Nanomaterials, which exist in the size range between the atomic and macroscopic levels, exhibit unique properties such as a high specific surface area, high reactivity, high strength, low thermal resistance, high specific heat capacity, high diffusivity, and special magnetic and optical properties [
1]. These characteristics render nanoparticles exceptionally versatile for biomedical applications.
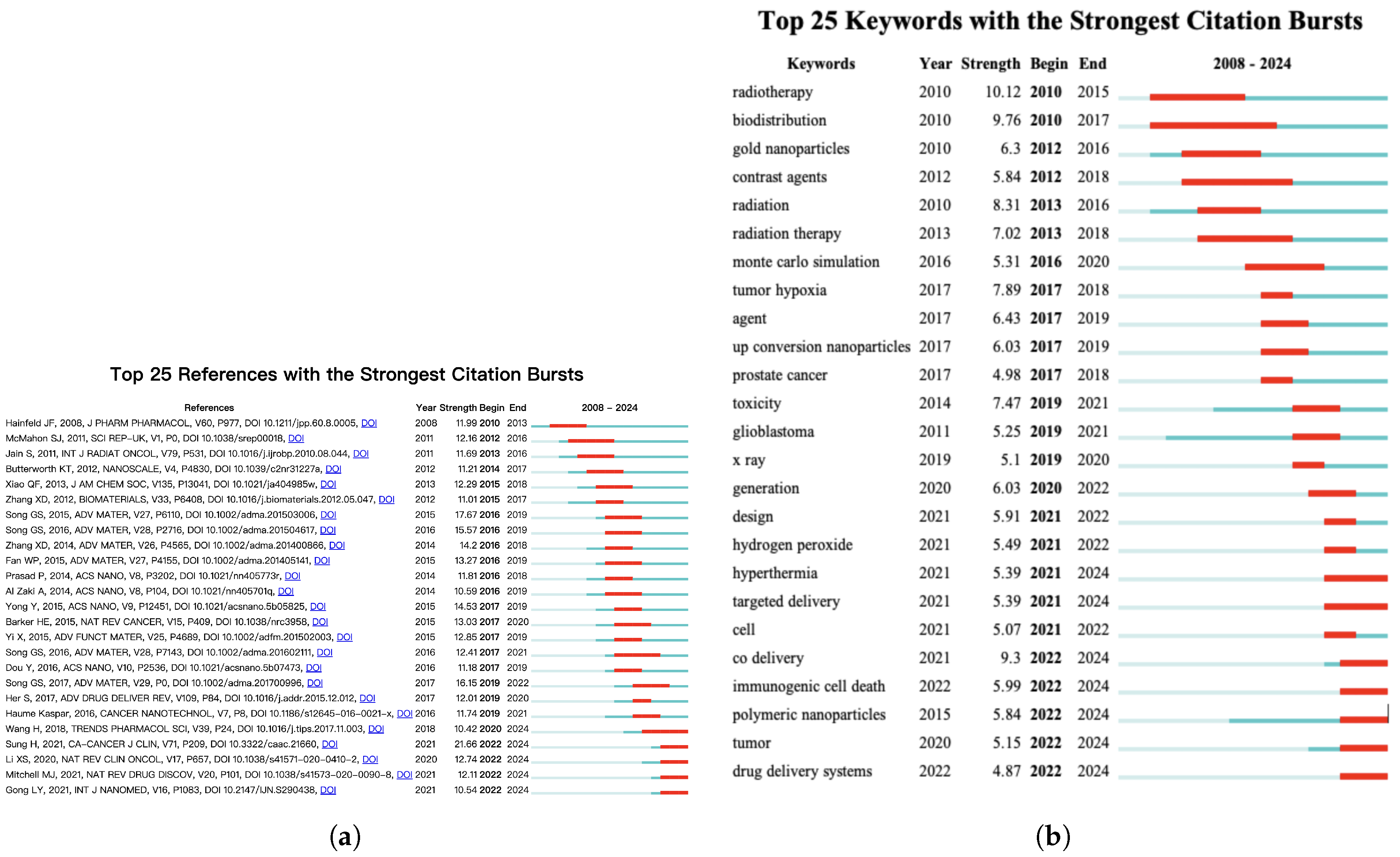
Based on the 20 most cited review articles and the most frequently occurring keywords over the past 20 years, research hotspots in this field can be broadly categorized in two primary directions. The first direction, nanomaterials used as radiosensitizers, includes photothermal therapy, photodynamic therapy, radiosensitizing materials, artificial intelligence, sonodynamic therapy, and catalytic oxygenation therapy. The second direction pertains to the use of nanomaterials in comprehensive cancer therapies, including targeted therapy, drug delivery, tumor microenvironment modulation, immunotherapy, and immune enhancement. Although we categorized research hotspots into two main domains, nanomaterials as radiosensitizers and nanomaterials for comprehensive cancer therapy, it is important to note that these categories are not mutually exclusive. For example, the use of nanomaterials in immunotherapy can enhance radiosensitivity and contribute to a comprehensive cancer treatment. Therefore, this classification provides a practical framework for understanding the literature, and the boundaries between these categories are inherently fluid and reflect the interdisciplinary and integrative nature of this evolving research field. Below, we provide a detailed overview of the research progress in these two areas.
4.2.1. Nanomaterials as Radiosensitizers
Radiotherapy has gained traction in clinical settings to eliminate tumors through the application of localized ionizing radiation beams. However, the efficacy of radiotherapy is typically limited by tumor hypoxia-associated radiation resistance [
8]. Additionally, radiotherapy has limited efficacy in controlling tumor metastasis, which is the primary cause of cancer-related mortality. Researchers have extensively investigated radiosensitization strategies to address relatively low radiation therapy efficiency. Radiosensitization refers to the process of augmenting the efficacy of radiation therapy by increasing the radiosensitivity of cancer cells [
9]. This concept is central to oncology, as it has the potential to significantly improve patient outcomes. The mechanisms underlying radiosensitization are multifaceted and can be categorized at the molecular, cellular, and microenvironmental levels, all of which play crucial roles in enhancing the effectiveness of radiotherapy.
At the molecular level, tumor cells typically rely on DNA repair pathways to mitigate radiation-induced damage [
10]. Radiosensitization can be achieved by inhibiting DNA repair pathways, particularly single- and double-strand breaks. Inhibition of key DNA repair proteins such as poly (ADP-ribose) polymerase (PARP), ataxia-telangiectasia mutated (ATM), and ATM- and Rad3-related (ATR) proteins can prevent the repair of radiation-induced damage, thereby enhancing radiosensitization [
11]. At the cellular level, the primary objective of radiosensitization is to modify cellular response mechanisms to radiation-induced damage [
12,
13,
14]. For example, the cell cycle influences cellular radiosensitivity, with cells in the G2/M phase exhibiting greater susceptibility to radiation-induced damage [
15]. Strategies such as synchronizing tumor cells in the G2/M phase using drugs [
16,
17,
18] or inhibiting cell cycle checkpoints using inhibitors can significantly improve sensitivity to radiotherapy [
19,
20]. Furthermore, the tumor microenvironment (TME) complicates the response to radiation. Hypoxia, an abnormal vasculature, and the presence of immune cells contribute to radiation resistance. Hypoxic regions are common in most solid tumors, exhibit radioresistant biological effects, and represent the most aggressive fraction of a tumor [
21]. Several preclinical studies, both in vitro and in vivo, have indicated that decreasing oxygen concentrations induces resistance to radiation [
22]. The TME enhances oxygen availability via strategies such as hypoxia-activated prodrugs or antiangiogenic therapies, thereby improving the tumor response to radiation therapy [
23,
24]. In addition, the immune microenvironment enhances radiosensitivity. Radiation therapy has the potential to induce immune responses that contribute to the eradication of tumor cells. By targeting DNA repair, cell cycle regulation, immune responses, signaling pathways, and the tumor microenvironment, researchers can mitigate radiotherapy resistance and improve the efficacy of radiotherapy.
Metallic radioactive nanoparticles (MRNPs) are a promising class of nanomaterials designed to enhance the efficacy of radiotherapy by improving radiation absorption, tumor targeting, and theragnostic capabilities [
25]. These nanoparticles, typically composed of high-atomic-number metals, such as gold, silver, and platinum, are known for their ability to generate heat and produce reactive oxygen species. They enhance radiation absorption and produce secondary electrons that damage cancerous cells. By integrating radionuclides, such as Iodine-131, Yttrium-90, and Lutetium-177, MRNPs deliver targeted radiation directly to tumors, thereby minimizing damage to the surrounding healthy tissues [
26]. Their high surface area and tunability enable the efficient loading of therapeutic agents, and functionalization with tumor-targeting ligands improves their specificity [
27]. In addition to MRNPs, inorganic-based nanocarriers, including carbon nanotubes (CNTs), graphene oxide (GO), and fullerenes, have gained traction as radiosensitizers in cancer radiotherapy owing to their unique properties such as their high surface area, biocompatibility, and strong interaction with radiation. CNTs have been extensively studied because of their ability to enhance radiation therapy. Their high surface area and ability to absorb and scatter radiation result in the generation of secondary electrons, which enhance DNA damage in tumor cells [
28]. Similarly, GO, which exhibits a two dimensional structure, has shown promise in radiotherapy by improving the delivery of radioactive isotopes, such as Iodine-131 or Yt-trium-90, and serving as a platform for the co-delivery of chemotherapeutic agents [
29]. Fullerenes are another class of carbon-based nanoparticles that have been explored for their potential in radionuclide therapy owing to their ability to encapsulate radioactive agents and enhance their therapeutic effects. Carbon-based nanoparticles can be functionalized with targeting ligands to improve tumor specificity and reduce off-target toxicity [
30]. Despite their potential, challenges such as biodegradation and immune system interactions remain, necessitating further investigations to ensure the safe and effective clinical application of CNTs in radiotherapy.
4.2.2. Nanomaterials for Comprehensive Cancer Therapy
Tumor tissues are characterized by abnormal vascular proliferation, including high vascular density, poor vascular wall integrity, wide interstitial spaces, and slow lymphatic drainage. These features enable nanoparticles of specific sizes to penetrate and accumulate in tumor tissues, thereby achieving efficient and accurate enrichment at the tumor site. This phenomenon is known as the “enhanced permeability and retention (EPR)” effect, which is a form of passive targeting [
31].This effect arises from the unique characteristics of the tumor vasculature. Unlike normal tissues, tumors often exhibit chaotic, highly permeable blood vessels with large fenestrations (ranging from 100 to 800 nm) that allow nanoparticles to extravasate more easily. In addition, tumors typically lack functional lymphatic drainage, which prevents the efficient removal of extravasated materials. These two factors, enhanced vascular permeability and impaired lymphatic clearance, together create a microenvironment that facilitates the passive accumulation and prolonged retention of nanoparticles at the tumor site. By attaching ligands that bind specifically to tumor markers (e.g., tumor-associated antigens or receptors), nanoparticles are directed to specific tumor sites, thereby facilitating drug accumulation within tumor tissues and reducing their distribution to nontumor areas. This approach converts passive targeting into active targeting. The common ligands include antibodies, small molecules, and aptamers. Polymeric and liposomal nanoparticles have also been widely studied for their potential to enhance cancer radiotherapy via improved drug delivery, circulation time-targeted therapy, and reduced systemic toxicity. Polymeric nanoparticles, typically composed of biocompatible polymers such as poly(lactic-co-glycolic) acid (PLGA) and polyethylene glycol (PEG), provide excellent stability, controlled release, and the ability to encapsulate both chemotherapeutic agents and radioactive isotopes [
32]. These nanoparticles can be functionalized with targeting ligands to enhance tumor specificity and improve the therapeutic index. Liposomal nanoparticles, which are composed of lipid bilayers that encapsulate drugs or radionuclides, offer similar advantages by increasing the solubility of hydrophobic agents and providing a platform for multifunctional therapy. Liposomes can be loaded with radionuclides for targeted radiotherapy while facilitating imaging techniques such as magnetic resonance imaging (MRI) and positron emission tomography [
33]. Both polymeric and liposomal nanoparticles have been designed to overcome challenges such as rapid clearance and nonspecific distribution by utilizing surface modifications such as PEGylation to extend the circulation time and enhance tumor accumulation [
34]. Among the nanocarriers, liposomes and albumin-bound paclitaxel formulations are already applied in clinical settings [
2]. Nanocarriers based on PLGA have been approved for specific clinical applications, such as lipid nanoparticles for vaccine delivery, including those used in COVID-19 vaccines [
35]. Additionally, iron-based nanomaterials, such as superparamagnetic iron oxide nanoparticles and ferromoxytol, have been approved for use as contrast agents in MRI [
36].
Furthermore, silica-based nanoparticles (SiNPs) have garnered significant attention in cancer radiotherapy owing to their unique physicochemical properties, including their high surface area, tunable porosity, and excellent biocompatibility [
37]. They provide stable and biocompatible platforms for encapsulating radionuclides, thereby ensuring a controlled release and prolonged therapeutic effect [
38]. The large surface area of SiNPs enables the efficient loading of radionuclides and chemotherapeutic agents, facilitating the controlled release and prolonged therapeutic effects at the tumor site [
39]. Despite their promising potential, challenges related to the biodegradation and clearance of silica nanoparticles are being actively addressed through the development of biodegradable silica-based systems that aim to enhance their safety and efficacy for clinical applications [
40]. Nanocarriers based on biological materials such as albumin nanoparticles are widely employed for long-term drug delivery and enhanced drug stability. Stimuli-responsive nanocarriers, which represent another promising class of materials, release drugs in response to specific stimuli, such as pH, temperature, light, the magnetic field, or sound, thereby enabling more precise and efficient drug delivery. Nanomaterials have also been explored for their use in immunotherapy. For instance, the interaction between CD47 and Signal Regulatory Protein (SIRP) is crucial for regulating the homeostasis of the immune system by acting as a “don’t eat me” signal that inhibits macrophage-mediated phagocytosis. Polymer-based nanoparticles have been used to display and block CD47 expression. Nanoparticles coated with CD47 can interact with SIRPα on macrophages to avoid clearance, while those designed to block CD47–SIRPα interactions can promote the phagocytosis of tumor cells by inhibiting this signaling pathway [
41]. Beyond these applications, nanomaterials can modulate the tumor microenvironment and improve immune cell activity against tumors [
42]. Researchers have used nanomaterials that encapsulate Stimulator of Interferon Gene (STING) agonists to improve their bioavailability and tumor penetration, which is crucial for effective immune modulation [
43]. Nanomaterials used to improve the sensitivity and specificity of detecting Circulating Tumor Cells (CTCs) have emerged as a prominent research focus in immunotherapy and demonstrate significant potential [
44]. Aljabali et al. developed various strategies using nanomaterials, including liposomes, polymers, and inorganic nanoparticles, highlighting the fact that nanomaterials can be designed for precise targeted delivery and to modulate the immune system for improved immunomodulatory efficacy [
45]. The classifications and applications of nanomaterials for cancer treatment are summarized in
Table 6.