Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An In Vitro Study on Polyurethane Foam Sheets
Abstract
1. Introduction
2. Materials and Methods
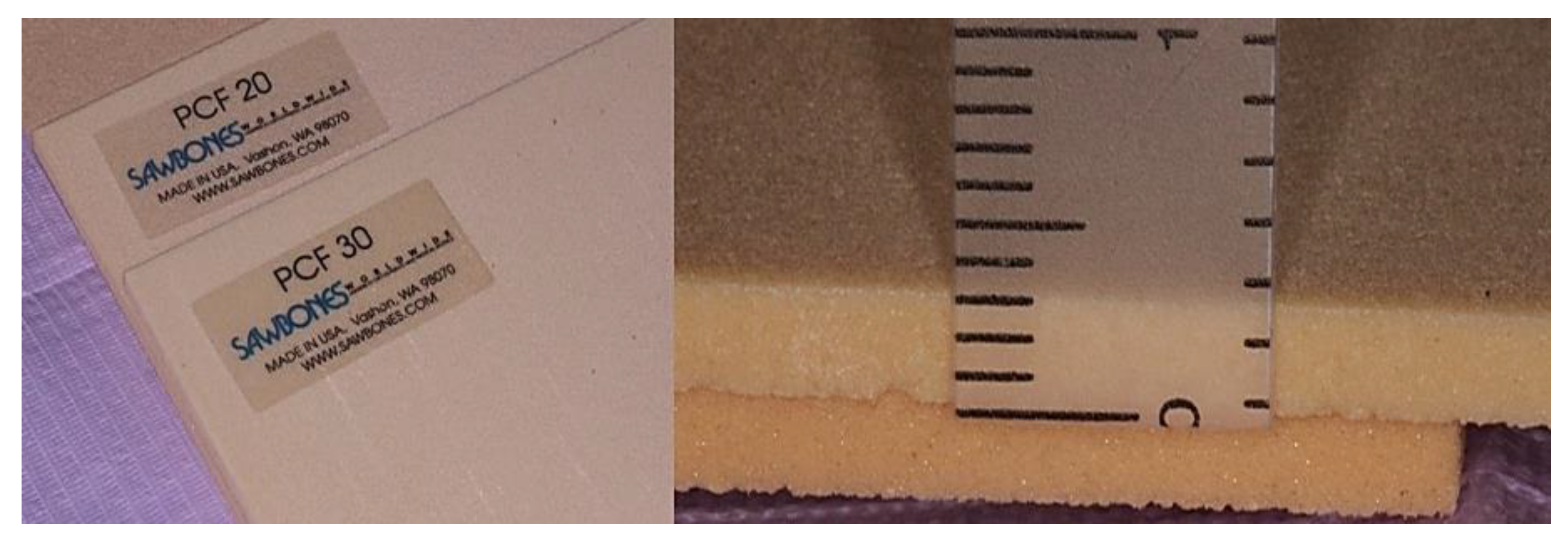
2.1. Implants, Polyurethane Foam Sheets and Study Design
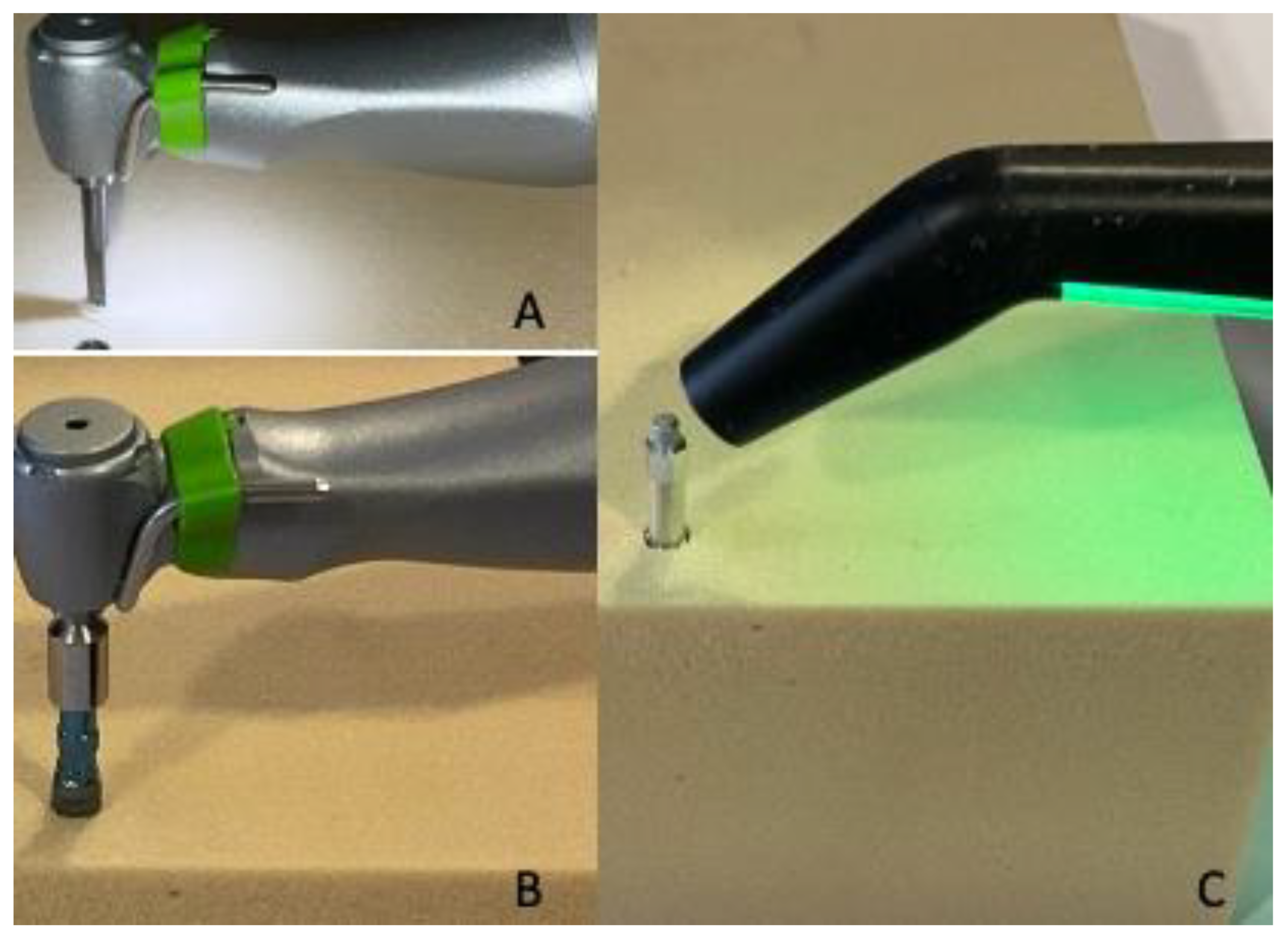
2.2. Drilling Protocol
2.3. Statistical Analysis
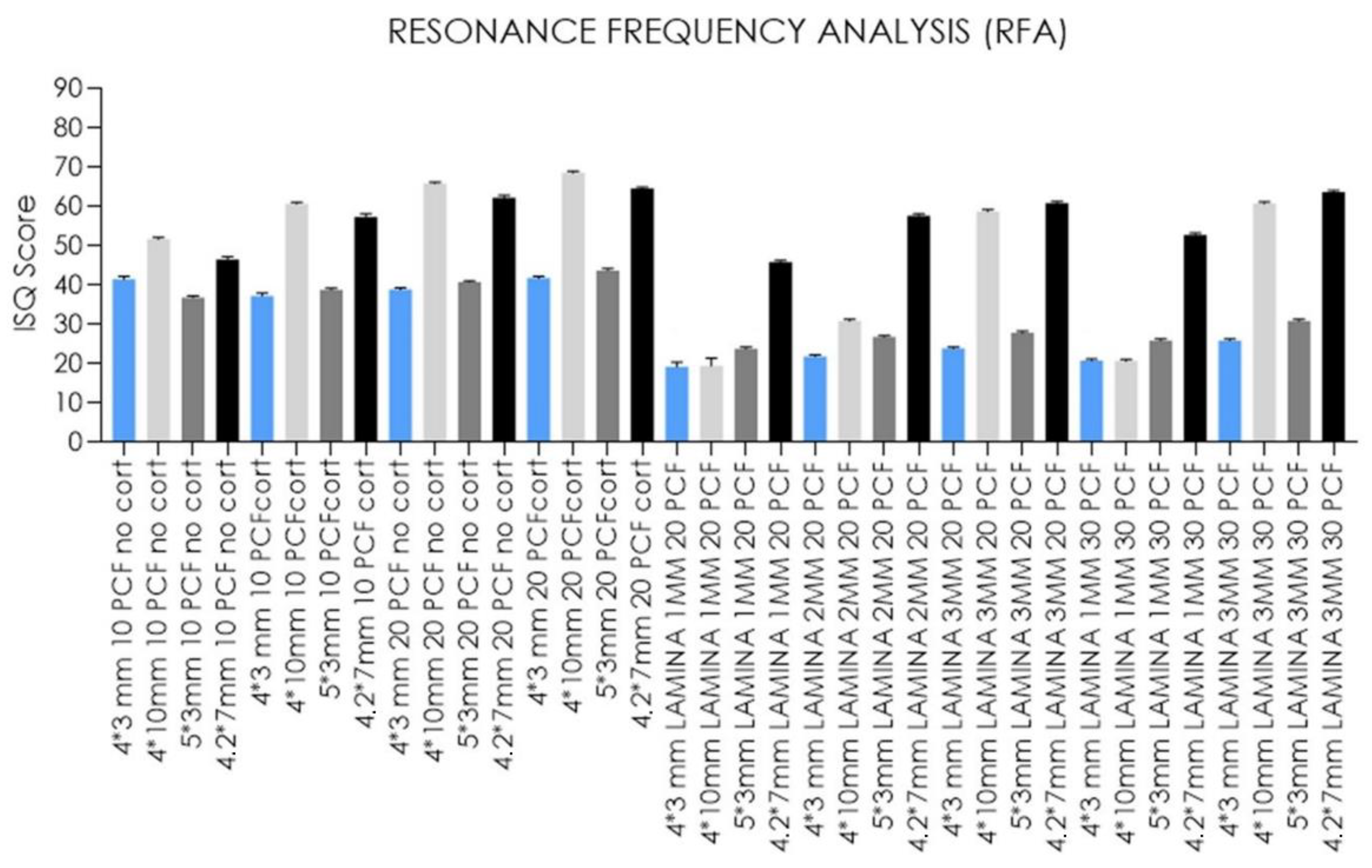
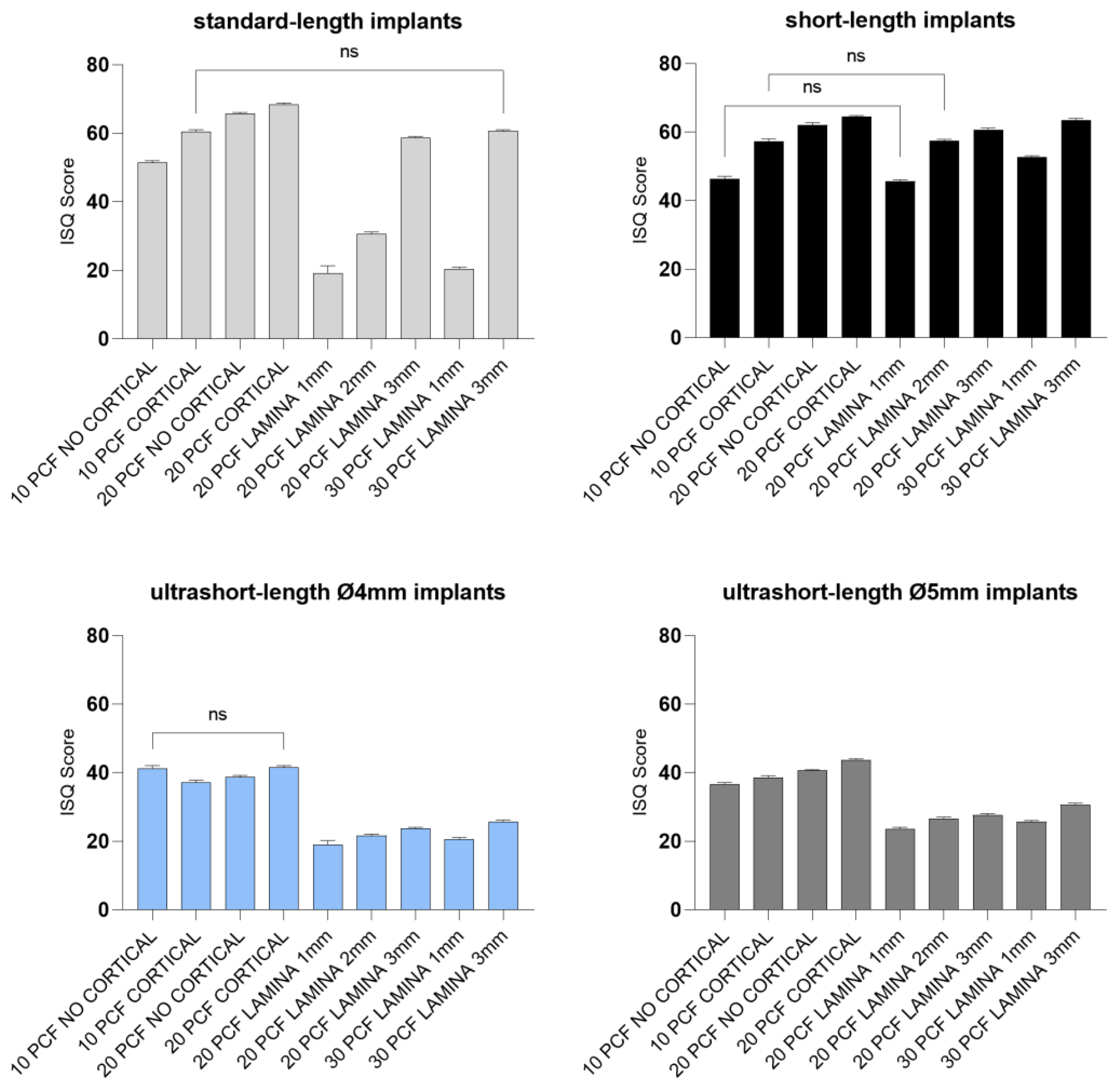
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Papaspyridakos, P.; De Souza, A.; Vazouras, K.; Gholami, H.; Pagni, S.; Weber, H.P. Survival rates of short dental implants (≤6 mm) compared with implants longer than 6 mm in posterior jaw areas: A meta-analysis. Clin. Oral Implants Res. 2018, 29, 8–20. [Google Scholar] [CrossRef] [PubMed]
- Ravidà, A.; Wang, I.C.; Sammartino, G.; Barootchi, S.; Tattan, M.; Troiano, G.; Laino, L.; Marenzi, G.; Covani, U.; Wang, H.L. Prosthetic Rehabilitation of the Posterior Atrophic Maxilla, Short (≤6 mm) or Long (≥10 mm) Dental Implants? A Systematic Review, Meta-analysis, and Trial Sequential Analysis: Naples Consensus Report Working Group A. Implant Dent. 2019, 28, 590–602. [Google Scholar] [CrossRef] [PubMed]
- Fan, T.; Li, Y.; Deng, W.W.; Wu, T.; Zhang, W. Short Implants (5 to 8 mm) Versus Longer Implants (>8 mm) with Sinus Lifting in Atrophic Posterior Maxilla: A Meta-Analysis of RCTs. Clin. Implant Dent. Relat. Res. 2017, 19, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Pauletto, P.; Carrera, E.R.; Gonçalves TM, S.V.; Philippi, A.G.; Donos, N.; Mezzomo, L.A. Fixed and Removable Full-Arch Restorations Supported by Short (≤8-mm) Dental Implants in the Mandible: A Systematic Review and Meta-Analysis. Int. J. Oral Maxillofac. Implants 2019, 34, 873–885. [Google Scholar] [CrossRef]
- Yu, X.; Xu, R.; Zhang, Z.; Yang, Y.; Deng, F. A Meta-Analysis Indicating Extra-Short Implants (≤6 Mm) as an Alternative to Longer Implants (≥8 Mm) with Bone Augmentation. Sci. Rep. 2021, 11, 8152. [Google Scholar] [CrossRef]
- Amine, M.; Guelzim, Y.; Benfaida, S.; Bennani, A.; Andoh, A. Short implants (5–8 mm) vs. long implants in augmented bone and their impact on peri-implant bone in maxilla and/or mandible: Systematic review. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 133–142. [Google Scholar] [CrossRef]
- Chen, S.; Ou, Q.; Wang, Y.; Lin, X. Short implants (5–8 mm) vs long implants (≥10 mm) with augmentation in atrophic posterior jaws: A meta-analysis of randomised controlled trials. J. Oral Rehabil. 2019, 46, 1192–1203. [Google Scholar] [CrossRef]
- Bitaraf, T.; Keshtkar, A.; Rokn, A.R.; Monzavi, A.; Geramy, A.; Hashemi, K. Comparing short dental implant and standard dental implant in terms of marginal bone level changes: A systematic review and meta-analysis of randomized controlled trials. Clin. Implant Dent. Relat. Res. 2019, 21, 796–812. [Google Scholar] [CrossRef]
- Ravidà, A.; Wang, I.C.; Barootchi, S.; Askar, H.; Tavelli, L.; Gargallo-Albiol, J.; Wang, H.L. Meta-analysis of randomized clinical trials comparing clinical and patient-reported outcomes between extra-short (≤6 mm) and longer (≥10 mm) implants. J. Clin. Periodontol. 2019, 46, 118–142. [Google Scholar] [CrossRef]
- Yan, Q.; Wu, X.; Su, M.; Hua, F.; Shi, B. Short implants (≤6 mm) versus longer implants with sinus floor elevation in atrophic posterior maxilla: A systematic review and meta-analysis. BMJ 2019, 9, e029826. [Google Scholar] [CrossRef]
- Monje, A.; Fu, J.-H.; Chan, H.-L.; Suarez, F.; Galindo-Moreno, P.; Catena, A.; Wang, H.-L. Do Implant Length and Width Matter for Short Dental Implants (<10 Mm)? A Meta-Analysis of Prospective Studies. J. Periodontol. 2013, 84, 1783–1791. [Google Scholar] [CrossRef] [PubMed]
- Lozano-Carrascal, N.; Anglada-Bosqued, A.; Salomó-Coll, O.; Hernández-Alfaro, F.; Wang, H.L.; Gargallo-Albiol, J. Short implants (<8 mm) versus longer implants (≥8 mm) with lateral sinus floor augmentation in posterior atrophic maxilla: A meta-analysis of RCT’s in humans. Med. Oral Patol. Oral Cir. Bucal 2020, 25, 168–179. [Google Scholar] [CrossRef]
- Lombardo, G.; Signoriello, A.; Marincola, M.; Nocini, P.F. Assessment of Peri-Implant Soft Tissues Conditions around Short and Ultra-Short Implant-Supported Single Crowns: A 3-Year Retrospective Study on Periodontally Healthy Patients and Patients with a History of Periodontal Disease. Int. J. Environ. Res. Public Health 2020, 17, 9354. [Google Scholar] [CrossRef] [PubMed]
- Pistilli, R.; Zucchelli, G.; Barausse, C.; Bonifazi, L.; Karaban, M.; Gasparro, R.; Felice, P. Minimally Invasive Fixed Rehabilitation of an Extremely Atrophic Posterior Mandible Using 4-Mm Ultrashort Implants: A Case Report with a 7-Year Follow-Up. Int. J. Periodontics Restor. Dent. 2020, 40, e235–e240. [Google Scholar] [CrossRef] [PubMed]
- Felice, P.; Barausse, C.; Pistilli, R.; Ippolito, D.R.; Esposito, M. Five-Year Results from a Randomised Controlled Trial Comparing Prostheses Supported by 5-Mm Long Implants or by Longer Implants in Augmented Bone in Posterior Atrophic Edentulous Jaws. Int. J. Oral Implantol. 2019, 12, 25–37. [Google Scholar]
- Comuzzi, L.; Iezzi, G.; Piattelli, A.; Tumedei, M. An In Vitro Evaluation, on Polyurethane Foam Sheets, of the Insertion Torque (IT) Values, Pull-Out Torque Values, and Resonance Frequency Analysis (RFA) of NanoShort Dental Implants. Polymers 2019, 11, 1020. [Google Scholar] [CrossRef]
- Pistilli, R.; Barausse, C.; Checchi, L.; Felice, P. Rehabilitation of the Atrophic Posterior Mandible with Short (4-Mm) Implants: A Case Report. Int. J. Periodontics Restor. Dent. 2014, 34, 713–718. [Google Scholar] [CrossRef]
- Comuzzi, L.; Tumedei, M.; De Angelis, F.; Lorusso, F.; Piattelli, A.; Iezzi, G. Influence of the dental implant macrogeometry and threads design on primary stability: An in vitro simulation on artificial bone blocks. Comput. Methods Biomech. Biomed. Eng. 2021, 24, 1242–1250. [Google Scholar] [CrossRef]
- Malchiodi, L.; Caricasulo, R.; Cucchi, A.; Vinci, R.; Agliardi, E.; Gherlone, E. Evaluation of Ultrashort and Longer Implants with Microrough Surfaces: Results of a 24- to 36-Month Prospective Study. Int. J. Oral Maxillofac. Implants 2017, 32, 171–179. [Google Scholar] [CrossRef]
- Maglione, M.; Bevilacqua, L.; Dotto, F.; Costantinides, F.; Lorusso, F.; Scarano, A. Observational Study on the Preparation of the Implant Site with Piezosurgery vs. Drill: Comparison between the Two Methods in terms of Postoperative Pain, Surgical Times, and Operational Advantages. BioMed Res. Int. 2019, 2019, 848–3658. [Google Scholar] [CrossRef]
- Carosi, P.; Arcuri, L.; Pinto, A.; Agrestini, C.; Laureti, M.; Ferrigno, N. Rehabilitation of a Severe Man-dibular Atrophy with Four Millimeter Extra-Short Implant and Guided Bone Regeneration (GBR): Case Report with 7-Years Follow-Up. J. Biol. Regul. Homeost. Agents 2020, 34, 35–43. [Google Scholar] [PubMed]
- Kulkarni, V.; Uttamani, J.R.; Asar, N.V.; Nares, S.; Tözüm, T.F. Evidence-Based Clinical Outcomes of Immediate and Early Loading of Short Endosseous Dental Implants: A Meta-Analysis. Int. J. Oral Maxillofac. Implants 2021, 36, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Seemann, R.; Marincola, M.; Seay, D.; Perisanidis, C.; Barger, N.; Ewers, R. Preliminary Results of Fixed, Fiber-Reinforced Resin Bridges on Four 4- × 5-Mm Ultrashort Implants in Compromised Bony Sites: A Pilot Study. J. Oral Maxillofac. Surg. 2015, 73, 630–640. [Google Scholar] [CrossRef] [PubMed]
- Pierfelice, T.V.; D’Amico, E.; Iezzi, G.; Piattelli, A.; Di Pietro, N.; D’Arcangelo, C.; Comuzzi, L.; Petrini, M. Nanoporous Titanium Enriched with Calcium and Phosphorus Promotes Human Oral Osteoblast Bioactivity. Int. J. Environ. Res. Public Health 2022, 19, 6212. [Google Scholar] [CrossRef]
- Lazzara, R.J. Bone response to dual acid-etched and machined titanium implant surfaces. In Bone Engineering; Davies, J.E., Ed.; EM Squared Incorporated: Toronto, ON, Canada, 2000; pp. 381–390. [Google Scholar]
- Park, J.Y.; Gemmell, C.H.; Davies, J.E. Platelet interactions with titanium: Modulation of platelet activity by surface topography. Biomaterials 2001, 22, 2671–2682. [Google Scholar] [CrossRef]
- Cordioli, G.; Majzoub, Z.; Piattelli, A.; Scarano, A. Removal Torque and Histomorphometric Investigation of 4 Different Titanium Surfaces: An Experimental Study in the Rabbit Tibia. Int. J. Oral Maxillofac. Implants 2000, 15, 668–674. [Google Scholar]
- Klokkevold, P.R.; Johnson, P.; Dadgostari, S.; Caputo, A.; Davies, J.E.; Nishimura, R.D. Early endosseous integration enhanced by dual acid etching of titanium: A torque removal study in the rabbit. Clin. Oral Implants Res. 2001, 12, 350–357. [Google Scholar] [CrossRef]
- Scarano, A.; Piattelli, A.; Quaranta, A.; Lorusso, F. Bone Response to Two Dental Implants with Different Sandblasted/Acid-Etched Implant Surfaces: A Histological and Histomorphometrical Study in Rabbits. BioMed Res. Int. 2017, 2017, 8724951. [Google Scholar] [CrossRef]
- Jemat, A.; Ghazali, M.J.; Razali, M.; Otsuka, Y. Surface Modifications and Their Effects on Titanium Dental Implants. BioMed Res. Int. 2015, 6, 1–11. [Google Scholar] [CrossRef]
- Di Stefano, D.A.; Arosio, P.; Gastaldi, G.; Gherlone, E. The insertion torque-depth curve integral as a measure of implant primary stability: An in vitro study on polyurethane foam blocks. J. Prosthet. Dent. 2018, 120, 706–714. [Google Scholar] [CrossRef]
- Tsolaki, I.N.; Tonsekar, P.P.; Najafi, B.; Drew, H.J.; Sullivan, A.J.; Petrov, S.D. Comparison of Osteotome and Conventional Drilling Techniques for Primary Implant Stability: An In Vitro Study. J. Oral Implantol. 2016, 42, 321–325. [Google Scholar] [CrossRef] [PubMed]
- García-Braz, S.H.; Prados-Privado, M.; Zanatta, L.C.S.; Calvo-Guirado, J.L.; Prados-Frutos, J.C.; Gehrke, S.A. A Finite Element Analysis to Compare Stress Distribution on Extra-Short Implants with Two Different Internal Connections. J. Clin. Med. 2019, 8, 1103. [Google Scholar] [CrossRef] [PubMed]
- Romanos, G.E.; Bastardi, D.J.; Moore, R.; Kakar, A.; Herin, Y.; Delgado-Ruiz, R.A. In Vitro Effect of Drilling Speed on the Primary Stability of Narrow Diameter Implants with Varying Thread Designs Placed in Different Qualities of Simulated Bone. Materials 2019, 12, 1350. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Tumedei, M.; Aramburú Júnior, J.; Treichel, T.L.E.; Kolerman, R.; Lepore, S.; Piattelli, A.; Iezzi, G. Histological and Histomorphometrical Evaluation of a New Implant Macrogeometry. A Sheep Study. Int. J. Environ. Res. Public Health 2020, 17, 3477. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Ramírez-Fernandez, M.P.; Granero Marín, J.M.; Barbosa Salles, M.; Del Fabbro, M.; Calvo Guirado, J.L. A Comparative Evaluation between Aluminium and Titanium Dioxide Microparticles for Blasting the Surface Titanium Dental Implants: An Experimental Study in Rabbits. Clin. Oral Implants Res. 2018, 29, 802–807. [Google Scholar] [CrossRef]
- Anitua, E.; Piñas, L.; Orive, G. Retrospective Study of Short and Extra-Short Implants Placed in Posterior Regions: Influence of Crown-to-Implant Ratio on Marginal Bone Loss. Clin. Implant Dent. Relat. Res. 2015, 17, 102–110. [Google Scholar] [CrossRef]
- Schimmel, M.; Müller, F.; Suter, V.; Buser, D. Implants for Elderly Patients. Periodontology 2000 2017, 73, 228–240. [Google Scholar] [CrossRef]
- Urdaneta, R.A.; Daher, S.; Leary, J.; Emanuel, K.M.; Chuang, S.-K. The Survival of Ultrashort Locking-Taper Implants. Int. J. Oral Maxillofac. Implants 2012, 27, 644–654. [Google Scholar]
- Gonçalves, T.M.S.V.; Bortolini, S.; Martinolli, M.; Alfenas, B.F.M.; Peruzzo, D.C.; Natali, A.; Berzaghi, A.; Garcia, R.C.M.R. Long-Term Short Implants Performance: Systematic Review and Meta-Analysis of the Essential Assessment Parameters. Braz. Dent. J. 2015, 26, 325–336. [Google Scholar] [CrossRef]
- De Oliveira, G.J.P.L.; Barros-Filho, L.A.B.; Barros, L.A.B.; Queiroz, T.P.; Marcantonio, E. In vitro evaluation of the primary stability of short and conventional implants. J. Oral Implantol. 2016, 42, 458–463. [Google Scholar] [CrossRef]
- Tumedei, M.; Piattelli, A.; Falco, A.; De Angelis, F.; Lorusso, F.; Di Carmine, M.; Iezzi, G. An in vitro evaluation on polyurethane foam sheets of the insertion torque, removal torque values, and resonance frequency analysis (RFA) of a self-tapping threads and round apex implant. Cell. Polym. 2021, 40, 20–30. [Google Scholar] [CrossRef]
- Romanos, G.E.; Delgado-Ruiz, R.A.; Sacks, D.; Calvo-Guirado, J.L. Influence of the implant diameter and bone quality on the primary stability of porous tantalum trabecular metal dental implants: An in vitro biomechanical study. Clin. Oral Implants Res. 2018, 29, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Marquezan, M.; Osório, A.; Sant’Anna, E.; Souza, M.M.; Maia, L. Does Bone Mineral Density Influence the Primary Stability of Dental Implants? A Systematic Review. Clin. Oral Implants Res. 2012, 23, 767–774. [Google Scholar] [CrossRef] [PubMed]
- Herekar, M.; Sethi, M.; Ahmad, T.; Fernandes, A.S.; Patil, V.; Kulkarni, H. A Correlation between Bone (B), Insertion Torque (IT), and Implant Stability (S): BITS Score. J. Prosthet. Dent. 2014, 112, 805–810. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Kniha, K.; Heussen, N.; Hölzle, F.; Modabber, A. Effects on Primary Stability of Three Different Techniques for Implant Site Preparation in Synthetic Bone Models of Different Densities. Br. J. Oral Maxillofac. Surg. 2016, 54, 980–986. [Google Scholar] [CrossRef]
- Misch, C.E. Bone density: A key determinant for clinical success. Contemp. Implant Dent. 1999, 8, 109–118. [Google Scholar]
- Afrashtehfar, K.I.; Katsoulis, J.; Koka, S.; Igarashi, K. Single versus splinted short implants at sinus augmented sites: A systematic review and meta-analysis. J. Stomatol. Oral Maxillofac. Surg. 2021, 122, 303–310. [Google Scholar] [CrossRef]





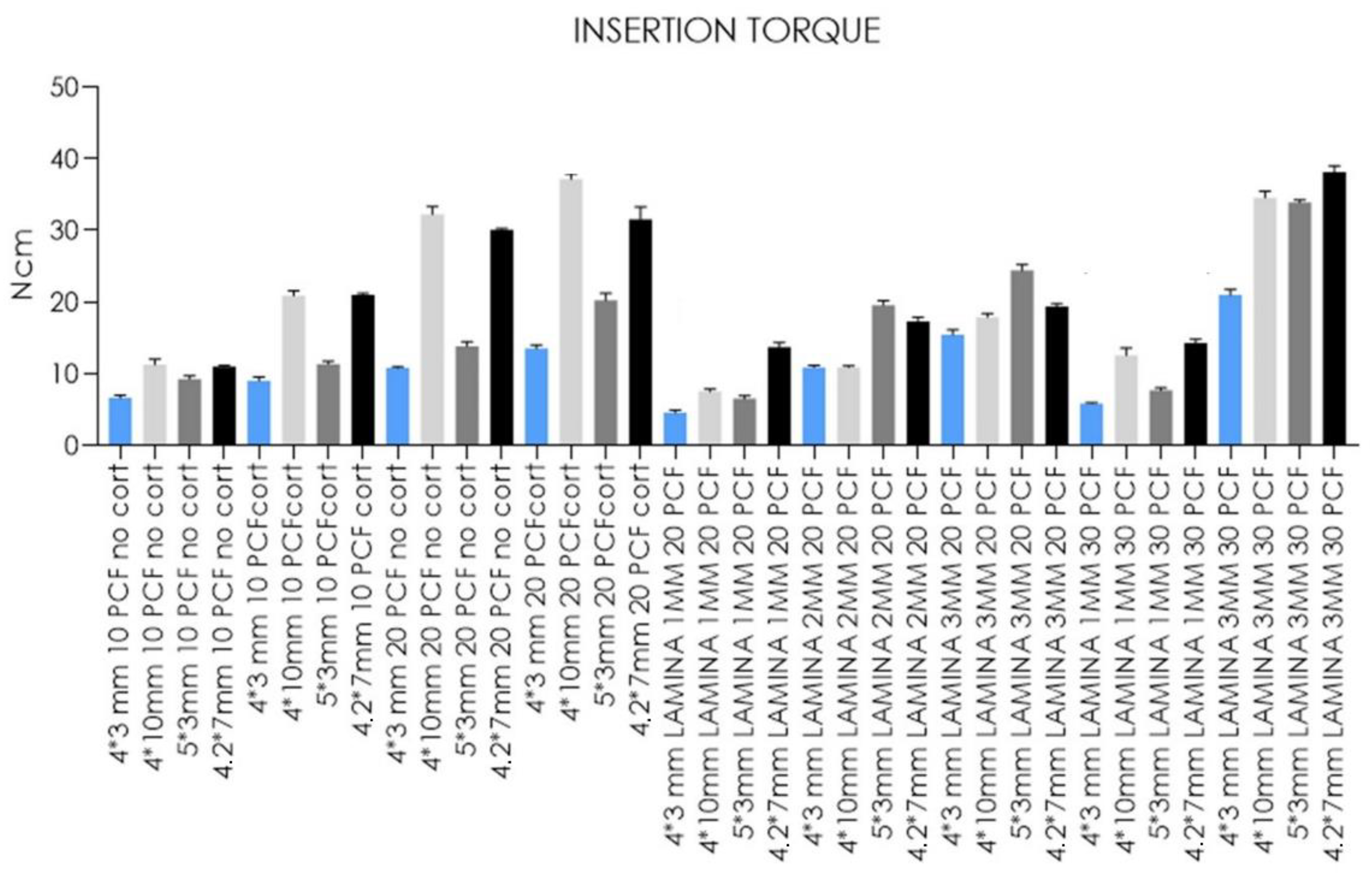
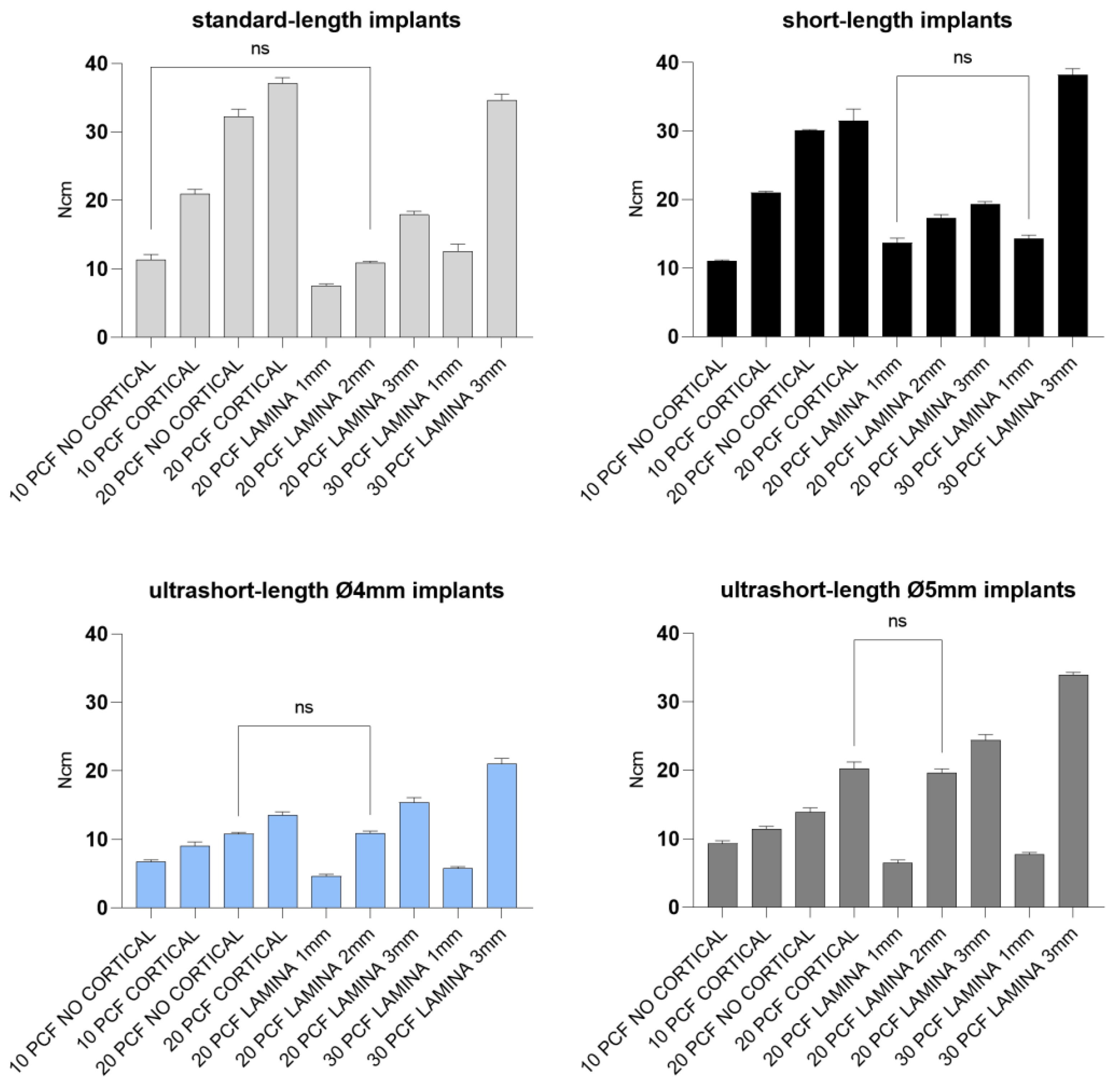

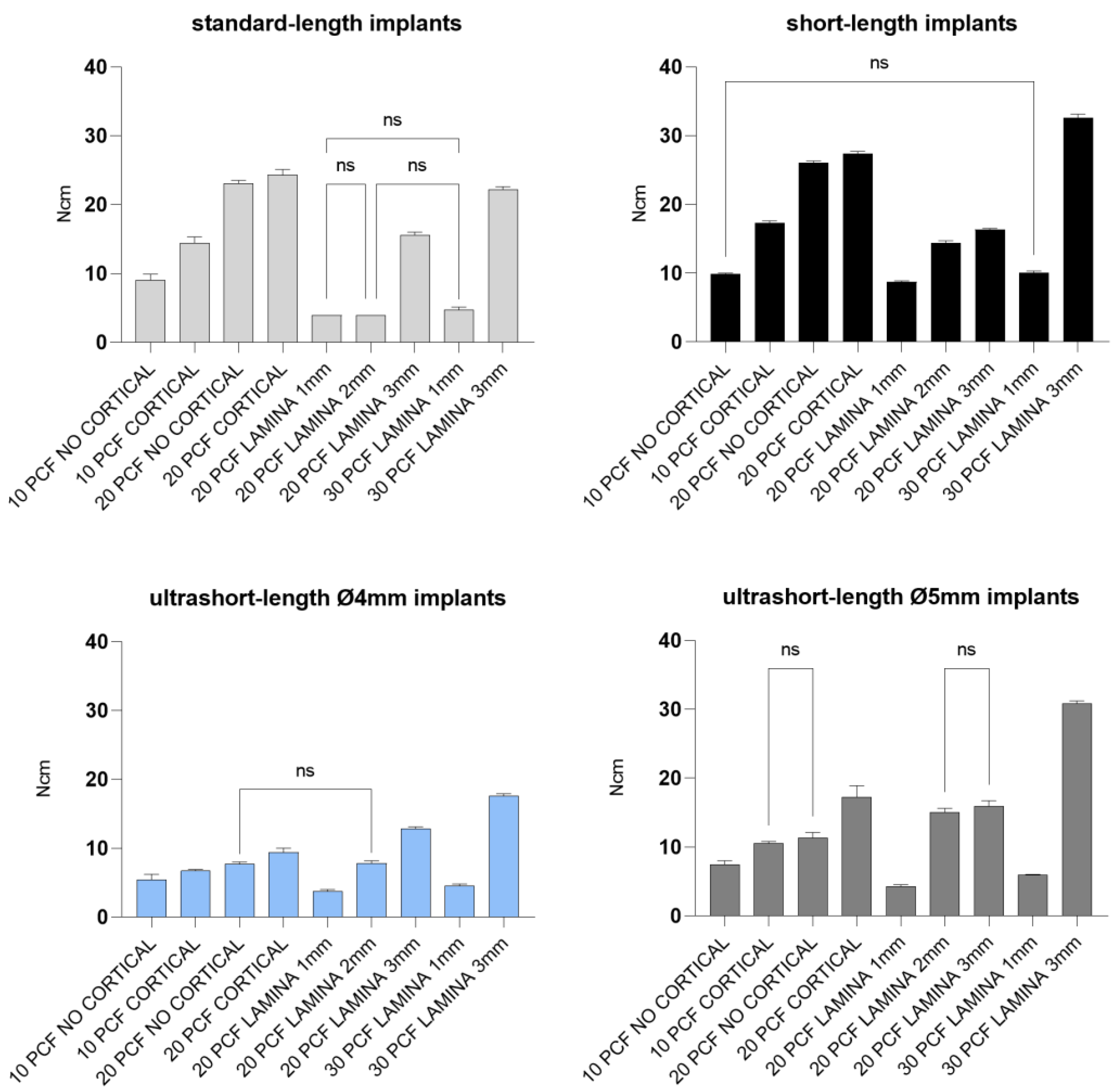
| IT | 10 PCF | 20 PCF | 20 PCF | 20 PCF | 20 PCF | 30 PCF | 30 PCF | |||||||||||||||||||||||||||||
| BLOCK NO CORT | BLOCK CORT | BLOCK NO CORT | BLOCK CORT | LAMINA 1 MM | LAMINA 2 MM | LAMINA 3 MM | LAMINA 1 MM | LAMINA 3 MM | ||||||||||||||||||||||||||||
| A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | |
| Mean | 6.7 | 11.3 | 9.3 | 11.0 | 9.0 | 20.9 | 11.4 | 21.0 | 10.8 | 32.2 | 13.9 | 30.1 | 13.5 | 37.1 | 20.2 | 31.5 | 4.6 | 7.5 | 6.5 | 13.7 | 10.9 | 10.9 | 19.6 | 17.3 | 15.4 | 17.9 | 24.4 | 19.3 | 5.8 | 12.6 | 7.7 | 14.3 | 21.0 | 34.6 | 33.9 | 38.2 |
| SD | 0.3 | 0.8 | 0.4 | 0.2 | 0.6 | 0.7 | 0.4 | 0.2 | 0.2 | 1.1 | 0.6 | 0.1 | 0.5 | 0.8 | 1.0 | 1.7 | 0.3 | 0.3 | 0.4 | 0.7 | 0.3 | 0.2 | 0.6 | 0.5 | 0.7 | 0.5 | 0.8 | 0.4 | 0.2 | 1.0 | 0.3 | 0.5 | 0.8 | 0.9 | 0.4 | 0.9 |
| SErr | 0.1 | 0.3 | 0.1 | 0.1 | 0.2 | 0.2 | 0.1 | 0.1 | 0.1 | 0.4 | 0.2 | 0.0 | 0.2 | 0.2 | 0.3 | 0.5 | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.1 | 0.2 | 0.2 | 0.2 | 0.2 | 0.3 | 0.1 | 0.0 | 0.3 | 0.1 | 0.2 | 0.2 | 0.3 | 0.1 | 0.3 |
| Lower 95% CI | 6.4 | 10.7 | 9.0 | 10.9 | 8.6 | 20.4 | 11.1 | 20.9 | 10.7 | 31.4 | 13.4 | 30.0 | 13.2 | 36.6 | 19.5 | 30.3 | 4.3 | 7.3 | 6.3 | 13.2 | 10.7 | 10.8 | 19.1 | 16.9 | 14.9 | 17.5 | 23.8 | 19.0 | 5.7 | 11.8 | 7.5 | 13.9 | 20.4 | 33.9 | 33.6 | 37.5 |
| Upper 95% CI | 6.9 | 11.8 | 9.6 | 11.2 | 9.4 | 21.4 | 11.7 | 21.2 | 11.0 | 33.0 | 14.3 | 30.2 | 13.9 | 37.7 | 21.0 | 32.8 | 4.8 | 7.7 | 6.8 | 14.2 | 11.1 | 11.0 | 20.0 | 17.7 | 15.9 | 18.3 | 25.0 | 19.6 | 6.0 | 13.3 | 7.9 | 14.7 | 21.5 | 35.2 | 34.2 | 38.8 |
| RT | 10 PCF | 20 PCF | 20 PCF | 20 PCF | 20 PCF | 30 PCF | 30 PCF | |||||||||||||||||||||||||||||
| BLOCK NO CORT | BLOCK CORT | BLOCK NO CORT | BLOCK CORT | LAMINA 1 MM | LAMINA 2 MM | LAMINA 3 MM | LAMINA 1 MM | LAMINA 3 MM | ||||||||||||||||||||||||||||
| A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | |
| Mean | 5.4 | 9.0 | 7.4 | 9.9 | 6.7 | 14.4 | 10.5 | 17.3 | 7.7 | 23.1 | 11.3 | 26.0 | 9.4 | 24.3 | 17.2 | 27.4 | 3.7 | 3.9 | 4.3 | 8.7 | 7.8 | 3.9 | 15.0 | 14.4 | 12.8 | 15.6 | 15.9 | 16.3 | 4.5 | 4.7 | 5.9 | 10.0 | 17.6 | 22.2 | 30.8 | 32.6 |
| SD | 0.8 | 0.9 | 0.6 | 0.1 | 0.2 | 0.9 | 0.3 | 0.3 | 0.3 | 0.4 | 0.8 | 0.3 | 0.6 | 0.8 | 1.7 | 0.3 | 0.3 | 0.0 | 0.2 | 0.2 | 0.4 | 0.0 | 0.6 | 0.3 | 0.3 | 0.4 | 0.8 | 0.2 | 0.3 | 0.4 | 0.1 | 0.3 | 0.3 | 0.4 | 0.4 | 0.5 |
| SErr | 0.3 | 0.3 | 0.2 | 0.0 | 0.1 | 0.3 | 0.1 | 0.1 | 0.1 | 0.1 | 0.3 | 0.1 | 0.2 | 0.3 | 0.5 | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | 0.0 | 0.2 | 0.1 | 0.1 | 0.1 | 0.3 | 0.1 | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 |
| Lower 95% CI | 4.8 | 8.4 | 7.0 | 9.8 | 6.6 | 13.8 | 10.3 | 17.0 | 7.5 | 22.8 | 10.7 | 25.8 | 9.0 | 23.7 | 16.0 | 27.2 | 3.5 | 3.9 | 4.1 | 8.5 | 7.6 | 3.9 | 14.6 | 14.1 | 12.6 | 15.3 | 15.4 | 16.1 | 4.3 | 4.4 | 5.8 | 9.8 | 17.4 | 22.0 | 30.5 | 32.2 |
| Upper 95% CI | 6.0 | 9.7 | 7.8 | 10.0 | 6.9 | 15.0 | 10.7 | 17.5 | 8.0 | 23.4 | 11.9 | 26.3 | 9.9 | 24.9 | 18.4 | 27.7 | 3.9 | 3.9 | 4.4 | 8.9 | 8.1 | 3.9 | 15.4 | 14.6 | 13.0 | 15.8 | 16.5 | 16.4 | 4.8 | 5.0 | 6.0 | 10.1 | 17.9 | 22.5 | 31.1 | 33.0 |
| RFA | 10 PCF | 20 PCF | 20 PCF | 20 PCF | 20 PCF | 30 PCF | 30 PCF | |||||||||||||||||||||||||||||
| BLOCK NO CORT | BLOCK CORT | BLOCK NO CORT | BLOCK CORT | LAMINA 1 MM | LAMINA 2 MM | LAMINA 3 MM | LAMINA 1 MM | LAMINA 3 MM | ||||||||||||||||||||||||||||
| A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | A | B | C | D | |
| Mean | 41.3 | 51.5 | 36.6 | 46.3 | 37.1 | 60.5 | 38.6 | 57.2 | 38.7 | 65.7 | 40.6 | 62.0 | 41.6 | 68.4 | 43.6 | 64.4 | 19.0 | 19.2 | 23.6 | 45.6 | 21.6 | 30.7 | 26.6 | 57.5 | 23.7 | 58.6 | 27.6 | 60.7 | 20.6 | 20.4 | 25.7 | 52.6 | 25.7 | 60.6 | 30.6 | 63.5 |
| SD | 0.8 | 0.5 | 0.5 | 0.8 | 0.7 | 0.5 | 0.5 | 0.8 | 0.5 | 0.4 | 0.3 | 0.7 | 0.5 | 0.5 | 0.5 | 0.4 | 1.2 | 2.1 | 0.5 | 0.5 | 0.5 | 0.5 | 0.4 | 0.4 | 0.4 | 0.4 | 0.5 | 0.5 | 0.4 | 0.5 | 0.4 | 0.5 | 0.4 | 0.4 | 0.5 | 0.5 |
| SErr | 0.2 | 0.1 | 0.1 | 0.2 | 0.2 | 0.1 | 0.1 | 0.2 | 0.2 | 0.1 | 0.1 | 0.2 | 0.1 | 0.2 | 0.2 | 0.1 | 0.4 | 0.7 | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 | 0.1 | 0.2 | 0.1 | 0.2 | 0.1 | 0.1 | 0.1 | 0.2 |
| Lower 95% CI | 40.7 | 51.2 | 36.3 | 45.7 | 36.6 | 60.2 | 38.3 | 56.6 | 38.3 | 65.4 | 40.4 | 61.5 | 41.3 | 68.0 | 43.2 | 64.1 | 18.1 | 17.7 | 23.3 | 45.3 | 21.3 | 30.3 | 26.2 | 57.2 | 23.4 | 58.2 | 27.3 | 60.3 | 20.2 | 20.0 | 25.4 | 52.2 | 25.4 | 60.2 | 30.3 | 63.1 |
| Upper 95% CI | 41.8 | 51.8 | 36.9 | 46.9 | 37.6 | 60.8 | 38.9 | 57.8 | 39.0 | 65.9 | 40.8 | 62.4 | 41.9 | 68.7 | 43.9 | 64.6 | 19.9 | 20.7 | 23.9 | 45.9 | 21.9 | 31.0 | 26.9 | 57.8 | 23.9 | 58.9 | 27.9 | 61.0 | 20.9 | 20.8 | 26.0 | 52.9 | 25.9 | 60.9 | 30.9 | 63.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comuzzi, L.; Tumedei, M.; Romasco, T.; Petrini, M.; Afrashtehfar, K.I.; Inchingolo, F.; Piattelli, A.; Di Pietro, N. Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An In Vitro Study on Polyurethane Foam Sheets. J. Funct. Biomater. 2023, 14, 10. https://doi.org/10.3390/jfb14010010
Comuzzi L, Tumedei M, Romasco T, Petrini M, Afrashtehfar KI, Inchingolo F, Piattelli A, Di Pietro N. Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An In Vitro Study on Polyurethane Foam Sheets. Journal of Functional Biomaterials. 2023; 14(1):10. https://doi.org/10.3390/jfb14010010
Chicago/Turabian StyleComuzzi, Luca, Margherita Tumedei, Tea Romasco, Morena Petrini, Kelvin I. Afrashtehfar, Francesco Inchingolo, Adriano Piattelli, and Natalia Di Pietro. 2023. "Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An In Vitro Study on Polyurethane Foam Sheets" Journal of Functional Biomaterials 14, no. 1: 10. https://doi.org/10.3390/jfb14010010
APA StyleComuzzi, L., Tumedei, M., Romasco, T., Petrini, M., Afrashtehfar, K. I., Inchingolo, F., Piattelli, A., & Di Pietro, N. (2023). Insertion Torque, Removal Torque, and Resonance Frequency Analysis Values of Ultrashort, Short, and Standard Dental Implants: An In Vitro Study on Polyurethane Foam Sheets. Journal of Functional Biomaterials, 14(1), 10. https://doi.org/10.3390/jfb14010010













