Abstract
In areas with high prevalence of macrolide-resistant Mycoplasma pneumoniae (MRMP) pneumonia, treatment in children has become challenging. This study aimed to analyze the efficacy of macrolides and doxycycline with regard to the presence of macrolide resistance. We analyzed children with MP pneumonia during the two recent epidemics of 2014–2015 and 2019–2020 from four hospitals in Korea. Nasopharyngeal samples were obtained from children with pneumonia for MP cultures and polymerase chain reaction (PCR). Macrolide resistance was determined by the analysis of 23S rRNA gene transition. Time to defervescence and to chest X-ray improvement were analyzed. Of 145 cases, the median age was 5.0 years and MRMP accounted for 59 (40.7%). Among macrolide-susceptible MP (MSMP), 78 (90.7%) were treated with macrolides and 21 (35.6%) in the MRMP group with doxycycline. In MRMP pneumonia, shorter days to defervescence (2 vs. 5 days, p < 0.001) and to chest X-ray improvement (3 vs. 6 days, p < 0.001) in the doxycycline group than in the macrolide group was observed, whereas no differences were observed among children with MSMP pneumonia. Compared to macrolides, treatment with doxycycline resulted in better outcomes with a shorter time to defervescence and to chest X-ray improvement among children with MRMP pneumonia.
1. Introduction
Mycoplasma pneumoniae (MP) is an important cause for community-acquired pneumonia in children and adults [1,2]. MP infections in children are known as mild and self-limiting; however, antimicrobial treatment is recommended in children with moderate to severe lower respiratory tract infections [1,3,4].
MP is distinguished from other bacteria due to unique microbiologic characteristics, including lack of a cell wall, which attributes to being intrinsically resistant towards beta-lactams [5]. Therefore, antibiotics that act on the bacterial ribosome and inhibit protein synthesis such as macrolides or tetracyclines or agents that inhibit DNA replication such as fluoroquinolones are active against MP [6,7]. Among these, macrolides are recommended as first-line treatment for MP pneumonia in children due to the potential toxicities of other agents in children. However, in cases with delay in defervescence and clinical deterioration, macrolide-resistance should be considered. Delayed effective treatment is associated with prolonged and/or more severe presentation [8]. Macrolide-resistance has emerged worldwide with a relatively high prevalence in Asia, ranging from 23.3% to over 84.8% [7]. Therefore, treatment with the increase in macrolide-resistance has become challenging.
In this study, we aimed to compare the efficacy of macrolides and doxycycline in children with MP pneumonia treated in the context of no information regarding macrolide resistance, which were retrospectively tested and classified as macrolide-sensitive MP (MSMP) and macrolide-resistant MP (MRMP).
2. Results
2.1. Patient Characteristics
During the two epidemics of 2014–2015 and 2019–2020, 173 cases were positive for MP PCR or culture and diagnosed with MP pneumonia. Among 173 cases, 21 cases were excluded due to at least one of the following: concomitant steroids (n = 14), underlying disease (n = 12), date of last fever not specified (n = 7), and follow up to other institution (n = 3) (Figure 1). Additionally, children treated for less than 5 days (macrolide n = 5, doxycycline n = 2) were also excluded. Finally, 145 cases were included in the analysis; 103 (71.0%) during the 2014–2015 season and 42 cases (29.0%) from the 2019–2020 season.
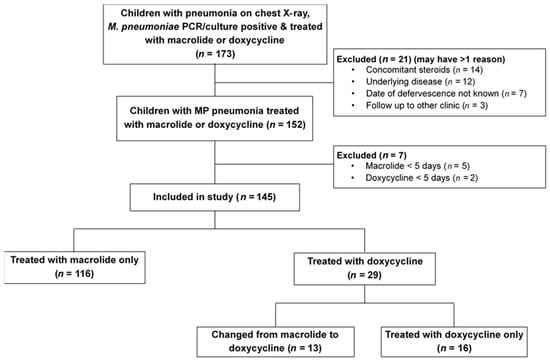
Figure 1.
Flow diagram of cases included in the study for comparison of antibiotic response between macrolides and doxycycline in children with Mycoplasma pneumoniae pneumonia according to macrolide resistance. MP, Mycoplasma pneumoniae.
The demographics and clinical characteristics of cases included in this study are shown in Table 1. Among 145 cases, 59 (40.7%) were male and the median age was 5.0 years. There was no difference of median age between MRMP and MSMP groups. Eight cases (5.5%) had underlying diseases (neurologic disease, n = 1; hematologic disease, n = 3; cardiac disease, n = 1; endocrine disease, n = 1; gastrointestinal disease, n = 2). Among the cases tested, 92.0% (127/138) were MP PCR positive, 62.7% (32/51) were anti-mycoplasma IgM positive, 48.3% (57/118) showed anti-mycoplasma IgG ≥ 1:640, and 94.6% (35/37) showed a four-fold increase. The median duration of fever was 7 days and children in the MRMP pneumonia group had significantly longer duration of fever (8 days vs. 7 days, p value = 0.003). Median duration of cough was 15 days and there was no significant difference according to macrolide resistance. More than one-third of the cases showed lobar consolidation and 11.0% had parapneumonic effusion. There was no difference in radiologic findings according to macrolide susceptibility. Among the cases, 12.4% had combined viral co-infection with a similar distribution between MSMP and MRMP groups. Oxygen therapy was required in 2.8% and there were no cases on mechanical ventilator. Two cases had complications including bronchiolitis obliterans and persistent large-scale atelectasis.

Table 1.
Demographics and clinical characteristics of children with Mycoplasma pneumoniae pneumonia according to macrolide resistance.
2.2. Macrolide Resistance and Clinical Efficacy
Cases of MRMP accounted for 40.7% (n = 59) in this study (Table 1). Macrolide resistance rate differed between institutions. Institutions in Seoul, Seongnam, and Daejeon showed macrolide resistance of 74.1%, 63.6%, and 66.7%, respectively. In contrast, macrolide resistance from the institution on Jeju Island was 10.8%. Macrolide resistance was 30.1% in the 2014–2015 season and 66.7% in the 2019–2020 season; the difference between the two seasons is related to the distribution in cases included according to district.
Among all cases, 116 (80.0%) were treated with macrolides only, 13 (9.0%) changed from macrolide to doxycycline, and 16 (11.0%) were treated with doxycycline only (Table 2). In the MSMP group, 78 (90.7%) were treated with macrolides; in the MRMP group, 21 (35.6%) were treated with doxycycline. According to the antibiotic regimen, children treated with doxycycline (including those changed from macrolides) were older than children treated with macrolides only (Table S1). The macrolide resistance rate was also higher in children initially treated with macrolides changed to doxycycline (11/13, 84.6%) and doxycycline only (10/16, 62.5%) compared with children treated with macrolide only (38/116, 32.8%) (p < 0.001) (Table S1).

Table 2.
Antibiotic treatment in of children with Mycoplasma pneumoniae pneumonia according to macrolide resistance.
Among children treated with macrolides, clarithromycin (n = 53) was most commonly prescribed, followed by roxithromycin (n = 42) and azithromycin (n = 6), and cases which changed the macrolide agent during therapy (n = 28) were also included in the study. The median duration of antibiotic use for macrolides and doxycycline were both 10 days, respectively. Among the 13 cases in which macrolide was changed to doxycycline, data on macrolide initiation date was available for 11 cases and the median days to change to doxycycline was 4 days.
In the analysis of clinical response according to macrolide resistance, the duration of fever and days to chest X-ray improvement after initiation of macrolides was shorter in MSMP compared with MRMP. There was no difference according to macrolide resistance in duration of fever or days to chest X-ray improvement in those treated with doxycycline (Table 3).

Table 3.
Clinical response according to antibiotic treatment in children with Mycoplasma pneumoniae pneumonia related to macrolide resistance.
When comparing clinical response between antibiotics, among MSMP there was no difference in duration of fever or days to chest X-ray improvement in the macrolide group compared with the doxycycline group (Table 3). However, in MRMP, fever duration was shorter in the doxycycline group by 3 days (5 days vs. 2 days, p = 0.003) and days to chest X-ray improvement was shorter in the doxycycline group (6 days vs. 3 days, p = 0.010) (Table 3). In MRMP, fever duration was also shorter in the macrolide to doxycycline group compared with macrolide only by 3 days (5 days vs. 2 days, p = 0.002) and days to chest X-ray improvement (6 days vs. 3 days, p = 0.002) (Table 3).
The response to antibiotics among children with MRMP pneumonia at different time points was also analyzed (Table 4, Figure 2). In children infected with MRMP, more children showed defervescence in the doxycycline treated groups at 2, 3, 4, and 5 days after antibiotic treatment. When analyzing the response of chest X-ray improvement, there was no difference at 2 days; however, at day 3–5 after antibiotic treatment, a significantly higher proportion of children showed improvement in the doxycycline treated groups.

Table 4.
Cumulative incidence of fever or chest X-ray improvement after antibiotic initiation in macrolide-resistant Mycoplasma pneumoniae pneumonia.
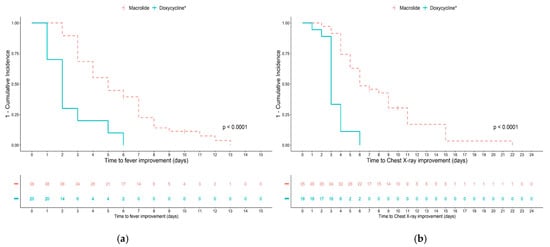
Figure 2.
Cumulative incidence analysis of fever and chest X-ray improvement according to antibiotic group in children with macrolide-resistant Mycoplasma pneumoniae pneumonia. (a) Time to resolution of fever; (b) time to chest X-ray improvement in children treated with macrolides only or doxycycline (* including macrolides changed to doxycycline and doxycycline only).
3. Discussion
Macrolide resistance in MP pneumonia in children has been an increasing conundrum due to limited alternative treatment options. In this study, we evaluated the clinical response to macrolides and doxycycline among children in macrolide-susceptible and macrolide-resistant cases. Among MSMP cases, there was no significant difference in clinical efficacy between macrolides and doxycycline when assessed by duration of fever or days to chest X-ray improvement after initiation of antibiotics. However, when comparing the response in MRMP, time to defervescence was reduced by 3 days and chest X-ray improvement was seen 3 days earlier in children treated with doxycycline compared to macrolides. Thus, cases with macrolide resistance showed significantly more rapid improvement of symptoms and radiologic findings with doxycycline compared with macrolides.
Doxycycline was used initially in a small number of cases among children of older ages in the 2019–2020 cohort based on the consideration of the high local macrolide resistance rate of up to 84.5%; there have been reports on the efficacy and safety of doxycycline in children and current recommendations are that children with moderate to severe disease may benefit from macrolides or tetracyclines (for children >7 years) [1,7,9]. The majority of cases which switched from macrolide to doxycycline were also in 2019–2020 (Table S1). The trend for prescription of doxycycline was related to an update in treatment guidelines for MP pneumonia in children in Korea in 2019, which recommends doxycycline as a second line therapy [10]. On the other hand, although over 40% of the subjects in this study were macrolide resistant, only 20% were treated with doxycycline as the final drug. This presumably attributes to the reluctancy of use of doxycycline in children. Taken together, macrolides stand as the first-line therapy in children; however, the difference between the two drugs in time to defervescence and chest X-ray improvement among cases with MRMP supports the benefits for switch to doxycycline in a timely manner.
As for the clinical characteristics of children with MSMP and MRMP, we found that age, sex, chest radiologic findings, viral co-infection, and need for oxygen therapy were not influenced by macrolide resistance. Additionally, there were no differences in laboratory findings, including anemia, leukocytosis, thrombocytopenia, LFT elevation, or CRP elevation (data not shown). These results correlate with previous reports, including a systemic review on the effect of macrolide resistance on clinical features in children [9,11,12,13,14]. Therefore, it is difficult to distinguish MSMP and MRMP cases based on clinical characteristics.
When comparing the subjects who changed antibiotics after initiation of macrolides according to macrolide resistance, the proportion was higher in the MRMP at 22.4% compared with MSMP, which had a proportion of 2.5%, which was previously reported in other studies [9,12,15,16,17,18]. For optimal treatment, it would be ideal to test macrolide resistance before treatment for MP pneumonia; however, this may not always be feasible. In this study, among children treated with macrolides, we found that 68.4% of children with MRMP had fever >72 h, whereas only one-third of MSMP had persistent fever. These results are similar to previous studies on macrolide resistance [9,12,16,19,20,21]. Thus, in selected cases with persistent fever or limited evidence of radiologic improvement after 3 days of macrolide treatment, change to doxycycline may be considered.
In this study, we did not compare the difference between macrolides. However, the most common point mutations A2063G and A2064G in domain V 23S rRNA causes significant increase in the MIC of all macrolide drugs [9,22]. Previous studies have shown no significant difference between different drugs of the macrolide class [16,20]. Doxycycline has good activity against both macrolide-susceptible and -resistant strains (MIC90 0.125–0.5 μg/mL and 0.5 μg/mL, respectively). To date, no acquired resistance to tetracyclines have been reported in MP. However, reduced susceptibility has been selected in vitro with target mutations in the tetracycline-binding pocket of 16S rRNA such as G1193A and T968C [7,23,24]. Therefore, judicious use of doxycyclines and monitoring for resistance is important with the increase of use.
The overall macrolide resistance rate in this study was 40.7%. This is lower than recent reports in Korea, which were based on institutions in Seoul and other metropolitan cities in Korea [25]. In this study, cases from Jeju Island (an isolated remote island approximately 780 km south of Seoul) were included, in which the macrolide resistance rate was recently reported to be approximately 10.9% [26]. The resistance rate was also higher in 2019–2020 compared with 2014–2015; however, rather than an increase or change in antimicrobial resistance rate, this difference is related to the difference in proportion of samples from a district with low macrolide resistance rate. Thus, the resistance rate in this study does not reflect the macrolide resistance rate in Korea. The reason for the large difference between Jeju Island and other areas is not clear; however, Jeju Island is a remote area and there may have been little opportunities for introduction of MRMP strains. The institution has good accessibility and children with relatively low severity may be admitted, whereas children non-responsive to macrolides may be more likely to be admitted to institutions in the metropolitan area.
Interestingly, recent reports from Japan have shown a decrease in macrolide resistance rate of children with MP pneumonia with a peak of 81.6% in 2012 followed by 59.3% in 2014 and 43.6% in 2015 [27]. On the other hand, a report from the US among respiratory specimens collected from hospitals in eight states during 2015 and 2018 showed MRMP in 7.5% of the samples [28]. MRMP prevalence in the south and east was higher at 18.3% compared to 2.1% in the west of the US. The wide variation in macrolide resistance between time and area emphasizes the need for continuous surveillance on the macrolide resistance rate in the community.
Use of tetracyclines in children have been limited due to reports of permanent dental discoloration in children under 8 years of age. However, recent data suggest that doxycycline is not likely to cause visible teeth staining or enamel hypoplasia in young children [2]. Based on this, the American Academy of Pediatrics state that doxycycline can be administered for short durations (21 days or less) regardless of age, yet patients should be careful to avoid excess sun exposure due to photosensitivity associated with doxycycline [29]. Although, doxycycline is not considered first-line therapy for MP pneumonia in children; in this context, it may be used in selected conditions in MRMP or in areas with high prevalence of MRMP.
This study has limitations. We were not able to assess the clinical efficacy of fluoroquinolones, another option for second line therapy in MRMP, due to limited number of subjects prescribed. Additionally, there was an uneven distribution among cases in the 2014–2015 season and 2019–2020 season, which was related to the COVID-19 pandemic. Since January 2020, in response to various public health policies to control the spread of COVID-19 in the pandemic, there was a substantial decrease in respiratory infections in Korea and many resources were focused on diagnosis and management of COVID-19 [30]. However, the focus of this study was to evaluate the response to antibiotics, and all patients were grouped according to macrolide susceptibility or antibiotic regimen rather than season of infection; therefore, the difference in number of cases between seasons would not affect the results of the analysis. Additionally, this study was not designed to assess safety issues of doxycycline. Gastrointestinal symptoms, photosensitivity, and, rarely, Steven Johnson Syndrome have been reported as adverse reactions with doxycycline; however, in the limited data collection, we did not experience any cases with the severe complications necessary for discontinuance before clinical improvement.
Regardless of these limitations, in this comprehensive study, we analyzed the macrolide resistance in children with MP pneumonia and compared the clinical responses against macrolides and doxycycline based on the duration of fever and days to radiological improvement. Among children with MSMP pneumonia, there was no difference in time to improvement between macrolides and doxycycline. However, among children with MRMP pneumonia, the duration of fever and days to chest X-ray improvement was significantly shorter in cases treated with doxycycline.
4. Materials and Methods
4.1. Study Design
We analyzed children under 18 years of age with MP pneumonia during the two recent epidemic seasons in 2014–2015 and 2019–2020. Four hospitals participated in this study, including Seoul National University Children’s Hospital (Seoul), Seoul National University Bundang Hospital (Seongnam), Chungnam University Hospital (Daejeon), and Jeju University Hospital (Jeju Island).
To compare the response between the antibiotics, the primary outcome was days to defervescence, and secondary outcome was days to improvement in chest radiography, defined as more than 30% improvement.
The inclusion criteria were the following: (1) children with febrile pneumonia, (2) treated with macrolides or doxycycline, (3) serologic evidence for MP infection [serum anti-mycoplasma IgM positive, single anti-mycoplasma IgG titer ≥ 1:640 or paired anti-mycoplasma IgG titer show 4-fold increase] and [culture or polymerase chain reaction (PCR) positive for MP], and (4) tested for macrolide resistance [31]. Anti-mycoplasma IgM and IgG were tested using ELISA (Seegene, Seoul Korea) and anti-mycoplasma IgG was titrated using an indirect particle agglutination test kit (SerodiaMycoII, Fujirebio, Tokyo, Japan) according to the manufacturer’s instructions. Pneumonia was defined with the presence of infiltration in chest radiography with clinical symptoms and signs such as fever (defined as ≥38 °C), cough, or sputum [11]. Children with underlying diseases, including chronic lung disease or immunodeficiency, bacteria co-infection such as Streptococcus pneumoniae, Staphylococcus aureus or Bordetella pertussis, treatment with steroids, children for whom data were not available for defervescence, and children lost to follow-up were excluded from the study. Additionally, to assess the response to antibiotics, children treated for at least 5 days or more were included.
Nasopharyngeal aspirates or swabs were obtained from children with acute lower respiratory tract infections as a strategy of routine patient care at admission. Multiplex PCR was performed to detect respiratory viruses, including respiratory syncytial virus, influenza virus, parainfluenza virus, adenovirus, rhinovirus, and coronavirus (Seeplex RV12 ACE detection kit, Seegene, Seoul, Korea). Residual samples were sent to the laboratory of the Seoul National University Children’s Hospital for the culture and PCR of MP and analysis of macrolide resistance. Macrolide resistance was analyzed retrospectively and results were not available during treatment.
4.2. Detection of Macrolide Resistance of MP
Culture and PCR of MP was performed as previously described [11]. Macrolide resistance was determined by the presence of gene transitions on the domain V of the 23S rRNA gene. Briefly, to amplify domain V of the 23S rRNA gene, PCR analysis was performed on cultured MP isolates or DNA extracted from nasopharyngeal samples. The primers used were MP23SV-F (5′-TAA CTA TAA CGG TCC TAA GG) and MP23SV-R (5′-ACA CTT AGA TGC TTT CAG CG). DNA from the reference strain M129 (ATCC 29342) was used as a positive control, and distilled water was used as a negative control; amplifications of samples were performed for 35 cycles. The 851-bp PCR products were purified using an AccuPrep® PCR Purification Kit (Bioneer, Inc., Daejeon, Korea), and samples were sequenced to identify the transitions in domain V macrolide resistance, such as A2063G and A2064G [32]. The minimal inhibitory concentration for macrolides in strains with 23S rRNA transition were previously reported [9]. Based on these results, cases were classified as MSMP or MRMP.
4.3. Clinical Data Collection and Assessment of Antimicrobial Response
The electronic medical records of all patients were reviewed. Data collected included demographic factors, clinical manifestations, laboratory results, antimicrobial agents, concomitant medication, and outcome including duration of symptoms. The duration of fever was defined as the number of days for which the patient had a body temperature of ≥38 °C with an interval of <24 h between each episode of fever. Medical records were reviewed by a physician in each hospital and collected on a standardized from.
Chest X-ray findings were categorized into homogeneous dense lobar consolidation, patchy consolidation, nodular opacities, and perihilar peribronchial infiltration [11]. Parapneumonic effusion, defined as ≥1 cm width on the decubitus view, was also included in the analysis. In the four participating hospitals, all physicians were unaware of the results of 23S rRNA mutation during the treatment.
According to treatment, children were classified into macrolide, doxycycline, and macrolide to doxycycline group. For evaluation of antimicrobial response, the days to defervescence and days to chest X-ray improvement was evaluated.
4.4. Statistical Analyses
All statistical analyses were performed with R version 4.0.1. (R Foundation for statistical computing, Vienna, Austria). Differences between categorical variables were tested using the Chi-squared or Fisher’s exact test. The Wilcoxon Rank Sum or Kruskal-Wallis test were used to compare the age, days to defervescence, and days to chest X-ray improvement between the treatment groups as appropriate. In all analyses, a p-value of ≤0.05 was considered statistically significant.
5. Conclusions
Doxycycline is effective and may be considered in selected cases in children with MRMP pneumonia.
Supplementary Materials
The following are available online at https://www.mdpi.com/2079-6382/10/2/192/s1. Table S1: Demographics and clinical characteristics of children with Mycoplasma pneumoniae pneumonia according to antibiotic treatment.
Author Contributions
Conceptualization, E.H.C. and H.L.; methodology, E.H.C. and H.L.; formal analysis, Y.K.K., Y.Y.C., E.Y.C., J.H.C., and Y.J.S.; investigation, J.Y.P., M.S.H., K.W.Y., and K.K.; data curation, Y.K.K., Y.Y.C., E.Y.C., and J.H.C.; writing—original draft preparation, H.L.; writing—review and editing, E.H.C. and H.L.; visualization, H.L.; supervision, E.H.C.; funding acquisition, E.H.C. and H.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Basic Science Research Program through the National Research Foundation of Korea, which is funded by the Ministry of Education, Science and Technology (NRF-2018R1D1A1A09082098), to E.H.C. and by the 2020 Seoul National University Bundang Hospital Research Fund to H.L. (grant number 02-2020-039).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (IRB No.B-2004/608-108).
Informed Consent Statement
Requirement for informed consent was waived due to the retrospective design of our study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Acknowledgments
The authors would like to thank Lee SY and Kim SJ for their excellent technical support and the Division of Statistics in Medical Research Collaborating Center at Seoul National University Bundang Hospital for statistical analyses.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bradley, J.S.; Byington, C.L.; Shah, S.S.; Alverson, B.; Carter, E.R.; Harrison, C.; Kaplan, S.L.; Mace, S.E.; McCracken, G.H., Jr.; Moore, M.R.; et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: Clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin. Infect. Dis. 2011, 53, e25–e76. [Google Scholar] [CrossRef] [PubMed]
- Lind, K.; Benzon, M.W.; Jensen, J.S.; Clyde, W.A., Jr. A seroepidemiological study of Mycoplasma pneumoniae infections in Denmark over the 50-year period 1946-1995. Eur. J. Epidemiol. 1997, 13, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Gardiner, S.J.; Gavranich, J.B.; Chang, A.B. Antibiotics for community-acquired lower respiratory tract infections secondary to Mycoplasma pneumoniae in children. Cochrane Database Syst. Rev. 2015, 1, CD004875. [Google Scholar] [CrossRef] [PubMed]
- Biondi, E.; McCulloh, R.; Alverson, B.; Klein, A.; Dixon, A.; Ralston, S. Treatment of Mycoplasma Pneumonia: A Systematic Review. Pediatrics 2014, 133, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- Bébéar, C.M.; Pereyre, S. Mechanisms of drug resistance in Mycoplasma pneumoniae. Curr. Drug Target -Infectious Disord. 2005, 5, 263–271. [Google Scholar] [CrossRef] [PubMed]
- Waites, K.B.; Xiao, L.; Liu, Y.; Balish, M.F.; Atkinson, T.P. Mycoplasma pneumoniae from the Respiratory Tract and Beyond. Clin. Microbiol. Rev. 2017, 30, 747–809. [Google Scholar] [CrossRef]
- Lee, H.; Yun, K.W.; Lee, H.J.; Choi, E.H. Antimicrobial therapy of macrolide-resistant Mycoplasma pneumoniae pneumonia in children. Expert. Rev. Anti. Infect. Ther. 2018, 16, 23–34. [Google Scholar] [CrossRef]
- Tsai, T.-A.; Tsai, C.-K.; Kuo, K.-C.; Yu, H.-R. Rational stepwise approach for Mycoplasma pneumoniae pneumonia in children. J. Microbiol. Immunol. Infect. 2020. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Hsu, W.-Y.; Chang, T.-H. Macrolide-Resistant Mycoplasma pneumoniae Infections in Pediatric Community-Acquired Pneumonia. Emerg. Infect. Dis. 2020, 26, 1382–1391. [Google Scholar] [CrossRef]
- The Korean Academy of Pediatric Allergy and Respiratory Disease; The Korean Society of Pediatric Infectious Diseases. Guidelines for Treating Macrolide Refractory Severe Mycoplasma Pneumonia in Children 2019, Korea; The Korean Academy of Pediatric Allergy and Respiratory Disease; The Korean Society of Pediatric Infectious Diseases: Seoul, Korea, 2019. [Google Scholar]
- Yoon, I.A.; Hong, K.B.; Lee, H.J.; Yun, K.W.; Park, J.Y.; Choi, Y.H.; Kim, W.S.; Lee, H.; Eun, B.W.; Ahn, Y.M.; et al. Radiologic findings as a determinant and no effect of macrolide resistance on clinical course of Mycoplasma pneumoniae pneumonia. BMC Infect. Dis. 2017, 17, 402. [Google Scholar] [CrossRef]
- Cardinale, F.; Chironna, M.; Chinellato, I.; Principi, N.; Esposito, S. Clinical Relevance of Mycoplasma pneumoniae Macrolide Resistance in Children. J. Clin. Microbiol. 2012, 51, 723–724. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.-M.; Wong, K.-S.; Huang, Y.-C.; Lai, S.-H.; Tsao, K.-C.; Lin, Y.-J.; Lin, T.-Y. Macrolide-resistant Mycoplasma pneumoniae in children in Taiwan. J. Infect. Chemother. 2013, 19, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S.; Yamazaki, T.; Narita, M.; Okazaki, N.; Suzuki, I.; Andoh, T.; Matsuoka, M.; Kenri, T.; Arakawa, Y.; Sasaki, T. Clinical Evaluation of Macrolide-Resistant Mycoplasma pneumoniae. Antimicrob. Agents Chemother. 2006, 50, 709–712. [Google Scholar] [CrossRef]
- Cheong, K.-N.; Chiu, S.S.; Chan, B.W.-K.; To, K.K.-W.; Chan, E.L.-Y.; Ho, P.L. Severe macrolide-resistant Mycoplasma pneumoniae pneumonia associated with macrolide failure. J. Microbiol. Immunol. Infect. 2016, 49, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Kawai, Y.; Miyashita, N.; Kubo, M.; Akaike, H.; Kato, A.; Nishizawa, Y.; Saito, A.; Kondo, E.; Teranishi, H.; Ogita, S.; et al. Therapeutic Efficacy of Macrolides, Minocycline, and Tosufloxacin against Macrolide-Resistant Mycoplasma pneumoniae Pneumonia in Pediatric Patients. Antimicrob. Agents Chemother. 2013, 57, 2252–2258. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, K.; Okada, T.; Matsushima, T.; Komiyama, O.; Iwata, S.; Morozumi, M.; Ubukata, K.; Shoji, M.; Ebihara, T.; Sato, Y.; et al. A comparative clinical study of macrolide-sensitive and macrolide-resistant Mycoplasma pneumoniae infections in pediatric patients. J. Infect. Chemother. 2009, 15, 380–383. [Google Scholar] [CrossRef] [PubMed]
- Miyashita, N.; the Atypical Pathogen Study Group; Kawai, Y.; Akaike, H.; Ouchi, K.; Hayashi, T.; Kurihara, T.; Okimoto, N. Macrolide-resistant Mycoplasma pneumoniae in adolescents with community-acquired pneumonia. BMC Infect. Dis. 2012, 12, 126. [Google Scholar] [CrossRef]
- Kawai, Y.; Miyashita, N.; Yamaguchi, T.; Saitoh, A.; Kondoh, E.; Fujimoto, H.; Teranishi, H.; Inoue, M.; Wakabayashi, T.; Akaike, H.; et al. Clinical efficacy of macrolide antibiotics against genetically determined macrolide-resistant Mycoplasma pneumoniae pneumonia in paediatric patients. Respirology 2012, 17, 354–362. [Google Scholar] [CrossRef]
- Ishiguro, N.; Koseki, N.; Kaiho, M.; Ariga, T.; Kikuta, H.; Togashi, T.; Oba, K.; Morita, K.; Nagano, N.; Nakanishi, M.; et al. Therapeutic efficacy of azithromycin, clarithromycin, minocycline and tosufloxacin against macrolide-resistant and macrolide-sensitive Mycoplasma pneumoniae pneumonia in pediatric patients. PLoS ONE 2017, 12, e0173635. [Google Scholar] [CrossRef] [PubMed]
- Lung, D.C.; Yip, E.K.T.; Lam, D.S.Y.; Que, T.L. Rapid Defervescence After Doxycycline Treatment of Macrolide-resistant Mycoplasma pneumoniae–Associated Community-acquired Pneumonia in Children. Pediatr. Infect. Dis. J. 2013, 32, 1396–1399. [Google Scholar] [CrossRef]
- Cao, B.; Zhao, C.; Yin, Y.; Zhao, F.; Song, S.; Bai, L.; Zhang, J.; Liu, Y.; Zhang, Y.; Wang, H.; et al. High Prevalence of Macrolide Resistance inMycoplasma pneumoniaeIsolates from Adult and Adolescent Patients with Respiratory Tract Infection in China. Clin. Infect. Dis. 2010, 51, 189–194. [Google Scholar] [CrossRef]
- Bébéar, C.; Pereyre, S.; Peuchant, O. Mycoplasma pneumoniae: Susceptibility and resistance to antibiotics. Futur. Microbiol. 2011, 6, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Dégrange, S.; Renaudin, H.; Charron, A.; Pereyre, S.; Bebear, C. Reduced susceptibility to tetracyclines is associated in vitro with the presence of 16S rRNA mutations in Mycoplasma hominis and Mycoplasma pneumoniae. J. Antimicrob. Chemother. 2008, 61, 1390–1392. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.K.; Lee, H.; Ahn, Y.M.; Eun, B.W.; Cho, E.Y.; Cho, H.J.; Yun, K.W.; Lee, H.J.; Choi, E.H. Clonal Expansion of Macrolide-Resistant Sequence Type 3Mycoplasma pneumoniae, South Korea. Emerg. Infect. Dis. 2018, 24, 1465–1471. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-J.; Shin, K.-S.; Lee, K.H.; Kim, Y.R.; Choi, J.H. Clinical Characteristics of Macrolide-Resistant Mycoplasma pneumoniae from Children in Jeju. J. Korean Med Sci. 2017, 32, 1642–1646. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Oishi, T.; Miyata, I.; Wakabayashi, S.; Kono, M.; Ono, S.; Kato, A.; Fukuda, Y.; Saito, A.; Kondo, E.; et al. Macrolide-Resistant Mycoplasma pneumoniae Infection, Japan, 2008–2015. Emerg. Infect. Dis. 2017, 23, 1703–1706. [Google Scholar] [CrossRef] [PubMed]
- Waites, K.B.; Ratliff, A.; Crabb, D.M.; Xiao, L.; Qin, X.; Selvarangan, R.; Tang, Y.W.; Zheng, X.; Bard, J.D.; Hong, T.; et al. Macrolide-Resistant Mycoplasma pneumoniae in the United States as Determined from a National Surveillance Program. J. Clin. Microbiol. 2019, 57, 11. [Google Scholar] [CrossRef] [PubMed]
- Pediatrics, A.A. Tetracyclines. In Red Book: 2018 Report of the Committee on Infectious Diseases; Kimberlin, D.W.B.M., Jackson, M.A., Long, S.S., Eds.; American Academy of Pediatrics: Elk Grove Village, IL, USA, 2018; pp. 905–906. [Google Scholar]
- Lee, H.; Lee, H.; Song, K.H.; Kim, E.S.; Park, J.S.; Jung, J.; Ahn, S.; Jeong, E.K.; Park, H.; Kim, H.B. Impact of Public Health Interventions on Seasonal Influenza Activity During the SARS-CoV-2 Outbreak in Korea. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Kim, N.H.; A Lee, J.; Eun, B.W.; Shin, S.H.; Chung, E.H.; Park, K.W.; Choi, E.H.; Lee, H.J. Comparison of Polymerase Chain Reaction and the Indirect Particle Agglutination Antibody Test for the Diagnosis of Mycoplasma pneumoniae Pneumonia in Children During Two Outbreaks. Pediatr. Infect. Dis. J. 2007, 26, 897–903. [Google Scholar] [CrossRef]
- Okazaki, N.; Narita, M.; Yamada, S.; Izumikawa, K.; Umetsu, M.; Kenri, T.; Sasaki, Y.; Arakawa, Y.; Sasaki, T. Characteristics of Macrolide-ResistantMycoplasma pneumoniaeStrains Isolated from Patients and Induced with ErythromycinIn Vitro. Microbiol. Immunol. 2001, 45, 617–620. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).