Candida Periprosthetic Joint Infection: Is It Curable?
Abstract
1. Introduction
2. Epidemiology
3. Pathogenesis and Risk Factors
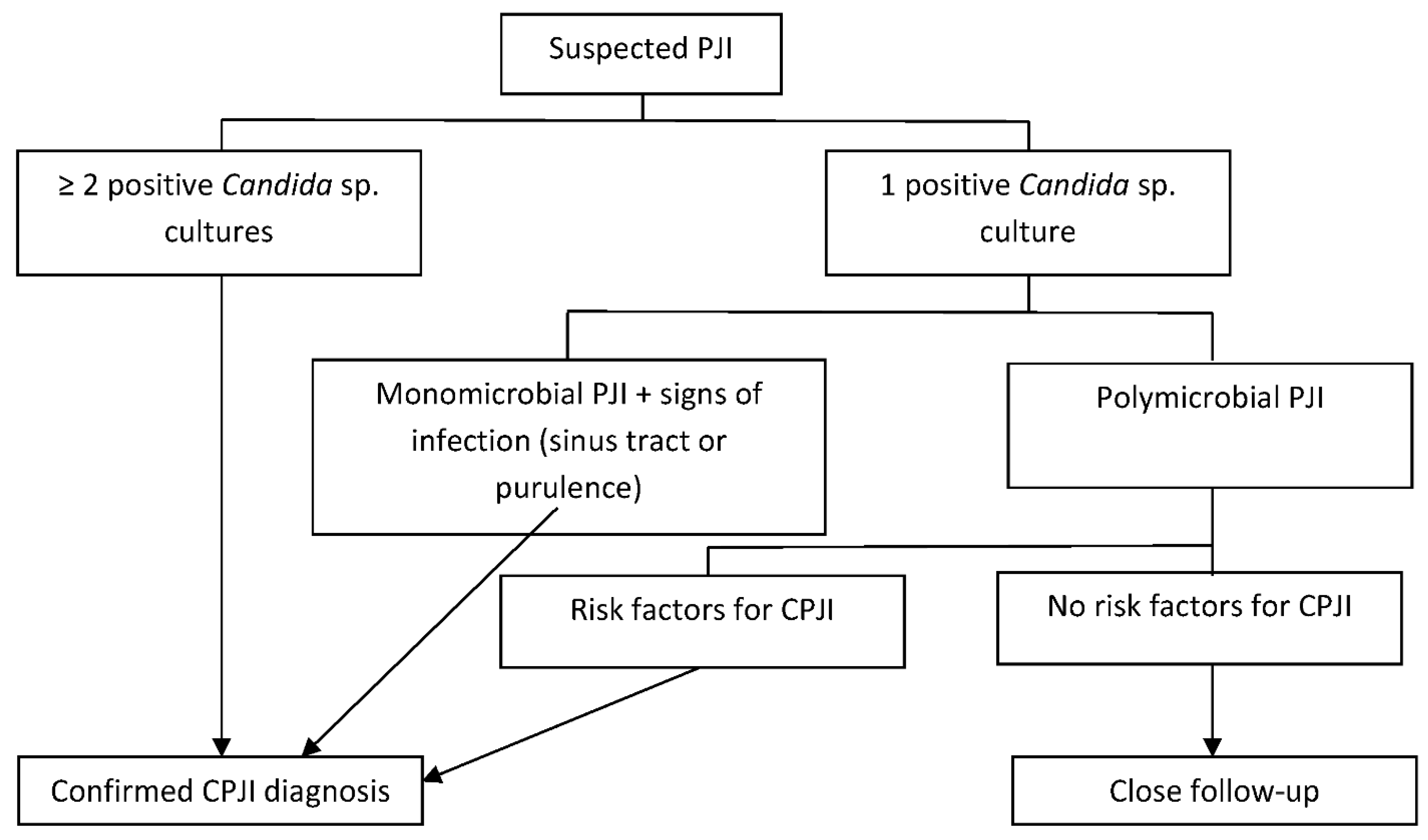
4. Clinical Manifestations and Diagnosis
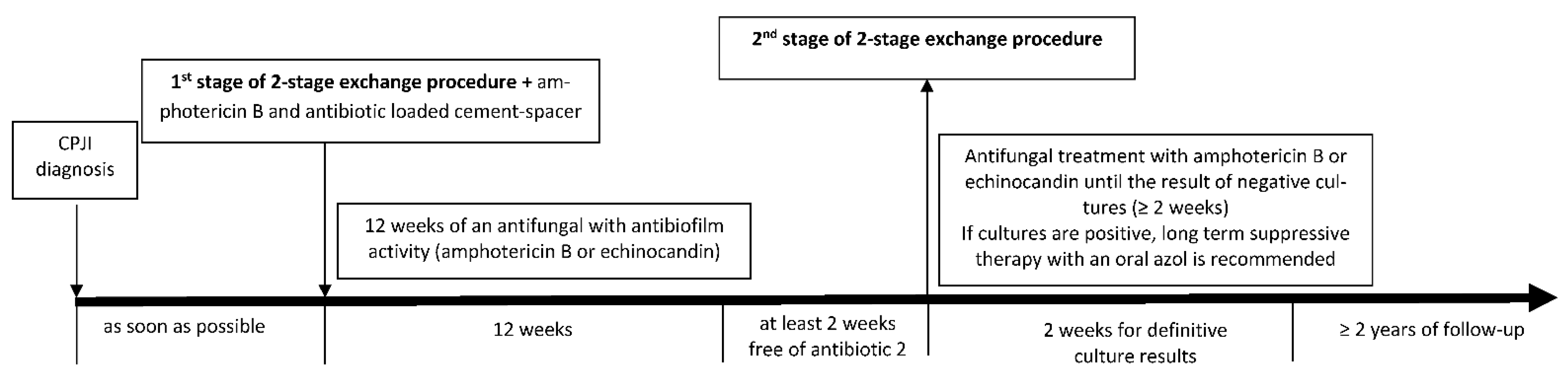
5. Medical and Surgical Treatment
6. Prognosis and Prevention
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| PJI | periprosthetic joint infection |
| CPJI | Candida periprosthetic joint infection |
References
- Tande, A.J.; Patel, R. Prosthetic Joint Infection. Clin. Microbiol. Rev. 2014, 27, 302–345. [Google Scholar] [CrossRef] [PubMed]
- Escolà-Vergé, L.; Rodríguez-Pardo, D.; Lora-Tamayo, J.; Morata, L.; Murillo, O.; Vilchez, H.; Sorli, L.; Carrión, L.G.; Barbero, J.M.; Palomino-Nicás, J.; et al. Candida Periprosthetic Joint Infection: A Rare and Difficult-to-Treat Infection. J. Infect. 2018, 77, 151–157. [Google Scholar] [CrossRef]
- Osmon, D.R.; Berbari, E.F.; Berendt, A.R.; Lew, D.; Zimmerli, W.; Steckelberg, J.M.; Rao, N.; Hanssen, A.; Wilson, W.R. Diagnosis and Management of Prosthetic Joint Infection: Clinical Practice Guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 2013, 56, e1–e25. [Google Scholar] [CrossRef] [PubMed]
- Ariza, J.; Cobo, J.; Baraia-Etxaburu, J.; Benito, N.; Bori, G.; Cabo, J.; Corona, P.; Esteban, J.; Horcajada, J.P.; Lora-Tamayo, J.; et al. Executive Summary of Management of Prosthetic Joint Infections. Clinical Practice Guidelines by the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC). Enferm. Infect. Microbiol. Clin. 2017, 35, 189–195. [Google Scholar] [CrossRef]
- Pappas, P.G.; Kauffman, C.A.; Andes, D.R.; Clancy, C.J.; Marr, K.A.; Ostrosky-Zeichner, L.; Reboli, A.C.; Schuster, M.G.; Vazquez, J.A.; Walsh, T.J.; et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin. Infect. Dis. 2015, civ933. [Google Scholar] [CrossRef]
- Parvizi, J.; Gehrke, T.; Chen, A.F. Proceedings of the International Consensus on Periprosthetic Joint Infection. Bone Jt. J. 2013, 95, 1450–1452. [Google Scholar] [CrossRef]
- Belden, K.; Cao, L.; Chen, J.; Deng, T.; Fu, J.; Guan, H.; Jia, C.; Kong, X.; Kuo, F.-C.; Li, R.; et al. Hip and Knee Section, Fungal Periprosthetic Joint Infection, Diagnosis and Treatment: Proceedings of International Consensus on Orthopedic Infections. J. Arthroplast. 2019, 34, S387–S391. [Google Scholar] [CrossRef]
- Benito, N.; Mur, I.; Ribera, A.; Soriano, A.; Rodríguez-Pardo, D.; Sorlí, L.; Cobo, J.; Fernández-Sampedro, M.; del Toro, M.; Guío, L.; et al. The Different Microbial Etiology of Prosthetic Joint Infections According to Route of Acquisition and Time after Prosthesis Implantation, Including the Role of Multidrug-Resistant Organisms. J. Clin. Med. 2019, 8, 673. [Google Scholar] [CrossRef]
- Benito, N.; Franco, M.; Ribera, A.; Soriano, A.; Rodriguez-Pardo, D.; Sorlí, L.; Fresco, G.; Fernández-Sampedro, M.; Dolores Del Toro, M.; Guío, L.; et al. Time Trends in the Aetiology of Prosthetic Joint Infections: A Multicentre Cohort Study. Clin. Microbiol. Infect. 2016, 22, 732.e1–732.e8. [Google Scholar] [CrossRef]
- Peel, T.N.; Cheng, A.C.; Buising, K.L.; Choong, P.F.M. Microbiological Aetiology, Epidemiology, and Clinical Profile of Prosthetic Joint Infections: Are Current Antibiotic Prophylaxis Guidelines Effective? Antimicrob. Agents Chemother. 2012, 56, 2386–2391. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, V.K.; Bakhshi, H.; Ecker, N.U.; Parvizi, J.; Gehrke, T.; Kendoff, D. Organism Profile in Periprosthetic Joint Infection: Pathogens Differ at Two Arthroplasty Infection Referral Centers in Europe and in the United States. J. Knee Surg. 2014, 27, 399–406. [Google Scholar] [CrossRef]
- Azzam, K.; Parvizi, J.; Jungkind, D.; Hanssen, A.; Fehring, T.; Springer, B.; Bozic, K.; Della Valle, C.; Pulido, L.; Barrack, R. Microbiological, Clinical, and Surgical Features of Fungal Prosthetic Joint Infections: A Multi-Institutional Experience. J. Bone Jt. Surg. Am. Vol. 2009, 91, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Riaz, T.; Tande, A.J.; Steed, L.L.; Demos, H.A.; Salgado, C.D.; Osmon, D.R.; Marculescu, C.E. Risk Factors for Fungal Prosthetic Joint Infection. J. Bone Jt. Infect. 2020, 5, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Saconi, E.S.; de Carvalho, V.C. Prosthetic Joint Infection Due to Candida Species. Medicine 2020, 99, e19735. [Google Scholar] [CrossRef] [PubMed]
- Cobo, F.; Rodríguez-Granger, J.; Sampedro, A.; Aliaga-Martínez, L.; Navarro-Marí, J.M. Candida Prosthetic Joint Infection. A Review of Treatment Methods. J. Bone Jt. Infect. 2017, 2, 114–121. [Google Scholar] [CrossRef]
- Pappas, P.G.; Lionakis, M.S.; Arendrup, M.C.; Ostrosky-Zeichner, L.; Kullberg, B.J. Invasive Candidiasis. Nat. Rev. Dis. Primers 2018, 4, 18026. [Google Scholar] [CrossRef] [PubMed]
- McCarty, T.P.; Pappas, P.G. Invasive Candidiasis. Infect. Dis. Clin. N. Am. 2016, 30, 103–124. [Google Scholar] [CrossRef] [PubMed]
- Kullberg, B.J.; Arendrup, M.C. Invasive Candidiasis. N. Engl. J. Med. 2015, 373, 1445–1456. [Google Scholar] [CrossRef]
- Hube, B. From Commensal to Pathogen: Stage- and Tissue-Specific Gene Expression of Candida albicans. Curr. Opin. Microbiol. 2004, 7, 336–341. [Google Scholar] [CrossRef]
- Finkel, J.S.; Mitchell, A.P. Genetic Control of Candida albicans Biofilm Development. Nat. Rev. Microbiol. 2011, 9, 109–118. [Google Scholar] [CrossRef]
- Kuhn, D.M. Comparison of Biofilms Formed by Candidaalbicans and Candidaparapsilosis on Bioprosthetic Surfaces. Infect. Immun. 2002, 70, 878–888. [Google Scholar] [CrossRef] [PubMed]
- Sam, Q.; Chang, M.; Chai, L. The Fungal Mycobiome and Its Interaction with Gut Bacteria in the Host. Int. J. Mol. Sci. 2017, 18, 330. [Google Scholar] [CrossRef] [PubMed]
- García-Oltra, E.; García-Ramiro, S.; Martínez, J.C.; Tibau, R.; Bori, G.; Bosch, J.; Mensa, J.; Soriano, A. Prosthetic joint infection by Candida spp. Rev. Esp. Quimioter. 2011, 24, 37–41. [Google Scholar] [PubMed]
- Brown, T.S.; Petis, S.M.; Osmon, D.R.; Mabry, T.M.; Berry, D.J.; Hanssen, A.D.; Abdel, M.P. Periprosthetic Joint Infection With Fungal Pathogens. J. Arthroplast. 2018, 33, 2605–2612. [Google Scholar] [CrossRef]
- Kuiper, J.W.; van den Bekerom, M.P.; van der Stappen, J.; Nolte, P.A.; Colen, S. 2-Stage Revision Recommended for Treatment of Fungal Hip and Knee Prosthetic Joint Infections: An Analysis of 164 Patients, 156 from the Literature and 8 Own Cases. Acta Orthop. 2013, 84, 517–523. [Google Scholar] [CrossRef]
- McNally, M.; Sousa, R.; Wouthuyzen-Bakker, M.; Chen, A.F.; Soriano, A.; Vogely, H.C.; Clauss, M.; Higuera, C.A.; Trebše, R. The EBJIS Definition of Periprosthetic Joint Infection: A Practical Guide for Clinicians. Bone Jt. J. 2021, 103, 18–25. [Google Scholar] [CrossRef]
- Kuhn, D.M.; George, T.; Chandra, J.; Mukherjee, P.K.; Ghannoum, M.A. Antifungal Susceptibility of Candida Biofilms: Unique Efficacy of Amphotericin B Lipid Formulations and Echinocandins. Antimicrob. Agents Chemother. 2002, 46, 1773–1780. [Google Scholar] [CrossRef]
- Nett, J.E. Future Directions for Anti-Biofilm Therapeutics Targeting Candida. Expert Rev. Anti Infect. Ther. 2014, 12, 375–382. [Google Scholar] [CrossRef]
- Iñigo, M.; Pemán, J.; Del Pozo, J.L. Antifungal Activity against Candida Biofilms. Int. J. Artif. Organs 2012, 35, 780–791. [Google Scholar] [CrossRef]
- Mukherjee, P.K.; Chandra, J. Candida Biofilms: Development, Architecture, and Resistance. Microbiol. Spectrum. 2015, 3. [Google Scholar] [CrossRef]
- Ueng, S.W.N.; Lee, C.-Y.; Hu, C.; Hsieh, P.-H.; Chang, Y. What Is the Success of Treatment of Hip and Knee Candidal Periprosthetic Joint Infection? Clin. Orthop. Relat. Res. 2013, 471, 3002–3009. [Google Scholar] [CrossRef]
- Hwang, B.H.; Yoon, J.Y.; Nam, C.H.; Jung, K.A.; Lee, S.C.; Han, C.D.; Moon, S.H. Fungal Peri-Prosthetic Joint Infection after Primary Total Knee Replacement. J. Bone Jt. Surg. Br. 2012, 94, 656–659. [Google Scholar] [CrossRef] [PubMed]
- Anagnostakos, K.; Kelm, J.; Schmitt, E.; Jung, J. Fungal Periprosthetic Hip and Knee Joint Infections. J. Arthroplast. 2012, 27, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Phelan, D.M.; Osmon, D.R.; Keating, M.R.; Hanssen, A.D. Delayed Reimplantation Arthroplasty for Candidal Prosthetic Joint Infection: A Report of 4 Cases and Review of the Literature. Clin. Infect. Dis. 2002, 34, 930–938. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Li, X.; Du, Y.; Peng, Y.; Wu, W.; Zhou, Y. Success Rate of Fungal Peri-Prosthetic Joint Infection Treated by 2-Stage Revision and Potential Risk Factors of Treatment Failure: A Retrospective Study. Med. Sci. Monit. 2018, 24, 5549–5557. [Google Scholar] [CrossRef] [PubMed]
- Selmon, G.P.F.; Slater, R.N.S.; Shepperd, J.N.; Wright, E.P. Successful 1-Stage Exchange Total Knee Arthroplasty for Fungal Infection. J. Arthroplast. 1998, 13, 114–115. [Google Scholar] [CrossRef]
- Klatte, T.O.; Kendoff, D.; Kamath, A.F.; Jonen, V.; Rueger, J.M.; Frommelt, L.; Gebauer, M.; Gehrke, T. Single-Stage Revision for Fungal Peri-Prosthetic Joint Infection: A Single-Centre Experience. Bone Jt. J. 2014, 96-B, 492–496. [Google Scholar] [CrossRef]
- Katragkou, A.; Chatzimoschou, A.; Simitsopoulou, M.; Dalakiouridou, M.; Diza-Mataftsi, E.; Tsantali, C.; Roilides, E. Differential Activities of Newer Antifungal Agents against Candida Albicans and Candida Parapsilosis Biofilms. Antimicrob. Agents Chemother. 2008, 52, 357–360. [Google Scholar] [CrossRef]
- Schoof, B.; Jakobs, O.; Schmidl, S.; Klatte, T.O.; Frommelt, L.; Gehrke, T.; Gebauer, M. Fungal Periprosthetic Joint Infection of the Hip: A Systematic Review. Orthop. Rev. 2015, 7. [Google Scholar] [CrossRef]
- Bruce, A.S.W.; Kerry, R.M.; Norman, P.; Stockley, I. Fluconazole-Impregnated Beads in the Management of Fungal Infection of Prosthetic Joints. J. Bone Jt. Surg. Br. Vol. 2001, 83, 183–184. [Google Scholar] [CrossRef]
- Deelstra, J.J.; Neut, D.; Jutte, P.C. Successful Treatment of Candida Albicans–Infected Total Hip Prosthesis with Staged Procedure Using an Antifungal-Loaded Cement Spacer. J. Arthroplast. 2013, 28, 374.e5–374.e8. [Google Scholar] [CrossRef] [PubMed]
- Marra, F.; Robbins, G.M.; Masri, B.A.; Duncan, C.; Wasan, K.M.; Kwong, E.H.; Jewesson, P.J. Amphotericin B-Loaded Bone Cement to Treat Osteomyelitis Caused by Candida albicans. Can. J. Surg. 2001, 44, 383. [Google Scholar]
- Goss, B.; Lutton, C.; Weinrauch, P.; Jabur, M.; Gillett, G.; Crawford, R. Elution and Mechanical Properties of Antifungal Bone Cement. J. Arthroplast. 2007, 22, 902–908. [Google Scholar] [CrossRef] [PubMed]
- Kweon, C.; McLaren, A.C.; Leon, C.; McLemore, R. Amphotericin B Delivery From Bone Cement Increases With Porosity but Strength Decreases. Clin. Orthop. Relat. Res. 2011, 469, 3002–3007. [Google Scholar] [CrossRef] [PubMed]
- Harmsen, S.; McLaren, A.C.; Pauken, C.; McLemore, R. Amphotericin B Is Cytotoxic at Locally Delivered Concentrations. Clin. Orthop. Relat. Res. 2011, 469, 3016–3021. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, B.; McLaren, A.C.; Pauken, C.; McLemore, R. Liposomal Formulation Increases Local Delivery of Amphotericin from Bone Cement: A Pilot Study. Clin. Orthop. Relat. Res. 2012, 470, 2671–2676. [Google Scholar] [CrossRef]
- Fagotti, L.; Tatka, J.; Salles, M.J.C.; Queiroz, M.C. Risk Factors and Treatment Options for Failure of a Two-Stage Exchange. Curr. Rev. Musculoskelet. Med. 2018, 11, 420–427. [Google Scholar] [CrossRef] [PubMed]
| Study (Year) | Number of Patients (n) | Surgical Treatment (n) | Antifungal Treatment (n) | Antifungal-Loaded Cement Spacers (n) | Follow-Up | Outcome (n) |
|---|---|---|---|---|---|---|
| Saconi et al. (2020) [14] | 11 | Resection arthroplasty 6 | Fluconazol 6 | No | Range 5.6–74 months | Remission 5 Lost to follow-up 1 |
| One-stage exchange 4 | Fluconazol 2 Itraconazol 1 Micafungin 1 | No | Range 2.1–84 months | Remission 2 Failure 1 Lost to follow-up 1 | ||
| Two-stage exchange 1 | Voriconazol, itraconazol 1 | No | 48 months | Remission 1 | ||
| Escolà-Vergé et al. (2018) [2] | 35 | Prosthesis removal 20 | Azoles 13 Antibiofilm-containing regimen * 6 No antifungal 1 | Amphotericin B 3 | 24 months | Remission 13 Failure 7 |
| Debridement with prosthesis retention 15 | Azoles 10 Antibiofilm-containing regimen * 5 | No | 24 months | Remission 4 Failure 11 | ||
| Brown et al. (2018) [24] | 25 | Two-stage exchange 11 | Fluconazol 25 | Amphotericin B 10 | Not reported | Remission 5 Failure 6 |
| Debridement with prosthesis retention 5 | No | Failure 5 | ||||
| Resection arthroplasty 5 | No | Remission 2 Failure 3 | ||||
| Prosthesis retention and suppressive therapy 3 | No | Remission 3 | ||||
| One-stage exchange 1 | No | Remission 1 | ||||
| Gao et al. (2018) [35] | 14 | Two-stage exchange 14 | Fluconazol 11 Caspofungin, fluconazol 1 Vorinconazol 1 Amphotericin B, caspofungin, fluconazol, voriconazol 1 | Amphotericin B 3 Voriconazol 2 Fluconazol 2 | Mean 65.1 months Range 25–129 months | Remission 10 Failure 4 |
| Ueng et al. (2013) [31] | 16 | Two-stage exchange 9 | Fluconazol 9 | Amphotericin B 5 | Mean 41 months Range 28–90 months | Remission 8 Failure 1 |
| Resection arthroplasty 7 | Fluconazol 7 | Amphotericin B 1 | Remission 4 Failure 3 | |||
| Hwang et al. (2012) [32] | 28 | Two-stage exchange 24 | Amphotericin B 21 Amphotericin B, fluconazol 3 Fluconazol 4 | No | Mean 4.3 years Range 2.6–6.1 years | Remission 22 Failure 2 |
| Debridement with prosthesis retention 4 | No | Failure 4 | ||||
| García-Oltra et al. (2011) [23] | 10 | Two-stage exchange 7 | Fluconazol 5 Anidulafungin, fluconazol 1 Caspofungin, fluconazol 1 | No | Mean 31 months Range 2–67 months | Failure 7 |
| Debridement with prosthesis retention 3 | Fluconazol 3 | No | Failure 3 | |||
| Azzam et al. (2009) [12] | 31 | Two-stage exchange 19 | Fluconazol 23 Caspofungin, fluconazol 3 Amphotericin B 5 | Amphotericin B 5 | Mean 45 months Range from 24 months to 11 years | Remission 9 Failure 10 |
| Resection arthroplasty 10 (5 with previous debridement failure) | Remission 6 Failure 4 | |||||
| Debridement with prosthesis retention 7 | No | Failure 7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Escolà-Vergé, L.; Rodríguez-Pardo, D.; Corona, P.S.; Pigrau, C. Candida Periprosthetic Joint Infection: Is It Curable? Antibiotics 2021, 10, 458. https://doi.org/10.3390/antibiotics10040458
Escolà-Vergé L, Rodríguez-Pardo D, Corona PS, Pigrau C. Candida Periprosthetic Joint Infection: Is It Curable? Antibiotics. 2021; 10(4):458. https://doi.org/10.3390/antibiotics10040458
Chicago/Turabian StyleEscolà-Vergé, Laura, Dolors Rodríguez-Pardo, Pablo S. Corona, and Carles Pigrau. 2021. "Candida Periprosthetic Joint Infection: Is It Curable?" Antibiotics 10, no. 4: 458. https://doi.org/10.3390/antibiotics10040458
APA StyleEscolà-Vergé, L., Rodríguez-Pardo, D., Corona, P. S., & Pigrau, C. (2021). Candida Periprosthetic Joint Infection: Is It Curable? Antibiotics, 10(4), 458. https://doi.org/10.3390/antibiotics10040458







