The Effects of Titanium Dioxide Nanoparticles on Osteoblasts Mineralization: A Comparison between 2D and 3D Cell Culture Models
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Characterization of TiO2 NPs
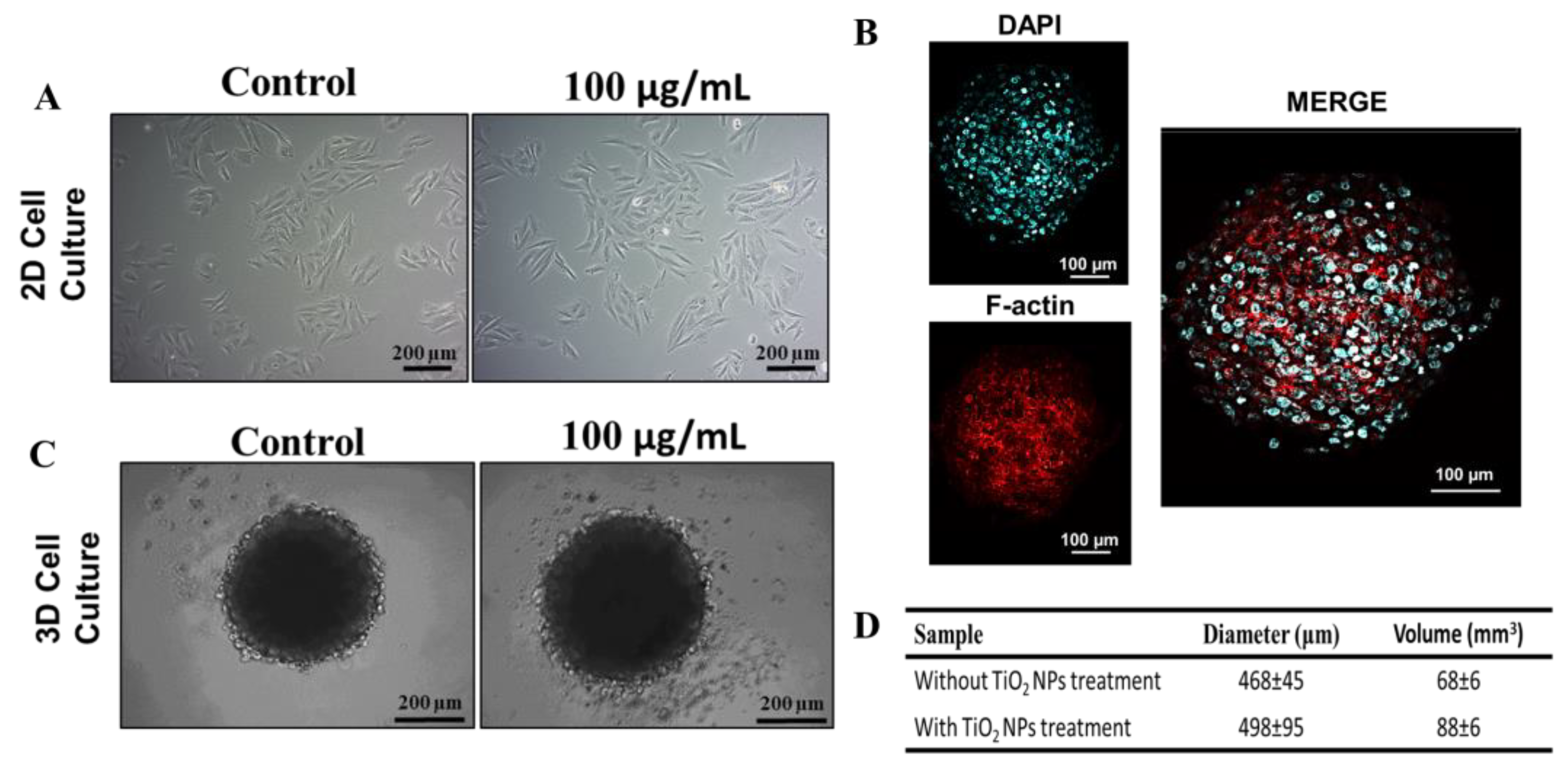
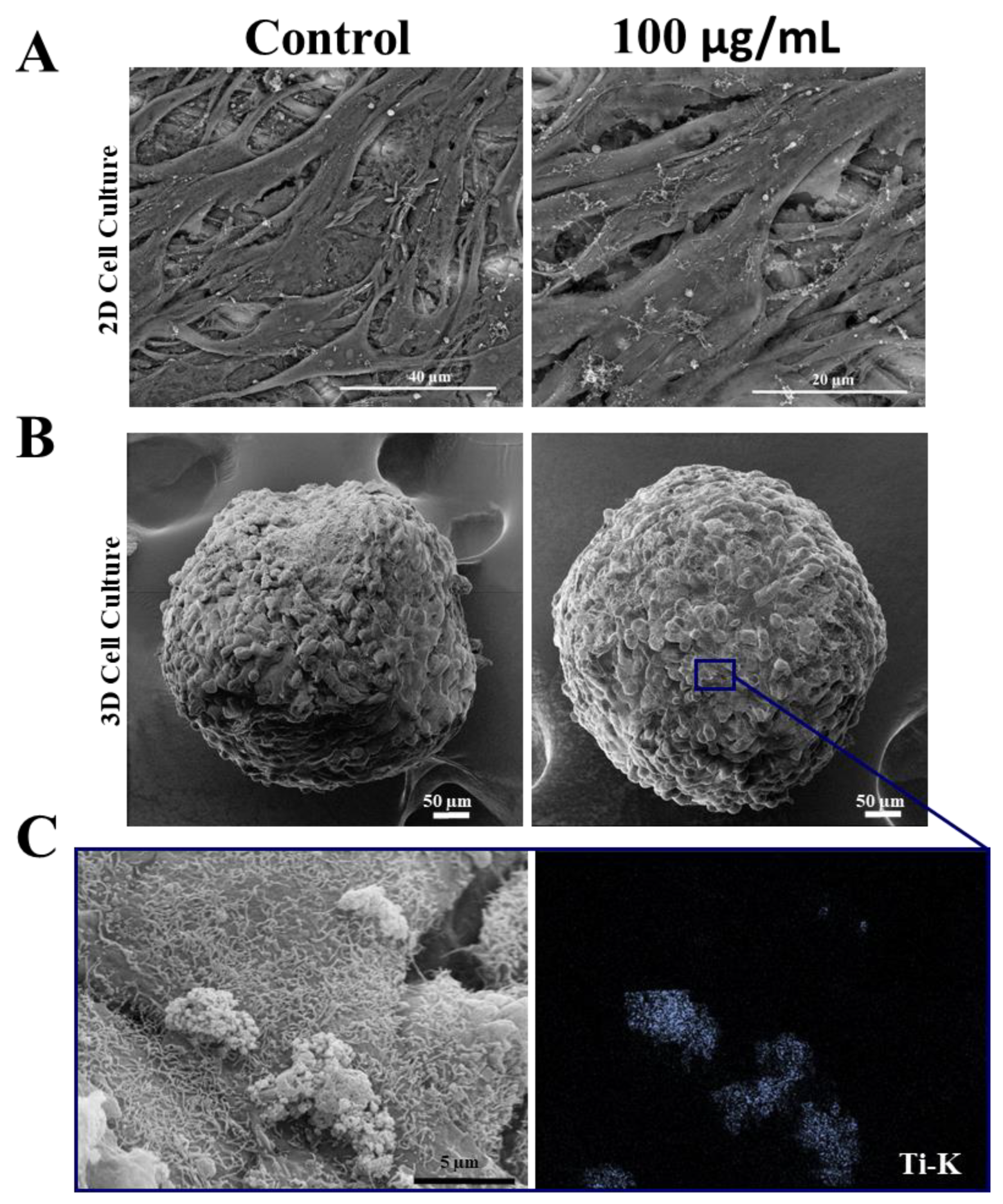
3.2. Effect of TiO2 NPs on the Morphology of 2D and 3D Human Osteoblasts
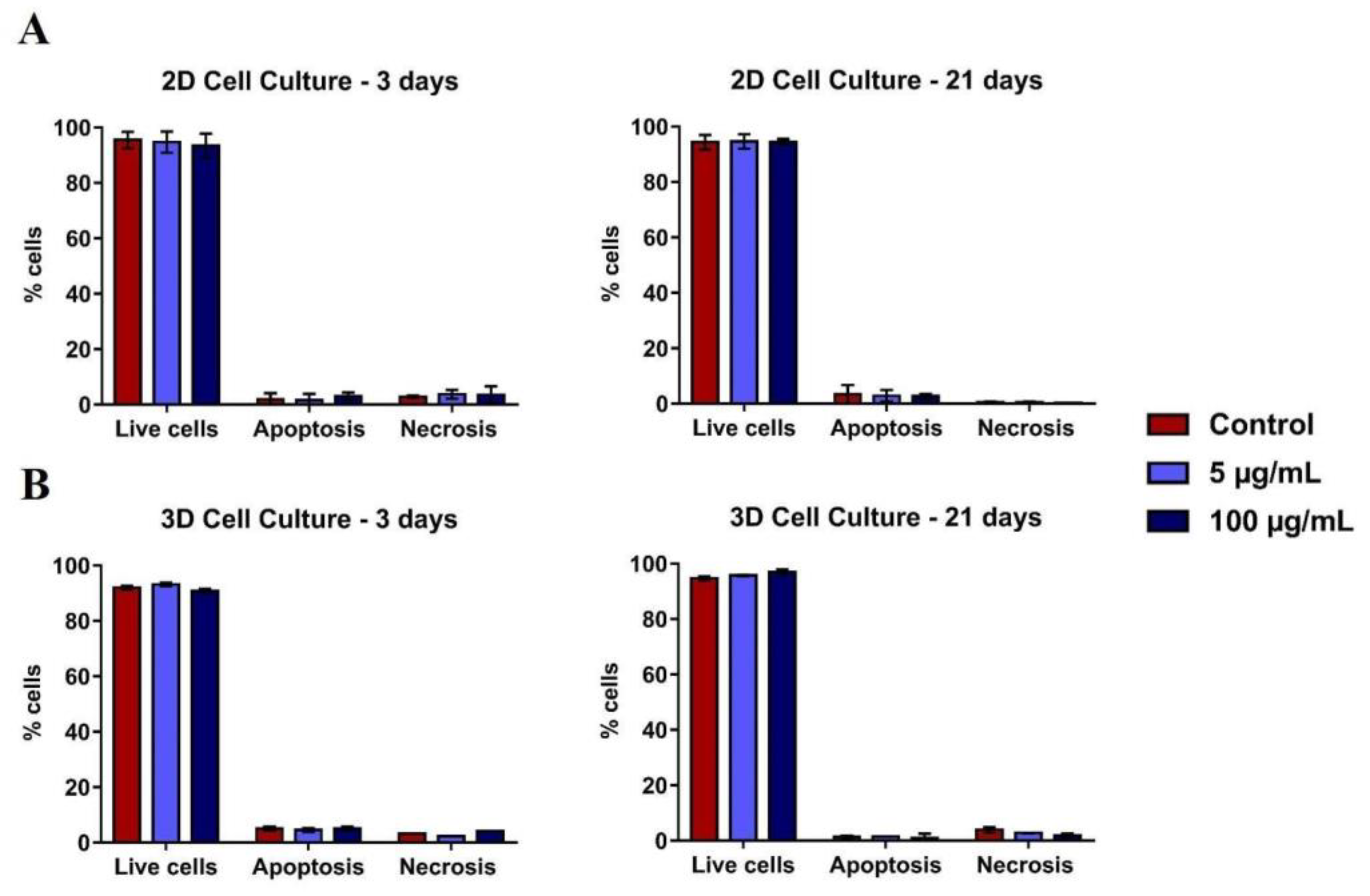
3.3. Effect of TiO2 NPs on Human Osteoblast Viability
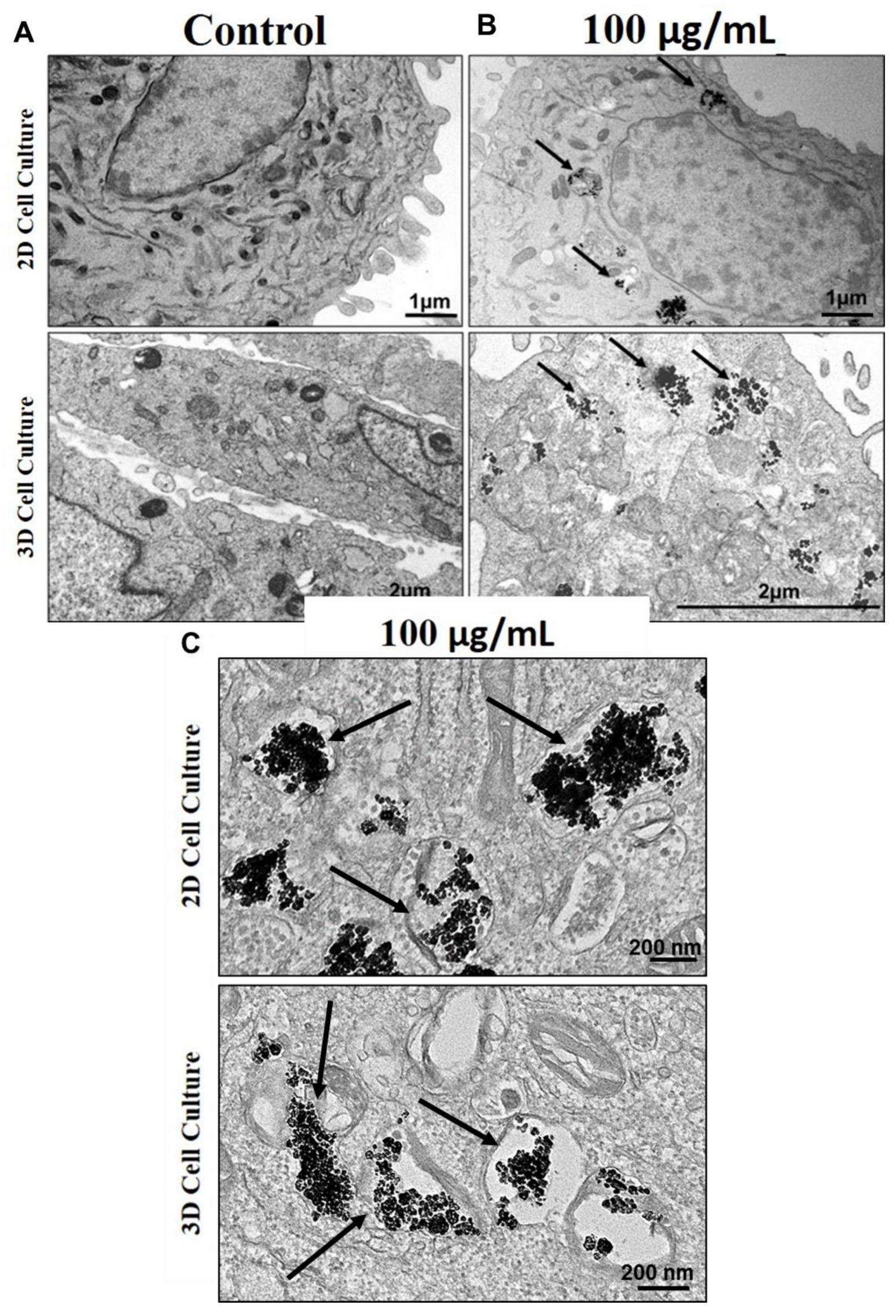
3.4. Internalization of TiO2 NPs in 2D and 3D Culture of Human Osteoblasts
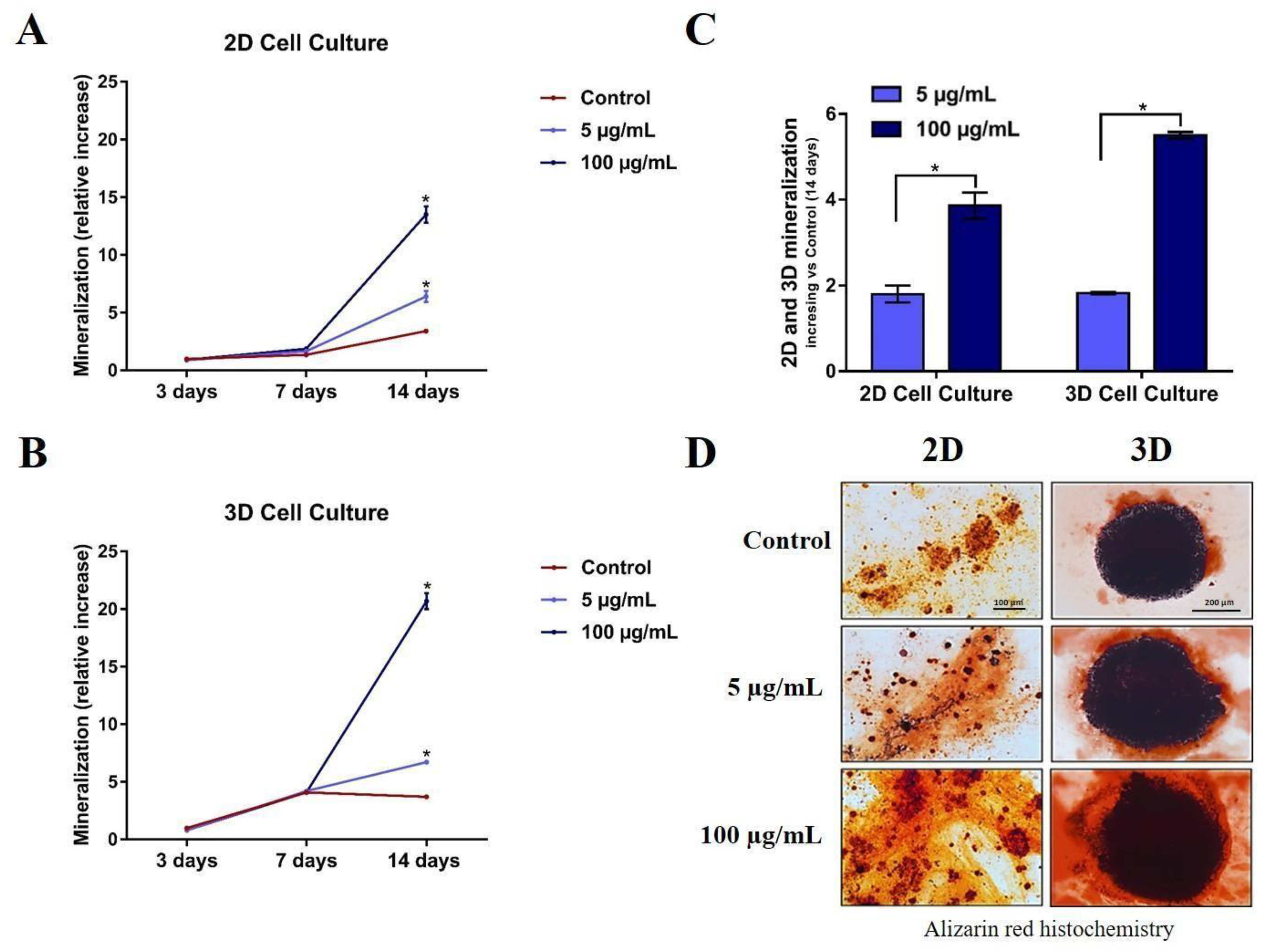
3.5. Differentiation and Mineralization of Human Osteoblasts after Exposure to TiO2 NPs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Awasthi, A.; Awasthi, K.K.; John, P.J. Nanomaterials in Biology. Environ. Sci. Pollut. Res. 2021, 28, 46334–46335. [Google Scholar] [CrossRef] [PubMed]
- Souza, W.; Piperni, S.G.; Laviola, P.; Rossi, A.L.; Rossi, M.I.D.; Archanjo, B.S.; Leite, P.E.; Fernandes, M.H.; Rocha, L.A.; Granjeiro, J.M.; et al. The Two Faces of Titanium Dioxide Nanoparticles Bio-Camouflage in 3D Bone Spheroids. Sci. Rep. 2019, 9, 9309. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Zhou, P.; Wang, L.; Hou, Y.; Zhang, X.; Zhu, S.; Guan, S. Investigation of Mg–XLi–Zn Alloys for Potential Application of Biodegradable Bone Implant Materials. J. Mater. Sci. Mater. Med. 2021, 32, 43. [Google Scholar] [CrossRef]
- Bayda, S.; Adeel, M.; Tuccinardi, T.; Cordani, M.; Rizzolio, F. The History of Nanoscience and Nanotechnology: From Chemical–Physical Applications to Nanomedicine. Molecules 2019, 25, 112. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, A.R.; Gemini-Piperni, S.; Travassos, R.; Lemgruber, L.; Silva, C.R.; Rossi, A.L.; Farina, M.; Anselme, K.; Shokuhfar, T.; Shahbazian-Yassar, R.; et al. Trojan-Like Internalization of Anatase Titanium Dioxide Nanoparticles by Human Osteoblast Cells. Sci. Rep. 2016, 6, 23615. [Google Scholar] [CrossRef]
- Delgado-Ruiz, R.; Romanos, G. Potential Causes of Titanium Particle and Ion Release in Implant Dentistry: A Systematic Review. Int. J. Mol. Sci. 2018, 19, 3585. [Google Scholar] [CrossRef]
- Kheder, W.; al Kawas, S.; Khalaf, K.; Samsudin, A.R. Impact of Tribocorrosion and Titanium Particles Release on Dental Implant Complications—A Narrative Review. Jpn. Dent. Sci. Rev. 2021, 57, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Kirmanidou, Y.; Sidira, M.; Drosou, M.-E.; Bennani, V.; Bakopoulou, A.; Tsouknidas, A.; Michailidis, N.; Michalakis, K. New Ti-Alloys and Surface Modifications to Improve the Mechanical Properties and the Biological Response to Orthopedic and Dental Implants: A Review. Biomed. Res. Int 2016, 2016, 2908570. [Google Scholar] [CrossRef] [PubMed]
- Amengual-Peñafiel, L.; Córdova, L.A.; Constanza Jara-Sepúlveda, M.; Brañes-Aroca, M.; Marchesani-Carrasco, F.; Cartes-Velásquez, R. Osteoimmunology Drives Dental Implant Osseointegration: A New Paradigm for Implant Dentistry. Jpn. Dent. Sci. Rev. 2021, 57, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.T.; Eo, M.Y.; Nguyen, T.T.H.; Kim, S.M. General Review of Titanium Toxicity. Int. J. Implant. Dent. 2019, 5, 10. [Google Scholar] [CrossRef]
- Romanos, G.; Fischer, G.; Delgado-Ruiz, R. Titanium Wear of Dental Implants from Placement, under Loading and Maintenance Protocols. Int. J. Mol. Sci. 2021, 22, 1067. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Shi, Q.; Wang, J.; Chen, X.; Hao, Y.; Zhang, Y.; Wang, X. The Unfavorable Role of Titanium Particles Released from Dental Implants. Nanotheranostics 2021, 5, 321–332. [Google Scholar] [CrossRef]
- Christo, S.N.; Diener, K.R.; Bachhuka, A.; Vasilev, K.; Hayball, J.D. Innate Immunity and Biomaterials at the Nexus: Friends or Foes. Biomed. Res. Int. 2015, 2015, 342304. [Google Scholar] [CrossRef] [PubMed]
- Goodman, S.B.; Davidson, J.A.; Song, Y.; Martial, N.; Fornasier, V.L. Histomorphological Reaction of Bone to Different Concentrations of Phagocytosable Particles of High-Density Polyethylene and Ti-6Al-4V Alloy in Vivo. Biomaterials 1996, 17, 1943–1947. [Google Scholar] [CrossRef] [PubMed]
- Bukata, S.V.; Gelinas, J.; Wei, X.; Rosier, R.N.; Puzas, J.E.; Zhang, X.; Schwarz, E.M.; Song, X.R.; Griswold, D.E.; O’Keefe, R.J. PGE2 and IL-6 Production by Fibroblasts in Response to Titanium Wear Debris Particles Is Mediated through a Cox-2 Dependent Pathway. J. Orthop. Res. 2004, 22, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.G.; Koh, H.S.; Kluess, D.; O’Connor, D.; Mathur, A.; Truskey, G.A.; Rubin, J.; Zhou, D.X.F.; Sung, K.-L.P. Effects of Titanium Particle Size on Osteoblast Functions in Vitro and in Vivo. Proc. Natl. Acad. Sci. USA 2005, 102, 4578–4583. [Google Scholar] [CrossRef]
- Tuan, R.S.; Lee, F.Y.-I.; Konttinen, Y.T.; Wilkinson, M.J.; Smith, R.L. What Are the Local and Systemic Biologic Reactions and Mediators to Wear Debris, and What Host Factors Determine or Modulate the Biologic Response to Wear Particles? J. Am. Acad. Orthop. Surg. 2008, 16, S42–S48. [Google Scholar] [CrossRef]
- Gutwein, L.G.; Webster, T.J. Increased Viable Osteoblast Density in the Presence of Nanophase Compared to Conventional Alumina and Titania Particles. Biomaterials 2004, 25, 4175–4183. [Google Scholar] [CrossRef]
- Neel, A.; Bozec, L.; Perez, R.A.; Kim, H.-W.; Knowles, J.C. Nanotechnology in Dentistry: Prevention, Diagnosis, and Therapy. Int. J. Nanomed. 2015, 10, 6371. [Google Scholar] [CrossRef]
- Bédard, P.; Gauvin, S.; Ferland, K.; Caneparo, C.; Pellerin, È.; Chabaud, S.; Bolduc, S. Innovative Human Three-Dimensional Tissue-Engineered Models as an Alternative to Animal Testing. Bioengineering 2020, 7, 115. [Google Scholar] [CrossRef]
- Yanagi, T.; Kajiya, H.; Fujisaki, S.; Maeshiba, M.; Yanagi-S, A.; Yamamoto-M, N.; Kakura, K.; Kido, H.; Ohno, J. Three-Dimensional Spheroids of Dedifferentiated Fat Cells Enhance Bone Regeneration. Regen. Ther. 2021, 18, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Gaitán-Salvatella, I.; López-Villegas, E.O.; González-Alva, P.; Susate-Olmos, F.; Álvarez-Pérez, M.A. Case Report: Formation of 3D Osteoblast Spheroid Under Magnetic Levitation for Bone Tissue Engineering. Front. Mol. Biosci. 2021, 8, 672518. [Google Scholar] [CrossRef] [PubMed]
- Schoichet, J.J.; Mourão, C.F.d.A.B.; Fonseca, E.d.M.; Ramirez, C.; Villas-Boas, R.; Prazeres, J.; Quinelato, V.; Aguiar, T.R.; Prado, M.; Cardarelli, A.; et al. Epidermal Growth Factor Is Associated with Loss of Mucosae Sealing and Peri-Implant Mucositis: A Pilot Study. Healthcare 2021, 9, 1277. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G. Current Concepts in the Use of Lasers in Periodontal and Implant Dentistry. J. Indian Soc. Periodontol. 2015, 19, 490. [Google Scholar] [CrossRef] [PubMed]
- Gebhard, C.; Gabriel, C.; Walter, I. Morphological and Immunohistochemical Characterization of Canine Osteosarcoma Spheroid Cell Cultures. Anat. Histol. Embryol. 2016, 45, 219–230. [Google Scholar] [CrossRef]
- Keller, L.; Idoux-Gillet, Y.; Wagner, Q.; Eap, S.; Brasse, D.; Schwinté, P.; Arruebo, M.; Benkirane-Jessel, N. Nanoengineered Implant as a New Platform for Regenerative Nanomedicine Using 3D Well-Organized Human Cell Spheroids. Int. J. Nanomed. 2017, 12, 447–457. [Google Scholar] [CrossRef] [PubMed]
- Maia-Pinto, M.O.C.; Brochado, A.C.B.; Teixeira, B.N.; Sartoretto, S.C.; Uzeda, M.J.; Alves, A.T.N.N.; Alves, G.G.; Calasans-Maia, M.D.; Thiré, R.M.S.M. Biomimetic Mineralization on 3D Printed PLA Scaffolds: On the Response of Human Primary Osteoblasts Spheroids and In Vivo Implantation. Polymers 2020, 13, 74. [Google Scholar] [CrossRef]
- Jensen, C.; Teng, Y. Is It Time to Start Transitioning From 2D to 3D Cell Culture? Front. Mol. Biosci. 2020, 7, 33. [Google Scholar] [CrossRef]
- Duval, K.; Grover, H.; Han, L.-H.; Mou, Y.; Pegoraro, A.F.; Fredberg, J.; Chen, Z. Modeling Physiological Events in 2D vs. 3D Cell Culture. Physiology 2017, 32, 266–277. [Google Scholar] [CrossRef]
- Białkowska, K.; Komorowski, P.; Bryszewska, M.; Miłowska, K. Spheroids as a Type of Three-Dimensional Cell Cultures—Examples of Methods of Preparation and the Most Important Application. Int. J. Mol. Sci. 2020, 21, 6225. [Google Scholar] [CrossRef]
- Holub, A.R.; Huo, A.; Patel, K.; Thakore, V.; Chhibber, P.; Erogbogbo, F. Assessing Advantages and Drawbacks of Rapidly Generated Ultra-Large 3D Breast Cancer Spheroids: Studies with Chemotherapeutics and Nanoparticles. Int. J. Mol. Sci. 2020, 21, 4413. [Google Scholar] [CrossRef] [PubMed]
- Anada, T.; Fukuda, J.; Sai, Y.; Suzuki, O. An Oxygen-Permeable Spheroid Culture System for the Prevention of Central Hypoxia and Necrosis of Spheroids. Biomaterials 2012, 33, 8430–8441. [Google Scholar] [CrossRef] [PubMed]
- Yuste, I.; Luciano, F.C.; González-Burgos, E.; Lalatsa, A.; Serrano, D.R. Mimicking Bone Microenvironment: 2D and 3D in Vitro Models of Human Osteoblasts. Pharmacol. Res. 2021, 169, 105626. [Google Scholar] [CrossRef] [PubMed]
- Sawa, N.; Fujimoto, H.; Sawa, Y.; Yamashita, J. Alternating Differentiation and Dedifferentiation between Mature Osteoblasts and Osteocytes. Sci. Rep. 2019, 9, 13842. [Google Scholar] [CrossRef]
- Buzea, C.; Pacheco, I.I.; Robbie, K. Nanomaterials and Nanoparticles: Sources and Toxicity. Biointerphases 2007, 2, MR17–MR71. [Google Scholar] [CrossRef] [PubMed]
- Corbo, C.; Molinaro, R.; Parodi, A.; Toledano Furman, N.E.; Salvatore, F.; Tasciotti, E. The Impact of Nanoparticle Protein Corona on Cytotoxicity, Immunotoxicity and Target Drug Delivery. Nanomedicine 2016, 11, 81–100. [Google Scholar] [CrossRef]
- Arora, S.; Rajwade, J.M.; Paknikar, K.M. Nanotoxicology and in Vitro Studies: The Need of the Hour. Toxicol. Appl. Pharmacol. 2012, 258, 151–165. [Google Scholar] [CrossRef]
- Ribeiro, A.R.; Mukherjee, A.; Hu, X.; Shafien, S.; Ghodsi, R.; He, K.; Gemini-Piperni, S.; Wang, C.; Klie, R.F.; Shokuhfar, T.; et al. Bio-Camouflage of Anatase Nanoparticles Explored by in Situ High-Resolution Electron Microscopy. Nanoscale 2017, 9, 10684–10693. [Google Scholar] [CrossRef]
- Gurumurthy, B.; Bierdeman, P.C.; Janorkar, A.V. Spheroid Model for Functional Osteogenic Evaluation of Human Adipose Derived Stem Cells. J. Biomed. Mater. Res. A 2017, 105, 1230–1236. [Google Scholar] [CrossRef]
- Yamada, Y.; Okano, T.; Orita, K.; Makino, T.; Shima, F.; Nakamura, H. 3D-Cultured Small Size Adipose-Derived Stem Cell Spheroids Promote Bone Regeneration in the Critical-Sized Bone Defect Rat Model. Biochem. Biophys. Res. Commun. 2022, 603, 57–62. [Google Scholar] [CrossRef]
- Ho, S.S.; Murphy, K.C.; Binder, B.Y.K.; Vissers, C.B.; Leach, J.K. Increased Survival and Function of Mesenchymal Stem Cell Spheroids Entrapped in Instructive Alginate Hydrogels. Stem Cells Transl Med. 2016, 5, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Cuevas-González, M.V.; Suaste-Olmos, F.; Cuevas-González, J.C.; Álvarez-Pérez, M.A. 3D Spheroid Cell Cultures and Their Role in Bone Regeneration: A Systematic Review. Odovtos Int. J. Dent. Sci. 2022, 24, 44–57. [Google Scholar] [CrossRef]
- Lee, H.-J.; Song, Y.-M.; Baek, S.; Park, Y.-H.; Park, J.-B. Vitamin D Enhanced the Osteogenic Differentiation of Cell Spheroids Composed of Bone Marrow Stem Cells. Medicina 2021, 57, 1271. [Google Scholar] [CrossRef] [PubMed]
- Rocha, A.L.; Bighetti-Trevisan, R.L.; Duffles, L.F.; de Arruda, J.A.A.; Taira, T.M.; Assis, B.R.D.; Macari, S.; Diniz, I.M.A.; Beloti, M.M.; Rosa, A.L.; et al. Inhibitory Effects of Dabigatran Etexilate, a Direct Thrombin Inhibitor, on Osteoclasts and Osteoblasts. Thromb. Res. 2020, 186, 45–53. [Google Scholar] [CrossRef]
- Daly, A.C.; Davidson, M.D.; Burdick, J.A. 3D Bioprinting of High Cell-Density Heterogeneous Tissue Models through Spheroid Fusion within Self-Healing Hydrogels. Nat. Commun. 2021, 12, 753. [Google Scholar] [CrossRef]
- Kim, J. bin Three-Dimensional Tissue Culture Models in Cancer Biology. Semin Cancer Biol. 2005, 15, 365–377. [Google Scholar] [CrossRef]
- Chatzinikolaidou, M. Cell Spheroids: The New Frontiers in in Vitro Models for Cancer Drug Validation. Drug Discov. Today 2016, 21, 1553–1560. [Google Scholar] [CrossRef]
- Senna, P.; Antoninha Del Bel Cury, A.; Kates, S.; Meirelles, L. Surface Damage on Dental Implants with Release of Loose Particles after Insertion into Bone. Clin. Implant. Dent. Relat. Res. 2015, 17, 681–692. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Souza Castro, G.; de Souza, W.; Lima, T.S.M.; Bonfim, D.C.; Werckmann, J.; Archanjo, B.S.; Granjeiro, J.M.; Ribeiro, A.R.; Gemini-Piperni, S. The Effects of Titanium Dioxide Nanoparticles on Osteoblasts Mineralization: A Comparison between 2D and 3D Cell Culture Models. Nanomaterials 2023, 13, 425. https://doi.org/10.3390/nano13030425
de Souza Castro G, de Souza W, Lima TSM, Bonfim DC, Werckmann J, Archanjo BS, Granjeiro JM, Ribeiro AR, Gemini-Piperni S. The Effects of Titanium Dioxide Nanoparticles on Osteoblasts Mineralization: A Comparison between 2D and 3D Cell Culture Models. Nanomaterials. 2023; 13(3):425. https://doi.org/10.3390/nano13030425
Chicago/Turabian Stylede Souza Castro, Gabriela, Wanderson de Souza, Thais Suelen Mello Lima, Danielle Cabral Bonfim, Jacques Werckmann, Braulio Soares Archanjo, José Mauro Granjeiro, Ana Rosa Ribeiro, and Sara Gemini-Piperni. 2023. "The Effects of Titanium Dioxide Nanoparticles on Osteoblasts Mineralization: A Comparison between 2D and 3D Cell Culture Models" Nanomaterials 13, no. 3: 425. https://doi.org/10.3390/nano13030425
APA Stylede Souza Castro, G., de Souza, W., Lima, T. S. M., Bonfim, D. C., Werckmann, J., Archanjo, B. S., Granjeiro, J. M., Ribeiro, A. R., & Gemini-Piperni, S. (2023). The Effects of Titanium Dioxide Nanoparticles on Osteoblasts Mineralization: A Comparison between 2D and 3D Cell Culture Models. Nanomaterials, 13(3), 425. https://doi.org/10.3390/nano13030425







