Porous Platinum Black-Coated Minimally Invasive Microneedles for Non-Enzymatic Continuous Glucose Monitoring in Interstitial Fluid
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents and Apparatus
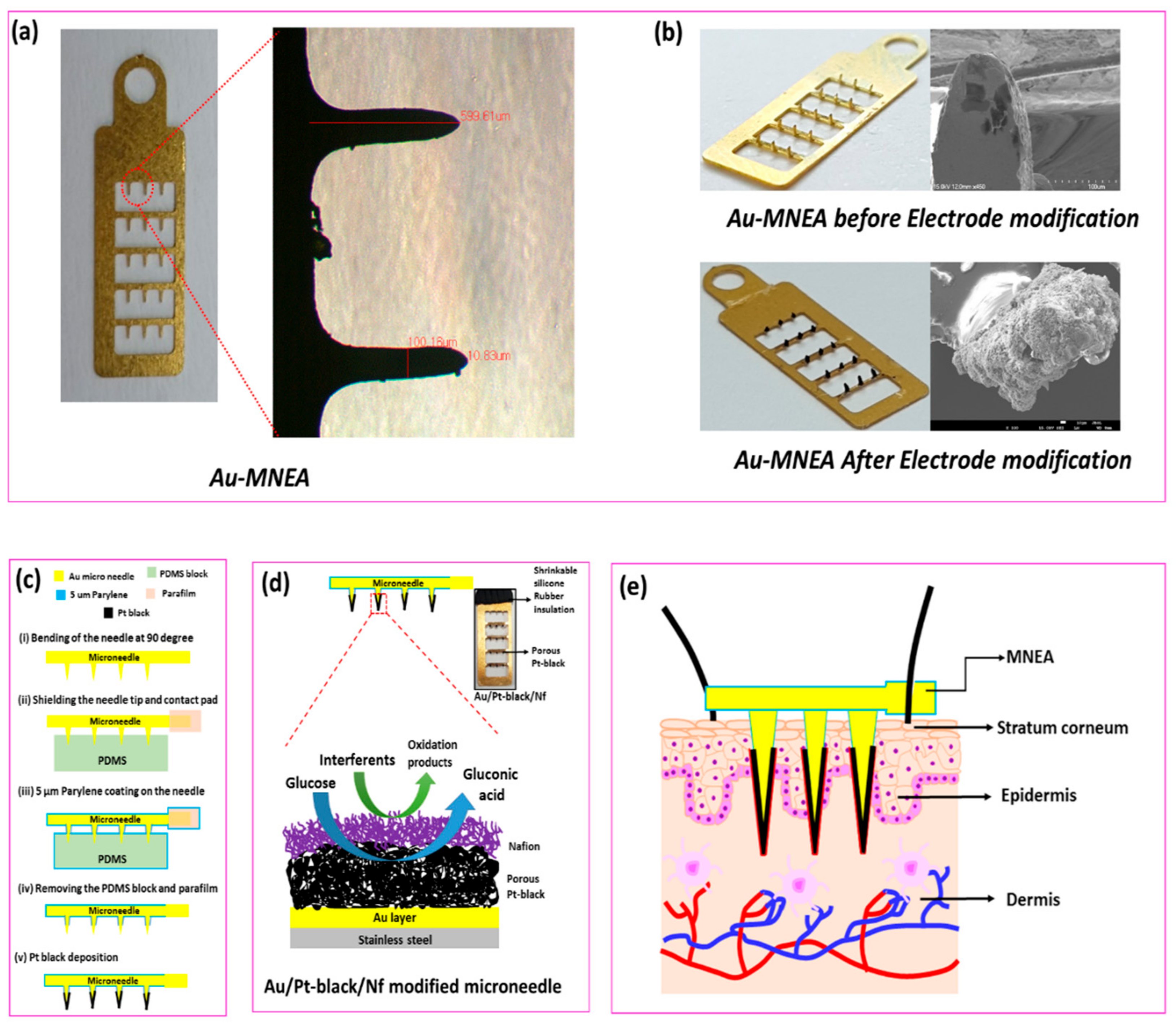
2.2. Fabrication of Au-MNEAs
2.3. Electrodeposition and Packaging of MNs
2.4. Electrochemical Measurements
2.5. Preparation of ISF
3. Results and Discussion
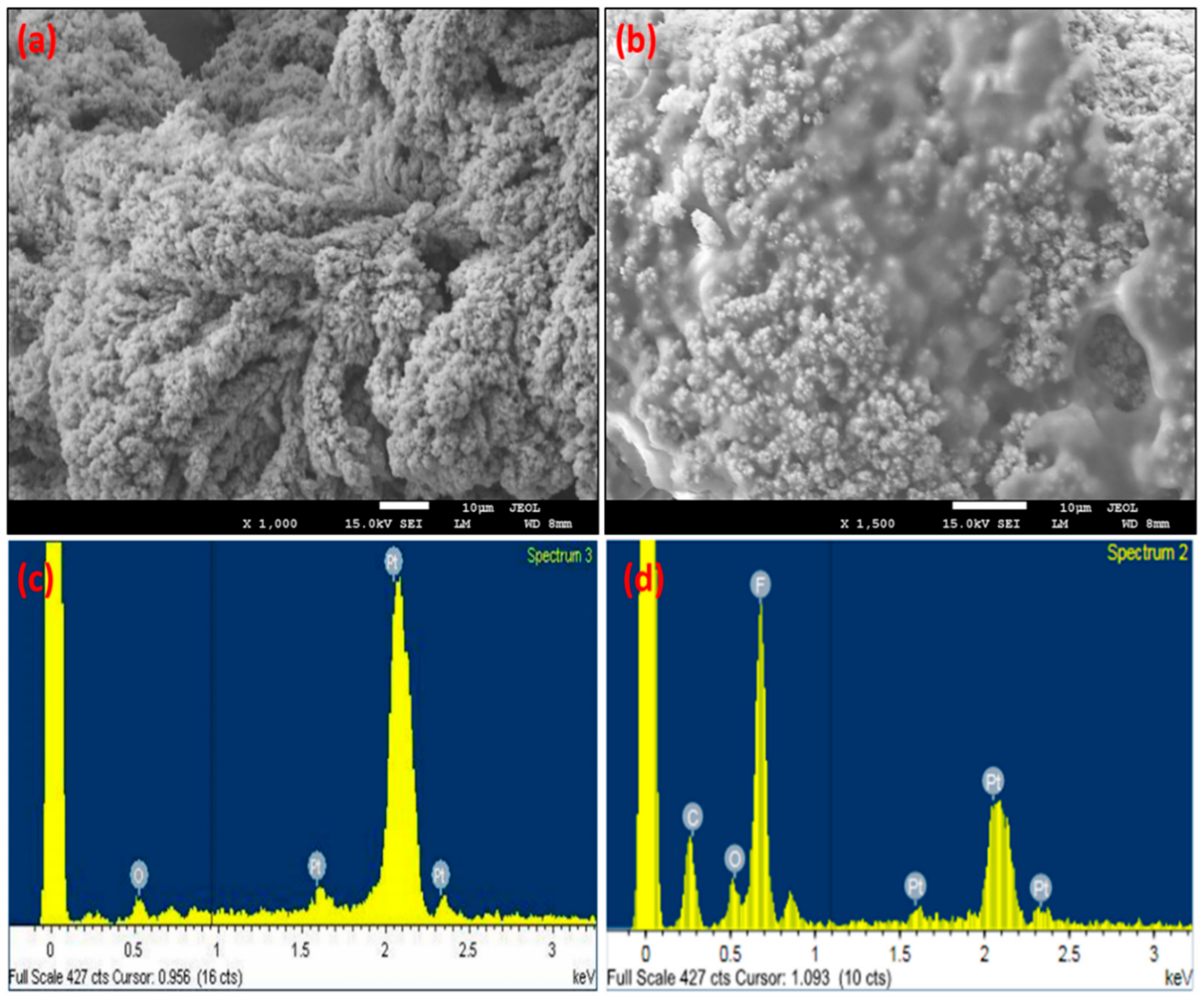
3.1. Surface Characteristics of MNEAs
SEM/EDX
3.2. Electrochemical Characterization of the MNEAs
3.2.1. EIS
3.2.2. Cyclic Voltammetry
3.2.3. Electrocatalysis of Glucose at the Modified Electrode
3.2.4. Scan Rate Study
3.3. Effects of the Electrode Array Size and Electrodeposition Time
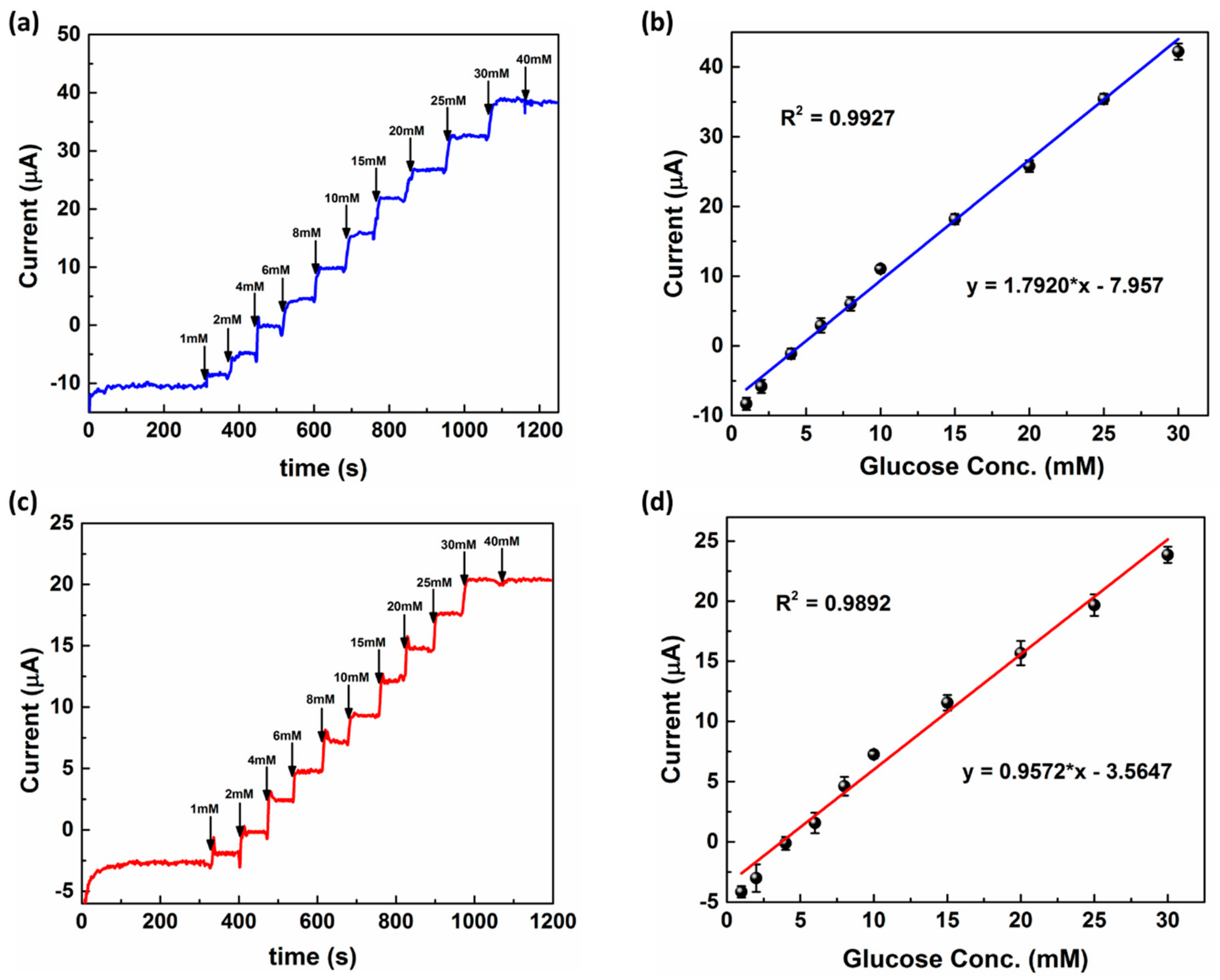
3.4. Response Studies of Modified MNEAs in PBS and ISF
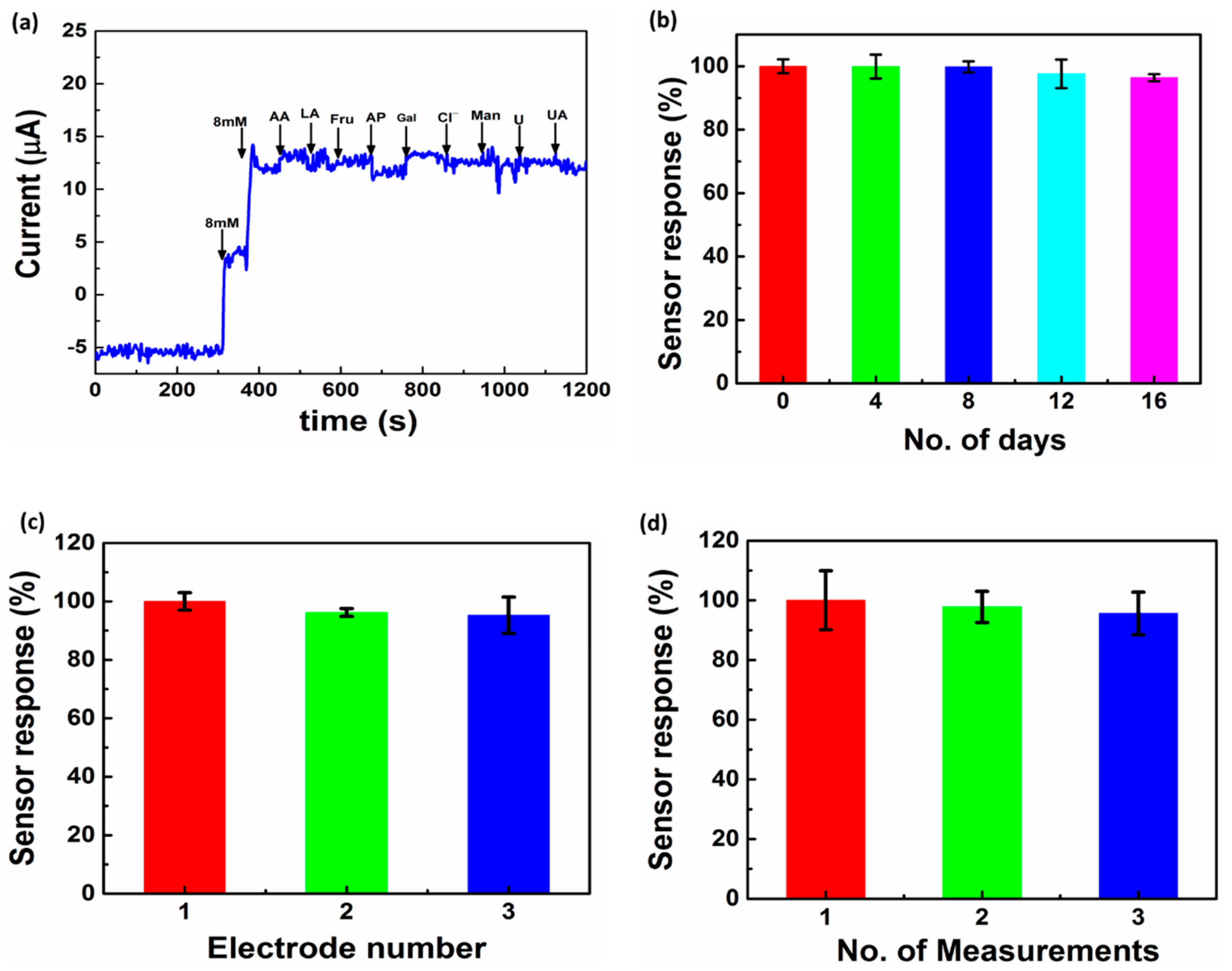
3.5. Stability, Precision, and Interference Study
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ventrelli, L.; Strambini, L.M.; Barillaro, G. Microneedles for Transdermal Biosensing: Current Picture and Future Direction. Adv. Healthc. Mater. 2015, 4, 2606–2640. [Google Scholar] [CrossRef] [PubMed]
- Chua, B.; Desai, S.P.; Tierney, M.J.; Tamada, J.A.; Jina, A.N. Effect of microneedles shape on skin penetration and minimally invasive continuous glucose monitoring in vivo. Sens. Actuators A Phys. 2013, 203, 373–381. [Google Scholar] [CrossRef]
- Chinnadayyala, S.R.; Park, K.D.; Cho, S. Review—In Vivo and In Vitro Microneedle Based Enzymatic and Non-Enzymatic Continuous Glucose Monitoring Biosensors. ECS J. Solid State Sci. Technol. 2018, 7, 3159–3171. [Google Scholar] [CrossRef]
- Hwa, K.-Y.; Subramani, B.; Chang, P.-W.; Chien, M.; Huang, J.-T. Transdermal Microneedle Array-based Sensor for Real Time Continuous Glucose Monitoring. Int. J. Electrochem. Sci. 2015, 10, 2455–2466. [Google Scholar]
- Adeel, M.; Rahman, M.M.; Caligiuri, I.; Canzonieri, V.; Rizzolio, F.; Daniele, S. Recent advances of electrochemical and optical enzyme-free glucose sensors operating at physiological conditions. Biosens. Bioelectron. 2020, 165, 112331. [Google Scholar] [CrossRef]
- Park, S.; Park, S.; Jeong, R.-A.; Boo, H.; Park, J.; Chan, H.K.; Chung, T.D. Nonenzymatic continuous glucose monitoring in human whole blood using electrified nanoporous Pt. Biosens. Bioelectron. 2012, 31, 284–291. [Google Scholar] [CrossRef]
- Ribet, F.; Stemme, G.; Roxhed, N. Real-time intradermal continuous glucose monitoring using a minimally invasive microneedle-based system. Biomed. Microdevices 2018, 20, 101. [Google Scholar] [CrossRef]
- Cengiz, E.; Tamborlane, W.V. A Tale of Two Compartments: Interstitial Versus Blood Glucose Monitoring. Diabetes Technol. Ther. 2009, 11, 11–16. [Google Scholar] [CrossRef]
- Sharma, S.; El-Laboudi, A.; Reddy, M.; Jugnee, N.; Sivasubramaniyam, S.; Sharkawy, M.E.; Georgiou, P.; Johnston, D.; Oliver, N.; Cass, A.E.G. A pilot study in humans of microneedle sensor arrays for continuous glucose monitoring. Anal. Methods 2018, 10, 2088–2095. [Google Scholar] [CrossRef]
- Hwang, K.; Kim, H.; Kim, D.J. Thickness of skin and subcutaneous tissue of the free flap donor sites: A histologic study. Microsurgery 2016, 36, 54. [Google Scholar] [CrossRef] [PubMed]
- Barrett, C.; Dawson, K.; Mahony, C.O.; Riordan, A.O. Development of low cost rapid fabrication of sharp polymer microneedles for in vivo glucose biosensing applications. ECS J. Solid State Sci. Technol. 2015, 4, 3053–3058. [Google Scholar] [CrossRef]
- Miller, P.; Moorman, M.; Manginell, R.; Ashlee, C.; Brener, I.; Wheeler, D.; Narayan, R.; Polsky, R. Towards an integrated microneedle total analysis chip for protein detection. Electroanalysis 2016, 28, 1305. [Google Scholar] [CrossRef]
- Miller, P.R.; Narayan, R.J.; Polsky, R. Microneedle-based sensors for medical diagnosis. J. Mater. Chem. B 2016, 4, 1379. [Google Scholar] [CrossRef] [PubMed]
- Goud, K.Y.; Moonla, C.; Mishra, R.K.; Yu, C.; Narayan, R.; Litvan, I.; Wang, J. Wearable electrochemical microneedle sensor for continuous monitoring of levodopa: Toward parkinson management. ACS Sens. 2019, 4, 2196–2204. [Google Scholar] [CrossRef]
- Windmiller, J.R.; Zhou, N.; Chuang, M.C.; Valdes-Ramirez, G.; Santhosh, P.; Miller, P.R.; Narayan, R.; Wang, J. Microneedle array-based carbon paste amperometric sensors and biosensors. Analyst 2011, 136, 1846–1851. [Google Scholar] [CrossRef] [PubMed]
- Windmiller, J.R.; Valds-Ramrez, G.; Zhou, N.; Zhou, M.; Miller, P.R.; Jin, C.; Brozik, S.M.; Polsky, R.; Katz, E.; Narayan, R.; et al. Biocomponent microneedle array biosensor for minimally-invasive glutamate monitoring. Electroanalysis 2011, 23, 2302–2309. [Google Scholar] [CrossRef]
- Li, C.G.; Joung, H.-A.; Noh, H.; Song, M.-B.; Kim, M.-G.; Jung, H. One-touch-activated blood multidiagnostic system using a minimally invasive hollow microneedle integrated with a paper-based sensor. Lab. Chip. 2015, 15, 3286–3292. [Google Scholar] [CrossRef] [PubMed]
- Bollella, P.; Gorton, L. Enzyme based amperometric biosensors. Curr. Opin. Electrochem. 2018, 10, 157–173. [Google Scholar] [CrossRef]
- Teymourian, H.; Moonla, C.; Tehrani, F.; Vargas, E.; Aghavali, R.; Barfidokht, A.; Tangkuaram, T.; Mercier, P.P.; Dassau, E.; Wang, J. Microneedle-Based Detection of Ketone Bodies along with Glucose and Lactate: Toward Real-Time Continuous Interstitial Fluid Monitoring of Diabetic Ketosis and Ketoacidosis. Anal. Chem. 2020, 92, 2291–2300. [Google Scholar] [CrossRef] [PubMed]
- Calio, A.; Dardano, P.; Palma, V.D.; Bevilacqua, M.; Matteo, A.D.; Iuele, H.; De Stefano, L. Polymeric microneedles based enzymatic electrodes for electrochemical biosensing of glucose and lactic acid. Sens. Actuators B Chem. 2016, 236, 343–349. [Google Scholar] [CrossRef]
- Chinnadayyala, S.R.; Park, I.; Cho, S. Nonenzymatic determination of glucose at near neutral pH values based on the use of nafion and platinum black coated microneedle electrode array. Microchim. Acta 2018, 185, 250. [Google Scholar] [CrossRef] [PubMed]
- McGarraugh, G. The chemistry of commercial continuous glucose monitors. Diabetes Technol. Ther. 2009, 11, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Das, P.; Das, M.; Chinnadayyala, S.R.; Singha, I.M.; Goswami, P. Recent advances on developing 3rd generation enzyme electrode for biosensor applications. Biosens. Bioelectron. 2016, 79, 386–397. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.; Turner, A.P.F. Glucose oxidase: An ideal enzyme. Biosens. Bioelectron. 1992, 7, 165–185. [Google Scholar] [CrossRef]
- Ju, J.; Hsieh, C.; Tian, Y.; Kang, J.; Chia, R.; Chang, H.; Bai, Y.; Xu, C.; Wang, X.; Liu, Q. Surface Enhanced Raman Spectroscopy based Biosensor with a Microneedle Array for Minimally Invasive In Vivo Glucose Measurements. ACS Sens. 2020, 5, 1777–1785. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.J.; Yoon, H.S.; Xuan, X.; Park, J.Y.; Paik, S.J.; Allen, M.G. A patch type non-enzymatic biosensor based on 3D SUS micro-needle electrode array for minimally invasive continuous glucose monitoring. Sens. Actuators B Chem. 2016, 222, 1144–1151. [Google Scholar] [CrossRef]
- Lee, Y.J.; Park, D.J.; Park, J.Y. Fully packaged nonenzymatic glucose microsensors with nanoporous platinum electrodes for anti-fouling. IEEE Sens. 2008, 8, 1922–1927. [Google Scholar] [CrossRef]
- Chinnadayyala, S.R.; Santhosh, M.; Singh, N.K.; Goswami, P. Alcohol oxidase protein mediated in-situ synthesized and stabilized gold nanoparticles for developing amperometric alcohol biosensor. Biosens. Bioelectron. 2015, 69, 155–161. [Google Scholar] [CrossRef]
- Saitou, M. Electrochemical characterization of platinum black electrodeposited from electrolyte including lead acetate trihydrate. Surf. Coat. Tech. 2006, 201, 3611–3614. [Google Scholar] [CrossRef]
- Feltham, A.M.; Spiro, M. Platinized platinum electrodes. Chem. Rev. 1971, 71, 177–193. [Google Scholar] [CrossRef]
- Chinnadayyala, S.R.; Park, J.; Kim, Y.H.; Choi, S.H.; Lee, S.-M.; Cho, W.W.; Lee, G.-Y.; Pyun, J.-C.; Cho, S. Electrochemical Detection of C-Reactive Protein in Human Serum Based on Self-Assembled Monolayer-Modified Interdigitated Wave-Shaped Electrode. Sensors 2019, 19, 5560. [Google Scholar] [CrossRef] [PubMed]
- Elliott, J.M.; Birkin, P.R.; Bartlett, P.N.; Attard, G.S. Platinum Microelectrodes with Unique High Surface Areas. Langmuir 1999, 15, 7411–7415. [Google Scholar] [CrossRef]
- Daniele, S.; Battistel, D.; Bergamin, S.; Bragato, C. Voltammetric Determination of Glucose at Bismuth-Modified Mesoporous Platinum Microelectrodes. Electroanalysis 2010, 22, 1511–1518. [Google Scholar] [CrossRef]
- Kim, J.; Kim, D.; Choi, S.Y.; Kim, S.-D.; Song, J.Y.; Kim, J. Electrochemical deposition of flat Nanoporous Pt layers with small pore dimensions. Electrochim. Acta 2016, 189, 196–204. [Google Scholar] [CrossRef]
- Toghill, K.E.; Compton, R.G. Electrochemical Non-Enzymatic Glucose Sensors: A Perspective and an Evaluation. Int. J. Electrochem. Sci. 2010, 5, 1246–1301. [Google Scholar]
- Wang, G.; He, X.; Wang, L.; Gu, A.; Huang, Y.; Fang, B.; Geng, B.; Zhang, X. Non-enzymatic electrochemical sensing of glucose. Microchim. Acta 2013, 180, 161–186. [Google Scholar] [CrossRef]
- Park, S.; Boo, H.; Chung, T.D. Electrochemical non-enzymatic glucose sensors. Anal. Chim. Acta 2006, 556, 46–57. [Google Scholar] [CrossRef]
- Dhara, K.; Mahapatra, D.R. Electrochemical nonenzymatic sensing of glucose using advanced nanomaterials. Microchim. Acta 2018, 185, 49. [Google Scholar] [CrossRef]
- Tian, H.; Jia, M.; Zhang, M.; Hu, J. Nonenzymatic glucose sensor based on nickel ion implanted-modified indium tin oxide electrode. Electrochim. Acta 2013, 96, 285–290. [Google Scholar] [CrossRef]
- Chinnadayyala, S.R.; Kakoti, A.; Santhosh, M.; Singh, N.K.; Goswami, P. A novel amperometric alcohol biosensor developed in a 3rd generation bioelectrode platform using peroxidase coupled ferrocene activated alcohol oxidase as biorecognition system. Biosens. Bioelectron. 2014, 55, 120–126. [Google Scholar] [CrossRef]
- Bilal, S.; Ullah, W.; Shah, A.H.A. Polyaniline@CuNi nanocomposite: A highly selective, stable and efficient electrode material for binder free non-enzymatic glucose sensor. Electrochim. Acta 2018, 284, 382–391. [Google Scholar] [CrossRef]
- Ryu, J.; Kim, K.; Kim, H.S.; Hahn, H.T.; Lashmore, D. Intense pulsed light induced platinum–gold alloy formation on carbon nanotubes for non-enzymatic glucose detection. Biosens. Bioelectron. 2010, 26, 602–607. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Zheng, B.; Jiang, Y.; Cai, Y.; Du, J.; Yuan, H.; Xiao, D. Improvement of sensitive CuO NFs–ITO nonenzymatic glucose sensor based on in situ electrospun fiber. Talanta 2012, 101, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Park, J.Y. A coral-like macroporous gold–platinum hybrid 3D electrode for enzyme-free glucose detection. Sens. Actuators B 2011, 155, 134–139. [Google Scholar] [CrossRef]
- Yuan, J.; Wang, K.; Xia, X. Highly Ordered Platinum-Nanotubule Arrays for Amperometric Glucose Sensing. Adv. Funct. Mater. 2005, 15, 803–809. [Google Scholar] [CrossRef]
- Yang, J.; Liang, X.; Cui, L.; Liu, H.; Xie, J.; Liu, W. A novel non-enzymatic glucose sensor based on Pt3Ru1 alloy nanoparticles with high density of surface defects. Biosens. Bioelectron. 2016, 80, 171–174. [Google Scholar] [CrossRef]
- Badhulika, S.; Paul, R.K.; Terse, R.T.; Mulchandani, A. Nonenzymatic glucose sensor based on platinum nanoflowers decorated multiwalled carbon nanotubes-graphene hybrid electrode. Electroanalysis 2014, 26, 103–108. [Google Scholar] [CrossRef]
- Chang, G.; Shu, H.; Huang, Q.; Oyama, M.; Ji, K.; Liu, X.; He, Y. Synthesis of highly dispersed Pt nanoclusters anchored graphene composites and their application for non-enzymatic glucose sensing. Electrochim. Acta 2015, 157, 149–157. [Google Scholar] [CrossRef]
- Wu, G.; Song, X.; Wu, Y.; Chen, X.; Luo, F.; Chen, X. Non-enzymatic electrochemical glucose sensor based on platinum nanoflowers supported on graphene oxide. Talanta 2013, 105, 379–385. [Google Scholar] [CrossRef]
- Rathod, D.; Dickinson, C.; Egan, D.; Dempsey, E. Platinum nanoparticle decoration of carbon materials with applications in non-enzymatic glucose sensing. Sens. Actuators B 2010, 143, 547–554. [Google Scholar] [CrossRef]
- Joo, S.; Park, S.; Chung, T.D.; Kim, H.C. Integration of a Nanoporous Platinum Thin Film into a Microfluidic System for Non-enzymatic Electrochemical Glucose Sensing. Anal. Sci. 2007, 23, 277–281. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Wang, C.; Chen, W.; Chen, Y.; Zhang, J.X. PVDF-Nafion nanomembranes coated microneedles for in vivo transcutaneous implantable glucose sensing. Biosens. Bioelectron. 2015, 74, 1047–1052. [Google Scholar] [CrossRef] [PubMed]



| Electrode | RS (Ω) | Constant Phase Element (CPE) | Chi Square | |
|---|---|---|---|---|
| T(×10−5 Ω−1·sP) | P | |||
| No parylene | 29.15 | 2.6155 | 0.8141 | 0.0534 |
| Parylene | 44.65 | 7.6058 | 0.8442 | 0.0743 |
| Au/Pt-black | 36.31 | 156.15 | 0.9290 | 0.0330 |
| Au/Pt-black/Nf | 42.52 | 74.244 | 0.8024 | 0.0107 |
| Electrode Configuration | Sensitivity (µA mM−1 cm−2) | Dynamic Range (mM) | Detection Limit (µM) | Reference |
|---|---|---|---|---|
| PANI@CuNi/GC | 1030 | 0.1–5.6 | 0.2 | [41] |
| Pt-Au/MWCNT | 10.71 | 0.04–24.4 | 10.0 | [42] |
| CuO NFs–ITO | 873 | 0.2–1.3 | 0.04 | [43] |
| Macroporous Au-Pt | 25 | 1.0–20.0 | 25.0 | [44] |
| Pt NTAEs | 0.1 | 2.0–14.0 | 1.0 | [45] |
| Pt3Ru1/GCE | 31.3 | 0.005–10.0 | 0.3 | [46] |
| Pt/MWNTs/graphene | 11.06 | 1.0–7.0 | 387.0 | [47] |
| PtNCs/graphene | 1.21 | 1.0–25.0 | 1.0 | [48] |
| PtNFs/GO | 1.26 | 0.002–10.3 | 2.0 | [49] |
| Pt/MWCNT | 1.10 | 2.0–20.0 | N.R | [50] |
| Nanoporous Pt | 1.65 | 1.0–10.0 | 97.0 | [51] |
| Au/Pt-black/Nf | 1.792 ± 0.25 | 1.0–30.0 | 7.2 | This work (PBS) |
| Au/Pt-black/Nf | 0.957 ± 0.14 | 1.0–30.0 | 22.0 | This work (ISF) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chinnadayyala, S.R.; Cho, S. Porous Platinum Black-Coated Minimally Invasive Microneedles for Non-Enzymatic Continuous Glucose Monitoring in Interstitial Fluid. Nanomaterials 2021, 11, 37. https://doi.org/10.3390/nano11010037
Chinnadayyala SR, Cho S. Porous Platinum Black-Coated Minimally Invasive Microneedles for Non-Enzymatic Continuous Glucose Monitoring in Interstitial Fluid. Nanomaterials. 2021; 11(1):37. https://doi.org/10.3390/nano11010037
Chicago/Turabian StyleChinnadayyala, Somasekhar R., and Sungbo Cho. 2021. "Porous Platinum Black-Coated Minimally Invasive Microneedles for Non-Enzymatic Continuous Glucose Monitoring in Interstitial Fluid" Nanomaterials 11, no. 1: 37. https://doi.org/10.3390/nano11010037
APA StyleChinnadayyala, S. R., & Cho, S. (2021). Porous Platinum Black-Coated Minimally Invasive Microneedles for Non-Enzymatic Continuous Glucose Monitoring in Interstitial Fluid. Nanomaterials, 11(1), 37. https://doi.org/10.3390/nano11010037






