Synthesis and Biological Evaluation of Novel Fusidic Acid Derivatives as Two-in-One Agent with Potent Antibacterial and Anti-Inflammatory Activity
Abstract
1. Introduction
2. Results and Discussion
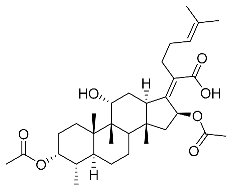
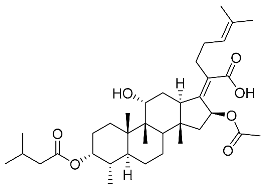
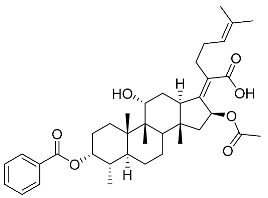
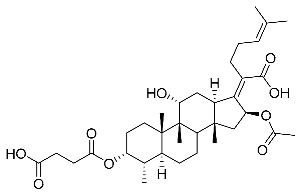
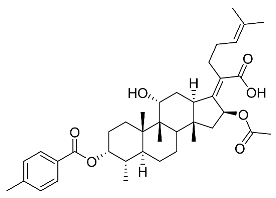
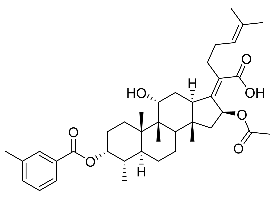
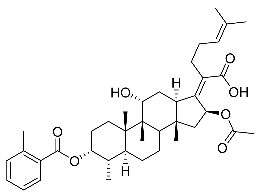
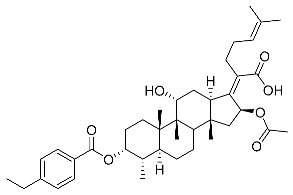
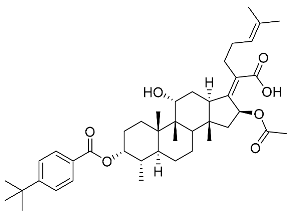
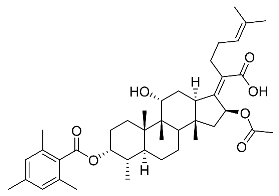
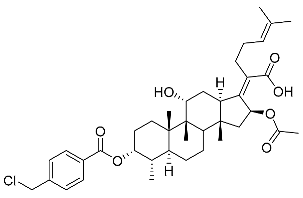
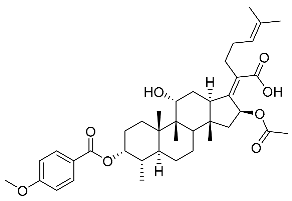
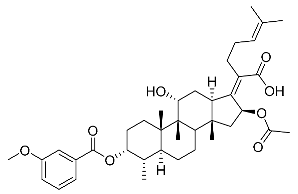
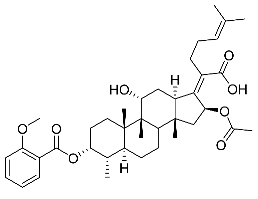
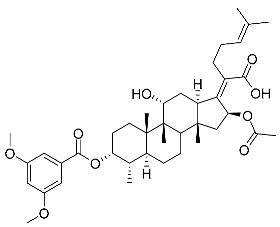
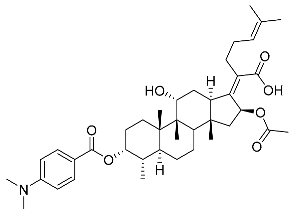
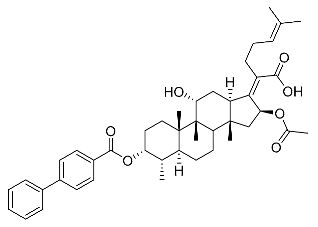
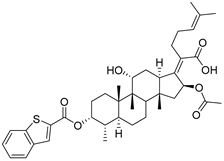
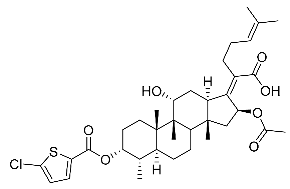
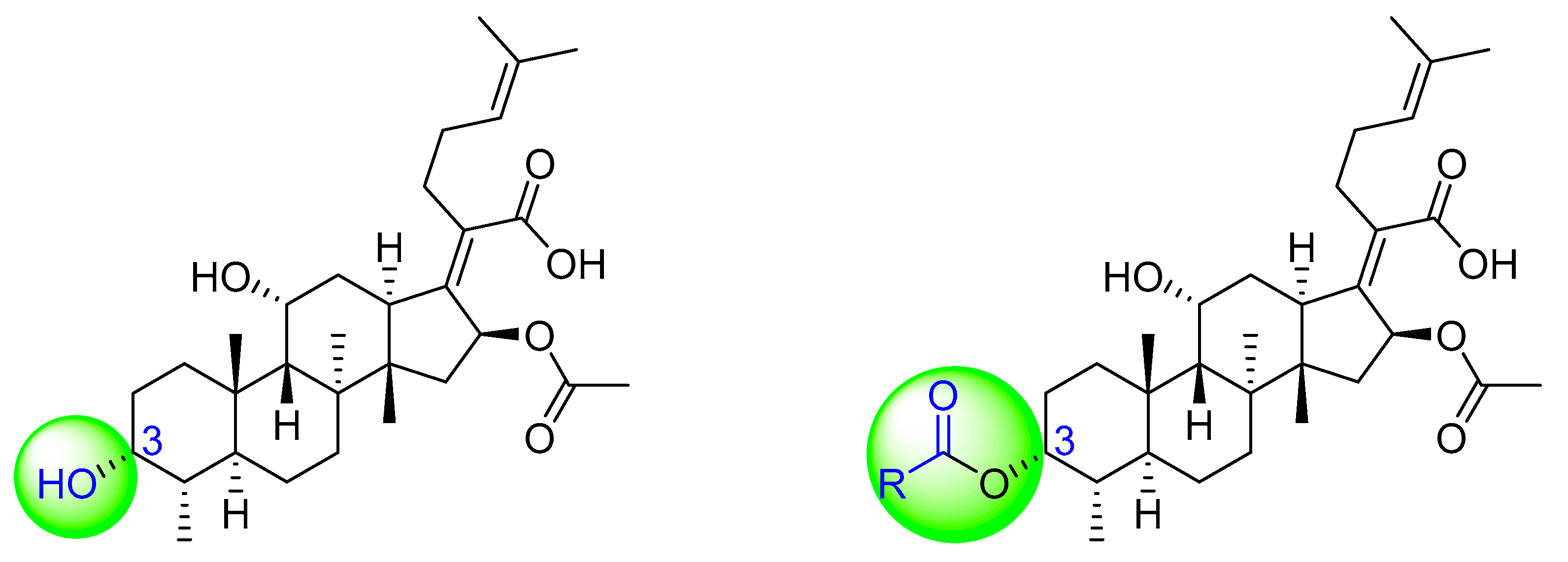
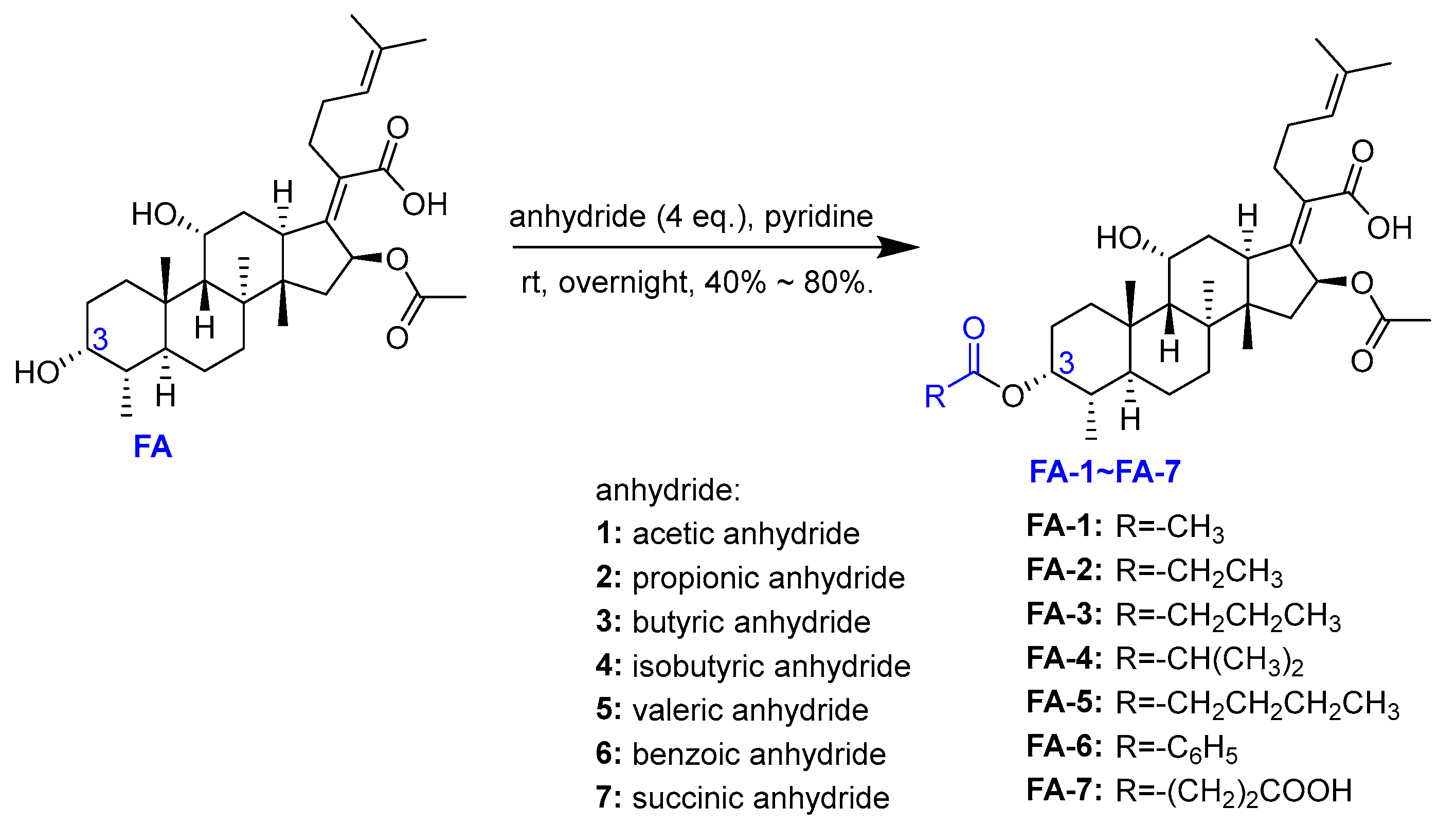
2.1. Chemistry
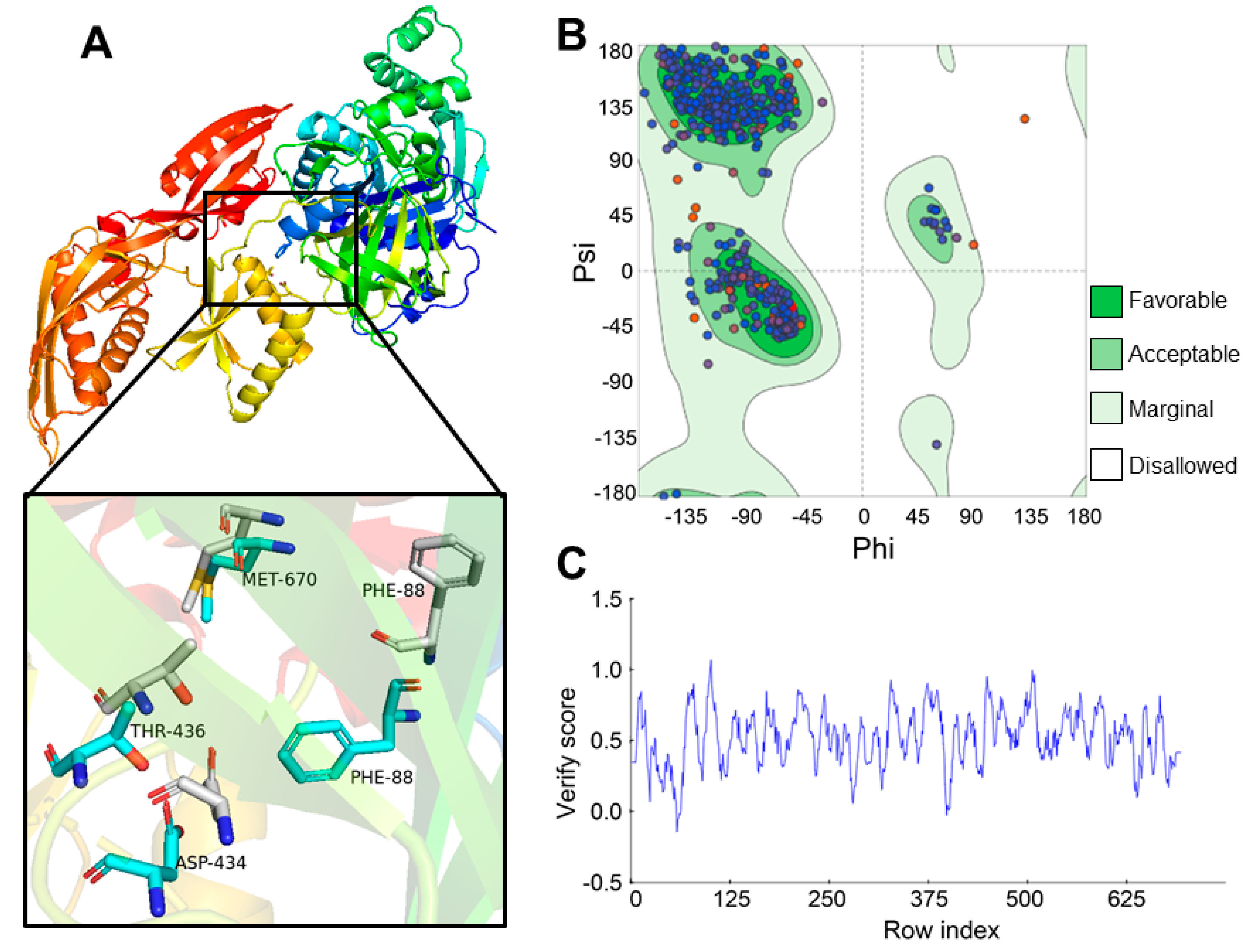
2.2. Antibacterial Activity
2.2.1. Agar Disk Diffusion Assay
2.2.2. The Minimum Inhibitory Concentration (MIC) Assay
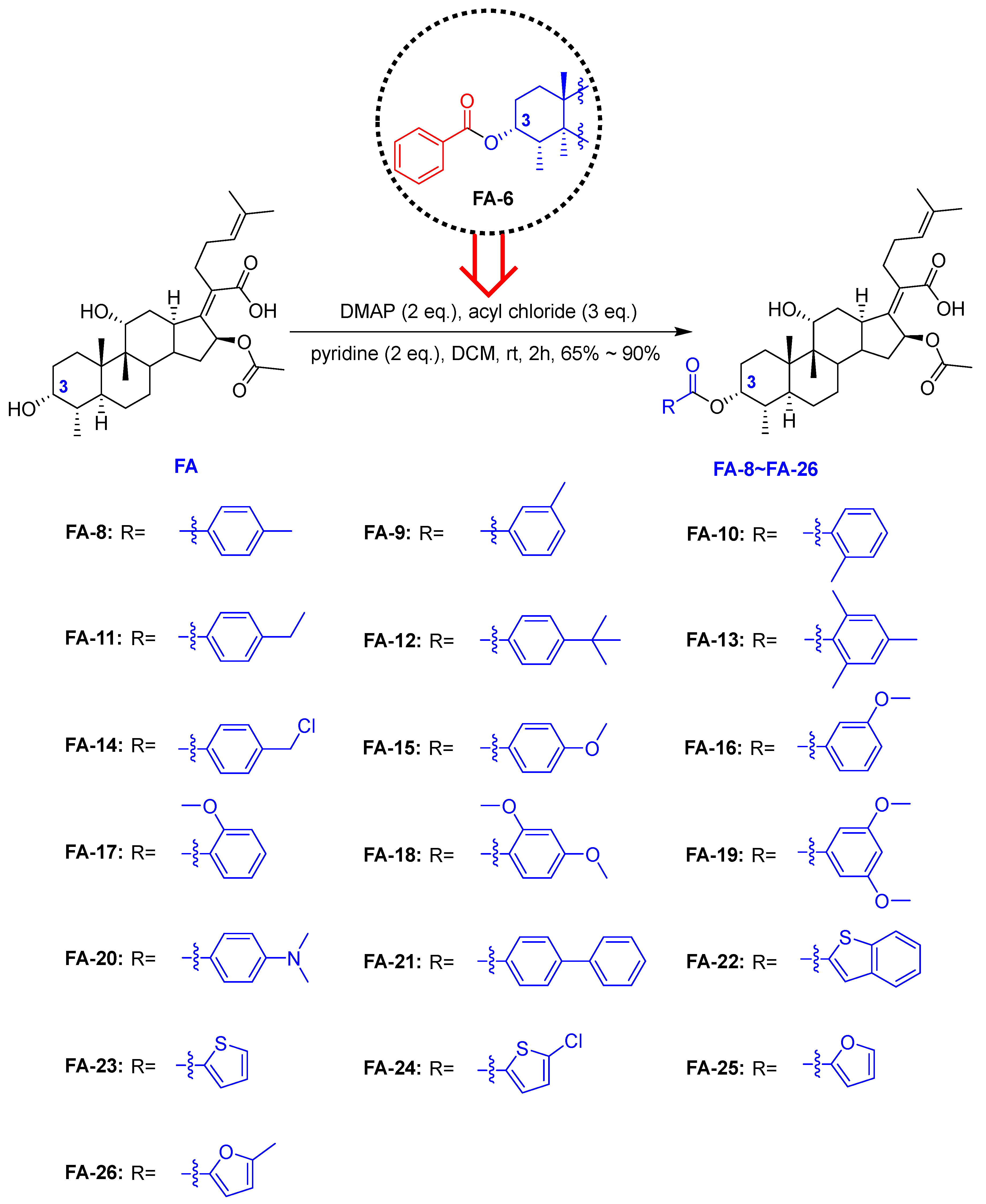
2.2.3. Growth Kinetics Assay
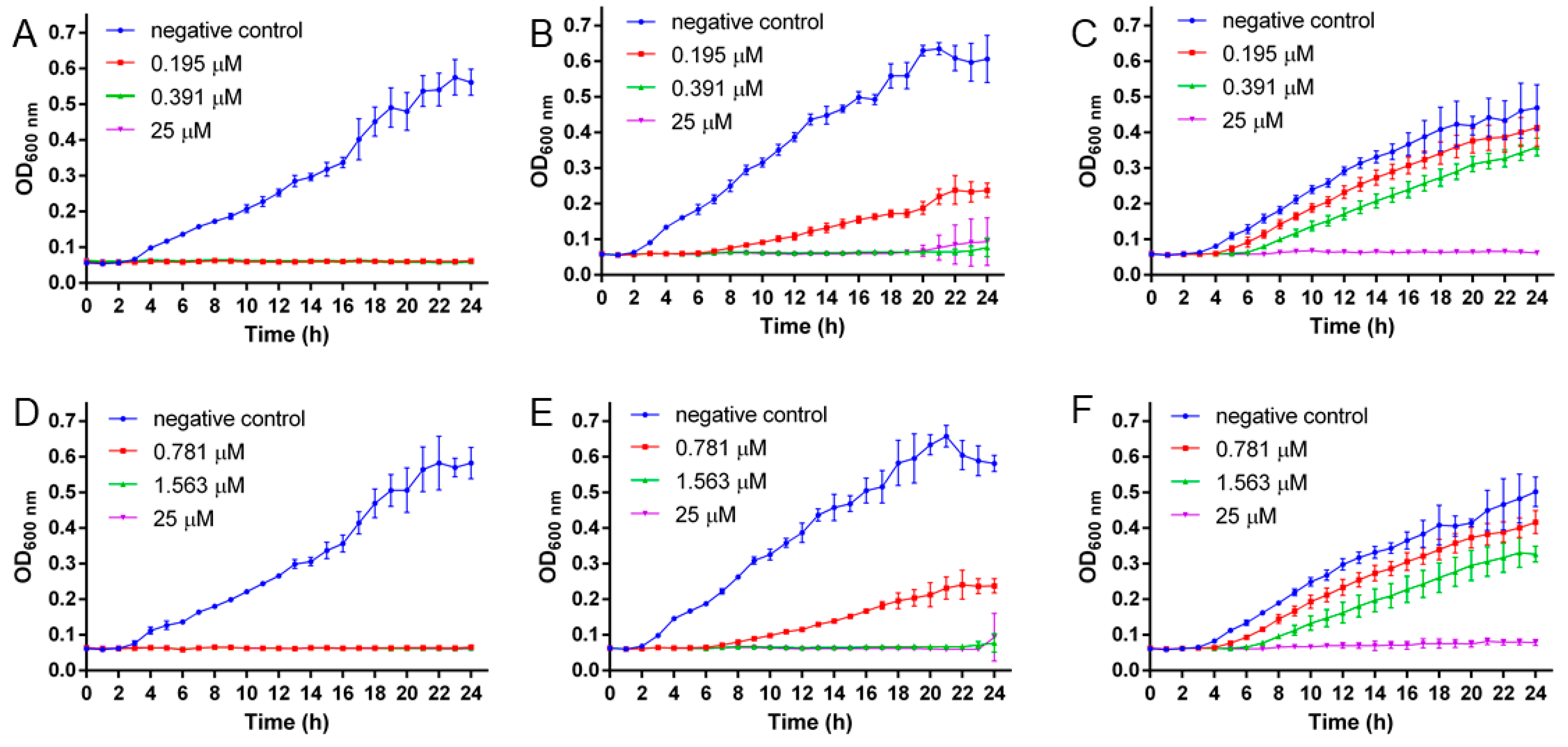
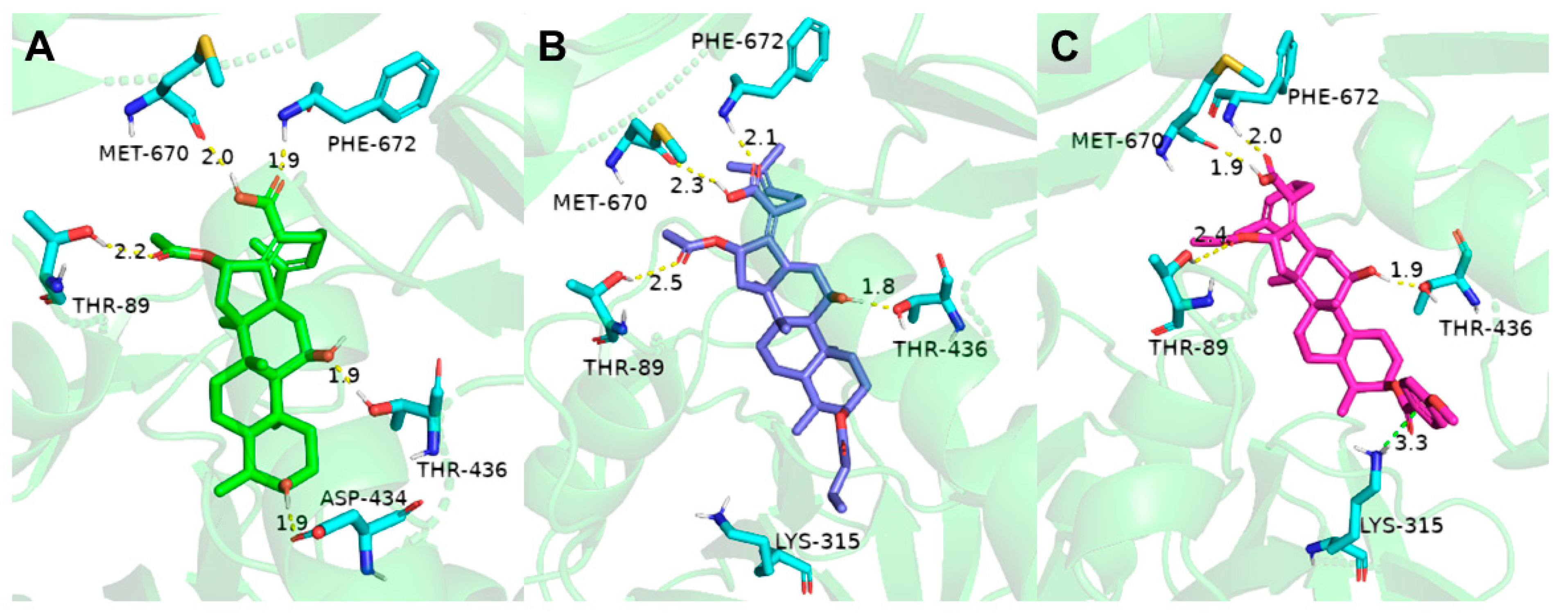
2.3. Molecular Docking
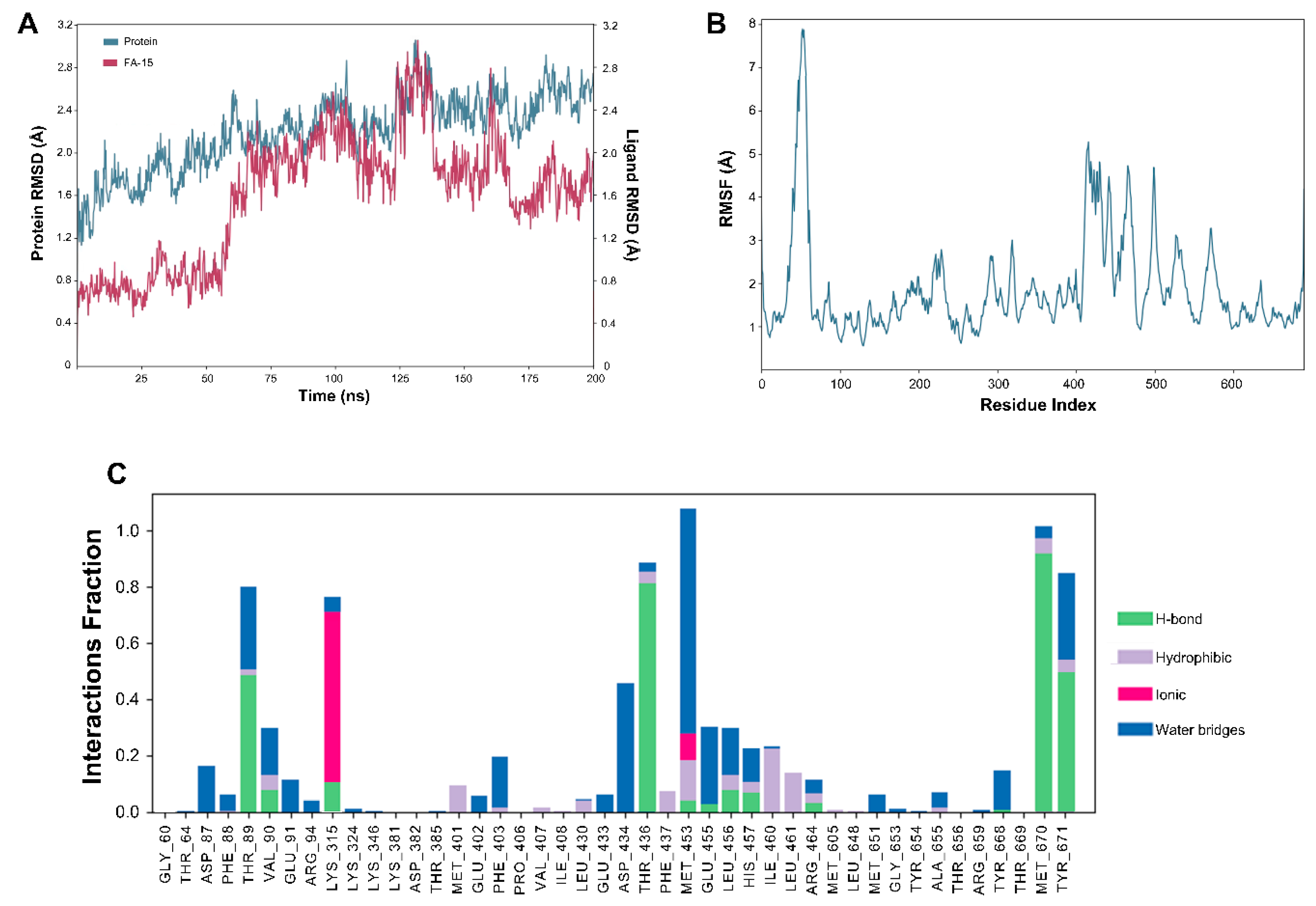
2.4. Molecular Dynamics (MD) Dimulation
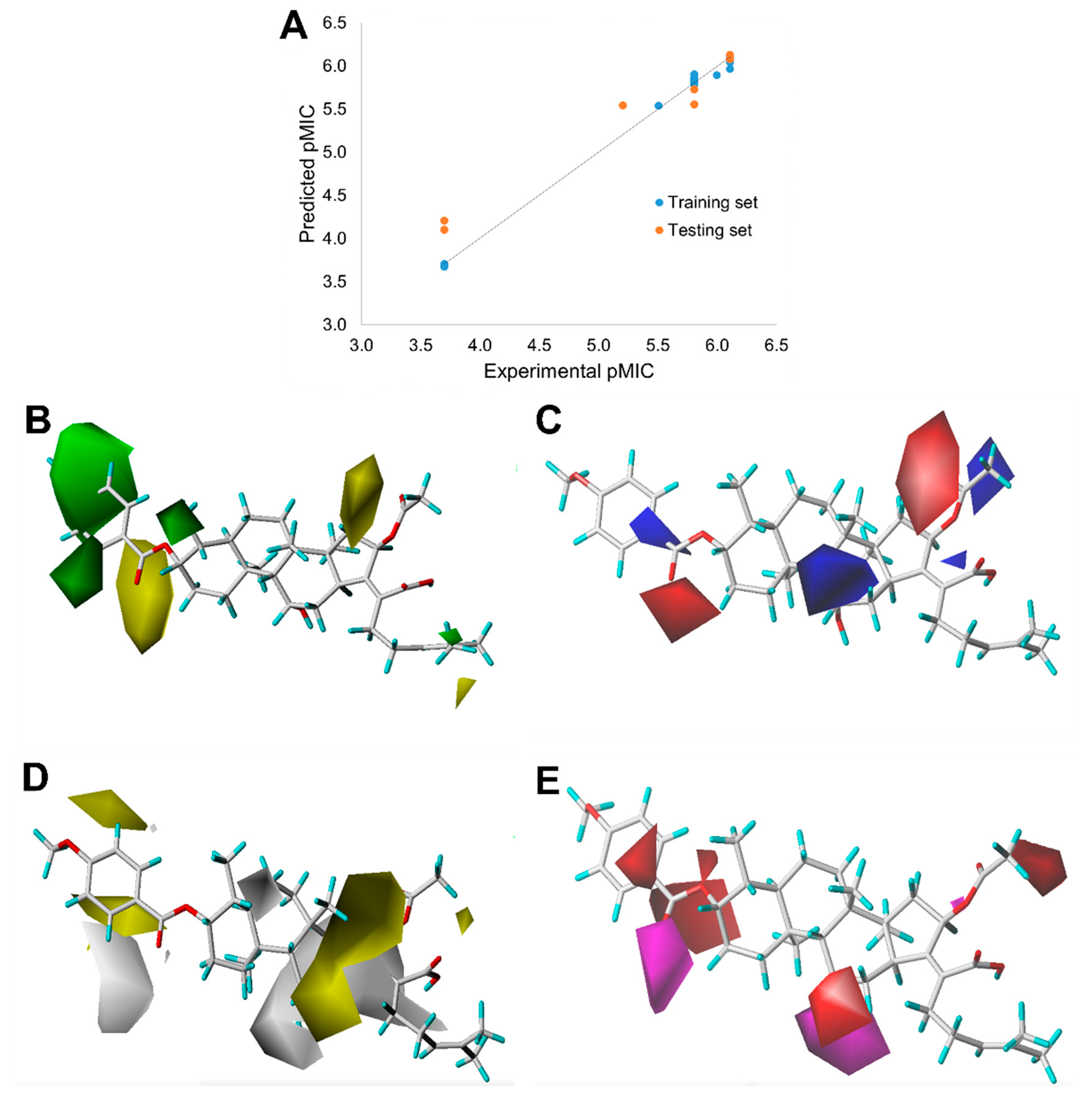
2.5. Quantitative Structure–Activity Relationship (QSAR)
2.6. In Vivo Anti-Inflammation Studies
3. Conclusions
4. Materials and Methods
4.1. Materials
4.2. Chemistry







4.3. Antibacterial Activity
4.3.1. Agar Disk Diffusion Method
4.3.2. The Minimum Inhibitory Concentration (MIC)
4.3.3. Growth Kinetics Assay
4.4. In Vivo Anti-Inflammation Studies
4.5. Homology Modeling
4.6. Molecular Docking
4.7. MD
4.8. QSAR
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lowy, F.D. Staphylococcus aureus infections. N. Engl. J. Med. 1998, 339, 520–532. [Google Scholar] [CrossRef] [PubMed]
- Patil, A.; Nandi, S.; Kale, N.; Bobade, C.; Banerjee, S.; Patil, Y.; Khandare, J. Designing 3D-nanosubstrates mimicking biological cell growth: Pitfalls osing 2D substrates in thvaluation of anticancefficiency. Nanoscale 2021, 13, 17473–17485. [Google Scholar] [CrossRef] [PubMed]
- Stryjewski, M.E.; Chambers, H.F. Skin and soft-tissue infections caused by community-acquired methicillin-resistant Staphylococcus aureus. Clin. Infect. Dis. 2008, 46, S368–S377. [Google Scholar] [CrossRef] [PubMed]
- Lakhundi, S.; Zhang, K. Methicillin-resistant Staphylococcus aureus: Molecular characterization, evolution, and epidemiology. Clin. Microbiol. Rev. 2018, 31, e00020-18. [Google Scholar] [CrossRef] [PubMed]
- Barber, M.; Rozwadowska-Dowzenko, M. Infection by penicillin resistant Staphylococci. Lancet 1948, 252, 641–644. [Google Scholar] [CrossRef]
- Finland, M. Emergence of antibiotic-resistant bacteria. N. Engl. J. Med. 1955, 253, 1019–1028. [Google Scholar] [CrossRef]
- Turnidge, J.; Lawson, P.; Munro, R.; Benn, R. A national survey of antimicrobial resistance in Staphylococcus aureus in Australian teaching hospitals. Med. J. Aust. 1989, 150, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, R.P.; Nettleman, M.D.; Jones, R.N.; Pfaller, M.A. Methicillin-resistant Staphylococcus aureus: Implications for the 1990s and effective control measures. Am. J. Med. 1991, 91, S221–S227. [Google Scholar] [CrossRef]
- Hiramatsu, K.; Hanaki, H.; Ino, T.; Yabuta, K.; Oguri, T.; Tenover, F.C. Methicillin-resistant Staphylococcus aureus clinical strain with reduced vancomycin susceptibility. J. Antimicrob. Chemother. 1997, 40, 135–136. [Google Scholar] [CrossRef]
- Godtfredsen, W.O.; Jahnsen, S.; Lorck, H.; Roholt, K.; Tybring, L. Fusidic acid: A new antibiotic. Nature 1962, 193, 987. [Google Scholar] [CrossRef]
- Pfaller, M.A.; Castanheira, M.; Sader, H.S.; Jones, R.N. Evaluation of the activity of fusidic acid tested against contemporary Gram-positive clinical isolates from the USA and Canada. Int. J. Antimicrob. Agents 2010, 35, 282–287. [Google Scholar] [CrossRef] [PubMed]
- McLaws, F.B.; Larsen, A.R.; Skov, R.L.; Chopra, I.; Neill, A.J. Distribution of fusidic acid resistanceterminants in methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2011, 55, 1173. [Google Scholar] [CrossRef] [PubMed]
- Bodley, J.W.; Zieve, F.J.; Lin, L.; Zieve, S.T. Formation of the ribosome-G factor-GDP complex in the presence of fusidic acid. Biochem. Biophys. Res. Commun. 1969, 37, 437–443. [Google Scholar] [CrossRef]
- Tanaka, N.; Kinoshita, T.; Masukawa, H. Mechanism of protein synthesis inhibition by fusidic acid and related antibiotics. Biochem. Biophys. Res. Commun. 1968, 30, 278–283. [Google Scholar] [CrossRef]
- Seo, H.-S.; Abedin, S.; Kamp, D.; Wilson, D.N.; Nierhaus, K.H.; Cooperman, B.S. EF-G-dependent GTPase on the ribosome. Conformational change and fusidic acid inhibition. Biochemistry 2006, 45, 2504–2514. [Google Scholar] [CrossRef] [PubMed]
- Cox, G.; Thompson, G.S.; Jenkins, H.T.; Peske, F.; Savelsbergh, A.; Rodnina, M.V.; Wintermeyer, W.; Homans, S.W.; Edwards, T.A.; Neill, A.J. Ribosome clearancy FusB-type proteins mediates resistance to the antibiotic fusidic acid. Proc. Natl. Acad. Sci. USA 2012, 109, 2102. [Google Scholar] [CrossRef] [PubMed]
- Godtfredsen, W.O.; Albrethsen, C.; von Daehne, W.; Tybring, L.; Vangedal, S. Transformations of fusidic acid and the relationship between structure and antibacterial activity. Antimicrob. Agents Chemother. 1965, 5, 132–137. [Google Scholar] [PubMed]
- Bucki, R.; Leszczynska, K.; Byfield, F.J.; Fein, D.E.; Won, E.; Cruz, K.; Namiot, A.; Kulakowska, A.; Namiot, Z.; Savage, P.B.; et al. Combined antibacterial and anti-inflammatory activity of a cationic disubstituted dexamethasone-spermine conjugate. Antimicrob Agents Chemother. 2010, 54, 2525–2533. [Google Scholar] [CrossRef]
- Wu, P.P.; He, H.; Hong, W.D.; Wu, T.R.; Huang, G.Y.; Zhong, Y.Y.; Tu, B.R.; Gao, M.; Zhou, J.; Zhao, S.Q.; et al. Thiological evaluation of fusidic acid and its hydrogenation derivative as antimicrobial and anti-inflammatory agents. Infect. Drug Resist. 2018, 11, 1945–1957. [Google Scholar] [CrossRef]
- Rautio, J.; Kumpulainen, H.; Heimbach, T.; Oliyai, R.; Oh, D.; Jarvinen, T.; Savolainen, J. Prodrugs: Design and clinical applications. Nat. Rev. Drug Discov. 2008, 7, 255–270. [Google Scholar] [CrossRef]
- Godtfredsen, W.O.; von Daehne, W.; Tybring, L.; Vangedal, S. Fusidic acid derivatives. I. Relationship between structure and antibacterial activity. J. Med. Chem. 1966, 9, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Riber, D.; Venkataramana, M.; Sanyal, S.; Duvold, T. Synthesis and biological evaluation of photoaffinity labeled fusidic acid analogues. J. Med. Chem. 2006, 49, 1503–1505. [Google Scholar] [CrossRef] [PubMed]
- Kong, F.-D.; Huang, X.-L.; Ma, Q.-Y.; Xie, Q.-Y.; Wang, P.; Chen, P.-W.; Zhou, L.-M.; Yuan, J.-Z.; Dai, H.-F.; Luo, D.-Q.; et al. Helvolic acid derivatives with antibacterial activities against Streptococcus agalactiae from the marine-derived fungus aspergillus fumigatus HNMF0047. J. Nat. Prod. 2018, 81, 1869–1876. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.-M.; Hu, D.; Gao, H.; Kushiro, T.; Awakawa, T.; Chen, G.-D.; Wang, C.-X.; Abe, I.; Yao, X.-S. Biosynthesis of helvolic acid and identification of an unusual C-4-demethylation procesistinct from sterol biosynthesis. Nat. Commun. 2017, 8, 1644. [Google Scholar] [CrossRef]
- Singh, K.; Kaur, G.; Shanika, P.S.; Dziwornu, G.A.; Okombo, J.; Chibale, K. Structure-activity relationship analyses of fusidic acid derivatives highlight crucial role of the C-21 carboxylic acid moiety to its anti-mycobacterial activity. Biorg. Med. Chem. 2020, 28, 115530. [Google Scholar] [CrossRef]
- Salimova, E.V.; Mamaev, A.G.; Tret’yakova, E.V.; Kukovinets, O.S.; Mavzyutov, A.R.; Shvets, K.Y.; Parfenova, L.V. Synthesis and Biological Activity of Cyanoethyl Derivatives of Fusidic Acid. Russ. J. Org. Chem. 2018, 54, 1411–1418. [Google Scholar] [CrossRef]
- Chouaïb, K.; Hichri, F.; Nguir, A.; Daami-Remadi, M.; Elie, N.; Touboul, D.; Ben Jannet, H.; Hamza, M.A. Semi-synthesis of new antimicrobial esters from the natural oleanolic and maslinic acids. Food Chem. 2015, 183, 8–17. [Google Scholar] [CrossRef]
- Gualtieri, M.; Bastide, L.; Villain-Guillot, P.; Michaux-Charachon, S.; Latouche, J.; Leonetti, J.P. In vitro activity of a new antibacterial rhodaninerivative against Staphylococcus pidermidiiofilms. J. Antimicrob. Chemother. 2006, 58, 778–783. [Google Scholar] [CrossRef]
- Sato, T.; Kawai, Y.; Matsuda, H.; Tateda, K.; Kimura, S.; Ishii, Y.; Yamaguchi, K.; Gotoh, N. In vitro and in vivo antibacterial activity of modithromycin against streptococci and Haemophilus influenzae. J. Antimicrob. Chemother. 2011, 66, 1547–1554. [Google Scholar] [CrossRef][Green Version]
- Haste, N.M.; Farnaes, L.; Perera, V.R.; Fenical, W.; Nizet, V.; Hensler, M.E. Bactericidal kinetics of marine-derived napyradiomycins against contemporary methicillin-resistant Staphylococcus aureus. Mar. Drugs 2011, 9, 680–689. [Google Scholar] [CrossRef]
- Kaur, G.; Singh, K.; Pavadai, E.; Njoroge, M.; Espinoza-Moraga, M.; De Kock, C.; Smith, P.J.; Wittlin, S.; Chibale, K. Synthesis of fusidic acid bioisosteres as antiplasmodial agents and moleculaocking studies in thinding site olongation factor-G. MedChemComm 2015, 6, 2023–2028. [Google Scholar] [CrossRef]
- Besier, S.; Ludwig, A.; Brade, V.; Wichelhaus, T.A. Molecular analysis of fusidic acid resistance in Staphylococcus aureus. Moleculaicrobiology 2003, 47, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Koripella, R.K.; Sanyal, S.; Selmer, M. Staphylococcus aureulongation factor G–structure and analysis of a target for fusidic acid. FEBS J. 2010, 277, 3789–3803. [Google Scholar] [CrossRef] [PubMed]
- Lu, J.; Ni, J.-X.; Wang, J.-A.; Liu, Z.-Y.; Shang, K.-L.; Bi, Y. Integration of multiscale molecular modeling approaches with thesign and discovery of fusidic acid derivatives. Future Med. Chem. 2019, 11, 1427–1442. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Liu, B.; Zhang, Y.; Wang, J.; Lu, Y.; Deng, J.; Wang, S. Application of CdTe/CdS/ZnS quantum dot in immunoassay for aflatoxin B1 and molecular modeling of antibody recognition. Anal. Chim. Acta 2019, 1047, 139–149. [Google Scholar] [CrossRef]
- Gao, Y.-G.; Selmer, M.; Dunham, C.M.; Weixlbaumer, A.; Kelley, A.C.; Ramakrishnan, V. The Structure of the Ribosome with Elongation Factor G Trapped in thosttranslocational State. Science 2009, 326, 694. [Google Scholar] [CrossRef] [PubMed]
- Zicheng, L.; Jing, Y.; Quan, D.; Xingjun, J.; Yuanyuan, Z.; Hao, Z.; Changrong, P.; Xueding, W.; Weiqing, Y.; Min, M. Synthesis and Quantitative Structure-activity Relationships Study for Arylpropenamide Derivatives as Inhibitors of Hepatitis B Virus Replication. Chem. Biol. Drug Des. 2016, 88, 451–459. [Google Scholar]
- Liu, W.; Li, Y.; Yue, Y.; Zhang, K.; Chen, Q.; Wang, H.; Lu, Y.; Huang, M.T.; Zheng, X.; Du, Z. Synthesis and biological evaluation of curcumin derivatives containing NSAIDs for their anti-inflammatory activity. Bioorg. Med. Chem. Lett. 2015, 25, 3044–3051. [Google Scholar] [CrossRef]
- Yetkin, E.; Ozturk, S.; Yetkin, I.G. Inflammation in coronary artery ectasia compared to atherosclerosis. Int. J. Oolecular Sci. 2018, 19, 2971. [Google Scholar] [CrossRef]
- Dar, B.A.; Lone, A.M.; Shah, W.A.; Qurishi, M.A. Synthesis and screening orsolic acid-benzylidinerivatives as potential anti-cancer agents. Eur. J. Med. Chem. 2016, 111, 26–32. [Google Scholar] [CrossRef]
- Wu, P.-P.; Zhang, B.-J.; Cui, X.-P.; Yang, Y.; Jiang, Z.-Y.; Zhou, Z.-H.; Zhong, Y.-Y.; Mai, Y.-Y.; Ouyang, Z.; Chen, H.-S.; et al. Synthesis and biological evaluation of novel ursolic acid analogues as potential α-glucosidase inhibitors. Sci. Rep. 2017, 7, 45578. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Wang, S.; Zhang, Q.; Chang, C.W.; Zhan, J. Three new fusidic acid derivatives and their antibacterial activity. Bioorganic Med. Chem. Lett. 2015, 25, 1920–1924. [Google Scholar] [CrossRef] [PubMed]
- Ulvatne, L.H.V.H. Bactericidal kinetics of 3 lactoferricins against Staphylococcus aureus and Escherichia coli. Scand. J. Infect. Dis. 2001, 33, 507–511. [Google Scholar]
- Pohlman, J.K.; Knapp, C.C.; Ludwig, M.D.; Washington, J.A. Timed killing kinetic studies of the interaction between ciprofloxacin and β-lactams against gram-negativacilli. Diagn. Microbiol. Infect. Dis. 1996, 26, 29–33. [Google Scholar] [CrossRef]
- Arhin, F.F.; McKay, G.A.; Beaulieu, S.; Sarmiento, I.; Parr, T.R.; Moeck, G. Time–kill kinetics of oritavancin and comparator agents against Streptococcus pyogenes. Int. J. Antimicrob. Agents 2009, 34, 550–554. [Google Scholar] [CrossRef]
- Momiyama, Y.; Adachi, H.; Fairweather, D.; Ishizaka, N.; Saita, E. Inflammation, atherosclerosis and coronary artery disease. Clin. Med. Insights Cardiol. 2014, 8, CMC.S39423. [Google Scholar] [CrossRef]
- Kuo, D.H.; Lai, Y.S.; Lo, C.Y.; Cheng, A.C.; Wu, H.; Pan, M.H. Inhibitory effect of magnolol on TPA-induced skin inflammation and tumor promotion in mice. J. Agric. Food. Chem. 2010, 58, 5777–5783. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Li, Y.; Zheng, X.; Zhang, K.; Du, Z. Potent inhibitory effect of silibinin from milk thistle on skin inflammation stimuli by 12-O-tetradecanoylphorbol-13-acetate. Food Funct. 2015, 6, 3712–3719. [Google Scholar] [CrossRef] [PubMed]
- Leong, H.N.; Kurup, A.; Tan, M.Y.; Kwa, A.L.H.; Liau, K.H.; Wilcox, M.H. Management of complicated skin and soft tissue infections with a special focus on the role of newer antibiotics. Infect. Drug Resist. 2018, 11, 1959–1974. [Google Scholar] [CrossRef]
- Abraham, M.J.; Murtola, T.; Schulz, R.; Páll, S.; Smith, J.C.; Hess, B.; Lindahl, E. GROMACS: High performance molecular simulations through multi-level parallelism from laptops to supercomputers. SoftwareX 2015, 1–2, 19–25. [Google Scholar] [CrossRef]
- Anand, K.; Palm, G.J.; Mesters, J.R.; Siddell, S.G.; Ziebuhr, J.; Hilgenfeld, R. Structure of coronavirus main proteinase reveals combination of a chymotrypsin fold with an extra alpha-helical domain. EMBO J. 2002, 21, 3213–3224. [Google Scholar] [CrossRef]
| Compound (Dosage = 0.16 nmol) | ZOIs (mm) | ||||
|---|---|---|---|---|---|
| S. aureus a | S. albu b | S. epidermidis c | E. coli d | S. typhimurium e | |
| FA | 20.31 ± 0.34 f | 19.43 ± 0.42 f | 19.91 ± 0.20 f | <6 | <6 |
| FA-1 | <6 | <6 | <6 | <6 | <6 |
| FA-2 | <6 | <6 | <6 | <6 | <6 |
| FA-3 | <6 | <6 | <6 | <6 | <6 |
| FA-4 | <6 | <6 | <6 | <6 | <6 |
| FA-5 | <6 | <6 | <6 | <6 | <6 |
| FA-6 | 19.01 ± 0.77 f | 19.39 ± 0.51 f | 16.41 ± 0.81 f | <6 | <6 |
| FA-7 | <6 | <6 | <6 | <6 | <6 |
| FA-8 | 19.57 ± 0.31 f | 19.49 ± 0.44 f | 21.04 ± 0.27 f | <6 | <6 |
| FA-9 | 20.52 ± 0.47 f | 18.79 ± 0.41 f | 18.26 ± 0.23 f | <6 | <6 |
| FA-10 | 20.39 ± 0.35 f | 18.77 ± 0.19 f | 20.67 ± 0.54 f | <6 | <6 |
| FA-11 | 21.15 ± 0.39 f | 19.87 ± 0.40 f | 20.79 ± 0.33 f | <6 | <6 |
| FA-12 | 19.44 ± 0.37 f | 20.88 ± 0.31 f | 17.44 ± 0.41 f | <6 | <6 |
| FA-13 | 13.61 ± 0.30 f | 14.48 ± 0.38 f | 11.69 ± 0.40 f | <6 | <6 |
| FA-14 | 20.88 ± 0.66 f | 19.97 ± 0.49 f | 20.30 ± 0.28 f | <6 | <6 |
| FA-15 | 20.27 ± 0.44 f | 21.73 ± 0.22 f | 20.66 ± 0.52 f | <6 | <6 |
| FA-16 | 20.23 ± 0.37 f | 19.57 ± 0.14 f | 20.69 ± 0.53 f | <6 | <6 |
| FA-17 | 19.01 ± 0.21 f | 19.95 ± 0.42 f | 19.07 ± 0.45 f | <6 | <6 |
| FA-18 | 20.47 ± 0.20 f | 19.85 ± 0.86 f | 21.38 ± 0.63 f | <6 | <6 |
| FA-19 | 17.95 ± 0.31 f | 19.35 ± 0.28 f | 18.68 ± 0.48 f | <6 | <6 |
| FA-20 | 17.71 ± 0.43 f | 18.15 ± 0.24 f | 18.67 ± 0.56 f | <6 | <6 |
| FA-21 | 19.53 ± 0.27 f | 20.33 ± 0.42 f | 20.79 ± 0.33 f | <6 | <6 |
| FA-22 | 20.65 ± 0.44 f | 20.81 ± 0.35 f | 20.27 ± 0.36 f | <6 | <6 |
| FA-23 | 20.05 ± 0.24 f | 19.42 ± 0.59 f | 19.47 ± 0.22 f | <6 | <6 |
| FA-24 | 20.89 ± 0.41 f | 19.91 ± 0.18 f | 21.34 ± 0.39 f | <6 | <6 |
| FA-25 | 20.12 ± 0.10 f | 20.52 ± 0.81 f | 18.26 ± 0.02 f | <6 | <6 |
| FA-26 | 18.33 ± 0.43 f | 20.37 ± 0.24 f | 18.79 ± 0.69 f | <6 | <6 |
| Compound | MIC (µM) | ||
|---|---|---|---|
| S. aureus a | S. albu b | S. epidermidis c | |
| FA | 0.194 | 0.391 | 0.625 |
| FA-1 | ≥200 | ≥200 | ≥200 |
| FA-2 | ≥200 | ≥200 | ≥200 |
| FA-3 | ≥200 | ≥200 | ≥200 |
| FA-4 | ≥200 | ≥200 | ≥200 |
| FA-5 | ≥200 | ≥200 | ≥200 |
| FA-6 | 1.563 | 3.125 | 3.125 |
| FA-7 | ≥200 | ≥200 | ≥200 |
| FA-8 | 1.563 | 1.563 | 3.125 |
| FA-9 | 1.563 | 1.563 | 3.125 |
| FA-10 | 1.563 | 3.125 | 1.563 |
| FA-11 | 0.781 | 1.563 | 3.125 |
| FA-12 | 0.781 | 1.563 | 3.125 |
| FA-13 | 6.250 | 6.250 | 6.250 |
| FA-14 | 1.563 | 1.563 | 1.563 |
| FA-15 | 0.781 | 1.563 | 1.563 |
| FA-16 | 0.781 | 1.563 | 1.563 |
| FA-17 | 0.781 | 1.563 | 1.563 |
| FA-18 | 1.563 | 3.125 | 3.125 |
| FA-19 | 1.563 | 1.563 | 1.563 |
| FA-20 | 1.563 | 3.125 | 1.563 |
| FA-21 | 0.781 | 1.563 | 1.563 |
| FA-22 | 1.563 | 1.563 | 1.563 |
| FA-23 | 1.563 | 1.563 | 1.563 |
| FA-24 | 0.781 | 1.563 | 1.563 |
| FA-25 | 1.563 | 3.125 | 3.125 |
| FA-26 | 1.563 | 1.563 | 1.563 |
| Compound | 9 mm Diameter Right Mouse Ear | |||
|---|---|---|---|---|
| Net Weight (mg) | Swelling Degree (mg) | Swelling Rate (%) | IR (%) | |
| Blank | 8.85 ± 0.35 a | 1.15 ± 0.35 a | NT | NT |
| TPA | 23.0 ± 0.99 | 13.5 ± 1.27 | 260.32% ± 21.59% | NT |
| FA (2 μg/μL) | 17.2 ± 0.42 a | 8.55 ± 0.21 b | 194.60% ± 12.57% | 36.46% ± 4.42% |
| FA (4 μg/μL) | 16.15 ± 0.78 a | 7.55 ± 0.92 b | 182.81% ± 16.09% | 44.15% ± 1.54% |
| FA (8 μg/μL) | 15.35 ± 0.35 a | 6.75 ± 0.35 a | 173.66% ± 10.93% | 49.90% ± 2.10% |
| FA-15 (2 μg/μL) | 19.3 ± 1.13 c | 10.3 ± 0.85 c | 218.00% ± 4.07% | 23.07% ± 13.54% |
| FA-15 (4 μg/μL) | 17.0 ± 0.85 a | 8.0 ± 1.13 b | 192.05% ± 1.92% | 40.08% ± 14.03% |
| FA-15 (8 μg/μL) | 14.3 ± 0.42 a | 5.3 ± 0.00 a | 161.81% ± 11.26% | 60.57% ± 3.72% |
| Dexamethasone (2.5 μg/μL) | 10.65 ± 0.07 a | 1.95 ± 0.35 a | 120.42% ± 4.01% | 85.37% ± 4.00% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tu, B.; Cao, N.; Zhang, B.; Zheng, W.; Li, J.; Tang, X.; Su, K.; Li, J.; Zhang, Z.; Yan, Z.; et al. Synthesis and Biological Evaluation of Novel Fusidic Acid Derivatives as Two-in-One Agent with Potent Antibacterial and Anti-Inflammatory Activity. Antibiotics 2022, 11, 1026. https://doi.org/10.3390/antibiotics11081026
Tu B, Cao N, Zhang B, Zheng W, Li J, Tang X, Su K, Li J, Zhang Z, Yan Z, et al. Synthesis and Biological Evaluation of Novel Fusidic Acid Derivatives as Two-in-One Agent with Potent Antibacterial and Anti-Inflammatory Activity. Antibiotics. 2022; 11(8):1026. https://doi.org/10.3390/antibiotics11081026
Chicago/Turabian StyleTu, Borong, Nana Cao, Bingjie Zhang, Wende Zheng, Jiahao Li, Xiaowen Tang, Kaize Su, Jinxuan Li, Zhen Zhang, Zhenping Yan, and et al. 2022. "Synthesis and Biological Evaluation of Novel Fusidic Acid Derivatives as Two-in-One Agent with Potent Antibacterial and Anti-Inflammatory Activity" Antibiotics 11, no. 8: 1026. https://doi.org/10.3390/antibiotics11081026
APA StyleTu, B., Cao, N., Zhang, B., Zheng, W., Li, J., Tang, X., Su, K., Li, J., Zhang, Z., Yan, Z., Li, D., Zheng, X., Zhang, K., Hong, W. D., & Wu, P. (2022). Synthesis and Biological Evaluation of Novel Fusidic Acid Derivatives as Two-in-One Agent with Potent Antibacterial and Anti-Inflammatory Activity. Antibiotics, 11(8), 1026. https://doi.org/10.3390/antibiotics11081026






