Clinical Impact of COVID-19 on Multi-Drug-Resistant Gram-Negative Bacilli Bloodstream Infections in an Intensive Care Unit Setting: Two Pandemics Compared
Abstract
:1. Introduction
2. Results
2.1. Microbiological Data
2.2. Hospitalization and Mortality Data
3. Discussion
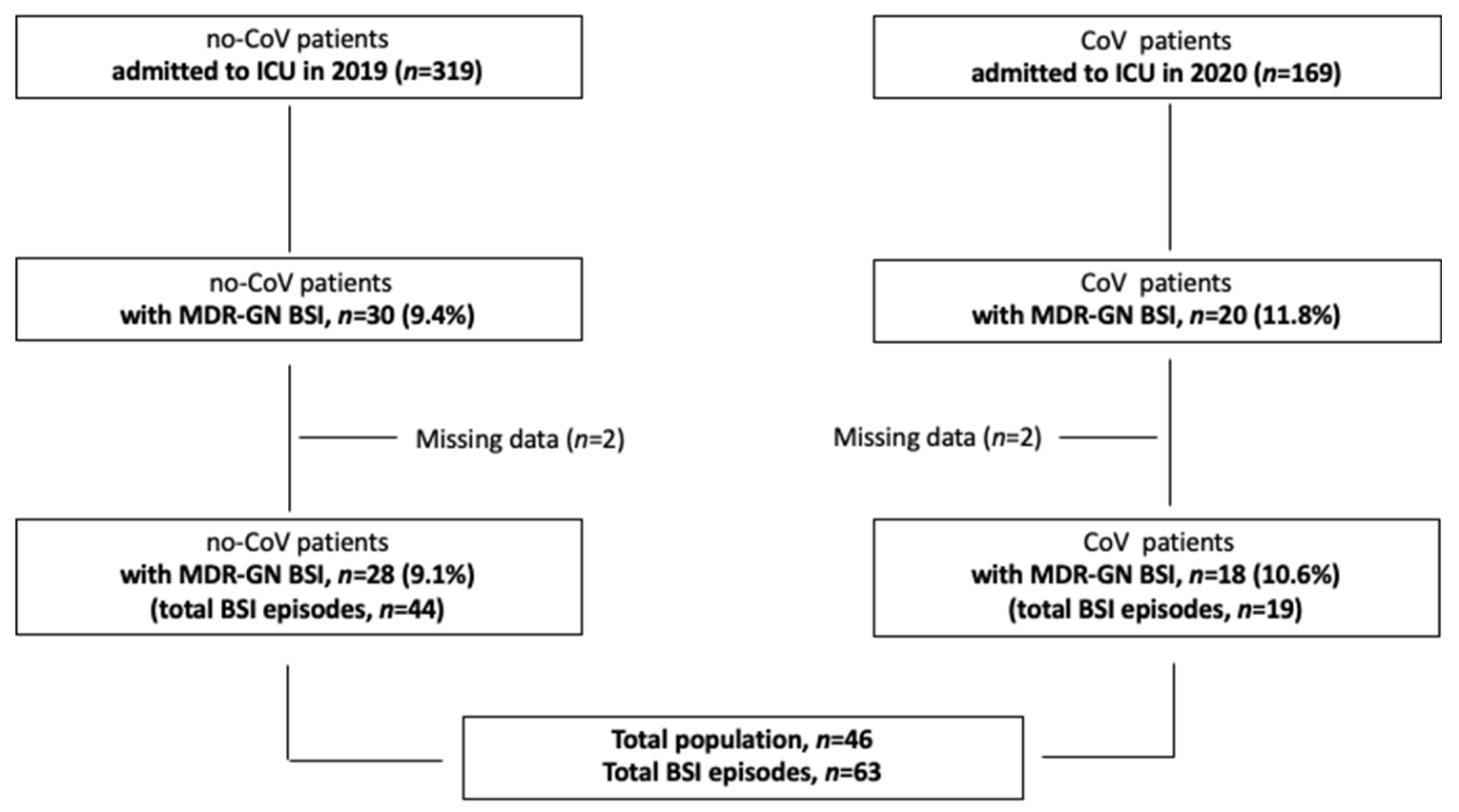
4. Materials and Methods
4.1. Definitions
4.2. Microbiological Analyses
Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 31 May 2022).
- Murray, C.J.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global Burden of Bacterial Antimicrobial Resistance in 2019: A Systematic Analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- WHO 10 Global Health Issues to Track in 2021. Available online: https://www.who.int/news-room/spotlight/10-global-health-issues-to-track-in-2021 (accessed on 13 May 2022).
- World Bank Drug-Resistant Infections: A Threat to Our Economic Future. Available online: https://www.worldbank.org/en/topic/health/publication/drug-resistant-infections-a-threat-to-our-economic-future (accessed on 13 May 2022).
- Monnet, D.L.; Harbarth, S. Will Coronavirus Disease (COVID-19) Have an Impact on Antimicrobial Resistance? Eurosurveillance 2020, 25, 2001886. [Google Scholar] [CrossRef] [PubMed]
- Rawson, T.M.; Ming, D.; Ahmad, R.; Moore, L.S.P.; Holmes, A.H. Antimicrobial Use, Drug-Resistant Infections and COVID-19. Nat. Rev. Microbiol. 2020, 18, 409–410. [Google Scholar] [CrossRef] [PubMed]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Soucy, J.-P.R.; Westwood, D.; Daneman, N.; MacFadden, D.R. Antibiotic Prescribing in Patients with COVID-19: Rapid Review and Meta-Analysis. Clin. Microbiol. Infect. 2021, 27, 520–531. [Google Scholar] [CrossRef]
- Kampmeier, S.; Tönnies, H.; Correa-Martinez, C.L.; Mellmann, A.; Schwierzeck, V. A Nosocomial Cluster of Vancomycin Resistant Enterococci among COVID-19 Patients in an Intensive Care Unit. Antimicrob. Resist. Infect. Control 2020, 9, 154. [Google Scholar] [CrossRef]
- Polly, M.; de Almeida, B.L.; Lennon, R.P.; Cortês, M.F.; Costa, S.F.; Guimarães, T. Impact of the COVID-19 Pandemic on the Incidence of Multidrug-Resistant Bacterial Infections in an Acute Care Hospital in Brazil. Am. J. Infect. Control 2022, 50, 32–38. [Google Scholar] [CrossRef]
- Porretta, A.D.; Baggiani, A.; Arzilli, G.; Casigliani, V.; Mariotti, T.; Mariottini, F.; Scardina, G.; Sironi, D.; Totaro, M.; Barnini, S.; et al. Increased Risk of Acquisition of New Delhi Metallo-Beta-Lactamase-Producing Carbapenem-Resistant Enterobacterales (NDM-CRE) among a Cohort of COVID-19 Patients in a Teaching Hospital in Tuscany, Italy. Pathogens 2020, 9, 635. [Google Scholar] [CrossRef]
- Garcia-Vidal, C.; Sanjuan, G.; Moreno-García, E.; Puerta-Alcalde, P.; Garcia-Pouton, N.; Chumbita, M.; Fernandez-Pittol, M.; Pitart, C.; Inciarte, A.; Bodro, M.; et al. Incidence of Co-Infections and Superinfections in Hospitalized Patients with COVID-19: A Retrospective Cohort Study. Clin. Microbiol. Infect. 2021, 27, 83–88. [Google Scholar] [CrossRef]
- Contou, D.; Claudinon, A.; Pajot, O.; Micaëlo, M.; Longuet Flandre, P.; Dubert, M.; Cally, R.; Logre, E.; Fraissé, M.; Mentec, H.; et al. Bacterial and Viral Co-Infections in Patients with Severe SARS-CoV-2 Pneumonia Admitted to a French ICU. Ann. Intensive Care 2020, 10, 119. [Google Scholar] [CrossRef]
- Hazel, K.; Skally, M.; Glynn, E.; Foley, M.; Burns, K.; O’Toole, A.; Boland, K.; Fitzpatrick, F. The Other “C”: Hospital-Acquired Clostridioides Difficile Infection during the Coronavirus Disease 2019 (COVID-19) Pandemic. Infect. Control Hosp. Epidemiol. 2022, 43, 540–541. [Google Scholar] [CrossRef]
- Buetti, N.; Ruckly, S.; de Montmollin, E.; Reignier, J.; Terzi, N.; Cohen, Y.; Siami, S.; Dupuis, C.; Timsit, J.-F. COVID-19 Increased the Risk of ICU-Acquired Bloodstream Infections: A Case–Cohort Study from the Multicentric OUTCOMEREA Network. Intensive Care Med. 2021, 47, 180–187. [Google Scholar] [CrossRef] [PubMed]
- Baccolini, V.; Migliara, G.; Isonne, C.; Dorelli, B.; Barone, L.C.; Giannini, D.; Marotta, D.; Marte, M.; Mazzalai, E.; Alessandri, F.; et al. The Impact of the COVID-19 Pandemic on Healthcare-Associated Infections in Intensive Care Unit Patients: A Retrospective Cohort Study. Antimicrob. Resist. Infect. Control 2021, 10, 87. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Tiseo, G.; Giordano, C.; Leonildi, A.; Menichini, M.; Vecchione, A.; Pistello, M.; Guarracino, F.; Ghiadoni, L.; Forfori, F.; et al. Predictors of Hospital-Acquired Bacterial and Fungal Superinfections in COVID-19: A Prospective Observational Study. J. Antimicrob. Chemother. 2021, 76, 1078–1084. [Google Scholar] [CrossRef] [PubMed]
- Fattorini, L.; Creti, R.; Palma, C.; Pantosti, A. Unit of Antibiotic Resistance and Special Pathogens; Unit of Antibiotic Resistance and Special Pathogens of the Department of Infectious Diseases, Istituto Superiore di Sanità, Rome Bacterial Coinfections in COVID-19: An Underestimated Adversary. Ann. Ist. Super. Sanita 2020, 56, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Mędrzycka-Dąbrowska, W.; Lange, S.; Zorena, K.; Dąbrowski, S.; Ozga, D.; Tomaszek, L. Carbapenem-Resistant Klebsiella Pneumoniae Infections in ICU COVID-19 Patients—A Scoping Review. J. Clin. Med. 2021, 10, 2067. [Google Scholar] [CrossRef] [PubMed]
- Thoma, R.; Seneghini, M.; Seiffert, S.N.; Vuichard Gysin, D.; Scanferla, G.; Haller, S.; Flury, D.; Boggian, K.; Kleger, G.-R.; Filipovic, M.; et al. The Challenge of Preventing and Containing Outbreaks of Multidrug-Resistant Organisms and Candida Auris during the Coronavirus Disease 2019 Pandemic: Report of a Carbapenem-Resistant Acinetobacter Baumannii Outbreak and a Systematic Review of the Literature. Antimicrob. Resist. Infect. Control 2022, 11, 12. [Google Scholar] [CrossRef]
- Serapide, F.; Quirino, A.; Scaglione, V.; Morrone, H.L.; Longhini, F.; Bruni, A.; Garofalo, E.; Matera, G.; Marascio, N.; Scarlata, G.G.M.; et al. Is the Pendulum of Antimicrobial Drug Resistance Swinging Back after COVID-19? Microorganisms 2022, 10, 957. [Google Scholar] [CrossRef]
- Pascale, R.; Bussini, L.; Gaibani, P.; Bovo, F.; Fornaro, G.; Lombardo, D.; Ambretti, S.; Pensalfine, G.; Appolloni, L.; Bartoletti, M.; et al. Carbapenem-Resistant Bacteria in an Intensive Care Unit during the Coronavirus Disease 2019 (COVID-19) Pandemic: A Multicenter before-and-after Cross-Sectional Study. Infect. Control Hosp. Epidemiol. 2022, 43, 461–466. [Google Scholar] [CrossRef]
- Russo, A.; Gavaruzzi, F.; Ceccarelli, G.; Borrazzo, C.; Oliva, A.; Alessandri, F.; Magnanimi, E.; Pugliese, F.; Venditti, M. Multidrug-Resistant Acinetobacter Baumannii Infections in COVID-19 Patients Hospitalized in Intensive Care Unit. Infection 2022, 50, 83–92. [Google Scholar] [CrossRef]
- Segala, F.V.; Bavaro, D.F.; Di Gennaro, F.; Salvati, F.; Marotta, C.; Saracino, A.; Murri, R.; Fantoni, M. Impact of SARS-CoV-2 Epidemic on Antimicrobial Resistance: A Literature Review. Viruses 2021, 13, 2110. [Google Scholar] [CrossRef]
- Magnasco, L.; Mikulska, M.; Giacobbe, D.R.; Taramasso, L.; Vena, A.; Dentone, C.; Dettori, S.; Tutino, S.; Labate, L.; Di Pilato, V.; et al. Spread of Carbapenem-Resistant Gram-Negatives and Candida Auris during the COVID-19 Pandemic in Critically Ill Patients: One Step Back in Antimicrobial Stewardship? Microorganisms 2021, 9, 95. [Google Scholar] [CrossRef]
- Chamieh, A.; Zgheib, R.; El-Sawalhi, S.; Yammine, L.; El-Hajj, G.; Zmerli, O.; Afif, C.; Rolain, J.-M.; Azar, E. Trends of Multidrug-Resistant Pathogens, Difficult to Treat Bloodstream Infections, and Antimicrobial Consumption at a Tertiary Care Center in Lebanon from 2015-2020: COVID-19 Aftermath. Antibiot. Basel Switz. 2021, 10, 1016. [Google Scholar] [CrossRef] [PubMed]
- Nebreda-Mayoral, T.; Miguel-Gómez, M.A.; March-Rosselló, G.A.; Puente-Fuertes, L.; Cantón-Benito, E.; Martínez-García, A.M.; Muñoz-Martín, A.B.; Orduña-Domingo, A. Infección Bacteriana/Fúngica En Pacientes Con COVID-19 Ingresados En Un Hospital de Tercer Nivel de Castilla y León, España. Enferm. Infecc. Microbiol. Clin. 2022, 40, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Scaravilli, V.; Mangioni, D.; Scudeller, L.; Alagna, L.; Bartoletti, M.; Bellani, G.; Biagioni, E.; Bonfanti, P.; Bottino, N.; et al. Hospital-Acquired Infections in Critically Ill Patients With COVID-19. Chest 2021, 160, 454–465. [Google Scholar] [CrossRef] [PubMed]
- Vijay, S.; Bansal, N.; Rao, B.K.; Veeraraghavan, B.; Rodrigues, C.; Wattal, C.; Goyal, J.P.; Tadepalli, K.; Mathur, P.; Venkateswaran, R.; et al. Secondary Infections in Hospitalized COVID-19 Patients: Indian Experience. Infect. Drug Resist. 2021, 14, 1893–1903. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Bassetti, M.; Tiseo, G.; Giordano, C.; Nencini, E.; Russo, A.; Graziano, E.; Tagliaferri, E.; Leonildi, A.; Barnini, S.; et al. Time to Appropriate Antibiotic Therapy Is a Predictor of Outcome in Patients with Bloodstream Infection Caused by KPC-Producing Klebsiella Pneumoniae. Crit. Care 2020, 24, 29. [Google Scholar] [CrossRef] [Green Version]
- Russo, A.; Giuliano, S.; Ceccarelli, G.; Alessandri, F.; Giordano, A.; Brunetti, G.; Venditti, M. Comparison of Septic Shock Due to Multidrug-Resistant Acinetobacter Baumannii or Klebsiella Pneumoniae Carbapenemase-Producing K. Pneumoniae in Intensive Care Unit Patients. Antimicrob. Agents Chemother. 2018, 62, e02562-17. [Google Scholar] [CrossRef] [Green Version]
- Machuca, I.; Gutiérrez-Gutiérrez, B.; Gracia-Ahufinger, I.; Rivera Espinar, F.; Cano, Á.; Guzmán-Puche, J.; Pérez-Nadales, E.; Natera, C.; Rodríguez, M.; León, R.; et al. Mortality Associated with Bacteremia Due to Colistin-Resistant Klebsiella Pneumoniae with High-Level Meropenem Resistance: Importance of Combination Therapy without Colistin and Carbapenems. Antimicrob. Agents Chemother. 2017, 61, e00406-17. [Google Scholar] [CrossRef] [Green Version]
- Oliva, A.; Miele, M.C.; Di Timoteo, F.; De Angelis, M.; Mauro, V.; Aronica, R.; Al Ismail, D.; Ceccarelli, G.; Pinacchio, C.; d’Ettorre, G.; et al. Persistent Systemic Microbial Translocation and Intestinal Damage During Coronavirus Disease-19. Front. Immunol. 2021, 12, 708149. [Google Scholar] [CrossRef]
- Spagnolello, O.; Pinacchio, C.; Santinelli, L.; Vassalini, P.; Innocenti, G.P.; Girolamo, G.D.; Fabris, S.; Giovanetti, M.; Angeletti, S.; Russo, A.; et al. Targeting Microbiome: An Alternative Strategy for Fighting SARS-CoV-2 Infection. Chemotherapy 2021, 66, 24–32. [Google Scholar] [CrossRef]
- Oliva, A.; Aversano, L.; De Angelis, M.; Mascellino, M.T.; Miele, M.C.; Morelli, S.; Battaglia, R.; Iera, J.; Bruno, G.; Corazziari, E.S.; et al. Persistent Systemic Microbial Translocation, Inflammation, and Intestinal Damage During Clostridioides Difficile Infection. Open Forum Infect. Dis. 2020, 7, ofz507. [Google Scholar] [CrossRef] [PubMed]
- Falcone, M.; Russo, A.; Iraci, F.; Carfagna, P.; Goldoni, P.; Vullo, V.; Venditti, M. Risk Factors and Outcomes for Bloodstream Infections Secondary to Clostridium Difficile Infection. Antimicrob. Agents Chemother. 2016, 60, 252–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A Severity of Disease Classification System. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Al-Hasan, M.N.; Lahr, B.D.; Eckel-Passow, J.E.; Baddour, L.M. Predictive Scoring Model of Mortality in Gram-Negative Bloodstream Infection. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2013, 19, 948–954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.-D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Magiorakos, A.-P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-Resistant, Extensively Drug-Resistant and Pandrug-Resistant Bacteria: An International Expert Proposal for Interim Standard Definitions for Acquired Resistance. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2012, 18, 268–281. [Google Scholar] [CrossRef] [Green Version]
- Tamma, P.D.; Aitken, S.L.; Bonomo, R.A.; Mathers, A.J.; van Duin, D.; Clancy, C.J. Infectious Diseases Society of America Guidance on the Treatment of Extended-Spectrum β-Lactamase Producing Enterobacterales (ESBL-E), Carbapenem-Resistant Enterobacterales (CRE), and Pseudomonas Aeruginosa with Difficult-to-Treat Resistance (DTR-P. Aeruginosa). Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2021, 72, e169–e183. [Google Scholar] [CrossRef]
- EUCAST EUCAST: Clinical Breakpoints and Dosing of Antibiotics. Available online: https://www.eucast.org/clinical_breakpoints/ (accessed on 17 May 2022).

| Characteristics | Total Population | No-CoV | CoV | p Value |
|---|---|---|---|---|
| (n 46) | (n 28) | (n 18) | ||
| General, n, % | ||||
| Age, years, median (IQR) | 65.5 (57–73) | 66.5 (56.7–73) | 63.5 (57.5–72.5) | ns |
| Gender, F/M | 14 (30.4)/32 (69.6) | 11 (39.3)/17 (60.7) | 3 (16.7)/15 (83.3) | ns |
| Other hospitalization in previous 90 days | 10 (21.7) | 8 (22.8) | 2 (10.5) | ns |
| Pre-hospitalization antibiotic therapy in previous 90 days | 13 (28.3) | 6 (20.4) | 7 (36.8) | ns |
| Pre-BSI antibiotic therapy | 45 (97.8) | 27 (95.4) | 18 (100) | ns |
| Patients with >1 BSI from different MDRO | 14 (30.4) | 13 (28.3) | 1 (2.2) | 0.003 |
| Comorbidities, n. (%) | ||||
| Myocardial infarction | 7 (15.2) | 5 (17.9) | 2 (11.1) | ns |
| Congestive heart failure | 14 (30.4) | 10 (35.7) | 4 (22.2) | ns |
| Peripheral vascular disease | 13 (28.3) | 8 (28.6) | 5 (27.8) | ns |
| Cerebrovascular disease | 4 (8.7) | 3 (10.7) | 1 (5.5) | ns |
| Dementia | 3 (6.5) | 2 (7.1) | 1 (5.5) | ns |
| Chronic obstructive pulmonary disease | 6 (13) | 6 (21.4) | 0 | NA |
| Liver disease {1} | 1 (2.2) | 1 (3.6) | 0 | NA |
| Diabetes mellitus | 11 (23.9) | 8 (28.6) | 3 (7.2) | ns |
| Hemiplegia | 1 (2.2) | 1 (3.6) | 0 | NA |
| Chronic kidney disease {2} | 2 (4.4) | 1 (3.6) | 1 (5.5) | ns |
| Solid tumor | 3 (6.5) | 3 (10.7) | 0 | NA |
| Leukemia | 1 (2.2) | 0 | 1 (5.5) | NA |
| Charlson Comorbidity Index, median (IQR) | 3.5 (2–6) | 4 (2–6) | 2 (1.25–4) | ns |
| APACHE II score {3}, median (IQR) | 18.5 (13–23) | 22 (16–23) | 11 (3.2–21.5) | 0.003 |
| Polytrauma | 9 (19.6) | 9 (32.1) | 0 (0) | 0.007 |
| Outcome, median (IQR) | ||||
| Days of hospitalization overall | 43 (29.5–98.75) | 69.5 (43.5–141.5) | 28.5(18.7–35.7) | 0.001 |
| Days of hospitalization until ICU admission | 2 (0–6) | 2 (0–9.75) | 2 (0.25–5) | ns |
| Days of hospitalization until BSI | 25.5 (12.25–37.5) | 29 (15–48.25) | 20 (9.5–26.75) | 0.02 |
| Days of ICU hospitalization | 31.5 (21.25–68) | 56 (28–91.25) | 25 (13.5–29.5) | 0.004 |
| Days of ICU hospitalization until BSI | 18.5 (9–29) | 23 (9.75–34.75) | 14.5 (9–21.75) | ns |
| Days of hospitalization from BSI to death | 15.5 (4.25–45.75) | 44 (14.5–117.5) | 5 (1.25–11.75) | 0.003 |
| Overall in-hospital mortality, n. (%) | 29 (63) | 15 (53.6) | 14 (77.8) | ns |
| Mortality 30 days from ICU admission, n. (%) | 20 (43.5) | 6 (21.4) | 14 (77.8) | <0.0001 |
| Mortality 30 days from BSI, n. (%) | 20 (43.5) | 6 (21.4) | 14 (77.8) | <0.0001 |
| BSI Characteristics | Total BSI | No-CoV | CoV | |
| (n 63) | (n 44) | (n 19) | ||
| Microbiological data, n (%) | ||||
| Pre-BSI infections from no MDRO {4} | 57 (90.6) | 43 (97.7%) | 14 (73.7) | 0.003 |
| Pre-BSI infections from MDRO {4} | 48 (76.2) | 38 (86.4) | 10 (52.6) | 0.004 |
| MDRO colonization | 45 (71.4) | 36 (81.8) | 9 (47.4) | 0.005 |
| Overall BSI incidence density, n per 100 patients | 16.5 | 11.2 | ns | |
| K. pneumoniae BSI | 26 (41.3) | 22 (50) | 4 (21) | 0.032 |
| -Incidence density, n per 100 patients | 8.2 | 2.4 | 0.012 | |
| A. baumannii BSI | 32 (50.8) | 17 (38.6) | 15 (78.9) | 0.003 |
| -Incidence density, n per 100 patients | 6.4 | 9 | ns | |
| P. aeruginosa BSI | 5 (7.9) | 5 (11.4) | 0 | ns |
| Source of BSI | ns | |||
| 31 (49.2) | 21 (47.7) | 10 (52.6) | |
| 5 (7.9) | 5 (11.4) | 0 | |
| 2 (3.2) | 2 (4.5) | 0 | |
| Primary BSI | 25 (39.7) | 16 (36.4) | 9 (47.4) | ns |
| Source control | 8 (12.7) | 4 (9.1) | 4 (21) | ns |
| Clinical data | ||||
| Septic shock at BSI onset, n (%) | 25 (39.7) | 12 (27.3) | 13 (68.4) | 0.003 |
| PITT score on the BSI day, median (IQR) | 3 (1–8) | 3 (1–5) | 8 (2–8) | 0.002 |
| Treatment data | ||||
| Early active therapy (<24 h), n (%) | 31 (49.2) | 21 (47.7) | 10 (52.6) | ns |
| Time to definite therapy, median (IQR) | 1 (1–2) | 1 (1–2) | 1 (1–2) | ns |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cogliati Dezza, F.; Arcari, G.; Alessi, F.; Valeri, S.; Curtolo, A.; Sacco, F.; Ceccarelli, G.; Raponi, G.; Alessandri, F.; Mastroianni, C.M.; et al. Clinical Impact of COVID-19 on Multi-Drug-Resistant Gram-Negative Bacilli Bloodstream Infections in an Intensive Care Unit Setting: Two Pandemics Compared. Antibiotics 2022, 11, 926. https://doi.org/10.3390/antibiotics11070926
Cogliati Dezza F, Arcari G, Alessi F, Valeri S, Curtolo A, Sacco F, Ceccarelli G, Raponi G, Alessandri F, Mastroianni CM, et al. Clinical Impact of COVID-19 on Multi-Drug-Resistant Gram-Negative Bacilli Bloodstream Infections in an Intensive Care Unit Setting: Two Pandemics Compared. Antibiotics. 2022; 11(7):926. https://doi.org/10.3390/antibiotics11070926
Chicago/Turabian StyleCogliati Dezza, Francesco, Gabriele Arcari, Federica Alessi, Serena Valeri, Ambrogio Curtolo, Federica Sacco, Giancarlo Ceccarelli, Giammarco Raponi, Francesco Alessandri, Claudio Maria Mastroianni, and et al. 2022. "Clinical Impact of COVID-19 on Multi-Drug-Resistant Gram-Negative Bacilli Bloodstream Infections in an Intensive Care Unit Setting: Two Pandemics Compared" Antibiotics 11, no. 7: 926. https://doi.org/10.3390/antibiotics11070926
APA StyleCogliati Dezza, F., Arcari, G., Alessi, F., Valeri, S., Curtolo, A., Sacco, F., Ceccarelli, G., Raponi, G., Alessandri, F., Mastroianni, C. M., Venditti, M., & Oliva, A. (2022). Clinical Impact of COVID-19 on Multi-Drug-Resistant Gram-Negative Bacilli Bloodstream Infections in an Intensive Care Unit Setting: Two Pandemics Compared. Antibiotics, 11(7), 926. https://doi.org/10.3390/antibiotics11070926








