Evaluating Glass Ionomer Cement Longevity in the Primary and Permanent Teeth—An Umbrella Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sources
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Data Collection
2.5. Quality Assessment and Risk of Bias
3. Results
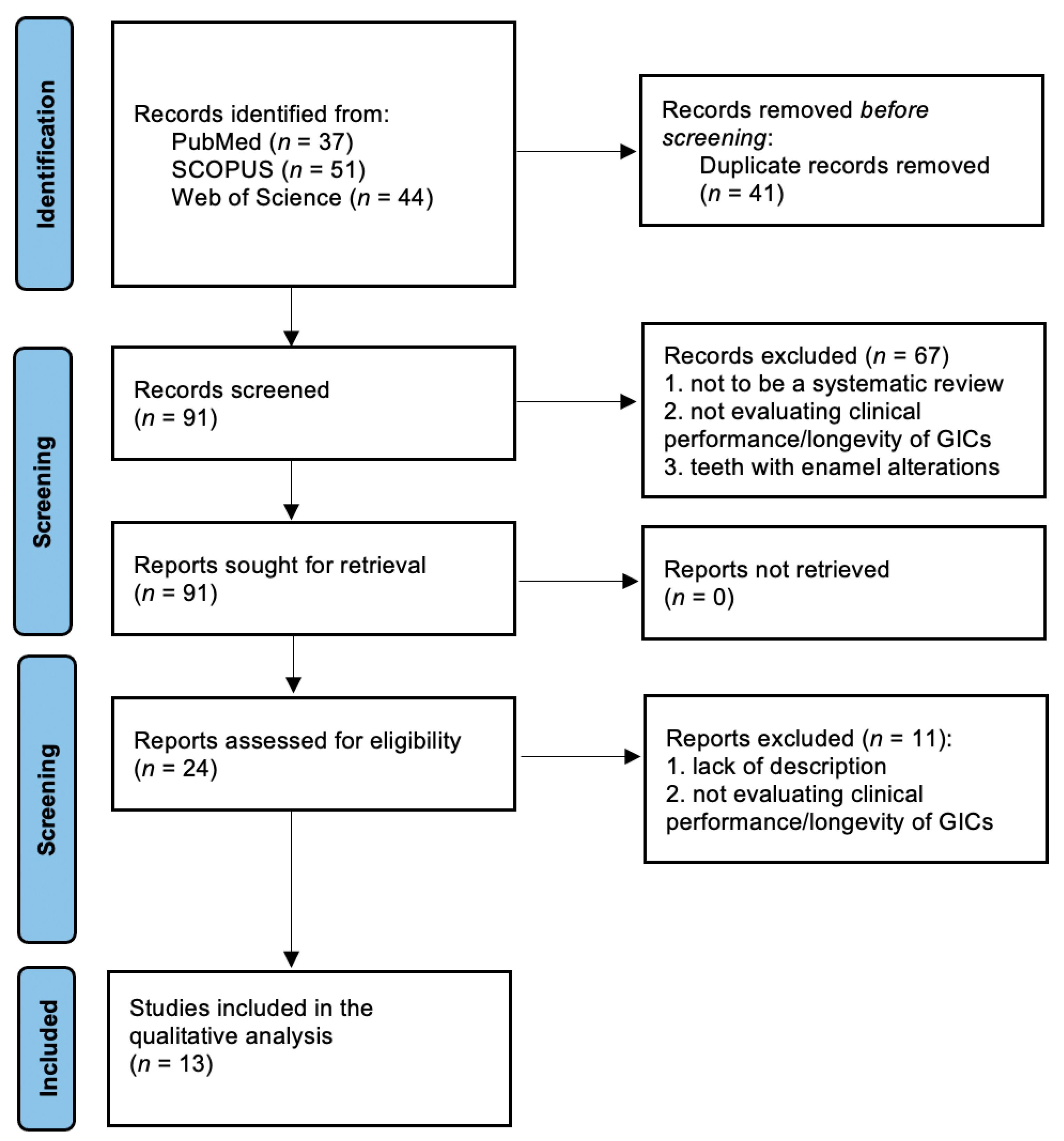
3.1. Study Selection
3.2. Characteristics of Included Studies and Quality Assessment
3.3. Risk of Bias
3.4. Quality Assessment Analysis
4. Discussion
4.1. Limitations of this Study
4.2. Recommendations for Future Studies
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- McCabe, J.F.; Yan, Z.; Al Naimi, O.T.; Mahmoud, G.; Rolland, S.L. Smart materials in dentistry—Future prospects. Dent. Mater. J. 2009, 28, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Wilson, A.D. Glass-ionomer cement–origins, development and future. Clin. Mater. 1991, 7, 275–282. [Google Scholar] [CrossRef]
- Smith, D.C. Development of glass-ionomer cement systems. Biomaterials 1998, 19, 467–478. [Google Scholar] [CrossRef] [PubMed]
- Veiga, N.; Figueiredo, R.; Correia, P.; Lopes, P.; Couto, P.; Fernandes, G.V.O. Methods of Primary Clinical Prevention of Dental Caries in the Adult Patient: An Integrative Review. Healthcare 2023, 11, 1635. [Google Scholar] [CrossRef]
- Figundio, N.; Lopes, P.; Tedesco, T.K.; Fernandes, J.C.H.; Fernandes, G.V.O.; Mello-Moura, A.C.V. Deep Carious Lesions the quality of the included studies were independently assessed by two reviewers using the RoB Management with Stepwise, 2 tool. Results: 5 out of 105 potentially eligible studies were included. Regarding the teeth included Selective, or Non-Selective Removal in Permanent Dentition: A Systematic Review of Randomized Clinical Trials. Healthcare 2023, 11, 2338. [Google Scholar] [CrossRef] [PubMed]
- Machado, C.F.A.; Fernandes, G.V.O.; Fernandes, J.C.H.; Seabra, M.; Figueiredo, A. Surface roughness of three different glass ionomers with or without finishing/polishing: An in vitro study. Int. J. Sci. Dent. 2024, 63, 146–167. [Google Scholar]
- Davidson, C.L. Advances in glass-ionomer cements. J. Appl. Oral. Sci. 2006, 14, 3–9. [Google Scholar] [CrossRef]
- Berg, J.H.; Croll, T.P. Glass ionomer restorative cement systems: An update. Pediatr. Dent. 2015, 37, 116–124. [Google Scholar]
- Khoroushi, M.; Keshani, F. A review of glass-ionomers: From conventional glass-ionomer to bioactive glass-ionomer. Dent. Res. J. 2013, 10, 411–420. [Google Scholar]
- de Lima Navarro, M.F.; Pascotto, R.C.; Borges, A.F.S.; Soares, C.J.; Raggio, D.P.; Rios, D.; Bresciani, E.; Molina, G.F.; Ngo, H.C.; Miletić, I.; et al. Consensus on glassionomer cement thresholds for restorative indications. J. Dent. 2021, 107, 103609. [Google Scholar] [CrossRef]
- Frankenberger, R.; Garcia-Godoy, F.; Krämer, N. Clinical Performance of Viscous Glass Ionomer Cement in Posterior Cavities over Two Years. Int. J. Dent. 2009, 2009, 781462. [Google Scholar] [CrossRef] [PubMed]
- Burke, F.J.T.; Lucarotti, P.S.K. The ultimate guide to restoration longevity in England and Wales. Part 3: Glass ionomer restorations—Time to next intervention and to extraction of the restored tooth. Br. Dent. J. 2018, 224, 865–874. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.F.; Smales, R.J.; Fang, D.T. A 2-year clinical study of two glass ionomer cements used in the atraumatic restorative treatment (ART) technique. Community Dent. Oral. Epidemiol. 1999, 27, 195–201. [Google Scholar] [CrossRef]
- Beyer, C.; Schwahn, C.; Meyer, G.; Söhnel, A. What German dentists choose for their teeth: A Web-based survey of molar restorations and their longevity. J. Prosthet. Dent. 2021, 125, 805–814. [Google Scholar] [CrossRef]
- Andas, K.; Knorst, J.K.; Bonifacio, C.C.; Kleverlaan, C.J.; Hesse, D. Compomers for the restorative treatment of dental caries in primary teeth: An umbrella review. J. Dent. 2023, 138, 104696. [Google Scholar] [CrossRef] [PubMed]
- Amend, S.; Seremidi, K.; Kloukos, D.; Bekes, K.; Frankenberger, R.; Gizani, S.; Krämer, N. Clinical Effectiveness of Restorative Materials for the Restoration of Carious Primary Teeth: An Umbrella Review. J. Clin. Med. 2022, 11, 3490. [Google Scholar] [CrossRef]
- Sidhu, S.K.; Nicholson, J.W. A Review of Glass-Ionomer Cements for Clinical Dentistry. J. Funct. Biomater. 2016, 7, 16. [Google Scholar] [CrossRef]
- Chung, K.H. The properties of metal-reinforced glass ionomer materials. J. Oral. Rehabil. 1993, 20, 79–87. [Google Scholar] [CrossRef]
- Hewlett, E.R.; Mount, G.J. Glass ionomers in contemporary restorative dentistry—A clinical update. J. Calif. Dent. Assoc. 2003, 31, 483–492. [Google Scholar] [CrossRef]
- Arita, K.; Lucas, M.E.; Nishino, M. The effect of adding hydroxyapatite on the flexural strength of glass ionomer cement. Dent. Mater. J. 2003, 22, 126–136. [Google Scholar] [CrossRef]
- Yap, A.U.; Pek, Y.S.; Kumar, R.A.; Cheang, P.; Khor, K.A. Experimental studies on a new bioactive material: HAIonomer cements. Biomaterials 2002, 23, 955–962. [Google Scholar] [CrossRef] [PubMed]
- Moshaverinia, A.; Ansari, S.; Moshaverinia, M.; Roohpour, N.; Darr, J.A.; Rehman, I. Effects of incorporation of hydroxyapatite and fluoroapatite nanobioceramics into conventional glass ionomer cements (GIC). Acta Biomater. 2008, 4, 432–440. [Google Scholar] [CrossRef] [PubMed]
- Moshaverinia, A.; Roohpour, N.; Chee, W.W.; Schricker, S.R. A review of powder modifications in conventional glass-ionomer dental cements. J. Mater. Chem. 2011, 21, 1319–1328. [Google Scholar] [CrossRef]
- Gu, Y.W.; Yap, A.U.; Cheang, P.; Koh, Y.L.; Khor, K.A. Development of zirconia-glass ionomer cement composites. J. Non-Cryst. Solids 2005, 351, 508–514. [Google Scholar] [CrossRef]
- Ab Rahman, I.; Ghazali, N.A.M.; Bakar, W.Z.W.; Masudi, S.A.M. Modification of glass ionomer cement by incorporating nanozirconia-hydroxyapatite-silica nanopowder composite by the one-pot technique for hardness and aesthetics improvement. Ceram. Int. 2017, 43, 13247–13253. [Google Scholar] [CrossRef]
- Aldhuwayhi, S.D.; Sajjad, A.; Bakar, W.Z.W.; Mohamad, D.; Kannan, T.P.; Moheet, I.A. Evaluation of Fracture Toughness, Color Stability, and Sorption Solubility of a Fabricated Novel Glass Ionomer Nano Zirconia-Silica-Hydroxyapatite Hybrid Composite Material. Int. J. Polym. Sci. 2021, 2021, 6626712. [Google Scholar] [CrossRef]
- Rajabzadeh, G.; Salehi, S.; Nemati, A.; Tavakoli, R.; Solati Hashjin, M. Enhancing glass ionomer cement features by using the HA/YSZ nanocomposite: A feed forward neural network modelling. J. Mech. Behav. Biomed. Mater. 2014, 29, 317–327. [Google Scholar] [CrossRef]
- Kobayashi, M.; Kon, M.; Miyai, K.; Asaoka, K. Strengthening of glass-ionomer cement by compounding short fibres with CaO-P2O5-SiO2-Al2O3 glass. Biomaterials 2000, 21, 2051–2058. [Google Scholar] [CrossRef]
- Lohbauer, U.; Frankenberger, R.; Clare, A.; Petschelt, A.; Greil, P. Toughening of dental glass ionomer cements with reactive glass fibres. Biomaterials 2004, 25, 5217–5225. [Google Scholar] [CrossRef]
- Yli-Urpo, H.; Lassila, L.V.; Närhi, T.; Vallittu, P.K. Compressive strength and surface characterization of glass ionomer cements modified by particles of bioactive glass. Dent. Mater. 2005, 21, 201–209. [Google Scholar] [CrossRef]
- Kumar, A.; Raj, A.; Singh, D.K.; Donthagani, S.; Kumar, M.; Ramesh, K. A New Zinc Reinforced Glass Ionomer Cement: A Boon in Dentistry. J. Pharm. Bioallied Sci. 2021, 13 (Suppl. 1), S272–S275. [Google Scholar] [CrossRef]
- Al-Angari, S.S.; Hara, A.T.; Chu, T.M.; Platt, J.; Eckert, G.; Cook, N.B. Physicomechanical properties of a zinc-reinforced glass ionomer restorative material. J. Oral. Sci. 2014, 56, 11–16. [Google Scholar] [CrossRef][Green Version]
- Bertolini, M.J.; Zaghete, M.A.; Gimenes, R.; Padovani, G.C. Determination of the properties of an experimental glass polyalkenoate cement prepared from niobium silicate powder containing fluoride. Dent. Mater. 2008, 24, 124–128. [Google Scholar] [CrossRef]
- Garcia, I.M.; Leitune, V.C.B.; Balbinot, G.S.; Samuel, S.M.W.; Collares, F.M. Influence of niobium pentoxide addition on the properties of glass ionomer cements. Acta Biomater. Odontol. Scand. 2016, 2, 138–143. [Google Scholar] [CrossRef]
- Mazzaoui, S.A.; Burrow, M.F.; Tyas, M.J.; Dashper, S.G.; Eakins, D.; Reynolds, E.C. Incorporation of casein phosphopeptide-amorphous calcium phosphate into a glass-ionomer cement. J. Dent. Res. 2003, 82, 914–918. [Google Scholar] [CrossRef]
- Reynolds, E.C. Anticariogenic complexes of amorphous calcium phosphate stabilized by casein phosphopeptides: A review. Spec. Care Dentist. 1998, 18, 8–16. [Google Scholar] [CrossRef]
- Ab Rahman, I.; Sam’an, M.M.; Luddin, N.; Shiekh, R.A. One-pot synthesis of hydroxyapatite–silica nanopowder composite for hardness enhancement of glass ionomer cement (GIC). Bull. Mater. Sci. 2014, 37, 213–219. [Google Scholar] [CrossRef]
- Moheet, I.A.; Luddin, N.; Rahman, I.A.; Kannan, T.P.; Nik Abd Ghani, N.R.; Masudi, S.M. Modifications of Glass Ionomer Cement Powder by Addition of Recently Fabricated Nano-Fillers and Their Effect on the Properties: A Review. Eur. J. Dent. 2019, 13, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Liu, R.; Wang, E.; Guo, Y.; Zhou, Q.; Zheng, Y.; Zhai, J.; Zhang, K.; Zhang, B. Enhanced antibacterial properties and promoted cell proliferation in glass ionomer cement by modified with fluorinated graphene-doped. J. Appl. Biomater. Funct. Mater. 2021, 19, 22808000211037487. [Google Scholar] [CrossRef] [PubMed]
- Silva, R.M.; Pereira, F.V.; Mota, F.A.; Watanabe, E.; Soares, S.M.; Santos, M.H. Dental glass ionomer cement reinforced by cellulose microfibers and cellulose nanocrystals. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 58, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Moradian, M.; Nosrat Abadi, M.; Jafarpour, D.; Saadat, M. Effects of Bacterial Cellulose Nanocrystals on the Mechanical Properties of Resin-Modified Glass Ionomer Cements. Eur. J. Dent. 2021, 15, 197–201. [Google Scholar] [CrossRef] [PubMed]
- Sun, J.; Xu, Y.; Zhu, B.; Gao, G.; Ren, J.; Wang, H.; Lin, Y.; Cao, B. Synergistic effects of titanium dioxide and cellulose on the properties of glass ionomer cement. Dent. Mater. J. 2019, 38, 41–51. [Google Scholar] [CrossRef]
- Dowling, A.H.; Stamboulis, A.; Fleming, G.J. The influence of montmorillonite clay reinforcement on the performance of a glass ionomer restorative. J. Dent. 2006, 34, 802–810. [Google Scholar] [CrossRef] [PubMed]
- Fareed, M.A.; Stamboulis, A. Effect of nanoclay dispersion on the properties of a commercial glass ionomer cement. Int. J. Biomater. 2014, 2014, 685389. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of health care interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Whiting, P.; Savović, J.; Higgins, J.P.; Caldwell, D.M.; Reeves, B.C.; Shea, B.; Davies, P.; Kleijnen, J.; Churchill, R.; ROBIS Group. ROBIS: A new tool to assess risk of bias in systematic reviews was developed. J. Clin. Epidemiol. 2016, 69, 225–234. [Google Scholar] [CrossRef]
- McMurray, J.J.; Adamopoulos, S.; Anker, S.D.; Auricchio, A.; Bohm, M.; Dickstein, K.; Falk, V.; Filippatos, G.; Fonseca, C.; Gomez-Sanchez, M.A.; et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2012, 33, 1787–1847. [Google Scholar]
- Santamaría, R.; Abudrya, M.; Gül, G.; Mourad, M.; Gomez, G.; Zandona, A. How to Intervene in the Caries Process: Dentin Caries in Primary Teeth. Caries Res. 2020, 54, 306–323. [Google Scholar] [CrossRef]
- Garbim, J.; Laux, C.; Tedesco, T.; Braga, M.; Raggio, D. Atraumatic restorative treatment restorations performed in different settings: Systematic review and meta-analysis. Aust. Dent. J. 2021, 66, 430–443. [Google Scholar] [CrossRef]
- Maia, T.; Lima, T.; Vieira, W.; Blumenberg, C.; Agostini, B.; Nascimento, G.; Paranhos, L.R.; Menezes, M.d.S. Survival of atraumatic restorative treatment restorations in the elderly patients: A systematic review. Braz. Oral. Res. 2021, 35, e130. [Google Scholar] [CrossRef]
- Santos, A.P.; Moreira, I.K.D.; Scarpelli, A.C.; Pordeus, I.A.; Paiva, S.M.; Martins, C.C. Survival of Adhesive Restorations for Primary Molars: A Systematic Review and Meta-analysis of Clinical Trials. Pediatr. Dent. 2016, 38, 370–378. [Google Scholar] [PubMed]
- Yengopal, V.; Harneker, S.Y.; Patel, N.; Siegfried, N. Dental fillings for the treatment of caries in the primary dentition. Cochrane Database Syst. Rev. 2009, 2, CD004483. [Google Scholar] [CrossRef]
- Ruengrungsom, C.; Palamara, J.E.A.; Burrow, M.F. Comparison of A.R.T and conventional techniques on clinical performance of glass-ionomer cement restorations in load bearing areas of permanent and primary dentitions: A systematic review. J. Dent. 2018, 78, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Loguercio, A.D.; Hanzen, T.A.; Reis, A.; Rousson, V. Clinical efficacy of resin-based direct posterior restorations and glass-ionomer restorations—An updated meta-analysis of clinical outcome parameters. Dent. Mater. 2022, 38, e109–e135. [Google Scholar] [CrossRef]
- Tedesco, T.K.; Gimenez, T.; Floriano, I.; Montagner, A.F.; Camargo, L.B.; Calvo, A.F.B.; Morimoto, S.; Raggio, D.P. Scientific evidence for the management of dentin caries lesions in pediatric dentistry: A systematic review and network meta-analysis. PLoS ONE 2018, 13, e0206296. [Google Scholar] [CrossRef]
- Kielbassa, A.M.; Glockner, G.; Wolgin, M.; Glockner, K. Systematic review on highly viscous glass-ionomer cement/resin coating restorations (Part. I): Do they merge Minamata Convention and minimum intervention dentistry? Quint. Int. 2016, 47, 813–823. [Google Scholar] [CrossRef]
- Studart, L.; da Franca, C.; Colares, V. Atraumatic Restorative Treatment in permanent molars: A systematic review. Braz. J. Oral. Sci. 2015, 11, 36–41. [Google Scholar]
- Amorim, R.; Frencken, J.; Raggio, D.; Chen, X.; Hu, X.; Leal, S. Survival percentages of atraumatic restorative treatment (ART)restorations and sealants in posterior teeth: An updated systematic review and meta-analysis. Clin. Oral. Investig. 2018, 22, 2703–2725. [Google Scholar] [CrossRef]
- Raggio, D.; Hesse, D.; Lenzi, T.L.; Guglielmi, C.A.B.; Braga, M. Is Atraumatic restorative treatment an option for restoring occlusoproxi mal caries lesions in primary teeth? A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2013, 23, 435–443. [Google Scholar] [CrossRef]
- Mickenautsch, S.; Yengopal, V. Failure Rate of Direct High -Viscosity Glass—Ionomer Versus Hybrid Resin Composite Restorations in Posterior Permanent Teeth—A Systematic Review. Open Dent. J. 2015, 9, 438–448. [Google Scholar] [CrossRef][Green Version]
- Manisha, S.; Shetty, S.S.; Mehta, V.; SA, R.; Meto, A. A Comprehensive Evaluation of Zirconia-Reinforced Glass Ionomer Cement’s Effectiveness in Dental Caries: A Systematic Review and Network Meta-Analysis. Dent. J. 2023, 11, 211. [Google Scholar] [CrossRef]
- Jamali, Z.; Najafpour, E.; Ebrahim Adhami, Z.; Sighari Deljavan, A.; Aminabadi, N.A.; Shirazi, S. Does the length of dental procedure influence children’s behavior during and after treatment? A systematic review and critical appraisal. J. Dent. Res. Dent. Clin. Dent. Prospect. 2018, 12, 68–76. [Google Scholar] [CrossRef] [PubMed]
- Dias, A.G.A.; Magno, M.B.; Delbem, A.C.B.; Cunha, R.F.; Maia, L.C.; Pessan, J.P. Clinical performance of glass ionomer cement and composite resin in Class II restorations in primary teeth: A systematic review and meta-analysis. J. Dent. 2018, 73, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Chisini, L.A.; Collares, K.; Cademartori, M.G.; de Oliveira, L.J.C.; Conde, M.C.M.; Demarco, F.F.; Correa, M.B. Restorations in primary teeth: A systematic review on survival and reasons for failures. Int. J. Paediatr. Dent. 2018, 28, 123–139. [Google Scholar] [CrossRef] [PubMed]
- Kilpatrick, N.M.; Neumann, A. Durability of amalgam in the restoration of class II cavities in primary molars: A systematic review of the literature. Eur. Arch. Paediatr. Dent. 2007, 8, 5–13. [Google Scholar] [CrossRef]
| Author (year) | Title | Objective of the Study | Pico | Protocol Registration | Articles Included | Meta-Analysis | Databases | Search Strategy | Duplicate Elimination | Included Languages | Number of Reviewers | Inclusion Criteria | Exclusion Criteria | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Santamaría et al., 2020 [48] | How to Intervene in the Caries Process: Dentin Caries in Primary Teeth | To evaluate the treatment and material used in primary dentition to effectively treat dentin carious lesions | Yes | No | 18 | No | MEDLINE/PubMed | Yes | Not specified | English, Spanish | 6 | Yes | Yes | |
| Garbim et al., 2021 [49] | Atraumatic Restorative Treatment Restorations Performed in Different Settings: Systematic Review and Meta-analysis | To evaluate the atraumatic restorative treatment (ART) longevity in primary and permanent dentition. | Yes | Yes | 34 | Yes | PubMed/MEDLINE, Scopus, Web of Science, Open Grey | Yes | Yes | English, no restrictions | 3 | Yes | Yes | |
| Maia et al., 2021 [50] | Survival of Atraumatic Restorative Treatment Restorations in the Elderly Patients: A Systematic Review | To evaluate the atraumatic restorative treatment (ART) longevity in elderly patients. | Yes | Yes | 7 | No | PubMed/MEDLINE, Scopus, LILACS, SciELO, Embase, Web of Science, OpenGrey, OpenThesis | Yes | Yes | English, Portuguese, no restrictions | 2 | Yes | Yes | |
| Santos et al., 2016 [51] | Survival of Adhesive Restorations for Primary Molars: A Systematic Review and Meta-analysis of Clinical Trials | To evaluate the longevity and clinical performance of different adhesive restorative materials in primary molars. | Yes | Yes | 11 | Yes | Cochrane Oral Health Group’s Trials Register, PubMed/MEDLINE, Web of Science, Cochrane Library, LILACS, Clinical Trials—U.S. National Institute of Health, National Institute for Health and Clinical Excellence | Yes | Yes | English, no restrictions | 6 | Yes | Yes | |
| Yengopal et al., 2009 [52] | Dental Fillings for the Treatment of Caries in the Primary Dentition | To compare the outcomes of different dental materials used in restorations of carious lesions in primary dentition. | No | Yes | 3 | No | The Cochrane Oral Health Group’s Trials Register, PubMed Central, PubMed/Medline, EMBASE, SIGLE | Yes | Yes | English, no restrictions | 2 | Yes | Yes | |
| Ruengrungsom et al., 2018 [53] | Comparison of ART and Conventional Techniques on Clinical Performance of Glass-ionomer Cement Restorations in Load-bearing Areas of Permanent and Primary Dentitions: A Systematic Review | To observe the clinical performance of glass-ionomer cement in Classes I and II restorations using the ART techniques. | No | No | 67 | No | PubMed | Yes | Not specified | English | Not specified | Yes | Yes | |
| Heintze et al., 2022 [54] | Clinical Efficacy of Resin-based Direct Posterior Restorations and Glass-ionomer Restorations—An Updated Meta-analysis of Clinical Outcome Parameters | To evaluate the longevity of Class I and II restorations performed with resin-based materials and glass ionomers. | Yes | No | 62 | Yes | PubMed, SCOPUS | Yes | Not specified | English | 2 | Yes | Yes | |
| Tedesco et al., 2018 [55] | Scientific Evidence for the Management of Dentin Caries Lesions in Pediatric Dentistry: A Systematic Review and Network Meta-analysis | To observe the success rate and effectiveness of dentin carious lesion treatments in primary dentition. | Yes | Yes | 15 | Yes | MEDLINE/PubMed, Web of Science, Scopus | Yes | Yes | English, no restrictions | 3 | Yes | Yes | |
| Kielbassa et al., 2016 [56] | Systematic Review on Highly Viscous Glass-ionomer Cement/Resin Coating Restorations (Part I): Do They Merge Minamata Convention and Minimum-intervention Dentistry? | To evaluate the clinical performance of high-viscosity glass-ionomer cement/resin coating (hvGIC/RC) in class I and II. | Yes | No | 7 | No | PubMed, Cochrane Library, EBSCO, EMBASE, SCOPUS | No | Yes | English | 5 | Yes | Yes | |
| Studart et al., 2012 [57] | Atraumatic Restorative Treatment in Permanent Molars: A Systematic Review | To evaluate clinical performance of ART technique in permanent molars. | No | No | 24 | No | PubMed/MEDLINE, LILACS | No | Not specified | English, Portuguese, Spanish | 3 | Yes | Yes | |
| Amorim, 2018 [58] | Survival Percentages of Atraumatic Restorative Treatment (ART) Restorations and Sealants in Posterior Teeth: An Updated Systematic Review and Meta-analysis | To assess ART restorations and sealants survival rates and carious preventive effects in permanent and primary posterior teeth. | No | Yes | 43 | Yes | PubMed, EMBASE, LILACS, BBO, CNKI, VIP | Yes | Not specified | English, Dutch, Spanish, Portuguese, Chinese | 6 | Yes | Yes | |
| Raggio et al., 2012 [59] | Is Atraumatic Restorative Treatment an Option For Restoring Occlusal-proximal Caries Lesions in Primary Teeth? A Systematic Review and Meta-analysis | To evaluate if ART is a viable option for occlusal-proximal restorations in the primary dentition. | No | No | 3 | Yes | PubMed | Yes | Not specified | English | 3 | Yes | Yes | |
| Mickenautsch et al., 2015 [60] | Failure Rate of Direct High-Viscosity Glass-ionomer Versus Hybrid Resin Composite Restorations in Posterior Permanent Teeth—a Aystematic Review | To evaluate the success rates/longevity of high-viscosity glass-ionomer cement compared to hybrid composite resins in single/multi-surface restorations in permanent posterior teeth. | Yes | Yes | 6 | No | PubMed/Medline, CENTRAL (Cochrane Library), Directory of Open Access Journals (DOAJ), Biomed Central, IndMed, Sabinet, OpenSIGLE, GoogleScholar | Yes | Yes | English | 2 | Yes | Yes | |
| Author (year) | Material Type | Follow-Up | Quality Analysis | Risk of Bias | Tools/Data Analysis | Outcome | Conclusions | |||||||
| Santamaría et al., 2020 [48] | Preformed metal crowns, amalgam, composite resin, glass ionomer cement, and compomer | At least 12 months after intervention | Yes | Yes | PRISMA statement, Cochrane risk of bias tool, Mendeley software, ORCA/EFCD consensus workshop | The studies included compared different dentin carious lesions techniques and approaches, such as selective carious tissue removal, no carious tissue removal, atraumatic restorative treatment (ART), ultraconservative treatment (UCT), and no treatment of carious lesions. Also, results compared the performance of different restorative dental materials. | Due to insufficient evidence and limited quality, a conclusion could not be drawn. But in general, there is not an ideal single treatment that must be considered when managing dentin carious lesions in primary teeth. | |||||||
| Garbim et al., 2021 [49] | High-viscosity glass ionomer | 12 or 36 months | Yes | Yes | PRISMA guidelines 2020, RoB 2.0 tool—Cochrane Handbook for Systematic Reviews of Interventions, ROBINS-I tools, Begg’s Test, Rstudio, ART evaluation criteria, United States Public Health Service (USPHS), GemertSchriks criteria | Different brands of glass-ionomer cements were compared regarding ART longevity in primary and permanent dentition, as well as in occlusal and multi-surface restorations. | ART restorations seem to have long-term survivability, making them reliable treatments in both primary and permanent dentition. | |||||||
| Maia et al., 2021 [50] | Glass ionomer | 6 months–5 years | Yes | Yes | Joanna Briggs Institute’s Critical Appraisal Tool, PRISMA guidelines | Conventional and resin-modified glass ionomer cements (RMGIC) were compared in terms of ART survivability, evaluating wear, marginal defects, and need for replacement. | Even though it would be ideal to conduct more studies with longer follow-ups, ART showed positive results in terms of longevity in elderly patients. | |||||||
| Santos et al., 2016 [51] | Composite resin (CR), conventional glass-ionomer cement (GIC), resin-modified glass ionomer (RMGIC), silver-reinforced glass-ionomer cement, and compomer | 18, 24, 36 months | Yes | Yes | PRISMA guidelines, Reference Manager 12.03.0, modified version of the Jadad scale (0–6 points), comprehensive Meta-Analysis Program (Biostat, Englewood, N.J., USA), United States Public Health Service (U.S.PHS) | Results compared how five different restorative materials performed in Classes I and II in 3–10-year-old patients in different settings, with different types of isolations. | More randomized controlled trials are needed, but from this study, all materials performed well when used for restorations in primary molars, except the silver-reinforced glass-ionomer cement, which had the worst survival rate. Glass-ionomer cements did not show lower survival rates compared to resin-based materials. | |||||||
| Yengopal et al., 2009 [52] | Resin-modified glass ionomer, amalgam, compomer | Minimum 6 months | Yes | Yes | Cochrane Collaboration statistical guidelines, Cochrane Highly Sensitive Search Strategy (CHSSS), Cochrane Handbook for Systematic Reviews of Interventions 5.0.1, Chi2 test for heterogeneity, Ryge criteria | Resin-modified glass-ionomer cement compared to amalgam in Class II restorations. The clinical success was evaluated by considering surface texture, marginal integrity, axial contour, wear, restoration placement, secondary caries, restoration fracture, and staining. | Due to the absence of scientific evidence, it is not possible to recommend a specific material. The three trials did not show any significant differences regarding the outcomes. | |||||||
| Ruengrungsom et al., 2018 [53] | Glass-ionomer cements | >1 year | No | Yes | ROBINS-I, PRISMA flow diagram | Comparison of single-/multi-surface restorations in load-bearing areas in permanent and primary teeth performed with conventional GIC technique versus ART technique and reasons for failure. | The conventional GIC technique showed better results compared to the ART technique, and it is preferred in primary dentition (lower annual failure rates). In general, multi-surface restorations showed greater failure rates compared to single-surface restorations. The main causes of failures were fracture and dislodgment. The RMGIC conventional technique showed promising results in restoring proximal cavities. | |||||||
| Heintze et al., 2022 [54] | Resin composite, compomer, or GIC restorations (high-viscous glass ionomer and resin-modified glass ionomer) | >2 years | No | Yes | Ryge criteria, Cochrane Collaboration’s tool | In the analysis, materials were divided into microhybrid, nanohybrid, and hybrid. Regarding composite filler and bulk fill materials, GICs and compomers were treated as separate categories. The conditioning and adhesive systems were: etch and rinse two and three steps, self-etch two and three steps, enamel etch and enamel bonding, and no etching/adhesive systems (polyacrid acid and GICs). Curing time ranged from 10–60 s. Follow-up periods ranged from 2–5 years. | Resin showed better results in terms of longevity compared to compomers and GICs due to fracture and excessive wear. | |||||||
| Tedesco et al., 2018 [55] | Low- and high-viscosity glass-ionomer cement, resin-modified glass-ionomer cement (RMGIC), resin composite, amalgam | >1 year | Yes | Yes | Cochrane Handbook for Systematic Reviews of Interventions, ROBINS-I, PRISMA-NMA extension, GRADE tool, I2 test, R package “stats” version 2.15.3 | Comparison between conventional restorative treatment (CRT), atraumatic restorative treatment (ART), non-restorative caries treatment (NRCT), and ultraconservative caries treatment (UCT) in occlusal/occlusal-proximal surfaces in primary dentition. | The success of the treatment depends on the depth of progression of the caries and the surfaces involved. Without information about the depth of progression of the carious lesions, the CRT technique with compomer showed the best results followed by the ART technique. The Hall technique (stainless-steel crowns) performed best in occlusal-proximal surfaces. Application of 38% silver diamine fluoride (SDF) twice per year showed a great increase in caries reduction. In the end, it is not possible to recommend the best treatment option due to few studies with a high risk of bias. | |||||||
| Kielbassa et al., 2016 [56] | High-viscosity glass-ionomer cement/resin coating | 6 months–6 years | Yes | Yes | Oxford quality-scoring system, PRISMA guidelines, US Public Health Service (USPHS) criteria | Resilience, wear, durability, abrasion resistance, chipping, color match, and marginal adaptation were considered when assessing the clinical performance of hvGIC/RC in Class I and II restorations. | Short–medium-term hvGIC/RC systems showed promising results in terms of abrasion resistance, retention rates, and clinical fracture toughness with high survival rates in both Class I and II restorations, although less longevity was shown in Class II compared to Class I. | |||||||
| Studart et al., 2012 [57] | Resin-modified glass-ionomer cements, low- and high-viscosity glass-ionomer cements, amalgam | >4 months | No | No | Not specified | Different ART restorative materials and methods in single- and multi-surface cavities in permanent molars were compared. | ART showed high survival rates in single (3 years) and multi-surface (2 years) restorations. Longevity in multi-surface restorations was lower compared to single surface. However more studies are required to draw conclusions. | |||||||
| Amorim, 2018 [58] | Low- and high-viscosity glass-ionomer cements | >1 year | Yes | Yes | PRISMA statement, I2 values, Cochrane Research Group | The survival rates of single-surface ART restorations in permanent posterior teeth were 87.1% over 3 years and 77% for multi-surface over 5 years. In primary dentition for single-surface restorations, the survival rate was 94.3%, and for multi-surface restorations, it was 65.4% over 2 years. The mean annual dentine carious lesion failure rates were 0.9% over 3 years and 1.9% over 5 years. | Both dentine carious lesion preventive effects and survival rates over 2–5 years of ART restorations in primary and permanent dentitions were relatively high, with the exception of restorations in primary posterior teeth over 2-year period, which showed lower survival rates. In general, multi-surface restorations present lower survival rates compared to a single surface. | |||||||
| Raggio et al., 2012 [59] | High-viscosity glass-ionomer cement | >6 months | Yes | No | Comprehensive Meta Analysis 2.2.064, US Public Health Service (USPHS) criteria | ART with high-viscosity glass-ionomer cements and conventional restorative techniques with amalgam or composite resin were compared, resulting in 48.7–88.9% survival rates in ART restorations and 42.9–100% in conventional restorations. | ART and conventional restoration techniques showed similar success rates and are a viable option for occlusal-proximal restorations in primary molars. More studies on factors such as pulp damage and caries lesion progression are needed. | |||||||
| Mickenautsch et al., 2015 [60] | High-viscosity glass-ionomers, hybrid resin composites | >1 year | No | No | Australian New Zealand Clinical Trials Registry, Clinical Trials US, EU Clinical Trials Register, metaRegister of Controlled Trials (mRCT), South African National Clinical Trials Register, WHO Clinical Trials, IADR abstracts, International Poster Journal of Dentistry and Oral Medicine, Rev Man 4.2, Berger VW. Selection bias and covariate imbalances in randomised clinical trials. Chichester, UK: John Wiley & Sons, Ltd. 2005, ITC software, I2 test, Cochrane’s Q-test | The statistical comparison between hvGIC and HRC in Class I and II restorations in permanent posterior teeth after 24–60 months showed no differences. | No final judgements can be made due to poor scientific evidence on this comparison. More studies are needed to draw conclusions. | |||||||
| Criteria | Was an ‘a Priori’ Design Provided? | Was There Duplicate Study Selection and Data Extraction? | Was a Comprehensive Literature Search Performed? | Was the Status of Publication (i.e., Grey Literature) Used as an Inclusion Criteria? | Was a List Od Studies (Included and Excluded) Provided? | Were the Characteristics of the Included Studies Provided? | Was the Scientific Quality of the Included Studies Assessed and Documented? | Was the Scientific Quality of the Included Studies Used Approprietely in Formulating Conclusions? | Were the Methods Used to Combine the Findings of Studies Appropriate? | Was the Likelihood of Publication Bias Assessed? | Was the Conflict of Interest Stated? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Author/Year | |||||||||||
| 1. Santamaría et al., 2020 [48] | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 2. Garbim et al., 2021 [49] | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 3. Maia et al., 2021 [50] | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 4. Santos et al., 2016 [51] | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 5. Yengopal et al., 2009 [52] | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 6. Ruengrungsom et al., 2018 [53] | No | No | Yes | No | Yes | Yes | No | Yes | No | Yes | No |
| 7. Heintze et al., 2022 [54] | No | No | Yes | No | Yes | Yes | No | Yes | No | Yes | No |
| 8. Tedesco et al., 2018 [55] | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 9. Kielbassa et al., 2016 [56] | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | Yes | No |
| 10. Studart et al., 2012 [57] | No | No | No | No | Yes | Yes | No | Yes | No | No | No |
| 11. Amorim et al., 2018 [58] | No | No | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 12. Raggio et al., 2012 [59] | No | No | Yes | No | Yes | Yes | Yes | Yes | No | No | No |
| 13. Mickenautsch et al., 2015 [60] | No | Yes | Yes | Yes | Yes | Yes | No | Yes | No | No | No |
| Phase 2 | Phase 3 | ||||
|---|---|---|---|---|---|
| Criteria | Study Eligibility | Identification and Selection of Studies | Data Collection and Study Appraisal | Synthesis and Findings | Risk of Bias in the Review |
| Author/Year | |||||
| 1. Santamaría et al., 2020 [48] | ? | ||||
| 2. Garbim et al., 2021 [49] | |||||
| 3. Maia et al., 2021 [50] | ? | ||||
| 4. Santos et al., 2016 [51] | |||||
| 5. Yengopal et al., 2009 [52] | ? | ||||
| 6. Ruengrungsom et al., 2018 [53] | |||||
| 7. Heintze et al., 2022 [54] | ? | ||||
| 8. Tedesco et al., 2018 [55] | |||||
| 9. Kielbassa et al., 2016 [56] | |||||
| 10. Studart et al., 2012 [57] | |||||
| 11. Amorim et al., 2018 [58] | ? | ||||
| 12. Raggio et al., 2012 [59] | |||||
| 13. Mickenautsch et al., 2015 [60] | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panetta, A.; Lopes, P.; Novaes, T.F.; Rio, R.; Fernandes, G.V.O.; Mello-Moura, A.C.V. Evaluating Glass Ionomer Cement Longevity in the Primary and Permanent Teeth—An Umbrella Review. J. Funct. Biomater. 2024, 15, 48. https://doi.org/10.3390/jfb15020048
Panetta A, Lopes P, Novaes TF, Rio R, Fernandes GVO, Mello-Moura ACV. Evaluating Glass Ionomer Cement Longevity in the Primary and Permanent Teeth—An Umbrella Review. Journal of Functional Biomaterials. 2024; 15(2):48. https://doi.org/10.3390/jfb15020048
Chicago/Turabian StylePanetta, Alessandro, Pedro Lopes, Tatiane Fernandes Novaes, Rute Rio, Gustavo Vicentis Oliveira Fernandes, and Anna Carolina Volpi Mello-Moura. 2024. "Evaluating Glass Ionomer Cement Longevity in the Primary and Permanent Teeth—An Umbrella Review" Journal of Functional Biomaterials 15, no. 2: 48. https://doi.org/10.3390/jfb15020048
APA StylePanetta, A., Lopes, P., Novaes, T. F., Rio, R., Fernandes, G. V. O., & Mello-Moura, A. C. V. (2024). Evaluating Glass Ionomer Cement Longevity in the Primary and Permanent Teeth—An Umbrella Review. Journal of Functional Biomaterials, 15(2), 48. https://doi.org/10.3390/jfb15020048









