Abstract
Implant abutments serve as the critical interface between dental implants and prosthodontic restorations, playing a central role in the functional and aesthetic success of implant-supported rehabilitations. With the development of CAD/CAM technologies, dental implantology has experienced a significant transformation. The latest and still unexplored field of science includes an advanced algorithm-driven process known as generative design. Generally, generative design is used to investigate a broad spectrum of design alternatives that satisfy predetermined criteria established by a designer. Prior to the application of generative design, it is essential to define the key parameters that influence the optimization of the designed object’s configuration, such as a hybrid implant abutment. A bibliographic search was performed using PubMed and Scopus databases to identify relevant studies published up to 1 July 2025. Studies that investigated transmucosal and prosthodontic height of implant abutments were selected for inclusion. Only 13 studies met inclusion criteria and were further analyzed. Included studies showed the importance of transmucosal and prosthodontic height of implant abutments in order to reduce possible complications. The review highlights the importance of optimizing the transmucosal and transgingival heights of implant abutments. For predictable biological and mechanical outcomes, both dimensions should be at least 2 mm. The obtained parameter values will be used to create the initial parametric model, which will then be utilized in the generative design process of hybrid implant abutments.
1. Introduction
The rapid advancement of digital technologies has significantly transformed diagnostics, treatment planning, and therapeutic procedures in dental medicine, most notably in the areas of implantology and implant prosthodontics. These innovations have introduced a broad range of new concepts, approaches, and workflows aimed to enhance clinical predictability and procedural efficiency while also minimizing the likelihood of complications [1,2,3,4]. Dental implants represent a widely accepted and clinically validated solution for the replacement of extracted or missing teeth with a high success rate of 90% [5,6,7]. Implant therapy with two-piece implant systems involves a multi-step process, integrating both surgical and prosthodontic components. The surgical component includes a dental implant, mostly made of titanium, a biocompatible material that is inserted into the alveolar bone of the mandible or maxilla [8]. Implant abutment serves as the critical connecting component in implant prosthodontic therapy, linking the implant to the prosthodontic restoration [9,10]. Choosing the right implant abutment is crucial for optimal function, aesthetics, and long-term success with dental implants [11].
Stock implant abutments offer several advantages, including low cost, reliable engagement with the implant body, and the capability to be prepared either intraorally or extraorally. However, stock abutments also have certain limitations, such as extended preparation time, particularly in cases of mispositioned dental implants, since they do not conform well to the anatomical complexities of the gingival contour [12]. Inadequate adaptation of the implant abutment to the gingival margin may lead to the retention of excess cement in the peri-implant tissues during the cementation process. Thus, cement in the peri-implant sulcus can result in inflammation of soft and hard tissues surrounding dental implants [13]. Stock implant abutments are commonly made from two different types of materials, depending on the clinical situation in terms of strength, function, and appearance. Titanium abutments are most frequently used because of their well-documented biological and mechanical benefits. Conversely, the grayish discoloration beneath the peri-implant mucosa fail to meet the optical and aesthetic requirements for implant-supported restorations [14,15]. Zirconia abutments have suitable optical characteristics [14] but some challenges have been observed with the clinical use of zirconia abutments, such as risk of fracture and wear on the titanium implant where it connects with the zirconia [16]. Nevertheless, stock abutments do not always offer enough options in terms of size, angulation, and emergence profile, which can make it challenging to fully adapt them [17].
Peri-implantitis represents one of the most prevalent biological complications associated with dental implants, with epidemiological data indicating that approximately 20% of patients are likely to develop the condition over time. Despite extensive research, clinical management of peri-implantitis remains complex and continues to present significant therapeutic challenges [18]. A certain number of mechanisms have been used to explain the beneficial effect of higher abutments on marginal bone levels. Firstly, higher abutments provide increased space for the establishment of the supracrestal soft tissue attachment. Secondly, by positioning the abutment–crown interface more coronally, higher abutments distance the microgap from the crestal bone [18,19]. Microgaps are strongly associated with the extent of peri-implant bacterial colonization, which may compromise the sealing capacity of the peri-implant mucosa and thereby increase the risk of peri-implantitis as well as mechanical complications [20]. The application of digital technologies allows the fabrication of prosthetic components with high precision, thereby minimizing manufacturing errors and reducing the incidence of microgaps [21].
With the advancement of CAD/CAM (Computer-Aided Design/Computer-Aided Manufacturing) technology, the fabrication of implant abutments has increasingly been carried out by usage of this digital approach. The advantages include fewer manual steps, enabling a simplified production process and offering high predictability. Additionally, digitally designed and manufactured implant abutments can be customized to each specific case, offering advantages like the capability to be fabricated from various materials, most notably titanium and zirconia [22]. A novel method for achieving both aesthetics and strength in implant dentistry is the hybrid-abutment approach [23,24]. Hybrid implant abutments combine the benefits of both zirconia and titanium implant abutments, including improved aesthetics, optimal biological response, and superior mechanical properties, without negatively effecting the implant–abutment interface [24]. Appropriate adhesive bonding procedures between titanium and zirconia components of a hybrid implant abutment is essential to prevent retention loss of a prosthodontic restoration [25]. Nowadays, hybrid implant abutments are most frequently fabricated through digital workflow which requires a digital impression which can be obtained either directly from the oral cavity by using a scan body or indirectly from a cast model. A suitable titanium insert can be selected based on a specific implant system, while CAD/CAM software is utilized to design the zirconia component of hybrid implant abutment [24]. CAD/CAM abutments are designed digitally by the clinician or technician [22], relying on their input to shape and fit the component, whereas generative design uses algorithms to automatically create optimized geometries [26,27]. In CAD/CAM, the final design depends largely on the operator’s experience, while generative design explores multiple possibilities based on mechanical, biological, and aesthetic factors. CAD/CAM provides predictable and standardized results, minimizing errors and microgaps, but it does not inherently optimize performance. Generative design, on the other hand, can produce patient-specific abutments with unique shapes that improve stress distribution and support healthier peri-implant tissues. While CAD/CAM focuses on accurately reproducing a planned design, generative design emphasizes solutions tailored to the individual needs of each case. Together, these approaches show how digital technology is evolving in implant prosthodontics, combining precision with performance-focused innovation.
However, despite the increasing popularity of hybrid abutments, the current design process remains largely manual and highly dependent on the clinician’s or technician’s experience. This is particularly challenging given the complex interplay of mechanical and aesthetic requirements inherent in hybrid configurations. One of the most critical issues is the structural vulnerability of the zirconia component, which is prone to fracture under functional loading. Such failures not only compromise the prosthodontic restoration but may also require redesigning both the zirconia and titanium parts to restore function and stability. As a result, designing hybrid abutments involves balancing multiple interdependent factors such as structural integrity, aesthetics, fit, and adhesive integrity, making it challenging to achieve consistent, optimal outcomes. This highlights the need for a more systematic design approach that can guide the user through these competing priorities and provide performance-based design support.
Generative design is a computer-based design approach where a designer sets the key parameters, like material type, function, anatomy, and aesthetics, and the software takes over from there, automatically generating a range of optimized design options. Unlike traditional CAD, where a designer manually creates the shape, generative design lets the system explore multiple possibilities and propose the best solutions based on a given criteria [26,27]. The range of parameter values must be determined prior to the design process to optimize the outcome and ensure the most effective performance of the final object. In implant prosthodontics, generative design allows exploration of a wide range of different solutions to identify the optimal configuration of a given structure (e.g., hybrid implant abutment). Published data regarding standardized requirements for optimal design of hybrid implant abutments are scarce and all decisions are made based on prior experience and case-specific considerations. Accordingly, the broad implementation of generative design within the context of implant prosthodontics is not feasible.
The purpose of the present study was to conduct a literature review on the transmucosal and prosthodontic height of implant abutments to determine their optimal dimensions. The study focused on defining the key preparatory steps required for the effective implementation of generative design in implant prosthodontics.
2. Materials and Methods
The scoping review was reported in accordance with the PRISMA 2020 (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [28] and was registered in the Open Science Framework (OSF) public registry (Registration DOI: https://doi.org/10.17605/OSF.IO/WNSKQ). A comprehensive literature search was conducted to identify all relevant studies addressing the primary purpose of the study. Studies that investigated transmucosal height of implant abutment and prosthodontic height of implant abutment in the last five years have been included in the literature review. The last five years have been selected to capture the most recent studies in the review and to ensure the inclusion of the most current and accurate evidence. This timeframe allows the analysis to reflect the latest advances and trends in the field. The exclusion criteria encompassed case series, editorials, and interview articles, as well as studies which were not written in the English language. A bibliographic search was performed across the PubMed and Scopus databases to identify relevant studies published up to 1 July 2025. Inclusion criteria comprised full-text studies published in the English language which were conducted on a human model. The search keywords were “transmucosal height of implant abutment” and “prosthodontic height of implant abutment”. The total number of studies included in the review is illustrated in a PRISMA-based flow diagram (Figure 1). Two experienced reviewers (V.P. and P.K.) independently assessed the titles of all retrieved studies based on predefined inclusion criteria. Subsequently, the abstracts of the selected studies were screened, and those deemed relevant were subjected to full-text evaluation. Inclusion of each study in the final analysis required consensus between both primary reviewers. In cases of disagreement or uncertainty, two additional reviewers (S.S. and A.C.) were consulted to reach the solution. The data extraction protocol encompassed the following parameters: authors and year of publication, study title, type of the study, sample size, and conclusion of the study (Table 1 and Table 2).
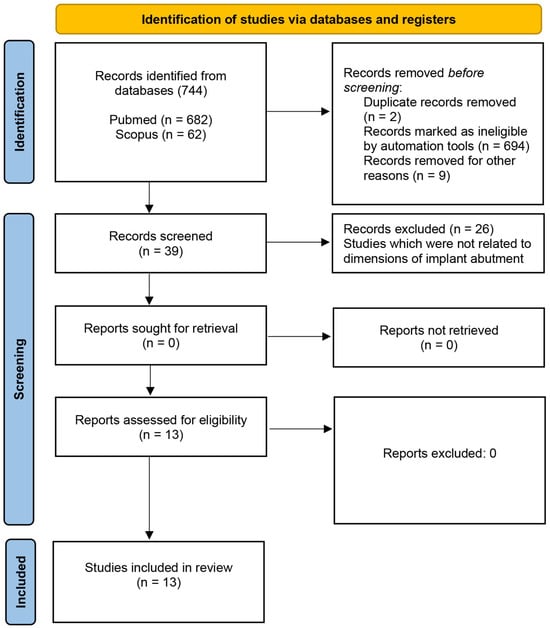
Figure 1.
PRISMA-based flowchart illustrating the identification, screening, and selection process of the records during the search.

Table 1.
Studies included in the review dealing with transmucosal height of implant abutments.

Table 2.
Studies included in the review dealing with prosthodontic height of implant abutments.
3. Results
Initially, a total of 744 studies were identified through the database search. Duplicates were removed and an automation tool was employed to remove ineligible studies which did not fulfill inclusion criteria. Thirty-nine studies entered the screening process. In the end, 13 studies fulfilled inclusion criteria and were further analyzed. Figure 1 shows a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses)-based flowchart illustrating the identification, screening, and selection process of the records during the search. Three out of thirteen studies were related to transmucosal height of implant abutment, while the rest of them were associated with prosthodontic height of implant abutments. Three studies that met inclusion criteria regarding transmucosal height of implant abutment include “Combined Effect of Abutment Height and Restoration Emergence Angle on Peri-Implant Bone Loss Progression: A Retrospective Analysis” by Misch et al. [29]; “Limited marginal bone loss in implant-supported fixed full-arch rehabilitations after 5 years of follow-up” by Galindo-Moreno et al. [30]; “Effects of Different Patient and Prosthetic Variables on Marginal Bone Behavior in Dental Implants: A Clinical Retrospective Study” by Gehrke et al. [31]. All aforementioned studies investigated the influence between transmucosal height of implant abutments and marginal bone loss and concluded that implant abutments should have height above 2 mm to reduce bone loss and to minimize the risk of peri-implantitis. Table 1 provides a synthesized summary of the data extracted from the studies included in the analysis. Studies which were associated with prosthodontic height of implant abutments are listed in Table 2. Six studies [32,33,34,35,36,37] investigated the influence of prosthodontic abutment height on marginal bone loss. The findings consistently indicate that a minimum prosthodontic implant abutment height of 2 mm is recommended to minimize marginal bone resorption around dental implants. The remaining four studies [38,39,40,41] focused on distinct aspects related to implant abutments: crown retention on implant abutments, the influence of abutment heights on screw loosening, the effect of abutment height on the pull-off force of crowns, and the fracture strength analysis of implant abutments, respectively. Retention of restorations was enhanced when longer implant abutments were utilized [38]. The height of the implant abutment has been shown to influence screw loosening [41] and long-term stability of restorations as well [40]. Only one study [39] comparing pull-off forces of cement-retained implant-supported single crowns on stock titanium abutments showed lesser influence of implant abutment height when compared to cement. From all of the above, the importance of optimal implant abutment dimensions becomes evident.
4. Discussion
Before applying generative design in implant prosthodontics, it is important to go through a careful parametrization process. This means identifying the biomechanical factors that will guide the design. This approach ensures that the generative design process remains within clinically relevant boundaries, producing outcomes that are not only anatomically accurate but also functionally appropriate for intraoral conditions. Parametrization acts as a foundation, helping the system understand what is important for each individual case. Without parametrization, the designs may not meet the practical needs of dental treatment. Therefore, a comprehensive review was conducted to collect and analyze the data related to the dimensional characteristics of implant abutments (transmucosal and prosthodontic height).
A review of three studies [29,30,31] (Table 1) that focused on transmucosal height of implant abutment showed coherent results. Misch et al. [29] analyzed the influence of transmucosal abutment height on marginal bone loss around bone-level implants. Marginal bone levels were assessed at two time intervals: 12–18 months post-crown placement (T0) and more than one year after the T0 radiograph (T1), on both mesial and distal aspects of the implant. The change in bone loss was determined as the difference between the measurements obtained at T0 and T1. Two different transmucosal abutment heights (<2 mm and >2 mm) were evaluated and it was concluded that abutments with a transmucosal height greater than 2 mm were significantly associated with a reduced incidence of peri-implantitis and marginal bone loss. A possible reason for this common observation is that short implant abutments do not leave enough vertical space for proper supracrestal tissue formation. This can lead to increased marginal bone loss, exposure of the implant’s rough surface, and even the implant threads, creating areas where plaque can accumulate and increasing the risk of peri-implantitis [29]. Galindo-Moreno et al. [30] investigated the influence of 4 different transmucosal heights of implant abutments (1 mm, 2 mm, 4 mm, and 6 mm) on marginal bone loss. Marginal bone levels were assessed by importing panoramic radiographs in DICOM (Digital Imaging and Communications in Medicine) format into an image analysis platform. Measurements were taken from the implant shoulder to the most coronal aspect of the supporting crestal bone, with negative values assigned when the bone crest was positioned apically relative to the implant shoulder. The results of the study showed that marginal bone loss was higher in 1 mm implant abutments when in comparison with 2 mm, 4 mm, and 6 mm implant abutments. This finding demonstrates that implant abutment height has a significant influence on marginal bone loss, following the principle that greater abutment height is associated with reduced marginal bone loss. The results of these two studies [29,30] are in accordance with the third included study in which Gehrke et al. [31] examined marginal bone-level alterations based on transmucosal abutment height. The transmucosal height of the evaluated abutments was categorized into three groups: the first group comprised abutments with heights of 0.8 and 1.5 mm; second group comprised abutments of 2.5 mm; and third group comprised abutments with heights ≥ 3.5 mm (3.5, 4.5, and 5.5 mm). Measurements were performed on radiographs obtained at time points C1 (rehabilitation installation) and C2 (final follow-up), and the change in values was calculated as the difference between C2 and C1. The authors concluded that implant abutment height greater than 2.5 mm has been associated with reduced peri-implant marginal bone loss. The observed differences in marginal bone loss among the groups indicate that, when clinically feasible, taller abutments should be preferred [31]. According to the recent study [29], implants with a transmucosal abutment height greater than 2 mm were found to have about four times less risk of developing peri-implantitis. The reviewed studies underscore the importance of optimizing implant abutment dimensions, emphasizing the critical role of precise parameterization before the generative design process.
A review of ten studies [32,33,34,35,36,37,38,39,40,41] (Table 2) dealing with prosthodontic height of implant abutment highlights its significant impact on soft tissue health, prosthodontic stability, and long-term implant success. Six studies [32,33,34,35,36,37] investigated the influence on marginal bone loss and showed congruent results. Studies showed that an abutment height of no less than 2 mm is recommended for optimal clinical outcomes. The impact of short abutments (<2 mm) on marginal bone loss may be attributed to two factors. Firstly, shorter abutments (<2 mm) are associated with reduced supracrestal tissue height and biological width, which may compromise the protective barrier around the initial bone-to-implant contact. Secondly, a shorter abutment (<2 mm) reduces the vertical distance between the implant shoulder and the prosthodontic interface, thereby positioning the oral microbiota in closer proximity to the first bone-to-implant contact, potentially facilitating bacterial infiltration and subsequent bone resorption [32].
One study [38] emphasized the impact of titanium-base (Ti-base) height on the retentive properties of hybrid abutment crowns. Two different implant abutment heights of 4 mm and 7 mm were tested. The 7 mm Ti-base showed noticeably stronger retention compared to the 4 mm Ti-base, regardless of the crown material used. The retention of fixed restoration is closely related to the total surface area of the implant abutment. Since all abutments in the analyzed study [38] had the same diameter, the surface area was mainly determined by their height. This means the longer abutments had more surface area than the shorter ones, which likely explains why they showed better retention. In conclusion the surface area of the abutment can be approximated by the product of its diameter and height [38]. The importance of the optimal abutment height is noticeable.
In a recent study [41], the authors compared the influence of different types (stock, cast, and milled) of abutments with standardized heights of 4 mm, 7 mm, and 10 mm on a screw loosening. Abutments with a 4 mm height demonstrated superior performance in maintaining screw torque compared to those of 7 mm and 10 mm heights [41]. Accordingly, height of abutment presents an essential factor which can affect the long-term success and mechanical stability of implant-supported restorations [41].
A study by Müller et al. [39] evaluated and compared the pull-off forces of cement-retained zirconia-reinforced lithium silicate single crowns placed on titanium abutments, focusing on how different abutment heights and types of implant cement affect retention. Abutment heights of 3 mm and 5 mm were utilized in the study [39]. The influence of abutment height on pull-off forces was found to be limited when compared to cements [39]. However, abutment height plays an important role in routine clinical practice.
Song et al. [40] examined fracture strength by adjusting the height (1 mm, 3 mm, and 5 mm) of the titanium insert. The goal was to determine which titanium insert height offers the best mechanical stability. The results of the study showed that the axial height of the titanium insert should be designed to be at least 3 mm [40]. A titanium insert with an axial height of 1 mm appears clinically inadequate due to its insufficient mechanical strength [40].
Choosing and adapting optimal implant abutment parameters clearly plays a key role in both biological response and technical performance of a restoration. It can make a real difference in how well the implant integrates with the bone, how stable the surrounding soft tissue remains, and how the restoration holds up over time. With modern tools like CAD/CAM and generative design, it is now possible to create solutions that are better tailored to each patient, leading to more reliable and long-lasting results.
Apart from the transmucosal and prosthodontic implant abutment heights, it is essential to define additional parameters before establishing the initial parametric model, to ensure optimal biomechanical performance, patient-specific adaptation, and the long-term clinical success of the implant-supported restoration. A careful analysis of additional factors should encompass both mechanical factors (implant abutment angulation, load distribution, and type of restoration) and biological factors (soft tissue phenotype, bone density, occlusal forces, and available interocclusal space), emphasizing that future studies should focus on these parameters.
The limitation of the present study may be that only the available literature across databases was considered, rather than all possible studies.
5. Conclusions
Based on the present scoping review, a set of fundamental parameters critical for the design of hybrid abutments has been identified: transmucosal and prosthodontic height of implant abutments. Representative values were established according to published data and clinical recommendations (>2 mm for each parameter). These parameters will serve as the foundation for constructing an initial parametric model to be used in generative design. This foundational model will be further developed and expanded based on ongoing literature insights, future experimental findings, and established knowledge from structural analysis and mechanical stability assessments.
In addition, the present study provides a comprehensive synthesis of existing evidence on the influence of abutment design parameters, helping to identify gaps in current research and guiding future investigations. By consolidating findings from multiple sources, the review offers suggestions for clinicians to invest more time and thought in selecting abutment designs to optimize peri-implant tissue health and mechanical performance. Furthermore, the study establishes a structured framework that can support development of more predictive and patient-specific implant abutment designs, ultimately contributing to improved clinical outcomes and advancing the field of implant prosthodontics.
6. Future Directions
In the future, studies on transmucosal and prosthodontic height of implant abutments will likely move toward more personalized designs that take into account each patient’s soft tissue thickness and aesthetic needs. Generative design in implant prosthodontics remains in its developmental phase, with definitive technical solutions and standardized clinical guidelines yet to be established. However, due to industry involvement and interest, it is expected to reach technical readiness in a short period of time. Using generative design to customize hybrid implant abutments could reshape treatment planning by making it easier to develop solutions that are both biologically compatible and functionally effective for prosthodontic use.
Author Contributions
Conceptualization, A.C. and S.S.; methodology, V.P.; investigation, P.K. and V.P.; writing—original draft preparation, V.P. and P.K.; writing—review and editing, A.C. and S.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by an EU project: Generative Design for Mass Personalization of Dental Implantoprosthetic Abutments (GENKON), grant number: NPOO.C3.2.R3-I1.04.0121.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original contributions of this study are detailed within the article. For additional information or clarifications, interested readers are encouraged to contact the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Ruhstorfer, M.; Güth, J.F.; Stimmelmayr, M.; Waltenberger, L.; Schubert, O.; Graf, T. Systematic review of peri-implant conditions and aesthetic outcomes of customized versus conventional healing abutments. Int. J. Implant. Dent. 2024, 10, 61. [Google Scholar] [CrossRef]
- Schweiger, J.; Edelhoff, D.; Güth, J.F. 3D Printing in Digital Prosthetic Dentistry: An Overview of Recent Developments in Additive Manufacturing. J. Clin. Med. 2021, 10, 2010. [Google Scholar] [CrossRef] [PubMed]
- Schubert, O.; Schweiger, J.; Stimmelmayr, M.; Nold, E.; Güth, J.F. Digital implant planning and guided implant surgery–Workflow and reliability. Br. Dent. J. 2019, 226, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Graf, T.; Keul, C.; Wismeijer, D.; Güth, J.F. Time and costs related to computer-assisted versus non-computer-assisted implant planning and surgery. A systematic review. Clin. Oral Implants Res. 2021, 32, 303–317. [Google Scholar] [CrossRef] [PubMed]
- Yağır, M.O.; Şen, Ş.; Şen, U. Examination of Various Abutment Designs Behavior Depending on Load Using Finite Element Analysis. Biomimetics 2024, 9, 498. [Google Scholar] [CrossRef]
- Saghiri, M.A.; Freag, P.; Fakhrzadeh, A.; Saghiri, A.M.; Eid, J. Current technology for identifying dental implants: A narrative review. Bull. Natl. Res. Cent. 2021, 45, 7. [Google Scholar] [CrossRef]
- Smojver, I.; Bjelica, R.; Vuletić, M.; Gerbl, D.; Budimir, A.; Gabrić, D. Antimicrobial Efficacy and Permeability of Various Sealing Materials in Two Different Types of Implant-Abutment Connections. Int. J. Mol. Sci. 2022, 23, 8031. [Google Scholar] [CrossRef]
- Nicholson, J. Titanium alloys for dental implants: A review. Prosthesis 2020, 2, 11. [Google Scholar] [CrossRef]
- Totou, D.; Naka, O.; Mehta, S.B.; Banerji, S. Aesthetic, mechanical, and biological outcomes of various implant abutments for single-tooth replacement in the anterior region: A systematic review of the literature. Int. J. Implant. Dent. 2021, 7, 85. [Google Scholar] [CrossRef]
- Shah, K.K.; Sivaswamy, V. A Literature Review on Implant Abutment Types, Materials, and Fabrication Processes. J. Long Term Eff. Med. Implant. 2023, 33, 57–66. [Google Scholar] [CrossRef]
- Strasding, M.; Marchand, L.; Merino, E.; Zarauz, C.; Pitta, J. Material and abutment selection for CAD/CAM implant-supported fixed dental prostheses in partially edentulous patients–A narrative review. Clin. Oral Implants Res. 2024, 35, 984–999. [Google Scholar] [CrossRef]
- Alsaadi, M.N.; Morad, M.L.; Darwich, K.; Kanout, S.; Husein, H.A. A Comparative Study Between Hybrid Abutments and Standard Abutments in Implant-Supported Prosthesis: A Split-Mouth Clinical Trial. Cureus 2022, 14, e31993. [Google Scholar] [CrossRef]
- Obădan, M.E.; Mitruț, I.; Ionescu, M.; Obădan, F.; Târtea, D.A.; Popescu, M.A.; Popescu, S.M.; Smarandache, A.M.; Manolea, H.O. Clinical Efficacy Analysis of the Personalization of Prosthetic Abutments in Implant Supported Restorations in Comparison to Available Standard Titanium Abutments. J. Pers. Med. 2023, 13, 1402. [Google Scholar] [CrossRef]
- Çeken, A.; Kılınç, H.; Turgut, S. Effect of abutment types and resin cements on the aesthetics of implant-supported restorations. J. Adv. Prosthodont. 2023, 15, 114–125. [Google Scholar] [CrossRef] [PubMed]
- Kilinc, H.; Sanal, F.A.; Turgut, S. Evaluation of the effect of different abutment materials on the final color of implant supported full ceramic restorations. Turkiye Klinikleri J. Dent. Sci. 2020, 26, 426–433. [Google Scholar] [CrossRef]
- Arif, R.; Yilmaz, B.; Mortazavi, A.; Ozcelik, T.B.; Johnston, W.M. Effect of metal opaquer on the final color of 3 ceramic crown types on 3 abutment configurations. J. Prosthet. Dent. 2018, 120, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Chmielewski, M.; Dąbrowski, W.; Ordyniec-Kwaśnica, I. The Fracture Resistance Comparison between Titanium and Zirconia Implant Abutments with and without Ageing: Systematic Review and Meta-Analysis. Dent. J. 2024, 12, 274. [Google Scholar] [CrossRef]
- Laleman, I.; Lambert, F. Implant connection and abutment selection as a predisposing and/or precipitating factor for peri-implant diseases: A review. Clin. Implant. Dent. Relat. Res. 2023, 25, 723–733. [Google Scholar] [CrossRef]
- Del Amo, F.S.; Romero-Bustillos, M.; Catena, A.; Galindo-Moreno, P.; Sánchez-Suárez, J.M.; Sánchez, R.; Garaicoa-Pazmino, C. Effect of Abutment Height on Marginal Bone Loss Around Dental Implants: A Systematic Review. Int. J. Prosthodont. 2024, 37, 95–102. [Google Scholar] [CrossRef]
- Yang, F.; Du, Y.; Zhang, Z.; Wang, M.; Yin, W.; Zhou, Z.; Li, S.; Hu, Y.; Chen, J.; Li, J.; et al. Evaluation of microgaps and microleakage at the implant-abutment interface of individualized abutments in the maxillary anterior region under functional loading: A pragmatic clinical trial. J. Prosthodont. Res. 2025, 69, 58–67. [Google Scholar] [CrossRef]
- Molinero-Mourelle, P.; Cascos-Sanchez, R.; Yilmaz, B.; Lam, W.Y.H.; Pow, E.H.N.; Del Río Highsmith, J.; Gómez-Polo, M. Effect of Fabrication Technique on the Microgap of CAD/CAM Cobalt-Chrome and Zirconia Abutments on a Conical Connection Implant: An In Vitro Study. Materials 2021, 14, 2348. [Google Scholar] [CrossRef] [PubMed]
- Târtea, D.A.; Ionescu, M.; Manolea, H.O.; Mercuț, V.; Obădan, E.; Amărăscu, M.O.; Mărășescu, P.C.; Dăguci, L.; Popescu, S.M. Comparative Study of Dental Custom CAD-CAM Implant Abutments and Dental Implant Stock Abutments. J. Clin. Med. 2023, 12, 2128. [Google Scholar] [CrossRef] [PubMed]
- Elshiyab, S.H.; Nawafleh, N.; Khan, U.; Öchsner, A.; George, R. Impact of Coping Veneering Techniques on the Survival of Implant-Supported Zirconia-Based-Crowns Cemented to Hybrid-Abutments: An-In-Vitro Study. Bioengineering 2020, 7, 117. [Google Scholar] [CrossRef] [PubMed]
- Mostafavi, A.S.; Mojtahedi, H.; Javanmard, A. Hybrid Implant Abutments: A Literature Review. Eur. J. Gen. Dent. 2021, 10, 106–115. [Google Scholar] [CrossRef]
- Takano, R.; Honda, J.; Kobayashi, T.; Kubochi, K.; Takata, H.; Komine, F. Fracture strength of implant-supported hybrid abutment crowns in premolar region fabricated using different restorative CAD/CAM materials. Dent. Mater. J. 2023, 42, 187–192. [Google Scholar] [CrossRef]
- Caetano, I.; Santos, L.; Leitão, A. Computational design in architecture: Defining parametric, generative, and algorithmic design. Front. Arch. Res. 2020, 9, 287–300. [Google Scholar] [CrossRef]
- Li, H.; Ye, Y.; Zhang, Z.; Yu, W.; Zhu, W. A comparative analysis of CAD modeling approaches for design solution space exploration. Adv. Mech. Eng. 2024, 16, 16878132241238088. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Misch, J.; Abu-Reyal, S.; Lohana, D.; Mandil, O.; Saleh, M.H.A.; Li, J.; Wang, H.L.; Ravidà, A. Combined Effect of Abutment Height and Restoration Emergence Angle on Peri-Implant Bone Loss Progression: A Retrospective Analysis. Clin. Oral Implants Res. 2025, 36, 600–612. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Ravidà, A.; Catena, A.; O’Valle, F.; Padial-Molina, M.; Wang, H.L. Limited marginal bone loss in implant-supported fixed full-arch rehabilitations after 5 years of follow-up. Clin. Oral Implants Res. 2022, 33, 1224–1232. [Google Scholar] [CrossRef]
- Gehrke, S.A.; Scarano, A.; Lorusso, F.; Balduino, T.Y.; Bianchini, M.A. Effects of Different Patient and Prosthetic Variables on Marginal Bone Behavior in Dental Implants: A Clinical Retrospective Study. Medicina 2025, 61, 1041. [Google Scholar] [CrossRef] [PubMed]
- Quispe-López, N.; Guadilla, Y.; Gómez-Polo, C.; López-Valverde, N.; Flores-Fraile, J.; Montero, J. The influence of implant depth, abutment height and mucosal phenotype on peri-implant bone levels: A 2-year clinical trial. J. Dent. 2024, 148, 105264. [Google Scholar] [CrossRef] [PubMed]
- Quintas-Hijós, J.; Pérez-Pevida, E. Influence of intermediate abutment height and timing of placement on marginal bone loss in single implant-supported crowns: A 12-month follow-up randomized clinical trial. Clin. Oral Investig. 2025, 29, 291. [Google Scholar] [CrossRef] [PubMed]
- Tajti, P.; Solyom, E.; Váncsa, S.; Mátrai, P.; Hegyi, P.; Varga, G.; Hermann, P.; Borbély, J.; Sculean, A.; Mikulás, K. Less marginal bone loss around bone-level implants restored with long abutments: A systematic review and meta-analysis. Periodontol. 2000 2024, 94, 627–638. [Google Scholar] [CrossRef]
- Ríos-Santos, J.V.; Tello-González, G.; Lázaro-Calvo, P.; Gil Mur, F.J.; Ríos-Carrasco, B.; Fernández-Palacín, A.; Herrero-Climent, M. One Abutment One Time: A Multicenter, Prospective, Controlled, Randomized Study. Int. J. Environ. Res. Public Health 2020, 17, 9453. [Google Scholar] [CrossRef]
- Arai, Y.; Takashima, M.; Matsuzaki, N.; Takada, S. Marginal bone loss in dental implants: A literature review of risk factors and treatment strategies for prevention. J. Prosthodont. Res. 2025, 69, 12–20. [Google Scholar] [CrossRef]
- Galindo-Moreno, P.; Catena, A.; Pérez-Sayáns, M.; Fernández-Barbero, J.E.; O’Valle, F.; Padial-Molina, M. Early marginal bone loss around dental implants to define success in implant dentistry: A retrospective study. Clin. Implant. Dent. Relat. Res. 2022, 24, 630–642. [Google Scholar] [CrossRef]
- Alseddiek, A.; Al-Zordk, W.; Attia, A. Retention of hybrid-abutment-crowns with offset implant placement: Influence of Crown materials and Ti-base height. BMC Oral Health 2023, 23, 784. [Google Scholar] [CrossRef]
- Müller, L.; Rauch, A.; Reissmann, D.R.; Schierz, O. Impact of cement type and abutment height on pull-off force of zirconia reinforced lithium silicate crowns on titanium implant stock abutments: An in vitro study. BMC Oral Health 2021, 21, 592. [Google Scholar] [CrossRef]
- Song, S.R.; Park, K.M.; Jung, B.Y. Fracture strength analysis of titanium insert-reinforced zirconia abutments according to the axial height of the titanium insert with an internal connection. PLoS ONE 2021, 16, e0249208. [Google Scholar] [CrossRef]
- Hendi, A.; Mirzaee, S.; Falahchai, M. The effect of different implant-abutment types and heights on screw loosening in cases with increased crown height space. Clin. Exp. Dent. Res. 2024, 10, e894. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).