Abstract
Background: Antibiotic resistance is one of the most pressing public health problems. Health authorities, patients, and health professionals, including dentists, are all involved in its development. COVID-19 pandemic restrictions on dental care may have had repercussions on antibiotic prescribing by dentists. The aim of this study was to assess the impact of the COVID-19 pandemic on antibiotic prescribing by dentists, and to review antibiotic consumption according to the WHO Access, Watch, Reserve classification. We conducted a natural, before-and-after, quasi-experimental study, using antibiotic prescription data covering the period from January 2017 to May 2021. A segmented regression analysis with interrupted time series data was used to analyse the differences between the numbers of defined daily doses (DDD) of antibiotics prescribed monthly. The outcomes showed an immediate significant decrease in overall antibiotic prescribing by primary-care dentists during lockdown, followed by a non-significant upward trend for the next year. This same pattern was, likewise, observed for Access and Watch antibiotics. COVID-19 pandemic restrictions on dental care influenced the prescription of antibiotics. During confinement, an initial decrease was observed, this trend changed when in person consultations were recovered. It might be beneficial to analyse the prescription of antibiotics using the WHO AWaRe classification, in order to monitor their appropriate use.
1. Introduction
Antibiotic resistance is one of the most pressing public health problems worldwide due to its impact on mortality, morbidity, and healthcare costs [1]. The excessive and inappropriate use of antibiotics contributes a great deal to this problem. Health authorities, patients, and health professionals are all involved in this misuse [2]. Dentists prescribe 10% of all antibiotics consumed [3,4] and it is estimated that, from this, only 30% are correctly prescribed [5,6], since in dentistry most of the processes can be resolved by local treatments, and antibiotics would only be indicated on limited occasions [7].
The COVID-19 pandemic has had repercussions on dental care, due to the risk of cross-contamination in dental clinics due to the characteristics of dental procedures, during which aerosols are generated, and due to the close proximity of the professional to the patient [8]. During the first months of the pandemic in Spain, medical care was dispensed by means of telephone consultations in which the professional decided whether a physical medical visit was necessary [9]. In patients with symptoms compatible with COVID-19 or suspicion of infection, and with pain or inflammation of dental origin, the visit had to be postponed for a minimum of two weeks, during which time dental professionals had to resort to pharmacological treatment with antibiotics and/or analgesics [10]. This telephone-based care, coupled with the initial difficulty of obtaining personal protective equipment, and the fear felt by professionals and patients alike of contracting the disease during treatment, may well have served to increase the number of antibiotic prescriptions issued without an accurate diagnosis of infection, since it is extremely complicated to make a differential diagnosis based exclusively on information provided by the patient [9,11,12,13].
Currently, the impact of the COVID-19 pandemic on the short-term prescribing of antibiotics is unknown. Hence, the principal aim of this study was to assess the impact of the pandemic on antibiotic prescribing by dentists whose practices come within the Spanish National Health System (NHS) in north-west Spain; the secondary aim was to try to assess the impact of COVID-19 on the prescribing of those antibiotic groups that are most closely related with the development of antibiotic resistance.
2. Results
2.1. Antibiotic Prescribing by the WHO AWaRe Classification
Primary-care dentists prescribed a mean of 35344 DDD of antibiotics before confinement, approximately 6% of which belonged to the Watch group, as shown in Table 1. No antibiotic was prescribed in the Reserve group. The mean DDD values of Access and Watch group antibiotics were similar before, during, and after confinement. Amoxicillin, amoxicillin combined with clavulanic acid, azithromycin, and clindamycin were the antibiotics most used by dentists. Azithromycin, belonging to the Watch group, was the third most prescribed antibiotic (Table S1).

Table 1.
Antibiotic consumption before, during and after lockdown [14].
2.2. Impact of the COVID-19 Pandemic on Antibiotic Prescribing
The monthly antibiotic prescribing trend from January 2017 to May 2021 for primary-care dentists is shown in Figure 1 and Table 2. As can be seen, after seasonal adjustment, there were changes in the antibiotic prescribing trend prior to the outbreak of the pandemic (B = −42.39). On the emergence of COVID-19, a significant decrease in antibiotic prescribing (B = −3572.73; p < 0.005) was observed during lockdown (equivalent to a decrease of 8.92% (95% CI: −3.80%; 14.13%)), followed by an immediate non-significant decrease (B = −1363.82) with respect to the pre-pandemic period, and a subsequent upward trend in the long term (B = 142.74).
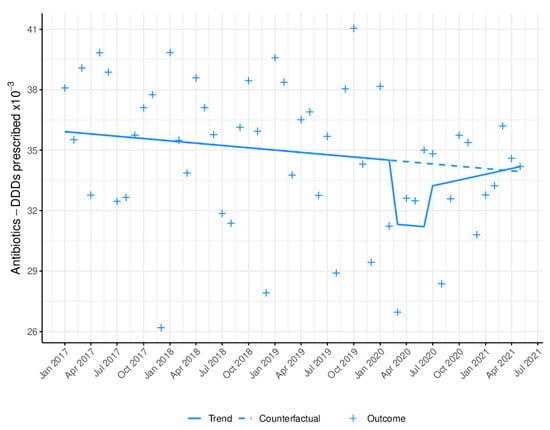
Figure 1.
Monthly antibiotic prescribing trend in defined daily doses (DDD). Blue line (−): trend, after model adjustment; blue dashed line: expected trend with no COVID-19 outbreak; +: monthly antibiotic prescribing in DDD.

Table 2.
Segmented regression analysis of interrupted time series data on antibiotic prescribing [14].
2.3. Impact of the COVID-19 Pandemic on the WHO Access Group
Figure 2 depicts the monthly prescribing trend in DDD among primary-care dentists for the group of antibiotics listed as Access by the WHO. Table 2 shows a statistically significant reduction (B = −2976.50, p = 0.0133) in antibiotic prescribing during lockdown (8.00% (95% CI: 2.68%; 13.46%) decrease) followed by an immediate non-significant reduction in prescribing (B = −991.28) and a non-significant upward trend in the long term (B = 136.05).
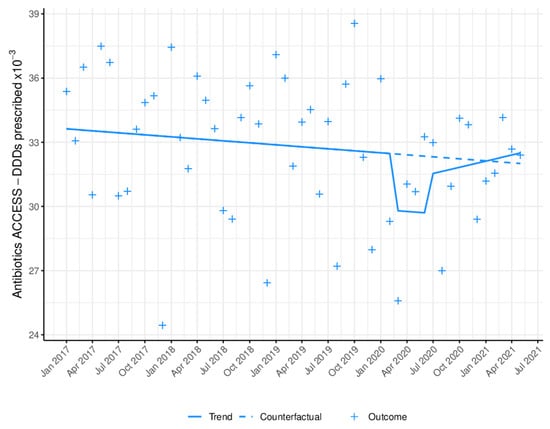
Figure 2.
Monthly WHO Access antibiotic prescribing trend in defined daily doses (DDD). Blue line (−): trend after model adjustment; blue dashed line: expected trend with no COVID-19 outbreak; +: monthly antibiotic prescriptions in DDD.
2.4. Impact of the COVID-19 Pandemic on the WHO Watch Group
Figure 3 depicts the monthly prescribing trend in DDD of Watch antibiotics. During lockdown, a statistically significant reduction (B = −651.02; p < 0.0001) in antibiotic prescribing was observed (decrease of 20.16% (95% CI: 14.05%; 26.26%)). Whereas the emergence of COVID-19 had a significant impact (B = −688.91) on the trend, with a reduction in prescribing (p = 0.0002); in the long-term, a non-significant increase was evident (B = 29.15).
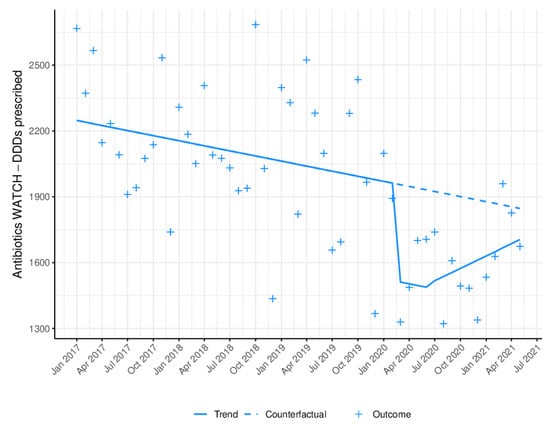
Figure 3.
Monthly WHO Watch antibiotic prescribing trend in defined daily doses (DDD). Blue line (−): trend, after model adjustment; blue dashed line: expected trend with no COVID-19 outbreak; +: monthly antibiotic prescriptions in DDD.
3. Discussion
The data yielded by this quasi-experimental study indicate that the COVID-19 pandemic had an important impact on antibiotic prescribing by NHS dentists in north-west Spain. In March 2020, coinciding with the Spanish Government’s declaration of a state of alarm and confinement, a significant decrease was observed in monthly antibiotic prescriptions, which was maintained during lockdown and followed by an upward trend across the following year. This pattern was, likewise, generally observed for antibiotics and for those in the Access and Watch groups, with 8.92%, 8.00%, and 20.16% respectively.
The initial decrease observed may be a consequence of the measures adopted during the first phase of confinement, in which care was dispensed by telephone consultation and, in rare cases, in person [9]. Hence, the suspension of non-urgent surgical treatments (such as extractions of asymptomatic teeth) may have led to a decrease in the prescribing of antibiotics associated with these types of procedures, and of Watch-type antibiotics in particular [15,16,17]. Patients’ fear of visiting dental clinics due to the risk of becoming infected with COVID-19, the smaller number of emergencies, and the increase in self-medication could also account for this initial decrease [18,19,20].
The sharp drop observed during confinement is consistent with that found in Australia [21], and contrary to that reported in the United Kingdom [22,23], where prescriptions were observed to increase after the onset of the pandemic. This may be due to differences in the clinical practice guidelines of these countries [24]: in the case of the United Kingdom, the fact that prophylactic treatment against infective endocarditis is not envisaged [25] indicates that lockdown could have increased antibiotic prescriptions in an attempt to delay dental care in non-urgent treatments [26]. However, in countries where prophylaxis with antibiotics is standard practice, the limiting of medical visits during lockdown also limited the prescribing of antibiotics as prophylaxis.
The increase observed after confinement can be attributed to the delay in treatment arising from confinement (owing to the lack of in-person care and/or patient fear) [27,28] which, due to the inherent progression of untreated processes, led to more severe clinical profiles [29]. This effect was also observed in other diseases (cancers, cardiovascular diseases, diabetes) [30,31,32].
Before the pandemic, a downward trend was observed in antibiotic prescribing by this group of professionals, similar to that reported by studies undertaken elsewhere [33] and the trend at a national level in Spain [34,35].
Amoxicillin is the leading antibiotic used by primary-care dentists, a finding in line with the results of other studies [33,35,36,37]. We detected that amoxicillin with clavulanic acid is the second leading antibiotic, ranking almost as high as amoxicillin prescribed alone, even though it is not the antibiotic of choice in most clinical guidelines [38,39,40]. Azithromycin ranks third in the prescribing order, despite being an antibiotic in the Watch group [14] and its use should be limited, due to the greater risk of the appearance of antibiotic resistance. The use of antibiotics such as clindamycin has been associated with an increased risk of C difficile infections. Some studies indicate that approximately 15% of community C difficile infections may be caused by odontogenic antibiotic prescribing [41]. Other macrolides, such as azithromycin or clarithromycin have been associated with a higher frequency of adverse reactions [42]. The use of WATCH-type antibiotics as well as other antibiotics, such as clindamycin, should be avoided because of their impact on antimicrobial resistance [14]. These findings are especially interesting, in that they could be the target for interventions that aim to improve dental prescribing.
We found no study that assessed the impact of the pandemic on antibiotic prescribing by dentists according to the classification proposed by the WHO, nor any study that applied this classification to analysing prescriptions in this field. This prevents us from comparing our results to those of previous studies and would indicate that this classification should also be used in studies on dentists.
Strengths and Weaknesses of the Study
The principal advantage of this study is the methodology used. The ITS design makes it possible to analyse the impact of the COVID-19 pandemic on antibiotic prescribing [43,44].
By way of limitations, the nature of the study per se should be mentioned. The model used assumes a linear trend in the outcome, and this assumption may only hold over short intervals. Furthermore, the introduction of data broken down by month means that neither individual changes nor the impact of the pandemic on specific days (at the beginning or end of lockdown) can be shown. The study was carried out in one region of Spain; therefore, this geographical limitation could compromise the generalizability. Another study limitation lies in the fact that we do not know whether the initial decrease in the number of prescriptions might have been linked to an increase in the DDD of antibiotics prescribed by dentists working in the private sector or in hospital emergency services. Another study limitation is that the DDD of antibiotics are not correlated to the numbers of in-person consultations and telephone consultations during the pandemic.
Lastly, it should be stressed that the type of data analysed do not record the reason for prescribing, which means that our design does not allow for the appropriateness of prescriptions to be assessed. Thus, there is a need for further studies that would enable long-term changes in trend to be analysed.
The results of this study demonstrate the usefulness of using the WATCH classification to monitor appropriate antibiotic prescribing. These results could be disseminated through specific educational interventions for dentists to raise awareness for the prudent use of antibiotics.
4. Materials and Methods
4.1. Settings
Galicia is a region situated in the north of Spain, with an area of 29,434 km2 and a population of 2.7 million. Healthcare for close to 100% of the population is covered by the Galician Health Service (Servizo Galego de Saúde/SERGAS). Dentistry forms part of primary care, with services including the examination of the oral cavity, treatment of acute processes and dental emergencies, oral surgeries, and preventative treatments. For the remaining dental procedures, such as root canal work or prosthetic rehabilitation, patients have to use a network of private clinics, which also provide the range of treatment offered by SERGAS dentists. This study was conducted using antibiotic prescription data relating to the dentists, some 100 in all, who work at SERGAS primary care buccodental health units [45]. In Spain, medications are dispensed at pharmacies and, in the case of antibiotics, are only available on prescriptions issued by dentists among other health professionals.
4.2. Study Design and Data Collection
We used a natural, before-and-after, quasi-experimental design, with monthly data for the period from January 2017 to May 2021. This design, which enables causal effects to be estimated after controlling for baseline levels and trends [46], is suitable for assessing the impact of the pandemic and confinement, since these are time-delimited interventions, and the longitudinal nature of the data provide the analysis with a special robustness [47,48].
The drug class targeted by this paper comprises antibacterials for systemic use (Anatomical Therapeutic Chemical code J01) [49], prescribed in outpatient settings by dentists in the public health sector.
4.3. Data Source
For study purposes, antibiotic prescription data were obtained from the SERGAS Pharmacy Information System for Complex Pharmacy Service Analyses (Sistema Corporativo de Información de Análisis Complejos Prestación Farmacéutica). This shows all medications dispensed by community pharmacies in the health area, based on official prescriptions billed to the Public Health Service. Data from primary-care dentists were selected. There was no change in the system across the study period.
4.4. Definition of Variables
We calculated the number of monthly defined daily doses (DDD), defined as the average maintenance dose per day for a drug for its main indication [50].
The World Health Organisation (WHO) suggests the use of the Access, Watch, Reserve (AWaRe) classification issued in 2019 and updated in 2021, for an improved evaluation and monitoring use of antibiotics. This tool makes it possible to reduce antibiotic resistance and access to all medicines [14]. The Watch group includes 110 first- or second-choice antibiotics that display a higher resistance potential when compared with the Access group, and thus should be strictly monitored and restricted to the limited indications, as well as prioritised as major targets for stewardship programs.
4.5. Statistical Analysis
An interrupted time series (ITS) analysis model based on a segmented regression approach [44,51,52,53] was purpose-designed to analyse the differences between monthly prescribed DDD of antibiotics [44]. This design allows for effects to be estimated by controlling for baseline levels and trends [46]. A segmented linear regression analysis model [47] was designed to analyse the differences observed from January 2017 to May 2021 in terms of prescribed antibiotics. The independent variables were defined as: time (t:1, 2, 3, 53); a binary variable (COVID) taking values of “0” before June 2020, and “1” after July 2020, corresponding to the time in which the effect of the pandemic was measured; a binary variable (lockdown) taking values of “1” in the months of lockdown (March 2020 to June 2020), and “0” in the other months; a variable for the time elapsed since the first COVID-19 case, which took the value of “0” before; and the values of “1”, “2”, “3”, corresponding to the months from July 2020 to May 2021. To identify possible seasonal changes in antibiotic prescribing, the X-13ARIMA-SEATS procedure was applied [53]. This method is an adaptation of the US Census Bureau X-13–Auto-Regressive Integrated Moving Average (ARIMA) model which produces a seasonally-adjusted time series. The Cumby-Huizinga test was used to check for autocorrelation (10 autocorrelation lags were tested). Based on the results of these tests, lags of the dependent variable were introduced to correct for autocorrelation. The relative changes due to immediate impact and their 95% CI were calculated according to the Boostrap methods described by Zhang [54]. A total of 10,000 replicates were simulated.
All analyses were performed using the free R statistical software environment (version 4.0.5) [55], except for the Cumby–Huizinga test, which was carried out with Stata version 12 [56].
5. Conclusions
The COVID-19 pandemic led to a decrease in antibiotic prescribing by primary-care dentists during the initial months, followed by an upward trend. This change was likewise observed for Access and Watch antibiotics. Due to the high percentage of antibiotic prescriptions issued by these professionals, it may well be of interest if future studies that analysed antibiotic prescribing among dentists were to use the WHO AWaRe classification.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/antibiotics11081018/s1, Table S1: Defined daily dose by active ingredient as prescribed by primary-care dentists, according to the AWaRe Classification [49].
Author Contributions
Conceptualization, A.F. and M.Z.-C.; Data curation, A.R.-F., O.V.-C., M.P.-L., A.F. and M.Z.-C.; Formal analysis, A.R.-F., M.P.-L., A.F. and M.Z.-C.; Funding acquisition, A.F. and M.Z.-C.; Investigation, A.R.-F., O.V.-C., M.P.-L., A.F. and M.Z.-C.; Methodology, O.V.-C., M.P.-L., A.F. and M.Z.-C.; Project administration, A.F. and M.Z.-C.; Resources, A.R.-F., O.V.-C., M.P.-L., A.F. and M.Z.-C.; Software, A.R.-F., O.V.-C., M.P.-L., A.F. and M.Z.-C.; Supervision, M.P.-L., A.F. and M.Z.-C.; Validation, A.R.-F., O.V.-C., M.P.-L., A.F. and M.Z.-C.; Visualization, A.R.-F., O.V.-C., M.P.-L., A.F. and M.Z.-C.; Writing—original draft, A.R.-F., O.V.-C., M.P.-L., A.F. and M.Z.-C.; Writing—review & editing, A.R.-F., O.V.-C., M.P.-L., A.F. and M.Z.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This study has been funded by the Instituto de Salud Carlos III (ISCIII) through the project PI19/01006, co-financed by FEDER, European Union.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
We would like to thank the Subdirectorate-General for Pharmacology of the Galician Regional Authority (Xunta de Galicia) for furnishing the prescription data needed to conduct this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization—WHO. Antibiotic Resistance. Available online: https://www.who.int/news-room/factsheets/detail/antimicrobial-resistance (accessed on 13 February 2022).
- Ferri, M.; Ranucci, E.; Romagnoli, P.; Giaccone, V. Antimicrobial resistance: A global emerging threat to public health systems. Crit. Rev. Food Sci. Nutr. 2017, 57, 2857–2876. [Google Scholar] [CrossRef] [PubMed]
- Bunce, J.T.; Hellyer, P. Antibiotic resistance and antibiotic prescribing by dentists in England 2007–2016. Br. Dent. J. 2018, 225, 81–84. [Google Scholar] [CrossRef]
- Marra, F.; George, D.; Chong, M.; Sutherland, S.; Patrick, D.M. Antibiotic prescribing by dentists has increased Why? J. Am. Dent. Assoc. 2016, 147, 320–327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chate, R.A.C.; White, S.; Hale, L.R.; Howat, A.P.; Bottomley, J.; Barnet-Lamb, J.; Lindsay, J.; Davies, T.I.; Heath, J.M. The impact of clinical audit on antibiotic prescribing in general dental practice. Br. Dent. J. 2006, 201, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Chopra, R.; Merali, R.; Paolinelis, G.; Kwok, J. An audit of antimicrobial prescribing in an acute dental care department. Prim. Dent. J. 2014, 3, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Swift, J.Q.; Gulden, W.S. Antibiotic therapy--managing odontogenic infections. Dent. Clin. Am. 2002, 46, 623–633. [Google Scholar] [CrossRef]
- Meng, L.; Hua, F.; Bian, Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J. Dent Res. 2020, 99, 481–487. [Google Scholar] [CrossRef] [Green Version]
- Trullols-Casas, M.C.; Ausina-Márquez, V.; Martínez-Beneyto, Y. Recommendations by the Spanish Society of Epidemiology and Oral Public Health (SESPO) for the healthcare adaptation of public health dental clinics in Spain during the COVID-19 pandemic. J. Clin. Exp. Dent. 2020, 12, e1183–e1188. [Google Scholar] [CrossRef]
- Ather, A.; Patel, B.; Ruparel, N.B.; Diogenes, A.; Hargreaves, K.M. Coronavirus Disease 19 (COVID-19): Implications for clinical dental care. J. Endod. 2020, 46, 584–595. [Google Scholar] [CrossRef]
- Ather, A.; Patel, B.; Ruparel, N.B.; Diogenes, A.; Hargreaves, K.M. Perceived vulnerability to Coronavirus infection: Impact on dental practice. Braz. Oral Res. 2020, 34, 584–595. [Google Scholar]
- Estai, M.; Bunt, S.; Kanagasingam, Y.; Kruger, E.; Tennant, M. Diagnostic accuracy of teledentistry in the detection of dental caries: A systematic review. J. Evid. Based Dent. Pract. 2016, 16, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Campus, G.; Betancourt, M.D.; Cagetti, M.; Giacaman, R.; Manton, D.; Douglas, G.; Carvalho, T.; Carvalho, J.; Vukovic, A.; Cortés-Martinicorena, F.; et al. The COVID-19 pandemic and its global effects on dental practice. An International survey. J. Dent. 2021, 114, 103749. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization-WHO—Home AWaRe. Available online: https://adoptaware.org/ (accessed on 13 February 2022).
- Posse, J.L.; Álvarez-Fernández, M.; Feijoo, J.F.; Henríquez, J.M.; Lockhart, P.B.; Chu, V.H.; Dios, P.D. Intravenous amoxicillin/clavulanate for the prevention of bacteraemia following dental procedures: A randomized clinical trial. J. Antimicrob. Chemother. 2016, 71, 2022–2030. [Google Scholar] [CrossRef] [PubMed]
- Lafaurie, G.I.; Noriega, L.A.; Torres, C.C.; Castillo, Y.; Moscoso, S.B.; Mosquera, S.; Díaz-Báez, D.; Chambrone, L. Impact of antibiotic prophylaxis on the incidence, nature, magnitude, and duration of bacteremia associated with dental procedures: A systematic review. J. Am. Dent. Assoc. 2019, 150, 948–959.e4. [Google Scholar] [CrossRef] [PubMed]
- Diz Dios, P.; Tomás Carmona, I.; Limeres Posse, J.; Medina Henríquez, J.; Fernández Feijoo, J.; Alvarez Fernández, M. Comparative efficacies of amoxicillin, clindamycin, and moxifloxacin in prevention of bacteremia following dental extractions. Antimicrob. Agents Chemother. 2006, 50, 2996–3002. [Google Scholar] [CrossRef] [Green Version]
- González-Olmo, M.J.; Delgado-Ramos, B.; Ortega-Martínez, A.R.; Romero-Maroto, M.; Carrillo-Díaz, M. Fear of COVID-19 in Madrid. Will patients avoid dental care? Int. Dent. J. 2021, 72, 76–82. [Google Scholar] [CrossRef]
- Salgarello, S.; Salvadori, M.; Mazzoleni, F.; Salvalai, V.; Francinelli, J.; Bertoletti, P.; Lorenzi, D.; Audino, E.; Garo, M.L. Urgent Dental Care During Italian Lockdown: A Cross-sectional Survey. J. Endod. 2021, 47, 204–214. [Google Scholar] [CrossRef]
- Ramírez, J.M.; Varela-Montes, L.; Gómez-Costa, D.; Giovannini, G.; Romero-Maroto, M.; Gómez de Diego, R. Management of odonto-stomatological emergencies during the COVID-19 alarm state in dental clinics in the Autonomous Community of Madrid (CAM), Spain: An observational study. Med. Oral Patol. Oral Cir. Bucal 2021, 26, e114–e117. [Google Scholar] [CrossRef] [PubMed]
- Mian, M.; Teoh, L.; Hopcraft, M. Trends in dental medication prescribing in australia during the COVID-19 pandemic. JDR Clin. Trans. Res. 2021, 6, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.; Wordley, V.; Thompson, W. How did COVID-19 impact on dental antibiotic prescribing across England? Br. Dent. J. 2020, 229, 601–604. [Google Scholar] [CrossRef]
- Duncan, E.M.; Goulao, B.; Clarkson, J.; Young, L.; Ramsay, C.R. “You had to do something”: Prescribing antibiotics in Scotland during the COVID-19 pandemic restrictions and remobilisation. Br. Dent. J. 2021, 23, 1–6. [Google Scholar] [CrossRef]
- Thornhill, M.H.; Dayer, M.; Lockhart, P.B.; McGurk, M.; Shanson, D.; Prendergast, B.; Chambers, J.B. Guidelines on prophylaxis to prevent infective endocarditis. Br. Dent. J. 2016, 220, 51–56. [Google Scholar] [CrossRef] [Green Version]
- Centre for Clinical Practice at NICE (UK). Prophylaxis against Infective Endocarditis Antimicrobial Prophylaxis against Infective Endocarditis in Adults and Children; National Institute for Health and Clinical Excellence: London, UK, 2008. [Google Scholar]
- Palmer, N.O.A.; Seoudi, N. The effect of SARS-CoV-2 on the prescribing of antimicrobials and analgesics by NHS general dental practitioners in England. Br. Dent. J. 2021, 21, 1–6. [Google Scholar] [CrossRef]
- Sari, A.; Bilmez, Z.Y. Effects of Coronavirus (COVID-19) Fear on Oral Health Status. Oral Health Prev. Dent. 2021, 19, 411–423. [Google Scholar]
- Samuel, S.R.; Kuduruthullah, S.; Khair, A.M.B.; Al Shayeb, M.; Elkaseh, A.; Varma, S.R.; Nadeem, G.; Elkhader, I.A.; Ashekhi, A. Impact of pain, psychological-distress, SARS-CoV2 fear on adults’ OHRQOL during COVID-19 pandemic. Saudi J. Biol. Sci. 2021, 28, 492–494. [Google Scholar] [CrossRef]
- Pitts, N.B.; Zero, D.T.; Marsh, P.D.; Ekstrand, K.; Weintraub, J.A.; Ramos-Gomez, F.; Tagami, J.; Twetman, S.; Tsakos, G.; Ismail, A. Dental caries. Nat. Rev. Dis. Primers 2017, 25, 17030. [Google Scholar] [CrossRef] [Green Version]
- Lai, A.G.; Pasea, L.; Banerjee, A.; Hall, G.; Denaxas, S.; Chang, W.H.; Katsoulis, M.; Williams, B.; Pillay, D.; Noursadeghi, M.; et al. Estimated impact of the COVID-19 pandemic on cancer services and excess 1-year mortality in people with cancer and multimorbidity: Near real-time data on cancer care, cancer deaths and a population-based cohort study. BMJ Open 2020, 10, e043828. [Google Scholar] [CrossRef]
- Seidu, S.; Kunutsor, S.K.; Cos, X.; Khunti, K. Indirect impact of the COVID-19 pandemic on hospitalisations for cardiometabolic conditions and their management: A systematic review. Prim. Care Diabetes 2021, 15, 653–681. [Google Scholar] [CrossRef]
- Fisher, L.; Polonsky, W.; Asuni, A.; Jolly, Y.; Hessler, D. The early impact of the COVID-19 pandemic on adults with type 1 or type 2 diabetes: A national cohort study. J. Diabetes Complicat. 2020, 34, 107748. [Google Scholar] [CrossRef]
- Smith, A.; Al-Mahdi, R.; Malcolm, W.; Palmer, N.; Dahlen, G.; Al-Haroni, M. Comparison of antimicrobial prescribing for dental and oral infections in England and Scotland with Norway and Sweden and their relative contribution to national consumption 2010–2016. BMC Oral Health 2020, 20, 172. [Google Scholar] [CrossRef] [PubMed]
- Agencia Española de Medicamentos y Productos Sanitarios (AEMPS). Plan. Nacional Frente a La Resistencia a Los Antibióticos 2019–2021. 2019. Available online: https://www.resistenciaantibioticos.es/es/publicaciones/plan-nacional-frente-la-resistencia-los-antibioticos-pran-2019-2021 (accessed on 11 February 2022).
- Park, J.S.; Page, A.T.; Kruger, E.; Tennant, M. Dispensing patterns of medicines prescribed by australian dentists from 2006 to 2018—A Pharmacoepidemiological Study. Int. Dent. J. 2021, 71, 106–112. [Google Scholar] [CrossRef]
- Halling, F.; Neff, A.; Heymann, P.; Ziebart, T. Trends in antibiotic prescribing by dental practitioners in Germany. J. Craniomaxillofac. Surg. 2017, 45, 1854–1859. [Google Scholar] [CrossRef] [PubMed]
- Struyf, T.; Vandael, E.; Leroy, R.; Mertens, K.; Catry, B. Antimicrobial prescribing by Belgian dentists in ambulatory care, from 2010 to 2016. Int. Dent. J. 2019, 69, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Urrusuno, R.; Grupo de Trabajo de la Guía. Guía de Terapéutica Antimicrobiana Del Área Aljarafe 3a Edición; Distrito Sanitario Aljarafe-Sevilla Norte y Hospital San Juan de Dios del Aljarafe: Sevilla, Spain, 2018. [Google Scholar]
- Scottish Dental Clinical Effectiveness Programme. Drug Prescribing for Dentistry. Dental Clinical Guidelines, 3rd ed.; The Royal Pharmaceutical Society of Great Britain and the BMJ Publishing Group Ltd.: Dundee, UK, 2016. [Google Scholar]
- Segura-Egea, J.J.; Gould, K.; Şen, B.H.; Jonasson, P.; Cotti, E.; Mazzoni, A.; Sunay, H.; Tjäderhane, L.; Dummer, P.M.H. European Society of Endodontology position statement: The use of antibiotics in endodontics. Int. Endod. J. 2018, 51, 20–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilson, W.R.; Gewitz, M.; Lockhart, P.B.; Bolger, A.F.; DeSimone, D.C.; Kazi, D.S.; Couper, D.J.; Beaton, A.; Kilmartin, C.; Miro, J.M.; et al. Prevention of viridans group streptococcal infective endocarditis: A scientific statement from the american heart association. Circulation 2021, 143, E963–E978. [Google Scholar] [CrossRef]
- Thornhill, M.; Dayer, M.; Durkin, M.; Lockhart, P.; Baddour, L. Risk of Adverse Reactions to Oral Antibiotics Prescribed by Dentists. J. Dent. Res. 2019, 98, 1081. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Silva, T.M.; Estrela, M.; Gomes, E.R.; Piñeiro-Lamas, M.; Figueiras, A.; Roque, F.; Herdeiro, M.T. The impact of the COVID-19 pandemic on antibiotic prescribing trends in outpatient care: A nationwide, quasi-experimental approach. Antibiotics 2021, 25, 1040. [Google Scholar] [CrossRef]
- Bernal, J.L.; Cummins, S.; Gasparrini, A. Interrupted time series regression for the evaluation of public health interventions: A tutorial. Int. J. Epidemiol. 2017, 46, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Servizo Galego de Saude. SERGAS. Memoria de Actividade Sergas. 2018. Available online: https://www.sergas.es/A-nosa-organizacion/Documents/832/MemoriaActividade2018.pdf (accessed on 13 February 2022).
- Sruamsiri, R.; Wagner, A.K.; Ross-Degnan, D.; Lu, C.Y.; Dhippayom, T.; Ngorsuraches, S.; Chaiyakunapruk, N. Expanding access to high-cost medicines through the E2 access program in Thailand: Effects on utilisation, health outcomes and cost using an interrupted time-series análisis. BMJ Open 2016, 6, e008671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef]
- Kontopantelis, E.; Doran, T.; Springate, D.A.; Buchan, I.; Reeves, D. Regression based quasi-experimental approach when randomisation is not an option: Interrupted time series analysis. BMJ 2015, 350, h2750. [Google Scholar] [CrossRef] [Green Version]
- WHOCC—ATC/DDD—Collaborating Centre for Drug Statistics Methodology, ATC Classification Index with DDDs. Available online: https://www.whocc.no/atc_ddd_index_and_guidelines/atc_ddd_index/ (accessed on 14 February 2022).
- WHOCC—Collaborating Centre for Drug Statistics Methodology. Definition and General Considerations for DDD Assignment. Available online: https://www.whocc.no/ddd/defi (accessed on 14 February 2022).
- Rodrigues, A.T.; Roque, F.; Piñeiro-Lamas, M.; Falcão, A.; Figueiras, A.; Herdeiro, M.T. Effectiveness of an intervention to improve antibiotic-prescribing behaviour in primary care: A controlled, interrupted time-series study. J. Antimicrob. Chemother. 2019, 74, 2788–2796. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Mourelle, R.; Carracedo-Martínez, E.; Figueiras, A. Impact of a change of bronchodilator medications in a hospital drug formulary on intra-and out-of-hospital drug prescriptions: Interrupted time series design with comparison group. Implement Sci. 2020, 15, 33. [Google Scholar] [CrossRef] [PubMed]
- Sax, C.; Eddelbuettel, D. Seasonal Adjustment by X-13ARIMA-SEATS in R. J. Stat. Softw. 2018, 87, 1–17. [Google Scholar] [CrossRef] [Green Version]
- Zhang, F.; Wagner, A.K.; Soumerai, S.B.; Ross-Degnan, D. Methods for estimating confidence intervals in interrupted time series analyses of health interventions. J. Clin. Epidemiol. 2009, 62, 143–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- R: The R Foundation. Available online: https://www.r-project.org/foundation/ (accessed on 13 February 2022).
- StataCorp. Stata Statistical Software: Release 12; StataCorp LP: College Station, TX, USA, 2011. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).