Survey of the Knowledge, Attitudes and Practice towards Antibiotic Use among Prospective Antibiotic Prescribers in Serbia
Abstract
1. Introduction
2. Results
2.1. Sociodemographic and Academic Characteristics
2.2. Students’ Knowledge Regarding the Antibiotics Use
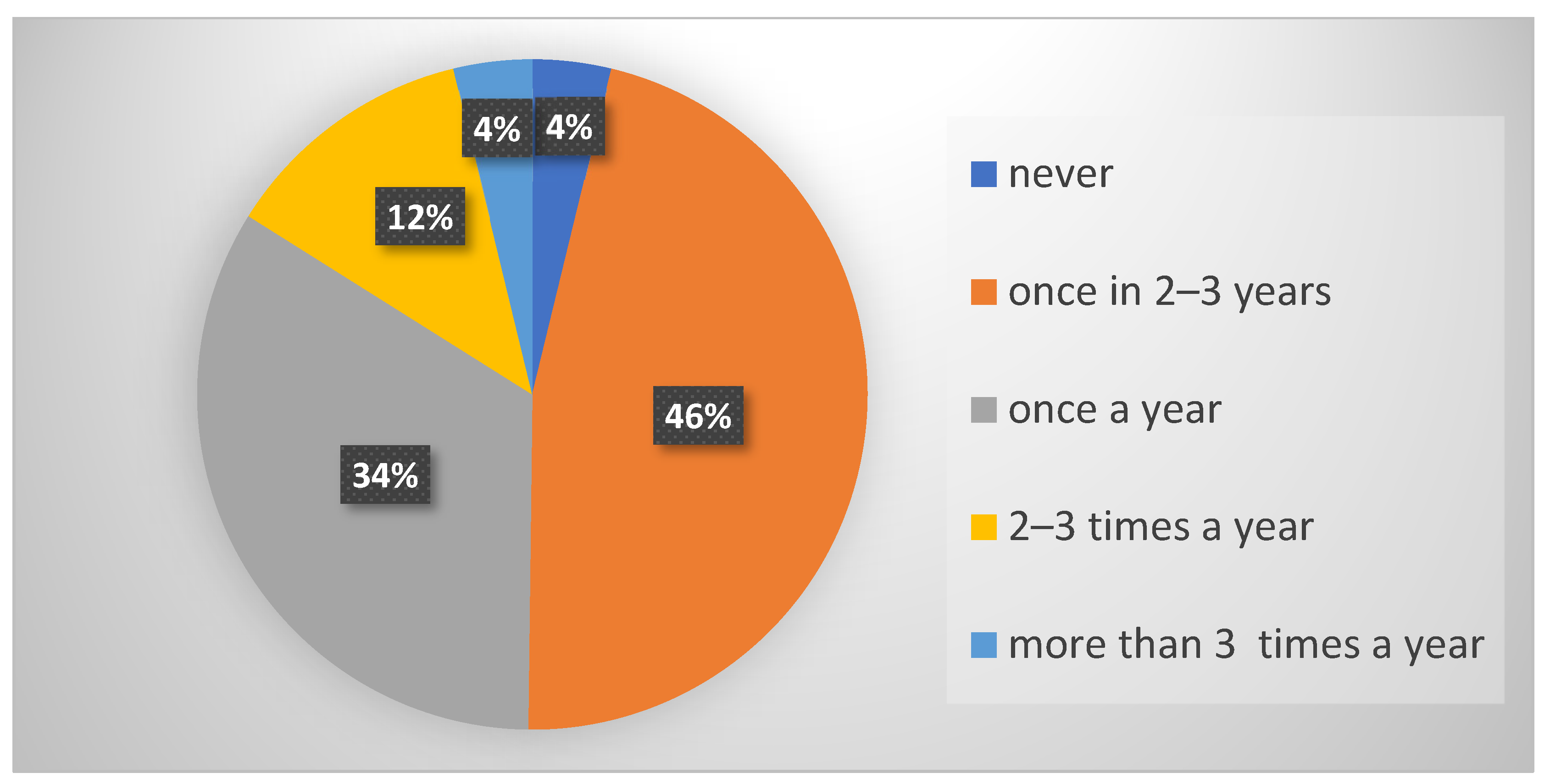
2.3. Practice and Attitudes of Respondents toward Antibiotics Use
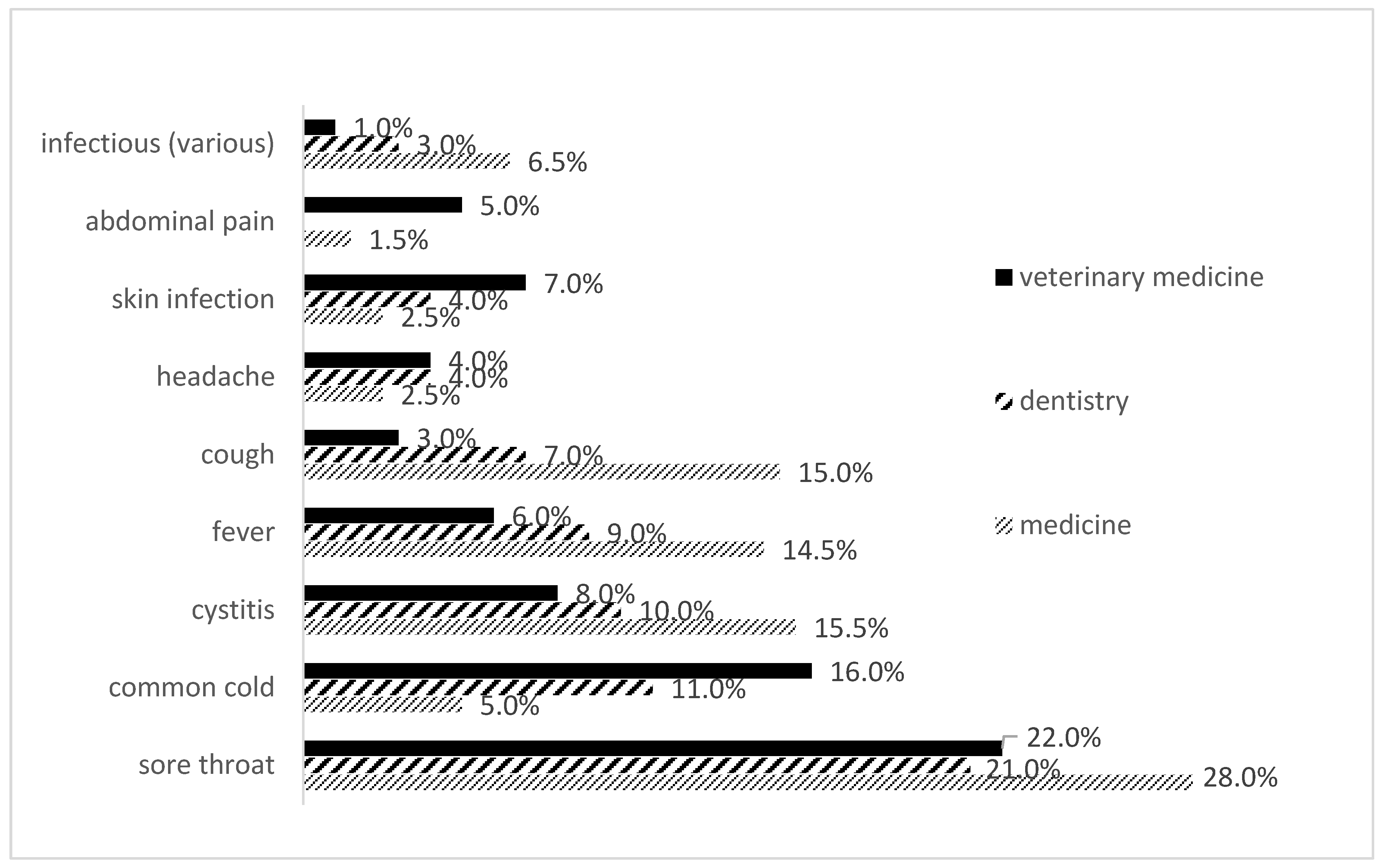
Reasons for Self-Medication with Antibiotics
3. Discussion
4. Materials and Methods
4.1. Study Design
4.2. Questionnaire Design
4.3. Data Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McEwen, S.A.; Collignon, P.J. Antimicrobial Resistance: A One Health Perspective. Microbiol. Spectr. 2018, 6, 2. [Google Scholar] [CrossRef]
- Lloyd, D.H.; Page, S.W.; Aarestrup, F.M.; Schwarz, S.; Shen, J.; Cavaco, L. Antimicrobial stewardship in veterinary medicine. Microbiol. Spectr. 2018, 6. [Google Scholar] [CrossRef]
- Graham, D.W.; Bergeron, G.; Bourassa, M.W.; Dickson, J.; Gomes, F.; Howe, A.; Kahn, L.H.; Morley, P.S.; Scott, H.M.; Simjee, S.; et al. Complexities in understanding antimicrobial resistance across domesticated animal, human, and environmental systems. Ann. N. Y. Acad. Sci. 2019, 1441, 17–30. [Google Scholar] [CrossRef]
- The Evolving Threat of Antimicrobial Resistance-Options for Action. Available online: http://apps.who.int/iris/bitstream/10665/44812/1/9789241503181_eng.pdf (accessed on 20 March 2022).
- Cantas, L.; Suer, K. The important bacterial zoonoses in “one health” concept. Front. Public Health 2014, 2, 144. [Google Scholar] [CrossRef] [PubMed]
- van den Bogaard, A.E.; Stobberingh, E.E. Epidemiology of resistance to antibiotics. Links between animals and humans. Int. J. Antimicrob. Agents 2000, 14, 327–335. [Google Scholar] [CrossRef]
- CDC. Core Elements of Hospital Antibiotic Stewardship Programs. Centers for Disease Control and Prevention. 2014. Available online: http://www.cdc.gov/getsmart/healthcare/pdfs/checklist.pdf (accessed on 22 September 2021).
- Gozdzielewska, L.; King, C.; Flowers, P.; Mellor, D.; Dunlop, P.; Price, L. Scoping review of approaches for improving antimicrobial stewardship in livestock farmers and veterinarians. Prev. Vet. Med. 2020, 180, 105025. [Google Scholar] [CrossRef]
- Suaifan, G.A. A cross-sectional study on knowledge, attitude and behavior related to antibiotic use and resistance among medical and non-medical university students in Jordan. Afr. J. Pharm. Pharmacol. 2012, 6. [Google Scholar] [CrossRef]
- Jairoun, A.; Hassan, N.; Ali, A.; Jairoun, O.; Shahwan, M. Knowledge, attitude and practice of antibiotic use among university students: A Cross Sectional Study in UAE. BMC Public Health 2019, 19, 518. [Google Scholar] [CrossRef]
- Sannathimmappa, M.B.; Nambiar, V.; Aravindakshan, R. A cross-sectional study to evaluate the knowledge and attitude of medical students concerning antibiotic usage and antimicrobial resistance. Int. J. Acad. Med. 2021, 7, 113–119. [Google Scholar] [CrossRef]
- Chapot, L.; Sarker, M.S.; Begum, R.; Hossain, D.; Akter, R.; Hasan, M.M.; Bayzid, M.; Salauddin, M.; Parvej, M.S.; Uddin, A.M.; et al. Knowledge, attitudes and practices regarding antibiotic use and resistance among veterinary students in Bangladesh. Antibiotics 2021, 10, 332. [Google Scholar] [CrossRef] [PubMed]
- Pena Betancourt, S.D.; Posadas Pena, S.D.; Parra-Forero, L.Y. The knowledge of antibiotics in veternary students and repercution in human health. Health 2020, 12, 1632–1639. [Google Scholar] [CrossRef]
- WHO. Central Asian and Eastern European Surveillance of Antimicrobial Resistance. Annual Report. 2020. Available online: http://www.euro.who.int/__data/assets/pdf_file/0007/386161/52238-WHO-CAESAR-AR2018_low_V11_web.pdf?ua=1 (accessed on 22 September 2021).
- WHO. Report on Surveillance of Antibiotic Consumption: 2016–2018. Early Implementation; World Health Organization: Geneva, Switzerland, 2018; Available online: https://www.who.int/medicines/areas/rational_use/who-amr-amc-report20181109.pdf (accessed on 16 September 2021).
- Republic of Serbia: National Antibiotic Resistance Control Programme for the Period 2019–2021. Available online: https://www.who.int/publications/m/item/republic-of-serbia-national-antibiotic-resistance-control-programme-for-the-period-2019-2021 (accessed on 22 September 2021).
- Horvat, O.J.; Tomas, A.D.; Paut Kusturica, M.M.; Savkov, A.V.; Bukumiric, D.U.; Tomic, Z.S.; Sabo, A.J. Is the level of knowledge a predictor of rational antibiotic use in Serbia? PLoS ONE 2017, 12, e0180799. [Google Scholar] [CrossRef]
- Huang, Y.; Gu, J.; Zhang, M.; Ren, Z.; Yang, W.; Chen, Y.; Fu, Y.; Chen, X.; Cals, J.W.; Zhang, F. Knowledge, attitude and practice of antibiotics: A questionnaire study among 2500 Chinese students. BMC Med. Educ. 2013, 13, 163. [Google Scholar] [CrossRef] [PubMed]
- Ganesh, M.; Sridevi, S.; Paul, C. Antibiotic use among medical and Para medical students: Knowledge, attitude and its practice in a tertiary health care Centre in Chennai—A scientific insight. Int. J. Sci. Res. 2014, 3, 332–335. [Google Scholar]
- Shehadeh, M.; Suaifan, G.; Darwish, R.M.; Wazaify, M.; Zaru, L.; Alja’fari, S. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm. J. 2012, 20, 125–133. [Google Scholar] [CrossRef] [PubMed]
- Scaioli, G.; Gualano, M.R.; Gili, R.; Masucci, S.; Bert, F.; Siliquini, R. Antibiotic use: A cross-sectional survey assessing the knowledge, attitudes and practices amongst students of a school of medicine in Italy. PLoS ONE 2015, 10, e0122476. [Google Scholar] [CrossRef]
- Sobierajski, T.; Mazińska, B.; Chajęcka-Wierzchowska, W.; Smiałek, M.; Hryniewicz, W. Antimicrobial and Antibiotic Resistance from the Perspective of Polish Veterinary Students: An Inter-University Study. Antibiotics 2022, 11, 115. [Google Scholar] [CrossRef]
- Humphreys, H.; Dillane, T.; O’Connell, B.; Luke, L.C. Survey of recent medical graduates’ knowledge and understanding of the treatment and prevention of infection. Ir. Med. J. 2006, 99, 58–59. [Google Scholar]
- Rusic, D.; Bozic, J.; Vilovic, M.; Bukic, J.; Zivkovic, P.M.; Leskur, D.; Seselja Perisin, A.; Tomic, S.; Modun, D. Attitudes and Knowledge Regarding Antimicrobial Use and Resistance Among Pharmacy and Medical Students at the University of Split, Croatia. Microb. Drug Resist. 2018, 24, 1521–1528. [Google Scholar] [CrossRef]
- Kaae, S.; Malaj, A.; Hoxha, I. Antibiotic knowledge, attitudes and behaviours of Albanian health care professionals and patients —A qualitative interview study. J. Pharm. Policy. Pract. 2017, 10, 13. [Google Scholar] [CrossRef]
- Zajmi, D.; Berisha, M.; Begolli, I.; Hoxha, R.; Mehmeti, R.; Mulliqi-Osmani, G.; Kurti, A.; Loku, A.; Raka, L. Public knowledge, attitudes and practices regarding antibiotic use in Kosovo. Pharm. Pract. 2017, 15, 827. [Google Scholar] [CrossRef] [PubMed]
- Alili-Idrizi, E.; Dauti, M.; Malaj, L. Validation of the parental knowledge and attitude towards antibiotic usage and resistance among children in Tetovo, the Republic of Macedonia. Pharm. Pract. 2014, 12, 467. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Azevedo, M.M.; Pinheiro, C.; Yaphe, J.; Baltazar, F. Portuguese students’ knowledge of antibiotics: A cross-sectional study of secondary school and university students in Braga. BMC Public Health 2009, 9, 359. [Google Scholar] [CrossRef]
- Dyar, O.J.; Howard, P.; Nathwani, D.; Pulcini, C. Knowledge, attitudes, and beliefs of French medical students about antibiotic prescribing and resistance. Med. Mal. Infect. 2013, 43, 423–430. [Google Scholar] [CrossRef]
- Jairoun, A.; Hassan, N.; Ali, A.; Jairoun, O.; Shahwan, M. A cross sectional study on knowledge, attitude and practice of medical students toward antibiotic resistance and its prescription, Iran. Adv. Environ. Biol. 2014, 8, 675–681. [Google Scholar]
- Jamshed, S.Q.; Elkalmi, R.; Rajiah, K.; Al-Shami, A.K.; Shamsudin, S.H.; Siddiqui, M.J.; Abdul Aziz, M.A.; Hanafi, M.B.; Mohammad Shariff, N.I.; Ramlan, N.H.; et al. Understanding of antibiotic use and resistance among final-year pharmacy and medical students: A pilot study. J. Infect. Dev. Ctries 2014, 8, 780–785. [Google Scholar] [CrossRef]
- Adembri, C.; Novelli, A. Pharmacokinetic and pharmacodynamic parameters of antimicrobials: Potential for providing dosing regimens that are less vulnerable to resistance. Clin. Pharmacokinet. 2009, 48, 517–528. [Google Scholar] [CrossRef]
- Popović, R.; Tomić, Z.; Tomas, A.; Anđelić, N.; Vicković, S.; Jovanović, G.; Bukumirić, D.; Horvat, O.; Sabo, A. Five-year surveillance and correlation of antibiotic consumption and resistance of Gram-negative bacteria at an intensive care unit in Serbia. J. Chemother. 2020, 32, 294–303. [Google Scholar] [CrossRef]
- Sobierajski, T.; Mazińska, B.; Wanke-Rytt, M.; Hryniewicz, W. Knowledge-based attitudes of medical students in antibiotic therapy and antibiotic resistance. A cross-sectional study. Int. J. Environ. Res. Public Health 2021, 18, 3930. [Google Scholar] [CrossRef]
- Golding, S.E.; Higgins, H.M.; Ogden, J. Assessing Knowledge, Beliefs, and Behaviors around Antibiotic Usage and Antibiotic Resistance among UK Veterinary Students: A Multi-Site, Cross-Sectional Survey. Antibiotics 2022, 11, 256. [Google Scholar] [CrossRef]
- Marta-Costa, A.; Miranda, C.; Silva, V.; Silva, A.; Martins, Â.; Pereira, J.E.; Maltez, L.; Capita, R.; Alonso-Calleja, C.; Igrejas, G.; et al. Survey of the Knowledge and Use of Antibiotics among Medical and Veterinary Health Professionals and Students in Portugal. Int. J. Environ. Res. Public Health 2021, 18, 2753. [Google Scholar] [CrossRef] [PubMed]
- Buke, C.; Hosgor-Limoncu, M.; Ermertcan, S.; Ciceklioglu, M.; Tuncel, M.; Kose, T.; Eren, S. Irrational use of antibiotics among university students. J. Infect. 2005, 51, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Alzahrani, A.A.H.; Alzahrani, M.S.A.; Aldannish, B.H.; Alghamdi, H.S.; Albanghali, M.A.; Almalki, S.S.R. Inappropriate dental antibiotic prescriptions: Potential driver of the antimicrobial resistance in Albaha region, Saudi Arabia. Risk Manag. Healthc. Policy 2020, 13, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Aljadeeah, S.; Wirtz, V.J.; Nagel, E. Outpatient Antibiotic Dispensing for the Population with Government Health Insurance in Syria in 2018–2019. Antibiotics 2020, 9, 570. [Google Scholar] [CrossRef]
- Jairoun, A.; Hassan, N.; Ali, A.; Jairoun, O.; Shahwan, M.; Hassali, M. University students’ knowledge, attitudes, and practice regarding antibiotic use and associated factors: A cross-sectional study in the United Arab Emirates. Int. J. Gen. Med. 2019, 12, 235–246. [Google Scholar] [CrossRef]
- Limaye, D.; Naware, S.; Bare, P.; Dalvi, S.; Dhurve, K.; Sydymanov, A.; Limaye, V.; Pitani, R.S.; Kanso, Z.; Fortwengel, G. Knowledge, attitude and practices of antibiotic usage among students from Mumbai University. Int. J. Res. Med. Sci. 2018, 6, 1908–1912. [Google Scholar] [CrossRef]
- Schröder, W.; Sommer, H.; Gladstone, B.P.; Foschi, F.; Hellman, J.; Evengard, B.; Tacconelli, E. Gender differences in antibiotic prescribing in the community: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2016, 71, 1800–1806. [Google Scholar] [CrossRef]
- Majeed, A.; Moser, K. Age-and sex-specific antibiotic prescribing patterns in general practice in England and Wales in 1996. Br. J. Gen. Pract. 1999, 49, 735–736. [Google Scholar]
- Odetokun, I.A.; Akpabio, U.; Alhaji, N.B.; Biobaku, K.T.; Oloso, N.O.; Ghali-Mohammed, I.; Biobaku, A.J.; Adetunji, V.O.; Fasina, F.O. Knowledge of antimicrobial resistance among veterinary students and their personal antibiotic use practices: A national cross-sectional survey. Antibiotics 2019, 8, 243. [Google Scholar] [CrossRef]
- Lv, B.; Zhou, Z.; Xu, G.; Yang, D.; Wu, L.; Shen, Q.; Jiang, M.; Wang, X.; Zhao, G.; Yang, S.; et al. Knowledge, attitudes and practices concerning self-medication with antibiotics among university students in western China. Trop. Med. Int. Health 2014, 19, 769–779. [Google Scholar] [CrossRef]
- Hardefeldt, L.; Nielsen, T.; Crabb, H.; Gilkerson, J.; Squires, R.; Heller, J.; Sharp, C.; Cobbold, R.; Norris, J.; Browning, G. Veterinary students’ knowledge and perceptions about antimicrobial stewardship and biosecurity—A national survey. Antibiotics 2018, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Benameur, T.; Al-Bohassan, H.; Al-Aithan, A.; Al-Beladi, A.; Al-Ali, H.; Al-Omran, H.; Saidi, N. Knowledge, attitude, behaviour of the future healthcare professionals towards the self-medication practice with antibiotics. J. Infect. Dev. Ctries 2019, 13, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Pant, N.; Sagtani, R.A.; Pradhan, M.; Bhattarai, A.; Sagtani, A. Self-medication with antibiotics among dental students of Kathmandu-prevalence and practice. Nepal Med. Coll. J. 2015, 17, 47–53. [Google Scholar]
- Banerjee, I.; Bhadury, T. Self-medication practice among undergraduate medical students in a tertiary care medical college, West Bengal. J. Postgrad. Med. 2012, 58, 127–131. [Google Scholar] [CrossRef] [PubMed]
- Elmahi, O.; Musa, R.; Shareef, A.; Omer, M.; Elmahi, M.; Altamih, R.; Mohamed, R.; Alsadig, T. Perception and practice of self-medication with antibiotics among medical students in Sudanese universities: A cross-sectional study. PLoS ONE 2022, 17, e0263067. [Google Scholar] [CrossRef]
- Dyar, O.J.; Hills, H.; Seitz, L.T.; Perry, A.; Ashiru-Oredope, D. Assessing the Knowledge, Attitudes and Behaviors of Human and Animal Health Students towards Antibiotic Use and Resistance: A Pilot Cross-Sectional Study in the UK. Antibiotics 2018, 7, 10. [Google Scholar] [CrossRef]
- Harakeh, S.; Almatrafi, M.; Ungapen, H.; Hammad, R.; Olayan, F.; Hakim, R.; Ayoub, M.; Bakhsh, N.; Almasaudi, S.B.; Barbour, E.; et al. Perceptions of medical students towards antibiotic prescribing for upper respiratory tract infections in Saudi Arabia. BMJ Open Respir. Res. 2015, 2, e000078. [Google Scholar] [CrossRef]
- Sarahroodi, S.; Arzi, A.; Sawalba, A.F.; Ashtarinezhad, A. Antibiotiotics self-medication among southern Iranian university students. Int. J. Pharmacol. 2010, 6, 48–52. [Google Scholar] [CrossRef]
| M | D | V | χ2 | p | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||
| Gender | Male | 75 | 37.5 | 26 | 26 | 49 | 49 | 11.285 | 0.004 | 150 | 37.5 |
| Female | 125 | 62.5 | 74 | 74 | 51 | 51 | 250 | 62.5 | |||
| Average grade | 6.00–7.99 | 21 | 10.5 | 8 | 8 | 39 | 39 | 46.031 | 0.001 | 68 | 17 |
| 8.00–10.00 | 179 | 89.5 | 92 | 92 | 61 | 61 | 332 | 83 | |||
| Place of living | with parents | 64 | 32 | 43 | 43 | 38 | 38 | 17.568 | 0.007 | 145 | 36.3 |
| in university dormitories | 33 | 16.5 | 7 | 7 | 14 | 14 | 54 | 13.5 | |||
| in rented apartments | 67 | 33.5 | 32 | 32 | 43 | 43 | 142 | 35.5 | |||
| in own apartment | 36 | 18 | 18 | 18 | 5 | 5 | 59 | 14.8 | |||
| Number of visits to GP in the last 12 months | None | 109 | 54.5 | 46 | 46 | 39 | 39.8 | 4.467 | 0.107 | 194 | 48.7 |
| 1–4 | 82 | 41 | 52 | 52 | 57 | 58.2 | 191 | 48 | |||
| 5–10 | 7 | 3.5 | 2 | 2 | 2 | 2 | 11 | 2.8 | |||
| >10 | 2 | 1 | 0 | 0 | 0 | 0 | 2 | 0.5 | |||
| Having a family member who is healthcare worker | Yes | 70 | 35 | 38 | 38 | 26 | 26 | 3.636 | 0.162 | 134 | 33.5 |
| No | 130 | 65 | 62 | 62 | 74 | 74 | 266 | 66.5 | |||
| M | D | V | χ2 | p | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Antibiotics are used to decrease fever | 174 | 87 | 91 | 91 | 75 | 75 | 11.234 | 0.004 |
| Antibiotics are used to decrease pain | 190 | 95 | 95 | 95 | 88 | 88 | 5.839 | 0.054 |
| Antibiotics are used to overcome malaise and fatigue | 197 | 98.5 | 97 | 97 | 97 | 97 | 1.023 | 0.501 |
| Antibiotics are used for common cold | 171 | 85.5 | 91 | 91 | 63 | 63 | 30.474 | <0.001 |
| Antibiotic treatment begins with an antibiotic found at home in order not to waste time | 180 | 90 | 95 | 95 | 94 | 94.9 | 3.551 | 0.169 |
| Antibiotic treatment is started after a visit to doctor and with a doctor’s prescription | 194 | 97 | 97 | 97 | 97 | 97 | 0.125 | 1 |
| Antibiotic treatment is started when it is advised by a pharmacist | 171 | 85.5 | 79 | 79 | 67 | 67 | 13.88 | <0.001 |
| Antibiotic is used until the symptoms disappear | 167 | 83.5 | 88 | 88 | 75 | 75 | 6.13 | 0.047 |
| Antibiotic is used until the bottle finishes | 136 | 68 | 65 | 65 | 55 | 55 | 4.98 | 0.084 |
| Antibiotic is used as long as the doctor prescribes | 194 | 97 | 97 | 97 | 96 | 96 | 0.239 | 0.933 |
| Taking the medicine twice a day means after waking up and before going to bed | 136 | 81.5 | 80 | 80 | 64 | 64 | 12.231 | 0.002 |
| Frequent and improper use of antibiotics is harmful and dangerous | 194 | 97 | 98 | 98 | 95 | 95 | 1.511 | 0.501 |
| M | D | V | χ2 | p | ||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Have you ever used antibiotics in order not to get ill? | ||||||||
| No | 200 | 100 | 100 | 100 | 100 | 100 | 1 | |
| Have you ever started antibiotics on your own when you got ill? | ||||||||
| Yes | 75 | 37.5 | 37 | 37 | 32 | 32 | 0.933 | 0.627 |
| Have you ever used antibiotics prescribed by the doctor irregularly? | ||||||||
| Yes | 42 | 21 | 21 | 21 | 34 | 34 | 6.9 | 0.032 |
| What do you do when you think that antibiotic you are taking is not effective? | ||||||||
| I stop taking it and go to the doctor | 36 | 18 | 22 | 22 | 43 | 43 | 32.444 | <0.001 |
| I stop taking it and go to another doctor | 8 | 4 | 1 | 1 | 6 | 6 | ||
| I use it for the recommended period | 144 | 72 | 65 | 65 | 43 | 43 | ||
| Other | 12 | 6 | 12 | 12 | 8 | 8 | ||
| How did you use antibiotics during your last infection? | ||||||||
| Until the bottle is finished | 38 | 19 | 27 | 27 | 22 | 22 | 9.634 | 0.047 |
| Until the symptoms disappeared | 13 | 6.5 | 12 | 12 | 15 | 15 | ||
| As advised by the doctor | 149 | 74.5 | 61 | 61 | 63 | 63 | ||
| How did you get antibiotics during your last infection? | ||||||||
| I used the antibiotic previously used or as advised by my friends or relatives | 5 | 2.5 | 8 | 8 | 5 | 5 | 8.354 | 0.392 |
| I used the antibiotic previously prescribed by my doctor | 17 | 8.5 | 4 | 4 | 9 | 9 | ||
| I visited my doctor and used the prescribed antibiotic | 144 | 72 | 73 | 73 | 69 | 69 | ||
| I asked the pharmacist and used the antibiotic recommended | 8 | 4 | 4 | 4 | 2 | 2 | ||
| I do not remember | 26 | 13 | 11 | 11 | 15 | 15 | ||
| Independent Variables | B | p | OR | 95% Confidence Intervals | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Male gender | Reference category | ||||
| Female gender | 0.571 | 0.02 | 1.8 | 1.095 | 0.571 |
| V | Reference category | ||||
| M | 0.082 | 0.006 | 2.23 | 1.25 | 3.96 |
| D | 0.769 | 0.026 | 2.16 | 1.09 | 4.24 |
| How often do you take antibiotics? | −0.214 | 0.132 | 0.087 | 0.611 | 1.07 |
| Average grade | 1.204 | <0.001 | 3.332 | 1.77 | 6.28 |
| Have you ever used antibiotics prescribed by the doctor irregularly? | −0.376 | 0.174 | 0.687 | 0.39 | 1.18 |
| How did you use antibiotics during your last infection? | |||||
| Until the symptoms disappeared | Reference category | ||||
| As advised by the doctor | 1.964 | <0.001 | 7.13 | 3.01 | 16.83 |
| Until the bottle is finished | 0.974 | 0.036 | 2.649 | 1.06 | 6.58 |
| Independent Variables | B | p | OR | 95% Confidence Intervals | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| How often do you take antibiotics? | 0.587 | <0.001 | 1.798 | 1.35 | 2.38 |
| Have you ever used antibiotics prescribed by the doctor irregularly? | 0.719 | 0.007 | 2.052 | 1.21 | 3.47 |
| As advised by the doctor | Reference category | ||||
| Until the bottle is finished | 1.01 | <0.001 | 2.746 | 1.62 | 4.65 |
| Until the symptoms disappeared | 2.142 | <0.001 | 8.514 | 3.33 | 21.76 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Horvat, O.; Petrović, A.T.; Paut Kusturica, M.; Bukumirić, D.; Jovančević, B.; Kovačević, Z. Survey of the Knowledge, Attitudes and Practice towards Antibiotic Use among Prospective Antibiotic Prescribers in Serbia. Antibiotics 2022, 11, 1084. https://doi.org/10.3390/antibiotics11081084
Horvat O, Petrović AT, Paut Kusturica M, Bukumirić D, Jovančević B, Kovačević Z. Survey of the Knowledge, Attitudes and Practice towards Antibiotic Use among Prospective Antibiotic Prescribers in Serbia. Antibiotics. 2022; 11(8):1084. https://doi.org/10.3390/antibiotics11081084
Chicago/Turabian StyleHorvat, Olga, Ana Tomas Petrović, Milica Paut Kusturica, Dragica Bukumirić, Bojana Jovančević, and Zorana Kovačević. 2022. "Survey of the Knowledge, Attitudes and Practice towards Antibiotic Use among Prospective Antibiotic Prescribers in Serbia" Antibiotics 11, no. 8: 1084. https://doi.org/10.3390/antibiotics11081084
APA StyleHorvat, O., Petrović, A. T., Paut Kusturica, M., Bukumirić, D., Jovančević, B., & Kovačević, Z. (2022). Survey of the Knowledge, Attitudes and Practice towards Antibiotic Use among Prospective Antibiotic Prescribers in Serbia. Antibiotics, 11(8), 1084. https://doi.org/10.3390/antibiotics11081084







