multicenter, with the participation of three public tertiary Spanish centers (not-for-profit and with free access) with a specialized BE unit, including patients of varying severity, meeting the referral criteria described by the Spanish Society of Pneumology and Thoracic Surgery (SEPAR) [32]. All the included patients were informed about the characteristics of the study and gave their informed consent. The project was approved by the Ethics Committee of the Hospital La Princesa (registry no. 3992). The study’s methodology follows the recommendations established for observational studies: STROBE (http://www.strobe-statement.org/).
2.2. Criteria for Inclusion and Exclusion
The criteria for inclusion were: a diagnosis of non-cystic fibrosis bronchiectasis (NCFBE) demonstrated by a high resolution computerized tomography (HRCT) chest scan, following the criteria of Naidich [33], with a compatible clinical picture [34]; adult status (18 years or more); and follow-up by the BE unit of one of the participating centers. The criteria for exclusion were: a change of residence to another Spanish Autonomous Community (resulting in a loss of follow-up) or refusal to participate in the study.
Initially, 173 consecutive patients diagnosed with BE were included, although 23 were later excluded (Figure 1). Finally, 150 patients completed the study (50 from each of the three participating centers).
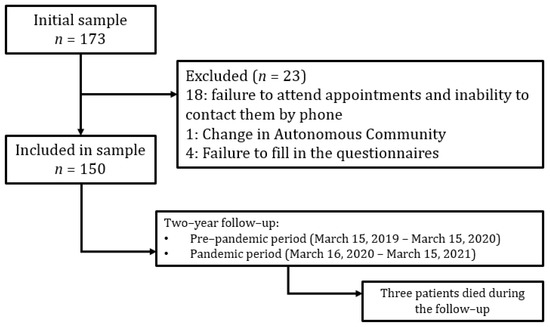
Figure 1.
Flowchart of the study.
2.3. Follow-Up
Considering 14 March 2020 (declaration of the state of emergency) as day 0 of the SARS-CoV-2 pandemic in Spain [35], two follow-up periods were established: one prior to the pandemic (15 March 2019–15 March 2020) and the other during the pandemic period (16 March 2020–15 March 2021). All the included patients underwent a complete follow-up in both phases of the study (pre-pandemic and pandemic) via appointments every 3–6 months, according to a clinician’s criteria, based on the severity presented by the patient.
Due to the restrictions imposed by the pandemic, some of the appointments during the pandemic period were conducted by telephone. Accordingly, all the patients had a telephone contact number for fulfilling the designated medical consultations and for providing information about exacerbation episodes, in case they could not attend in person.
2.4. Analyzed Variables
2.4.1. Baseline Variables
The following baseline variables were analyzed: age, gender, body mass index (BMI), smoking habit, age at diagnosis of BE, etiology, number of lobes affected in the HRCT, uni- or bilateral distribution, and morphology (cylindrical or cystic), as well as the Charlson [36] and BACI (Bronchiectasis Aetiology Comorbidity Index) indexes [37].
2.4.2. Variables Compared between the Pre-Pandemic and Pandemic Periods
The following variables were recorded at the first appointment in the pre-pandemic period and the last in the pandemic, for the purposes of comparison: the quantity and type of expectoration, according to Murray’s classification [38]; the degree of dyspnea on the mMRC (modified Medical Research Council) scale [39]; lung function studies (FVC and FEV1); changes in usual treatment; analytical data: leukocytes, neutrophils, eosinophils, erythrocyte sedimentation rate (ESR), fibrinogen, albumin, C-reactive protein (CRP); the FACED [40] and e-FACED [23] scores; the BSI (Bronchiectasis Severity Index) score [41]; and the HADS (Hospital Anxiety and Depression Scale) [42] and CAT (COPD Assessment Test) questionnaires [43]. Cut-offs of 11 or less points in the HADS-A or HADS-D questionnaires [44] and more than 10 in the CAT symptoms questionnaire were considered pathological.
The following data were recorded at all the appointments undertaken in both periods: the number and severity of the exacerbations, the number of oral and intravenous antibiotic courses, the total number of days of antibiotic therapy, and infection (or not) by the SARS-CoV-2 virus.
An exacerbation [45] was defined as a situation in which a patient presented a worsening of three or more of the following symptoms in the previous 48 h: cough, volume and/or consistency of sputum, purulence of sputum, dyspnea and/or intolerance of exercise, asthenia and/or general malaise, and hemoptysis, as well as a need for a change in treatment and the exclusion of other causes of clinical deterioration.
An exacerbation was considered mild–moderate when it required the prescription of treatment by the oral route and severe when it required intravenous antibiotic therapy and/or hospitalization.
Moreover, the following microbiological data were recorded at each appointment: the percentage of valid sputum samples (>25 polymorphonuclear and <10 epithelial cells) [46], the percentage of sputum samples positive for a potentially pathogenic microorganism (PPM) [47], and the percentage of sputum samples positive for Pseudomonas aeruginosa (PA), Haemophilus influenzae (HI), and Staphylococcus aureus (SA). Culture results were expressed as CFU per milliliter and ≥103 CFU were considered positive for a given PPM.
In the case of death, this was confirmed by the corresponding official death certificate.
2.5. Statistical Analysis
The results were presented as the mean ± standard deviation, median and interquartile range (IQR), or absolute number and percentage, depending on whether the variables were quantitative or qualitative and whether or not they followed a normal distribution, as verified by the Kolmogorov–Smirnov test.
Both parametrical (Student’s t-test for repeated measurements) and non-parametrical (Wilcoxon) tests were used to compare the quantitative variables recorded during the pre-pandemic and pandemic periods. In the case of qualitative variables, proportions were compared by means of the chi-square test, as well as Fisher’s exact test, where necessary. The statistical package IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY was used.
In the absence of any supporting data in the literature at the start of the study, we established: the main variable as a reduction by at least one exacerbation per patient per year between the pre-pandemic and pandemic period; an approximation of loss of patients of 10%; an alpha error of 0.05%; and a statistical power of 20% for repeated measurements, making the number of patients needed to perform the analyses 150. In order to achieve the greatest representation possible for all three centers taking part in the study, each was required to include 50 valid, consecutive patients for analysis before the study could be considered complete. We used PASS 2022, the Power analysis and sample size program (NCSS Statistical Software, Kaysville, UT, USA) as a sample size software.
3. Results
3.1. Baseline Characteristics of the Patients
As can be seen in Table 1, of the 150 patients who were finally included, 115 (76.7%) were women with a mean age of 61.3 ± 16.1 years. The Charlson Index was 2.9 ± 1.9 and the most frequent etiology was post-infection (49.3%). The mean FACED and BSI scores were 1.6 ± 1.4 and 5.4 ± 3.6, respectively. The percentage of FEV1 was 75.6% ± 25 and the median of exacerbations was 1 (IQR: 1–2).

Table 1.
Baseline characteristics of the patients.
3.2. Comparison between the Pre-Pandemic and Pandemic Periods
The mean number of days of follow-up in the pre-pandemic period was 357 ± 35 days, whilst it was 361 ± 37 days in the pandemic, with no significant differences between the two (p = 0.99). Three patients died during the follow-up. Twelve patients (8.7%) presented infection by SARS-CoV-2 but none of them required hospitalization. The median of in-person appointments was 3 (IQR: 2–4) and 2 (IQR: 1–2), p = 0.001, and that of telephone appointments was 0 (IQR: 0–1) and 2 (IQR: 2–3), p < 0.001, in the pre-pandemic and pandemic periods, respectively.
3.2.1. Exacerbations
In the pre-pandemic period, the median of the total number of exacerbations was 1 (IQR: 1–2) and the mean was 1.4 ± 1.2, while during the pandemic, the median was 0 (IQR: 0–1) and the mean was 0.6 ± 0.8, which corresponded to p < 0.0001 and p < 0.001, respectively (Figure 2). This represented a 57% drop in the total number of exacerbations.
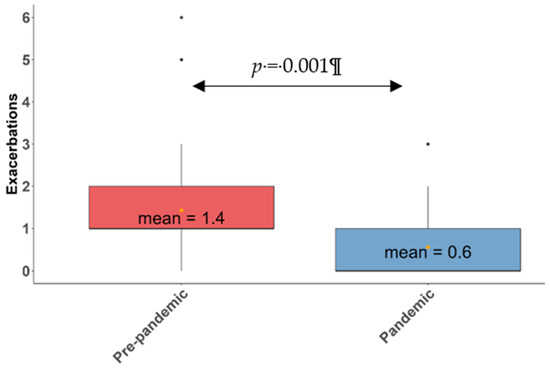
Figure 2.
Box plot. Mean and median of exacerbations in the pre-pandemic and pandemic periods. The thick black line represents the median, and the yellow dot represents the mean.
The proportion of patients without any exacerbations thus rose from 22.6% in the pre-pandemic period to 63.1% in the pandemic (p < 0.001) (Figure 3). Furthermore, the percentage of patients with one exacerbation fell from 37.3% to 22.1% (p = 0.012), while that of patients with two exacerbations fell from 23.3% to 10.7% (p = 0.031), that of patients with three fell from 12.6% to 4% (p = 0.039), and that of those with more than three went from 4% to 0% (p = 0.042).
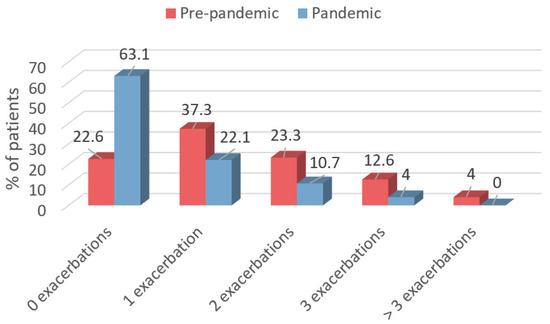
Figure 3.
Percentage of patients who experienced 0, 1, 2, 3, or >3 exacerbations in the pre-pandemic and pandemic periods.
Figure 3 shows the percentage of patients who experienced 0, 1, 2, 3, or >3 exacerbations in the pre-pandemic period (red) and the pandemic period (blue).
Furthermore, as can be seen in Table 2, the median of the number of courses of oral antibiotic therapy in the pre-pandemic period went from 1 (IQR: 1–2) to 0 (IQR: 0–1) in the pandemic (p < 0.0001), while the median of the days of oral antibiotic therapy dropped from 14 (IQR: 6–23,25) to 0 (IQR: 0–14) (p < 0.0001) and the mean fell from 16.9 ± 16 to 7.3 ± 12.5 (p < 0.001). Similarly, the percentage of patients who experienced at least one severe exacerbation fell from 13.5% to 6.8% (p = 0.013), representing a 50% reduction. Moreover, the mean of the days of intravenous antibiotic therapy decreased from 1.96 ± 5.44 to 0.83 ± 3.64 (p = 0.009).

Table 2.
Antibiotic courses and accumulated days of oral and intravenous antibiotic therapy.
3.2.2. Microbiological Aspects
The median of the sputum samples collected before the pandemic was 2 (IQR: 1–3), while during the pandemic it was 1 (IQR: 0–3); p < 0.01. Of these, the means of sputum samples positive for PPM were, respectively, 1 (0–3) and 1 (0–2); p = 0.02. The percentage of patients from whom it was possible to collect valid sputum samples was greater in the pre-pandemic period, with a mean (range) of 2.5 (0–9), as opposed to 1.2 (0–6) during the pandemic; p = 0.012. As can be seen in Table 3, during the pandemic there was a 13.3% reduction, in those patients capable of expectorating, in the percentage of positive sputum samples for any PPM other than SA, including HI (7.3%) and PA (10%).

Table 3.
Percentage of positive sputum samples for potentially pathogenic microorganisms during the pre-pandemic and pandemic periods.
3.2.3. Severity Scores
The mean score of the E-FACED scale fell from 1.8 ± 1.5 to 1.43 ± 1.43 (p = 0.030) (Figure 4) and that of the BSI fell from 5.4 ± 3.6 to 4.4 ± 3.3 (p = 0.047) (Figure 5). There was also a drop in the FACED score, but this was not statistically significant (Table 4).
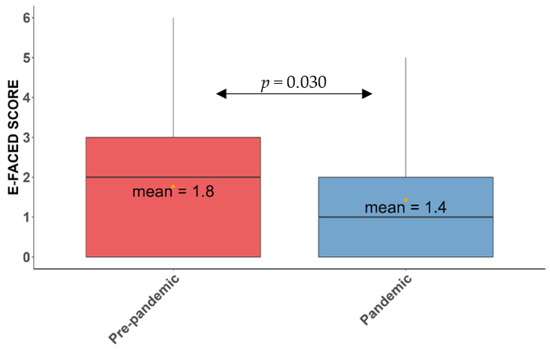
Figure 4.
Mean score of the E-FACED scale in the pre-pandemic and pandemic periods. The yellow dots represent the mean of the E-FACED in the pre-pandemic (red) and pandemic (blue) periods.
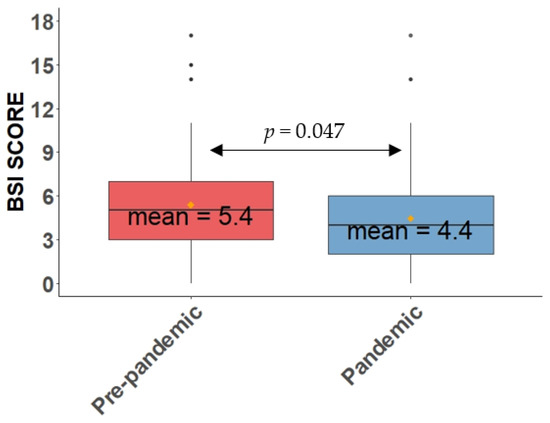
Figure 5.
Mean score of the BSI scale in the pre-pandemic and pandemic periods. The yellow dots represent the mean of the BSI in the pre-pandemic (red) and pandemic (blue) periods.

Table 4.
Comparison of the FACED, E-FACED, and BSI scales and the CAT and HADS questionnaires during the pre-pandemic and pandemic periods.
3.2.4. Quality of Life and Psychomorbidity
Table 4 shows that there were no differences in the CAT scores, although the percentage of patients with clear symptoms of anxiety or depression (cut-off point > 11 in the HADS questionnaire) decreased during the pandemic compared with the pre-pandemic period.
3.2.5. Clinical, Functional, Analytical, and Therapeutic Aspects
As regards the clinical manifestations, a comparison between the two periods did not reveal any statistically significant differences in the degree of dyspnea, according to the mMRC scale, or the presence of expectoration, or any differences in lung function, analytical parameters, or the usual treatment (Table 5).

Table 5.
Comparison of the symptoms, lung function, analytical parameters, and usual treatment in the pre-pandemic and pandemic periods.
4. Discussion
According to our results, there was a reduction in the general severity of BE during the pandemic (compared with the pre-pandemic period), due to a very significant drop in both the number and severity of exacerbations and in their treatments, along with a decrease in the isolations of PPM, including PA and HI. No changes were observed in clinical, analytical, functional, or therapeutic aspects, or in the quality of life, despite a decrease in the percentage of patients with symptoms of anxiety and depression.
Regarding the decrease in the number and severity of exacerbations, our results are very similar to those obtained in other studies of patients with BE or COPD. In this respect, Crichton ML et al. [30] observed a reduction in the mean of exacerbations from 2.01 in the period 2019–2020 to 1.12 in 2020–2021, with an increase in the percentage of patients free from exacerbations from 25.6% to 52.3%; there was also a decrease in the corresponding courses of systemic antibiotic therapy. Similarly, a meta-analysis by Alqahtani et al. [25] found a 50% reduction in hospitalizations due to exacerbations of COPD during the pandemic. These results can probably be explained by measures adopted during the pandemic period investigated in study (16 March 2020–15 March 2021) in Spain, such as the mandatory use of a mask and hand disinfection, lockdown (15 March 2020–12 June 2020), curfew, shop closures, social distancing and restriction of massive events, leading to a decrease in viral infections, which cause a considerable percentage of exacerbations in BE patients. [48]. These results are hugely significant in terms of both epidemiology and clinical application, since it has already been proven that both the number and the severity of exacerbations have a negative impact on the natural history of BE patients [48,49,50,51]. Moreover, the data provided could have implications in the management of these patients, and by extension to patients with other chronic respiratory diseases, in favor of the recommendation to use mask in crowded places, visits to hospitals, or other healthcare centers, and promotion of teleconsultation and domiciliary treatments, with the purpose to avoid overexposure to respiratory germs.
From the microbiological viewpoint, although the quantity of patients presenting a valid sputum sample was significantly lower in the pandemic period, there was also a very noteworthy drop in the percentage of sputum samples positive for PPM, particularly HI and PA—a finding closely related to severity and exacerbations in BE [28,29,49,50,52,53,54,55]—even though no differences were observed in the baseline treatments between the two time periods. Once again, respiratory protection and social distancing that impede the transmission of viruses, along with fewer exacerbations, prevented a subsequent growth of pathogenic bacteria (bacterial superinfection), thereby increasing the time free from exacerbation and probably helping the immune system to achieve control over chronic bacterial infection or eradicate PPM from the bronchial mucosa [56]. Another explanation may be that the “threshold” quantity of bacteria allowing detection in culture is exceed more often in the pre-pandemic era due to more frequent exacerbations, however we were not able to analyze this hypothesis since we have not information about quantitative cultures in samples from an exacerbation phase and stable condition.
Another noteworthy aspect is the lack of improvement in the quality of life and the parameters of anxiety and depression (factors that are normally closely linked) that would be expected to accompany a decrease in the severity of BE [44]. Any slight impact on the quality of life and psychomorbidity could be limited, however, by the negative impact of the lack of improvement in baseline symptoms, in a context of fear of contagion, reduced social contacts, and increased loneliness in the pandemic, particularly during lockdown. Nevertheless, not surprisingly, the severity scores for BE that include exacerbations and the microbiological pattern, such as BSI and E-FACED, significantly improved, while FACED does not have a sufficient discriminatory capacity as it does not include the number and severity of exacerbations.
Among the strengths of this study, it should be noted that it is the first to be designed to evaluate the effect of the pandemic on BE patients on a multidimensional basis (measuring both objective and subjective parameters), as well as being multicentered, with participation from hospitals from the center, east, and south of Spain. Among the limitations of this study, it is important to point out some of them: firstly, the follow-up of the patients was necessarily conducted in a different way as a consequence of the pandemic, with a significant reduction in the number of in-person appointments and collections of sputum samples during that period. Accordingly, the analyses were carried out with data related to the percentage of total sputum samples collected (in both exacerbation stable phase) and samples positive for PPM in both periods, rather than with absolute data; secondly, we have no data on quantitative cultures; thirdly, all three centers included had specialized BE clinics so we cannot rule out a severity bias towards more severe cases, and finally, we cannot rule out an underestimate of exacerbations, especially in their milder forms, in the times of less direct contact with the patients, although a continuous, on-demand telephone service was established in every case to minimize this circumstance.
5. Conclusions
In conclusion, the number and severity of exacerbations and the degree of infection by PPM dropped significantly in BE patients during the SAR-CoV-2 pandemic compared with the period prior to the pandemic. Although no causal relationship could be established, it is highly probable that these results are linked to the increase in respiratory protection measures and social distancing that would impede contagion, especially from viruses. Controlled, prospective studies are needed to confirm whether the implementation of such measures is—as the present study suggests—effective in preventing exacerbations in BE patients.
Author Contributions
Conceptualization, R.M.G.M., M.Á.M.-G., C.O. and A.M.-V.; methodology, R.M.G.M., M.Á.M.-G., C.O., A.M.-V. and G.O.; validation, R.M.G.M., M.Á.M.-G. and C.O.; formal analysis, R.M.G.M., M.Á.M.-G., A.M.-V.,and A.P.; investigation, R.M.G.M., M.Á.M.-G., A.M.-V., M.V.G., G.O. and A.P.; resources, R.M.G.M., M.Á.M.-G., A.M.-V., M.V.G., G.O. and J.A.; data curation, R.M.G.M., M.Á.M.-G., A.M.-V., M.V.G., G.O., J.A. and A.P.; writing—original draft preparation, A.M.-V., R.M.G.M., M.Á.M.-G. and C.O.; writing—review and editing, A.M.-V., R.M.G.M., M.Á.M.-G. and C.O.; visualization, A.M.-V., R.M.G.M., M.Á.M.-G. and C.O.; supervision, R.M.G.M., M.Á.M.-G. and C.O.; project administration, R.M.G.M., M.Á.M.-G. and C.O.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The project was approved by the Ethics Committee of the Hospital La Princesa (registry no. 3992).
Informed Consent Statement
All the included patients were informed about the characteristics of the study and gave their informed consent.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Torres, A.; Arguimbau, M.; Bermejo-Martín, J.; Campo, R.; Ceccato, A.; Fernandez-Barat, L.; Ferrer, R.; Jarillo, N.; Lorente-Balanza, J.; Menéndez, R.; et al. CIBERESUCICOVID: A strategic project for a better understanding and clinical management of COVID-19 in critical patients. Arch Bronconeumol. 2021, 57, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Golpe, R.; Blanco, N.; Castro-Añón, O.; Corredoira, J.; García-Pais, M.J.; Pérez-de-Llano, L.A.; Rabuñal, R.; Romay, E.; Suárez, R. Factors Associated to Hospital Admission in a Care Protocol in COVID-19. Arch Bronconeumol. 2020, 56, 676–677. [Google Scholar] [CrossRef] [PubMed]
- López-Reyes, R.; Oscullo, G.; Jiménez, D.; Cano, I.; García-Ortega, A. Thrombotic Risk and Covid-19: Review of Current Evidence for a Better Diagnostic and Therapeutic Approach. Arch. Bronconeumol. 2021, 57, 55–64. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Haupert, S.R.; Zimmermann, L.; Shi, X.; Fritsche, L.G.; Mukherjee, B. Global Prevalence of Post COVID-19 Condition or Long COVID: A Meta-Analysis and Systematic Review. J. Infect. Dis. 2022. online ahead of print. [Google Scholar] [CrossRef]
- Tabernero Huguet, E.; Urrutia Gajarte, A.; Ruiz Iturriaga, L.A.; Serrano Fernandez, L.; Marina Malanda, N.; Iriberri Pascual, M.; Zalacain Jorge, R. Pulmonary Function in Early Follow-up of patients with COVID-19 Pneumonia. Arch. Bronconeumol. 2021, 57, 75–76. [Google Scholar] [CrossRef]
- Posso, M.; Comas, M.; Román, M.; Domingo, L.; Louro, J.; González, C.; Sala, M.; Anglès, A.; Cirera, I.; Cots, F.; et al. Comorbidities and Mortality in Patients With COVID-19 Aged 60 Years and Older in a University Hospital in Spain. Arch. Bronconeumol. 2020, 56, 756–758. [Google Scholar] [CrossRef]
- Dessie, Z.G.; Zewotir, T. Mortality-related risk factors of COVID-19: A systematic review and meta-analysis of 42 studies and 423,117 patients. BMC Infect. Dis. 2021, 21, 855. [Google Scholar] [CrossRef]
- Candal-Pedreira, C.; Fernández-Villar, A.; López-Campos, J.L.; Ruano-Ravina, A. Prognostic Scales of COVID-19 Morbidity and Mortality: Necessary but also Reliable. Arch. Bronconeumol. 2021, 57, 62–63. [Google Scholar] [CrossRef]
- Ahn, D.G.; Shin, H.J.; Kim, M.H.; Lee, S.; Kim, H.S.; Myoung, J.; Kim, B.T.; Kim, S.J. Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19). J. Microbiol. Biotechnol. 2020, 30, 313–324. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Systematic review of COVID-19 in children shows milder cases and a better prognosis than adults. Acta Paediatr 2020, 109, 1088–1095. [Google Scholar] [CrossRef]
- Ríos-Barnés, M.; Lanaspa, M.; Noguera-Julian, A.; Baleta, L.; De Sevilla, M.F.; Ferri, D.; Götzens, J.; Jordan, I.; Lecina, L.; Monfort, L.; et al. The Spectrum of COVID-19 Disease in Adolescents. Arch. Bronconeumol. 2021, 57, 84–85. [Google Scholar] [CrossRef] [PubMed]
- Chavasse, R.; Almario, A.; Christopher, A.; Kappos, A.; Shankar, A. The Indirect Impact of COVID-19 on Children With Asthma. Arch. Bronconeumol. 2020, 56, 768–769. [Google Scholar] [CrossRef]
- Aleem, A.; Akbar Samad, A.B.; Slenker, A.K. Emerging Variants of SARS-CoV-2 And Novel Therapeutics Against Coronavirus (COVID-19). In StatPearls [Internet]; StatPearls: Treasure Island, FL, USA, 12 May 2022. [Google Scholar]
- Gülsen, A.; König, I.R.; Jappe, U.; Drömann, D. Effect of comorbid pulmonary disease on the severity of COVID-19: A systematic review and meta-analysis. Respirology 2021, 26, 552–565. [Google Scholar] [CrossRef] [PubMed]
- Burgos Rincón, F.; Martínez Llorens, J.; Cordovilla Pérez, R. Impact of the COVID-19 Pandemic on Lung Function Laboratories: Considerations for “Today” and the “Day After”. Arch. Bronconeumol. 2020, 56, 611–612. [Google Scholar] [CrossRef] [PubMed]
- Alkhathami, M.G.; Advani, S.M.; Abalkhail, A.A.; Alkhathami, F.M.; Alshehri, M.K.; Albeashy, E.E.; Alsalamah, J.A. Prevalence and mortality of lung comorbidities among patients with COVID-19: A systematic review and meta-analysis. Lung India 2021, 38, S31–S40. [Google Scholar] [CrossRef] [PubMed]
- Izquierdo Alonso, J.L.; Rodríguez González-Moro, J.M. Pneumology in the Days of COVID-19. Arch. Bronconeumol. 2020, 56, 1–2. [Google Scholar] [CrossRef]
- Tiotiu, A. Impact of COVID-19 on the Most Frequent Middle and Lower Obstructive Airway Diseases/Syndromes in Adult Population. Arch. Bronconeumol. 2021, 57, 7–8. [Google Scholar] [CrossRef]
- Guan, W.J.; Liang, W.H.; Zhao, Y.; Liang, H.R.; Chen, Z.S.; Li, Y.M.; Liu, X.Q.; Chen, R.C.; Tang, C.L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: A nationwide analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef]
- Alcázar-Navarrete, B.; Molina París, J.; Martín Sánchez, F.J. Management and Follow up of Respiratory Patients in the Post-COVID-19 Era: Are We Ready Yet? Arch. Bronconeumol. 2020, 56, 685–686. [Google Scholar] [CrossRef]
- Isea de la Viña, J.; Mayol, J.; Ortega, A.L.; Alcázar Navarrete, B. Lung Cancer Patients on the Waiting List in the Midst of the COVID-19 Crisis: What Do We Do Now? Arch. Bronconeumol. 2020, 56, 602–604. [Google Scholar] [CrossRef]
- Halpin, D.M.G.; Vogelmeier, C.F.; Agusti, A.A. COPD & COVID-19. Arch. Bronconeumol. 2021, 57, 162–164. [Google Scholar] [CrossRef] [PubMed]
- de la Rosa Carrillo, D.; Athanazio, R.; Girón Moreno, R.M.; Máiz Carro, L.; Olveira, C.; de Gracia, J.; Vendrell, M.; Prados Sánchez, C.; Gramblicka, G.; Corso Pereira, M.; et al. The annual prognostic ability of FACED and E-FACED scores to predict mortality in patients with bronchiectasis. ERJ Open Res. 2018, 4, 00139-2017. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.H.; Guan, W.J.; Xu, G.; Lin, Z.Y.; Tang, Y.; Lin, Z.M.; Gao, Y.; Li, H.M.; Zhong, N.S.; Zhang, G.J.; et al. The role of viral infection in pulmonary exacerbations of bronchiectasis in adults: A prospective study. Chest 2015, 147, 1635–1643. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, J.S.; Oyelade, T.; Aldhahir, A.M.; Mendes, R.G.; Alghamdi, S.M.; Miravitlles, M.; Mandal, S.; Hurst, J.R. Reduction in hospitalised COPD exacerbations during COVID-19: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0255659. [Google Scholar] [CrossRef] [PubMed]
- Tan, J.Y.; Conceicao, E.P.; Wee, L.E.; Sim, X.Y.J.; Venkatachalam, I. COVID-19 public health measures: A reduction in hospital admissions for COPD exacerbations. Thorax 2021, 76, 512–513. [Google Scholar] [CrossRef] [PubMed]
- Koutsakos, M.; Wheatley, A.K.; Laurie, K.; Kent, S.J.; Rockman, S. Influenza lineage extinction during the COVID-19 pandemic? Nat. Rev. Microbiol. 2021, 19, 741–742. [Google Scholar] [CrossRef]
- de la Rosa, D.; Martínez-Garcia, M.A.; Olveira, C.; Girón, R.; Máiz, L.; Prados, C. Annual direct medical costs of bronchiectasis treatment: Impact of severity, exacerbations, chronic bronchial colonization and chronic obstructive pulmonary disease coexistence. Chron. Respir. Dis. 2016, 13, 361–371. [Google Scholar] [CrossRef]
- Hernández, C.; Abreu, J.; Jiménez, A.; Fernández, R.; Martín, C. Pulmonary function and quality of life in relation to bronchial colonization in adults with bronchiectasis not caused by cystic fibrosis. Med. Clin. 2002, 118, 130–134. [Google Scholar] [CrossRef]
- Crichton, M.L.; Shoemark, A.; Chalmers, J.D. The Impact of the COVID-19 Pandemic on Exacerbations and Symptoms in Bronchiectasis: A Prospective Study. Am. J. Respir. Crit Care Med. 2021, 204, 857–859. [Google Scholar] [CrossRef]
- Martinez-García, M.A.; Villa, C.; Dobarganes, Y.; Girón, R.; Maíz, L.; García-Clemente, M.; Sibila, O.; Golpe, R.; Rodríguez, J.; Barreiro, E.; et al. RIBRON: The spanish Online Bronchiectasis Registry. Characterization of the First 1912 Patients. Arch. Bronconeumol. 2021, 57, 28–35. [Google Scholar] [CrossRef]
- Martínez-García, M.; Máiz, L.; Olveira, C.; Girón, R.M.; de la Rosa, D.; Blanco, M.; Cantón, R.; Vendrell, M.; Polverino, E.; de Gracia, J.; et al. Spanish Guidelines on Treatment of Bronchiectasis in Adults. Arch. Bronconeumol. 2018, 54, 88–98. [Google Scholar] [CrossRef] [PubMed]
- Webb, W.R.; Müller, N.L.; Naidich, D.P.; Ovid Technologies, I. High-Resolution CT of the Lung, 3rd ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Aliberti, S.; Goeminne, P.C.; O’Donnell, A.E.; Aksamit, T.R.; Al-Jahdali, H.; Barker, A.F.; Blasi, F.; Boersma, W.G.; Crichton, M.L.; De Soyza, A.; et al. Criteria and definitions for the radiological and clinical diagnosis of bronchiectasis in adults for use in clinical trials: International consensus recommendations. Lancet Respir. Med. 2022, 10, 298–306. [Google Scholar] [CrossRef]
- Ministerio de la Presidencia Relaciones con las Cortes y Memoria Democrática. Gobierno de España. Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la crisis sanitaria ocasionada por el COVID-19. Boletín Oficial del Estado. 2020, 67, 25390–25400. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- McDonnell, M.J.; Aliberti, S.; Goeminne, P.C.; Restrepo, M.I.; Finch, S.; Pesci, A.; Dupont, L.J.; Fardon, T.C.; Wilson, R.; Loebinger, M.R.; et al. Comorbidities and the risk of mortality in patients with bronchiectasis: An international multicentre cohort study. Lancet Respir. Med. 2016, 4, 969–979. [Google Scholar] [CrossRef]
- Murray, M.P.; Pentland, J.L.; Turnbull, K.; MacQuarrie, S.; Hill, A.T. Sputum colour: A useful clinical tool in non-cystic fibrosis bronchiectasis. Eur Respir. J. 2009, 34, 361–364. [Google Scholar] [CrossRef]
- Bestall, J.C.; Paul, E.A.; Garrod, R.; Garnham, R.; Jones, P.W.; Wedzicha, J.A. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999, 54, 581–586. [Google Scholar] [CrossRef]
- Martínez-García, M.; de Gracia, J.; Vendrell Relat, M.; Girón, R.M.; Máiz Carro, L.; de la Rosa Carrillo, D.; Olveira, C. Multidimensional approach to non-cystic fibrosis bronchiectasis: The FACED score. Eur Respir. J. 2014, 43, 1357–1367. [Google Scholar] [CrossRef]
- McDonnell, M.J.; Aliberti, S.; Goeminne, P.C.; Dimakou, K.; Zucchetti, S.C.; Davidson, J.; Ward, C.; Laffey, J.G.; Finch, S.; Pesci, A.; et al. Multidimensional severity assessment in bronchiectasis: An analysis of seven European cohorts. Thorax 2016, 71, 1110–1118. [Google Scholar] [CrossRef]
- Olveira, C.; Olveira, G.; Espildora, F.; Girón, R.M.; Vendrell, M.; Dorado, A.; Martínez-García, M. Mediterranean diet is associated on symptoms of depression and anxiety in patients with bronchiectasis. Gen. Hosp. Psychiatry 2014, 36, 277–283. [Google Scholar] [CrossRef]
- De la Rosa Carrillo, D.; Olveira, C.; García-Clemente, M.; Girón-Moreno, R.M.; Nieto-Royo, R.; Navarro-Rolon, A.; Prados-Sánchez, C.; Sibila, O.; Martínez-García, M. COPD Assessment Test in Bronchiectasis: Minimum Clinically Important Difference and Psychometric Validation: A Prospective Study. Chest 2020, 157, 824–833. [Google Scholar] [CrossRef] [PubMed]
- Colomo, N.; Olveira, C.; Hernández-Pedrosa, J.; Bergero, T.; Fábrega-Ruz, J.; Porras, N.; Girón, M.V.; de Rota, L.F.; Olveira, G. Validity of Self-rating Screening Scales for the Diagnosis of Depression and Anxiety in Adult Patients With Bronchiectasis. Arch. Bronconeumol. 2021, 57, 179–185. [Google Scholar] [CrossRef]
- Hill, A.T.; Haworth, C.S.; Aliberti, S.; Barker, A.; Blasi, F.; Boersma, W.; Chalmers, J.D.; De Soyza, A.; Dimakou, K.; Elborn, J.S.; et al. Pulmonary exacerbation in adults with bronchiectasis: A consensus definition for clinical research. Eur Respir. J. 2017, 49, 1700051. [Google Scholar] [CrossRef] [PubMed]
- Gleckman, R.; DeVita, J.; Hibert, D.; Pelletier, C.; Martin, R. Sputum gram stain assessment in community-acquired bacteremic pneumonia. J. Clin. Microbiol. 1988, 26, 846–849. [Google Scholar] [CrossRef] [PubMed]
- de la Rosa Carrillo, D.; López-Campos, J.L.; Alcázar Navarrete, B.; Calle Rubio, M.; Cantón Moreno, R.; García-Rivero, J.L.; Máiz Carro, L.; Olveira Fuster, C.; Martínez-García, M.; Documento, C.A.d.; et al. Consensus Document on the Diagnosis and Treatment of Chronic Bronchial Infection in Chronic Obstructive Pulmonary Disease. Arch. Bronconeumol. 2020, 56, 651–664. [Google Scholar] [CrossRef]
- Chen, C.L.; Huang, Y.; Yuan, J.J.; Li, H.M.; Han, X.R.; Martinez-Garcia, M.A.; de la Rosa-Carrillo, D.; Chen, R.C.; Guan, W.J.; Zhong, N.S. The Roles of Bacteria and Viruses in Bronchiectasis Exacerbation: A Prospective Study. Arch. Bronconeumol. 2020, 56, 621–629. [Google Scholar] [CrossRef]
- Martinez-Garcia, M.; Athanazio, R.; Gramblicka, G.; Corso, M.; Cavalcanti Lundgren, F.; Fernandes de Figueiredo, M.; Arancibia, F.; Rached, S.; Girón, R.; Máiz Carro, L.; et al. Prognostic Value of Frequent Exacerbations in Bronchiectasis: The Relationship With Disease Severity. Arch. Bronconeumol. 2019, 55, 81–87. [Google Scholar] [CrossRef]
- Martinez-García, M.A. Infection and exacerbations in bronchiectasis: More questions than answers. Eur Respir. J. 2018, 51, 1702497. [Google Scholar] [CrossRef]
- Monsó, E. Look at the wood and not at the tree: The Microbiome in Chronic Obstructive Lung Disease and Cystic Fibrosis. Arch. Bronconeumol. 2020, 56, 5–6. [Google Scholar] [CrossRef]
- Wilson, R.; Aksamit, T.; Aliberti, S.; De Soyza, A.; Elborn, J.S.; Goeminne, P.; Hill, A.T.; Menendez, R.; Polverino, E. Challenges in managing Pseudomonas aeruginosa in non-cystic fibrosis bronchiectasis. Respir. Med. 2016, 117, 179–189. [Google Scholar] [CrossRef]
- Aliberti, S.; Lonni, S.; Dore, S.; McDonnell, M.J.; Goeminne, P.C.; Dimakou, K.; Fardon, T.C.; Rutherford, R.; Pesci, A.; Restrepo, M.I.; et al. Clinical phenotypes in adult patients with bronchiectasis. Eur Respir. J. 2016, 47, 1113–1122. [Google Scholar] [CrossRef] [PubMed]
- Finch, S.; McDonnell, M.J.; Abo-Leyah, H.; Aliberti, S.; Chalmers, J.D. A Comprehensive Analysis of the Impact of Pseudomonas aeruginosa Colonization on Prognosis in Adult Bronchiectasis. Ann. Am. Thorac Soc. 2015, 12, 1602–1611. [Google Scholar] [CrossRef] [PubMed]
- Martinez-García, M.A.; Oscullo, G.; Posadas, T.; Zaldivar, E.; Villa, C.; Dobarganes, Y.; Girón, R.; Olveira, C.; Maíz, L.; García-Clemente, M.; et al. Pseudomonas aeruginosa and lung function decline in patients with bronchiectasis. Clin. Microbiol. Infect. 2021, 27, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Klein, E.Y.; Monteforte, B.; Gupta, A.; Jiang, W.; May, L.; Hsieh, Y.H.; Dugas, A. The frequency of influenza and bacterial coinfection: A systematic review and meta-analysis. Influenza Other Respir. Viruses 2016, 10, 394–403. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).