Antimicrobial Stewardship in College and University Health Settings: A Public Health Opportunity
Abstract
:1. Introduction
2. Antibiotic Use and Misuse among University Students
2.1. Global Context for Antibiotic Use and Misuse
2.1.1. Low- and Middle-Income Countries
2.1.2. High-Income Countries
3. Students’ Knowledge and Attitudes toward Antibiotic Use and Misuse
Students in Health-Related Disciplines
4. AMS in College and University Settings
4.1. Health Literacy and Shared Decision-Making
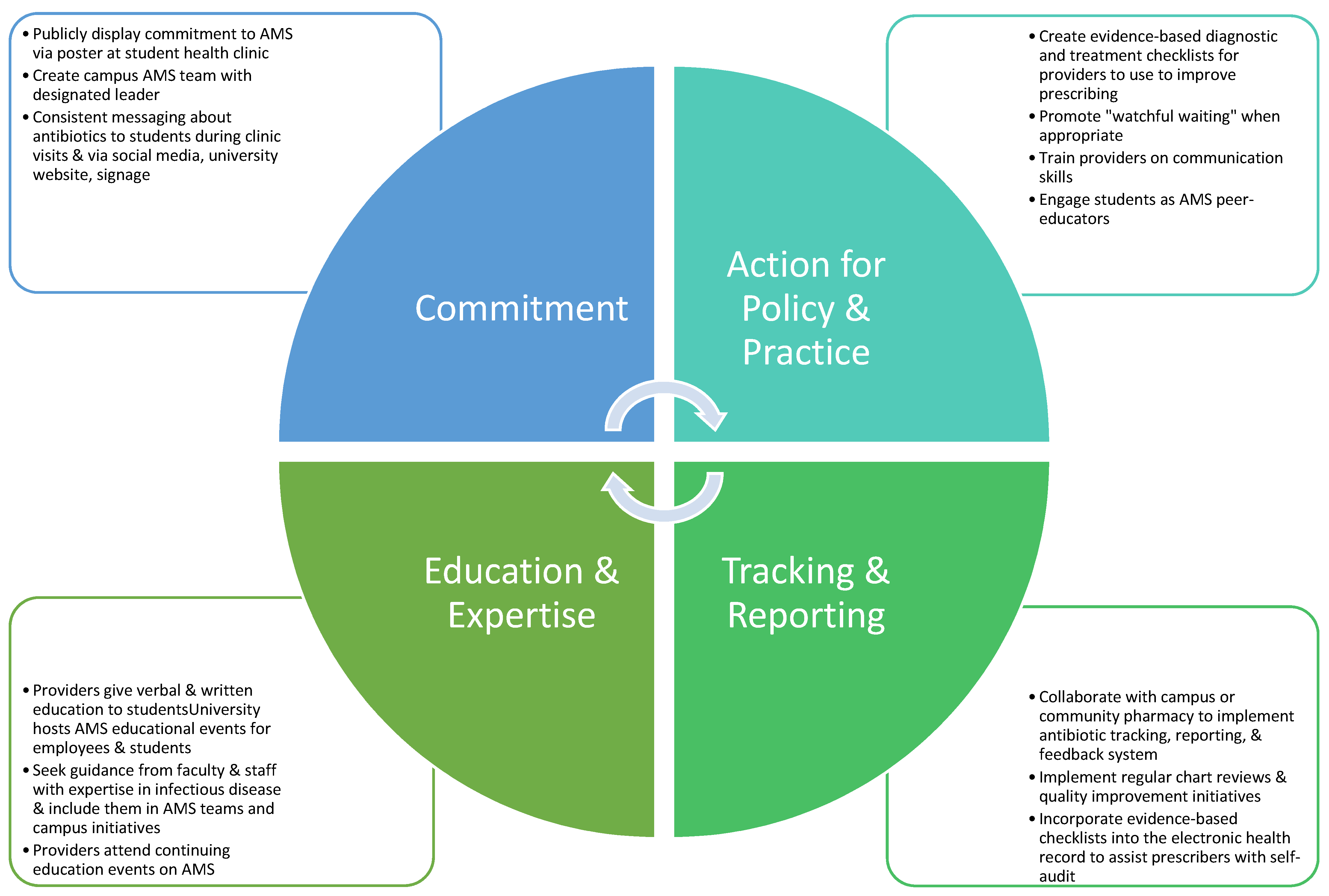
4.2. Opportunities for AMS in College and University Health Settings
Global Context for AMS in College and University Settings
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2019; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2019. [Google Scholar] [CrossRef] [Green Version]
- Nelson, R.E.; Hatfield, K.M.; Wolford, H.; Samore, M.H.; Scott, R.D.; Reddy, S.C.; Olubajo, B.; Paul, P.; Jernigan, J.A.; Baggs, J. National Estimates of Healthcare Costs Associated with Multidrug-Resistant Bacterial Infections among Hospitalized Patients in the United States. Clin. Infect. Dis. 2021, 72 (Suppl. 1), S17–S26. [Google Scholar] [CrossRef]
- Murray, A.K. The Novel Coronavirus COVID-19 Outbreak: Global Implications for Antimicrobial Resistance. Front. Microbiol. 2020, 11, 1020. [Google Scholar] [CrossRef]
- Baccolini, V.; Migliara, G.; Isonne, C.; Dorelli, B.; Barone, L.C.; Giannini, D.; Marotta, D.; Marte, M.; Mazzalai, E.; Alessandri, F.; et al. The impact of the COVID-19 pandemic on healthcare-associated infections in intensive care unit patients: A retrospective cohort study. Antimicrob. Resist. Infect. Control 2021, 10, 87. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Measuring Outpatient Antibiotic Prescribing. 14 October 2020. Available online: https://www.cdc.gov/antibiotic-use/data/outpatient-prescribing/index.html (accessed on 22 July 2021).
- Russo, P.L.; Shaban, R.Z.; Macbeth, D.; Carter, A.; Mitchell, B.G. Impact of electronic healthcare-associated infection surveillance software on infection prevention resources: A systematic review of the literature. J. Hosp. Infect. 2018, 99, 1–7. [Google Scholar] [CrossRef]
- Migliara, G.; di Paolo, C.; Barbato, D.; Baccolini, V.; Salerno, C.; Nardi, A.; Alessandri, F.; Giordano, A.; Tufi, D.; Marinelli, A.; et al. Multimodal surveillance of healthcare associated infections in an intensive care unit of a large teaching hospital. Ann. Ig. Med. Prev. Comunita 2019, 31, 399–413. [Google Scholar] [CrossRef]
- Mitchell, B.G.; Russo, P.L. Preventing healthcare-associated infections: The role of surveillance. Nurs. Stand. 2015, 29, 52–58. [Google Scholar] [CrossRef]
- Marcelin, J.R.; Chung, P.; van Schooneveld, T.C. Antimicrobial stewardship in the outpatient setting: A review and proposed framework. Infect. Control Hosp. Epidemiol. 2020, 41, 833–840. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Antimicrobial Resistance. 2015. Available online: https://www.who.int/publications/i/item/9789241509763 (accessed on 22 July 2021).
- Sanchez, G.; Fleming-Dutra, K.; Roberts, R.; Hicks, L. Core Elements of Outpatient Antibiotic Stewardship. MMWR Recomm. Rep. 2016, 65, 1308–1316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yates, T.D.; Davis, M.E.; Taylor, Y.J.; Davidson, L.; Connor, C.D.; Buehler, K.; Spencer, M. Not a magic pill: A qualitative exploration of provider perspectives on antibiotic prescribing in the outpatient setting. BMC Fam. Pract. 2018, 19, 96. [Google Scholar] [CrossRef] [PubMed]
- Hertz, B.T. Easing the strain of unnecessary antibiotic requests. Physicians called on to change patient expectations about antibiotic use; experts say it’s about communication. Med. Econ. 2014, 91, 32–35. [Google Scholar] [PubMed]
- Boiko, O.; Gulliford, M.C.; Burgess, C. Revisiting patient expectations and experiences of antibiotics in an era of antimicrobial resistance: Qualitative study. Health Expect. 2020, 23, 1250–1258. [Google Scholar] [CrossRef]
- Lee, C.R.; Lee, J.H.; Kang, L.W.; Jeong, B.C.; Lee, S.H. Educational effectiveness, target, and content for prudent antibiotic use. BioMed Res. Int. 2015, 2015, 214021. [Google Scholar] [CrossRef] [PubMed]
- Hermsen, E.D.; MacGeorge, E.L.; Andresen, M.L.; Myers, L.M.; Lillis, C.J.; Rosof, B.M. Decreasing the peril of antimicrobial resistance through enhanced health literacy in outpatient settings: An underrecognized approach to advance antimicrobial stewardship. Adv. Ther. 2020, 37, 918–932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haltiwanger, K.A.; Hayden, G.F.; Weber, T.; Evans, B.A.; Possner, A.B. Antibiotic-seeking behavior in college students: What do they really expect? J. Am. Coll. Health 2001, 50, 9–13. [Google Scholar] [CrossRef]
- American College Health Association. American College Health Association-National College Health Assessment III: Reference Group Executive Summary Fall 2019; American College Health Association: Silver Spring, MD, USA, 2020. [Google Scholar]
- Centers for Disease Control and Prevention. Sexually Transmitted Diseases: Adolescents and Young Adults. 8 April 2021. Available online: https://www.cdc.gov/std/life-stages-populations/adolescents-youngadults.htm (accessed on 28 July 2021).
- Al-Kubaisi, K.A.; de Ste Croix, M.; Vinson, D.; Ellis, L.; Sharif, S.I.; Abduelkarem, A.R. What drives using antibiotic without prescriptions? A qualitative interview study of university students in United Arab Emirates. Pharm. Pract. 2018, 16, 1172. [Google Scholar] [CrossRef]
- Pan, H.; Cui, B.; Zhang, D.; Farrar, J.; Law, F.; Ba-Thein, W. Prior knowledge, older age, and higher allowance are risk factors for self-medication with antibiotics among university students in southern China. PLoS ONE 2012, 7, e41314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peng, D.; Wang, X.; Xu, Y.; Sun, C.; Zhou, X. Antibiotic misuse among university students in developed and less developed regions of China: A cross-sectional survey. Glob. Health Action 2018, 11, 1496973. [Google Scholar] [CrossRef] [PubMed]
- Shahpawee, N.S.; Chaw, L.L.; Muharram, S.H.; Goh, H.P.; Hussain, Z.; Ming, L.C. University students’ antibiotic use and knowledge of antimicrobial resistance: What are the common myths? Antibiotics 2020, 9, 349. [Google Scholar] [CrossRef]
- Dyar, O.; Hills, H.; Seitz, L.T.; Perry, A.; Ashiru-Oredope, D. Assessing the knowledge, attitudes and behaviors of human and animal health students toward antibiotic use and resistance: A pilot cross-sectional study in the UK. Antibiotics 2018, 7, 10. [Google Scholar] [CrossRef] [Green Version]
- Zoorob, R.J.; Larzelere, M.M.; Malpani, S.; Zoorob, R. Use and perceptions of antibiotics for upper respiratory infections among college students. J. Fam. Pract. 2001, 50, 32–37. [Google Scholar]
- Centers for Disease Control and Prevention. Antibiotic Use in the United States, 2018 Update: Progress and Opportunities. 2019. Available online: https://www.cdc.gov/antibiotic-use/stewardship-report/pdf/stewardship-report-2018-508.pdf (accessed on 31 October 2021).
- Tattevin, P.; Levy Hara, G.; Toumi, A.; Enani, M.; Coombs, G.; Voss, A.; Wertheim, H.; Poda, A.; Daoud, Z.; Laxminarayan, R.; et al. Advocacy for Increased International Efforts for Antimicrobial Stewardship Actions in Low-and Middle-Income Countries on Behalf of Alliance for the Prudent Use of Antimicrobials (APUA), Under the Auspices of the International Society of Antimicrobial Chemotherapy (ISAC). Front. Med. 2020, 7, 503. [Google Scholar] [CrossRef]
- Xu, R.; Mu, T.; Wang, G.; Shi, J.; Wang, X.; Ni, X. Self-Medication with antibiotics among university students in LMIC: A systematic review and meta-analysis. J. Infect. Dev. Ctries. 2019, 13, 678–689. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jairoun, A.; Hassan, N.; Ali, A.; Jairoun, O.; Shahwan, M. Knowledge, attitude and practice of antibiotic use among university students: A cross sectional study in UAE. BMC Public Health 2019, 19, 518. [Google Scholar] [CrossRef] [PubMed]
- Sakr, S.; Ghaddar, A.; Hamam, B.; Sheet, I. Antibiotic use and resistance: An unprecedented assessment of university students’ knowledge, attitude and practices (KAP) in Lebanon. BMC Public Health 2020, 20, 535. [Google Scholar] [CrossRef] [Green Version]
- Moes, K.; Carrico, C.; Hall, A. Knowledge of antibiotic use in college students: A quality improvement project. Build. Healthy Acad. Communities J. 2018, 2, 21–32. [Google Scholar] [CrossRef]
- Blyer, K.; Hulton, L. College students, shared decision-making, and the appropriate use of antibiotics for respiratory tract infections: A systematic literature review. J. Am. Coll. Health 2016, 64, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Ellis, J.; Vassilev, I.; Kennedy, A.; Moore, M.; Rogers, A. Help seeking for antibiotics; is the influence of a personal social network relevant? BMC Fam. Pract. 2019, 20, 63. [Google Scholar] [CrossRef]
- Ramchand, R.; Ahluwalia, S.C.; Xenakis, L.; Apaydin, E.; Raaen, L.; Grimm, G. A systematic review of peer-supported interventions for health promotion and disease prevention. Prev. Med. 2017, 101, 156–170. [Google Scholar] [CrossRef]
- Abiodun, O.; Ovat, F.; Olu-Abiodun, O. Provider-Related Predictors of Utilization of University Health Services in Nigeria. Ethiop. J. Health Sci. 2019, 29, 239–250. [Google Scholar] [CrossRef]
- National Center for Education Statistics. Fast Facts: Back to School Statistics. 2021. Available online: https://nces.ed.gov/fastfacts/display.asp?id=372#College_enrollment (accessed on 22 August 2021).
- Unwin, B.; Goodie, J.; Reamy, B.; Quinlan, J. Care of the College Student. Am. Fam. Physician 2013, 88, 596–604. [Google Scholar]
| Author (Year) | Country | Sample | Methods | Findings | Recommendations |
|---|---|---|---|---|---|
| Al-Kubaisi et al. (2018) [20] | United Arab Emirates | n = 15 college students enrolled in their first year at a healthcare university | Semi-structured face-to-face interviewing to gain an enhance understanding of knowledge, attitude, belief, and experience of college students related to antibiotic use without prescription; Andersen model was applied as the theoretical thematic analysis used to identify, analyze, and report repeated themes within responses | 4 themes were identified: (1) Medication habits and practices, (2) reasons for self-medication, (3) access to antibiotics without a prescription, (4) perceptions of antibiotic and the development of resistance; Students had misconceptions that antibiotics are appropriate to use for viral illnesses, and many students reported access to antibiotics without a prescription. Most students were familiar with antibiotic resistance and self-medication of antibiotics worsens resistance. Previous experience with antibiotics was an influencing factor as well as time saving factor, perceived urgency, costs, family/friend advice | Need more research to determine how policy change could improve self-prescribing behaviors, to fully understand student experiences with medication, and to examine legal prohibition of selling antibiotics without prescription; Recommend awareness campaign target towards physician over-prescribing |
| Blyer et al. (2016) [32] | United States | 12 peer-reviewed articles | PRISMA framework used for review and the following inclusion criteria applied: (1) articles about shared decision-making for respiratory infections, (2) articles about college students or adults, (3) articles about antibiotic use for respiratory tract infections | Shared decision-making was preferred among college students and young, educated adults; Some studies suggested shared decision-making was an effective tool for decreasing antibiotic use for respiratory infections | Shared decision-making is a promising strategy for decreasing antibiotic misuse in college students; College health centers should enhance prescribing practices and education to promote a better understanding of AMS in college health; Recommend future research on shared decision-making in college students and international students |
| Dyar et al. (2018) [24] | United Kingdom | n = 255 human and animal health students from 25 universities during the 2016 Antibiotic Guardian campaign | 25 question, cross-sectional survey, which assessed knowledge, attitudes, and practices with antibiotic use and awareness of AMS, emailed to students enrolled in different human and animal health courses; Survey also temporarily available on the Public Health England website | Only 5.8% students used antibiotics obtained from friends/family, online source, or leftover from previous illness; 100% knew bacteria could develop resistance to antibiotics and 41% believed human body could develop resistance; 92% were are that most respiratory illnesses improve without antibiotics; Students believed antibiotic resistance was a bigger global challenge (mean of 9 on a scale of 1–10) compared to climate change, food security, gender inequality, and obesity (p < 0.001); 44% students were aware of AMS with higher level students more likely to be aware (p < 0.01). 20% students believed their knowledge was sufficient for future clinical practice with many requesting more information | Overall, students from diverse healthcare courses were knowledgeable with good attitudes toward antibiotic resistance; Recommend development of curricula that addresses core principles of AMS; Recommend global and national campaigns to increase awareness as well as interprofessional learning experiences to improve AMS |
| Haltiwanger et al. (2001) [17] | United States | n = 129 college students with respiratory symptoms seen in student health clinic in Virginia | 30 question survey divided into 2 parts—Part 1 administered pre-visit to assess understanding of illness and knowledge of antibiotics; Part 2 administered post-visit to assess demographics, past antibiotic use and medical visits | 71 (55%) students expected an antibiotic prescription; Satisfaction most likely if students received antibiotic (p = 0.01) and when specific diagnosis was given (p < 0.01) and when students received clear explanation of why antibiotics were or were not necessary (p < 0.01) | Appropriate communication is necessary to instill good health behaviors related to antibiotic use; Providers should use alternative terminology that is less suggestive of infection and provide education to students; Educational handout created for college students |
| Jairoun et al. (2019) [29] | United Arab Emirates | n = 1200 college students from Ajman University
| 33 question survey assessed antibiotic knowledge, attitudes, and self-medications practices among students; mixed qualitative and quantitative questions; scores were compared between medical and non-medical students | Students scored highest in attitudes at 76% then knowledge at 59% and practice at 45%; Overall, medical students scored significantly higher than non-medical students in knowledge, attitudes, and practices, respectively (p = 0.0001; p = 0.000; p = 0.002). All students reported overuse of antibiotics for respiratory tract infections | Recommend educational campaigns to address lack of awareness that antibiotic resistance is a national and international problem. Specifically, better education is needed to address knowledge deficits related to antibiotic use for viral respiratory illnesses |
| Moes et al. (2018) [31] | United States | n = 44 college students who visited a college health clinic in Nebraska | 19-item survey assessed student knowledge of respiratory infections, especially how antibiotics work against bacteria, viruses, and all germs; students completed the pre-visit survey then received education by the provider with a handout then completed a post-visit survey | Knowledge of antibiotics improved following the educational intervention (p = 0.1). Changes in knowledge about efficacy and provider trust was mixed. Knowledge regarding correct use was high before and after. 98% students were satisfied with the visit regardless of antibiotic prescription | Recommend future research involving larger, more diverse samples of college students to determine how educational interventions will improve their knowledge of antibiotics; Recommend analyzing effect of educational intervention at a later interval to ensure knowledge was truly improved and retained. Recommend educational handouts and verbal review by provider about viral respiratory infections and antibiotics |
| Pan et al. (2012) [21] | China | n = 1300 college students from Shantou University | 36-question, quantitative and qualitative survey assessed students’ demographics and self-medication behaviors and knowledge of antibiotics; Respondents were divided into 2 groups: (1) PKA group = students with prior knowledge of antibiotics (all medical students except 1st years), and (2) non-PKA group = students without prior knowledge of antibiotics (1st year medical students and non-medical students) | 47.8% reported antibiotic self-treatment; Risk factors for self-medication of antibiotics included PKA, older age, and higher monthly allowance; Students commonly self-treated respiratory symptoms and fever with antibiotics; PKA group had better knowledge regarding correct antibiotic use and common adverse reactions (p < 0.05); Higher knowledge yet higher rates of self-treatment with antibiotics among the PKA group suggested that PKA may create “a false sense of confidence in self-diagnosis and self-management” | Education was shown to improve the PKA group’s knowledge of appropriate antibiotic use, which suggests education may benefit all students; Recommend targeted education to college students through workshops, seminars, and social media; Recommend stricter government laws to regulate the sale of non-prescribed medications in Chinese pharmacies |
| Peng et al. (2018) [22] | China | n = 3995 college students from developed (Zhejiang) and less developed (Guizhou) regions | Cross-sectional survey assessed antibiotic use behaviors and socio-demographic factors; associations between socio-demographic factors and behaviors were examined | Guizhou students were significantly more associated with misuse of antibiotics, which included antibiotic self-medication (p < 0.001), over the counter use (p < 0.001), asking for prescription from doctor (p < 0.001), and prophylactic use (p < 0.001). Students with medical backgrounds were significantly associated with better antibiotic use behaviors, however students with medical parents engaged in poorer antibiotic use behaviors. Higher education level was associated with increased antibiotic misuse | Recommend health education programs on antibiotic use targeted to the general public and college students; Recommend initiatives to eliminate the problem of people taking leftover antibiotics: (1) regulate physician overprescribing, (2) educate patients how to correctly take antibiotics as prescribed, (3) ban antibiotic distribution in pharmacies without prescriptions, (4) instruct patients to throw away leftover antibiotics; Recommend future research to determine causal relationships |
| Sakr et al. (2020) [30] | Lebanon | n = 750 college students
| Cross-sectional survey assessed knowledge, attitudes, and practices related to antibiotic use and resistance; scores were compared between health students and non-health students | 80.2% health students had knowledge related to antibiotics effectiveness to treat bacterial/viral infections compared to 36.9% of non-health students (p < 0.001); 94% of health students answered correctly that it is not okay to use friends’ or family members’ antibiotics compared to 85.2% of non-health students (p < 0.001); 84.4% health students reported checking expiration of antibiotics prior to use compared to 74.5% non-health students (p < 0.001) | Recommend education programs, such as seminars, workshops, and course curricula, targeted toward college students without health background; Encouraged campaigns to promote vaccination and hygiene, public health courses in curricula, media campaigns, and proactive pharmacist roles |
| Shahpawee et al. (2020) [23] | Brunei Darussalam | n = 130 college students at the Universiti Brunei Darussalam
| Cross-sectional survey assessed antibiotic use and knowledge | 69% had previously used antibiotics with most acquired from healthcare provider. Less than 4% obtained antibiotics from friend/family or from leftover supply; 51% students had good level of knowledge of antibiotic use and resistance (mean score 9 out of 14). 41% had misconceptions that antibiotics were appropriate to treat viral illnesses; 76% believed the body could become resistant to antibiotics | Overall, good level of knowledge was found. Recommend increasing awareness of correct antibiotic use to correct misconceptions. More research is needed in this population |
| Xu et al. (2019) [28] | Several low- and middle-income countries in Africa (10), Asia (36), Europe (1), and South America (2) | 49 peer-reviewed articles | Meta-analysis and systematic review performed; Agency for Healthcare Research and Quality 11-item checklist used to appraise quality | Total prevalence of self-medication with antibiotics (SMA) was 49%; Africa had highest SMA with 55.3% and South America had lowest SMA with 38.3%; More educated students were more likely to engage in SMA | Recommend pharmacological education, national policy and law changes, and improved provider practices in university clinics and hospitals |
| Zoorob et al. (2001) [25] | United States | n = 425 college students from 3 college campuses in Louisiana and Indiana | Cross-sectional surveys asked participants to provide answers regarding their perceptions and use of antibiotics in three different clinical scenarios in which symptoms of different illnesses were described | Use of antibiotics were higher in students who believed antibiotics were the correct treatment for the common cold; Older students were associated with increased antibiotic use (p = 0.001) and students utilizing the campus health clinic were more likely to seek care (p < 0.001) | Recommend targeted education to providers and students to (1) decrease use of campus health clinic for self-limiting viral illnesses, (2) decrease antibiotic misuse, (3) promote evidence-based options for non-prescription treatments |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dambrino, K.L.; Green, M. Antimicrobial Stewardship in College and University Health Settings: A Public Health Opportunity. Antibiotics 2022, 11, 89. https://doi.org/10.3390/antibiotics11010089
Dambrino KL, Green M. Antimicrobial Stewardship in College and University Health Settings: A Public Health Opportunity. Antibiotics. 2022; 11(1):89. https://doi.org/10.3390/antibiotics11010089
Chicago/Turabian StyleDambrino, Kathryn L., and Montgomery Green. 2022. "Antimicrobial Stewardship in College and University Health Settings: A Public Health Opportunity" Antibiotics 11, no. 1: 89. https://doi.org/10.3390/antibiotics11010089
APA StyleDambrino, K. L., & Green, M. (2022). Antimicrobial Stewardship in College and University Health Settings: A Public Health Opportunity. Antibiotics, 11(1), 89. https://doi.org/10.3390/antibiotics11010089






