Knowledge, Attitude, and Practices (KAP) Survey among Veterinarians, and Risk Factors Relating to Antimicrobial Use and Treatment Failure in Dairy Herds of India
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design and Questionnaire Development
2.2. Sampling Procedure
2.3. Ethical Statement
2.4. Statistical Analysis
3. Results
3.1. Demographic Information
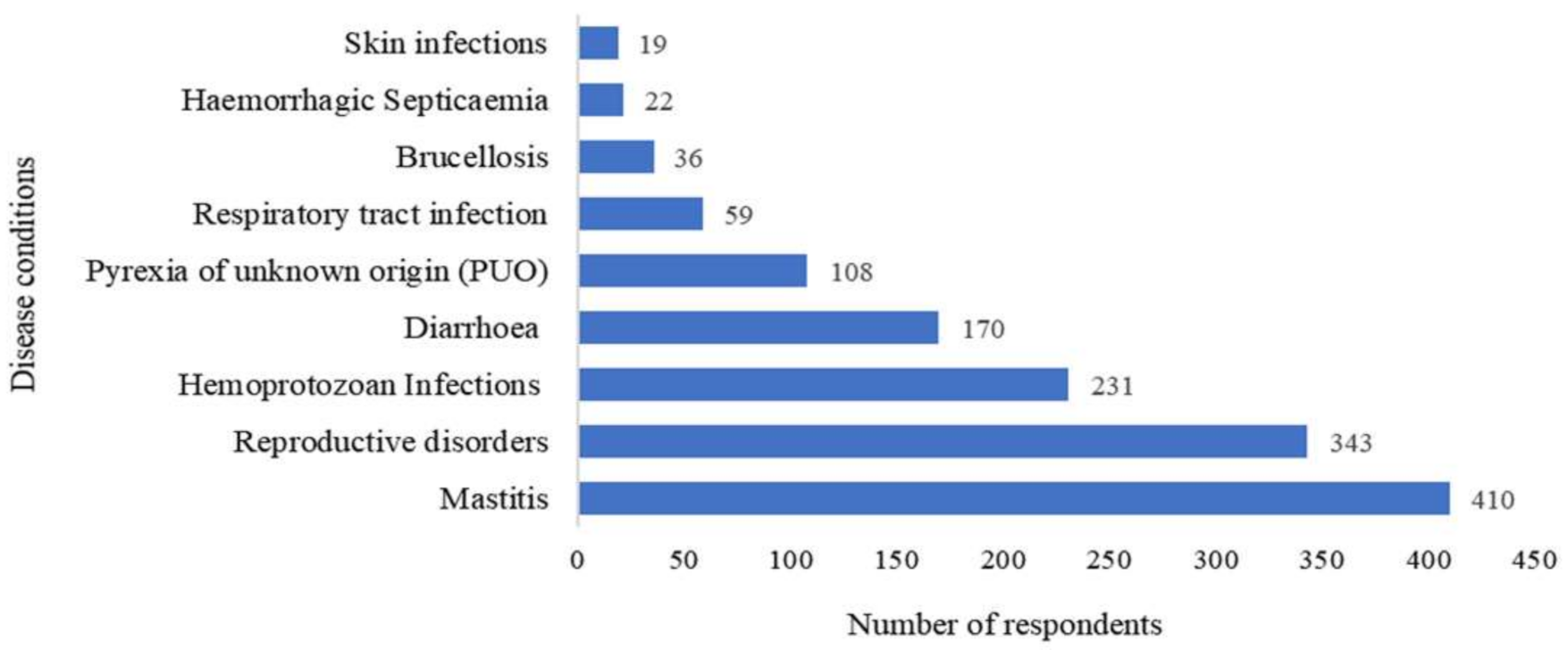
3.2. Common Diseases Requiring Antibiotic Usage in Bovines
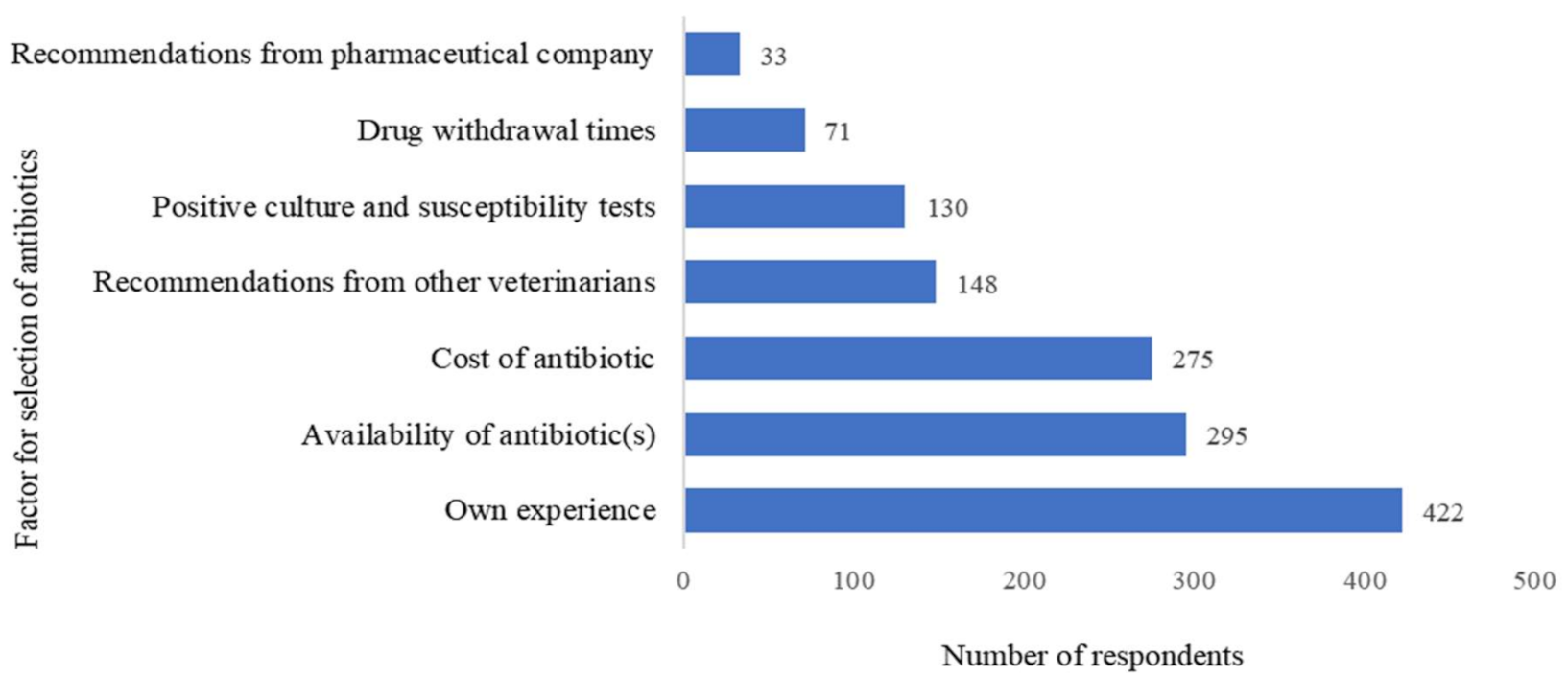
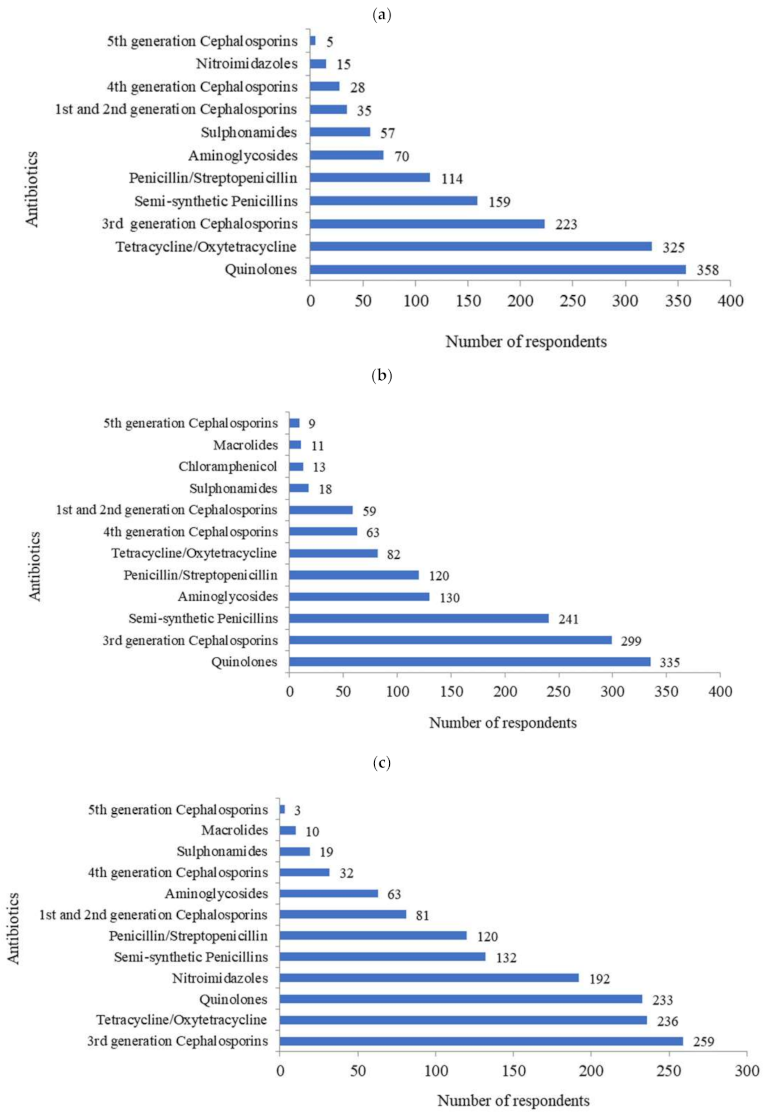
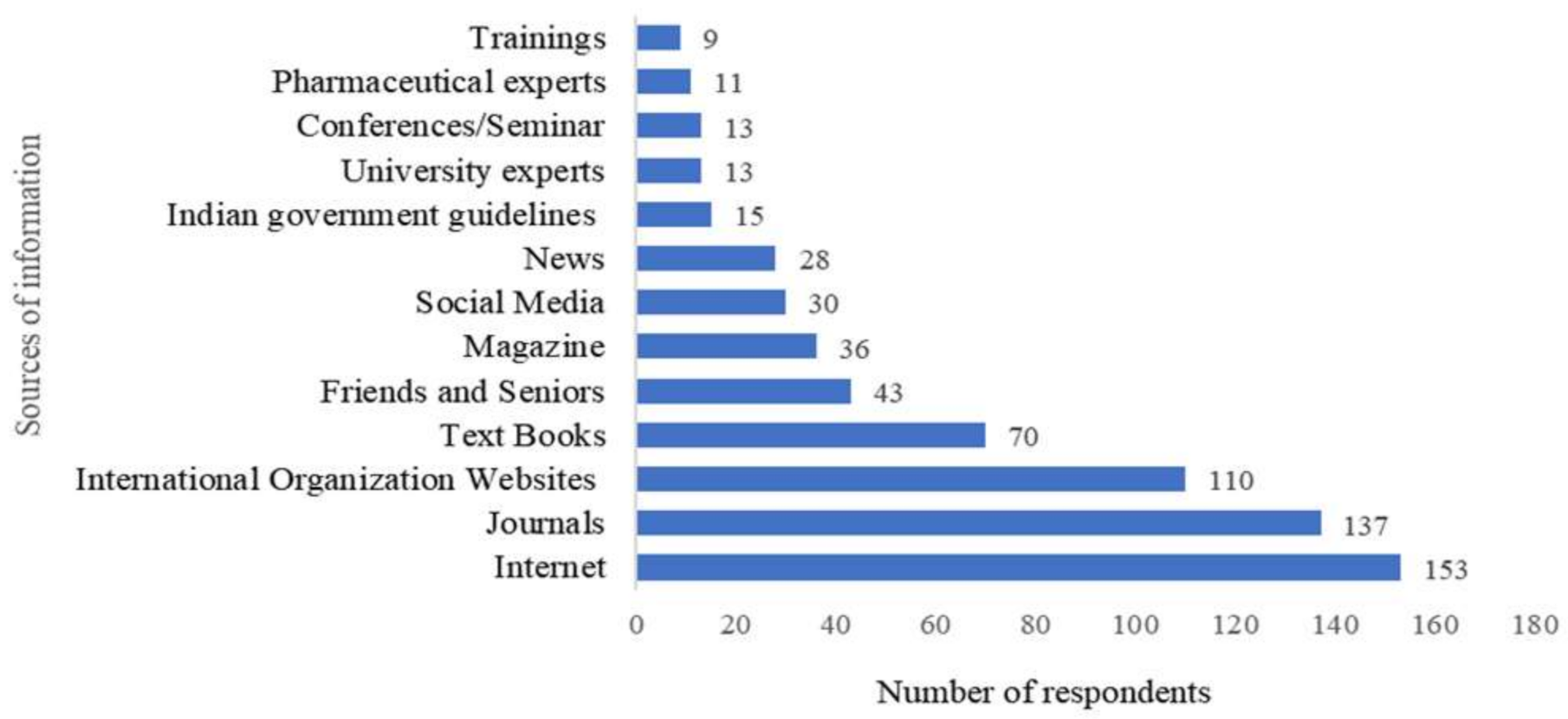
3.3. Antibiotic Prescribing Decisions
3.4. Knowledge, Attitude, and Practice (KAP) Analysis
3.5. Association of KAP Scores with Demographic Characteristics
3.6. Correlation between Knowledge, Attitude and Practice Scores
3.7. Risk Factors Associated with Treatment Failure
3.8. Univariable and Multivariable Analysis
3.9. Veterinarian’s Recommendations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- O’Neill, J. Review on Antimicrobial Resistance. Tackling Drug-Resistant Infections Globally: Final Report and Recommendations. 2016. Available online: https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf (accessed on 8 April 2020).
- Van Boeckel, T.P.; Brower, C.; Gilbert, M.; Grenfell, B.T.; Levin, S.A.; Robinson, T.P.; Teillant, A.; Laxminarayan, R. Global trends in antimicrobial use in food animals. Proc. Natl. Acad. Sci. USA 2015, 112, 5649–5654. [Google Scholar] [CrossRef] [PubMed]
- Bellet, C.; Rushton, J. World food security, globalisation and animal farming: Unlocking dominant paradigms of animal health science. Rev. Sci. Tech. 2019, 38, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Economou, V.; Gousia, P. Agriculture and food animals as a source of antimicrobial-resistant bacteria. Infect. Drug Resist. 2015, 8, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Founou, L.L.; Founou, R.C.; Essack, S.Y. Antibiotic resistance in the food chain: A developing country-perspective. Front. Microbiol. 2016, 7, 1–19. [Google Scholar] [CrossRef]
- 20th Livestock Census 2019—All India Report. Department of Animal Husbandry and Dairying (AH&D). Available online: http://dadf.gov.in/sites/default/filess/20th%20Livestock%20census-2019%20All%20India%20Report.pdf (accessed on 6 July 2020).
- Mahato, S.; Mistry, H.U.; Chakraborty, S.; Sharma, P.; Saravanan, R.; Bhandari, V. Identification of variable traits among the methicillin resistant and sensitive coagulase negative staphylococci in milk samples from mastitic cows in India. Front. Microbiol. 2017, 8, 1446. [Google Scholar] [CrossRef]
- Khan, J.A.; Rathore, R.S.; Abulreesh, H.H.; Al-Thubiani, A.S.; Khan, S.; Ahmad, I. Diversity of antibiotic-resistant Shiga toxin-producing Escherichia coli serogroups in foodstuffs of animal origin in northern India. J. Food Saf. 2018, 38, 12566. [Google Scholar] [CrossRef]
- Moudgil, P.; Bedi, J.S.; Moudgil, A.D.; Gill, J.P.S.; Aulakh, R.S. Emerging issue of antibiotic resistance from food producing animals in India: Perspective and legal framework. Food Rev. Int. 2018, 34, 447–462. [Google Scholar] [CrossRef]
- Sharma, C.; Rokana, N.; Chandra, M.; Singh, B.P.; Gulhane, R.D.; Gill, J.P.S.; Ray, P.; Puniya, A.K.; Panwar, H. Antimicrobial resistance: Its surveillance, impact, and alternative management strategies in dairy animals. Front. Vet. Sci. 2018, 4, 237. [Google Scholar] [CrossRef]
- Walia, K.; Madhumathi, J.; Veeraraghavan, B.; Chakrabarti, A.; Kapil, A.; Ray, P.; Singh, H.; Sistla, S.; Ohri, V. Establishing antimicrobial resistance surveillance & research network in India: Journey so far. Indian J. Med. Res. 2019, 149, 164–179. [Google Scholar]
- Mutua, F.; Sharma, G.; Grace, D.; Bandyopadhyay, S.; Shome, B.; Lindahl, J. A review of animal health and drug use practices in India, and their possible link to antimicrobial resistance. Antimicrob. Resist. Infect. Control 2020, 9, 103. [Google Scholar] [CrossRef]
- Kirchhelle, C. Pharming animals: A global history of antibiotics in food production (1935–2017). Palgrave Commun. 2018, 4, 1–13. [Google Scholar] [CrossRef]
- Speksnijder, D.C.; Jaarsma, D.A.C.; Verheij, T.J.M.; Wagenaar, J.A. Attitudes and perceptions of Dutch veterinarians on their role in the reduction of antimicrobial use in farm animals. Prev. Vet. Med. 2015, 121, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Coyne, L.A.; Latham, S.M.; Dawson, S.; Donald, I.J.; Pearson, R.B.; Smith, R.F.; Williams, N.J.; Pinchbeck, G.L. Antimicrobial use practices, attitudes and responsibilities in UK farm animal veterinary surgeons. Prev. Vet. Med. 2018, 161, 115–126. [Google Scholar] [CrossRef]
- Norris, J.M.; Zhuo, A.; Govendir, M.; Rowbotham, S.J.; Labbate, M.; Degeling, C.; Gilbert, G.L.; Dominey-Howes, D.; Ward, M.P. Factors influencing the behaviour and perceptions of Australian veterinarians towards antibiotic use and antimicrobial resistance. PLoS ONE 2019, 14, e0223534. [Google Scholar]
- World Health Organization. WHO List of Critically Important Antimicrobials. 2019. Available online: https://www.who.int/foodsafety/areas_work/antimicrobial-resistance/cia/en (accessed on 26 February 2020).
- World Health Organization. WHO AWaRe Classification Antibiotics. 2019. Available online: https://www.who.int/medicines/news/2019/WHO_releases2019AWaRe_classification_antibiotics/en/#:~:text=RESERVE%20GROUP%20ANTIBIOTICS&text=22%20antibiotics%20have%20been%20classified,Model%20List%20of%20Essential%20Medicines (accessed on 26 February 2020).
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- National Action Plan on Antimicrobial Resistance. India. 2017. Available online: https://www.ncdc.gov.in/WriteReadData/linkimages/AMR/File645.pdf (accessed on 3 March 2020).
- Ayukekbong, J.A.; Ntemgwa, M.; Atabe, A.N. The threat of antimicrobial resistance in developing countries: Causes and control strategies. Antimicrob. Resist. Infect. Control 2017, 6, 47. [Google Scholar] [CrossRef]
- Verma, H.; Rawat, S.; Sharma, N.; Jaiswal, V.; Singh, R.; Harshit, V. Prevalence, bacterial etiology and antibiotic susceptibility pattern of bovine mastitis in Meerut. J. Entomol. Zool. Stud. 2018, 6, 706–709. [Google Scholar]
- De Briyne, N.; Atkinson, J.; Pokludová, L.; Borriello, S.P.; Price, S. Factors influencing antibiotic prescribing habits and use of sensitivity testing amongst veterinarians in Europe. Vet. Rec. 2013, 173, 475. [Google Scholar] [CrossRef]
- Varshney, J.P.; Naresh, R. Comparative efficacy of homeopathic and allopathic systems of medicine in the management of clinical mastitis of Indian dairy cows. Homeopathy 2005, 94, 81–85. [Google Scholar] [CrossRef]
- Mishra, S.; Sharma, S.; Vasudevan, P.; Bhatt, R.K.; Pandey, S.; Singh, M.; Meena, B.S.; Pandey, S.N. Livestock feeding and traditional healthcare practices in Bundelkhand region of Central India. Indian J. Tradit. Knowl. 2010, 9, 333–337. [Google Scholar]
- Sen, S.; Chakraborty, R.; De, B. Challenges and opportunities in the advancement of herbal medicine: India’s position and role in a global context. J. Herb. Med. 2011, 1, 67–75. [Google Scholar] [CrossRef]
- Gibbons, J.F.; Boland, F.; Buckley, J.F.; Butler, F.; Egan, J.; Fanning, S.; Markey, B.K.; Leonard, F.C. Influences on antimicrobial prescribing behaviour of veterinary practitioners in cattle practice in Ireland. Vet. Rec. 2013, 172, 14. [Google Scholar] [CrossRef] [PubMed]
- McDougall, S.; Compton, C.W.R.; Botha, N. Factors influencing antimicrobial prescribing by veterinarians and usage by dairy farmers in New Zealand. N. Z. Vet. J. 2017, 65, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Postma, M.; Speksnijder, D.C.; Jaarsma, A.D.C. Opinions of veterinarians on antimicrobial use in farm animals in Flanders and the Netherlands. Vet. Rec. 2016, 179, 68. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Gupta, J.; Meena, H.R. Assessment of Awareness about Antibiotic Resistance and Practices Followed by Veterinarians for Judicious Prescription of Antibiotics: An Exploratory Study in Eastern Haryana Region of India. Trop. Anim. Health Prod. 2019, 51, 677–687. [Google Scholar] [CrossRef] [PubMed]
- Hopman, N.E.; Mughini-Gras, L.; Speksnijder, D.C.; Wagenaar, J.A.; Van Geijlswijk, I.M.; Broens, E.M. Attitudes and perceptions of Dutch companion animal veterinarians towards antimicrobial use and antimicrobial resistance. Prev. Vet. Med. 2019, 170, 104717. [Google Scholar] [CrossRef] [PubMed]
- De Briyne, N.; Atkinson, J.; Pokludová, L. Antibiotics used most commonly to treat animals in Europe. Vet. Rec. 2014, 175, 325. [Google Scholar] [CrossRef]
- Coyne, L.A.; Latham, S.M.; Williams, N.J.; Dawson, S.; Donald, I.J.; Pearson, R.B.; Smith, R.F.; Pinchbeck, G.L. Understanding the culture of antimicrobial prescribing in agriculture: A qualitative study of UK pig veterinary surgeons. J. Antimicrob. Chemother. 2016, 71, 3300–3312. [Google Scholar] [CrossRef] [PubMed]
- Peterson, L.R.; Dalhoff, A. Towards targeted prescribing: Will the cure for antimicrobial resistance be specific, directed therapy through improved diagnostic testing? J. Antimicrob. Chemother. 2014, 53, 902–905. [Google Scholar] [CrossRef]
- Rather, I.A.; Kim, B.C.; Bajpai, V.K. Self-medication and antibiotic resistance: Crisis, current challenges, and prevention. Saudi J. Biol. Sci. 2017, 24, 808–812. [Google Scholar] [CrossRef]
- Robinson, T.P.; Bu, D.P.; Carrique-Mas, J.; Fèvre, E.M.; Gilbert, M.; Grace, D.; Hay, S.I.; Jiwakanon, J.; Kakkar, M.; Kariuki, S.; et al. Antibiotic resistance is the quintessential One Health issue. Trans. R. Soc. Trop. Med. Hyg. 2016, 110, 377–380. [Google Scholar] [CrossRef]
- Sarita, S.; Gautam, S.P.; Ahuja, R. An analysis of constraints perceived by dairy farmers in Murrah tract of Haryana state. Int. J. Pure App. Biosci. 2017, 5, 1048–1053. [Google Scholar]
- Chauhan, A.S.; George, M.S.; Chatterjee, P.; Lindahl, J.F.; Grace, D.; Kakkar, M. The social biography of antibiotic use in smallholder dairy farms in India. Antimicrob. Resist. Infect. Control 2018, 7, 60. [Google Scholar] [CrossRef] [PubMed]
- Kramer, T.; Jansen, L.E.; Lipman, L.J.; Smit, L.A.; Heederik, D.J.; Dorado-García, A.; Dorado-García, A. Farmers’ knowledge and expectations of antimicrobial use and resistance are strongly related to usage in Dutch livestock sectors. Prev. Vet. Med. 2017, 147, 142–148. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | n | (%) |
|---|---|---|
| Age (years) | ||
| <30 | 148 | 31.8 |
| 30–40 | 175 | 37.5 |
| 40–50 | 103 | 22.1 |
| 50–60 | 32 | 6.9 |
| 60–70 | 8 | 1.7 |
| Sex | ||
| Male | 326 | 70.0 |
| Female | 140 | 30.0 |
| Level of education | ||
| Bachelor of Veterinary Sciences and Animal husbandry (B.V.Sc and A.H) | 208 | 44.6 |
| Master of Veterinary Sciences (M.V.Sc) | 224 | 48.1 |
| Ph.D. | 34 | 7.3 |
| Field Experience (years) | ||
| <10 | 293 | 62.9 |
| 10–20 | 105 | 22.5 |
| 20–30 | 50 | 10.7 |
| 30–40 | 17 | 3.6 |
| 40–50 | 1 | 0.2 |
| Regional distribution (6 regions: 25 States) | ||
| Northern Region (Jammu and Kashmir, Haryana, Himachal Pradesh, Punjab, Delhi, Uttarakhand, Uttar Pradesh) | 181 | 38.8 |
| Southern Region (Andhra Pradesh, Telangana, Karnataka, Kerala, Tamil Nadu) | 158 | 33.9 |
| Western Region (Rajasthan, Gujarat, Maharashtra) | 55 | 11.8 |
| Eastern Region (Bihar, Orissa, West Bengal) | 38 | 8.1 |
| Central Region (Madhya Pradesh, Chhattisgarh) | 22 | 4.7 |
| North-East Region (Assam, Sikkim, Nagaland, Meghalaya, Mizoram) | 12 | 2.6 |
| Type of Hospital | ||
| Veterinary Hospital (Institutes with basic facilities for day-to-day treatment and care of livestock) | 399 | 85.6% |
| Veterinary Polyclinic (Institutes with specialized facilities including diagnostic laboratories) | 67 | 14.4% |
| KAP Parameters ¶ | Correct Answer | Percentage (%) |
|---|---|---|
| Knowledge parameters | ||
| Is there an ongoing antibiotic abuse in therapeutics in the veterinary sector? | 401 | 86.0 |
| Do you know about the critically important list of antimicrobials specified by the World Health Organization (WHO)? | 212 | 45.5 |
| Is antibiotic resistance a serious public health issue? | 460 | 98.7 |
| Is antibiotic resistance a natural as well as anthropogenic phenomenon? | 268 | 57.5 |
| Does irrational antibiotics use in animals lead to resistance in humans? | 409 | 87.8 |
| Are you familiar with superbug New Delhi metallo-beta-lactamase 1? | 233 | 50.0 |
| Are you familiar with Livestock-associated methicillin-resistant Staphylococcus aureus (LA-MRSA)? | 297 | 63.7 |
| Does the use of expired antibiotics lead to emergence of resistance? | 195 | 41.8 |
| Does injudicious use of antibiotics lead to antibiotic residues in milk and meat? | 450 | 96.6 |
| Does antibiotic residues in milk/meat lead to emergence of resistance? | 427 | 91.6 |
| Are you aware about recommendations of National Antimicrobial Resistance Plan 2017 of India? | 97 | 20.8 |
| Attitude parameters | ||
| I believe the use of two or more classes of antibiotics in combination is always a better choice to control infections | 18 387 * | 3.9 83.0 |
| I believe a broad spectrum antibiotics is a better choice than using highly selective antibiotics, even when narrow-spectrum drugs are available | 24 | 5.1 |
| I believe priority antibiotics must be restricted for human-use only | 190 | 40.8 |
| I believe that skipping 1 or 2 doses of antibiotics contributes to the development of resistance | 269 | 57.7 |
| Practice parameters | ||
| What is your first line of treatment for pyrexia of unknown origin (PUO)? | 138 | 29.6 |
| How often do you use bacterial culture and susceptibility testing to select the appropriate antibiotics during your treatment? | 15 161 * | 3.2 34.5 |
| Illegitimate demands of farmers lead to use of antibiotics in conditions which do not require their use | 163 | 35.0 |
| How often do you advise the farmer to administer antibiotics through a telephonic conversation (vocal prescription)? | 284 | 60.9 |
| Do you write a prescription of antibiotics to farmers who come to you at the hospital without presenting their animals? | 253 | 54.3 |
| How often do you give free samples of antibiotics to farmers? | 189 | 40.6 |
| Do you use antibiotics for prophylaxis? | 284 | 60.9 |
| Do you check the expiry date of the antibiotics before use? | 439 | 94.2 |
| Do you allow the farmer to inject the subsequent doses of antibiotics after you have administered the first dose of the treatment? | 292 | 62.7 |
| After antibiotic treatment, do you advise farmers about not to use or sell milk up to recommended withdrawal period? | 233 197 * | 50.0 42.3 |
| Do you adhere to the recommendations of the National Antimicrobial Resistance Plan of India? | 48 180 * | 10.3 38.6 |
| Have you attended any trainings/conferences to update your knowledge on antibiotic usage and antimicrobial resistance? | 127 | 27.2 |
| Have you conducted/organized any training to improve the knowledge of farmers on antibiotic usage and antimicrobial resistance emergence? | 148 | 31.8 |
| Variables | Median Knowledge Score | p-Value * | Median Attitude Score | p-Value * | Median Practice Score | p-Value * |
|---|---|---|---|---|---|---|
| Age group (years) ¶ | ||||||
| <30 | 8.0 | 0.03 | 1.5 | 0.08 | 6.0 | 0.73 |
| 30–40 | 7.0 | 1.0 | 6.0 | |||
| 40–50 | 7.0 | 1.0 | 5.5 | |||
| 50–60 | 7.0 | 0.8 | 5.8 | |||
| 60–70 | 5.5 | 1.3 | 6.8 | |||
| Educational qualification ¶ | ||||||
| B.V.Sc and A.H | 7.0 | 0.00 | 1.0 | 0.19 | 6.0 | 0.19 |
| M.V.Sc | 8.0 | 1.5 | 6.0 | |||
| PhD | 9.0 | 1.3 | 7.0 | |||
| Years of Experience ¶ | ||||||
| <10 | 8.0 | 0.00 | 1.5 | 0.24 | 6.0 | 0.33 |
| 10–20 | 7.0 | 1.0 | 5.5 | |||
| 20–30 | 7.0 | 1.3 | 6.5 | |||
| 30–40 | 5.0 | 0.5 | 5.5 | |||
| Gender # | ||||||
| Male | 7.5 | 0.44 | 1.0 | 0.37 | 6.0 | 0.50 |
| Female | 8.0 | 1.5 | 6.0 | |||
| Region ¶ | ||||||
| Northern | 8.0 | 0.12 | 1.5 | 0.09 | 5.5 | 0.02 |
| Southern | 7.0 | 1.5 | 6.3 | |||
| Central | 8.0 | 0.5 | 5.5 | |||
| Western | 8.0 | 1.0 | 7.0 | |||
| Eastern | 8.0 | 1.5 | 5.5 | |||
| North Eastern | 8.5 | 1.5 | 6.3 | |||
| Type of hospital # | ||||||
| Veterinary hospital | 7.0 | 0.03 | 1.5 | 0.63 | 6.0 | 0.40 |
| Veterinary polyclinic | 8.0 | 1.5 | 6.0 | |||
| Variables | Odds Ratio (95% C.I.) | p-Value |
|---|---|---|
| (a) | ||
| Use of antibiotics for prophylaxis | 1.6 (1.0–2.4) | 0.05 |
| Allowing farmer to inject the subsequent doses of antibiotics after administering the first dose of treatment | 1.8 (1.2–2.8) | 0.009 |
| After antibiotic treatment, advising farmers not to use or sell milk up to the recommended withdrawal period | 1.1 (0.7–1.7) | 0.74 |
| Checking of expiry date of the antibiotics before use | 1.9 (0.8–4.3) | 0.14 |
| Vocal prescription of antibiotics to farmers | 1.5 (0.8–2.6) | 0.20 |
| Giving free samples of antibiotic to farmers | 1.3 (0.7–2.2) | 0.39 |
| Skipping of 1 or 2 doses of antibiotics in the course | 1.7 (1.1–2.6) | 0.02 |
| (b) | ||
| Illegitimate demand of farmers for antibiotics in conditions that do not require their use | 3.7 (2.3–6.0) | 0.00 |
| Farmer’s non-cooperation in completion of the antibiotic course specified by the veterinarians | 1.9 (1.2–3.1) | 0.007 |
| Farmers acquiring antibiotics directly from a pharmacy without prescription | 2.2 (1.1–4.4) | 0.03 |
| Variable | B | S.E | Odds Ratio (95% C.I.) | p-Value |
|---|---|---|---|---|
| (a) | ||||
| Skipping of 1 or 2 doses of antibiotics in the course | 0.5 | 0.2 | 1.7 (1.1–2.6) | 0.02 |
| Allowing the farmer to inject the subsequent doses of antibiotics after administering the first dose of treatment | 0.6 | 0.2 | 1.8 (1.1–2.8) | 0.01 |
| Constant | −1.8 | 0.2 | 0.2 | 0.00 |
| Hosmer–Lemeshow test for Goodness of Fit: p-value = 0.93 | ||||
| (b) | ||||
| Illegitimate demand of farmers for antibiotics in conditions that do not require their use | 1.3 | 0.2 | 3.6 (2.3–5.8) | 0.00 |
| Farmer’s non-cooperation in completion of antibiotic course specified by the veterinarians | 0.6 | 0.2 | 1.8 (1.1–3.0) | 0.02 |
| Constant | −2.1 | 0.2 | 0.1 | 0.00 |
| Hosmer–Lemeshow test for Goodness of Fit: p-value = 0.55 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vijay, D.; Bedi, J.S.; Dhaka, P.; Singh, R.; Singh, J.; Arora, A.K.; Gill, J.P.S. Knowledge, Attitude, and Practices (KAP) Survey among Veterinarians, and Risk Factors Relating to Antimicrobial Use and Treatment Failure in Dairy Herds of India. Antibiotics 2021, 10, 216. https://doi.org/10.3390/antibiotics10020216
Vijay D, Bedi JS, Dhaka P, Singh R, Singh J, Arora AK, Gill JPS. Knowledge, Attitude, and Practices (KAP) Survey among Veterinarians, and Risk Factors Relating to Antimicrobial Use and Treatment Failure in Dairy Herds of India. Antibiotics. 2021; 10(2):216. https://doi.org/10.3390/antibiotics10020216
Chicago/Turabian StyleVijay, Deepthi, Jasbir Singh Bedi, Pankaj Dhaka, Randhir Singh, Jaswinder Singh, Anil Kumar Arora, and Jatinder Paul Singh Gill. 2021. "Knowledge, Attitude, and Practices (KAP) Survey among Veterinarians, and Risk Factors Relating to Antimicrobial Use and Treatment Failure in Dairy Herds of India" Antibiotics 10, no. 2: 216. https://doi.org/10.3390/antibiotics10020216
APA StyleVijay, D., Bedi, J. S., Dhaka, P., Singh, R., Singh, J., Arora, A. K., & Gill, J. P. S. (2021). Knowledge, Attitude, and Practices (KAP) Survey among Veterinarians, and Risk Factors Relating to Antimicrobial Use and Treatment Failure in Dairy Herds of India. Antibiotics, 10(2), 216. https://doi.org/10.3390/antibiotics10020216







