Outpatient Antibiotic and Antiviral Utilization Patterns in Patients Tested for Respiratory Pathogens in the United States: A Real-World Database Study
Abstract
:1. Introduction
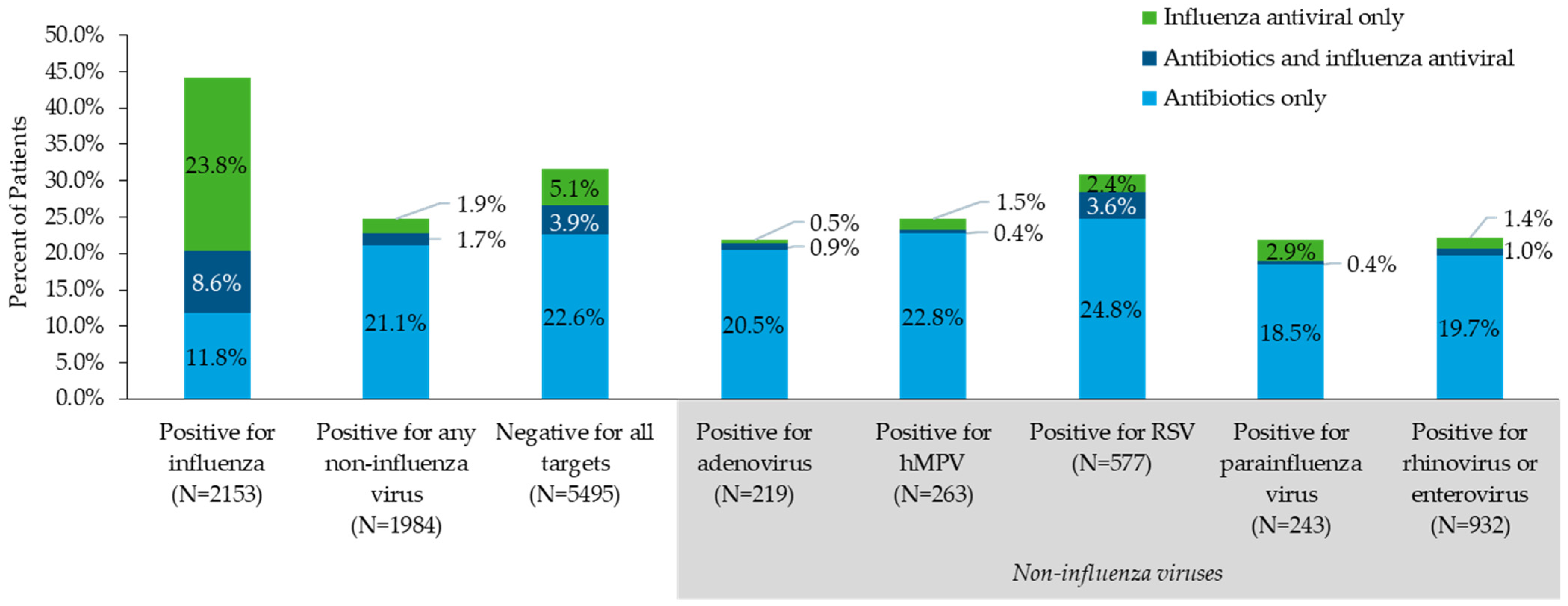
2. Results
3. Discussion
4. Methods
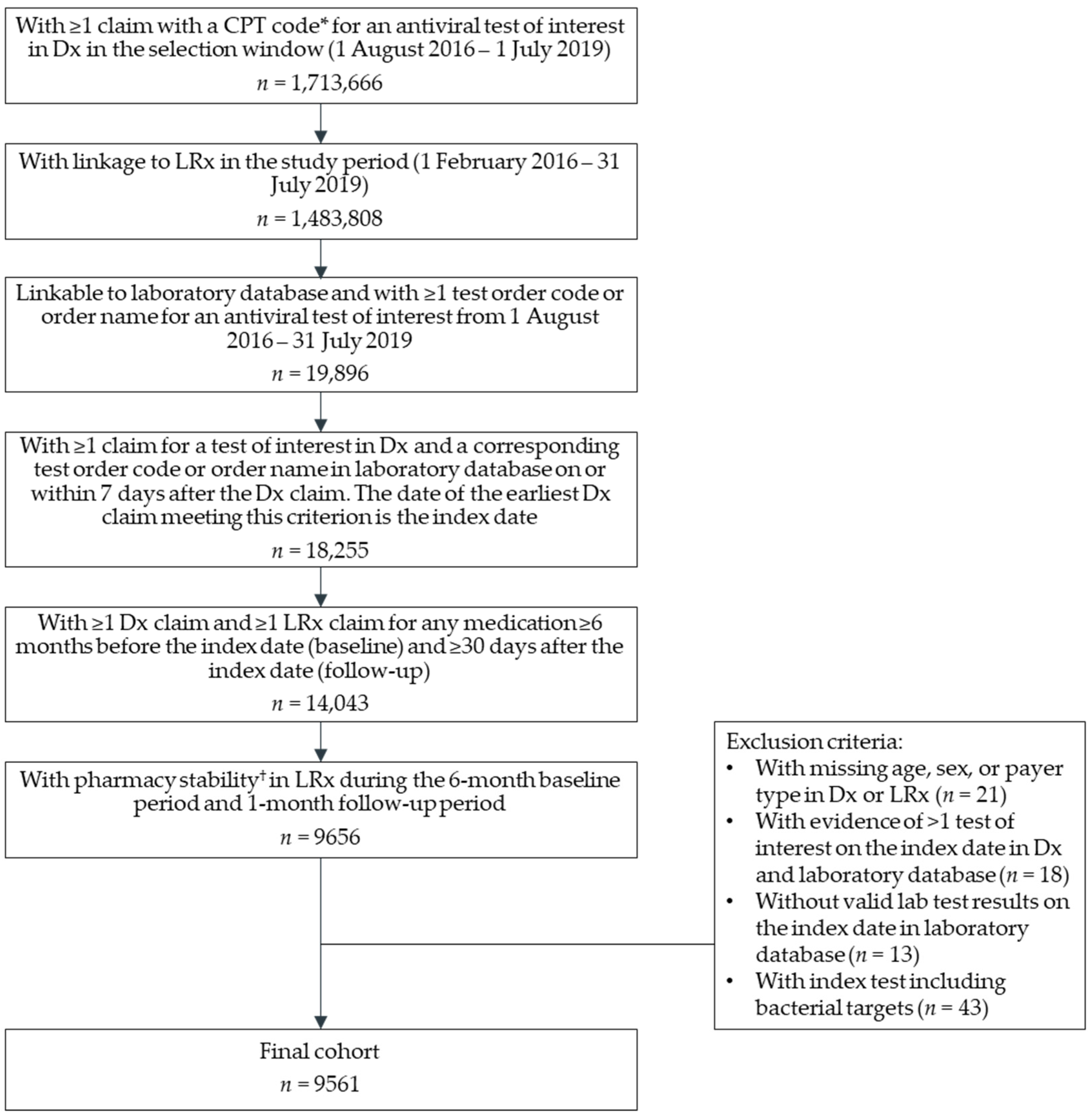
4.1. Study Population
4.2. Study Measures
4.3. Statistical Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fendrick, A.M.; Monto, A.S.; Nightengale, B.; Sarnes, M. The economic burden of non-influenza-related viral respiratory tract infection in the United States. Arch. Intern. Med. 2003, 163, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, D.J.; Hicks, L.A.; Pavia, A.T.; Hersh, A.L. Antibiotic prescribing for adults in ambulatory care in the USA, 2007-09. J. Antimicrob. Chemother. 2014, 69, 234–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCaig, L.F.; Hughes, J.M. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA 1995, 273, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Grijalva, C.G.; Nuorti, J.P.; Griffin, M.R. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA J. Am. Med Assoc. 2009, 302, 758–766. [Google Scholar] [CrossRef] [Green Version]
- Havers, F.P.; Hicks, L.A.; Chung, J.R.; Gaglani, M.; Murthy, K.; Zimmerman, R.K.; Jackson, L.A.; Petrie, J.G.; McLean, H.Q.; Nowalk, M.P.; et al. Outpatient Antibiotic Prescribing for Acute Respiratory Infections During Influenza Seasons. JAMA Netw. Open 2018, 1, e180243. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Antibiotic Use in the United States, 2018 Update: Progress and Opportunities. Available online: https://www.cdc.gov/antibiotic-use/stewardship-report/pdf/stewardship-report-2018-508.pdf (accessed on 15 October 2021).
- Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States. 2019. Available online: https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf (accessed on 15 October 2021).
- U.S. Department of Health and Human Services. National Action Plan for Combating Antibiotic-Resistant Bacteria, 2020–2025. Available online: https://aspe.hhs.gov/sites/default/files/migrated_legacy_files//196436/CARB-National-Action-Plan-2020-2025.pdf (accessed on 15 October 2021).
- Curren, E.J.; Lutgring, J.D.; Kabbani, S.; Diekema, D.J.; Gitterman, S.; Lautenbach, E.; Morgan, D.J.; Rock, C.; Salerno, R.M.; McDonald, L.C. Advancing Diagnostic Stewardship for Healthcare Associated Infections, Antibiotic Resistance, and Sepsis. Clin. Infect. Dis. 2022, 74, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Beganovic, M.; McCreary, E.K.; Mahoney, M.V.; Dionne, B.; Green, D.A.; Timbrook, T.T. Interplay between Rapid Diagnostic Tests and Antimicrobial Stewardship Programs among Pa..atients with Bloodstream and Other Severe Infections. J. Appl. Lab. Med. 2019, 3, 601–616. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- U.S. Food & Drug Administration. Nucleic Acid Based Tests. Available online: https://www.fda.gov/medical-devices/in-vitro-diagnostics/nucleic-acid-based-tests (accessed on 1 November 2021).
- Hanson, K.E.; Azar, M.M.; Banerjee, R.; Chou, A.; Colgrove, R.C.; Ginocchio, C.C.; Hayden, M.K.; Holodiny, M.; Jain, S.; Koo, S.; et al. Molecular Testing for Acute Respiratory Tract Infections: Clinical and Diagnostic Recommendations From the IDSA’s Diagnostics Committee. Clin. Infect. Dis. 2020, 71, 2744–2751. [Google Scholar] [CrossRef]
- Brendish, N.J.; Malachira, A.K.; Armstrong, L.; Houghton, R.; Aitken, S.; Nyimbili, E.; Ewings, S.; Lillie, P.J.; Clark, T.W. Routine molecular point-of-care testing for respiratory viruses in adults presenting to hospital with acute respiratory illness (ResPOC): A pragmatic, open-label, randomised controlled trial. Lancet Respir. Med. 2017, 5, 401–411. [Google Scholar] [CrossRef]
- Andrews, D.; Chetty, Y.; Cooper, B.S.; Virk, M.; Glass, S.K.; Letters, A.; Kelly, P.A.; Sudhanva, M.; Jeyaratnam, D. Multiplex PCR point of care testing versus routine, laboratory-based testing in the treatment of adults with respiratory tract infections: A quasi-randomised study assessing impact on length of stay and antimicrobial use. BMC Infect. Dis. 2017, 17, 671. [Google Scholar] [CrossRef] [Green Version]
- Semret, M.; Schiller, I.; Jardin, B.A.; Frenette, C.; Loo, V.G.; Papenburg, J.; McNeil, S.A.; Dendukuri, N. Multiplex Respiratory Virus Testing for Antimicrobial Stewardship: A Prospective Assessment of Antimicrobial Use and Clinical Outcomes Among Hospitalized Adults. J. Infect. Dis. 2017, 216, 936–944. [Google Scholar] [CrossRef] [Green Version]
- Rappo, U.; Schuetz, A.N.; Jenkins, S.G.; Calfee, D.P.; Walsh, T.J.; Wells, M.T.; Hollenberg, J.P.; Glesby, M.J. Impact of Early Detection of Respiratory Viruses by Multiplex PCR Assay on Clinical Outcomes in Adult Patients. J. Clin. Microbiol. 2016, 54, 2096–2103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rogers, B.B.; Shankar, P.; Jerris, R.C.; Kotzbauer, D.; Anderson, E.J.; Watson, J.R.; O’Brien, L.A.; Uwindatwa, F.; McNamara, K.; Bost, J.E. Impact of a rapid respiratory panel test on patient outcomes. Arch. Pathol. Lab. Med. 2015, 139, 636–641. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burrowes, S.A.B.; Rader, A.; Ni, P.; Drainoni, M.L.; Barlam, T.F. Low Uptake of Rapid Diagnostic Tests for Respiratory Tract Infections in an Urban Safety Net Hospital. Open Forum Infect. Dis. 2020, 7, ofaa057. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Influenza Antiviral Medications: Summary for Clinicians. Available online: https://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm (accessed on 29 November 2021).
- Rzewuska, M.; Duncan, E.M.; Francis, J.J.; Morris, A.M.; Suh, K.N.; Davey, P.G.; Grimshaw, J.M.; Ramsay, C.R. Barriers and Facilitators to Implementation of Antibiotic Stewardship Programmes in Hospitals in Developed Countries: Insights From Transnational Studies. Front. Sociol. 2020, 5, 41. [Google Scholar] [CrossRef] [PubMed]
- The Pew Charitable Trusts. National Survey Reveals Barriers to Outpatient Antibiotic Stewardship Efforts. Available online: https://www.pewtrusts.org/-/media/assets/2020/09/nationalsurveyrevealsbarriersoutpatientantibioticstewardshipefforts.pdf (accessed on 15 February 2022).
- MacVane, S.H.; Nolte, F.S. Benefits of Adding a Rapid PCR-Based Blood Culture Identification Panel to an Established Antimicrobial Stewardship Program. J. Clin. Microbiol. 2016, 54, 2455–2463. [Google Scholar] [CrossRef] [Green Version]
- Banerjee, R.; Teng, C.B.; Cunningham, S.A.; Ihde, S.M.; Steckelberg, J.M.; Moriarty, J.P.; Shah, N.D.; Mandrekar, J.N.; Patel, R. Randomized Trial of Rapid Multiplex Polymerase Chain Reaction-Based Blood Culture Identification and Susceptibility Testing. Clin. Infect. Dis. 2015, 61, 1071–1080. [Google Scholar] [CrossRef] [Green Version]
- Covert, K.; Bashore, E.; Edds, M.; Lewis, P.O. Utility of the respiratory viral panel as an antimicrobial stewardship tool. J. Clin. Pharm. Ther. 2021, 46, 277–285. [Google Scholar] [CrossRef]
- Weiss, Z.F.; Cunha, C.B.; Chambers, A.B.; Carr, A.V.; Rochat, C.; Raglow-Defranco, M.; Parente, D.M.; Angus, A.; Mermel, L.A.; Sivaprasad, L.; et al. Opportunities Revealed for Antimicrobial Stewardship and Clinical Practice with Implementation of a Rapid Respiratory Multiplex Assay. J. Clin. Microbiol. 2019, 57, e00861-19. [Google Scholar] [CrossRef] [Green Version]
- Schroeder, A.M.; Lewis, S.S.; Sahmoun, A.E.; Beal, J.R. Antibiotic utilization for adult acute respiratory tract infections in United States Emergency Departments. Am. J. Emerg. Med. 2021, 47, 66–69. [Google Scholar] [CrossRef]
- Li, J.; Kang-Birken, S.L.; Mathews, S.K.; Kenner, C.E.; Fitzgibbons, L.N. Role of rapid diagnostics for viral respiratory infections in antibiotic prescribing decision in the emergency department. Infect. Control Hosp. Epidemiol. 2019, 40, 974–978. [Google Scholar] [CrossRef] [PubMed]
- Bizune, D.J.; Palms, D.; King, L.M.; Bartoces, M.; Link-Gelles, R.; Hicks, L.; Fleming-Dutra, K.E. 23. Regional Variation in Outpatient Antibiotic Prescribing in a Commercially-Insured Population, United States, 2017. Open Forum. Infect. Dis. 2020, 7, S12. [Google Scholar] [CrossRef]
- Zhang, Y.; Steinman, M.A.; Kaplan, C.M. Geographic variation in outpatient antibiotic prescribing among older adults. Arch. Intern. Med. 2012, 172, 1465–1471. [Google Scholar] [CrossRef] [PubMed]
- King, L.M.; Kusnetsov, M.; Filippoupolitis, A.; Arik, D.; Bartoces, M.; Roberts, R.M.; Tsay, S.V.; Kabbani, S.; Bizune, D.; Rathore, A.S.; et al. Using machine learning to examine drivers of.f inappropriate outpatient antibiotic prescribing in acute respiratory illnesses. Infect. Control Hosp. Epidemiol. 2022, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Kumar, D.; Ferreira, V.H.; Blumberg, E.; Silveira, F.; Cordero, E.; Perez-Romero, P.; Aydillo, T.; Danziger-Isakov, L.; Limaye, A.P.; Carratala, J.; et al. A 5-Year Prospective Multicenter Evaluation of Influenza Infection in Transplant Recipients. Clin. Infect. Dis. 2018, 67, 1322–1329. [Google Scholar] [CrossRef]
- Hammond, J.; Leister-Tebbe, H.; Gardner, A.; Abreu, P.; Bao, W.; Wisemandle, W.; Baniecki, M.; Hendrick, V.M.; Damle, B.; Simón-Campos, A.; et al. Oral Nirmatrelvir for High-Risk, Nonhospitalized Adults with Covid-19. N. Engl. J. Med. 2022, 386, 1397–1408. [Google Scholar] [CrossRef]
- Jayk Bernal, A.; Gomes da Silva, M.M.; Musungaie, D.B.; Kovalchuk, E.; Gonzalez, A.; Delos Reyes, V.; Martín-Quirós, A.; Caraco, Y.; Williams-Diaz, A.; Brown, M.L.; et al. Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients. N. Engl. J. Med. 2022, 386, 509–520. [Google Scholar] [CrossRef]
- Koonin, L.M.; Patel, A. Timely Antiviral Administration During an Influenza Pandemic: Key Components. Am. J. Public Health 2018, 108, S215–S220. [Google Scholar] [CrossRef]
- Stephenson, J. FDA Authorizes Pharmacists to Prescribe Oral Antiviral Medication for COVID-19. JAMA Health Forum 2022, 3, e222968. [Google Scholar] [CrossRef]
- Bendala Estrada, A.D.; Calderón Parra, J.; Fernández Carracedo, E.; Muiño Míguez, A.; Ramos Martínez, A.; Muñez Rubio, E.; Rubio-Rivas, M.; Agudo, P.; Arnalich Fernández, F.; Estrada Perez, V.; et al. Inadequate use of antibiotics in the covid-19 era: Effectiveness of antibiotic therapy. BMC Infect. Dis. 2021, 21, 1144. [Google Scholar] [CrossRef]
- Rawson, T.M.; Moore, L.S.P.; Zhu, N.; Ranganathan, N.; Skolimowska, K.; Gilchrist, M.; Satta, G.; Cooke, G.; Holmes, A. Bacterial and Fungal Coinfection in Individuals With Coronavirus: A Rapid Review To Support COVID-19 Antimicrobial Prescribing. Clin. Infect. Dis. 2020, 71, 2459–2468. [Google Scholar] [CrossRef] [PubMed]
- Suda, K.J.; Hicks, L.A.; Roberts, R.M.; Hunkler, R.J.; Matusiak, L.M.; Schumock, G.T. Antibiotic Expenditures by Medication, Class, and Healthcare Setting in the United States, 2010–2015. Clin. Infect. Dis. 2018, 66, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Ober, N.S.; Grubmuller, J.; Farrell, M.; Wentworth, C.; Gilbert, T.; Barrett, K.; Davis, S.; Nordman, E.; Grenier, R. System and Method for Generating De-Identified Health Care Data. Patent 6,732,113, 4 May 2004. [Google Scholar]
- Zubeldia, K.; Romney, G.W. Anonymously Linking a Plurality of Data Records. Patent 6,397,224, 28 May 2002. [Google Scholar]
- Fleming-Dutra, K.E.; Hersh, A.L.; Shapiro, D.J.; Bartoces, M.M.; Enns, E.A.; File, T.M., Jr.; Finkelstein, J.A.; Gerber, J.S.; Hyun, D.Y.; Linder, J.A.; et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010–2011. JAMA 2016, 315, 1864–1873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Measures | Overall Cohort n = 9561 |
|---|---|
| Age (years), continuous | |
| Mean (SD) | 36.1 (30.8) |
| Median (Q1, Q3) | 29 (5, 68) |
| Age categories, n (%) | |
| 0–4 | 2150 (22.5) |
| 5–17 | 2182 (22.8) |
| 18–49 | 1308 (13.7) |
| 50–64 | 982 (10.3) |
| 65–74 | 1655 (17.3) |
| ≥75 | 1284 (13.4) |
| Sex, n (%) | |
| Female | 5626 (58.8) |
| Male | 3935 (41.2) |
| Geographic region, n (%) | |
| Northeast | 4125 (43.1) |
| South | 3172 (33.2) |
| West | 1621 (17.0) |
| Midwest | 643 (6.7) |
| Payer type, n (%) | |
| Commercial | 6751 (70.6) |
| Medicare, including Medicare Part D | 2805 (29.3) |
| Medicaid | 5 (0.1) |
| Charlson Comorbidity Index score, n (%) | |
| 0 | 6608 (69.1) |
| 1 | 1561 (16.3) |
| 2 | 750 (7.8) |
| 3 | 270 (2.8) |
| ≥4 | 372 (3.9) |
| Specific comorbidities, n (%) | |
| Chronic pulmonary disease * | 1188 (12.4) |
| Asthma | 854 (8.9) |
| Diabetes (mild to moderate) | 710 (7.4) |
| Diabetes with chronic complications | 374 (3.9) |
| Any malignancy | 410 (4.3) |
| Renal disease | 339 (3.5) |
| Congestive heart failure | 281 (2.9) |
| History of smoking | 252 (2.6) |
| Peripheral vascular disease | 228 (2.4) |
| Cerebrovascular disease | 188 (2.0) |
| Rheumatologic disease | 174 (1.8) |
| Dementia | 70 (0.7) |
| Myocardial infarction | 49 (0.5) |
| HIV/AIDS | 43 (0.4) |
| Metastatic solid tumor | 25 (0.3) |
| Peptic ulcer disease | 25 (0.3) |
| Hemiplegia or paraplegia | 23 (0.2) |
| Moderate or severe liver disease | 14 (0.1) |
| Cystic fibrosis | 10 (0.1) |
| Measures | Overall Cohort n = 9561 |
|---|---|
| Timing of the index date, n (%) | |
| During an influenza season (1 October–31 May) | 8787 (91.9) |
| Outside an influenza season (1 June–30 September) | 774 (8.1) |
| Specific respiratory-related diagnosis code on the index date, n (%) * | |
| Upper respiratory tract infection, unspecified | 2115 (22.1) |
| Influenza | 1790 (18.7) |
| Pharyngitis | 1591 (16.6) |
| Acute bronchitis | 760 (7.9) |
| Sinusitis | 379 (4.0) |
| Pneumonia | 257 (2.7) |
| Acute nasopharyngitis (common cold) | 238 (2.5) |
| Otitis media | 137 (1.4) |
| Tonsillitis | 127 (1.3) |
| Laryngitis/tracheitis | 84 (0.9) |
| No respiratory-related diagnosis on the index date | 3872 (40.5) |
| Respiratory-related diagnosis code tiers on the index date, n (%) | |
| Tier 1 (antibiotics almost always indicated) | 257 (2.7) |
| Tier 2 (antibiotics potentially indicated) | 1984 (20.8) |
| Tier 3 (antibiotics not indicated) | 3448 (36.1) |
| Ordering provider specialty (n, %) | |
| Primary care | 4415 (46.2) |
| Pediatrician | 3312 (34.6) |
| Unspecified/missing | 1197 (12.5) |
| Other specialist | 423 (4.4) |
| Respiratory or infectious disease specialist | 214 (2.2) |
| Results of the index test, n (%) † | |
| Negative for all targets | 5495 (57.5) |
| Positive for influenza | 2153 (22.5) |
| Positive for any non-influenza virus | 1984 (20.8) |
| Co-infected with influenza and non-influenza virus | 71 (0.7) |
| Variables | Overall Cohort |
|---|---|
| n = 9561 | |
| Odds Ratio (95% CI) | |
| Index test result (vs. Positive for influenza only) | |
| Positive for non-influenza target only | 1.28 (1.09, 1.51) * |
| Co-infected with influenza and non-influenza target | 1.15 (0.63, 2.10) |
| Negative for all targets | 1.33 (1.17, 1.50) * |
| Respiratory-related diagnosis code tiers on the index date (vs. Tier 3 [antibiotics not indicated]) | |
| Tier 1 (antibiotics almost always indicated) | 1.70 (1.30, 2.24) * |
| Tier 2 (antibiotics potentially indicated) | 1.50 (1.32, 1.71) * |
| No respiratory-specific diagnosis on the index date | 1.05 (0.94, 1.17) |
| Age group (vs. 18–49) | |
| 0–4 | 0.90 (0.74, 1.10) |
| 5–17 | 0.79 (0.65, 0.96) * |
| 50–64 | 1.27 (1.05, 1.55) * |
| 65–74 | 1.40 (1.14, 1.72) * |
| ≥75 | 1.27 (1.01, 1.59) * |
| Female (vs. Male) | 1.00 (0.91, 1.11) |
| Commercial payer (vs. Medicare or Medicaid) | 0.90 (0.76, 1.06) |
| Geographic region (vs. Northeast) | |
| Midwest | 1.63 (1.34, 1.99) * |
| South | 1.34 (1.20, 1.50) * |
| West | 1.53 (1.34, 1.76) * |
| Prescriber specialty (vs. Primary care) | |
| Pediatrician | 1.05 (0.89, 1.23) |
| Other/missing | 0.94 (0.82, 1.07) |
| CCI score (vs. 0) | |
| 1 | 1.02 (0.89, 1.16) |
| ≥2 | 1.08 (0.93, 1.25) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tse, J.; Near, A.M.; Cheng, M.; Karichu, J.; Lee, B.; Chang, S.N. Outpatient Antibiotic and Antiviral Utilization Patterns in Patients Tested for Respiratory Pathogens in the United States: A Real-World Database Study. Antibiotics 2022, 11, 1058. https://doi.org/10.3390/antibiotics11081058
Tse J, Near AM, Cheng M, Karichu J, Lee B, Chang SN. Outpatient Antibiotic and Antiviral Utilization Patterns in Patients Tested for Respiratory Pathogens in the United States: A Real-World Database Study. Antibiotics. 2022; 11(8):1058. https://doi.org/10.3390/antibiotics11081058
Chicago/Turabian StyleTse, Jenny, Aimee M. Near, Mindy Cheng, James Karichu, Brian Lee, and Susan N. Chang. 2022. "Outpatient Antibiotic and Antiviral Utilization Patterns in Patients Tested for Respiratory Pathogens in the United States: A Real-World Database Study" Antibiotics 11, no. 8: 1058. https://doi.org/10.3390/antibiotics11081058
APA StyleTse, J., Near, A. M., Cheng, M., Karichu, J., Lee, B., & Chang, S. N. (2022). Outpatient Antibiotic and Antiviral Utilization Patterns in Patients Tested for Respiratory Pathogens in the United States: A Real-World Database Study. Antibiotics, 11(8), 1058. https://doi.org/10.3390/antibiotics11081058






