The Comparative Effectiveness of Ceftolozane/Tazobactam versus Aminoglycoside- or Polymyxin-Based Regimens in Multi-Drug-Resistant Pseudomonas aeruginosa Infections
Abstract
:1. Introduction
2. Results
3. Discussion
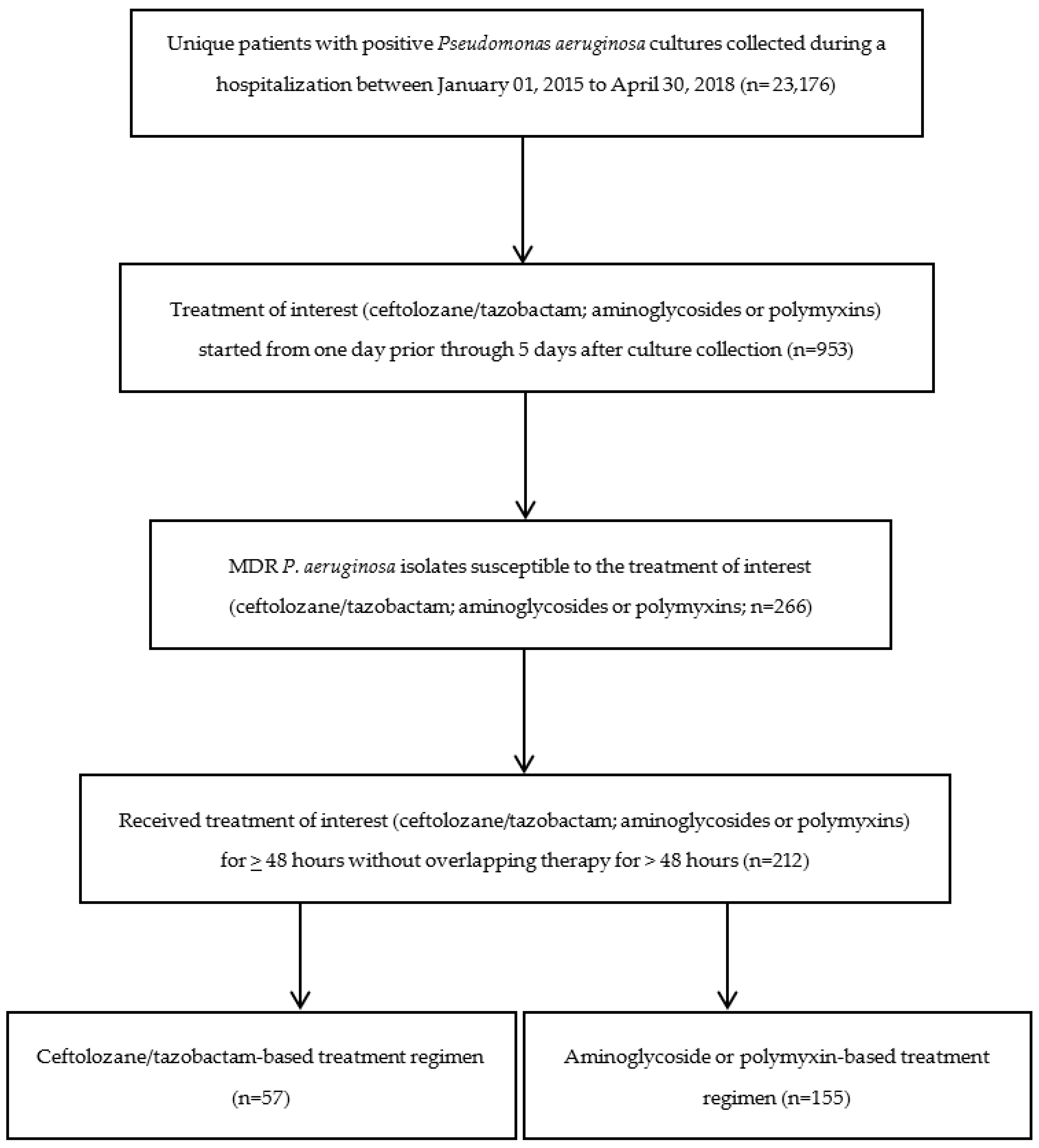
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bassetti, M.; Vena, A.; Croxatto, A.; Righi, E.; Guery, B. How to manage Pseudomonas aeruginosa infections. Drugs Context 2018, 7, 212527. [Google Scholar] [CrossRef] [PubMed]
- O'Donnell, J.N.; Bidell, M.R.; Lodise, T.P. Approach to the Treatment of Patients with Serious Multidrug-Resistant Pseudomonas aeruginosa Infections. Pharmacotherapy 2020, 40, 952–969. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.F.; Silva, C.A.; Barbieri, C.D.; Oliveira, G.M.; Zanetta, D.M.; Burdmann, E.A. Prevalence and risk factors for aminoglycoside nephrotoxicity in intensive care units. Antimicrob. Agents Chemother. 2009, 53, 2887–2891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vidal, L.; Gafter-Gvili, A.; Borok, S.; Fraser, A.; Leibovici, L.; Paul, M. Efficacy and safety of aminoglycoside monotherapy: Systematic review and meta-analysis of randomized controlled trials. J. Antimicrob. Chemother. 2007, 60, 247–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oliota, A.F.; Penteado, S.T.; Tonin, F.S.; Fernandez-Llimos, F.; Sanches, A.C. Nephrotoxicity prevalence in patients treated with polymyxins: A systematic review with meta-analysis of observational studies. Diagn. Microbiol. Infect. Dis. 2019, 94, 41–49. [Google Scholar] [CrossRef] [PubMed]
- Van Duin, D.; Lok, J.J.; Earley, M.; Cober, E.; Richter, S.S.; Perez, F.; Salata, R.A.; Kalayjian, R.C.; Watkins, R.R.; Doi, Y.; et al. Colistin Versus Ceftazidime-Avibactam in the Treatment of Infections Due to Carbapenem-Resistant Enterobacteriaceae. Clin. Infect. Dis. 2018, 66, 163–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pogue, J.M.; Kaye, K.S.; Veve, M.P.; Patel, T.S.; Gerlach, A.T.; Davis, S.L.; Puzniak, L.A.; File, T.M.; Olson, S.; Dhar, S.; et al. Ceftolozane/Tazobactam vs Polymyxin or Aminoglycoside-based Regimens for the Treatment of Drug-resistant Pseudomonas aeruginosa. Clin. Infect. Dis. 2020, 71, 304–310. [Google Scholar] [CrossRef] [PubMed]
- Horcajada, J.P.; Montero, M.; Oliver, A.; Sorlí, L.; Luque, S.; Gómez-Zorrilla, S.; Benito, N.; Grau, S. Epidemiology and Treatment of Multidrug-Resistant and Extensively Drug-Resistant Pseudomonas aeruginosa Infections. Clin. Microbiol. Rev. 2019, 32, e00031-19. [Google Scholar] [CrossRef] [PubMed]
- Karlowsky, J.A.; Lob, S.H.; Young, K.; Motyl, M.R.; Sahm, D.F. Activity of imipenem-relebactam against multidrug-resistant Pseudomonas aeruginosa from the United States—SMART 2015–2017. Diagn. Microbiol. Infect. Dis. 2019, 95, 212–215. [Google Scholar] [CrossRef]
- Vena, A.; Giacobbe, D.R.; Mussini, C.; Cattelan, A.; Bassetti, M.; Group, C.S. Clinical Efficacy of Ceftolozane-Tazobactam Versus Other Active Agents for the Treatment of Bacteremia and Nosocomial Pneumonia due to Drug-Resistant Pseudomonas aeruginosa. Clin. Infect. Dis. 2020, 71, 1799–1801. [Google Scholar] [CrossRef]
- Kang, C.I.; Kim, S.H.; Kim, H.B.; Park, S.W.; Choe, Y.J.; Oh, M.D.; Kim, E.C.; Choe, K.W. Pseudomonas aeruginosa bacteremia: Risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin. Infect. Dis. 2003, 37, 745–751. [Google Scholar] [CrossRef] [Green Version]
- Gallagher, J.C.; Satlin, M.J.; Elabor, A.; Saraiya, N.; McCreary, E.K.; Molnar, E.; El-Beyrouty, C.; Jones, B.M.; Dixit, D.; Heil, E.L.; et al. Ceftolozane-Tazobactam for the Treatment of Multidrug-Resistant. Open Forum Infect. Dis. 2018, 5, ofy280. [Google Scholar] [CrossRef] [PubMed]
- Timsit, J.F.; de Kraker, M.E.; Sommer, H.; Weiss, E.; Bettiol, E.; Wolkewitz, M.; Nikolakopoulos, S.; Wilson, D.; Harbarth, S. Appropriate endpoints for evaluation of new antibiotic therapies for severe infections: A perspective from COMBACTE’s STAT-Net. Intensive Care Med. 2017, 43, 1002–1012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Cruz, A.; Alba, N.; Semiglia-Chong, M.A.; Padilla, B.; Rodríguez-Macías, G.; Kwon, M.; Cercenado, E.; Chamorro-de-Vega, E.; Machado, M.; Pérez-Lago, L.; et al. A Case-Control Study of Real-Life Experience with Ceftolozane-Tazobactam in Patients with Hematologic Malignancy and Pseudomonas aeruginosa Infection. Antimicrob. Agents Chemother. 2019, 63, e02340-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pogue, J.M.; Kaye, K.S.; Bonomo, R.A.; Perez, F. Reply to Vena et al. Clin. Infect. Dis. 2020, 71, 1801–1802. [Google Scholar] [CrossRef] [PubMed]
- Puzniak, L.; Dillon, R.; Palmer, T.; Collings, H.; Enstone, A. Real-world use of ceftolozane/tazobactam: A systematic literature review. Antimicrob. Resist. Infect. Control 2021, 10, 68. [Google Scholar] [CrossRef] [PubMed]
| Baseline Demographics and Clinical Characteristics | Ceftolozane/Tazobactam (n = 57) | Aminoglycosides/Polymyxins (n = 155) | p-Value |
|---|---|---|---|
| Age, years | |||
| Mean (standard deviation) | 67.5 (9.5) | 71.1 (12.6) | 0.03 |
| Body mass index | |||
| Mean (standard deviation) | 27.4 (7.0) | 27.1 (7.3) | 0.77 |
| Male | 55 (96.5%) | 154 (99.4%) | 0.18 |
| White | 38 (66.7%) | 109 (70.3%) | 0.61 |
| Hispanic or Latino | <5 (<8.8%) | 35 (22.6%) | 0.0003 |
| Married | 33 (57.9%) | 63 (40.7%) | 0.03 |
| Admission source | |||
| Home/community | 24 (42.1%) | 54 (34.8%) | 0.33 |
| Hospital | <5 (<8.8%) | 12 (7.7%) | 0.76 |
| Nursing home | 7 (12.3%) | 5 (3.2%) | 0.02 |
| Treating specialty | |||
| Medicine | 19 (33.3%) | 66 (42.6%) | 0.22 |
| Intensive care | 14 (24.6%) | 43 (27.7%) | 0.64 |
| Surgery | 11 (19.3%) | 12 (7.7%) | 0.02 |
| Other | 12 (21.1%) | 19 (12.3%) | 0.11 |
| Intensive care during admission | 36 (63.2%) | 89 (57.4%) | 0.45 |
| Surgery during admission | 21 (36.8%) | 57 (36.8%) | 0.99 |
| Charlson score | |||
| Median (interquartile range) | 5 (3–7) | 3 (2–6) | 0.01 |
| Elixhauser score | |||
| Median (interquartile range) | 7 (4–10) | 5 (3–8) | 0.006 |
| APACHE score | |||
| Median (interquartile range) | 40 (29–52) | 43 (33–57) | 0.29 |
| Primary diagnosis | |||
| Osteomyelitis | <5 (<8.8%) | <5 (<3.2%) | 0.38 |
| Pneumonia | <5 (<8.8%) | 5 (3.2%) | 0.44 |
| Septicemia | 16 (28.1%) | 34 (21.9%) | 0.35 |
| Urinary tract infection | <5 (<8.8%) | 12 (7.7%) | 0.76 |
| Other infections | <5 (<8.8%) | 6 (3.9%) | 0.19 |
| Infection diagnosis during admission | |||
| Bacterial Infection | 50 (87.7%) | 123 (79.4%) | 0.16 |
| Chronic osteomyelitis | 12 (21.1%) | 13 (8.4%) | 0.01 |
| Intraabdominal infection | 7 (12.3%) | 22 (14.2%) | 0.72 |
| Osteomyelitis | 18 (31.6%) | 28 (18.1%) | 0.03 |
| Pneumonia | 30 (52.6%) | 87 (56.1%) | 0.65 |
| Septicemia | 40 (70.2%) | 98 (63.2%) | 0.35 |
| Skin and Subcutaneous | 13 (22.8%) | 26 (16.8%) | 0.31 |
| infection | |||
| Ulcers | 23 (40.4%) | 72 (46.5%) | 0.43 |
| Urinary tract infection | 33 (57.9%) | 97 (62.6%) | 0.53 |
| Current medical problems | |||
| Respiratory failure | 34 (59.7%) | 89 (57.4%) | 0.77 |
| Fever of unknown origin | 14 (24.6%) | 30 (19.4%) | 0.41 |
| Acute renal failure | 32 (56.1%) | 88 (56.8%) | 0.93 |
| Shock | 26 (45.6%) | 55 (35.5%) | 0.18 |
| Complications of surgical | 25 (43.9%) | 55 (35.5%) | 0.26 |
| procedures or medical care | |||
| Osteomyelitis | 18 (31.6%) | 30 (19.4%) | 0.06 |
| Spinal cord injury | 22 (38.6%) | 34 (21.9%) | 0.02 |
| Medical history | |||
| Acute myocardial infarction | <5 (<8.8%) | 10 (6.5%) | 0.52 |
| Congestive heart failure | 21 (36.8%) | 38 (24.5%) | 0.08 |
| Acute cerebrovascular disease | 10 (17.5%) | 19 (12.3%) | 0.32 |
| Cognitive disorders | 14 (24.6%) | 43 (27.7%) | 0.64 |
| Chronic obstructive | 25 (43.9%) | 60 (38.7%) | 0.49 |
| pulmonary disease | |||
| Diabetes without | 27 (47.4%) | 75 (48.4%) | 0.89 |
| complications | 22 (38.6%) | 47 (30.3%) | 0.25 |
| Diabetes with complications | 11 (19.3%) | 41 (26.5%) | 0.28 |
| Malignancy | 16 (28.1%) | 47 (30.3%) | 0.75 |
| Metastatic solid tumor | 8 (14.0%) | 19 (12.3%) | 0.73 |
| Spinal cord injury | |||
| Healthcare exposures, 30 daysprior to admission | |||
| Hospitalization | 17 (29.8%) | 36 (23.2%) | 0.33 |
| Nursing home | <5 (<8.8%) | <5 (<3.2%) | 0.02 |
| Intensive care | <5 (<8.8%) | 6 (3.9%) | 0.70 |
| Surgery | <5 (<8.8%) | 9 (5.8%) | 1.00 |
| Length of hospital stay, days | |||
| Median (interquartile range) | 43 (16–80) | 31 (13–107) | 0.69 |
| MDR P. aeruginosa culture source | |||
| Respiratory | 21 (36.8%) | 55 (35.5%) | 0.85 |
| Urine | 13 (22.8%) | 80 (51.6%) | 0.0002 |
| Skin and tissue | 10 (17.5%) | 13 (8.4%) | 0.06 |
| Blood | 8 (14.0%) | 14 (9.0%) | 0.29 |
| Bone joint | 7 (12.3%) | <5 (<3.2%) | <0.0001 |
| Intra-abdominal | <5 (<8.8%) | <5 (<3.2%) | 1.00 |
| Other | 5 (8.8%) | <5 (<3.2%) | 0.03 |
| Previous positive P. aeruginosa culture, prior 30 days | 31 (54.4%) | 60 (38.7%) | 0.04 |
| Culture source of prior positive P. aeruginosa | |||
| Respiratory | 14 (24.6%) | 35 (22.6%) | 0.76 |
| Urine | 10 (17.5%) | 15 (9.7%) | 0.12 |
| Skin and tissue | 5 (8.8%) | 6 (3.9%) | 0.17 |
| Blood | 6 (10.5%) | 7 (4.5%) | 0.11 |
| Bone joint | <5 (<8.8%) | <5 (<3.2%) | 0.06 |
| Intra-abdominal | <5 (<8.8%) | <5 (<3.2%) | 1.00 |
| Other | <5 (<8.8%) | <5 (<3.2%) | 0.06 |
| Resistance | |||
| Aminoglycosides | 35 (61.4%) | 82 (52.9%) | 0.27 |
| Carbapenem | 53 (98.2%) | 138 (91.4%) | 0.12 |
| Extended-spectrum | 55 (96.5%) | 138 (89.0%) | 0.09 |
| cephalosporin | |||
| Fluoroquinolone | 52 (91.2%) | 142 (91.6%) | 1.00 |
| Piperacillin/tazobactam | 35 (70.0%) | 120 (88.2%) | 0.003 |
| Treatment Characteristics | Ceftolozane/Tazobactam (n = 57) | Aminoglycosides/ Polymyxins (n = 155) | p-Value |
|---|---|---|---|
| Total number of changes in therapy during hospital admission | |||
| Median (interquartile range) | 7 (3–14) | 6 (3–15) | 0.92 |
| Time to study drug from initial antibiotics during hospital admission, days | |||
| Median (interquartile range) | 13 (4–46) | 9 (3–36) | 0.27 |
| Time to study drug from culture collection, days | |||
| Median (interquartile range) | 3 (1–4) | 3 (2–4) | 0.93 |
| Inpatient antimicrobial duration, days | |||
| Median (interquartile range) | 34 (16–60) | 23 (10–63) | 0.18 |
| Duration of study drug, days | |||
| Median (interquartile range) | 12 (5–18) | 7 (4–14) | 0.005 |
| Number of changes in therapy before the start of study drug | |||
| Median (interquartile range) | 5 (1–10) | 3 (1–8) | 0.13 |
| Number of days from hospital admission to start of study drug | |||
| Median (interquartile range) | 14 (4–48) | 11 (4–46) | 0.36 |
| Time to antipseudomonal antibiotics * from admission, days | |||
| Median (interquartile range) | 0 (−2) | 1 (0–6) | 0.03 |
| Any antibiotics, 30 days prior to the start of study drug | 55 (96.5%) | 144 (92.9%) | 0.33 |
| Previous antibiotics, 30 days to 8 days prior to the start of study drug | |||
| Amikacin | <5 (<8.8%) | 5 (3.2%) | 1.00 |
| Aztreonam | <5 (<8.8%) | <5 (<3.2%) | 0.47 |
| Cefepime | 8 (14.0%) | 20 (12.9%) | 0.83 |
| Ceftazidime | <5 (<8.8%) | <5 (<8.8%) | 0.18 |
| Cilastatin/imipenem | <5 (<8.8%) | 8 (5.2%) | 0.45 |
| Ciprofloxacin | 10 (17.5%) | 15 (9.7%) | 0.11 |
| Daptomycin | 9 (15.8%) | 8 (5.2%) | 0.02 |
| Levofloxacin | 9 (15.8%) | 12 (7.7%) | 0.08 |
| Gentamicin | 6 (10.5%) | 5 (3.2%) | 0.07 |
| Meropenem | 14 (24.6%) | 18 (11.6%) | 0.02 |
| Piperacillin/tazobactam | 20 (35.1%) | 26 (16.8%) | 0.004 |
| Polymyxin B | <5 (<8.8%) | <5 (<3.2%) | 0.57 |
| Sulfamethoxazole/trimethoprim | 7 (12.3%) | 9 (5.8%) | 0.14 |
| Tobramycin | <5 (<8.8%) | <5 (<3.2%) | 0.35 |
| Vancomycin | 24 (42.1%) | 53 (34.2%) | 0.29 |
| Previous antibiotics class, 30 days to 8 days prior to the start of study drug | |||
| Aminoglycosides | 9 (15.8%) | 13 (8.4%) | 0.12 |
| Carbapenem | 15 (26.3%) | 25 (16.1%) | 0.09 |
| Extended-spectrum | 9 (15.8%) | 21 (13.6%) | 0.68 |
| cephalosporin | |||
| Fluoroquinolone | 17 (29.8%) | 25 (16.1%) | 0.03 |
| Piperacillin/tazobactam | 20 (35.1%) | 26 (16.8%) | 0.004 |
| Previous antibiotics, 7 days to 1 day prior to the start of study drug | |||
| Amikacin | 6 (10.5%) | <5 (<3.2%) | 0.01 |
| Aztreonam | <5 (<8.8%) | <5 (<3.2%) | 0.29 |
| Cefepime | 9 (15.8%) | 24 (15.5%) | 0.96 |
| Ceftazidime | 6 (10.5%) | <5 (<3.2%) | 0.03 |
| Cilastatin/imipenem | <5 (<8.8%) | 12 (7.7%) | 0.36 |
| Ciprofloxacin | 5 (8.8%) | 12 (7.7%) | 0.78 |
| Colistin | <5 (<8.8%) | <5 (<3.2%) | 0.06 |
| Daptomycin | 7 (12.3%) | 8 (5.2%) | 0.13 |
| Levofloxacin | 5 (8.8%) | 19 (12.3%) | 0.48 |
| Gentamicin | <5 (<8.8%) | <5 (<3.2%) | 0.21 |
| Meropenem | 16 (28.1%) | 26 (16.8%) | 0.07 |
| Piperacillin/tazobactam | 19 (33.3%) | 38 (24.5%) | 0.20 |
| Polymyxin B | <5 (<8.8%) | 7 (4.5%) | 0.68 |
| Sulfamethoxazole/trimethoprim | <5 (<8.8%) | 7 (4.5%) | 0.73 |
| Tobramycin | <5 (<8.8%) | <5 (<3.2%) | 0.02 |
| Vancomycin | 27 (47.4%) | 72 (46.5%) | 0.91 |
| Previous antibiotics class, 7 days to 1 day prior to the start of study drug | |||
| Aminoglycosides | 12 (21.1%) | 8 (5.2%) | 0.0004 |
| Carbapenem | 18 (31.6%) | 37 (23.9%) | 0.26 |
| Extended-spectrum | 15 (26.3%) | 28 (18.1%) | 0.18 |
| cephalosporin | |||
| Fluoroquinolone | 10 (17.5%) | 30 (19.4%) | 0.75 |
| Piperacillin/tazobactam | 19 (33.3%) | 38 (24.5%) | 0.20 |
| Concomitant antibiotics from start of study drug up to 15 days | |||
| Aztreonam | <5 (<8.8%) | 5 (3.2%) | 1.00 |
| Cefepime | 9 (15.8%) | 41 (26.5%) | 0.10 |
| Ceftazidime | <5 (<8.8%) | 10 (6.5%) | 1.00 |
| Imipenem | <5 (<8.8%) | 17 (11.0%) | 0.09 |
| Ciprofloxacin | <5 (<8.8%) | 13 (8.4%) | 0.36 |
| Daptomycin | 6 (10.5%) | 13 (8.4%) | 0.63 |
| Levofloxacin | <5 (<8.8%) | 18 (11.6%) | 0.07 |
| Meropenem | 9 (15.8%) | 47 (30.3%) | 0.03 |
| Piperacillin/tazobactam | 14 (24.6%) | 42 (27.1%) | 0.71 |
| Sulfamethoxazole/trimethoprim | <5 (<8.8%) | <5 (<3.2%) | 0.39 |
| Concomitant antibiotics class, start of study drug up to 15 days | |||
| Carbapenem | 11 (19.3%) | 60 (38.7%) | 0.008 |
| Extended-spectrum | 11 (19.3%) | 47 (30.3%) | 0.11 |
| cephalosporin | |||
| Fluoroquinolone | <5 (<8.8%) | 30 (19.4%) | 0.03 |
| Piperacillin/tazobactam | 14 (24.6%) | 42 (27.1%) | 0.71 |
| Outcomes | No. of Events/No. of Patients (%) Ceftolozane/Aminoglycosides/ Tazobactam Polymyxins | Adjusted Odds Ratio 1 (95% Confidence Interval) | |
|---|---|---|---|
| Inpatient mortality | 9/57 (15.8%) | 43/155 (27.7%) | 0.39 (0.16–0.93) 5 |
| Readmission within 30 days of discharge | 12/48 (25.0%) | 31/112 (27.7%) | 0.87 (0.40–1.89) 6 |
| Persistent positive culture 2 | 7/31 (22.6%) | 39/93 (41.9%) | 0.38 (0.13–1.06) 7 |
| Microbiological clearance 3 | 13/42 (31.0%) | 33/108 (30.6%) | 0.88 (0.35–2.21) 8 |
| Acute kidney injury 4 | 8/48 (16.7%) | 16/129 (12.4%) | 0.86 (0.32–2.33) 9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Caffrey, A.R.; Appaneal, H.J.; Liao, J.X.; Piehl, E.C.; Lopes, V.; Dillon, R.J.; Puzniak, L.A.; LaPlante, K.L. The Comparative Effectiveness of Ceftolozane/Tazobactam versus Aminoglycoside- or Polymyxin-Based Regimens in Multi-Drug-Resistant Pseudomonas aeruginosa Infections. Antibiotics 2022, 11, 626. https://doi.org/10.3390/antibiotics11050626
Caffrey AR, Appaneal HJ, Liao JX, Piehl EC, Lopes V, Dillon RJ, Puzniak LA, LaPlante KL. The Comparative Effectiveness of Ceftolozane/Tazobactam versus Aminoglycoside- or Polymyxin-Based Regimens in Multi-Drug-Resistant Pseudomonas aeruginosa Infections. Antibiotics. 2022; 11(5):626. https://doi.org/10.3390/antibiotics11050626
Chicago/Turabian StyleCaffrey, Aisling R., Haley J. Appaneal, J. Xin Liao, Emily C. Piehl, Vrishali Lopes, Ryan J. Dillon, Laura A. Puzniak, and Kerry L. LaPlante. 2022. "The Comparative Effectiveness of Ceftolozane/Tazobactam versus Aminoglycoside- or Polymyxin-Based Regimens in Multi-Drug-Resistant Pseudomonas aeruginosa Infections" Antibiotics 11, no. 5: 626. https://doi.org/10.3390/antibiotics11050626
APA StyleCaffrey, A. R., Appaneal, H. J., Liao, J. X., Piehl, E. C., Lopes, V., Dillon, R. J., Puzniak, L. A., & LaPlante, K. L. (2022). The Comparative Effectiveness of Ceftolozane/Tazobactam versus Aminoglycoside- or Polymyxin-Based Regimens in Multi-Drug-Resistant Pseudomonas aeruginosa Infections. Antibiotics, 11(5), 626. https://doi.org/10.3390/antibiotics11050626






