Prescription Patterns of Drugs Given to Hospitalized COVID-19 Patients: A Cross-Sectional Study in Colombia
Abstract
:1. Introduction
2. Results
Comparisons of Drug Use
3. Discussion
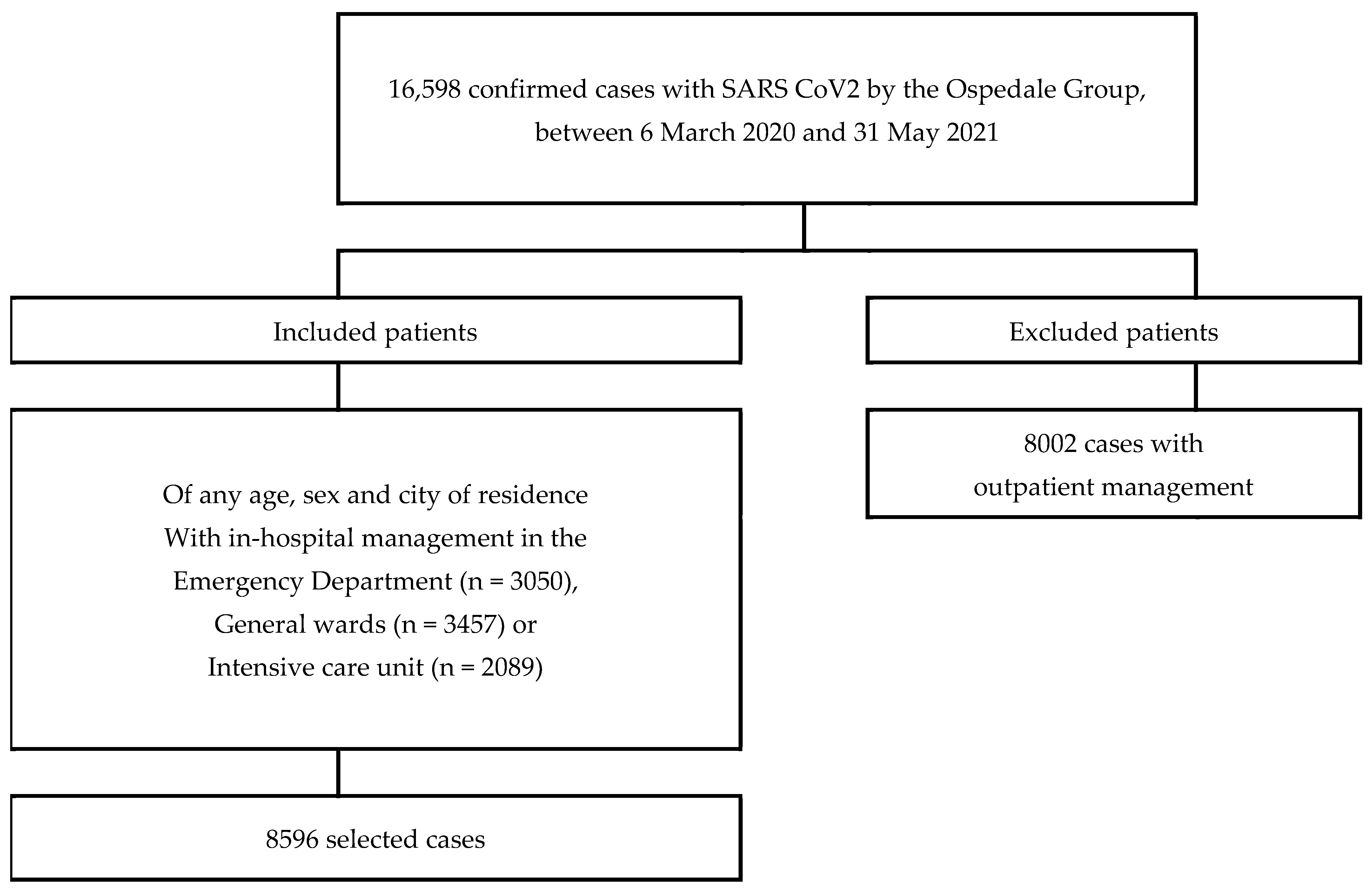
4. Materials and Methods
- 1.
- Sociodemographic: sex, age (<18 years, 18–39 years, 40–64 years, 65 or more years), and city. The place of care was categorized by department and region of Colombia, taking into account the classification of the National Administrative Department of Statistics (DANE) of Colombia, as follows:
- Caribbean region: Atlántico (Barranquilla), Bolívar (Cartagena);
- Central region: Caldas (Manizales), Quindío (Armenia), Risaralda (Pereira);
- Bogotá-Cundinamarca region: Bogotá;
- Pacific region: Cauca (Popayán), Valle del Cauca (Cali).
- 2.
- Clinical: comorbidities (arterial hypertension, chronic obstructive pulmonary disease, obesity, dyslipidemia, diabetes mellitus, depression, anxiety, chronic kidney disease, asthma, heart failure, ischemic heart disease, among others) and clinical manifestations (cough, dyspnea, fever, fatigue, odynophagia, precordial pain, asthenia/adynamia, among others).
- 3.
- Place of care: emergency room, general ward, or ICU.
- 4.
- Supplemental oxygen: oxygen requirement, mechanical ventilation, and need for tracheostomy.
- 5.
- Medications that have been used in patients with COVID-19 include systemic corticosteroids (dexamethasone, hydrocortisone, methylprednisolone, prednisolone, betamethasone, prednisone), anticoagulants (unfractionated heparin, low molecular weight heparins), antimalarials (chloroquine, hydroxychloroquine), ivermectin, lopinavir/ritonavir, colchicine, tocilizumab, nitazoxanide, tofacitinib and remdesivir (not available in the country).
- 6.
- Comedications: they were grouped into the following categories: (a) antidiabetics, (b) antihypertensives and diuretics, (c) lipid-lowering drugs; (d) antiulcer drugs, (e) antidepressants, (f) anxiolytics and hypnotics, (g) thyroid hormone, (h) antipsychotics, (i) antiepileptics, (j) antiarrhythmics, (k) antihistamines, (l) antiplatelets, (m) analgesics and anti-inflammatories, (n) systemic antibiotics, (o) bronchodilators and inhaled corticosteroids, (p) vasopressors and inotropics, (q) muscle relaxants, (r) hypnotics and sedatives, and (s) others.
Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Harapan, H.; Itoh, N.; Yufika, A.; Winardi, W.; Keam, S.; Te, H.; Megawati, D.; Hayati, Z.; Wagner, A.L.; Mudatsir, M. Coronavirus disease 2019 (COVID-19): A literature review. J. Infect. Public Health 2020, 13, 667–673. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Johns Hopkins University Medicine. Coronavirus Resource Center. Available online: https://coronavirus.jhu.edu/map.html (accessed on 11 October 2021).
- Instituto Nacional de Salud. Corononavirus (COVID-19) en Colombia. Reporte 10 de Octubre de 2021. Available online: https://www.ins.gov.co/Noticias/paginas/coronavirus.aspx (accessed on 11 October 2021).
- Serafim, R.B.; Póvoa, P.; Souza-Dantas, V.; Kalil, A.C.; Salluh, J.I.F. Clinical course and outcomes of critically ill patients with COVID-19 infection: A systematic review. Clin. Microbiol. Infect. 2021, 27, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Tan, E.; Song, J.; Deane, A.M.; Plummer, M.P. Global Impact of Coronavirus Disease 2019 Infection Requiring Admission to the ICU: A Systematic Review and Meta-analysis. Chest 2021, 159, 524–536. [Google Scholar] [CrossRef]
- Wu, S.S.; Zhou, Q.X.; Zeng, X.Y.; Zhang, J.X.; Yang, Z.R.; Yang, Q.Q.; Zhang, Z.L.; Chen, Y.H.; Sun, F.; Zhan, S.Y. Comparative effectiveness and safety of 32 pharmacological interventions recommended by guidelines for coronavirus disease 2019: A systematic review and network meta-analysis combining 66 trials. Chin. Med. J. 2021, 134, 1920–1929. [Google Scholar] [CrossRef] [PubMed]
- Abeldaño Zuñiga, R.A.; Coca, S.M.; Abeldaño, G.F.; González-Villoria, R.A.M. Clinical effectiveness of drugs in hospitalized patients with COVID-19: A systematic review and meta-analysis. Ther. Adv. Respir. Dis. 2021, 15, 17534666211007214. [Google Scholar] [CrossRef]
- Rajaiah, R.; Abhilasha, K.V.; Shekar, M.A.; Vogel, S.N.; Vishwanath, B.S. Evaluation of mechanisms of action of re-purposed drugs for treatment of COVID-19. Cell Immunol. 2020, 358, 104240. [Google Scholar] [CrossRef]
- Yousefi, H.; Mashouri, L.; Okpechi, S.C.; Alahari, N.; Alahari, S.K. Repurposing existing drugs for the treatment of COVID-19/SARS-CoV-2 infection: A review describing drug mechanisms of action. Biochem. Pharmacol. 2021, 183, 114296. [Google Scholar] [CrossRef]
- Diaz-Arocutipa, C.; Brañez-Condorena, A.; Hernandez, A.V. QTc prolongation in COVID-19 patients treated with hydroxychloroquine, chloroquine, azithromycin, or lopinavir/ritonavir: A systematic review and meta-analysis. Pharmacoepidemiol. Drug Saf. 2021, 30, 694–706. [Google Scholar] [CrossRef]
- Awortwe, C.; Cascorbi, I. Meta-analysis on outcome-worsening comorbidities of COVID-19 and related potential drug-drug interactions. Pharmacol. Res. 2020, 161, 105250. [Google Scholar] [CrossRef]
- Ruíz-Quiñonez, J.A.; Guzmán-Priego, C.G.; Nolasco-Rosales, G.A.; Tovilla-Zarate, C.A.; Flores-Barrientos, O.I.; Narváez-Osorio, V.; Baeza-Flores, G.D.C.; Gonzalez-Castro, T.B.; López-Brito, C.R.; Denis-García, C.A.; et al. Features of patients that died for COVID-19 in a hospital in the south of Mexico: A observational cohort study. PLoS ONE 2021, 16, e0245394. [Google Scholar] [CrossRef] [PubMed]
- García-Posada, M.; Aruachan-Vesga, S.; Mestra, D.; Humánez, K.; Serrano-Coll, H.; Cabrales, H.; Faccini, Á.; Mattar, S. Clinical outcomes of patients hospitalized for COVID-19 and evidence-based on the pharmacological management reduce mortality in a region of the Colombian Caribbean. J. Infect. Public Health 2021, 14, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Stroever, S.J.; Ostapenko, D.; Scatena, R.; Pusztai, D.; Coritt, L.; Frimpong, A.A.; Nee, P. Medication Use Among Patients With COVID-19 in a Large, National Dataset: Cerner Real-World Data™. Clin. Ther. 2021, 43, e173–e196. [Google Scholar] [CrossRef]
- Watanabe, J.H.; Kwon, J.; Nan, B.; Abeles, S.R.; Jia, S.; Mehta, S.R. Medication Use Patterns in Hospitalized Patients With COVID-19 in California During the Pandemic. JAMA Netw. Open 2021, 4, e2110775. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Vélez, C.; Urrunaga-Pastor, D.; Romero-Cerdán, A.; Peña-Sánchez, E.R.; Mogollon, J.L.F.; Chafloque, J.D.C.; Ascoy, G.C.M.; Benites-Zapata, V.A. Risk factors for mortality in hospitalized patients with COVID-19 from three hospitals in Peru: A retrospective cohort study. F1000Research 2021, 10, 224. [Google Scholar] [CrossRef]
- Hueda-Zavaleta, M.; Copaja-Corzo, C.; Bardales-Silva, F.; Flores-Palacios, R.; Barreto-Rocchetti, L.; Benites-Zapata, V.A. Factors associated with mortality due to COVID-19 in patients from a public hospital in Tacna, Peru. Rev. Peru Med. Exp. Salud Publica 2021, 38, 214–223. [Google Scholar] [CrossRef] [PubMed]
- COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: A prospective cohort study. Intensive Care Med. 2021, 47, 60–73. [Google Scholar] [CrossRef]
- Murthy, S.; Archambault, P.M.; Atique, A.; Carrier, F.M.; Cheng, M.P.; Codan, C.; Daneman, N.; Dechert, W.; Douglas, S.; Fiest, K.M.; et al. Characteristics and outcomes of patients with COVID-19 admitted to hospital and intensive care in the first phase of the pandemic in Canada: A national cohort study. CMAJ Open 2021, 9, E181–E188. [Google Scholar] [CrossRef]
- Laake, J.H.; Buanes, E.A.; Småstuen, M.C.; Kvåle, R.; Olsen, B.F.; Rustøen, T.; Strand, K.; Sørensen, V.; Hofsø, K. Characteristics, management and survival of ICU patients with coronavirus disease-19 in Norway, March-June 2020. A prospective observational study. Acta Anaesthesiol. Scand. 2021, 65, 618–628. [Google Scholar] [CrossRef]
- Wang, Y.; Yao, S.; Liu, X.; Cao, Y.; Wang, Y.; Xie, M. Risk Factors of Coronavirus Disease 2019-Related Mortality and Optimal Treatment Regimens: A Retrospective Study. Med. Sci. Monit. 2021, 27, e926751. [Google Scholar] [CrossRef]
- Sun, F.; Kou, H.; Wang, S.; Lu, Y.; Zhao, H.; Li, W.; Zhou, Q.; Jiang, Q.; Cheng, Y.; Yang, K.; et al. An analytical study of drug utilization, disease progression, and adverse events among 165 COVID-19 patients. Ann. Transl. Med. 2021, 9, 306. [Google Scholar] [CrossRef]
- Best, J.H.; Kong, A.M.; Kaplan-Lewis, E.; Brawley, O.W.; Baden, R.; Zazzali, J.L.; Miller, K.S.; Loveless, J.; Jariwala-Parikh, K.; Mohan, S.V. Treatment patterns in US patients hospitalized with COVID-19 and pulmonary involvement. J. Med. Virol. 2021, 93, 5367–5375. [Google Scholar] [CrossRef]
- Alvarez, A.; Cabia, L.; Trigo, C.; Bandrés, A.C.; Bestué, M. Prescription profile in patients with SARS-CoV-2 infection hospitalised in Aragon, Spain. Eur. J. Hosp. Pharm. 2020, 156, 88–89. [Google Scholar] [CrossRef]
- Akhtar, H.; Akhtar, S.; Rahman, F.U.; Afridi, M.; Khalid, S.; Ali, S.; Akhtar, N.; Khader, Y.S.; Ahmad, H.; Khan, M.M. An Overview of the Treatment Options Used for the Management of COVID-19 in Pakistan: Retrospective Observational Study. JMIR Public Health Surveill. 2021, 7, e28594. [Google Scholar] [CrossRef]
- Gadi, N.; Wu, S.C.; Spihlman, A.P.; Moulton, V.R. What’s Sex Got to Do With COVID-19? Gender-Based Differences in the Host Immune Response to Coronaviruses. Front. Immunol. 2020, 11, 2147. [Google Scholar]
- Ortonobes Roig, S.; Soler-Blanco, N.; Torrente Jiménez, I.; Van den Eynde Otero, E.; Moreno-Ariño, M.; Gómez-Valent, M. Variables clínicas y farmacológicas de pacientes nonagenarios hospitalizados por COVID-19 [Clinical and pharmacological data in COVID-19 hospitalized nonagenarian patients]. Rev. Esp. Quimioter. 2021, 34, 145–150. [Google Scholar] [CrossRef]
- Huh, K.; Ji, W.; Kang, M.; Hong, J.; Bae, G.H.; Lee, R.; Na, Y.; Jung, J. Association of prescribed medications with the risk of COVID-19 infection and severity among adults in South Korea. Int. J. Infect. Dis. 2021, 104, 7–14. [Google Scholar] [CrossRef]
- Dorjee, K.; Kim, H.; Bonomo, E.; Dolma, R. Prevalence and predictors of death and severe disease in patients hospitalized due to COVID-19: A comprehensive systematic review and meta-analysis of 77 studies and 38,000 patients. PLoS ONE 2020, 15, e0243191. [Google Scholar] [CrossRef]
- Thakur, B.; Dubey, P.; Benitez, J.; Torres, J.P.; Reddy, S.; Shokar, N.; Aung, K.; Mukherjee, D.; Dwivedi, A.K. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci. Rep. 2021, 11, 8562. [Google Scholar] [CrossRef]
- Eleni, M.; Evangelia, M.; Eleftheria, K.; Vasilios, V.; Vana, S.; Vissaria, S.; Evangelos, B.; Ioannis, K. Clinical features and outcomes of hospitalized COVID-19 patients in a low burden region. Pathog Glob. Health 2021, 115, 243–249. [Google Scholar]
- Pinzón, M.A.; Cardona Arango, D.; Betancur, J.F.; Ortiz, S.; Holguín, H.; Arias Arias, C.; Muñoz Palacio, B.J.; Amarillo, M.; Llano, J.F.; Montoya, P. Clinical outcome of patients with COVID-19 Pneumonia treated with corticosteroids and colchicine in Colombia. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 66. [Google Scholar] [CrossRef] [PubMed]
- Machado-Alba, J.E.; Valladales-Restrepo, L.F.; Machado-Duque, M.E.; Gaviria-Mendoza, A.; Sánchez-Ramírez, N.; Usma-Valencia, A.F.; Rodríguez-Martínez, E.; Rengifo-Franco, E.; Forero-Supelano, V.H.; Gómez-Ramirez, D.M.; et al. Factors associated with admission to the intensive care unit and mortality in patients with COVID-19, Colombia. PLoS ONE 2021, 16, e0260169. [Google Scholar] [CrossRef] [PubMed]
- RECOVERY Collaborative Group. Dexamethasone in Hospitalized Patients with Covid-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- Bhimraj, A.; Morgan, R.L.; Shumaker, A.H.; Lavergne, V.; Baden, L.; Cheng, V.C.C.; Edwards, K.M.; Gandhi, R.; Muller, W.J.; O’Horo, J.C.; et al. Infectious Diseases Society of America Guidelines on the Treatment and Management of Patients with COVID-19. Infectious Diseases Society of America 2021, Version 5.1.1. Available online: https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/ (accessed on 14 September 2021).
- National Institutes of Health. COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. Available online: https://www.covid19treatmentguidelines.nih.gov/ (accessed on 6 October 2021).
- World Health Organization. COVID-19 Clinical Management: Living Guidance. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-1 (accessed on 6 October 2021).
- Saavedra Trujillo, C.H. Consenso Colombiano De Atención, Diagnóstico Y Manejo De La Infección Por Sars-Cov-2/COVID-19 En Establecimientos De Atención De La Salud: Recomendaciones Basadas En Consenso De Expertos E Informadas En La Evidencia ACIN-ISTS. Terc. Edición Infect. 2021, 25, 262–292. [Google Scholar]
- Colchicine. In Drug Point Summary; [database on the Internet]; IBM Corporation: Greenwood Village, CO, USA, 2021; Available online: www.micromedexsolutions.com (accessed on 8 October 2021).
- Nawangsih, E.N.; Kusmala, Y.Y.; Rakhmat, I.I.; Handayani, D.R.; Juliastuti, H.; Wibowo, A.; Lim, M.A.; Pranata, R. Colchicine and mortality in patients with coronavirus disease 2019 (COVID-19) pneumonia: A systematic review, meta-analysis, and meta-regression. Int. Immunopharmacol. 2021, 96, 107723. [Google Scholar] [CrossRef] [PubMed]
- Elshafei, M.N.; El-Bardissy, A.; Khalil, A.; Danjuma, M.; Mubasher, M.; Abubeker, I.Y.; Mohamed, M.F. Colchicine use might be associated with lower mortality in COVID-19 patients: A meta-analysis. Eur. J. Clin. Investig. 2021, 51, e13645. [Google Scholar] [CrossRef]
- Golpour, M.; Mousavi, T.; Alimohammadi, M.; Mosayebian, A.; Shiran, M.; Alizadeh Navaei, R.; Rafiei, A. The effectiveness of Colchicine as an anti-inflammatory drug in the treatment of coronavirus disease 2019: Meta-analysis. Int. J. Immunopathol. Pharmacol. 2021, 35, 20587384211031763. [Google Scholar] [CrossRef]
- Ding, J.; Liu, W.; Guan, H.; Feng, Y.; Bao, Y.; Li, H.; Wang, X.; Zhou, Z.; Chen, Z. interval in hospitalized patients with coronavirus disease 2019: Focus on drugs therapy. Medicine (Baltimore) 2021, 100, e26538. [Google Scholar] [CrossRef]
- Valladales-Restrepo, L.F.; Constain-Mosquera, C.A.; Álvarez-Amaya, V.; Machado-Alba, J.E. Study of prescription-indication of tetracyclines in a population in Colombia. Fundam. Clin. Pharmacol. 2021. Online ahead of print. [Google Scholar] [CrossRef]
- Machado-Alba, J.E.; Valladales-Restrepo, L.F.; Gaviria-Mendoza, A.; Machado-Duque, M.E.; Figueras, A. Patterns of Antibiotic Prescription in Colombia: Are There Differences between Capital Cities and Municipalities? Antibiotics 2020, 9, 389. [Google Scholar] [CrossRef]
| Variables | Men | Women | p | ||
|---|---|---|---|---|---|
| n = 4583 | % | n = 4013 | % | ||
| Age, median (IQR) | 55.6 (41.0–69.0) | 50.2 (33.0–67.0) | <0.001 * | ||
| Geographic region | |||||
| Pacific region | 1588 | 34.6 | 1130 | 28.2 | <0.001 |
| Central region | 1218 | 26.6 | 1185 | 29.5 | 0.002 |
| Caribbean region | 949 | 20.7 | 807 | 20.1 | 0.493 |
| Bogota-Cundinamarca region | 828 | 18.1 | 891 | 22.2 | <0.001 |
| Comorbidities | |||||
| Arterial hypertension | 1483 | 32.4 | 1302 | 32.4 | 0.932 |
| Diabetes mellitus | 646 | 14.1 | 521 | 13.0 | 0.133 |
| Chronic obstructive pulmonary disease | 186 | 4.1 | 140 | 3.5 | 0.168 |
| Chronic kidney disease | 177 | 3.9 | 114 | 2.8 | 0.009 |
| Dyslipidemia | 139 | 3.0 | 124 | 3.1 | 0.878 |
| Place of care | |||||
| Emergency department or observation | 1436 | 31.3 | 1614 | 40.2 | <0.001 |
| Hospitalization in general wards | 1819 | 39.7 | 1638 | 40.8 | 0.288 |
| Intensive care unit | 1328 | 29.0 | 761 | 19.0 | <0.001 |
| Treatment | |||||
| Supplemental oxygen | 2879 | 62.8 | 1963 | 48.9 | <0.001 |
| Invasive mechanical ventilation | 998 | 21.8 | 607 | 15.1 | <0.001 |
| Tracheostomy | 54 | 1.2 | 17 | 0.4 | <0.001 |
| Corticosteroids | 3107 | 67.8 | 2358 | 58.8 | <0.001 |
| Dexamethasone | 2916 | 63.6 | 2179 | 54.3 | <0.001 |
| Methylprednisolone | 521 | 11.4 | 372 | 9.3 | 0.001 |
| Hydrocortisone | 244 | 5.3 | 146 | 3.6 | <0.001 |
| Betamethasone | 84 | 1.8 | 62 | 1.5 | 0.303 |
| Prednisolone | 40 | 0.9 | 42 | 1.0 | 0.408 |
| Prednisone | 2 | 0.0 | 44 | 1.1 | <0.001 |
| Parenteral anticoagulants | 3151 | 68.8 | 2149 | 53.6 | <0.001 |
| Low molecular weight heparins | 3049 | 66.5 | 2047 | 51.0 | <0.001 |
| Unfractionated heparin | 600 | 13.1 | 395 | 9.8 | <0.001 |
| Colchicine | 670 | 14.6 | 428 | 10.7 | <0.001 |
| Azithromycin | 513 | 11.2 | 248 | 6.2 | <0.001 |
| Ivermectin | 351 | 7.7 | 198 | 4.9 | <0.001 |
| Hydroxychloroquine | 46 | 1.0 | 20 | 0.5 | 0.007 |
| Chloroquine | 28 | 0.6 | 20 | 0.5 | 0.485 |
| Lopinavir-Ritonavir | 9 | 0.2 | 6 | 0.1 | 0.603 |
| Tocilizumab | 7 | 0.2 | 2 | 0.0 | 0.188 ** |
| Comedications | |||||
| Analgesics-anti-inflammatories | 3301 | 72.0 | 2913 | 72.6 | 0.561 |
| Antiulcer | 2968 | 64.8 | 2111 | 52.6 | <0.001 |
| Systemic antibiotics | 2903 | 63.3 | 2016 | 50.2 | <0.001 |
| Antihypertensives and diuretics | 1771 | 38.6 | 1305 | 32.5 | <0.001 |
| Hypno-sedatives | 1181 | 25.8 | 770 | 19.2 | <0.001 |
| Mortality | 812 | 17.7 | 480 | 12.0 | <0.001 |
| Variables | <18 Years | 18–39 Years | 40–64 Years | ≥65 Years | ||||
|---|---|---|---|---|---|---|---|---|
| n = 179 | % | n = 2236 | % | n = 3457 | % | n = 2541 | % | |
| Men | 77 | 43.0 | 949 | 42.4 | 2031 | 58.8 | 1440 | 56.7 |
| Geographic region | ||||||||
| Pacific region | 35 | 19.6 | 458 | 20.5 | 1159 | 33.5 | 1061 | 41.8 |
| Central region | 36 | 20.1 | 703 | 31.4 | 826 | 23.9 | 670 | 26.4 |
| Caribbean region | 53 | 29.6 | 503 | 22.5 | 750 | 21.7 | 447 | 17.6 |
| Bogota-Cundinamarca region | 55 | 30.7 | 572 | 25.6 | 722 | 20.9 | 363 | 14.3 |
| Comorbidities | ||||||||
| Arterial hypertension | 9 | 5.0 | 245 | 11.0 | 1060 | 30.7 | 1462 | 57.5 |
| Diabetes mellitus | 3 | 1.7 | 67 | 3.0 | 474 | 13.7 | 617 | 24.3 |
| Chronic obstructive pulmonary disease | 0 | 0.0 | 3 | 0.1 | 47 | 1.4 | 268 | 10.5 |
| Chronic kidney disease | 0 | 0.0 | 13 | 0.6 | 100 | 2.9 | 178 | 7.0 |
| Dyslipidemia | 0 | 0.0 | 20 | 0.9 | 150 | 4.3 | 93 | 3.7 |
| Place of care | ||||||||
| Emergency department or observation | 97 | 54.2 | 1287 | 57.6 | 1185 | 34.3 | 456 | 17.9 |
| Hospitalization in general wards | 57 | 31.8 | 763 | 34.1 | 1413 | 40.9 | 1085 | 42.7 |
| Intensive care unit | 25 | 14.0 | 186 | 8.3 | 859 | 24.8 | 1000 | 39.4 |
| Treatment | ||||||||
| Supplemental oxygen | 47 | 26.3 | 585 | 26.2 | 2072 | 59.9 | 2027 | 79.8 |
| Invasive mechanical ventilation | 10 | 5.6 | 138 | 6.2 | 624 | 18.1 | 792 | 31.2 |
| Tracheostomy | 0 | 0.0 | 7 | 0.3 | 20 | 0.6 | 42 | 1.7 |
| Corticosteroids | 42 | 23.5 | 974 | 43.6 | 2327 | 67.3 | 1995 | 78.5 |
| Dexamethasone | 29 | 16.2 | 870 | 38.9 | 2198 | 63.6 | 1872 | 73.7 |
| Methylprednisolone | 8 | 4.5 | 120 | 5.4 | 336 | 9.7 | 405 | 15.9 |
| Hydrocortisone | 6 | 3.4 | 53 | 2.4 | 157 | 4.5 | 165 | 6.5 |
| Betamethasone | 1 | 0.6 | 20 | 0.9 | 51 | 1.5 | 70 | 2.8 |
| Prednisolone | 0 | 0.0 | 14 | 0.6 | 28 | 0.8 | 36 | 1.4 |
| Prednisone | 1 | 0.6 | 40 | 1.8 | 3 | 0.1 | 1 | 0.0 |
| Parenteral anticoagulants | 12 | 6.7 | 626 | 28.0 | 2330 | 67.4 | 2218 | 87.3 |
| Low molecular weight heparins | 12 | 6.7 | 608 | 27.2 | 2267 | 65.6 | 2119 | 83.4 |
| Unfractionated heparin | 2 | 1.1 | 64 | 2.9 | 322 | 9.3 | 556 | 21.9 |
| Colchicine | 1 | 0.6 | 101 | 4.5 | 503 | 14.6 | 440 | 17.3 |
| Azithromycin | 3 | 1.7 | 70 | 3.1 | 372 | 10.8 | 314 | 12.4 |
| Ivermectin | 3 | 1.7 | 63 | 2.8 | 247 | 7.1 | 236 | 9.3 |
| Hydroxychloroquine | 0 | 0.0 | 12 | 0.5 | 37 | 1.1 | 17 | 0.7 |
| Chloroquine | 0 | 0.0 | 8 | 0.4 | 30 | 0.9 | 10 | 0.4 |
| Lopinavir-Ritonavir | 0 | 0.0 | 4 | 0.2 | 7 | 0.2 | 4 | 0.2 |
| Tocilizumab | 0 | 0.0 | 2 | 0.1 | 5 | 0.1 | 2 | 0.1 |
| Comedications | ||||||||
| Analgesics-anti-inflammatories | 91 | 50.8 | 1649 | 73.7 | 2600 | 75.2 | 1733 | 68.2 |
| Antiulcer | 31 | 17.3 | 724 | 32.4 | 2176 | 62.9 | 2038 | 80.2 |
| Systemic antibiotics | 68 | 38.0 | 699 | 31.3 | 2102 | 60.8 | 1956 | 77.0 |
| Antihypertensives and diuretics | 10 | 5.6 | 217 | 9.7 | 1129 | 32.7 | 1653 | 65.1 |
| Hypno-sedatives | 14 | 7.8 | 200 | 8.9 | 750 | 21.7 | 937 | 36.9 |
| Mortality | 3 | 1.7 | 52 | 2.3 | 418 | 12.1 | 810 | 31.9 |
| Variables | Pacific Region | Central Region | Caribbean Region | Bogota-Cundinamarca Region | ||||
|---|---|---|---|---|---|---|---|---|
| n = 2718 | % | n = 2403 | % | n = 1756 | % | n = 1719 | % | |
| Age, median (IQR) | 59.0 (44.0–72.0) | 51.0 (34.0–68.0) | 51.0 (36.0–65.0) | 47.0 (32.0–62.0) | ||||
| Men | 1588 | 58.4 | 1218 | 50.7 | 949 | 54.0 | 828 | 48.2 |
| Comorbidities | ||||||||
| Arterial hypertension | 852 | 31.3 | 864 | 36.0 | 660 | 37.6 | 409 | 23.8 |
| Diabetes mellitus | 405 | 11.9 | 315 | 13.1 | 290 | 16.5 | 157 | 9.1 |
| Chronic obstructive pulmonary disease | 114 | 4.2 | 138 | 5.7 | 30 | 1.7 | 44 | 2.6 |
| Chronic kidney disease | 121 | 4.5 | 59 | 2.5 | 73 | 4.2 | 38 | 2.2 |
| Dyslipidemia | 80 | 2.9 | 113 | 4.7 | 41 | 2.3 | 29 | 1.7 |
| Place of care | ||||||||
| Emergency department or observation | 774 | 28.5 | 713 | 29.7 | 408 | 23.2 | 1155 | 67.2 |
| Hospitalization in general wards | 949 | 34.9 | 1330 | 55.3 | 835 | 47.6 | 343 | 20.0 |
| Intensive care unit | 995 | 36.6 | 360 | 15.0 | 513 | 29.2 | 221 | 12.9 |
| Treatment | ||||||||
| Supplemental oxygen | 1859 | 68.4 | 1304 | 54.3 | 900 | 51.3 | 779 | 45.3 |
| Invasive mechanical ventilation | 657 | 24.2 | 465 | 19.4 | 289 | 16.5 | 194 | 11.3 |
| Tracheostomy | 50 | 1.8 | 18 | 0.7 | 3 | 0.2 | 0 | 0.0 |
| Corticosteroids | 1865 | 68.6 | 1600 | 66.6 | 1048 | 59.7 | 952 | 55.4 |
| Dexamethasone | 1772 | 65.2 | 1519 | 63.2 | 883 | 50.3 | 921 | 53.6 |
| Methylprednisolone | 294 | 10.8 | 329 | 13.7 | 223 | 12.7 | 47 | 2.7 |
| Hydrocortisone | 146 | 5.4 | 103 | 4.3 | 115 | 6.5 | 26 | 1.5 |
| Betamethasone | 2 | 0.1 | 13 | 0.5 | 23 | 1.3 | 8 | 0.5 |
| Prednisolone | 34 | 1.3 | 88 | 3.7 | 6 | 0.3 | 18 | 1.0 |
| Prednisone | 35 | 1.3 | 38 | 1.3 | 3 | 0.2 | 6 | 0.3 |
| Parenteral anticoagulants | 1991 | 73.3 | 1337 | 55.6 | 1125 | 64.1 | 847 | 49.3 |
| Low molecular weight heparins | 1939 | 71.3 | 1219 | 50.7 | 1116 | 63.6 | 822 | 47.8 |
| Unfractionated heparin | 512 | 18.8 | 357 | 14.9 | 37 | 2.1 | 89 | 5.2 |
| Colchicine | 457 | 16.8 | 374 | 15.6 | 240 | 13.7 | 27 | 1.6 |
| Azithromycin | 690 | 25.4 | 9 | 0.4 | 62 | 3.5 | 0 | 0.0 |
| Ivermectin | 483 | 17.8 | 49 | 2.0 | 15 | 0.9 | 2 | 0.1 |
| Hydroxychloroquine | 17 | 0.6 | 4 | 0.2 | 40 | 2.3 | 5 | 0.3 |
| Chloroquine | 38 | 1.4 | 9 | 0.4 | 1 | 0.1 | 0 | 0.0 |
| Lopinavir-Ritonavir | 6 | 0.2 | 6 | 0.2 | 3 | 0.2 | 0 | 0.0 |
| Tocilizumab | 4 | 0.1 | 0 | 0.0 | 5 | 0.3 | 0 | 0.0 |
| Comedications | ||||||||
| Analgesics-anti-inflammatories | 2013 | 74.1 | 1841 | 76.6 | 1208 | 68.8 | 1152 | 67.0 |
| Antiulcer | 1999 | 73.5 | 1390 | 57.8 | 1036 | 59.0 | 654 | 38.0 |
| Systemic antibiotics | 1727 | 63.5 | 1241 | 51.6 | 1239 | 70.6 | 712 | 41.4 |
| Antihypertensives and diuretics | 1242 | 45.7 | 865 | 36.0 | 552 | 31.4 | 417 | 24.3 |
| Hypno-sedatives | 799 | 29.4 | 575 | 23.9 | 363 | 20.7 | 214 | 12.4 |
| Mortality | 567 | 20.9 | 196 | 8.2 | 314 | 17.9 | 215 | 12.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Valladales-Restrepo, L.F.; Giraldo-Correa, J.A.; Aristizábal-Carmona, B.S.; Constain-Mosquera, C.A.; Sabogal-Ortiz, A.; Machado-Alba, J.E. Prescription Patterns of Drugs Given to Hospitalized COVID-19 Patients: A Cross-Sectional Study in Colombia. Antibiotics 2022, 11, 333. https://doi.org/10.3390/antibiotics11030333
Valladales-Restrepo LF, Giraldo-Correa JA, Aristizábal-Carmona BS, Constain-Mosquera CA, Sabogal-Ortiz A, Machado-Alba JE. Prescription Patterns of Drugs Given to Hospitalized COVID-19 Patients: A Cross-Sectional Study in Colombia. Antibiotics. 2022; 11(3):333. https://doi.org/10.3390/antibiotics11030333
Chicago/Turabian StyleValladales-Restrepo, Luis Fernando, Jaime Andrés Giraldo-Correa, Brayan Stiven Aristizábal-Carmona, Camilo Alexander Constain-Mosquera, Alejandra Sabogal-Ortiz, and Jorge Enrique Machado-Alba. 2022. "Prescription Patterns of Drugs Given to Hospitalized COVID-19 Patients: A Cross-Sectional Study in Colombia" Antibiotics 11, no. 3: 333. https://doi.org/10.3390/antibiotics11030333
APA StyleValladales-Restrepo, L. F., Giraldo-Correa, J. A., Aristizábal-Carmona, B. S., Constain-Mosquera, C. A., Sabogal-Ortiz, A., & Machado-Alba, J. E. (2022). Prescription Patterns of Drugs Given to Hospitalized COVID-19 Patients: A Cross-Sectional Study in Colombia. Antibiotics, 11(3), 333. https://doi.org/10.3390/antibiotics11030333







