Management of Children Admitted to Hospitals across Bangladesh with Suspected or Confirmed COVID-19 and the Implications for the Future: A Nationwide Cross-Sectional Study
Abstract
:1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Setting and Design
4.2. The Data Collection Tool and Analysis
4.3. Patient and Hospital Anonymity and Ethical Approval
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Abbas, K.; Procter, S.R.; van Zandvoort, K.; Clark, A.; Funk, S.; Mengistu, T.; Hogan, D.; Dansereau, E.; Jit, M.; Flasche, S.; et al. Routine childhood immunisation during the COVID-19 pandemic in Africa: A benefit–risk analysis of health benefits versus excess risk of SARS-CoV-2 infection. Lancet Glob. Health 2020, 8, e1264–e1272. [Google Scholar] [CrossRef]
- Gaythorpe, K.A.; Abbas, K.; Huber, J.; Karachaliou, A.; Thakkar, N.; Woodruff, K.; Li, X.; Echeverria-Londono, S.; Fouda, A.A.B.; Cutts, F.; et al. Impact of COVID-19-related disruptions to measles, meningococcal A, and yellow fever vaccination in 10 countries. eLife 2021, 10, e67023. [Google Scholar] [CrossRef] [PubMed]
- Hussain, M.; Al Mamun, M.A. COVID-19 in children in Bangladesh: Situation analysis. Asia Pac. J. Paediatr. Child Health 2020, 3, 59–65. [Google Scholar]
- Lassi, Z.; Naseem, R.; Salam, R.; Siddiqui, F.; Das, J. The Impact of the COVID-19 Pandemic on Immunization Campaigns and Programs: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 988. [Google Scholar] [CrossRef] [PubMed]
- Sama, B.K.; Kaur, P.; Thind, P.S.; Verma, M.K.; Kaur, M.; Singh, D.D. Implications of COVID-19-induced nationwide lockdown on children’s behaviour in Punjab, India. Child Care Health Dev. 2020, 47, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Muhoza, P.; Danovaro-Holliday, M.C.; Diallo, M.S.; Murphy, P.; Sodha, S.V.; Requejo, J.H.; Wallace, A.S. Routine Vaccination Coverage—Worldwide, 2020. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 1495–1500. [Google Scholar] [CrossRef] [PubMed]
- Rana, S.; Shah, R.; Ahmed, S.; Mothabbir, G. Post-disruption catch-up of child immunisation and health-care services in Bangladesh. Lancet Infect. Dis. 2021, 21, 913. [Google Scholar] [CrossRef]
- Mantovani, A.; Rinaldi, E.; Zusi, C.; Beatrice, G.; Saccomani, M.D.; Dalbeni, A. Coronavirus disease 2019 (COVID-19) in children and/or adolescents: A meta-analysis. Pediatr. Res. 2020, 89, 733–737. [Google Scholar] [CrossRef]
- Kanthimathinathan, H.K.; Dhesi, A.; Hartshorn, S.; Ali, S.H.; Kirk, J.; Nagakumar, P.; Jyothish, D. COVID-19: A UK Children’s Hospital Experience. Hosp. Pediatr. 2020, 10, 802–805. [Google Scholar] [CrossRef]
- Mehta, N.S.; Mytton, O.T.; Mullins, E.W.S.; Fowler, T.A.; Falconer, C.L.; Murphy, O.B.; Langenberg, C.; Jayatunga, W.J.P.; Eddy, D.H.; Nguyen-Van-Tam, J.S. SARS-CoV-2 (COVID-19): What do we know about children? A systematic review. Clin. Infect. Dis. 2020, 71, 2469–2479. [Google Scholar] [CrossRef] [PubMed]
- Bhuiyan, M.U.; Stiboy, E.; Hassan, M.Z.; Chan, M.; Islam, M.S.; Haider, N.; Jaffe, A.; Homaira, N. Epidemiology of COVID-19 infection in young children under five years: A systematic review and meta-analysis. Vaccine 2021, 39, 667–677. [Google Scholar] [CrossRef]
- Irfan, O.; Muttalib, F.; Tang, K.; Jiang, L.; Lassi, Z.S.; Bhutta, Z. Clinical characteristics, treatment and outcomes of paediatric COVID-19: A systematic review and meta-analysis. Arch. Dis. Child. 2021, 106, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Cui, X.; Zhao, Z.; Zhang, T.; Guo, W.; Guo, W.; Zheng, J.; Zhang, J.; Dong, C.; Na, R.; Zheng, L.; et al. A systematic review and meta-analysis of children with coronavirus disease 2019 (COVID-19). J. Med. Virol. 2020, 93, 1057–1069. [Google Scholar] [CrossRef]
- Haque, M.; Gowere, M.; Nusrat, N.; Chowdhury, K.; Godman, B. The response to COVID 19 across countries and the implications for future pandemics. Bangladesh J. Med. Sci. 2021, 20, 7–14. [Google Scholar] [CrossRef]
- Mansourian, M.; Ghandi, Y.; Habibi, D.; Mehrabi, S. COVID-19 infection in children: A systematic review and meta-analysis of clinical features and laboratory findings. Arch. Pédiatrie 2021, 28, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.A.; Kundu, S.; Alam, S.S.; Hossan, T.; Kamal, M.A.; Hassan, R. Prevalence and characteristics of fever in adult and paediatric patients with coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis of 17515 patients. PLoS ONE 2021, 16, e0249788. [Google Scholar] [CrossRef]
- Mustafa, Z.U.; Salman, M.; Aldeyab, M.; Kow, C.S.; Hasan, S.S. Antimicrobial consumption among hospitalized patients with COVID-19 in Pakistan. SN Compr. Clin. Med. 2021, 3, 1691–1695. [Google Scholar] [CrossRef]
- Saini, V.; Jain, C.; Singh, N.; Alsulimani, A.; Gupta, C.; Dar, S.; Haque, S.; Das, S. Paradigm Shift in Antimicrobial Resistance Pattern of Bacterial Isolates during the COVID-19 Pandemic. Antibiotics 2021, 10, 954. [Google Scholar] [CrossRef] [PubMed]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Westwood, D.; MacFadden, D.R.; Soucy, J.-P.R.; Daneman, N. Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020, 26, 1622–1629. [Google Scholar] [CrossRef]
- Langford, B.J.; So, M.; Raybardhan, S.; Leung, V.; Soucy, J.-P.R.; Westwood, D.; Daneman, N.; MacFadden, D.R. Antibiotic prescribing in patients with COVID-19: Rapid review and meta-analysis. Clin. Microbiol. Infect. 2021, 27, 520–531. [Google Scholar] [CrossRef]
- Cheng, L.S.-K.; Chau, S.K.-Y.; Tso, E.Y.-K.; Tsang, S.W.-C.; Li, I.Y.-F.; Wong, B.K.-C.; Fung, K.S.-C. Bacterial co-infections and antibiotic prescribing practice in adults with COVID-19: Experience from a single hospital cluster. Ther. Adv. Infect. Dis. 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Grau, S.; Hernández, S.; Echeverría-Esnal, D.; Almendral, A.; Ferrer, R.; Limón, E.; Horcajada, J.P.; On behalf of the Catalan Infection Control Antimicrobial Stewardship Program. Antimicrobial Consumption among 66 Acute Care Hospitals in Catalonia: Impact of the COVID-19 Pandemic. Antibiotics 2021, 10, 943. [Google Scholar] [CrossRef] [PubMed]
- Molla, M.A.; Yeasmin, M.; Islam, K.; Sharif, M.; Amin, R.; Nafisa, T.; Ghosh, A.K.; Parveen, M.; Arif, M.H.; Alam, J.A.J.; et al. Antibiotic Prescribing Patterns at COVID-19 Dedicated Wards in Bangladesh: Findings from a Single Center Study. Infect. Prev. Pract. 2021, 3, 100134. [Google Scholar] [CrossRef] [PubMed]
- Mah-E-Muneer, S.; Hassan, Z.; Biswas, A.A.J.; Rahman, F.; Akhtar, Z.; Das, P.; Islam, A.; Chowdhury, F. Use of Antimicrobials among Suspected COVID-19 Patients at Selected Hospitals, Bangladesh: Findings from the First Wave of COVID-19 Pandemic. Antibiotics 2021, 10, 738. [Google Scholar] [CrossRef]
- Hofer, U. The cost of antimicrobial resistance. Nat. Rev. Genet. 2018, 17, 3. [Google Scholar] [CrossRef]
- Founou, R.C.; Founou, L.L.; Essack, S.Y. Clinical and economic impact of antibiotic resistance in developing countries: A systematic review and meta-analysis. PLoS ONE 2017, 12, e0189621. [Google Scholar] [CrossRef] [Green Version]
- Cassini, A.; Högberg, L.D.; Plachouras, D.; Quattrocchi, A.; Hoxha, A.; Simonsen, G.S.; Colomb-Cotinat, M.; Kretzschmar, M.E.; Devleesschauwer, B.; Cecchini, M.; et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: A population-level modelling analysis. Lancet Infect. Dis. 2019, 19, 56–66. [Google Scholar] [CrossRef] [Green Version]
- Godman, B.; Egwuenu, A.; Haque, M.; Malande, O.; Schellack, N.; Kumar, S.; Saleem, Z.; Sneddon, J.; Hoxha, I.; Islam, S.; et al. Strategies to Improve Antimicrobial Utilization with a Special Focus on Developing Countries. Life 2021, 11, 528. [Google Scholar] [CrossRef]
- Haque, M.; Meyer, J.C.; Godman, B. Potential ways to address antimicrobial resistance across India and wider exacerbated by COVID-19. J. Appl. Pharm. Sci. 2021, 11, i–vii. [Google Scholar] [CrossRef]
- Hsu, J. How COVID-19 is accelerating the threat of antimicrobial resistance. BMJ 2020, 369, m1983. [Google Scholar] [CrossRef]
- Adebisi, Y.A.; Alaran, A.J.; Okereke, M.; Oke, G.I.; Amos, O.A.; Olaoye, O.C.; Oladunjoye, I.; Olanrewaju, A.Y.; Ukor, N.A.; Lucero-Prisno, D.E. COVID-19 and Antimicrobial Resistance: A Review. Infect. Dis. Res. Treat. 2021, 14. [Google Scholar] [CrossRef] [PubMed]
- Majumder, A.A.; Rahman, S.; Cohall, D.; Bharatha, A.; Singh, K.; Haque, M.; Hilaire, M.G.-S. Antimicrobial Stewardship: Fighting Antimicrobial Resistance and Protecting Global Public Health. Infect. Drug Resist. 2020, 13, 4713–4738. [Google Scholar] [CrossRef]
- Ahmed, I.; Rabbi Md, B.; Sultana, S. Antibiotic resistance in Bangladesh: A systematic review. Int. J. Infect. Dis. 2019, 80, 54–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Global Antibiotic Resistance Partnership—Bangladesh, GARP-Bangladesh National Working Group. Antibiotic Use and Resistance in Bangladesh—Situational Analysis and Recommendations. 2018. Available online: https://cddep.org/wp-content/uploads/2018/08/ANTIBIOTIC-USE-RESISTANCE-IN-BD_2018.pdf (accessed on 1 December 2021).
- Nusrat, T.; Akter, N.; A Rahman, N.A.; Godman, B.; Rozario, D.T.D.; Haque, M. Antibiotic resistance and sensitivity pattern of Metallo-β-Lactamase Producing Gram-Negative Bacilli in ventilator-associated pneumonia in the intensive care unit of a public medical school hospital in Bangladesh. Hosp. Pract. 2020, 48, 128–136. [Google Scholar] [CrossRef] [PubMed]
- Haque, M.; Godman, B. Potential Strategies to Improve Antimicrobial Utilisation in Hospitals in Bangladesh Building on Experiences Across Developing Countries. Bangladesh J. Med. Sci. 2021, 20, 469–477. [Google Scholar] [CrossRef]
- Mardi, P.; Esmaeili, M.; Iravani, P.; Abdar, M.E.; Pourrostami, K.; Qorbani, M. Characteristics of Children With Kawasaki Disease-Like Signs in COVID-19 Pandemic: A Systematic Review. Front. Pediatr. 2021, 9, 625377. [Google Scholar] [CrossRef]
- Yasuhara, J.; Watanabe, K.; Takagi, H.; Sumitomo, N.; Kuno, T. COVID-19 and multisystem inflammatory syndrome in children: A systematic review and meta-analysis. Pediatr. Pulmonol. 2021, 56, 837–848. [Google Scholar] [CrossRef]
- Hobbs, C.V.; Khaitan, A.; Kirmse, B.M.; Borkowsky, W. COVID-19 in Children: A Review and Parallels to Other Hyperinflammatory Syndromes. Front. Pediatr. 2020, 8, 593455. [Google Scholar] [CrossRef]
- WHO. Who Discontinues Hydroxychloroquine and Lopinavir/Ritonavir Treatment Arms for COVID-19. Available online: https://www.who.int/news-room/detail/04-07-2020-who-discontinues-hydroxychloroquine-and-lopinavir-ritonavir-treatment-arms-for-covid-19 (accessed on 10 October 2021).
- Horby, P.W.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Emberson, J.; Palfreeman, A.; Raw, J.; Elmahi, E.; Prudon, B.; et al. Lopinavir–ritonavir in patients admitted to hospital with COVID-19 (RECOVERY): A randomised, controlled, open-label, platform trial. Lancet 2020, 396, 1345–1352. [Google Scholar] [CrossRef]
- Gil Martínez, V.; Salas, A.A.; Ballestín, S.S. Antiviral Therapeutic Approaches for SARS-CoV-2 Infection: A Systematic Review. Pharmaceuticals 2021, 14, 736. [Google Scholar] [CrossRef]
- The RECOVERY Collaborative Group. Effect of Hydroxychloroquine in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2020, 383, 2030–2040. [Google Scholar] [CrossRef] [PubMed]
- Dyer, O. COVID-19: Remdesivir has little or no impact on survival, WHO trial shows. BMJ 2020, 371, m4057. [Google Scholar] [CrossRef] [PubMed]
- Charan, J.; Kaur, R.J.; Bhardwaj, P.; Haque, M.; Sharma, P.; Misra, S.; Godman, B. Rapid review of suspected adverse drug events due to remdesivir in the WHO database; findings and implications. Expert Rev. Clin. Pharmacol. 2020, 14, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Abubakar, A.R.; Sani, I.H.; Godman, B.; Kumar, S.; Islam, S.; Jahan, I.; Haque, M. Systematic Review on the Therapeutic Options for COVID-19: Clinical Evidence of Drug Efficacy and Implications. Infect. Drug Resist. 2020, 13, 4673–4695. [Google Scholar] [CrossRef] [PubMed]
- Wadvalla, B.-A. COVID-19: Ivermectin’s politicisation is a warning sign for doctors. BMJ 2021, 373, n747. [Google Scholar] [CrossRef] [PubMed]
- Garegnani, L.I.; Madrid, E.; Meza, N. Misleading clinical evidence and systematic reviews on ivermectin for COVID-19. BMJ Evid.-Based Med. 2021. [Google Scholar] [CrossRef]
- Cruciani, M.; Pati, I.; Masiello, F.; Malena, M.; Pupella, S.; De Angelis, V. Ivermectin for Prophylaxis and Treatment of COVID-19: A Systematic Review and Meta-Analysis. Diagnostics 2021, 11, 1645. [Google Scholar] [CrossRef]
- Abena, P.M.; Decloedt, E.H.; Bottieau, E.; Suleman, F.; Adejumo, P.; Sam-Agudu, N.A.; TamFum, J.J.M.; Seydi, M.; Eholie, S.P.; Mills, E.J.; et al. Chloroquine and Hydroxychloroquine for the Prevention or Treatment of COVID-19 in Africa: Caution for Inappropriate Off-label Use in Healthcare Settings. Am. J. Trop. Med. Hyg. 2020, 102, 1184–1188. [Google Scholar] [CrossRef]
- Haque, M.; Godman, B. Key findings regarding COVID 19 in Bangladesh and wider and their implications. Bangladesh J. Med. Sci. 2021, 20, 199–205. [Google Scholar] [CrossRef]
- Haque, M.; Islam, S.; Iqbal, S.; Urmi, U.L.; Kamal, Z.M.; Rahman, A.; Kamal, M.; Haque, M.; Jahan, I.; Islam, Z.; et al. Availability and price changes of potential medicines and equipment for the prevention and treatment of COVID-19 among pharmacy and drug stores in Bangladesh; findings and implications. Bangladesh J. Med. Sci. 2020, 19, S36–S50. [Google Scholar] [CrossRef]
- Haque, M.; Abubakar, A.R.; O Ogunleye, O.; Sani, I.H.; Sefah, I.; Kurdi, A.; Islam, S.; Godman, B. Changes in availability, utilization, and prices of medicines and protection equipment for COVID-19 in an Urban population of Northern Nigeria. J. Res. Pharm. Pract. 2021, 10, 17–22. [Google Scholar] [CrossRef]
- World Health Organisation. Operational Considerations for Case Management of COVID-19 in Health Facility and Community: Interim Guidance. 19 March 2020. Available online: https://apps.who.int/iris/handle/10665/331492 (accessed on 3 November 2021).
- World Health Organisation. Coronavirus Disease (COVID-19) Advice for the Public: Myth Busters. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters (accessed on 3 November 2021).
- WHO. Countering Misinformation about COVID-19. 2020. Available online: https://www.who.int/news-room/feature-stories/detail/countering-misinformation-about-covid-19 (accessed on 2 November 2021).
- ECDC. Vaccines and Treatment of COVID-19. 2020. Available online: https://www.ecdc.europa.eu/en/covid-19/latest-evidence/vaccines-and-treatment (accessed on 2 November 2021).
- BMJ. Best Practice—Coronavirus Disease 2019 (COVID-19). 2021. Available online: https://bestpractice.bmj.com/topics/en-gb/3000201 (accessed on 2 November 2021).
- Kache, S.; Chisti, M.J.; Gumbo, F.; Mupere, E.; Zhi, X.; Nallasamy, K.; Nakagawa, S.; Lee, J.H.; Di Nardo, M.; de la Oliva, P.; et al. COVID-19 PICU guidelines: For high- and limited-resource settings. Pediatr. Res. 2020, 88, 705–716. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Family Welfare. Government of the People’s Republic of Bangladesh. National Guidelines on Clinical Management of Coronavirus Disease 2019 (COVID-19). 2020. Available online: http://file.portal.gov.bd/files/cs.sylhet.gov.bd/notices/245c5244_369b_4305_958d_1f70d99d6681/4c021caf6cf2915278aa3598e74f5c09.pdf (accessed on 1 November 2021).
- Bangladesh Paediatric Association (BPA). Management Guideline for Paediatric COVID-19. November 2020. Available online: https://www.bpabd.org/asset/uploads/file/COVID_BPA_2nd%20ED_3.pdf (accessed on 1 November 2021).
- Nusrat, N.; Haque, M.; Chowdhury, K.; Adnan, N.; Lutfor, A.B.; Karim, E.; Hassan, M.; Rabbany, A.; Begum, D.; Hasan, M.N.; et al. Pilot Study on the Current Management of Children with COVID-19 In Hospitals in Bangladesh; Findings and Implications. Bangladesh J. Med. Sci. 2021, 188–198. [Google Scholar] [CrossRef]
- Kumar, S.; Haque, M.; Shetty, A.; Acharya, J.; Kumar, M.; Sinha, V.; Manohar, B.; Gowere, M.; Godman, B. Current Management of Children with COVID-19 in Hospitals in India; Pilot Study and Findings. Adv. Hum. Biol. 2022, 12, 16–21. [Google Scholar]
- Ministry of Health & Family Welfare Government of India. Guidelines for Management of COVID-19 in Children (Below 18 Years). 2021. Available online: https://www.mohfw.gov.in/pdf/GuidelinesforManagementofCOVID19inCHILDREN18June2021final.pdf (accessed on 1 November 2021).
- Ministry of Health Kenya. Guidelines on the Case Management of COVID-19 in Kenya. 2021. Available online: https://www.health.go.ke/wp-content/uploads/2021/10/Final-guidelines-on-the-Management-of-Covid-19-in-Kenya-2021-Edition.pdf (accessed on 2 November 2021).
- Abu-Rub, L.; Abdelrahman, H.; Johar, A.-R.; Alhussain, H.; Hadi, H.; Eltai, N. Antibiotics Prescribing in Intensive Care Settings during the COVID-19 Era: A Systematic Review. Antibiotics 2021, 10, 935. [Google Scholar] [CrossRef]
- Nathwani, D.; Varghese, D.; Stephens, J.; Ansari, W.; Martin, S.; Charbonneau, C. Value of hospital antimicrobial stewardship programs [ASPs]: A systematic review. Antimicrob. Resist. Infect. Control 2019, 8, 1–13. [Google Scholar] [CrossRef]
- Akpan, M.R.; Isemin, N.U.; Udoh, A.E.; Ashiru-Oredope, D. Implementation of antimicrobial stewardship programmes in African countries: A systematic literature review. J. Glob. Antimicrob. Resist. 2020, 22, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Van den Bergh, D.; Messina, A.P.; Goff, D.A.; van Jaarsveld, A.; Coetzee, R.; de Wet, Y.; Bronkhorst, E.; Brink, A.; Mendelson, M.; Richards, G.A.; et al. A pharmacist-led prospective antibiotic stewardship intervention improves compliance to community-acquired pneumonia guidelines in 39 public and private hospitals across South Africa. Int. J. Antimicrob. Agents 2020, 56, 106189. [Google Scholar] [CrossRef]
- Mwita, J.C.; O Ogunleye, O.; Olalekan, A.; Kalungia, A.C.; Kurdi, A.; Saleem, Z.; Sneddon, J.; Godman, B. Key Issues Surrounding Appropriate Antibiotic Use for Prevention of Surgical Site Infections in Low- and Middle-Income Countries: A Narrative Review and the Implications. Int. J. Gen. Med. 2021, 14, 515–530. [Google Scholar] [CrossRef] [PubMed]
- Sneddon, J.; Cooper, L.; Afriyie, D.K.; A Sefah, I.; Cockburn, A.; Kerr, F.; Cameron, E.; Goldthorpe, J.; Kurdi, A.; Seaton, R.A. Supporting antimicrobial stewardship in Ghana: Evaluation of the impact of training on knowledge and attitudes of healthcare professionals in two hospitals. JAC-Antimicrob. Resist. 2020, 2, dlaa092. [Google Scholar] [CrossRef]
- Lee, C.F.; Cowling, B.J.; Feng, S.; Aso, H.; Wu, P.; Fukuda, K.; Seto, W.H. Impact of antibiotic stewardship programmes in Asia: A systematic review and meta-analysis. J. Antimicrob. Chemother. 2018, 73, 844–851. [Google Scholar] [CrossRef]
- Morales, A.; Campos, M.; Juarez, J.M.; Canovas-Segura, B.; Palacios, F.; Marin, R. A decision support system for antibiotic prescription based on local cumulative antibiograms. J. Biomed. Inform. 2018, 84, 114–122. [Google Scholar] [CrossRef] [PubMed]
- Klinker, K.P.; Hidayat, L.K.; DeRyke, C.A.; DePestel, D.D.; Motyl, M.; Bauer, K.A. Antimicrobial stewardship and antibiograms: Importance of moving beyond traditional antibiograms. Ther. Adv. Infect. Dis. 2021, 8. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, T.P. Antimicrobial Stewardship in Bangladesh: A Pharmacist’s Perspective. 2020. Available online: https://www.idstewardship.com/antimicrobial-stewardship-bangladesh-pharmacists-perspective/ (accessed on 1 November 2021).
- Hsia, Y.; Lee, B.R.; Versporten, A.; Yang, Y.; Bielicki, J.; Jackson, C.; Newland, J.; Goossens, H.; Magrini, N.; Sharland, M.; et al. Use of the WHO Access, Watch, and Reserve classification to define patterns of hospital antibiotic use (AWaRe): An analysis of paediatric survey data from 56 countries. Lancet Glob. Health 2019, 7, e861–e871. [Google Scholar] [CrossRef] [Green Version]
- Sharland, M.; Pulcini, C.; Harbarth, S.; Zeng, M.; Gandra, S.; Mathur, S.; Magrini, N. Classifying antibiotics in the WHO Essential Medicines List for optimal use—be AWaRe. Lancet Infect. Dis. 2018, 18, 18–20. [Google Scholar] [CrossRef] [Green Version]
- Broom, J.; Broom, A.; Adams, K.; Plage, S. What prevents the intravenous to oral antibiotic switch? A qualitative study of hospital doctors’ accounts of what influences their clinical practice. J. Antimicrob. Chemother. 2016, 71, 2295–2299. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.; Huttner, B.; Madaras-Kelly, K.; Nechodom, K.; Nielson, C.; Goetz, M.B.; Neuhauser, M.M.; Samore, M.H.; Rubin, M.A. Parenteral to Oral Conversion of Fluoroquinolones: Low-Hanging Fruit for Antimicrobial Stewardship Programs? Infect. Control. Hosp. Epidemiol. 2012, 33, 362–367. [Google Scholar] [CrossRef]
- Cunha, B.A. Beyond IV to PO Switch Therapy: Oral Antimicrobial Therapy. Infectious Disease News. 2015. Available online: https://www.healio.com/news/infectious-disease/20151014/beyond-iv-to-po-switch-therapy-oral-antimicrobial-therapy (accessed on 1 December 2021).
- Hoque, R.; Ahmed, S.M.; Naher, N.; Islam, M.A.; Rousham, E.K.; Islam, B.Z.; Hassan, S. Tackling antimicrobial resistance in Bangladesh: A scoping review of policy and practice in human, animal and environment sectors. PLoS ONE 2020, 15, e0227947. [Google Scholar] [CrossRef] [Green Version]
- Simba, J.; Sinha, I.; Mburugu, P.; Agweyu, A.; Emadau, C.; Akech, S.; Kithuci, R.; Oyiengo, L.; English, M. Is the effect of COVID-19 on children underestimated in low- and middle- income countries? Acta Paediatr. 2020, 109. [Google Scholar] [CrossRef]
- Paramadhas, B.D.A.; Tiroyakgosi, C.; Mpinda-Joseph, P.; Morokotso, M.; Matome, M.; Sinkala, F.; Gaolebe, M.; Malone, B.; Molosiwa, E.; Shanmugam, M.G.; et al. Point prevalence study of antimicrobial use among hospitals across Botswana; findings and implications. Exp. Rev. Anti-Infect. Ther. 2019, 17, 535–546. [Google Scholar] [CrossRef]
- Saleem, Z.; Hassali, M.A.; Versporten, A.; Godman, B.; Hashmi, F.K.; Goossens, H.; Saleem, F. A multicenter point prevalence survey of antibiotic use in Punjab, Pakistan: Findings and implications. Exp. Rev. Anti-Infect. Ther. 2019, 17, 285–293. [Google Scholar] [CrossRef] [Green Version]
- Saleem, Z.; Hassali, M.A.; Godman, B.; Versporten, A.; Hashmi, F.K.; Saeed, H.; Saleem, F.; Salman, M.; Rehman, I.U.; Khan, T.M. Point prevalence surveys of antimicrobial use: A systematic review and the implications. Exp. Rev. Anti-Infect. Ther. 2020, 18, 897–910. [Google Scholar] [CrossRef]
- Skosana, P.; Schellack, N.; Godman, B.; Kurdi, A.; Bennie, M.; Kruger, D.; Meyer, J. A point prevalence survey of antimicrobial utilisation patterns and quality indices amongst hospitals in South Africa; findings and implications. Exp. Rev. Anti-Infect. Ther. 2021, 19, 1353–1366. [Google Scholar] [CrossRef]
- Ogunleye, O.O.; Oyawole, M.R.; Odunuga, P.T.; Kalejaye, F.; Yinka-Ogunleye, A.F.; Olalekan, A.; Ogundele, S.O.; Ebruke, B.E.; Richard, A.K.; Paramadhas, B.D.A.; et al. A multicentre point prevalence study of antibiotics utilization in hospitalised patients in an urban secondary and a tertiary healthcare facilities in Nigeria: Findings and implications. Exp. Rev. Anti-Infect. Ther. 2021, 1–10. [Google Scholar] [CrossRef]
- Mustafa, Z.U.; Salman, M.; Yasir, M.; Godman, B.; Majeed, H.A.; Kanwal, M.; Iqbal, M.; Riaz, M.B.; Hayat, K.; Hasan, S.S. Antibiotic consumption among hospitalized neonates and children in Punjab province, Pakistan. Exp. Rev. Anti-Infect. Ther. 2021, 1–9. [Google Scholar] [CrossRef]
- Okoth, C.; Opanga, S.; Okalebo, F.; Oluka, M.; Kurdi, A.; Godman, B. Point prevalence survey of antibiotic use and resistance at a referral hospital in Kenya: Findings and implications. Hosp. Pract. 2018, 46, 128–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurdi, A.; Hasan, A.J.; Baker, K.I.; Seaton, R.A.; Ramzi, Z.S.; Sneddon, J.; Godman, B. A multicentre point prevalence survey of hospital antibiotic prescribing and quality indices in the Kurdistan regional government of Northern Iraq: The need for urgent action. Exp. Rev. Anti-Infect. Ther. 2020, 19, 805–814. [Google Scholar] [CrossRef] [PubMed]
- Afriyie, D.K.; A Sefah, I.; Sneddon, J.; Malcolm, W.; McKinney, R.; Cooper, L.; Kurdi, A.; Godman, B.; Seaton, R.A. Antimicrobial point prevalence surveys in two Ghanaian hospitals: Opportunities for antimicrobial stewardship. JAC-Antimicrob. Resist. 2020, 2, dlaa001. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Momanyi, L.; Opanga, S.; Nyamu, D.; Oluka, M.; Kurdi, A.; Godman, B. Antibiotic prescribing patterns at a leading referral hospital in Kenya: A point prevalence survey. J. Res. Pharm. Pract. 2019, 8, 149–154. [Google Scholar] [CrossRef]
- Panfili, F.M.; Roversi, M.; D’Argenio, P.; Rossi, P.; Cappa, M.; Fintini, D. Possible role of vitamin D in COVID-19 infection in pediatric population. J. Endocrinol. Investig. 2020, 44, 27–35. [Google Scholar] [CrossRef]
- Caliskan, T.; Saylan, B. Smoking and comorbidities are associated with COVID-19 severity and mortality in 565 patients treated in Turkey: A retrospective observational study. Rev. Assoc. Med. Bras. 2020, 66, 1679–1684. [Google Scholar] [CrossRef]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Sharland, M.; Gandra, S.; Huttner, B.; Moja, L.; Pulcini, C.; Zeng, M.; Mendelson, M.; Cappello, B.; Cooke, G.; Magrini, N.; et al. Encouraging AWaRe-ness and discouraging inappropriate antibiotic use—the new 2019 Essential Medicines List becomes a global antibiotic stewardship tool. Lancet Infect. Dis. 2019, 19, 1278–1280. [Google Scholar] [CrossRef]
- Hsia, Y.; Sharland, M.; Jackson, C.; Wong, I.C.K.; Magrini, N.; A Bielicki, J. Consumption of oral antibiotic formulations for young children according to the WHO Access, Watch, Reserve (AWaRe) antibiotic groups: An analysis of sales data from 70 middle-income and high-income countries. Lancet Infect. Dis. 2018, 19, 67–75. [Google Scholar] [CrossRef]
- Van den Bosch, C.M.; Hulscher, M.E.; Akkermans, R.P.; Wille, J.; Geerlings, S.E.; Prins, J.M. Appropriate antibiotic use reduces length of hospital stay. J. Antimicrob. Chemother. 2016, 72, 923–932. [Google Scholar] [CrossRef]
- Cyriac, J.M.; James, E. Switch over from intravenous to oral therapy: A concise overview. J. Pharmacol. Pharmacother. 2014, 5, 83–87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The RECOVERY Collaborative Group. Dexamethasone in Hospitalized Patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef]
- Kumar, P.; Kumar, M.; Bedi, O.; Gupta, M.; Kumar, S.; Jaiswal, G.; Rahi, V.; Yedke, N.G.; Bijalwan, A.; Sharma, S.; et al. Role of vitamins and minerals as immunity boosters in COVID-19. Inflammopharmacology 2021, 29, 1001–1016. [Google Scholar] [CrossRef]
- Milani, G.; Macchi, M.; Guz-Mark, A. Vitamin C in the Treatment of COVID-19. Nutrients 2021, 13, 1172. [Google Scholar] [CrossRef]
- Versporten, A.; Zarb, P.; Caniaux, I.; Gros, M.-F.; Drapier, N.; Miller, M.; Jarlier, V.; Nathwani, D.; Goossens, H.; Koraqi, A.; et al. Antimicrobial consumption and resistance in adult hospital inpatients in 53 countries: Results of an internet-based global point prevalence survey. Lancet Glob. Health 2018, 6, e619–e629. [Google Scholar] [CrossRef] [Green Version]
- Niaz, Q.; Godman, B.; Campbell, S.; Kibuule, D. Compliance to prescribing guidelines among public health care facilities in Namibia; findings and implications. Int. J. Clin. Pharm. 2020, 42, 1227–1236. [Google Scholar] [CrossRef]
- Nakwatumbah, S.; Kibuule, D.; Godman, B.; Haakuria, V.; Kalemeera, F.; Baker, A.; Mubita, M.; Mwangana, M. Compliance to guidelines for the prescribing of antibiotics in acute infections at Namibia’s national referral hospital: A pilot study and the implications. Exp. Rev. Anti-Infect. Ther. 2017, 15, 713–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olaru, I.D.; Meierkord, A.; Godman, B.; Ngwenya, C.; Fitzgerald, F.; Dondo, V.; Ferrand, R.A.; Kranzer, K. Assessment of antimicrobial use and prescribing practices among pediatric inpatients in Zimbabwe. J. Chemother. 2020, 32, 456–459. [Google Scholar] [CrossRef] [PubMed]
- Sefah, I.A.; Essah, D.O.; Kurdi, A.; Sneddon, J.; Alalbila, T.M.; Kordorwu, H.; Godman, B. Assessment of adherence to pneumonia guidelines and its determinants in an ambulatory care clinic in Ghana: Findings and implications for the future. JAC-Antimicrob. Resist. 2021, 3, dlab080. [Google Scholar] [CrossRef] [PubMed]
- Gitaka, J.; Kamita, M.; Mureithi, D.; Ndegwa, D.; Masika, M.; Omuse, G.; Ngari, M.; Makokha, F.; Mwaura, P.; Mathai, R.; et al. Combating antibiotic resistance using guidelines and enhanced stewardship in Kenya: A protocol for an implementation science approach. BMJ Open 2020, 10, e030823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, S.M.; Meyer, J.C.; Godman, B. Why Compliance to National Prescribing Guidelines is Important Especially across Sub-Saharan Africa and Suggestions for the Future. J. Biomed. Pharm. Sci. 2021, 4, 309. [Google Scholar]
- MacBride-Stewart, S.; McTaggart, S.; Kurdi, A.; Sneddon, J.; McBurney, S.; Nascimento, R.C.R.M.; Mueller, T.; Kwon, H.Y.; Morton, A.; Seaton, R.A.; et al. Initiatives and reforms across Scotland in recent years to improve prescribing; findings and global implications of drug prescriptions. Int. J. Clin. Exp. Med. 2021, 14, 2563–2586. [Google Scholar]
- Godman, B.; Fadare, J.; Kwon, H.-Y.; Dias, C.Z.; Kurdi, A.; Godói, I.P.D.; Kibuule, D.; Hoxha, I.; Opanga, S.; Saleem, Z.; et al. Evidence-based public policy making for medicines across countries: Findings and implications for the future. J. Comp. Eff. Res. 2021, 10, 1019–1052. [Google Scholar] [CrossRef]
- Dlamini, N.N.; Meyer, J.C.; Kruger, D.; Kurdi, A.; Godman, B.; Schellack, N. Feasibility of using point prevalence surveys to assess antimicrobial utilisation in public hospitals in South Africa: A pilot study and implications. Hosp. Pract. 2019, 47, 88–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Adults/General (May 2020) | Treatment (General)
|
| Children (November 2020) | Diagnosis and comorbidity
|
| Hospital | Date Survey Conducted | Total Number of Admitted Children during the Study Period | Total Number with COVID-19 (No.) | % of Admitted Children with COVID-19 | Number of Children with Confirmed COVID-19 (No. and %) | Number of Boys (No.) | Number of Girls (No.) | 0 to 5 Years of Age (no.) | 6 to 10 Years of Age (No.) | 11 to 18 Years of Age (No.) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1—Priv | 20 July 2021 | 14 | 2 | 14.3% | 2 (100%) | 0 | 2 | 1 | 0 | 1 |
| 2—Priv | 25 July 2021 | 18 | 1 | 5.6% | 1 (100%) | 1 | 0 | 0 | 1 | 0 |
| 3—Priv | 30 July 2021 | 19 | 2 | 10.5% | 1 (one susp.) | 1 | 1 | 1 | 1 | 0 |
| 4—Priv | 16 July 2021 | 32 | 2 | 6.3% | 0 (2 susp.) | 1 | 1 | 2 | 0 | 0 |
| 5—Priv | 11 August 2021 | 40 | 5 | 12.5% | 5 (100%) | 2 | 3 | 2 | 2 | 1 |
| 6—Priv | 30 July 2021 | 41 | 3 | 7.3% | 3 (100%) | 3 | 0 | 2 | 0 | 1 |
| 7—Pub | 04 February 2021 | 44 | 13 | 29.5% | 1 (12 susp.) | 5 | 8 | 11 | 2 | 0 |
| 8—Priv | 11 July 2021 | 50 | 5 | 10.0% | 0 (5 susp.) | 4 | 11 | 3 | 2 | 0 |
| 9—Priv | 24 July 2021 | 61 | 5 | 8.2% | 5 (100%) | 3 | 2 | 1 | 2 | 2 |
| 10—Priv | 11 August 2021 | 65 | 3 | 4.6% | 3 (100%) | 2 | 1 | 3 | 0 | 0 |
| 11—Priv | 01 August 2021 | 68 | 6 | 8.8% | 6 (100%) | 5 | 1 | 3 | 3 | 0 |
| 12—Priv | 30 July 21 | 75 | 15 | 20.0% | 15 (100%) | 9 | 6 | 4 | 9 | 2 |
| 13—Priv | 10 August 2021 | 85 | 4 | 4.7% | 4 (100%) | 2 | 2 | 3 | 1 | 0 |
| 14—Priv | 04 August 2021 | 103 | 14 | 13.6% | 0 (14 susp.) | 10 | 4 | 13 | 0 | 1 |
| 15—Pub | 31 July 2021 | 105 | 1 | 1.0% | 1 (100%) | 1 | 0 | 1 | 0 | 0 |
| 16—Pub | 31 August 2021 | 125 | 5 | 4.0% | 5 (100%) | 4 | 1 | 2 | 3 | 0 |
| 17—Pub | 04 August 2021 | 68 | 3 | 4.4% | 3 (100%) | 2 | 1 | 2 | 0 | 1 |
| 18—Pub | 31 July 2021 | 210 | 26 | 12.4% | 26 (100%) | 15 | 11 | 13 | 6 | 7 |
| 19—Pub | 11 July 2021 | 256 | 3 | 1.2% | 3 (100%) | 2 | 1 | 2 | 1 | 0 |
| 20—Pub | 08 October 2021 | 362 | 3 | 0.55% | 3 (100%) | 1 | 2 | 0 | 0 | 3 |
| 21—Pub | 11 July 2021 | 382 | 3 | 0.8% | 2 (1 susp) | 2 | 1 | 3 | 0 | 0 |
| 22—Pub | 08 November 2021 | 583 | 8 | 1.4% | 8 (100%) | 5 | 3 | 6 | 1 | 1 |
| 23—Pub | 08 November 2021 | 442 | 5 | 1.1% | 5 (100%) | 1 | 4 | 4 | 1 | 0 |
| 24—Pub | 17 July 2021 | 654 | 9 | 1.4% | 9 (100% | 5 | 4 | 9 | 0 | 0 |
| 3902 | 146 | 3.7% | 111—76% confirmed | 86 (58.9%) | 60 (41.1%) | 91 (62.3%) | 35 (24.0%) | 20 (13.7%) |
| Hospital | Principal Documented Reasons for Hospital Admission for Children with Suspected COVID-19 during the Study Period | Total Number of Children Subsequently Admitted with COVID-19 to PICUs | Principal Reasons for PICU Admission |
|---|---|---|---|
| 1—Priv | Respiratory distress | 2 | Low oxygen saturation, comorbidities |
| 2—Priv | Fever, coughing, vomiting | 0 | Not applicable |
| 3—Priv | Fever, cough, low SPO2, respiratory distress, vomiting, diarrhoea | 0 | Not applicable |
| 4—Priv | Fever, cough, respiratory distress | 0 | Not applicable |
| 5—Priv | Prolonged fever, respiratory distress, diarrhoea | 1 | Low oxygen saturation, extensive involvement in high-resolution CT scan |
| 6—Priv | Prolonged fever, cough, respiratory distress | 0 | Not applicable |
| 7—Pub | Fever, cough, respiratory distress | 0 (1 referred) * | Unexplained bleeding |
| 8—Priv | Prolonged fever, breathing difficulties, diarrhoea | 1 | Shock |
| 9—Priv | Fever, cough, feeding difficulties | 1 | Shock, myocarditis |
| 10—Priv | Respiratory distress, cough, feeding difficulties | 0 | Not applicable |
| 11—Priv | Fever, cough, feeding difficulties | 2 | Low oxygen saturation, respiratory distress, shock |
| 12—Priv | Fever, respiratory distress, feeding difficulty | 0 | Not applicable |
| 13—Priv | Prolonged fever, cough, breathing difficulty/respiratory distress | 0 | Not applicable |
| 14—Priv | Fever, respiratory distress, feeding difficulty | 0 | Not applicable |
| 15—Pub | Fever, cough, respiratory distress | 0 | Not applicable |
| 16—Pub | Prolonged fever, cough, Breathing difficulties/respiratory distress, diarrhoea | 0 | Not applicable |
| 17—Pub | Fever, cough, respiratory distress | 0 | Not applicable |
| 18—Pub | Fever, cough, low SPO2, respiratory distress, vomiting | 9 | Fever, shock, low oxygen saturation, vomiting, feeding difficulties |
| 19—Pub | Fever, cough, respiratory distress | 0 | Not applicable |
| 20—Pub | Fever, cough, respiratory distress | 1 | Low oxygen saturation and comorbidities |
| 21—Pub | Prolonged fever, cough, respiratory distress | 0 | Not applicable |
| 22—Pub | Fever, cough, respiratory distress | 2 | Perinatal asphyxia, feeding difficulty, low oxygen saturation |
| 23—Pub | Fever, cough, respiratory distress | 0 | Not applicable |
| 24—Pub | Prolonged fever, respiratory distress, feeding difficulties | 0 | Not appliable |
| Hospital | Number and % Prescribed Antibiotics | Empiric or Following CST | Principal Antibiotics Prescribed (Actual or Class) for Children with COVID-19 | Antiviral Medicines Prescribed | Antiparasitic Medicines Prescribed | Duration of Antibiotic Prescribing (Days) | Clinical Assessment of Antibiotics (Days after Start of Treatment) |
|---|---|---|---|---|---|---|---|
| 1—Priv | 2 (100%) | All Empiric | Carbapenem, cephalosporins | No | No | 4–7 | 3 |
| 2—Priv | 1 (100%) | All Empiric | Ceftriaxone | No | No | 5 | 5 |
| 3—Priv | 2 (100%) | All Empiric | Ceftriaxone, ciprofloxacin | No | No | 3 and 5 | 3–5 |
| 4—Priv | 2 (100%) | All Empiric | Ampicillin, aminoglycosides, cephalosporins | No | No | 5 | 2 |
| 5—Priv | 5 (100%) | All Empiric | Cephalosporins, quinolones | Remdesivir (2 patients) | No | 7 | 2 |
| 6—Priv | 2 (66.7%) | All Empiric | Cephalosporins | No | No | 5–7 | 5–7 |
| 7—Pub | 13 (100%) | All Empiric | Ceftriaxone, amikacin, meropenem | No | No | 5–7 | 3 |
| 8—Priv | 5 (100%) | All Empiric | Carbapenem, aminoglycosides, cephalosporins | No | No | 5–7 | 3 |
| 9—Priv | 2 (40%) | All Empiric | Vancomycin, meropenem, co-amoxiclav | Remdesivir (1 patient) | No | 7–10 | 3 |
| 10—Priv | 3 (100%) | All Empiric | Ceftriaxone | No | No | 10 | 3 |
| 11—Priv | 4 (66.7%) | All Empiric | Ceftriaxone, ciprofloxacin, amikacin | Remdesivir (1 patient) | No | 3–7 | 3 |
| 12—Priv | 2 (13.3%) | 1 Empiric/1 CST | Aminoglycosides, cephalosporins, quinolones | No | No | 5–7 | Not recorded |
| 13—Priv | 4 (100%) | All Empiric | Aminoglycosides, carbapenems, cephalosporins | No | Ivermectin (1 patient) | 10 | 3–5 |
| 14—Priv | 14 (100%) | All Empiric | Aminoglycosides, penicillin, cephalosporins | No | No | 5–7 | 3 |
| 15—Pub | 1 (100%) | All Empiric | Cefixime | No | No | 7 | 3 |
| 16—Pub | 5 (100%) | All Empiric | Aminoglycosides, carbapenems, cephalosporins | No | No | 7–10 | 2–3 |
| 17—Pub | 3 (100%) | All Empiric | Ceftriaxone, ceftazidim, gentamicin | No | No | 3–7 | 3 |
| 18—Pub | 26 (100%) | All Empiric | Ceftriaxone, ceftazidim, meropenem, vancomycin, flucloxacillin, amikacin | No | No | 5–11 | 5–10 |
| 19—Pub | 3 (100%) | All Empiric | Ceftriaxone, meropenem | No | No | 7 | 3 |
| 20—Pub | 3 (100%) | All Empiric | Penicillin, carbapenem, aminoglycosides | Remdesivir (3 patients), acyclovir (1 patient) | No | 8–14 | 3 |
| 21—Pub | 3 (100%) | All Empiric | Amikacin, meropenem, clarithromycine | No | No | 7 | 2 |
| 22—Pub | 7 (87.5%) | 6 Empiric/1 CST | Ceftriaxone, amikacin, meropenem | No | No | 4–7 | 3 |
| 23—Pub | 5 (100%) | All Empiric | Ceftriaxone, amikacin, meropenem | No | No | 7–14 | 3 |
| 24—Pub | 9 (100%) | All Empiric | Aminoglycosides, carbapenem, macrolides | No | No | 7 days (minimum) | 3 |
| Total | 126 children—(86.3%) | 124 empiric (98.4%) | 8 children (5.5%) | 1 child (0.7%) |
| Guideline adherence | Number of Children Administered Antibiotics | Number of Children Not Administered Antibiotics | % Administered Antibiotics |
|---|---|---|---|
| Hospitals where clinicians stated that they had followed the Paediatric Association guidelines | 74 | 15 | 83.1% (n = 89) |
| Hospitals where clinicians stated that they had not followed the Paediatric Association guidelines | 52 | 5 | 91.2% (n = 57) |
| Key Data Sets | Rationale |
|---|---|
| Number of paediatric patients being treated in the hospital during the ten-day period and the number with COVID-19 | To gain insight into current prevalence rates among children admitted to hospitals in Bangladesh compared with other conditions |
| Whether COVID-19 was suspected or confirmed—confirmed with PCR tests | To gain additional insight into current COVID-diagnostic practices |
| The ages of admitted children | Patients’ ages were broken down into 3 bands: 0–5 years; 6–10 years; 11–18 years for comparative purposes based on the pilot study in both Bangladesh and India [62,63] |
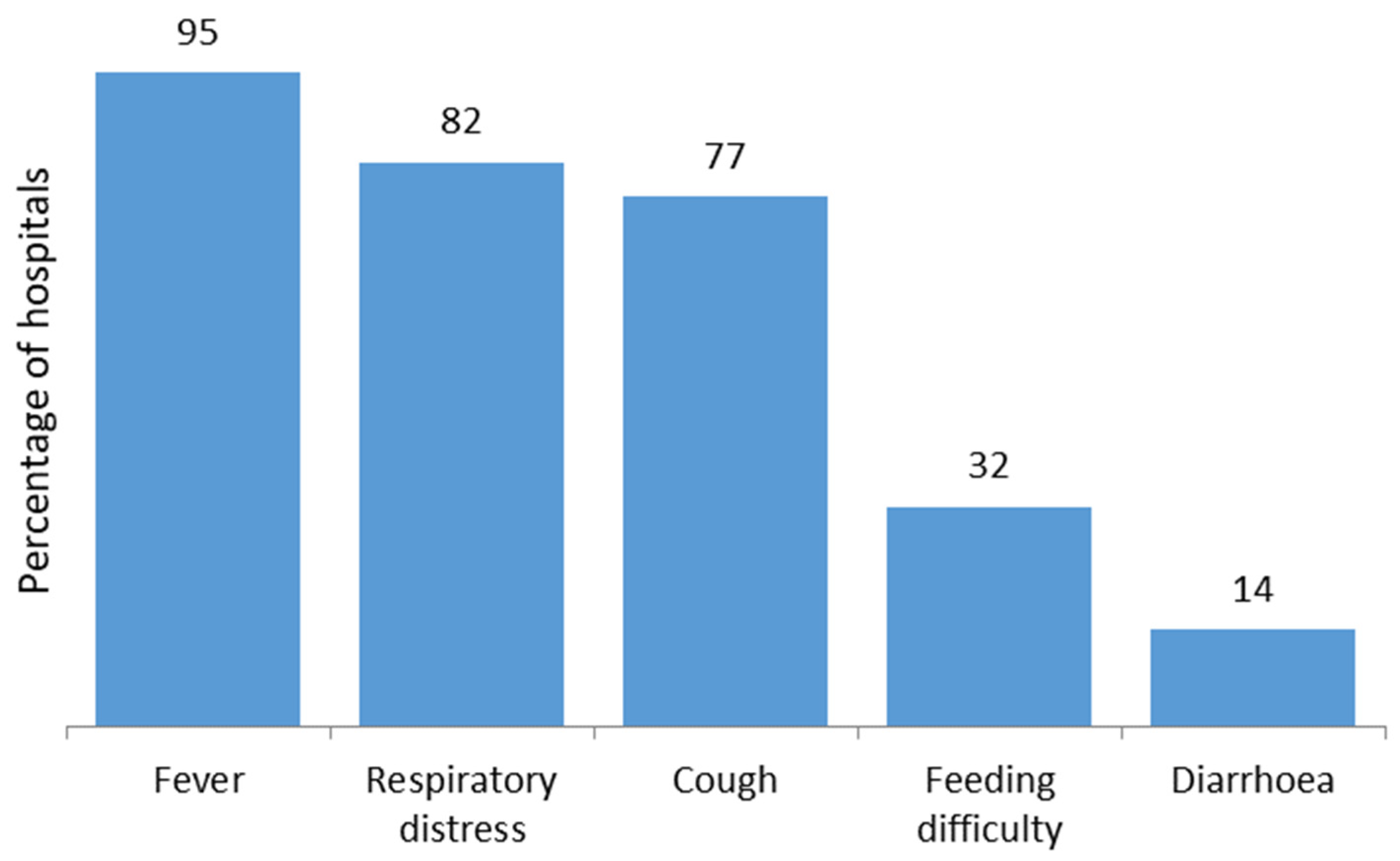
| Principal reason for admission to hospital with actual/suspected COVID-19 |
|
| Comorbidities | Based on evidence amongst adults that certain comorbidities do have an impact on morbidity and mortality associated with COVID-19 [94,95] |
| Number of children admitted to PICU and the rationale |
|
| Number of children prescribed antibiotics and the antibiotics prescribed (by ATC Level 4 Grouping or individual antibiotics), and whether empiric or following CST findings |
|
| Route of administration, whether the rationale for antibiotic prescribing was re-assessed, and, if so, after how many days, and total length of antibiotic prescriptions |
|
| The extent of prescribing of antivirals, e.g., remdesivir, antimalarials, e.g., hydroxychloroquine, and antiparasitic medicines, e.g., ivermectin |
|
| The extent of prescribing of dexamethasone and other steroids, including methylprednisolone | Seen as potentially beneficial, especially among hospitalised patients, and endorsed in the guidelines [46,61,100] |
| Use of supplements/immune boosters including vitamins C or D or zinc | Discussed in the Bangladesh Paediatric Guidelines, with publications suggesting potential benefit [61,101,102] |
| Adherence to current guidelines, including those developed by the Bangladesh Paediatric Association —Table 1 [50] | |
| Outcome—fully recovered, morbidity or mortality |
|
| Possible costs (principally private hospitals) (based on local currency) |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chowdhury, K.; Haque, M.; Nusrat, N.; Adnan, N.; Islam, S.; Lutfor, A.B.; Begum, D.; Rabbany, A.; Karim, E.; Malek, A.; et al. Management of Children Admitted to Hospitals across Bangladesh with Suspected or Confirmed COVID-19 and the Implications for the Future: A Nationwide Cross-Sectional Study. Antibiotics 2022, 11, 105. https://doi.org/10.3390/antibiotics11010105
Chowdhury K, Haque M, Nusrat N, Adnan N, Islam S, Lutfor AB, Begum D, Rabbany A, Karim E, Malek A, et al. Management of Children Admitted to Hospitals across Bangladesh with Suspected or Confirmed COVID-19 and the Implications for the Future: A Nationwide Cross-Sectional Study. Antibiotics. 2022; 11(1):105. https://doi.org/10.3390/antibiotics11010105
Chicago/Turabian StyleChowdhury, Kona, Mainul Haque, Nadia Nusrat, Nihad Adnan, Salequl Islam, Afzalunnessa Binte Lutfor, Dilara Begum, Arif Rabbany, Enamul Karim, Abdul Malek, and et al. 2022. "Management of Children Admitted to Hospitals across Bangladesh with Suspected or Confirmed COVID-19 and the Implications for the Future: A Nationwide Cross-Sectional Study" Antibiotics 11, no. 1: 105. https://doi.org/10.3390/antibiotics11010105
APA StyleChowdhury, K., Haque, M., Nusrat, N., Adnan, N., Islam, S., Lutfor, A. B., Begum, D., Rabbany, A., Karim, E., Malek, A., Jahan, N., Akter, J., Ashraf, S., Hasan, M. N., Hassan, M., Akhter, N., Mazumder, M., Sihan, N., Naher, N., ... Godman, B. (2022). Management of Children Admitted to Hospitals across Bangladesh with Suspected or Confirmed COVID-19 and the Implications for the Future: A Nationwide Cross-Sectional Study. Antibiotics, 11(1), 105. https://doi.org/10.3390/antibiotics11010105










