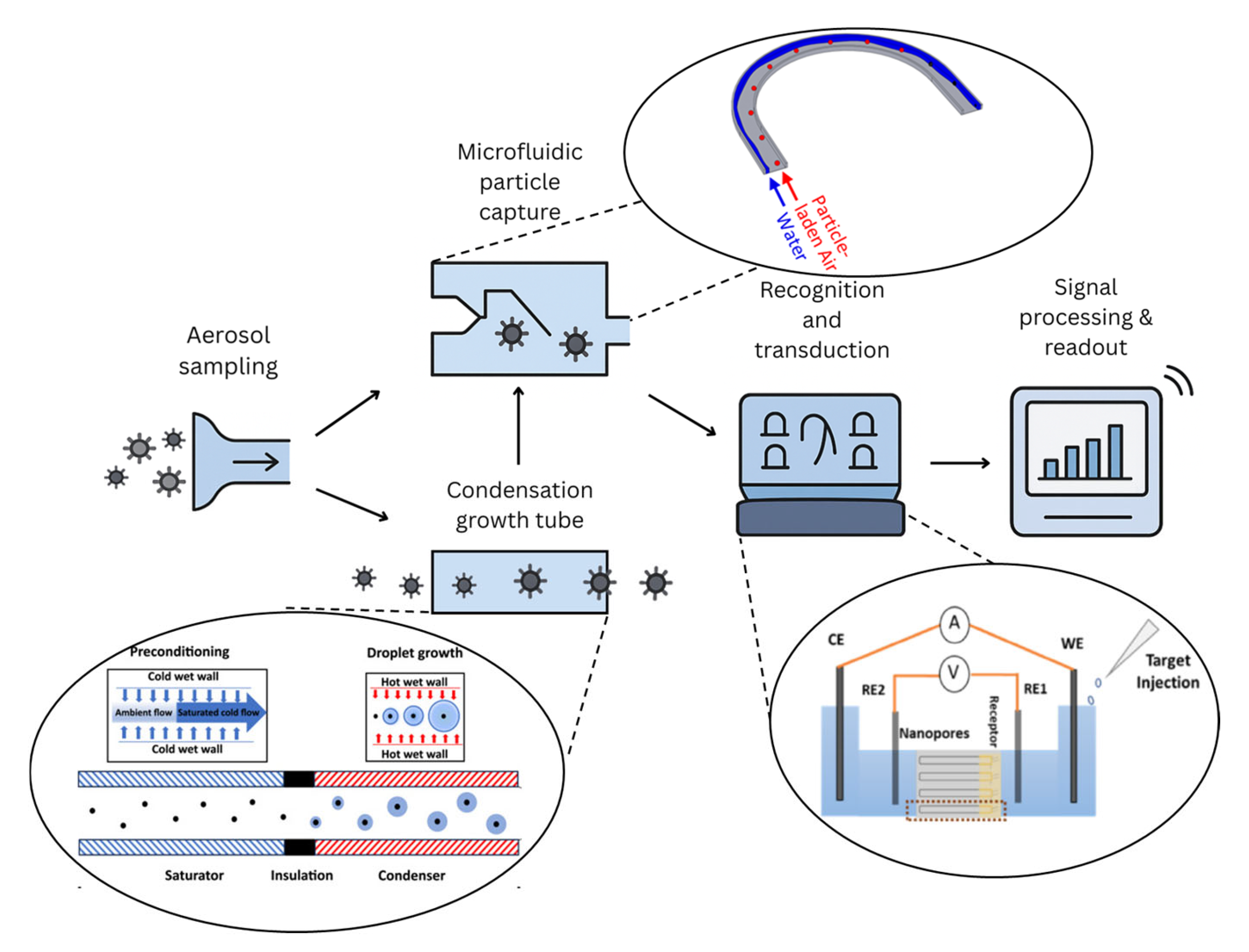
From Aerosol to Signal: Advances in Biosensor Technologies for Airborne Biothreat Detection
Abstract
1. Introduction
2. Biothreats and Their History
Biowarfare and Bioterrorism
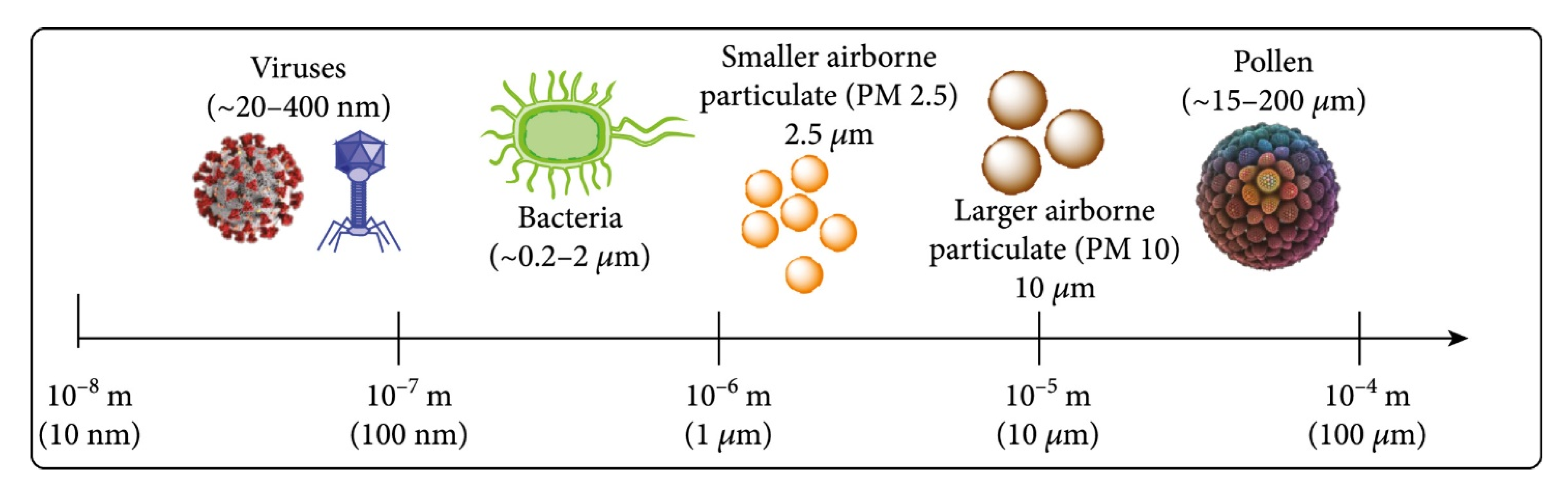
3. Particle Capture
3.1. Microfluidic-Based Capture
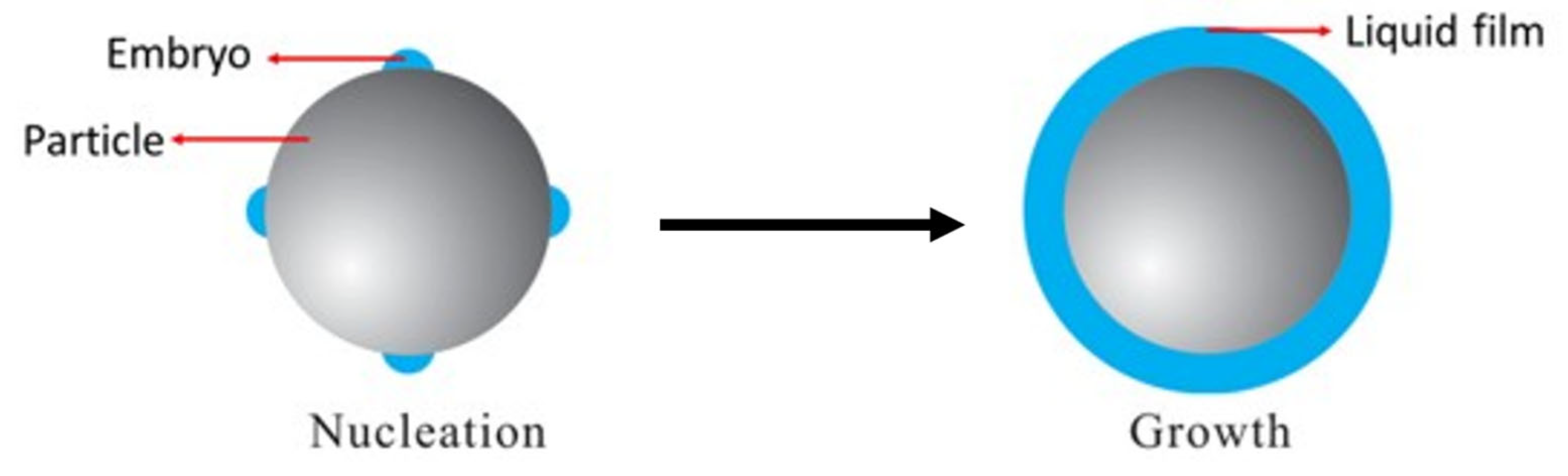
3.2. Condensation-Based Growth Tube for Submicron Particles
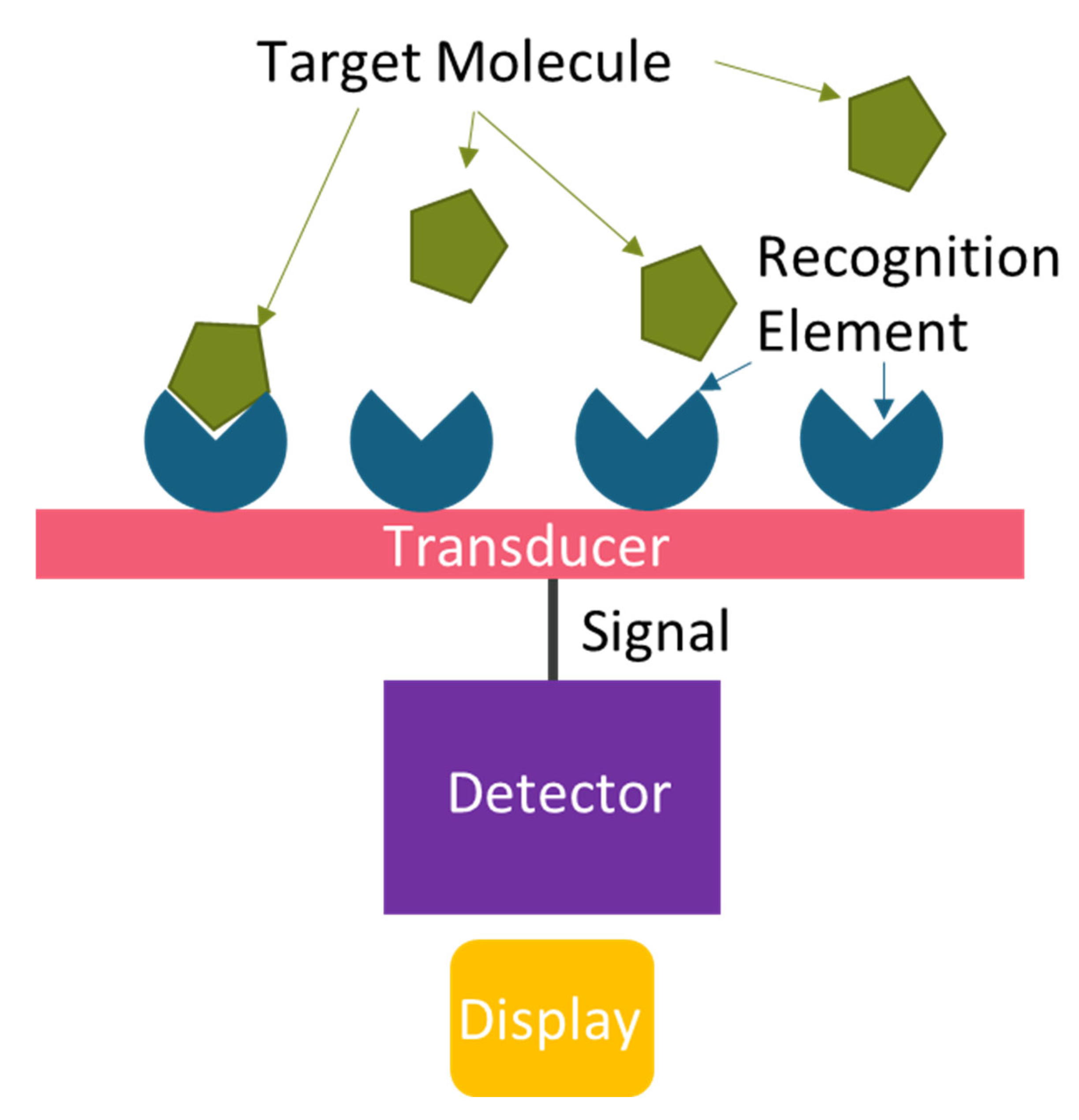
4. Biosensors
4.1. Recognition Elements
4.2. Transduction Mechanisms
4.2.1. Optical Biosensors
4.2.2. Electrochemical Biosensors
4.3. Enhancement Using Nanomaterials
5. Challenges and Future Directions
5.1. Capture Efficiency
5.2. Detection Sensitivity and Specificity
5.3. Real-Time and Continuous Monitoring
5.4. Multiplexing and Broader Detection Capabilities
5.5. Scalability and Field Deployment
5.6. Future Research Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Research Council. Globalization, Biosecurity, and the Future of the Life Sciences; National Academies Press: Washington, DC, USA, 2006; ISBN 9780309653885. [Google Scholar]
- Mousavian, Z.; Fahimi-Kashani, E.; Nafisi, V.; Fahimi-Kashani, N. Recent Advances in Development of Biosensors for Monitoring of Airborne Microorganisms. Iran. J. Biotechnol. 2024, 22, e3722. [Google Scholar] [CrossRef]
- Ma, J.; Du, M.; Wang, C.; Xie, X.; Wang, H.; Zhang, Q. Advances in Airborne Microorganisms Detection Using Biosensors: A Critical Review. Front. Environ. Sci. Eng. 2021, 15, 47. [Google Scholar] [CrossRef] [PubMed]
- Nagel, B.; Dellweg, H.; Gierasch, L.M. Glossary for Chemists of Terms Used in Biotechnology (IUPAC Recommendations 1992). Pure Appl. Chem. 1992, 64, 143–168. [Google Scholar] [CrossRef]
- Leffel, E.K.; Reed, D.S. Marburg and Ebola Viruses as Aerosol Threats. Biosecur. Bioterror. 2004, 2, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Jernigan, D.B.; Raghunathan, P.L.; Bell, B.P.; Brechner, R.; Bresnitz, E.A.; Butler, J.C.; Cetron, M.; Cohen, M.; Doyle, T.; Fischer, M.; et al. Investigation of Bioterrorism-Related Anthrax, United States, 2001: Epidemiologic Findings. Emerg. Infect. Dis. 2002, 8, 1019–1028. [Google Scholar] [CrossRef]
- Borio, L.; Inglesby, T.; Peters, C.J.; Schmaljohn, A.L.; Hughes, J.M.; Jahrling, P.B.; Ksiazek, T.; Johnson, K.M.; Meyerhoff, A.; O’Toole, T.; et al. Hemorrhagic Fever Viruses as Biological WeaponsMedical and Public Health Management. J. Am. Med. Assoc. 2002, 287, 2391–2405. [Google Scholar] [CrossRef]
- Morawska, L.; Milton, D.K. It Is Time to Address Airborne Transmission of Coronavirus Disease 2019 (COVID-19). Clin. Infect. Dis. 2020, 71, 2311–2313. [Google Scholar] [CrossRef]
- Pan, M.; Lednicky, J.A.; Wu, C.-Y. Collection, Particle Sizing and Detection of Airborne Viruses. J. Appl. Microbiol. 2019, 127, 1596–1611. [Google Scholar] [CrossRef]
- Zhang, J.; Yan, S.; Yuan, D.; Alici, G.; Nguyen, N.-T.; Warkiani, M.E.; Li, W. Fundamentals and Applications of Inertial Microfluidics: A Review. Lab Chip 2015, 16, 10–34. [Google Scholar] [CrossRef]
- Ahasan, K.; Schnoebelen, N.J.; Shrotriya, P.; Kingston, T.A. Continuous Sampling of Aerosolized Particles Using Stratified Two-Phase Microfluidics. ACS Sens. 2024, 9, 2915–2924. [Google Scholar] [CrossRef]
- Banerjee, S.; Hemmat, M.A.; Shubham, S.; Gosai, A.; Devarakonda, S.; Jiang, N.; Geekiyanage, C.; Dillard, J.A.; Maury, W.; Shrotriya, P.; et al. Structurally Different Yet Functionally Similar: Aptamers Specific for the Ebola Virus Soluble Glycoprotein and GP1,2 and Their Application in Electrochemical Sensing. Int. J. Mol. Sci. 2023, 24, 4627. [Google Scholar] [CrossRef]
- Bian, J.; Gui, H.; Xie, Z.; Yu, T.; Wei, X.; Wang, W.; Liu, J. Simulation of Three-Stage Operating Temperature for Supersaturation Water-Based Condensational Growth Tube. J. Environ. Sci. 2020, 90, 275–285. [Google Scholar] [CrossRef]
- Walper, S.A.; Lasarte Aragonés, G.; Sapsford, K.E.; Brown, C.W.I.; Rowland, C.E.; Breger, J.C.; Medintz, I.L. Detecting Biothreat Agents: From Current Diagnostics to Developing Sensor Technologies. ACS Sens. 2018, 3, 1894–2024. [Google Scholar] [CrossRef]
- Piret, J.; Boivin, G. Pandemics Throughout History. Front. Microbiol. 2021, 11, 631736. [Google Scholar] [CrossRef]
- Alchon, S.A. A Pest in the Land: New World Epidemics in a Global Perspective; UNM Press: Albuquerque, NM, USA, 2003. [Google Scholar]
- Number of Deaths Due to HIV/AIDS. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/number-of-deaths-due-to-hiv-aids (accessed on 30 July 2025).
- WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 30 June 2025).
- Shipman, P.L. The Bright Side of the Black Death. Available online: https://www.americanscientist.org/article/the-bright-side-of-the-black-death (accessed on 27 November 2023).
- Riedel, S. Edward Jenner and the History of Smallpox and Vaccination. Proc. Bayl. Univ. Med. Cent. 2005, 18, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Dye, C. After 2015: Infectious Diseases in a New Era of Health and Development. Philos. Trans. R Soc. Lond. B Biol. Sci. 2014, 369, 20130426. [Google Scholar] [CrossRef] [PubMed]
- Christian, M.D. Biowarfare and Bioterrorism. Crit. Care Clin. 2013, 29, 717–756. [Google Scholar] [CrossRef] [PubMed]
- Hilleman, M.R. Overview: Cause and Prevention in Biowarfare and Bioterrorism. Vaccine 2002, 20, 3055–3067. [Google Scholar] [CrossRef]
- Frischknecht, F. The History of Biological Warfare. EMBO Rep. 2003, 4, S47–S52. [Google Scholar] [CrossRef]
- Jansen, H.J.; Breeveld, F.J.; Stijnis, C.; Grobusch, M.P. Biological Warfare, Bioterrorism, and Biocrime. Clin. Microbiol. Infect. 2014, 20, 488–496. [Google Scholar] [CrossRef]
- Rathjen, N.A.; Shahbodaghi, S.D. Bioterrorism. Am. Fam. Physician 2021, 104, 376–385. [Google Scholar] [PubMed]
- Borio, L.L.; Henderson, D.A.; Hynes, N.A. Bioterrorism. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases; Elsevier: Amsterdam, The Netherlands, 2015; pp. 178–190.e2. [Google Scholar]
- Barras, V.; Greub, G. History of Biological Warfare and Bioterrorism. Clin. Microbiol. Infect. 2014, 20, 497–502. [Google Scholar] [CrossRef] [PubMed]
- Whitesides, G.M. The Origins and the Future of Microfluidics. Nature 2006, 442, 368–373. [Google Scholar] [CrossRef]
- Islam, M.S. Hybrid Separation of Circulating Tumor Cells in Zigzag and Contraction-Expansion Microfluidic Channels. Master’s Thesis, Washington State University, Pullman, WA, USA, 2022. [Google Scholar]
- Islam, M.S.; Uddin, M.R.; Chen, X. Circulating Tumor Cell Separation in a Zigzag Channel Using Dielectrophoresis Based Inertial Microfluidics; American Society of Mechanical Engineers Digital Collection; American Society of Mechanical Engineers: New York, NY, USA, 2023. [Google Scholar]
- Sackmann, E.K.; Fulton, A.L.; Beebe, D.J. The Present and Future Role of Microfluidics in Biomedical Research. Nature 2014, 507, 181–189. [Google Scholar] [CrossRef]
- Mark, D.; Haeberle, S.; Roth, G.; von Stetten, F.; Zengerle, R. Microfluidic Lab-on-a-Chip Platforms: Requirements, Characteristics and Applications. Chem. Soc. Rev. 2010, 39, 1153–1182. [Google Scholar] [CrossRef]
- Ahasan, K.; Landry, C.M.; Chen, X.; Kim, J.-H. Effect of Angle-of-Attacks on Deterministic Lateral Displacement (DLD) with Symmetric Airfoil Pillars. Biomed. Microdevices 2020, 22, 42. [Google Scholar] [CrossRef]
- Bhagat, A.A.S.; Bow, H.; Hou, H.W.; Tan, S.J.; Han, J.; Lim, C.T. Microfluidics for Cell Separation. Med. Biol. Eng. Comput. 2010, 48, 999–1014. [Google Scholar] [CrossRef]
- Pemathilaka, R.L.; Caplin, J.D.; Aykar, S.S.; Montazami, R.; Hashemi, N.N. Placenta-on-a-Chip: In Vitro Study of Caffeine Transport across Placental Barrier Using Liquid Chromatography Mass Spectrometry. Glob. Chall. 2019, 3, 1800112. [Google Scholar] [CrossRef]
- Hamacher, T.; Berendsen, W.J.T.; van Dongen, J.E.; van der Hee, R.M.; Cornelissen, M.J.J.L.; Broekhuijse, J.M.L.W.; Segerink, L.I. Virus Removal from Semen with a Pinched Flow Fractionation Microfluidic Chip. Lab Chip 2021, 21, 4477–4486. [Google Scholar] [CrossRef]
- Narayana Iyengar, S.; Kumar, T.; Mårtensson, G.; Russom, A. High Resolution and Rapid Separation of Bacteria from Blood Using Elasto-Inertial Microfluidics. Electrophoresis 2021, 42, 2538–2551. [Google Scholar] [CrossRef]
- Wu, Z.; Willing, B.; Bjerketorp, J.; Jansson, K.J.; Hjort, K. Soft Inertial Microfluidics for High Throughput Separation of Bacteria from Human Blood Cells. Lab Chip 2009, 9, 1193–1199. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.S.; Chen, X. Continuous CTC Separation through a DEP-Based Contraction–Expansion Inertial Microfluidic Channel. Biotechnol. Prog. 2023, 39, e3341. [Google Scholar] [CrossRef] [PubMed]
- Sarowar, M.T.; Islam, M.S.; Chen, X. Separation of CTCs From Blood Cells Using Curved Contraction-Expansion Microchannel Equipped With DEP Force; American Society of Mechanical Engineers Digital Collection; American Society of Mechanical Engineers: New York, NY, USA, 2024. [Google Scholar]
- Ahasan, K.; Kim, J.-H. Study of Angle-of-Attack (AoA) for Airfoil in Deterministic Lateral Displacement (DLD). In Proceedings of the ASME 2019 International Mechanical Engineering Congress and Exposition, Volume 10: Micro- and Nano-Systems Engineering and Packaging. Salt Lake City, Utah, USA, 11–14 November 2019; American Society of Mechanical Engineers: New York, NY, USA, 2019; p. V010T12A020. [Google Scholar]
- Ahasan, K.; Senf, B.L.; Kim, J.-H. Controls on the Transport of Particles/Cells in Deterministic Lateral Displacement via Symmetric Airfoil with Angle of Attacks. In Proceedings of the 2020 IEEE 70th Electronic Components and Technology Conference (ECTC), Orlando, FL, USA, 3–30 June 2020; IEEE: Orlando, FL, USA, 2020; pp. 2185–2190. [Google Scholar]
- Ahasan, K.; Islam, M.S.; Shrotriya, P.; Kingston, T.A. Stratified Two-Phase Microfluidic Device for Continuous Sampling of Sub-Micron Aerosolized Particles. J. Aerosol Sci. 2025, 191, 106697. [Google Scholar] [CrossRef]
- Jiang, X.; Jing, W.; Sun, X.; Liu, Q.; Yang, C.; Liu, S.; Qin, K.; Sui, G. High-Throughput Microfluidic Device for LAMP Analysis of Airborne Bacteria. ACS Sens. 2016, 1, 958–962. [Google Scholar] [CrossRef]
- Jing, W.; Jiang, X.; Zhao, W.; Liu, S.; Cheng, X.; Sui, G. Microfluidic Platform for Direct Capture and Analysis of Airborne Mycobacterium Tuberculosis. Anal. Chem. 2014, 86, 5815–5821. [Google Scholar] [CrossRef]
- Jing, W.; Zhao, W.; Liu, S.; Li, L.; Tsai, C.-T.; Fan, X.; Wu, W.; Li, J.; Yang, X.; Sui, G. Microfluidic Device for Efficient Airborne Bacteria Capture and Enrichment. Anal. Chem. 2013, 85, 5255–5262. [Google Scholar] [CrossRef]
- Liu, Q.; Zhang, X.; Yao, Y.; Jing, W.; Liu, S.; Sui, G. A Novel Microfluidic Module for Rapid Detection of Airborne and Waterborne Pathogens. Sens. Actuators B Chem. 2018, 258, 1138–1145. [Google Scholar] [CrossRef]
- Liu, Q.; Zhang, Y.; Jing, W.; Liu, S.; Zhang, D.; Sui, G. First Airborne Pathogen Direct Analysis System. Analyst 2016, 141, 1637–1640. [Google Scholar] [CrossRef]
- Li, X.; Zhang, X.; Liu, Q.; Zhao, W.; Liu, S.; Sui, G. Microfluidic System for Rapid Detection of Airborne Pathogenic Fungal Spores. ACS Sens. 2018, 3, 2095–2103. [Google Scholar] [CrossRef]
- Bian, X.; Lan, Y.; Wang, B.; Zhang, Y.S.; Liu, B.; Yang, P.; Zhang, W.; Qiao, L. Microfluidic Air Sampler for Highly Efficient Bacterial Aerosol Collection and Identification. Anal. Chem. 2016, 88, 11504–11512. [Google Scholar] [CrossRef]
- Inami, H.; Tsuge, K.; Matsuzawa, M.; Sasaki, Y.; Togashi, S.; Komano, A.; Seto, Y. Semi-Automated Bacterial Spore Detection System with Micro-Fluidic Chips for Aerosol Collection, Spore Treatment and ICAN DNA Detection. Biosens. Bioelectron. 2009, 24, 3299–3305. [Google Scholar] [CrossRef]
- Shen, F.; Tan, M.; Wang, Z.; Yao, M.; Xu, Z.; Wu, Y.; Wang, J.; Guo, X.; Zhu, T. Integrating Silicon Nanowire Field Effect Transistor, Microfluidics and Air Sampling Techniques For Real-Time Monitoring Biological Aerosols. Environ. Sci. Technol. 2011, 45, 7473–7480. [Google Scholar] [CrossRef] [PubMed]
- Mirzaee, I.; Song, M.; Charmchi, M.; Sun, H. A Microfluidics-Based on-Chip Impinger for Airborne Particle Collection. Lab A Chip 2016, 16, 2254–2264. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.S.; Lee, K.S.; Kim, S.S.; Bae, G.-N.; Jung, J.H. Real-Time Detection of an Airborne Microorganism Using Inertial Impaction and Mini-Fluorescent Microscopy. Lab A Chip 2014, 14, 244–251. [Google Scholar] [CrossRef]
- Damit, B. Droplet-Based Microfluidics Detector for Bioaerosol Detection. Aerosol Sci. Technol. 2017, 51, 488–500. [Google Scholar] [CrossRef]
- Hong, S.C.; Kang, J.S.; Lee, J.E.; Kim, S.S.; Jung, J.H. Continuous Aerosol Size Separator Using Inertial Microfluidics and Its Application to Airborne Bacteria and Viruses. Lab Chip 2015, 15, 1889–1897. [Google Scholar] [CrossRef]
- Ma, Z.; Zheng, Y.; Cheng, Y.; Xie, S.; Ye, X.; Yao, M. Development of an Integrated Microfluidic Electrostatic Sampler for Bioaerosol. J. Aerosol Sci. 2016, 95, 84–94. [Google Scholar] [CrossRef]
- Resina-Pelfort, O.; Comas-Riu, J.; Vives-Rego, J. Effects of Deflected Droplet Electrostatic Cell Sorting on the Viability and Exoproteolytic Activity of Bacterial Cultures and Marine Bacterioplankton. Syst. Appl. Microbiol. 2001, 24, 31–36. [Google Scholar] [CrossRef]
- Choi, J.; Hong, S.C.; Kim, W.; Jung, J.H. Highly Enriched, Controllable, Continuous Aerosol Sampling Using Inertial Microfluidics and Its Application to Real-Time Detection of Airborne Bacteria. ACS Sens. 2017, 2, 513–521. [Google Scholar] [CrossRef]
- Chua, M.H.; Cheng, W.; Goh, S.S.; Kong, J.; Li, B.; Lim, J.Y.C.; Mao, L.; Wang, S.; Xue, K.; Yang, L.; et al. Face Masks in the New COVID-19 Normal: Materials, Testing, and Perspectives. Research 2020, 2020, 7286735. [Google Scholar] [CrossRef]
- Englert, N. Fine Particles and Human Health—A Review of Epidemiological Studies. Toxicol. Lett. 2004, 149, 235–242. [Google Scholar] [CrossRef]
- Kowalski, W.J.; Bahnfleth, W. Airborne Respiratory Diseases and Mechanical Systems for Control of Microbes. HPAC Heat. Pip. Air Cond. 1998, 70, 7. [Google Scholar]
- Chatterjee, S. Understanding the Nature of Variations in Structural Sequences Coding for Coronavirus Spike, Envelope, Membrane and Nucleocapsid Proteins of SARS-CoV-2. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Harris, A.; Cardone, G.; Winkler, D.C.; Heymann, J.B.; Brecher, M.; White, J.M.; Steven, A.C. Influenza virus pleiomorphy characterized by cryoelectron tomography. Proc. Natl. Acad. Sci. USA 2006, 103, 19123–19127. [Google Scholar] [CrossRef] [PubMed]
- Battles, M.B.; McLellan, J.S. Respiratory Syncytial Virus Entry and How to Block It. Nat. Rev. Microbiol. 2019, 17, 233–245. [Google Scholar] [CrossRef]
- Colf, L.A.; Juo, Z.S.; Garcia, K.C. Structure of the Measles Virus Hemagglutinin. Nat. Struct. Mol. Biol. 2007, 14, 1227–1228. [Google Scholar] [CrossRef]
- Frost, J.R.; Shaikh, S.; Severini, A. Exploring the Mumps Virus Glycoproteins: A Review. Viruses 2022, 14, 1335. [Google Scholar] [CrossRef]
- Tang, J.W. The Effect of Environmental Parameters on the Survival of Airborne Infectious Agents. J. R. Soc. Interface 2009, 6, S737–S746. [Google Scholar] [CrossRef]
- Haddrell, A.E.; Lewis, D.; Church, T.; Vehring, R.; Murnane, D.; Reid, J.P. Pulmonary Aerosol Delivery and the Importance of Growth Dynamics. Ther. Deliv. 2017, 8, 1051–1061. [Google Scholar] [CrossRef]
- Yurt, A.; Daaboul, G.H.; Connor, J.H.; Goldberg, B.B.; Ünlü, M.S. Single Nanoparticle Detectors for Biological Applications. Nanoscale 2012, 4, 715–726. [Google Scholar] [CrossRef]
- Podzimek, J. John Aitken’s Contribution to Atmospheric and Aerosol Sciences—One Hundred Years of Condensation Nuclei Counting. Bull. Am. Meteorol. Soc. 1989, 70, 1538–1545. [Google Scholar] [CrossRef]
- Esq, J.A. On Improvements in the Apparatus for Counting the Dust Particles in the Atmosphere. Proc. R. Soc. Edinb. 1890, 16, 135–172. [Google Scholar] [CrossRef]
- Ahasan, K.; Hu, H.; Shrotriya, P.; Kingston, T.A. Heterogeneous Condensation on Simplified Viral Envelope Protein Structures. ACS Appl. Mater. Interfaces 2025, 17, 27829–27838. [Google Scholar] [CrossRef] [PubMed]
- Tammaro, M.; Di Natale, F.; Salluzzo, A.; Lancia, A. Heterogeneous Condensation of Submicron Particles in a Growth Tube. Chem. Eng. Sci. 2012, 74, 124–134. [Google Scholar] [CrossRef]
- Thomson, W. On the Equilibrium of Vapour at a Curved Surface of Liquid. Lond. Edinb. Dublin Philos. Mag. J. Sci. 1871, 42, 448–452. [Google Scholar] [CrossRef]
- Holländer, W.; Dunkhorst, W.; Lödding, H.; Windt, H. Theoretical Simulation and Experimental Characterization of an Expansion-Type Kelvin Spectrometer with Intrinsic Calibration. J. Atmos. Ocean. Technol. 2002, 19, 1811–1825. [Google Scholar] [CrossRef]
- Smorodin, V.Y.; Hopke, P.K. Condensation Activation and Nucleation on Heterogeneous Aerosol Nanoparticles. J. Phys. Chem. B 2004, 108, 9147–9157. [Google Scholar] [CrossRef]
- Fan, Y.; Qin, F.; Luo, X.; Lin, L.; Gui, H.; Liu, J. Heterogeneous Condensation on Insoluble Spherical Particles: Modeling and Parametric Study. Chem. Eng. Sci. 2013, 102, 387–396. [Google Scholar] [CrossRef]
- Agarwal, J.K.; Sem, G.J. Continuous Flow, Single-Particle-Counting Condensation Nucleus Counter. J. Aerosol Sci. 1980, 11, 343–357. [Google Scholar] [CrossRef]
- McMurry, P.H. The History of Condensation Nucleus Counters. Aerosol Sci. Technol. 2000, 33, 297–322. [Google Scholar] [CrossRef]
- Sinclair, D.; Hoopes, G.S. A Continuous Flow Condensation Nucleus Counter. J. Aerosol Sci. 1975, 6, 1–7. [Google Scholar] [CrossRef]
- Hering, S.V.; Stolzenburg, M.R. A Method for Particle Size Amplification by Water Condensation in a Laminar, Thermally Diffusive Flow. Aerosol Sci. Technol. 2005, 39, 428–436. [Google Scholar] [CrossRef]
- Hering, S.V.; Stolzenburg, M.R.; Quant, F.R.; Oberreit, D.R.; Keady, P.B. A Laminar-Flow, Water-Based Condensation Particle Counter (WCPC). Aerosol Sci. Technol. 2005, 39, 659–672. [Google Scholar] [CrossRef]
- Lewis, G.S.; Hering, S.V. Minimizing Concentration Effects in Water-Based, Laminar-Flow Condensation Particle Counters. Aerosol Sci. Technol. 2013, 47, 645–654. [Google Scholar] [CrossRef]
- Hering, S.V.; Spielman, S.R.; Lewis, G.S. Moderated, Water-Based, Condensational Particle Growth in a Laminar Flow. Aerosol Sci. Technol. 2014, 48, 401–408. [Google Scholar] [CrossRef]
- Hering, S.V.; Lewis, G.S.; Spielman, S.R.; Eiguren-Fernandez, A.; Kreisberg, N.M.; Kuang, C.; Attoui, M. Detection near 1-Nm with a Laminar-Flow, Water-Based Condensation Particle Counter. Aerosol Sci. Technol. 2017, 51, 354–362. [Google Scholar] [CrossRef]
- Hering, S.V.; Lewis, G.S.; Spielman, S.R.; Eiguren-Fernandez, A. A MAGIC Concept for Self-Sustained, Water-Based, Ultrafine Particle Counting. Aerosol Sci. Technol. 2019, 53, 63–72. [Google Scholar] [CrossRef]
- Oh, S.; Anwar, D.; Theodore, A.; Lee, J.-H.; Wu, C.-Y.; Wander, J. Development and Evaluation of a Novel Bioaerosol Amplification Unit (BAU) for Improved Viral Aerosol Collection. J. Aerosol Sci. 2010, 41, 889–894. [Google Scholar] [CrossRef]
- Pan, M.; Eiguren-Fernandez, A.; Hsieh, H.; Afshar-Mohajer, N.; Hering, S.V.; Lednicky, J.; Fan, Z.H.; Wu, C.-Y. Efficient Collection of Viable Virus Aerosol through Laminar-Flow, Water-Based Condensational Particle Growth. J. Appl. Microbiol. 2016, 120, 805–815. [Google Scholar] [CrossRef]
- Pan, M.; Carol, L.; Lednicky, J.A.; Eiguren-Fernandez, A.; Hering, S.; Fan, Z.H.; Wu, C.-Y. Determination of the Distribution of Infectious Viruses in Aerosol Particles Using Water-Based Condensational Growth Technology and a Bacteriophage MS2 Model. Aerosol Sci. Technol. 2019, 53, 583–593. [Google Scholar] [CrossRef]
- Pan, M.; Carol, L.; Lednicky, J.A.; Eiguren-Fernandez, A.; Hering, S.; Fan, Z.H.; Wu, C.-Y. Collection of Airborne Bacteria and Yeast through Water-Based Condensational Growth. Aerobiologia 2018, 34, 337–348. [Google Scholar] [CrossRef]
- Pan, M.; Bonny, T.S.; Loeb, J.; Jiang, X.; Lednicky, J.A.; Eiguren-Fernandez, A.; Hering, S.; Fan, Z.H.; Wu, C.-Y. Collection of Viable Aerosolized Influenza Virus and Other Respiratory Viruses in a Student Health Care Center through Water-Based Condensation Growth. mSphere 2017, 2, e00251-17. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Park, J.; Im, H.; Jung, H. A Microfluidic ATP-Bioluminescence Sensor for the Detection of Airborne Microbes. Sens. Actuators B Chem. 2008, 132, 443–448. [Google Scholar] [CrossRef]
- Yu, Y.; Zhang, J.; Zhong, H. Heterogeneous Condensation of Water Vapor on Fine SiO 2 Particles in Two-Section Growth Tube. Energy Fuels 2018, 32, 12750–12757. [Google Scholar] [CrossRef]
- Tammaro, M. Heterogeneous Condensation for Submicronic Particles Abatement. Ph.D. Thesis, Università Degli Studi di Napoli Federico II, Naples, Italy, 2010. [Google Scholar]
- Xu, J.; Yu, Y.; Zhang, J.; Meng, Q.; Zhong, H. Heterogeneous Condensation of Water Vapor on Particles at High Concentration. Powder Technol. 2017, 305, 71–77. [Google Scholar] [CrossRef]
- Yu, Y.; Lu, Y.; Sang, C.; Xu, C.; Nie, T.; Xing, S.; Fu, C. Growth Characteristics of Submicron Particles by Water Vapor Condensation in the Multi-Section Growth Tube. Powder Technol. 2024, 440, 119797. [Google Scholar] [CrossRef]
- Yu, Y.; Zhang, J.; Xu, C. Numerical Simulation on the Growth of Polydisperse Fine SiO2 Particles by Water Vapor Condensation. Powder Technol. 2021, 385, 537–545. [Google Scholar] [CrossRef]
- Kwon, H.-B.; Yoo, S.-J.; Kim, Y.-J. Microfluidic Condensation Nanoparticle Counter Using Water as the Condensing Liquid for Assessing Individual Exposure to Airborne Nanoparticles. Lab A Chip 2020, 20, 1092–1102. [Google Scholar] [CrossRef]
- Kwon, H.-B.; Yoo, S.-J.; Hong, U.-S.; Kim, K.; Han, J.; Kim, M.-K.; Kang, D.-H.; Hwang, J.; Kim, Y.-J. MEMS-Based Condensation Particle Growth Chip for Optically Measuring the Airborne Nanoparticle Concentration. Lab A Chip 2019, 19, 1471–1483. [Google Scholar] [CrossRef]
- Balendra, S.; Kale, A.; Pongetti, J.; Kazemimanesh, M.; Haugen, M.; Weller, L.; Boies, A. Condensation Particle Counters: Exploring the Limits of Miniaturisation. J. Aerosol Sci. 2024, 175, 106266. [Google Scholar] [CrossRef]
- Yoo, S.-J.; Oh, J.; Hong, S.-J.; Kim, M.; Hwang, J.; Kim, Y.-J. Microfluidics-Based Condensation Bioaerosol Sampler for Multipoint Airborne Virus Monitoring. Biosens. Bioelectron. 2024, 264, 116658. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhou, Q.; Li, G.; Chang, L.; Chen, L.; Li, Y. Investigation into Detection Efficiency Deviations in Aviation Soot and Calibration Particles Based on Condensation Particle Counting. Symmetry 2024, 16, 244. [Google Scholar] [CrossRef]
- Li, Y.; Chen, X.; Wu, J.; Zhang, Q.; Zhang, Z.; Hao, J.; Jiang, J. A Convertible Condensation Particle Counter Using Alcohol or Water as the Working Fluid. Aerosol Sci. Technol. 2025, 59, 185–194. [Google Scholar] [CrossRef]
- Chen, K.; Xu, W.; Wang, J.; Li, Q.; Lin, Y. Optimization of Guide Blades Structure for Swirl Growth Tube Based on Revised Steam Phase Change Particle Agglomeration Model. Chem. Eng. Res. Des. 2025, 213, 66–77. [Google Scholar] [CrossRef]
- Dai, A.; Zhang, J.; Li, A. Growth Characteristics of Atmospheric Fine Particles in Turbulent Water Vapor Environment. J. Environ. Eng. 2024, 150, 04024033. [Google Scholar] [CrossRef]
- Wang, Q.; Wang, L.; Wu, H.; Yang, H. Promoting Fine Particle Removal in Double-Tower Cascade Wet Flue Gas Desulfurization System by Flue Gas Temperature Reduction. Powder Technol. 2020, 373, 581–589. [Google Scholar] [CrossRef]
- Yang, L.; Bao, J.; Yan, J.; Liu, J.; Song, S.; Fan, F. Removal of Fine Particles in Wet Flue Gas Desulfurization System by Heterogeneous Condensation. Chem. Eng. J. 2010, 156, 25–32. [Google Scholar] [CrossRef]
- Rajapaksha, P.; Elbourne, A.; Gangadoo, S.; Brown, R.; Cozzolino, D.; Chapman, J. A Review of Methods for the Detection of Pathogenic Microorganisms. Analyst 2019, 144, 396–411. [Google Scholar] [CrossRef]
- Franco-Duarte, R.; Černáková, L.; Kadam, S.; Kaushik, K.S.; Salehi, B.; Bevilacqua, A.; Corbo, M.R.; Antolak, H.; Dybka-Stępień, K.; Leszczewicz, M.; et al. Advances in Chemical and Biological Methods to Identify Microorganisms—From Past to Present. Microorganisms 2019, 7, 130. [Google Scholar] [CrossRef]
- Parida, M.M.; Dash, P.K.; Shukla, J. Advance Detection Technologies for Select Biothreat Agents. In Handbook on Biological Warfare Preparedness; Elsevier: Amsterdam, The Netherlands, 2020; pp. 83–102. [Google Scholar] [CrossRef]
- Cesewski, E.; Johnson, B.N. Electrochemical Biosensors for Pathogen Detection. Biosens. Bioelectron. 2020, 159, 112214. [Google Scholar] [CrossRef]
- Alhajj, M.; Zubair, M.; Farhana, A. Enzyme Linked Immunosorbent Assay. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Aydin, S. A Short History, Principles, and Types of ELISA, and Our Laboratory Experience with Peptide/Protein Analyses Using ELISA. Peptides 2015, 72, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, S.; Putalun, W.; Vimolmangkang, S.; Phoolcharoen, W.; Shoyama, Y.; Tanaka, H.; Morimoto, S. Enzyme-Linked Immunosorbent Assay for the Quantitative/Qualitative Analysis of Plant Secondary Metabolites. J. Nat. Med. 2018, 72, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Garibyan, L.; Avashia, N. Research Techniques Made Simple: Polymerase Chain Reaction (PCR). J. Invest. Dermatol. 2013, 133, e6. [Google Scholar] [CrossRef] [PubMed]
- Bhalla, N.; Jolly, P.; Formisano, N.; Estrela, P. Introduction to Biosensors. Essays Biochem. 2016, 60, 1–8. [Google Scholar] [CrossRef]
- Mehrotra, P. Biosensors and Their Applications—A Review. J. Oral Biol. Craniofacial Res. 2016, 6, 153. [Google Scholar] [CrossRef]
- Varnakavi, N.; Lee, N. A Review on Biosensors and Recent Development of Nanostructured Materials-Enabled Biosensors. Sensors 2021, 21, 1109. [Google Scholar] [CrossRef]
- Samuel, V.R.; Rao, K.J. A Review on Label Free Biosensors. Biosens. Bioelectron. X 2022, 11, 100216. [Google Scholar] [CrossRef]
- Morales, M.A.; Mark Halpern, J. Guide to Selecting a Biorecognition Element for Biosensors. Bioconjug. Chem. 2018, 29, 3231–3239. [Google Scholar] [CrossRef]
- Sharma, S.; Byrne, H.; O’Kennedy, R.J. Antibodies and Antibody-Derived Analytical Biosensors. Essays Biochem. 2016, 60, 9–18. [Google Scholar] [CrossRef]
- Clark, L.C., Jr.; Lyons, C. Electrode Systems for Continuous Monitoring in Cardiovascular Surgery. Ann. N Y Acad. Sci. 1962, 102, 29–45. [Google Scholar] [CrossRef]
- Rocchitta, G.; Spanu, A.; Babudieri, S.; Latte, G.; Madeddu, G.; Galleri, G.; Nuvoli, S.; Bagella, P.; Demartis, M.I.; Fiore, V.; et al. Enzyme Biosensors for Biomedical Applications: Strategies for Safeguarding Analytical Performances in Biological Fluids. Sensors 2016, 16, 780. [Google Scholar] [CrossRef]
- BelBruno, J.J. Molecularly Imprinted Polymers. Chem. Rev. 2019, 119, 94–119. [Google Scholar] [CrossRef]
- Xu, Y.; Jiang, X.; Zhou, Y.; Ma, M.; Wang, M.; Ying, B. Systematic Evolution of Ligands by Exponential Enrichment Technologies and Aptamer-Based Applications: Recent Progress and Challenges in Precision Medicine of Infectious Diseases. Front. Bioeng. Biotechnol. 2021, 9, 704077. [Google Scholar] [CrossRef] [PubMed]
- Ning, Y.; Hu, J.; Lu, F. Aptamers Used for Biosensors and Targeted Therapy. Biomed. Pharmacother. 2020, 132, 110902. [Google Scholar] [CrossRef] [PubMed]
- Sett, A.; Das, S.; Sharma, P.; Bora, U. Aptasensors in Health, Environment and Food Safety Monitoring. Open J. Appl. Biosens. 2012, 1, 9–19. [Google Scholar] [CrossRef]
- De Penning, S.; Murphy, M.P.; Kingston, T.A.; Nilsen-Hamilton, M.; Shrotriya, P. Influence of Crosslinker on Aptamer Immobilization and Aptasensor Sensing Response for Non-Metallic Surfaces. Biosens. Bioelectron. 2025, 270, 116933. [Google Scholar] [CrossRef]
- Justino, C.I.L.; Duarte, A.C.; Rocha-Santos, T.A.P. Recent Progress in Biosensors for Environmental Monitoring: A Review. Sensors 2017, 17, 2918. [Google Scholar] [CrossRef]
- Lv, L.; Xu, Z.; Zhou, Y.; Wu, J.; Zhang, X.; Qi, H. A Biosensor Based on Commercial R-SAW for Rapid and Sensitive Detection of E. Coli. Chemosensors 2025, 13, 308. [Google Scholar] [CrossRef]
- Alanazi, N.; Almutairi, M.; Alodhayb, A.N. A Review of Quartz Crystal Microbalance for Chemical and Biological Sensing Applications. Sens Imaging 2023, 24, 10. [Google Scholar] [CrossRef]
- Liu, Y.; Tuleouva, N.; Ramanculov, E.; Revzin, A. Aptamer-Based Electrochemical Biosensor for Interferon Gamma Detection. Anal. Chem. 2010, 82, 8131–8136. [Google Scholar] [CrossRef]
- Sassolas, A.; Leca-Bouvier, B.D.; Blum, L.J. DNA Biosensors and Microarrays. Chem. Rev. 2008, 108, 109–139. [Google Scholar] [CrossRef]
- Fan, X.; White, I.M.; Shopova, S.I.; Zhu, H.; Suter, J.D.; Sun, Y. Sensitive Optical Biosensors for Unlabeled Targets: A Review. Anal. Chim. Acta 2008, 620, 8–26. [Google Scholar] [CrossRef] [PubMed]
- Damborský, P.; Švitel, J.; Katrlík, J. Optical Biosensors. Essays Biochem. 2016, 60, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Syahir, A.; Usui, K.; Tomizaki, K.; Kajikawa, K.; Mihara, H. Label and Label-Free Detection Techniques for Protein Microarrays. Microarrays 2015, 4, 228–244. [Google Scholar] [CrossRef]
- Sikora, T.; Osuchowski, Ł.; Maziejuk, M.; Lisowski, W. Mobile Device for Detection of Biological Threat. In Proceedings of the 2017 International Carnahan Conference on Security Technology (ICCST), Madrid, Spain, 23–26 October 2017; pp. 1–4. [Google Scholar]
- Petrovszki, D.; Valkai, S.; Gora, E.; Tanner, M.; Bányai, A.; Fürjes, P.; Dér, A. An Integrated Electro-Optical Biosensor System for Rapid, Low-Cost Detection of Bacteria. Microelectron. Eng. 2021, 239–240, 111523. [Google Scholar] [CrossRef]
- Janik, M.; Brzozowska, E.; Czyszczoń, P.; Celebańska, A.; Koba, M.; Gamian, A.; Bock, W.J.; Śmietana, M. Optical Fiber Aptasensor for Label-Free Bacteria Detection in Small Volumes. Sens. Actuators B Chem. 2021, 330, 129316. [Google Scholar] [CrossRef]
- Fernández Blanco, A.; Hernández Pérez, M.; Moreno Trigos, Y.; García-Hernández, J. Development of Optical Label-Free Biosensor Method in Detection of Listeria Monocytogenes from Food. Sensors 2023, 23, 5570. [Google Scholar] [CrossRef]
- Shen, R.; Hui, W.; Wu, W.; Yang, N.; Lin, X.; Mak, P.-I.; Martins, R.P.; Liu, A.; Jia, Y. A Cost-Effective and Field-Deployable Sensing System for Chip-Integrated Detection of Bacteria with the Naked Eye. Sens. Actuators B Chem. 2024, 410, 135668. [Google Scholar] [CrossRef]
- Jiao, C.; Li, X.; Zhang, Z.; Wu, Y.; Ren, X.; Pawliszyn, J.; Zeng, J. Field-Deployable Immuno-Solid-Phase Microextraction Coupled with Photothermal Imaging for Rapid Pathogen Surveillance in Environmental and Clinical Matrices. Anal. Chem. 2025, 97, 20602–20610. [Google Scholar] [CrossRef]
- Roda, A.; Michelini, E.; Zangheri, M.; Di Fusco, M.; Calabria, D.; Simoni, P. Smartphone-Based Biosensors: A Critical Review and Perspectives. TrAC Trends Anal. Chem. 2016, 79, 317–325. [Google Scholar] [CrossRef]
- Pohanka, M. Overview of Piezoelectric Biosensors, Immunosensors and DNA Sensors and Their Applications. Materials 2018, 11, 448. [Google Scholar] [CrossRef]
- Lazcka, O.; Campo, F.J.D.; Muñoz, F.X. Pathogen Detection: A Perspective of Traditional Methods and Biosensors. Biosens. Bioelectron. 2007, 22, 1205–1217. [Google Scholar] [CrossRef] [PubMed]
- Turner, A.P.F. Biosensors: Sense and Sensibility. Chem. Soc. Rev. 2013, 42, 3184–3196. [Google Scholar] [CrossRef]
- Grieshaber, D.; MacKenzie, R.; Vörös, J.; Reimhult, E. Electrochemical Biosensors—Sensor Principles and Architectures. Sensors 2008, 8, 1400–1458. [Google Scholar] [CrossRef] [PubMed]
- Setterington, E.B.; Alocilja, E.C. Electrochemical Biosensor for Rapid and Sensitive Detection of Magnetically Extracted Bacterial Pathogens. Biosensors 2012, 2, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Pintavirooj, C.; Vongmanee, N.; Sukjee, W.; Sangma, C.; Visitsattapongse, S. Biosensors for Klebsiella Pneumoniae with Molecularly Imprinted Polymer (MIP) Technique. Sensors 2022, 22, 4638. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Jeffries, L.; Mach, K.E.; Craft, D.W.; Thomas, N.J.; Gau, V.; Liao, J.C.; Wong, P.K. A Multiplex Electrochemical Biosensor for Bloodstream Infection Diagnosis. SLAS Technol. 2017, 22, 466–474. [Google Scholar] [CrossRef]
- Wei, H.; Bu, S.; Zhang, W.; Ma, L.; Liu, X.; Wang, Z.; Li, Z.; Hao, Z.; He, X.; Wan, J. An Electrochemical Biosensor for the Detection of Pathogenic Bacteria Based on Dual Signal Amplification of Cu3(PO4)2-Mediated Click Chemistry and DNAzymes. Analyst 2021, 146, 4841–4847. [Google Scholar] [CrossRef]
- Hannah, A.J.; Ward, A.C.; Connolly, P. Rapidly Detected Common Wound Pathogens via Easy-to-Use Electrochemical Sensors. J. Biomed. Eng. Biosci. JBEB 2021, 8, 11–20. [Google Scholar] [CrossRef]
- Wu, Q.; Ya, Y.; Jin, C.; Zhao, Y.; Yan, F.; Feng, D.; Huang, K.-J.; Xie, S.; Tan, X. From Leaf to Lab-on-Cloth: Spatial DNA Nanorobotics and 2D Graphyne Synergy Enable Ultra-Precise Electrochemical Tracking of Sugarcane Pokkah Boeng Disease. Biosens. Bioelectron. 2025, 283, 117548. [Google Scholar] [CrossRef]
- Qiu, W.; Xu, H.; Takalkar, S.; Gurung, A.S.; Liu, B.; Zheng, Y.; Guo, Z.; Baloda, M.; Baryeh, K.; Liu, G. Carbon Nanotube-Based Lateral Flow Biosensor for Sensitive and Rapid Detection of DNA Sequence. Biosens. Bioelectron. 2015, 64, 367–372. [Google Scholar] [CrossRef] [PubMed]
- Pinals, R.L.; Ledesma, F.; Yang, D.; Navarro, N.; Jeong, S.; Pak, J.E.; Kuo, L.; Chuang, Y.-C.; Cheng, Y.-W.; Sun, H.-Y.; et al. Rapid SARS-CoV-2 Spike Protein Detection by Carbon Nanotube-Based Near-Infrared Nanosensors. Nano Lett. 2021, 21, 2272–2280. [Google Scholar] [CrossRef] [PubMed]
- Jiang, N.; Shrotriya, P.; Dassanayake, R.P. NK-Lysin Antimicrobial Peptide-Functionalized Nanoporous Alumina Membranes as Biosensors for Label-Free Bacterial Endotoxin Detection. Biochem. Biophys. Res. Commun. 2022, 636, 18–23. [Google Scholar] [CrossRef]
- Anisuzzaman, S.; Alimoradi, N.; Singappuli-Arachchige, D.; Banerjee, S.; Pogorelko, G.V.; Kaiyum, Y.A.; Johnson, P.E.; Shrotriya, P.; Nilsen-Hamilton, M. Pyoverdine Binding Aptamers and Label-Free Electrochemical Detection of Pseudomonads. Front. Chem. 2024, 12, 1438710. [Google Scholar] [CrossRef]
- Gosai, A.; Hau Yeah, B.S.; Nilsen-Hamilton, M.; Shrotriya, P. Label Free Thrombin Detection in Presence of High Concentration of Albumin Using an Aptamer-Functionalized Nanoporous Membrane. Biosens. Bioelectron. 2019, 126, 88–95. [Google Scholar] [CrossRef]
- Santos, A.; Kumeria, T.; Losic, D. Nanoporous Anodic Aluminum Oxide for Chemical Sensing and Biosensors. TrAC Trends Anal. Chem. 2013, 44, 25–38. [Google Scholar] [CrossRef]
- Zelada-Guillén, G.A.; Blondeau, P.; Rius, F.X.; Riu, J. Carbon Nanotube-Based Aptasensors for the Rapid and Ultrasensitive Detection of Bacteria. Methods 2013, 63, 233–238. [Google Scholar] [CrossRef]
| Date (Year) | Epidemics/Pandemics | Pathogen | Death Toll (Millions) |
|---|---|---|---|
| 165–180 | Antonine Plague | Variola virus a | 5–10 |
| 541–549 | Plague of Justinian | Yersinia pestis | 15–100 |
| 735–737 | Japanese smallpox | Variola virus | 2 |
| 1346–1353 | Black Death | Yersinia pestis | 75–200 |
| 1519–1520 | Mexico smallpox epidemic | Variola virus | 5–8 |
| 1545–1548 | Cocoliztli epidemic | Salmonella enterica a | 5–15 |
| 1576–1580 | Cocoliztli epidemic | Salmonella enterica a | 2–2.5 |
| 1629–1631 | Italian plague | Yersinia pestis | 1 |
| 1656–1658 | Naples Plague | Yersinia pestis | 1.25 |
| 1772–1773 | Persian Plague | Yersinia pestis | 2 |
| 1846–1860 | Cholera pandemic | Vibrio cholerae | 1+ |
| 1855–1960 | Third Plague Pandemic | Yersinia pestis | 12–15 |
| 1889–1890 | Flu pandemic | Influenza A/H3N8 a | 1 |
| 1918–1920 | Spanish flu | Influenza A/H1N1 | 17–100 |
| 1918–1922 | Russia typhus epidemic | Rickettsia prowazekii | 2–3 |
| 1957–1958 | Influenza pandemic | Influenza A/H2N2 | 1–4 |
| 1968–1969 | Hong Kong flu | Influenza A/H3N2 | 1–4 |
| 1981–present | HIV/AIDS pandemic | HIV-1 | 44+ (as of July 2025) |
| 2019–present | COVID-19 pandemic | SARS-CoV-2 | 7 (as of June 2025) |
| Category | Disease | Pathogen | Historical Abuse |
|---|---|---|---|
| A | Anthrax | Bacillus anthracis | World War I, World War II, Soviet Union (1979), Japan (1995), USA (2001) |
| Botulism | Clostridium botulinum | - | |
| Hemorrhagic Fever | Marburg virus | Soviet bioweapons program | |
| - | Ebola virus | - | |
| - | Arenaviruses | - | |
| Plague | Yersinia pestis | Fourteenth-century Europe, World War II | |
| Smallpox | Variola major | Eighteenth-century North America | |
| Tularemia | Francisella tularensis | World War II | |
| B | Brucellosis | Brucella | - |
| Cholera | Vibrio cholera | World War II | |
| Encephalitis | Alphaviruses | World War II | |
| Food Poisoning | Salmonella, Shigella | World War II, USA (1990s) | |
| Glanders | Burkholderia mallei | World War I, World War II | |
| Psittacosis | Chlamydia psittaci | - | |
| Q Fever | Coxiella burnetii | - | |
| Typhus | Rickettsia prowazekii | World War II | |
| Various Toxic Syndromes | Various bacteria | World War II | |
| C | Emerging pathogens | ||
| Operating Mechanism | Microfluidic Design | Target Particle/Organism | Advantages/Limitations |
|---|---|---|---|
| Inertia-based/Passive mixing | Staggered herringbone microchannels [45,46,47,48,49] | E. coli, M. smegmatis, M. tuberculosis | Simple design, efficient for bacteria; longer capture times (1–3 h) |
| Herringbone microchannels [50] | Aspergillus niger spores | Good for spores; limited real-time sensitivity | |
| Three-loop spiral with herringbone & sawtooth [51] | General aerosol particles | Improved mixing; manual steps required | |
| On-chip impinger [54] | Microorganisms | Moderate throughput; simple operation | |
| Inertial forces + mini fluorescent microscopy [55] | Microorganisms | Real-time detection; limited scale | |
| Droplet-based + wet-cyclone sampler [56] | Particles 2–5 µm | Captures medium particles; poor submicron efficiency | |
| Size-based separation microfluidic system [57] | Submicron particles | Size-selective; complex operation, ~70% efficiency | |
| U-shaped stratified liquid stream [60] | Particles 0.6–2.1 µm | High submicron efficiency; more complex channel design | |
| U-shaped stratified flow microchannel [11,44] | Aerosol particles | Validated numerically & experimentally; improved capture | |
| Electrostatic | Electrostatic microfluidic sampler [58] | Particles < 5 µm | Can target small particles; may alter biological properties, ~40% efficiency |
| Filtration-based | PDMS microfilter-based membrane [48] | General bioaerosols | Simple and passive; low throughput, time-intensive |
| Sensor-based/Electrical | Silicon nanowire FET + microfluidic [53] | Influenza virus | Enables electrical detection; limited sensitivity (20–30% signal increase) |
| Integrated/Multi-step | Semi-automated microfluidic chip [52] | Spores | Combines collection & amplification; multi-step, moderate throughput |
| Recognition Element | Typical Targets | Advantages | Limitations | Field-Deployability |
|---|---|---|---|---|
| Antibodies | Proteins, toxins, pathogens | High specificity and affinity; well-established | Expensive; sensitive to temperature, pH, humidity | Low–Moderate |
| Enzymes | Toxins, metabolites, small molecules | Rapid signal; high catalytic specificity | Short shelf life; denatures easily | Low |
| DNA/RNA Probes | Nucleic Acid Sequences | Sequence-specific; strong specificity | Limited to known nucleic acid targets; cannot detect whole pathogens | Moderate |
| Aptamers | Proteins, toxins, pathogens, small molecules | Chemically stable; easily modified; high affinity; suitable for portable devices | SELEX can be slow; some non-specific adsorption | High |
| Molecularly Imprinted Polymers (MIPs) | Small molecules, proteins, toxins | Synthetic and robust; long shelf life; inexpensive | Lower selectivity; less sensitive in complex samples | High |
| Author | Sensor Type | Target(s) | Performance (LoD/Time) | Specificity | Nanomaterial |
|---|---|---|---|---|---|
| Sikora et al. [139] | Optical | Multiple bacteria | 102–106 CFU/mL/Real-time | High | None |
| Petrovszki et al. [140] | Optical | E. coli | ~102 CFU/mL/N/A | High | None |
| Janik et al. [141] | Optical | E. coli O157:H7 | 10 CFU/mL/N/A | High | None |
| Fernández Blanco et al. [142] | Optical | Listeria monocytogenes | 102 CFU/mL/4 h | High | None |
| Shen et al. [143] | Optical | E. coli, S. enterica | 3 copies/Few hours | High | None |
| Jiao et al. [144] | Optical | SARS-CoV-2 N, Flu A NP | 68–75 pg/mL/15 min | High | None |
| Qiu et al. [156] | Optical | Specific DNA sequences | 40 pM/min | High | Multi-walled carbon nanotubes (MWCNTs) |
| Pinals et al. [157] | Optical | SARS-CoV-2 spike protein | 12.6 nM/Minutes | High | Single-walled carbon nanotubes (SWCNTs) |
| Setterington & Alocilja [150] | Electrochemical | Bacillus cereus, E. coli O157:H7 | 40 CFU/mL/65 min (B. cereus); 6 CFU/mL/65 min (E. coli) | Moderate | None |
| Pintavirooj et al. [151] | Electrochemical | Klebsiella pneumoniae | 0.012 CFU/mL/N/A | High | None |
| Gao et al. [152] | Electrochemical | Bloodstream bacteria (16S rRNA) | 290 CFU/mL/1 h | High | None |
| Wei et al. [153] | Electrochemical | Salmonella typhimurium | 10 CFU/mL/N/A | High | None |
| Hannah et al. [154] | Electrochemical | Proteus mirabilis, Pseudomonas aeruginosa, Staphylococcus aureus | 7.4 × 106 CFU/mL/1–2.5 h | Moderate | None |
| Wu et al. [155] | Electrochemical | Pokkah boeng pathogen (sugarcane) | 16.6 aM/N/A | High | None |
| Jiang et al. [158] | Electrochemical | LPS (Gram-negative), LTA (Gram-positive) | 10 ng/mL/N/A | High | NAAO |
| Anisuzzaman et al. [159] | Electrochemical | Pyoverdine Pf5 (Pseudomonas) | 1.3 nM/N/A | High | NAAO |
| Banerjee et al. [12] | Electrochemical | Ebola virus sGP, GP1,2 | 150 pM/N/A | High | NAAO |
| Gosai et al. [160] | Electrochemical | α-Thrombin | 10 pM/N/A | High | NAAO |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Penning, S.; Islam, M.S.; Ahasan, K.; Kingston, T.A.; Shrotriya, P. From Aerosol to Signal: Advances in Biosensor Technologies for Airborne Biothreat Detection. Biosensors 2025, 15, 764. https://doi.org/10.3390/bios15120764
De Penning S, Islam MS, Ahasan K, Kingston TA, Shrotriya P. From Aerosol to Signal: Advances in Biosensor Technologies for Airborne Biothreat Detection. Biosensors. 2025; 15(12):764. https://doi.org/10.3390/bios15120764
Chicago/Turabian StyleDe Penning, Samuel, Md Sadiqul Islam, Kawkab Ahasan, Todd A. Kingston, and Pranav Shrotriya. 2025. "From Aerosol to Signal: Advances in Biosensor Technologies for Airborne Biothreat Detection" Biosensors 15, no. 12: 764. https://doi.org/10.3390/bios15120764
APA StyleDe Penning, S., Islam, M. S., Ahasan, K., Kingston, T. A., & Shrotriya, P. (2025). From Aerosol to Signal: Advances in Biosensor Technologies for Airborne Biothreat Detection. Biosensors, 15(12), 764. https://doi.org/10.3390/bios15120764





