Association between Periodontal Disease and Systemic Inflammatory Conditions Using Electronic Health Records: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
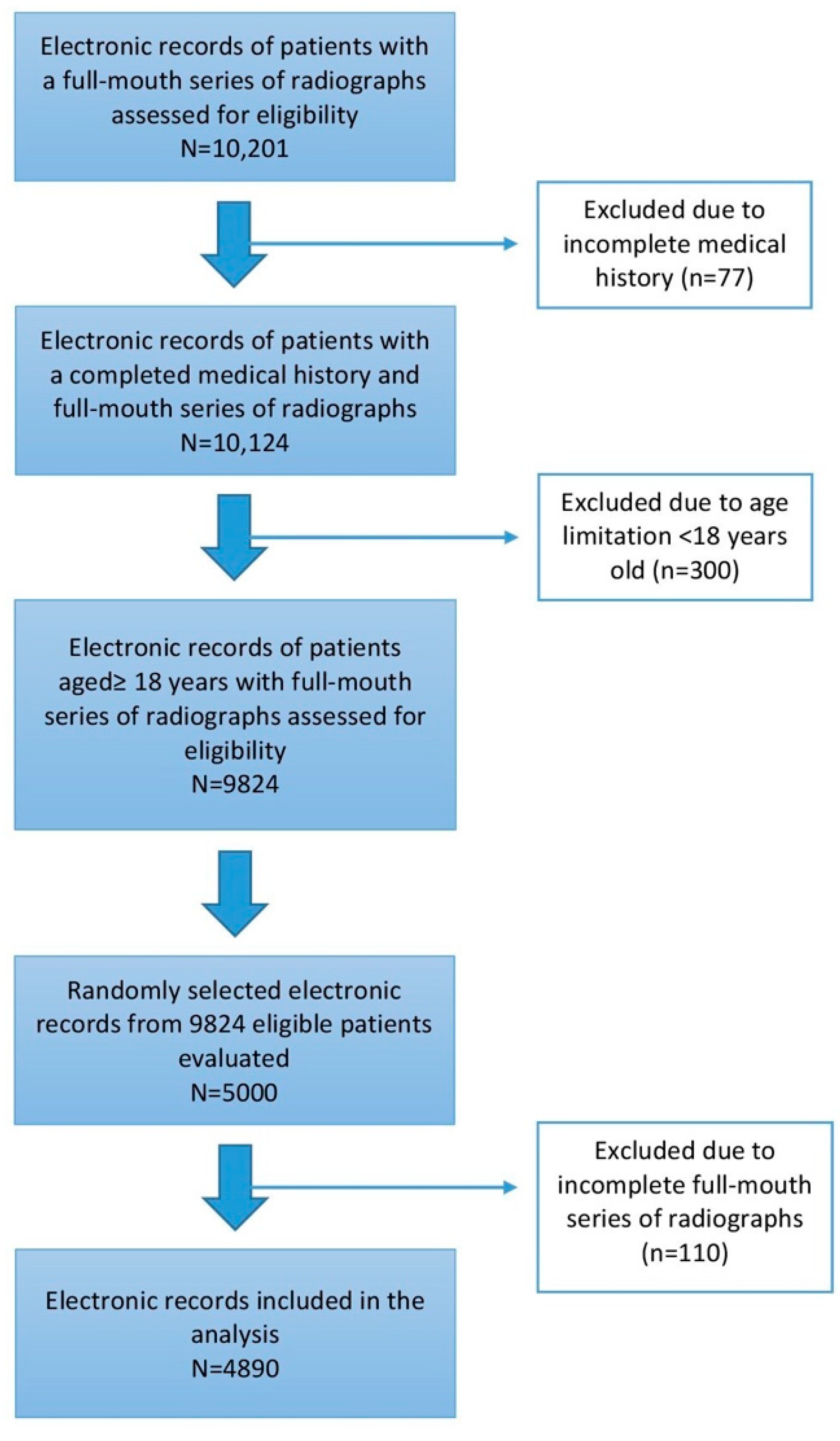
2.1. Sample
2.2. Data Extraction
- (1)
- None/mild bone loss when the examined individuals presented generalized (>30% of the teeth) bone loss of ≤25%.
- (2)
- Moderate bone loss when the examined individuals exhibited generalized (>30% of the teeth) bone loss of 26–50%.
- (3)
- Severe bone loss when the examined individuals showed generalized (>30% of the teeth) bone loss of >50% or ≥4 posterior teeth (premolars and/or molars) with >50% bone loss.
2.3. Inter-/Intraexaminer Calibration
2.4. Statistical Analysis
3. Results
3.1. Patient Records Included and Population Characteristics
3.2. Prevalence of Self-Reported Systemic Conditions
3.3. Self-Reported Systemic Conditions Associated with Severity of Bone Loss
3.4. Self-Reported Systemic Conditions Associated with Missing Teeth
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Miller, W. The human mouth as a focus of infection. Dent. Cosm. 1891, 33, 689–713. [Google Scholar] [CrossRef]
- Baltch, A.L.; Pressman, H.L.; Schaffer, C.; Smith, R.P.; Hammer, M.C.; Shayegani, M.; Michelsen, P. Bacteremia in patients undergoing oral procedures. Study following parenteral antimicrobial prophylaxis as recommended by the American Heart Association, 1977. Arch. Intern. Med. 1988, 148, 1084–1088. [Google Scholar] [CrossRef]
- Williams, R.C.; Offenbacher, S. Periodontal medicine: The emergence of a new branch of periodontology. Periodontology 2000 2003, 23, 9–12. [Google Scholar] [CrossRef]
- Kinane, D.F.; Attstrom, R. Advances in the pathogenesis of periodontitis. Group B consensus report of the fifth European Workshop in Periodontology. J. Clin. Periodontol. 2005, 32 (Suppl. 6), 130–131. [Google Scholar] [CrossRef]
- Van Dyke, T.E.; van Winkelhoff, A.J. Infection and inflammatory mechanisms. J. Periodontol. 2013, 84 (Suppl. 4), S1–S7. [Google Scholar]
- Loos, B.G. Periodontal medicine: Work in progress. J. Clin. Periodontol. 2016, 43, 470–471. [Google Scholar] [CrossRef]
- Molloy, J.; Wolff, L.F.; Lopez-Guzman, A.; Hodges, J.S. The association of periodontal disease parameters with systemic medical conditions and tobacco use. J. Clin. Periodontol. 2004, 31, 625–632. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Grossi, S.; Genco, R.; Machtet, E.; Ho, A.; Koch, G.; Dunford, R.; Zambon, J.; Hausmann, E. Assessment of risk for periodontal disease. II. Risk indicators for alveolar bone loss. J. Periodontol. 1995, 66, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Torrungruang, K.; Nisapakultorn, K.; Sutdhibhisal, S.; Tamsailom, S.; Rojanasomsith, K.; Vanichjakvong, O.; Prapakamol, S.; Premsirinirund, T.; Pusiri, T.; Jaratkulangkoon, O.; et al. The effect of cigarette smoking on the severity of periodontal disease among older Thai adults. J. Periodontol. 2005, 76, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Tomar, S.L.; Asma, S. Smoking-attributable periodontitis in the United States: Findings from NHANES III. National Health and Nutrition Examination Survey. J. Periodontol. 2000, 71, 743–751. [Google Scholar] [CrossRef]
- Leech, M.T.; Bartold, P.M. The association between rheumatoid arthritis and periodontitis. Best Pract. Res. Clin. Rheumatol. 2015, 29, 189–201. [Google Scholar] [CrossRef]
- de Pablo, P.; Dietrich, T.; McAlindon, T.E. Association of periodontal disease and tooth loss with rheumatoid arthritis in the US population. J. Rheumatol. 2008, 35, 70–76. [Google Scholar]
- Shen, T.C.; Chang, P.Y.; Lin, C.L.; Wei, C.-C.; Tu, C.-Y.; Hsia, T.-C.; Shih, C.-M.; Hsu, W.-H.; Sung, F.-C.; Kao, C.-H. Risk of periodontal disease in patients with asthma: A nationwide population-based retrospective cohort study. J. Periodontol. 2017, 88, 723–730. [Google Scholar] [CrossRef]
- Hyyppä, T.M.; Koivikko, A.; Paunio, K.U. Studies on periodontal conditions in asthmatic children. Acta Odontol. Scand. 1979, 37, 15–20. [Google Scholar] [CrossRef]
- Laurikainen, K.; Kuusisto, P. Comparison of the oral health status and salivary flow rate of asthmatic patients with those of nonasthmatic adults—Results of a pilot study. Allergy 1998, 53, 316–319. [Google Scholar] [CrossRef]
- Stensson, M.; Wendt, L.K.; Koch, G.; Oldaeus, G.; Ramberg, P.; Birkhed, D. Oral health in young adults with long-term, controlled asthma. Acta Odontol. Scand. 2011, 69, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Gomes-Filho, I.S.; Soledade-Marques, K.R.; Seixas da Cruz, S.; Passos-Soares, J.D.S.; Trindade, S.C.; Souza-Machado, A.; Rubira-Bullen, I.R.F.; Cerqueira, E.D.M.M.; Barreto, M.L.; De Santana, T.C.; et al. Does periodontal infection have an effect on severe asthma in adults? J. Periodontol. 2013, 85, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Bandyopadhyay, D.; Marlow, N.M.; Fernandes, J.K.; Leite, R.S. Periodontal disease progression and glycaemic control among Gullah African Americans with type-2 diabetes. J. Clin. Periodontol. 2010, 37, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.W.; Burt, B.A.; Becker, M.P.; Genco, R.J.; Shlossman, M. Glycemic control and alveolar bone loss progression in type 2 diabetes. Ann. Periodontol. 1998, 3, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Dandona, P.; Aljada, A.; Bandyopadhyay, A. Inflammation: The link between insulin resistance, obesity and diabetes. Trends Immunol. 2004, 25, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.A.; Dobmeyer, J.M.; Dobmeyer, T.S.; Pape, M.; Ottmann, O.G.; Helm, E.B.; Hoelzer, D.; Rossol, R. Demonstration of the Th1 to Th2 cytokine shift during the course of HIV-1 infection using cytoplasmic cytokine detection on single cell level by flow cytometry. AIDS 1997, 11, 1111–1118. [Google Scholar] [CrossRef]
- Pinching, A.J.; McManus, T.J.; Jeffries, D.J.; Moshtael, O.; Donaghy, M.; Parkin, J.M.; Munday, P.E.; Harris, J.R. Studies of cellular immunity in male homosexuals in London. Lancet 1983, 2, 126–130. [Google Scholar] [CrossRef]
- Roux-Lombard, P.; Modoux, C.; Cruchaud, A.; Dayer, J.M. Purified blood monocytes from HIV 1-infected patients produce high levels of TNF alpha and IL-1. Clin. Immunol. Immunopathol. 1989, 50, 374–384. [Google Scholar] [CrossRef]
- Robinson, P.G.; Adegboye, A.; Rowland, R.W.; Yeung, S.; Johnson, N.W. Periodontal diseases and HIV infection. Oral Dis. 2002, 8, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Hileman, C.O.; Eckard, A.R.; McComsey, G.A. Bone loss in HIV: A contemporary review. Curr. Opin. Endocrinol. Diabetes Obes. 2015, 22, 446–451. [Google Scholar] [CrossRef] [PubMed]
- Aukrust, P.; Haug, C.J.; Ueland, T.; Lien, E.; Müller, F.; Espevik, T.; Bollerslev, J.; Frøland, S.S. Decreased bone formative and enhanced resorptive markers in human immunodeficiency virus infection: Indication of normalization of the bone-remodeling process during highly active antiretroviral therapy. J. Clin. Endocrinol. Metab. 1999, 84, 145–150. [Google Scholar]
- Ryder, M.I. An update on HIV and periodontal disease. J. Periodontol. 2002, 73, 1071–1078. [Google Scholar] [CrossRef]
- Aichelmann-Reidy, M.E.; Wrigley, D.L.; Gunsolley, J.C. HIV infection and bone loss due to periodontal disease. J. Periodontol. 2010, 81, 877–884. [Google Scholar] [CrossRef]
- Loe, H.; Anerud, A.; Boysen, H.; Morrison, E. Natural history of periodontal disease in man: Rapid, moderate and no loss of attachment in Sri Lankan laborers 14–46 years of age. J. Clin. Periodontol. 1986, 13, 431–445. [Google Scholar] [CrossRef]
- Patel, M.H.; Kumar, J.V.; Moss, M.E. Diabetes and tooth loss: An analysis of data from the National Health and Nutrition Examination Survey, 2003–2004. J. Am. Dent. Assoc. 2013, 144, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Kapp, J.M.; Boren, S.A.; Yun, S.; LeMaster, J. Diabetes and tooth loss in a national sample of dentate adults reporting annual dental visits. Prev. Chronic Dis. 2007, 4, A59. [Google Scholar] [PubMed]
- Marques, C.P.C.; Maor, Y.; De Andrade, M.S.; Rodrigues, V.P.; Benatti, B.B. Possible evidence of systemic lupus erythematosus and periodontal disease association mediated by Toll-like receptors 2 and 4. Clin. Exp. Immunol. 2016, 183, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Corrêa, J.D.; Calderaro, D.C.; Ferreira, G.A.; Mendonça, S.M.S.; Fernandes, G.R.; Xiao, E.; Teixeira, A.L.; Leys, E.J.; Graves, D.T.; Silva, T.A. Subgingival microbiota dysbiosis in systemic lupus erythematosus: Association with periodontal status. Microbiome 2017, 5, 34. [Google Scholar] [CrossRef]
- Elter, J.R.; Offenbacher, S.; Toole, J.F.; Beck, J.D. Relationship of periodontal disease and edentulism to stroke/TIA. J. Dent. Res. 2003, 82, 998–1001. [Google Scholar] [CrossRef] [PubMed]
- Joshipura, K.J.; Hung, H.C.; Rimm, E.B.; Willett, W.C.; Ascherio, A. Periodontal disease, tooth loss, and incidence of ischemic stroke. Stroke 2003, 34, 47–52. [Google Scholar] [CrossRef]
- Lowe, G.D. Dental disease, coronary heart disease and stroke, and inflammatory markers: What are the associations, and what do they mean? Circulation 2004, 109, 1076–1078. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Van Steenberghe, D. From osseoperception to implant-mediated sensory-motor interactions and related clinical implications. J. Oral. Rehabil. 2006, 33, 282–292. [Google Scholar] [CrossRef]
- Listl, S. Oral health conditions and cognitive functioning in middle and later adulthood. BMC Oral Health 2014, 14, 70. [Google Scholar] [CrossRef]
- Wada, K.; Yatsuya, H.; Ouyang, P.; Otsuka, R.; Mitsuhashi, H.; Takefuji, S.; Matsushita, K.; Sugiura, K.; Hotta, Y.; Toyoshima, H.; et al. Self-reported medical history was generally accurate among Japanese workplace population. J. Clin. Epidemiol. 2009, 62, 306–313. [Google Scholar] [CrossRef]
- Newell, S.A.; Girgis, A.; Sanson-Fisher, R.W.; Savolainen, N.J. The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: A critical review. Am. J. Prev. Med. 1999, 17, 211–229. [Google Scholar] [CrossRef]
- Martin, L.M.; Leff, M.; Calonge, N.; Garrett, C.; Nelson, D.E. Validation of self-reported chronic conditions and health services in a managed care population. Am. J. Prev. Med. 2000, 18, 215–218. [Google Scholar] [CrossRef]
- Hirschfeld, J.; Higham, J.; Chatzistavrianou, D.; Blair, F.; Richards, A.; Chapple, I.L.C. Systemic disease or periodontal disease? Distinguishing causes of gingival inflammation: A guide for dental practitioners. Part 1: Immune-mediated, autoinflammatory, and hereditary lesions. Br. Dent. J. 2019, 227, 961–966. [Google Scholar] [CrossRef] [PubMed]
- Hirschfeld, J.; Higham, J.; Blair, F.; Richards, A.; Chapple, I.L.C. Systemic disease or periodontal disease? Distinguishing causes of gingival inflammation: A guide for dental practitioners. Part 2: Cancer related, infective, and other causes of gingival pathology. Br. Dent. J. 2019, 227, 1029–1034. [Google Scholar] [CrossRef] [PubMed]
- Alshihayb, T.S.; Kaye, E.A.; Zhao, Y.; Leone, C.W.; Heaton, B. The impact of periodontitis exposure misclassification bias from partial-mouth measurements on association with diabetes and cardiovascular disease. J. Clin. Periodontol. 2020, 47, 1457–1465. [Google Scholar] [CrossRef] [PubMed]
- Akesson, L.; Håkansson, J.; Rohlin, M. Comparison of panoramic and intraoral radiography and pocket probing for the measurement of the marginal bone level. J. Clin. Periodontol. 1992, 19, 326–332. [Google Scholar] [CrossRef]
- Isacco, C.G.; Ballini, A.; De Vito, D.; Nguyen, K.C.D.; Cantore, S.; Bottalico, L.; Quagliuolo, L.; Boccellino, M.; Di Domenico, M.; Santacroce, L.; et al. Rebalance the oral microbiota as efficacy tool in endocrine, metabolic, and immune disorders. Endocr. Metab. Immune Disord. Drug Targets 2020. [Google Scholar] [CrossRef] [PubMed]
- Hajishengallis, G. Periodontitis: From microbial immune subversion to systemic inflammation. Nat. Rev. Immunol. 2015, 15, 30–44. [Google Scholar] [CrossRef]
- Cooper, P.R.; Palmer, L.J.; Chapple, I.L. Neutrophil extracellular traps as a new paradigm in innate immunity: Friend or foe? Periodontology 2013, 63, 165–197. [Google Scholar] [CrossRef]
- Giuggia, B.; Bergandi, L.; Comba, A.; Alovisi, M.; Carpegna, G.; Scotti, N.; Pasqualini, D.; Berutti, E. Variation of vascular and blood indicators of early endothelial dysfunction after root canal therapy: A clinical and biomolecular study. G. Ital. Endod. 2019, 33. [Google Scholar] [CrossRef]
- Hatanaka, E.; Monteagudo, P.T.; Marrocos, M.S.; Campa, A. Neutrophils and monocytes as potentially important sources of proinflammatory cytokines in diabetes. Clin. Exp. Immunol. 2006, 146, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Yasunari, K.; Watanabe, T.; Nakamura, M. Reactive oxygen species formation by polymorphonuclear cells and mononuclear cells as a risk factor of cardiovascular diseases. Curr. Pharm. Biotechnol. 2006, 7, 73–80. [Google Scholar] [CrossRef] [PubMed]
| Total Population (N = 4890) | Bone Loss | p-Value * | |||
|---|---|---|---|---|---|
| None to Mild (n = 3837–78.5%) | Moderate (n = 730–14.9%) | Severe (n = 323–6.6%) | |||
| Age (mean ± SD) in years | 54.06 ± 17.85 | 51.72 ± 18.23 | 63.86 ± 13.21 | 59.61 ± 13.05 | <0.001 † |
| Males (%) | 52.7 | 51.2 | 55.2 | 63.8 | <0.001 ‡ |
| Missing teeth (mean ± SD) | 3.54 ± 3.93 | 2.87 ± 3.47 | 5.77 ± 4.43 | 6.52 ± 4.67 | <0.001 † |
| Tobacco use (%) | 14.9 | 13.1 | 18.1 | 30.0 | <0.001 ‡ |
| Self-Reported Systemic Inflammatory Diseases | Total (n = 4890) | Males (n = 2575) | Females (n = 2315) | p-Value * |
|---|---|---|---|---|
| Hypertension | 29.1 | 31.9 | 25.9 | <0.001 |
| Arthritis | 21.6 | 17.2 | 26.3 | <0.001 |
| Asthma | 11.1 | 6.1 | 11.1 | <0.001 |
| Diabetes | 10.6 | 11.7 | 9.3 | <0.001 |
| Cancer | 9.1 | 8.9 | 9.5 | 0.49 |
| Irritable bowel syndrome | 3.9 | 2.0 | 6.0 | <0.001 |
| Hepatitis | 2.0 | 2.3 | 1.6 | 0.06 |
| Lupus | 0.5 | 0.0 | 1.0 | <0.001 |
| HIV positive/AIDS | 0.5 | 0.9 | 0.1 | <0.001 |
| Parkinson’s disease | 0.3 | 0.4 | 0.2 | 0.19 |
| Self-Reported Systemic Inflammatory Diseases | Bone Loss | p-Value | |||
|---|---|---|---|---|---|
| Total Population (n = 4890) | None to Mild (n = 3837–78.5%) | Moderate (n = 730–14.9%) | Severe (n = 323–6.6%) | ||
| Hypertension | 1421 (29.1) | 1000 (26.1) | 291 (39.9) | 130 (40.2) | <0.001 |
| Arthritis | 1054 (21.6) | 777 (20.3) | 209 (28.6) | 68 (21.1) | <0.001 |
| Asthma | 415 (8.5) | 355 (9.3) | 42 (5.8) | 18 (5.6) | 0.001 |
| Diabetes | 516 (10.6) | 348 (9.1) | 115 (15.8) | 53 (16.4) | 0.006 |
| Cancer | 447 (9.1) | 338 (8.8) | 83 (11.4) | 26 (8.0) | 0.07 |
| Irritable bowel syndrome | 191 (3.9) | 158 (4.1) | 26 (3.6) | 7 (2.2) | 0.19 |
| Hepatitis | 96 (2.0) | 70 (1.8) | 21 (2.9) | 5 (1.5) | 0.15 |
| Lupus | 23 (0.5) | 16 (0.4) | 3 (0.4) | 4 (1.2) | 0.11 |
| HIV positive/AIDS | 26 (0.5) | 14 (0.4) | 8 (1.1) | 4 (1.2) | 0.009 |
| Parkinson’s disease | 14 (0.3) | 8 (0.2) | 5 (0.7) | 1 (0.3) | 0.09 |
| Self-Reported Systemic Inflammatory Diseases | Adjusted Odds Ratio * (95% Confidence Interval) | p-Value |
|---|---|---|
| Hypertension | 1.517 (1.372–1.678) | <0.001 |
| Arthritis | 1.180 (1.056–1.320) | 0.004 |
| Asthma | 0.695 (0.564–0.857) | <0.001 |
| Diabetes | 1.515 (1.323–1.735) | <0.001 |
| HIV positive/AIDS | 2.017 (1.239–3.282) | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chatzopoulos, G.S.; Cisneros, A.; Sanchez, M.; Wolff, L.F. Association between Periodontal Disease and Systemic Inflammatory Conditions Using Electronic Health Records: A Pilot Study. Antibiotics 2021, 10, 386. https://doi.org/10.3390/antibiotics10040386
Chatzopoulos GS, Cisneros A, Sanchez M, Wolff LF. Association between Periodontal Disease and Systemic Inflammatory Conditions Using Electronic Health Records: A Pilot Study. Antibiotics. 2021; 10(4):386. https://doi.org/10.3390/antibiotics10040386
Chicago/Turabian StyleChatzopoulos, Georgios S., Alejandro Cisneros, Miguel Sanchez, and Larry F. Wolff. 2021. "Association between Periodontal Disease and Systemic Inflammatory Conditions Using Electronic Health Records: A Pilot Study" Antibiotics 10, no. 4: 386. https://doi.org/10.3390/antibiotics10040386
APA StyleChatzopoulos, G. S., Cisneros, A., Sanchez, M., & Wolff, L. F. (2021). Association between Periodontal Disease and Systemic Inflammatory Conditions Using Electronic Health Records: A Pilot Study. Antibiotics, 10(4), 386. https://doi.org/10.3390/antibiotics10040386






