Clostridioides Difficile Enteritis: Case Report and Literature Review
Abstract
1. Introduction
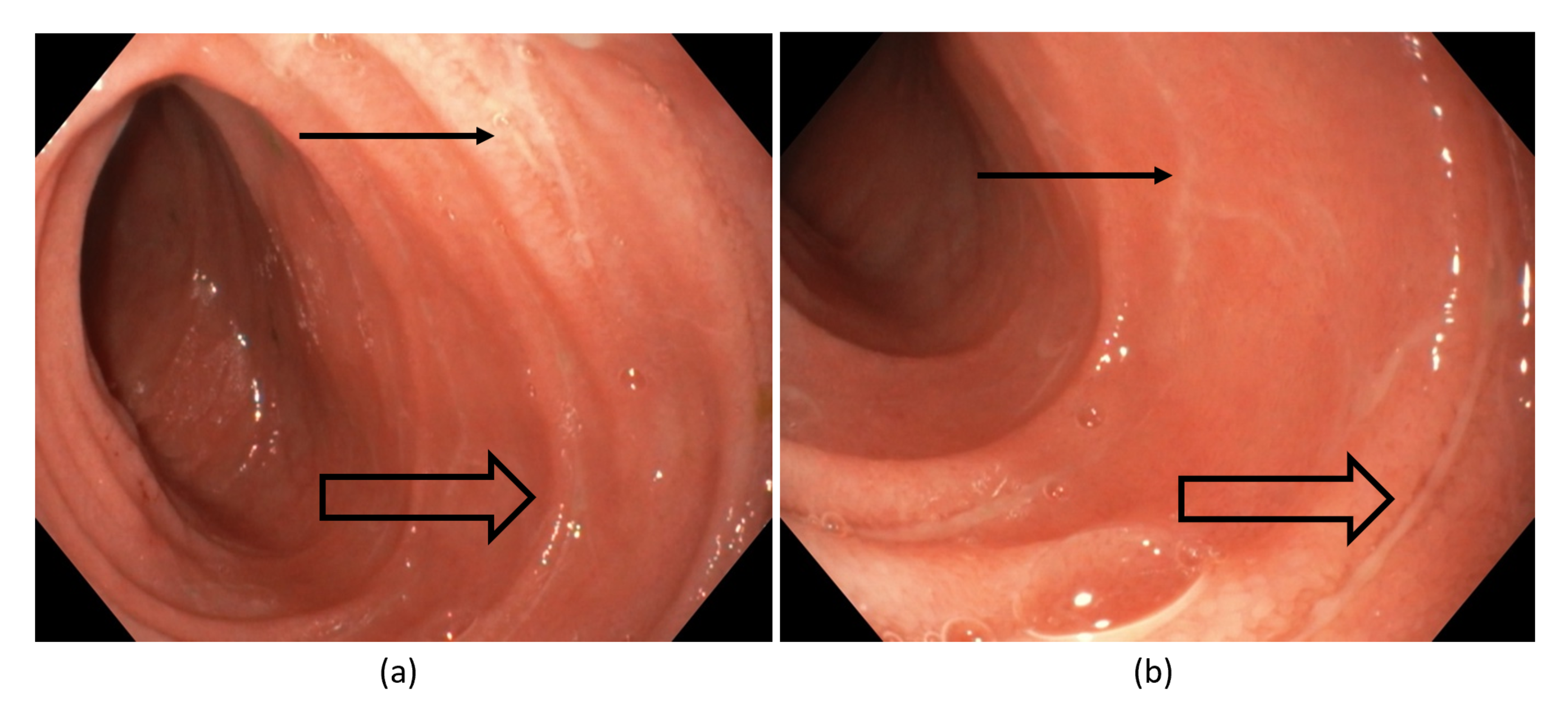
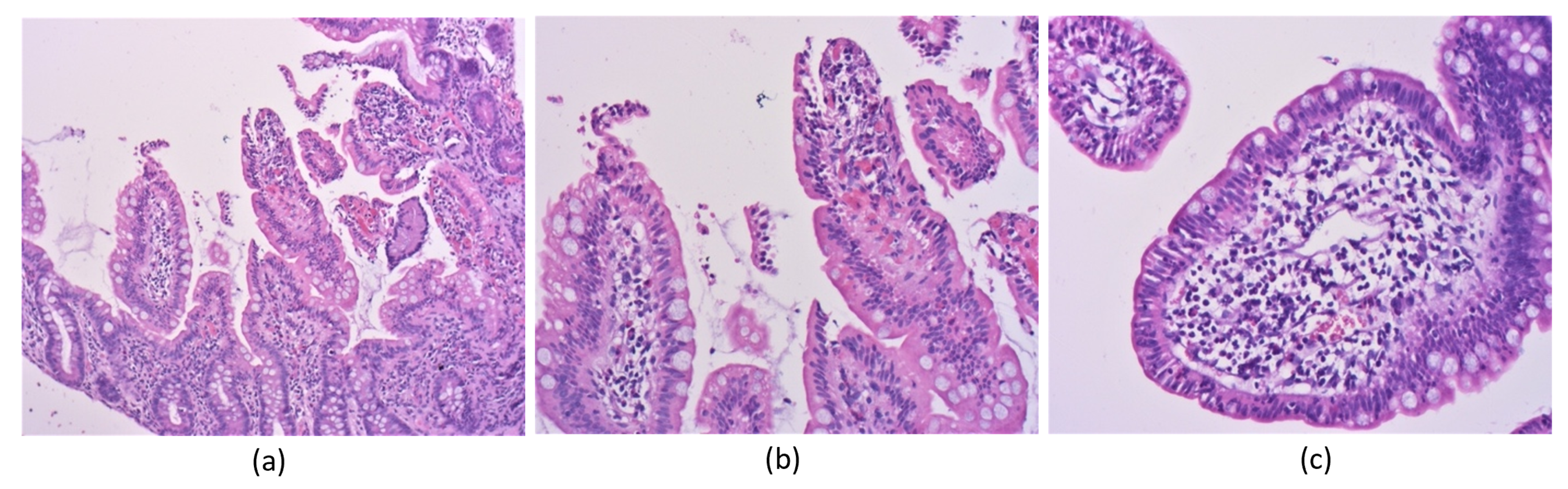
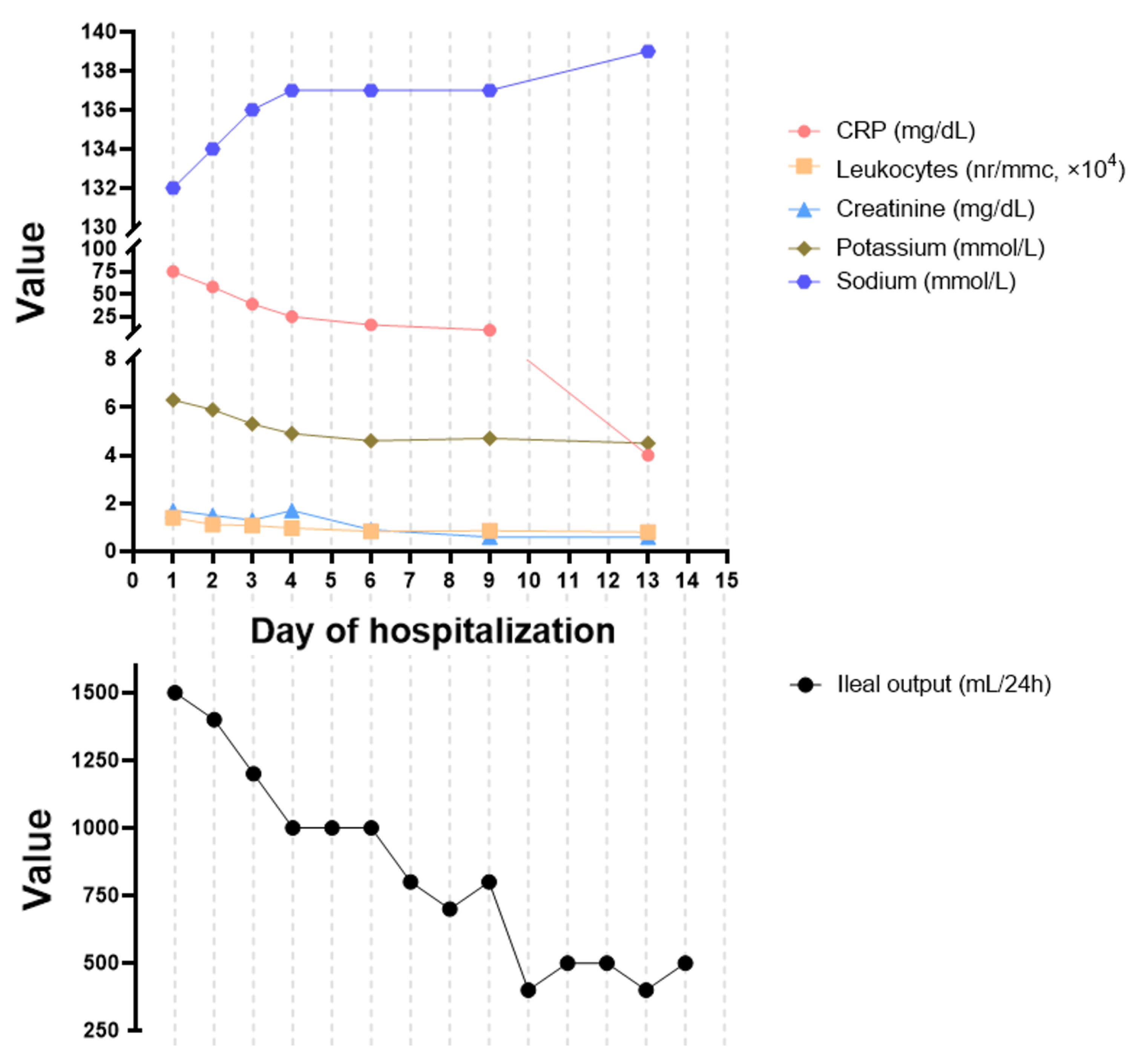
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Balsells, E.; Shi, T.; Leese, C.; Lyell, I.; Burrows, J.; Wiuff, C.; Campbell, H.; Kyaw, M.H.; Nair, H. Global burden of Clostridium difficile infections: A systematic review and meta-analysis. J. Glob. Health 2019, 9, 010407. [Google Scholar] [CrossRef]
- Seril, D.N.; Shen, B. Clostridium difficile infection in the postcolectomy patient. Inflamm. Bowel Dis. 2014, 20, 2450–2469. [Google Scholar] [CrossRef]
- Beal, E.W.; Bass, R.; Harzman, A.E. Two Patients with Fulminant Clostridium difficile Enteritis Who Had Not Undergone Total Colectomy: A Case Series and Review of the Literature. Case Rep. Surg. 2015, 2015, 957257. [Google Scholar] [CrossRef]
- LaMont, J.T.; Trnka, Y.M. Therapeutic implications of Clostridium difficile toxin during relapse of chronic inflammatory bowel disease. Lancet 1980, 315, 381–383. [Google Scholar] [CrossRef]
- Shortland, J.R.; Spencer, R.C.; Williams, J.L. Pseudomembranous colitis associated with changes in an ileal conduit. J. Clin. Pathol. 1983, 36, 1184–1187. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Miller, D.L.; Sedlack, J.D.; Holt, R.W. Perforation complicating rifampin-associated pseudomembranous enteritis. Arch. Surg. 1989, 124, 1082. [Google Scholar] [CrossRef]
- Kuntz, D.P.; Shortsleeve, M.J.; Kantrowitz, P.A.; Gauvin, G.P. Clostridium difficile enteritis. A cause of intramural gas. Dig. Dis. Sci. 1993, 38, 1942–1944. [Google Scholar] [CrossRef] [PubMed]
- Tsutaoka, B.; Hansen, J.; Johnson, D.; Holodniy, M. Antibiotic-associated pseudomembranous enteritis due to Clostridium difficile. Clin. Infect. Dis. 1994, 18, 982–984. [Google Scholar] [CrossRef]
- Yee, H.F., Jr.; Brown, R.S., Jr.; Ostroff, J.W. Fatal Clostridium difficile enteritis after total abdominal colectomy. J. Clin. Gastroenterol. 1996, 22, 45–47. [Google Scholar] [CrossRef] [PubMed]
- Kralovich, K.A.; Sacksner, J.; Karmy-Jones, R.A.; Eggenberger, J.C. Pseudomembranous colitis with associated fulminant ileitis in the defunctionalized limb of a jejunal-ileal bypass. Report of a case. Dis. Colon Rectum 1997, 40, 622–624. [Google Scholar] [CrossRef]
- Vesoulis, Z.; Williams, G.; Matthews, B. Pseudomembranous enteritis after proctocolectomy: Report of a case. Dis. Colon Rectum 2000, 43, 551–554. [Google Scholar] [CrossRef] [PubMed]
- Freiler, J.F.; Durning, S.J.; Ender, P.T. Clostridium difficile small bowel enteritis occurring after total colectomy. Clin. Infect. Dis. 2001, 33, 1429–1431. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, A.; Barnard, K.; Fishel, R.; Gradon, J.D. Extracolonic manifestations of Clostridium difficile infections. Presentation of 2 cases and review of the literature. Medicine 2001, 80, 88–101. [Google Scholar] [CrossRef] [PubMed]
- Tjandra, J.J.; Street, A.; Thomas, R.J.; Gibson, R.; Eng, P.; Cade, J. Fatal Clostridium difficile infection of the small bowel after complex colorectal surgery. ANZ J. Surg. 2001, 71, 500–503. [Google Scholar] [CrossRef]
- Mann, S.D.; Pitt, J.; Springall, R.G.; Thillainayagam, A.V. Clostridium difficile infection—An unusual cause of refractory pouchitis: Report of a case. Dis. Colon Rectum 2003, 46, 267–270. [Google Scholar] [CrossRef]
- Hayetian, F.D.; Read, T.E.; Brozovich, M.; Garvin, R.P.; Caushaj, P.F. Ileal perforation secondary to Clostridium difficile enteritis: Report of 2 cases. Arch. Surg. 2006, 141, 97–99. [Google Scholar] [CrossRef]
- Kim, K.A.; Wry, P.; Hughes, E., Jr.; Butcher, J.; Barbot, D. Clostridium difficile small-bowel enteritis after total proctocolectomy: A rare but fatal, easily missed diagnosis. Report of a case. Dis. Colon Rectum 2007, 50, 920–923. [Google Scholar] [CrossRef]
- Lundeen, S.J.; Otterson, M.F.; Binion, D.G.; Carman, E.T.; Peppard, W.J. Clostridium difficile enteritis: An early postoperative complication in inflammatory bowel disease patients after colectomy. J. Gastrointest. Surg. 2007, 11, 138–142. [Google Scholar] [CrossRef]
- Boland, E.; Thompson, J.S. Fulminant Clostridium difficile enteritis after proctocolectomy and ileal pouch-anal anastamosis. Gastroenterol. Res. Pract. 2008, 2008, 985658. [Google Scholar] [CrossRef]
- El Muhtaseb, M.S.; Apollos, J.K.; Dreyer, J.S. Clostridium difficile enteritis: A cause for high ileostomy output. ANZ J. Surg. 2008, 78, 416. [Google Scholar] [CrossRef]
- Follmar, K.E.; Condron, S.A.; Turner, I.I.; Nathan, J.D.; Ludwig, K.A. Treatment of metronidazole-refractory Clostridium difficile enteritis with vancomycin. Surg. Infect. 2008, 9, 195–200. [Google Scholar] [CrossRef]
- Wood, M.J.; Hyman, N.; Hebert, J.C.; Blaszyk, H. Catastrophic Clostridium difficile enteritis in a pelvic pouch patient: Report of a case. J. Gastrointest. Surg. 2008, 12, 350–352. [Google Scholar] [CrossRef]
- Yafi, F.A.; Selvasekar, C.R.; Cima, R.R. Clostridium difficile enteritis following total colectomy. Tech. Coloproctol. 2008, 12, 73–74. [Google Scholar]
- Causey, M.W.; Spencer, M.P.; Steele, S.R. Clostridium difficile enteritis after colectomy. Am. Surg. 2009, 75, 1203–1206. [Google Scholar] [CrossRef] [PubMed]
- Fleming, F.; Khursigara, N.; O’Connell, N.; Darby, S.; Waldron, D. Fulminant small bowel enteritis: A rare complication of Clostridium difficile-associated disease. Inflamm. Bowel Dis. 2009, 15, 801–802. [Google Scholar] [CrossRef] [PubMed]
- Lavallée, C.; Laufer, B.; Pépin, J.; Mitchell, A.; Dubé, S.; Labbé, A.C. Fatal Clostridium difficile enteritis caused by the BI/NAP1/027 strain: A case series of ileal C. difficile infections. Clin. Microbiol. Infect. 2009, 15, 1093–1099. [Google Scholar] [CrossRef] [PubMed]
- Peacock, O.; Speake, W.; Shaw, A.; Goddard, A. Clostridium difficile enteritis in a patient after total proctocolectomy. BMJ Case Rep. 2009, 2009, bcr1020081165. [Google Scholar] [CrossRef]
- Shen, B.; Remzi, F.H.; Fazio, V.W. Fulminant Clostridium difficile-associated pouchitis with a fatal outcome. Nat. Rev. Gastroenterol. Hepatol. 2009, 6, 492–495. [Google Scholar] [CrossRef]
- Wee, B.; Poels, J.A.; McCafferty, I.J.; Taniere, P.; Olliff, J. A description of CT features of Clostridium difficile infection of the small bowel in four patients and a review of literature. Br. J. Radiol. 2009, 82, 890–895. [Google Scholar] [CrossRef]
- Williams, R.N.; Hemingway, D.; Miller, A.S. Enteral Clostridium difficile, an emerging cause for high-output ileostomy. J. Clin. Pathol. 2009, 62, 951–953. [Google Scholar] [CrossRef]
- Gagandeep, D.; Ira, S. Clostridium difficile enteritis 9 years after total proctocolectomy: A rare case report. Am. J. Gastroenterol. 2010, 105, 962–963. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Levy, D.; Mann, S. Clostridium difficile infection in the absence of a colon. BMJ Case Rep. 2010, 2010, bcr0220102728. [Google Scholar] [CrossRef]
- Kurtz, L.E.; Yang, S.S.; Bank, S. Clostridium difficile-associated small bowel enteritis after total proctocolectomy in a Crohn’s disease patient. J. Clin. Gastroenterol. 2010, 44, 76–77. [Google Scholar] [CrossRef] [PubMed]
- Malkan, A.D.; Pimiento, J.M.; Maloney, S.P.; Palesty, J.A.; Scholand, S.J. Unusual manifestations of Clostridium difficile infection. Surg. Infect. 2010, 11, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Hariri, S.; Gouin, P.; Tuech, J.J.; Veber, B.; Dureuil, B. Clostridium difficile infection causing multiple organ failure and small-bowel enteritis. Clin. Res. Hepatol. Gastroenterol. 2011, 35, 142–144. [Google Scholar] [CrossRef] [PubMed]
- Holmer, C.; Zurbuchen, U.; Siegmund, B.; Reichelt, U.; Buhr, H.J.; Ritz, J.P. Clostridium difficile infection of the small bowel—Two case reports with a literature survey. Int. J. Colorectal Dis. 2011, 26, 245–251. [Google Scholar] [CrossRef]
- Ramos Martínez, A.; Romero Pizarro, Y.; Martínez Arrieta, F.; Balandín Moreno, B.; Múñez Rubio, E.; Cuiñas León, K.; Sánchez Romero, I.; Cantos López de Ibargüen, B.; Asensio Vegas, A. Clostridium difficile enteritis. Gastroenterol. Hepatol. 2011, 34, 539–545. [Google Scholar] [CrossRef]
- Thomas, K.; Taylor, J.; Everitt, L.; Nelson, R. Clostridium difficile does not only affect the colon: A case series. Colorectal Dis. 2011, 13, e156–e157. [Google Scholar] [CrossRef]
- Wiggelinkhuizen, M.; Gerrits, M.A. Clostridium difficile-induced necrotizing enteritis. Ned. Tijdschr. Geneeskd. 2011, 155, A2414. [Google Scholar]
- Dineen, S.P.; Bailey, S.H.; Pham, T.H.; Huerta, S. Clostridium difficile enteritis: A report of two cases and systematic literature review. World J. Gastrointest. Surg. 2013, 5, 37–42. [Google Scholar] [CrossRef]
- Thai, H.; Guerron, A.D.; Bencsath, K.P.; Liu, X.; Loor, M. Fulminant Clostridium difficile enteritis causing abdominal compartment syndrome. Surg. Infect. 2014, 15, 821–825. [Google Scholar] [CrossRef]
- Khan, S.A.; Towheed, A.; Tul Llah, S.; Bin Abdulhak, A.; Tilson-Mallett, N.R.; Salkind, A. Atypical Presentation of C. Difficile Infection: Report of a Case with Literature Review. Cureus 2016, 8, e563. [Google Scholar] [CrossRef]
- Tarasiuk-Rusek, A.; Shah, K.J. Clostridium difficile ileitis in a patient, after total colectomy. BMJ Case Rep. 2016, 2016, bcr2015214319. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, J.; Campion, T.; Wei, R.; Kuzmich, S. Clostridium difficile enteritis: Diffuse small bowel radiological changes in a patient with abdominal sepsis. BMJ Case Rep. 2018, 2018, bcr2017222209. [Google Scholar] [CrossRef]
- Abid, H.; Bischof, E. An Unusual Presentation of Severe Sepsis Due to Clostridium difficile Enteritis. Cureus 2019, 11, e4162. [Google Scholar] [CrossRef] [PubMed]
- Aujla, A.K.; Averbukh, L.D.; Potashinsky, A.; Rossi, L. A Rare Case of Clostridium difficile Enteritis: A Common Bug in an Uncommon Place. Cureus 2019, 11, e4519. [Google Scholar] [CrossRef] [PubMed]
- Nasser, H.; Munie, S.; Shakaroun, D.; Ivanics, T.; Nalamati, S.; Killu, K. Clostridium difficile Enteritis after Total Abdominal Colectomy for Ulcerative Colitis. Case Rep. Crit. Care 2019, 2019, 2987682. [Google Scholar] [CrossRef]
- Ulrich, R.J.; Bott, J.; Imlay, H.; Lopez, K.; Cinti, S.; Rao, K. Clostridioides Difficile Enteritis in Patients Following Total Colectomy—A Rare but Genuine Clinical Entity. Open Forum Infect. Dis. 2019, 6, ofz409. [Google Scholar] [CrossRef]
- Velez, D.R.; Ahmeti, M. Clostridioides difficile Enteritis Induced Anastomotic Rupture: A Case Report and Literature Review. Case Rep. Surg. 2020, 2020, 9794823. [Google Scholar] [CrossRef]
- Park, S.W.; Lee, Y.J.; Ryoo, E. Difference in Vitamin D Levels between Children with Clostridioides difficile Enteritis and Those with Other Acute Infectious Enteritis. Pediatr. Gastroenterol. Hepatol. Nutr. 2021, 24, 81–89. [Google Scholar] [CrossRef]
- Deshpande, A.; Pasupuleti, V.; Thota, P.; Pant, C.; Rolston, D.D.; Sferra, T.J.; Hernandez, A.V.; Donskey, C.J. Community-associated Clostridium difficile infection and antibiotics: A meta-analysis. J. Antimicrob. Chemother. 2013, 68, 1951–1961. [Google Scholar] [CrossRef] [PubMed]
- Brown, K.A.; Khanafer, N.; Daneman, N.; Fisman, D.N. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob. Agents Chemother. 2013, 57, 2326–2332. [Google Scholar] [CrossRef] [PubMed]
- Ionescu, E.M.; Curte, A.M.; Olteanu, A.O.; Preda, C.M.; Tieranu, I.; Klimko, A.; Tieranu, C.G. Rare Clinical Association between Clostridioides difficile Infection and Ischemic Colitis: Case Report and Literature Review. Medicina 2021, 57, 705. [Google Scholar] [CrossRef] [PubMed]
| Survived CDE (n = 54) | Did Not Survive CDE (n = 23) | p-Value | |
|---|---|---|---|
| Sex | |||
| Male | 26 (48.1%) | 14 (60.9%) | 0.331 |
| Female | 28 (51.9%) | 9 (39.1%) | |
| Age (Years) | |||
| Mean (SD) | 49.0 (18.6) | 70.2 (10.5) | <0.001 |
| Median [Min, Max] | 49.0 [18.0, 83.0] | 69.0 [53.0, 91.0] | |
| Inflammatory bowel disease | |||
| Crohn’s Disease | 8 (14.8%) | 1 (4.3%) | 0.049 |
| Ulcerative colitis | 23 (42.6%) | 5 (21.7%) | |
| None | 23 (42.6%) | 17 (73.9%) | |
| Gastrointestinal cancer (previously or concurrent) | |||
| No | 50 (92.6%) | 14 (60.9%) | 0.00157 |
| Yes | 4 (7.4%) | 9 (39.1%) | |
| Recent hospitalization | |||
| Surgical admission | 42 (77.8%) | 19 (82.6%) | 0.903 |
| Non-surgical admission | 7 (13.0%) | 3 (13.0%) | |
| No recent hospitalization | 5 (9.3%) | 1 (4.3%) | |
| History of surgery | |||
| IPAA | 25 (46.3%) | 2 (8.7%) | 0.0171 |
| Total colectomy | 7 (13.0%) | 4 (17.4%) | |
| Hemicolectomy | 6 (11.1%) | 5 (21.7%) | |
| Non-GI | 1 (1.9%) | 2 (8.7%) | |
| Other | 11 (20.4%) | 7 (30.4%) | |
| None | 4 (7.4%) | 3 (13.0%) | |
| Concurrent CD colitis | |||
| Yes | 9 (16.7%) | 4 (17.4%) | 1 |
| No | 45 (83.3%) | 19 (82.6%) | |
| Was CDE caused by surgery for which the patient was admitted? | |||
| Yes | 29 (53.7%) | 14 (60.9%) | 0.835 |
| No, other surgery | 16 (29.6%) | 6 (26.1%) | |
| No, non-surgical | 9 (16.7%) | 3 (13.0%) | |
| Predisposing antibiotic use | |||
| Yes | 39 (72.2%) | 16 (69.6%) | 0.913 |
| No | 3 (5.6%) | 2 (8.7%) | |
| Unknown | 12 (22.2%) | 5 (21.7%) | |
| Immunosuppressed | |||
| Yes | 15 (27.8%) | 8 (34.8%) | 0.894 |
| No | 29 (53.7%) | 11 (47.8%) | |
| Unknown | 10 (18.5%) | 4 (17.4%) | |
| Treatment administered | |||
| Metronidazole with vancomycin | 24 (44.4%) | 13 (56.5%) | 0.626 |
| Metronidazole | 13 (24.1%) | 4 (17.4%) | |
| Vancomycin | 11 (20.4%) | 2 (8.7%) | |
| Other | 3 (5.6%) | 2 (8.7%) | |
| Unknown | 3 (5.6%) | 2 (8.7%) | |
| Surgical treatment of CDE | |||
| Yes | 14 (25.9%) | 9 (39.1%) | 0.283 |
| No | 40 (74.1%) | 14 (60.9%) | |
| ICU transfer | |||
| Yes | 17 (31.5%) | 22 (95.7%) | <0.001 |
| No | 37 (68.5%) | 1 (4.3%) | |
| Time to outcome (Resolution of infection or death) | |||
| <2 weeks | 27 (50.0%) | 9 (39.1%) | 0.766 |
| >2 weeks | 24 (44.4%) | 13 (56.5%) | |
| Unknown | 3 (5.6%) | 1 (4.3%) | |
| Readmission | |||
| Yes | 4 (7.4%) | 0 (0%) | - |
| No | 50 (92.6%) | 0 (0%) | |
| Not applicable | 0 (0%) | 23 (100%) | |
| Antibiotic | Case Load |
|---|---|
| Cephalosporins | 21 (27.3%) |
| Fluoroquinolones | 10 (13.0%) |
| Penicillins | 9 (11.7%) |
| Carbapenems | 2 (2.6%) |
| Metronidazole | 2 (2.6%) |
| Trimethoprim / Sulfamethoxazole | 2 (2.6%) |
| Doxycycline | 1 (1.3%) |
| Vancomycin | 1 (1.3%) |
| Rifampin | 1 (1.3%) |
| Clindamycin | 1 (1.3%) |
| Unknown | 22 (28.6%) |
| None | 5 (6.5%) |
| Author and Year | Cases Reviewed | Case Year Range | CDE Mortality Rate |
|---|---|---|---|
| Freiler et al., 2001 [12] | 10 | 1980–2001 | 60% |
| Lundeen et al., 2007 [18] | 20 | 1980–2007 | 45% |
| Holmer et al., 2011 [36] | 56 | 1980–2011 | 32.1% |
| Beal et al., 2015 [3] | 63 | 1980–2015 | 30.1% |
| Present study | 77 | 2001–2021 | 29.8% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klimko, A.; Tieranu, C.G.; Curte, A.-M.; Preda, C.M.; Tieranu, I.; Olteanu, A.O.; Ionescu, E.M. Clostridioides Difficile Enteritis: Case Report and Literature Review. Antibiotics 2022, 11, 206. https://doi.org/10.3390/antibiotics11020206
Klimko A, Tieranu CG, Curte A-M, Preda CM, Tieranu I, Olteanu AO, Ionescu EM. Clostridioides Difficile Enteritis: Case Report and Literature Review. Antibiotics. 2022; 11(2):206. https://doi.org/10.3390/antibiotics11020206
Chicago/Turabian StyleKlimko, Artsiom, Cristian George Tieranu, Ana-Maria Curte, Carmen Monica Preda, Ioana Tieranu, Andrei Ovidiu Olteanu, and Elena Mirela Ionescu. 2022. "Clostridioides Difficile Enteritis: Case Report and Literature Review" Antibiotics 11, no. 2: 206. https://doi.org/10.3390/antibiotics11020206
APA StyleKlimko, A., Tieranu, C. G., Curte, A.-M., Preda, C. M., Tieranu, I., Olteanu, A. O., & Ionescu, E. M. (2022). Clostridioides Difficile Enteritis: Case Report and Literature Review. Antibiotics, 11(2), 206. https://doi.org/10.3390/antibiotics11020206






