In Vitro Study of the Interaction of Gentamicin with Ceftriaxone and Azithromycin against Neisseria gonorrhoeae Using Agar Dilution Method
Abstract
:1. Introduction
2. Methods
2.1. N. gonorrhoeae Isolates
2.2. Antimicrobial Susceptibility Testing
2.3. Synergy Testing
2.4. Statistical Analysis
3. Results
3.1. Antimicrobial Susceptibility Results of 380 N. gonorrhoeae Isolates
3.2. Synergy of Three Dual Antimicrobial Combinations
3.3. MICs of the Indicated Antibiotics as Monotherapy and in Combination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Quillin, S.J.; Seifert, H.S. Neisseria gonorrhoeae host adaptation and pathogenesis. Nat. Rev. Microbiol. 2018, 16, 226–240. [Google Scholar] [CrossRef] [PubMed]
- Rowley, J.; Vander Hoorn, S.; Korenromp, E.; Low, N.; Unemo, M.; Abu-Raddad, L.J.; Chico, R.M.; Smolak, A.; Newman, L.; Gottlieb, S.; et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: Global prevalence and incidence estimates, 2016. Bull. World Health Organ. 2019, 97, 548–562. [Google Scholar] [CrossRef] [PubMed]
- Unemo, M.; Seifert, H.S.; Hook, E.W., 3rd; Hawkes, S.; Ndowa, F.; Dillon, J.R. Gonorrhoea. Nat. Rev. Dis. Primers 2019, 5, 79. [Google Scholar] [CrossRef]
- Unemo, M.; Ross, J.; Serwin, A.B.; Gomberg, M.; Cusini, M.; Jensen, J.S. 2020 European guideline for the diagnosis and treatment of gonorrhoea in adults. Int. J. STD AIDS 2020, 32, 956462420949126. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Update to CDC’s Sexually transmitted diseases treatment guidelines, 2010: Oral cephalosporins no longer a recommended treatment for gonococcal infections. MMWR Morb. Mortal. Wkly. Rep. 2012, 61, 590–594. [Google Scholar]
- World Health Organization. WHO Guidelines for the Treatment of Neisseria gonorrhoeae. In WHO Guidelines Approved by the Guidelines Review Committee; World Health Organization: Geneva, Switzerland, 2016; pp. 17–18. Available online: https://www.ncbi.nlm.nih.gov/books/NBK379221/ (accessed on 1 June 2022).
- Dong, H.V.; Klausner, J.D. Neisseria gonorrhoeae resistance driven by antibiotic use. Nat. Rev. Urol. 2019, 16, 509–510. [Google Scholar] [CrossRef]
- Chen, S.C.; Han, Y.; Yuan, L.F.; Zhu, X.Y.; Yin, Y.P. Identification of Internationally Disseminated Ceftriaxone-Resistant Neisseria gonorrhoeae Strain FC428, China. Emerg. Infect. Dis. 2019, 25, 1427–1429. [Google Scholar] [CrossRef] [Green Version]
- Williamson, D.A.; Fairley, C.K.; Howden, B.P.; Chen, M.Y.; Stevens, K.; De Petra, V.; Denham, I.; Chow, E.P.F. Trends and Risk Factors for Antimicrobial-Resistant Neisseria gonorrhoeae, Melbourne, Australia, 2007 to 2018. Antimicrob. Agents Chemother. 2019, 63, e01211–e1219. [Google Scholar] [CrossRef] [Green Version]
- Seña, A.C.; Bachmann, L.; Johnston, C.; Wi, T.; Workowski, K.; Hook, E.W., 3rd; Hocking, J.S.; Drusano, G.; Unemo, M. Optimising treatments for sexually transmitted infections: Surveillance, pharmacokinetics and pharmacodynamics, therapeutic strategies, and molecular resistance prediction. Lancet Infect. Dis. 2020, 20, e181–e191. [Google Scholar] [CrossRef]
- Campoccia, D.; Montanaro, L.; Arciola, C.R. A review of the biomaterials technologies for infection-resistant surfaces. Biomaterials 2013, 34, 8533–8554. [Google Scholar] [CrossRef]
- Workowski, K.A.; Bachmann, L.H.; Chan, P.A.; Johnston, C.M.; Muzny, C.A.; Park, I.; Reno, H.; Zenilman, J.M.; Bolan, G.A. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Morb. Mortal. Wkly. Rep. Recomm. Rep. 2021, 70, 1–187. [Google Scholar] [CrossRef] [PubMed]
- Matoga, M.; Chen, J.S.; Krysiak, R.; Ndalama, B.; Massa, C.; Bonongwe, N.; Mathiya, E.; Kamtambe, B.; Jere, E.; Chikaonda, T.; et al. Gentamicin susceptibility in Neisseria gonorrhoeae and treatment outcomes for urogenital gonorrhea after twenty-five years of sustained gentamicin use in Malawi. Sex. Transm. Dis. 2022, 49, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.W.; Xu, W.Q.; Zhu, X.Y.; Dai, X.Q.; Chen, S.C.; Han, Y.; Liu, J.; Chen, X.S.; Yin, Y.P. Gentamicin susceptibility of Neisseria gonorrhoeae isolates from 7 provinces in China. Infect. Drug Resist. 2019, 12, 2471–2476. [Google Scholar] [CrossRef] [Green Version]
- Dowell, D.; Kirkcaldy, R.D. Effectiveness of gentamicin for gonorrhoea treatment: Systematic review and meta-analysis. Sex. Transm. Infect. 2012, 88, 589–594. [Google Scholar] [CrossRef] [PubMed]
- Kirkcaldy, R.D.; Weinstock, H.S.; Moore, P.C.; Philip, S.S.; Wiesenfeld, H.C.; Papp, J.R.; Kerndt, P.R.; Johnson, S.; Ghanem, K.G.; Hook, E.W., 3rd. The efficacy and safety of gentamicin plus azithromycin and gemifloxacin plus azithromycin as treatment of uncomplicated gonorrhea. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2014, 59, 1083–1091. [Google Scholar] [CrossRef] [Green Version]
- Unemo, M.; Shafer, W.M. Antimicrobial resistance in Neisseria gonorrhoeae in the 21st century: Past, evolution, and future. Clin. Microbiol. Rev. 2014, 27, 587–613. [Google Scholar] [CrossRef] [Green Version]
- Bollenbach, T. Antimicrobial interactions: Mechanisms and implications for drug discovery and resistance evolution. Curr. Opin. Microbiol. 2015, 27, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Unemo, M.; Ballard, R.; Ison, C.; Lewis, D.; Ndowa, F.; Peeling, R. Laboratory Diagnosis of Sexually Transmitted Infections, including Human Immunodeficiency Virus; World Health Organization: Geneva, Switzerland, 2013; pp. 39–44. Available online: https://apo.who.int/publications/i/item/9789241505840 (accessed on 7 June 2022).
- Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing, 29th ed.; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2019; pp. 78–82. Available online: https://clsi.org/media/pqlom3b5/_m100_archived_drugs_table.pdf (accessed on 10 June 2022).
- Li, X.; Le, W.; Lou, X.; Wang, B.; Genco, C.A.; Rice, P.A.; Su, X. In Vitro Efficacy of Gentamicin Alone and in Combination with Ceftriaxone, Ertapenem, and Azithromycin against Multidrug-Resistant Neisseria gonorrhoeae. Microbiol. Spectr. 2021, 9, e0018121. [Google Scholar] [CrossRef]
- White, R.L.; Burgess, D.S.; Manduru, M.; Bosso, J.A. Comparison of three different in vitro methods of detecting synergy: Time-kill, checkerboard, and E test. Antimicrob. Agents Chemother. 1996, 40, 1914–1918. [Google Scholar] [CrossRef] [Green Version]
- Odds, F.C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 2003, 52, 1. [Google Scholar] [CrossRef]
- Bidaud, A.L.; Schwarz, P.; Chowdhary, A.; Dannaoui, E. In Vitro Antifungal Combination of Terbinafine with Itraconazole against Isolates of Trichophyton Species. Antimicrob. Agents Chemother. 2022, 66, e0144921. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Yan, J.; Zhang, J.; van der Veen, S. Evaluation of alternative antibiotics for susceptibility of gonococcal isolates from China. Int. J. Antimicrob. Agents 2020, 55, 105846. [Google Scholar] [CrossRef] [PubMed]
- Barbee, L.A.; Soge, O.O.; Holmes, K.K.; Golden, M.R. In vitro synergy testing of novel antimicrobial combination therapies against Neisseria gonorrhoeae. J. Antimicrob. Chemother. 2014, 69, 1572–1578. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wind, C.M.; de Vries, H.J.; van Dam, A.P. Determination of in vitro synergy for dual antimicrobial therapy against resistant Neisseria gonorrhoeae using Etest and agar dilution. Int. J. Antimicrob. Agents 2015, 45, 305–308. [Google Scholar] [CrossRef] [Green Version]
- Sopirala, M.M.; Mangino, J.E.; Gebreyes, W.A.; Biller, B.; Bannerman, T.; Balada-Llasat, J.M.; Pancholi, P. Synergy testing by Etest, microdilution checkerboard, and time-kill methods for pan-drug-resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 2010, 54, 4678–4683. [Google Scholar] [CrossRef] [Green Version]
- Singh, V.; Bala, M.; Bhargava, A.; Kakran, M.; Bhatnagar, R. In vitro efficacy of 21 dual antimicrobial combinations comprising novel and currently recommended combinations for treatment of drug resistant gonorrhoea in future era. PLoS ONE 2018, 13, e0193678. [Google Scholar] [CrossRef]
- Sood, S.; Agarwal, S.K.; Singh, R.; Gupta, S.; Sharma, V.K. In vitro assessment of gentamicin and azithromycin-based combination therapy against Neisseria gonorrhoeae isolates in India. J. Med. Microbiol. 2019, 68, 555–559. [Google Scholar] [CrossRef]
- Bharat, A.; Martin, I.; Zhanel, G.G.; Mulvey, M.R. In vitro potency and combination testing of antimicrobial agents against Neisseria gonorrhoeae. J. Infect. Chemother. Off. J. Jpn. Soc. Chemother. 2016, 22, 194–197. [Google Scholar] [CrossRef]
- Triggs, E.; Charles, B. Pharmacokinetics and therapeutic drug monitoring of gentamicin in the elderly. Clin. Pharmacokinet. 1999, 37, 331–341. [Google Scholar] [CrossRef]
- Crokaert, F.; Hubloux, A.; Cauchie, P. A Phase I Determination of Azithromycin in Plasma during a 6-Week Period in Normal Volunteers after a Standard Dose of 500 mg Once Daily for 3 Days. Clin. Drug Investig. 1998, 16, 161–166. [Google Scholar] [CrossRef]
| Antimicrobial | Characterization | Number of Isolates for Which MIC to GEN Was | Total | Correlation to Gen | ||||
|---|---|---|---|---|---|---|---|---|
| ≤2 mg/L | 4 mg/L | 8 mg/L | 16 mg/L | 32 mg/L | ||||
| Gentamicin | - | 27 | 112 | 173 | 60 | 8 | 380 | - |
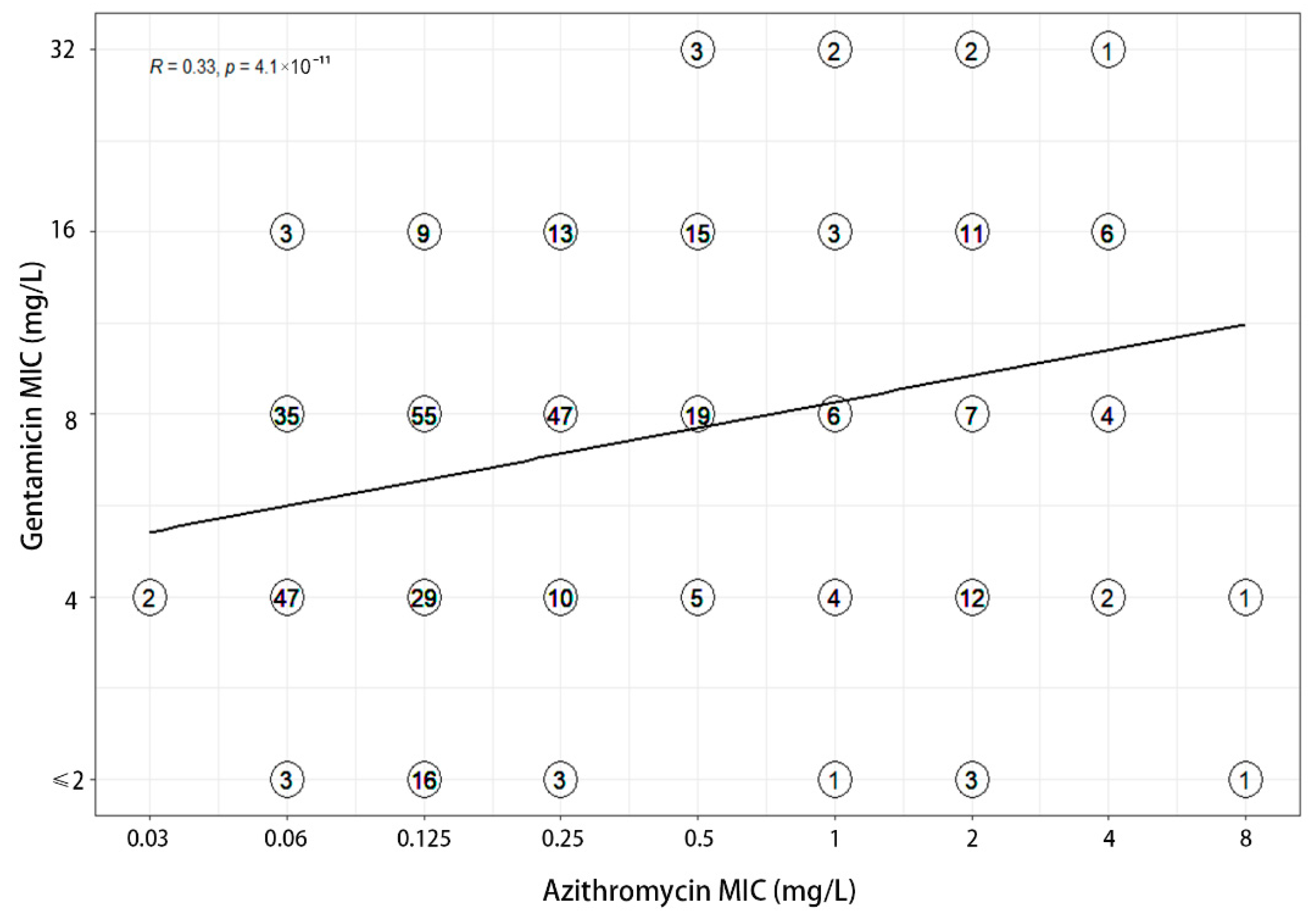
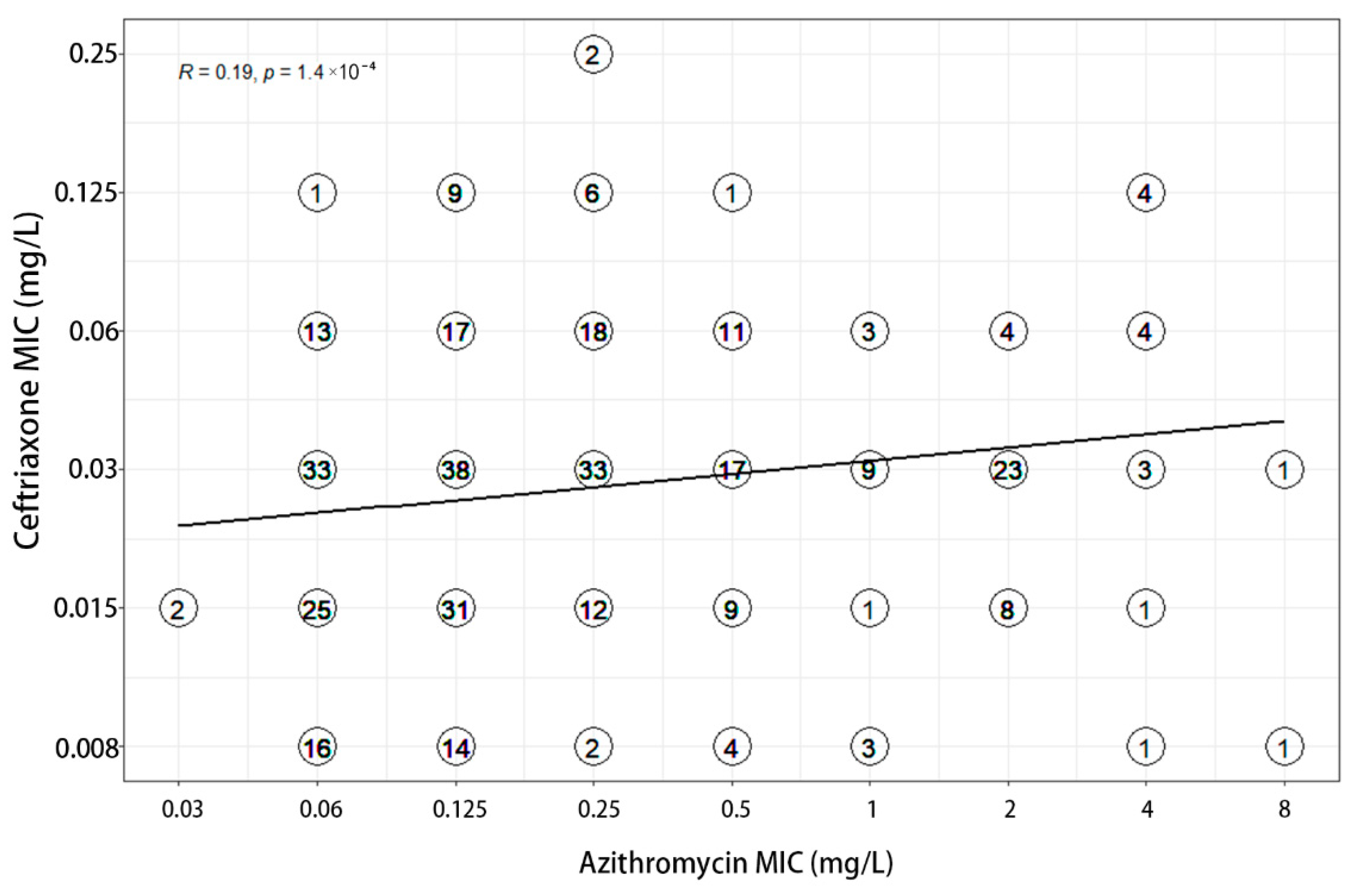
| Azithromycin | Susceptible | 22 | 93 | 156 | 40 | 3 | 314 | R = 0.33 |
| Resistant | 5 | 19 | 17 | 20 | 5 | 66 | ||
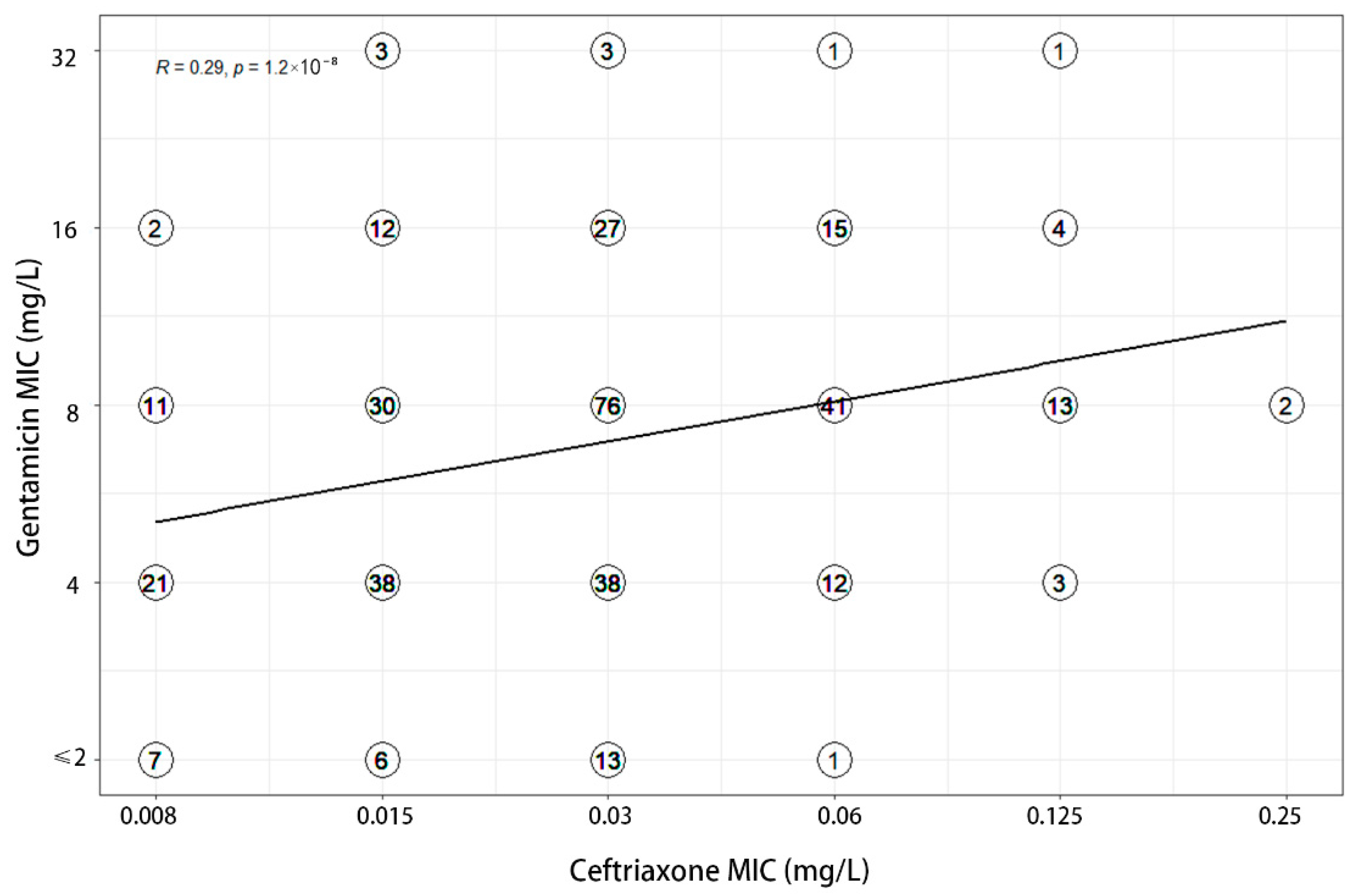
| Ceftriaxone | Susceptible | 27 | 112 | 171 | 60 | 8 | 378 | R = 0.29 |
| Resistant | 0 | 0 | 2 | 0 | 0 | 2 | ||
| Effect. | GEN and CRO | GEN and AZM | AZM and CRO |
|---|---|---|---|
| Synergistic [n (%)] | 43 (11.3) | 15 (3.9) | 42 (11.1) |
| Indifferent [n (%)] | 335 (88.2) | 365 (96.1) | 333 (87.6) |
| Antagonistic [n (%)] | 2 (0.5) | 0 (0) | 5 (1.3) |
| FICI (geometric mean) | 0.832 (0.370–4.5) | 0.987 (0.280–3) | 0.874 (0.280–6.167) |
| Classification overall | Indifferent | Indifferent | Indifferent |
| MIC Geometric Mean (Range) (mg/L) | FICI | Interpretation | ||||
|---|---|---|---|---|---|---|
| MICA | MICA (with B) | MICB | MICB (with A) | |||
| GEN and CRO | ||||||
| CRO MIC ≤ 0.125 mg/L (n = 378) | 6.758 (1–32) | 2.320 (1–16) | 0.027 (0.004–0.125) | 0.013 (0.004–0.125) | 0.833 (0.37–4.5) | indifference |
| CRO MIC ≥ 0.25 mg/L (n = 2) | 8 | 4 | 0.25 | 0.03 | 0.62 | indifference |
| GEN and CRO all isolates (n = 380) | 6.764 (1–32) | 2.327 (1–16) | 0.027 (0.008–0.25) | 0.014 (0.004–0.125) | 0.832 (0.370–4.5) | indifference |
| GEN and AZM | ||||||
| AZM MIC ≤ 0.5 mg/L (n = 314) | 6.515 (1–32) | 3.504 (1–16) | 0.143 (0.03–0.5) | 0.052 (0.015–0.25) | 1.004 (0.365–3) | indifference |
| AZM MIC ≥ 1 mg/L (n = 66) | 8.084 (2–32) | 5.367 (1–16) | 2.021 (1–8) | 0.314 (0.06–4) | 0.919 (0.28–3) | indifference |
| GEN + AZM all isolates (n = 380) | 6.764 (1–32) | 3.773 (1–16) | 0.226 (0.03–8) | 0.072 (0.015–4) | 0.987 (0.280–3) | indifference |
| AZM and CRO all isolates (n = 380) | 0.226 (0.03–8) | 0.1 (0.015–4) | 0.027 (0.008–0.25) | 0.017 (0.004–0.25) | 0.874 (0.280–6.167) | indifference |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, W.; Zhou, Q.; Liu, J.; Zhang, Y.; Zhu, X.; Zhu, B.; Yin, Y. In Vitro Study of the Interaction of Gentamicin with Ceftriaxone and Azithromycin against Neisseria gonorrhoeae Using Agar Dilution Method. Antibiotics 2022, 11, 1083. https://doi.org/10.3390/antibiotics11081083
Xu W, Zhou Q, Liu J, Zhang Y, Zhu X, Zhu B, Yin Y. In Vitro Study of the Interaction of Gentamicin with Ceftriaxone and Azithromycin against Neisseria gonorrhoeae Using Agar Dilution Method. Antibiotics. 2022; 11(8):1083. https://doi.org/10.3390/antibiotics11081083
Chicago/Turabian StyleXu, Wenqi, Qian Zhou, Jingwei Liu, Yan Zhang, Xiaoyu Zhu, Bangyong Zhu, and Yueping Yin. 2022. "In Vitro Study of the Interaction of Gentamicin with Ceftriaxone and Azithromycin against Neisseria gonorrhoeae Using Agar Dilution Method" Antibiotics 11, no. 8: 1083. https://doi.org/10.3390/antibiotics11081083
APA StyleXu, W., Zhou, Q., Liu, J., Zhang, Y., Zhu, X., Zhu, B., & Yin, Y. (2022). In Vitro Study of the Interaction of Gentamicin with Ceftriaxone and Azithromycin against Neisseria gonorrhoeae Using Agar Dilution Method. Antibiotics, 11(8), 1083. https://doi.org/10.3390/antibiotics11081083






