Successful Management of Public Health Projects Driven by AI in a BANI Environment
Abstract
1. Introduction
- 1.
- Quantify the impact of emergency-related factors, such as population displacement, healthcare disruptions, and periodic emergent events, on disease transmission, misinformation, and panic, using time-varying parameters to reflect long-term trends.
- 2.
- Conduct qualitative and quantitative analyses to identify critical risks (e.g., increased transmission, misinformation surges) and opportunities (e.g., AI-enabled fact-checking, infrastructure recovery) that influence public health outcomes.
- 3.
- Provide actionable insights for public health practitioners by evaluating the effectiveness of AI-driven interventions (e.g., predictive analytics, real-time monitoring, mental health support) in mitigating epidemic peaks and enhancing resilience.
- 4.
- Contribute to the broader understanding of AI’s role in managing public health crises in BANI environments, offering a scalable framework applicable to other conflicts or crisis settings.
2. Current Research Analysis
3. Materials and Methods
- 1.
- Disease spread (SEIR)—incorporates emergency-induced factors like displacement and healthcare disruption, which increase transmission rates.
- 2.
- Misinformation spread—models rapid misinformation dissemination via social media, amplified by targeted disinformation.
- 3.
- Panic spread—links panic to emergency events and misinformation, affecting disease transmission.
- 4.
- Emergency impact—introduces parameters for displacement, infrastructure damage, and disrupted interventions.
- Closed population (ignoring migration for simplicity).
- Homogeneous mixing within the city, though displacement increases contact rates.
- Emergency events are periodic, modelled as a constant factor for simplicity.
- Healthcare disruption and displacement are uniform across the population.
4. Results
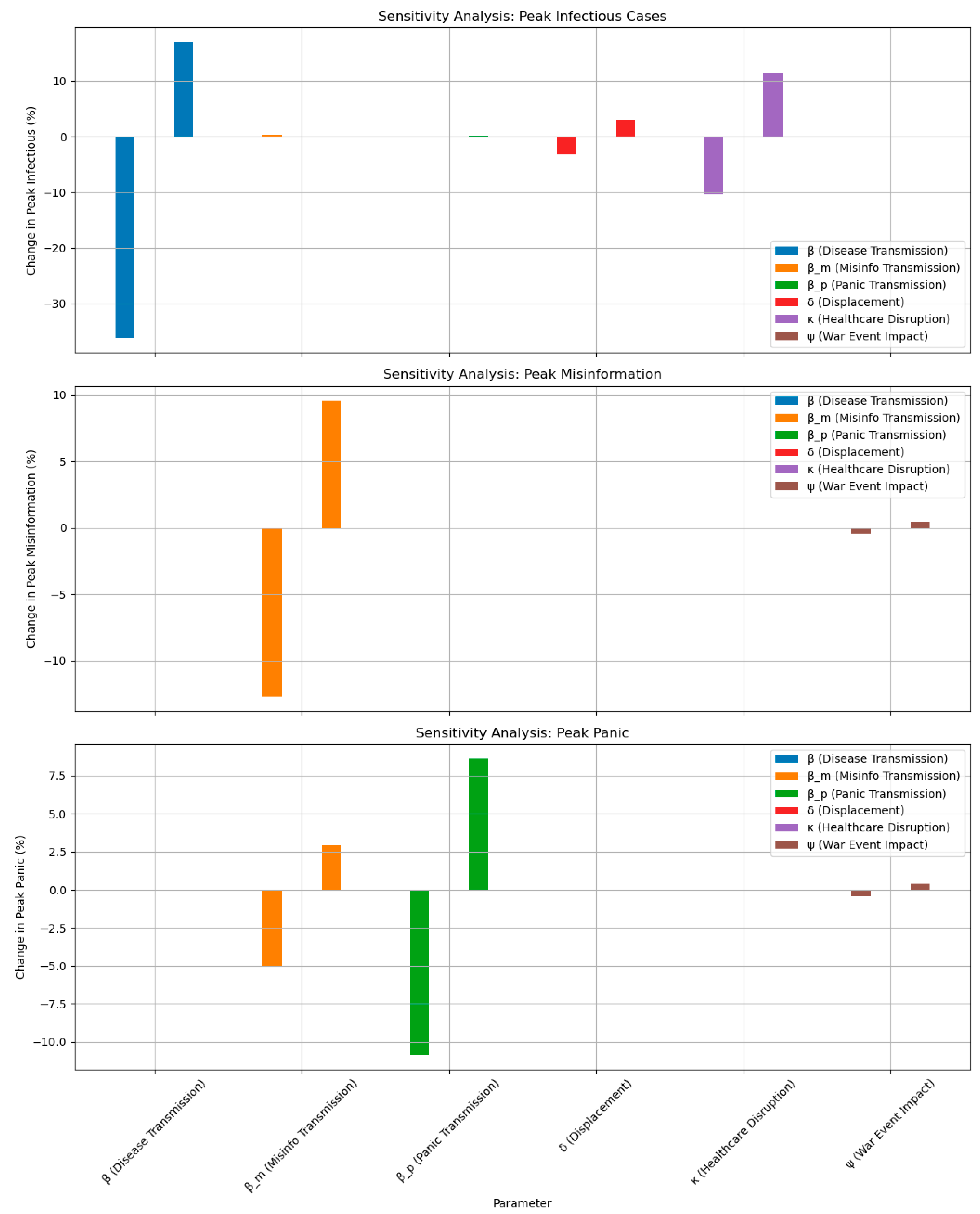
- Enhanced disease spread due to displacement (increase in β to 0.36).
- Increased misinformation (increase in βm to 0.72).
- Increased panic (increase in βp to 0.6).
- Greater displacement (increase in δ to 0.24).
- More infrastructure damage (increase in κ to 0.36).
- Effective misinformation countering (increase in γm to 0.15).
- Effective panic calming (increase in γp to 0.3).
- Infrastructure recovery (decrease in κ to 0.15)
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| BANI | Brittle, anxious, non-linear, incomprehensible |
| SEIR | Susceptible–exposed–infected–recovered |
| AI | Artificial intelligence |
| COVID-19 | Coronavirus disease 2019 |
| NLP | Natural language processing |
| ML | Machine learning |
| LSTM | Long Short-Term Memory |
| IDP | Internally displaced person |
| PTSD | Post-traumatic stress disorder |
References
- Dotsenko, N.; Chumachenko, I.; Kraivskyi, B.; Railian, M.; Litvinov, A. Methodological Support for Managing of Critical Competences in Agile Transformation Projects within a Multi-Project Medical Environment. Adv. Inf. Syst. 2024, 8, 26–33. [Google Scholar] [CrossRef]
- Bushuyev, S.; Chumachenko, I.; Galkin, A.; Bushuiev, D.; Dotsenko, N. Sustainable Development Projects Implementing in BANI Environment Based on AI Tools. Sustainability 2025, 17, 2607. [Google Scholar] [CrossRef]
- Patterson, A.; Clark, M.A. COVID-19 and Power in Global Health. Int. J. Health Policy Manag. 2020, 9, 429–431. [Google Scholar] [CrossRef]
- Chumachenko, D.; Piletskiy, P.; Sukhorukova, M.; Chumachenko, T. Predictive Model of Lyme Disease Epidemic Process Using Machine Learning Approach. Appl. Sci. 2022, 12, 4282. [Google Scholar] [CrossRef]
- Necesito, I.V.; Mark, J.; Jung, J.; Bae, Y.H.; Yoo, Y.; Kim, S.; Kim, H.S. Predicting COVID-19 Cases in South Korea Using Stringency and Niño Sea Surface Temperature Indices. Front. Public Health 2022, 10, 871354. [Google Scholar] [CrossRef]
- Kaur, J.; Sharma, P.; Kumar, V.; Duggal, M.; Diamond-Smith, N.G.; Ayadi, A.E.; Vosburg, K.; Singh, P. Exploring the Role of Chatbots in Tackling COVID-19 Vaccine Hesitancy among Pregnant and Breastfeeding Women in Rural Northern India. Proc. ACM Hum. Comput. Interact. 2024, 8, 55. [Google Scholar] [CrossRef]
- Waqar, A.; Andri, A.; Qureshi, A.H.; Almujibah, H.R.; Tanjung, L.E.; Utami, C. Evaluation of Success Factors of Utilizing AI in Digital Transformation of Health and Safety Management Systems in Modern Construction Projects. Ain Shams Eng. J. 2023, 14, 102551. [Google Scholar] [CrossRef]
- Bushuyev, S.; Ivko, A.; Mudra, M.; Murovanskiy, G.; Piliuhina, K. Adaptability in Managing Innovative Projects within the Bani Environment. Manag. Dev. Complex Syst. 2023, 54, 5–11. [Google Scholar] [CrossRef]
- Prasetyo, M.L.; Peranginangin, R.A.; Martinovic, N.; Ichsan, M.; Wicaksono, H. Artificial Intelligence in Open Innovation Project Management: A Systematic Literature Review on Technologies, Applications, and Integration Requirements. J. Open Innov. Technol. Mark. Complex. 2024, 11, 100445. [Google Scholar] [CrossRef]
- Dotsenko, N.; Chumachenko, I.; Skachkov, O.; Husieva, Y. Development and Implementation of Intelligent Programming Tool for Agile Transformation of Human Resource Management Processes. CEUR Workshop Proc. 2024, 3777, 361–368. [Google Scholar]
- Ajirotutu, R.O.; Patrick Garba, B.M.; Johnson, S.O. AI-Driven Risk Mitigation: Transforming Project Management in Construction and Infrastructure Development. World J. Adv. Eng. Technol. Sci. 2024, 13, 611–623. [Google Scholar] [CrossRef]
- Bushuyev, S.; Babayev, I.; Bushuiev, D.; Bushuyeva, N.; Babayev, J. Emotional Behavior in the “Infodemic vs. Panicdemic vs. Pandemic” Modeling COVID-19. CEUR Workshop Proc. 2021, 2851, 391–400. [Google Scholar]
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The Role of Artificial Intelligence in Healthcare: A Structured Literature Review. BMC Med. Inform. Decis. Mak. 2021, 21, 125. [Google Scholar] [CrossRef]
- Waqar, A.; Othman, I.; Sor, N.H.; Alshehri, A.; Almujibah, H.; Alotaibi, B.S.; Abuhussain, M.A.; Bageis, A.S.; Althoey, F.; Hayat, S.; et al. Modeling Relation among Implementing AI-Based Drones and Sustainable Construction Project Success. Front. Built Environ. 2023, 9, 1208807. [Google Scholar] [CrossRef]
- Bellei, E.A.; Carolina, A. Championing Health Systems Management with Digital Innovation and Applications in the Age of Artificial Intelligence: Protocol for a Research Program. F1000Research 2024, 13, 741. [Google Scholar] [CrossRef]
- Chumachenko, D.; Butkevych, M.; Lode, D.; Frohme, M.; Schmailzl, K.J.G.; Nechyporenko, A. Machine Learning Methods in Predicting Patients with Suspected Myocardial Infarction Based on Short-Time HRV Data. Sensors 2022, 22, 7033. [Google Scholar] [CrossRef]
- Bushuyev, S.; Babayev, I.; Bushuieva, V.; Bushuyeva, N.; Babayev, J.; Bushuiev, D. Managing Project Success with “Infodemic” vs. “Pandemic” Environment on the COVID-19 Pandemic Case. In Proceedings of the 2021 IEEE International Conference on Smart Information Systems and Technologies (SIST), Nur-Sultan, Kazakhstan, 28–30 April 2021; pp. 1–7. [Google Scholar] [CrossRef]
- Vrchota, J.; Řehoř, P.; Maříková, M.; Pech, M. Critical Success Factors of the Project Management in Relation to Industry 4.0 for Sustainability of Projects. Sustainability 2020, 13, 281. [Google Scholar] [CrossRef]
- Li, Y.; Song, H.; Sang, P.; Chen, P.-H.; Liu, X. Review of Critical Success Factors (CSFs) for Green Building Projects. Build. Environ. 2019, 158, 182–191. [Google Scholar] [CrossRef]
- Ika, L.A.; Diallo, A.; Thuillier, D. Critical Success Factors for World Bank Projects: An Empirical Investigation. Int. J. Proj. Manag. 2012, 30, 105–116. [Google Scholar] [CrossRef]
- Santos, C.; Varajão, J.; Takagi, N.; Gonçalves, A.M. Model of Driving Factors for Success in Public Health Project Management Using Structural Equation Modeling. Sci. Rep. 2024, 14, 24647. [Google Scholar] [CrossRef]
- Padalko, H.; Chomko, V.; Chumachenko, D. A Novel Approach to Fake News Classification Using LSTM-Based Deep Learning Models. Front. Big Data 2024, 6, 1320800. [Google Scholar] [CrossRef]
- Marion, G.; Hadley, L.; Isham, V.; Mollison, D.; Panovska-Griffiths, J.; Pellis, L.; Tomba, G.S.; Scarabel, F.; Swallow, B.; Trapman, P.; et al. Modelling: Understanding Pandemics and How to Control Them. Epidemics 2022, 39, 100588. [Google Scholar] [CrossRef]
- Haque, U.; Bukhari, M.H.; Fiedler, N.; Wang, S.; Korzh, O.; Espinoza, J.; Ahmad, M.; Holovanova, I.; Chumachenko, T.; Marchak, O.; et al. A Comparison of Ukrainian Hospital Services and Functions before and during the Russia-Ukraine War. JAMA Health Forum 2024, 5, e240901. [Google Scholar] [CrossRef]
- Guo, X.; Tong, J.; Chen, P.; Fan, W. The Suppression Effect of Emotional Contagion in the COVID-19 Pandemic: A Multi-Layer Hybrid Modelling and Simulation Approach. PLoS ONE 2021, 16, e0253579. [Google Scholar] [CrossRef]
- Rhodes, T.; Lancaster, K.; Lees, S.; Parker, M. Modelling the Pandemic: Attuning Models to Their Contexts. BMJ Glob. Health 2020, 5, e002914. [Google Scholar] [CrossRef]
- Libkind, S.; Baas, A.; Halter, M.; Patterson, E.; Fairbanks, J.P. An Algebraic Framework for Structured Epidemic Modelling. Philos. Trans. R. Society. Math. Phys. Eng. Sci. 2022, 380, 20210309. [Google Scholar] [CrossRef]
- Mohammadi, A.; Meniailov, I.; Bazilevych, K.; Yakovlev, S.; Chumachenko, D. Comparative Study of Linear Regression and SIR Models of COVID-19 Propagation in Ukraine before Vaccination. Radioelectron. Comput. Syst. 2021, 2021, 5–18. [Google Scholar] [CrossRef]
- Bellomo, N.; Brezzi, F.; Chaplain, M.A.J. Modeling Virus Pandemics in a Globally Connected World a Challenge towards a Mathematics for Living Systems. Math. Models Methods Appl. Sci. 2021, 31, 2391–2397. [Google Scholar] [CrossRef]
- Schaber, K.L.; Kumar, S.; Lubwama, B.; Desai, A.; Majumder, M.S. An Epidemic Model for Multi-Intervention Outbreaks. medRxiv 2023. [Google Scholar] [CrossRef]
- Ogden, N.H.; Fazil, A.; Arino, J.; Berthiaume, P.; Fisman, D.N.; Greer, A.L.; Ludwig, A.; Ng, V.; Tuite, A.R.; Turgeon, P.; et al. Modelling Scenarios of the Epidemic of COVID-19 in Canada. Can. Commun. Dis. Rep. 2020, 46, 198–204. [Google Scholar] [CrossRef]
- Alfaleh, R.; Alsuwailem, W.A.; Almazyad, R.T.; Alanazi, F.F.; Alanazi, L.T. The Impact of Armed Conflicts on the Prevalence, Transmission, and Management of Infectious Diseases: A Systematic Review. Cureus 2025, 17, e79450. [Google Scholar] [CrossRef]
- Ghorbani, M.; Suleimenova, D.; Jahani, A.; Saha, A.; Xue, Y.; Mintram, K.; Anagnostou, A.; Tas, A.; Low, W.; Taylor, S.J.E.; et al. Flee 3: Flexible Agent-Based Simulation for Forced Migration. J. Comput. Sci. 2024, 81, 102371. [Google Scholar] [CrossRef]
- Vasylyev, M.; Lamberink, H.; Svyst, I.; Khlypnyach, O.; Sluzhynska, O.; Sluzhynska, M.; Shtoiko, I.; Hrushynska, O.; Demianenko, D.; Rokx, C. The Infectious Disease Burden among War Related Internally Displaced People in the Lviv Region of Ukraine. Germs 2024, 14, 322–343. [Google Scholar] [CrossRef]
- Rodríguez, A.; Cuevas, E.; Zaldivar, D.; Morales-Castañeda, B.; Sarkar, R.; Houssein, E.H. An Agent-Based Transmission Model of COVID-19 for Re-Opening Policy Design. Comput. Biol. Med. 2022, 148, 105847. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Highlighting a Population’s Health Information Needs During Health Emergencies Through New Infodemic Management Tools and Frameworks. Available online: http://who.int/news/item/13-04-2023-highlighting-a-population-s-health-information-needs-during-health-emergencies-through-new-infodemic-management-tools-and-frameworks/ (accessed on 17 June 2025).
- Thakur, N.; Han, C.Y. Multimodal Approaches for Indoor Localization for Ambient Assisted Living in Smart Homes. Information 2021, 12, 114. [Google Scholar] [CrossRef]
- Albín-Rodríguez, A.-P.; De-La-Fuente-Robles, Y.-M.; López-Ruiz, J.-L.; Verdejo-Espinosa, Á.; Estévez, M.E. UJAmI Location: A Fuzzy Indoor Location System for the Elderly. Int. J. Environ. Res. Public Health 2021, 18, 8326. [Google Scholar] [CrossRef]
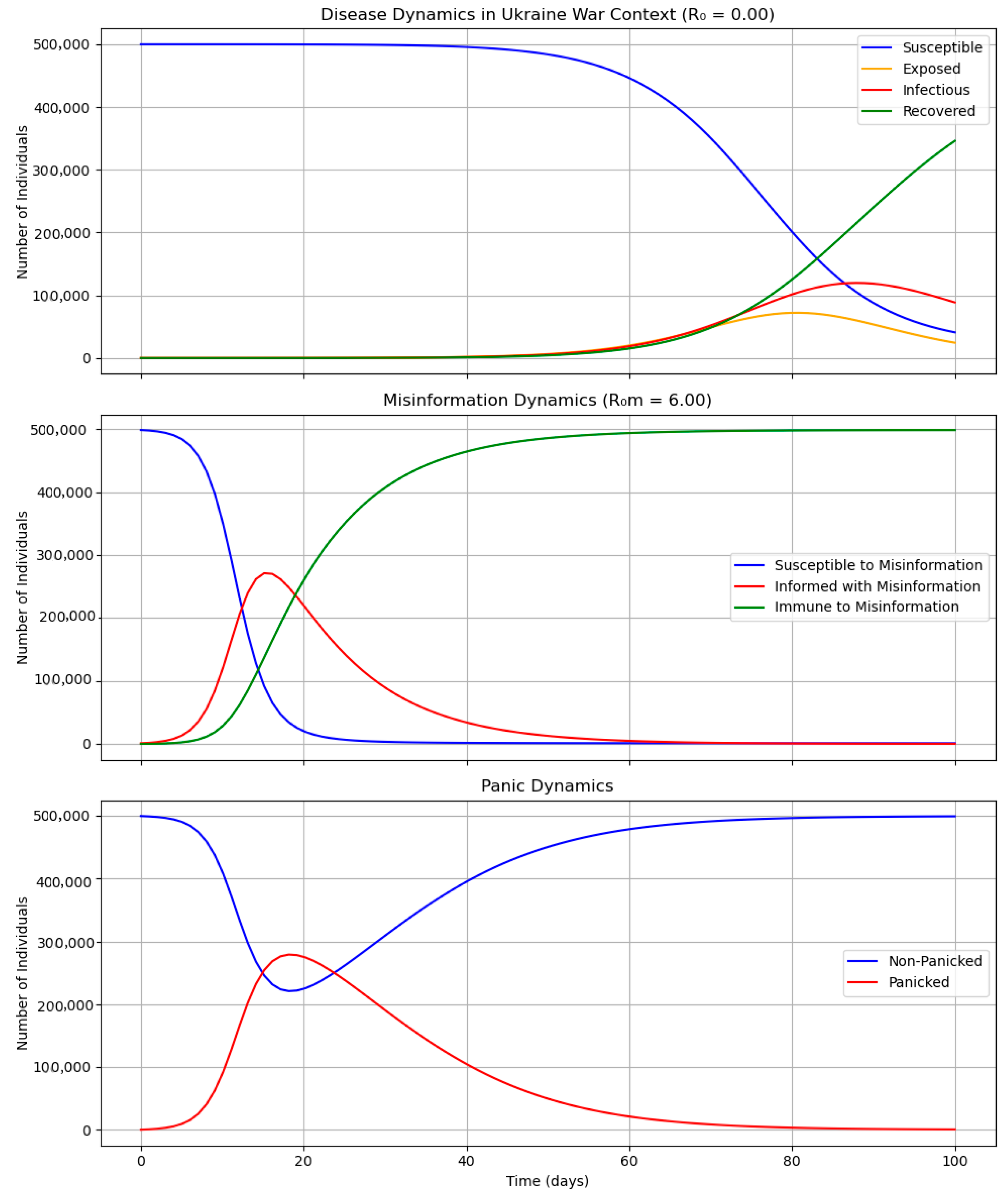
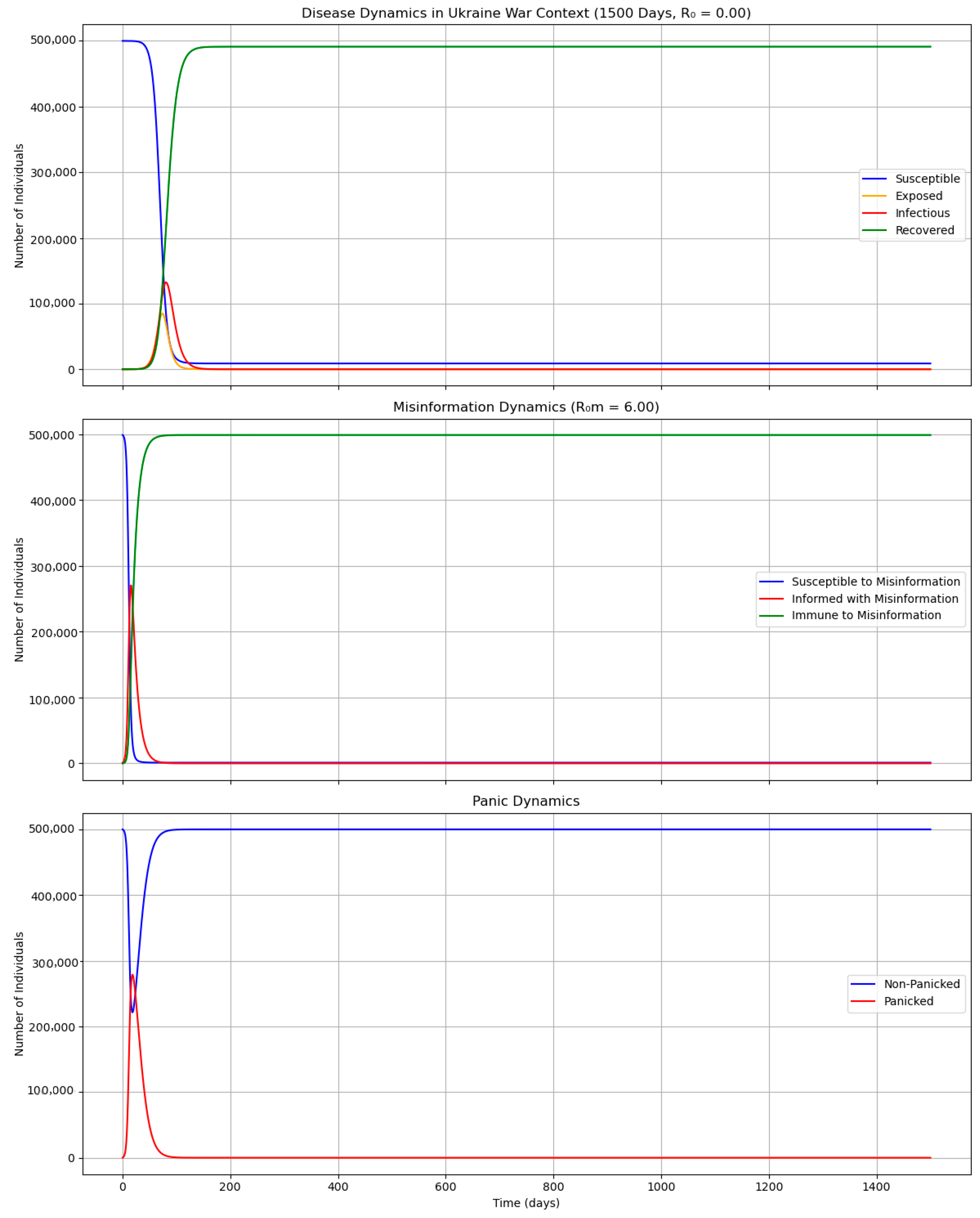
| Parameter | Description | Initial Value |
|---|---|---|
| β | baseline transmission rate | 0.3 |
| Σ | progression rate from “Exposed” to “Infectious” | 0.2 |
| γ | recovery rate | 0.1429 |
| N | population | 500,000 |
| δ | displacement factor | 0.2 |
| κ | healthcare disruption factor | 0.3 |
| βm | misinformation transmission rate | 0.6 |
| γm | misinformation recovery rate | 0.1 |
| R0m = βm/γm | misinformation reproduction number | 0 |
| βp | panic transmission rate | 0.5 |
| γp | panic recovery rate | 0.2 |
| ω | emergency event frequency | 0.1 |
| α | panic amplification factor for disease transmission | 0.5 |
| ψ | emergency event impact on misinformation and panic | 0.3 |
| Category | Risk | Description | Likelihood | Impact | Mitigation Measures |
|---|---|---|---|---|---|
| Technical | Data Quality | Inaccurate or incomplete data (EMR, IoT, social media) due to war disruptions. | High | High | Use AI for data cleaning, integrate multiple sources. |
| Technical | Infrastructure Failures | Damage to servers or power grids from attacks. | Medium | High | Cloud platforms (AWS), backup systems. |
| Organisational | Staff Shortages | Lack of AI specialists due to emigration. | High | Medium | International collaboration, remote training. |
| Organisational | Resistance to Change | Distrust in AI among the medical staff or public. | Medium | Medium | Trust-building campaigns, algorithm transparency. |
| Ethical | AI Bias | Algorithms may discriminate against vulnerable groups (IDPs). | Medium | High | Algorithm audits, WHO ethical standards. |
| Ethical | Privacy Breaches | Data leaks due to cyberattacks. | High | High | Encryption, GDPR compliance. |
| Regulatory | Non-Compliance | Violation of GDPR or WHO standards due to rapid AI deployment. | Low | High | Legal audits, regulatory consultations. |
| Military | Increased Misinformation | Propaganda (Telegram) undermines health trust. | High | High | AI-NLP monitoring, counter-misinformation campaigns. |
| Military | Population Displacement | IDP camps increase outbreak risks. | High | High | Mobile clinics, IoT monitoring. |
| Category | Risk | Description | Likelihood | Impact | Mitigation Measures |
|---|---|---|---|---|---|
| Technical | AI Forecasting | Accurate outbreak predictions (LSTM, Random Forest). | High | High | Integrate EMR, IoT, social data. |
| Technical | Automation | AI optimises logistics and planning. | Medium | High | Implement AI-PM tools. |
| Organisational | International Support | Aid for infrastructure. | High | High | Direct funds to AI and health tech. |
| Organisational | Public Trust | Transparent AI dashboards build trust. | Medium | Medium | Develop AR/VR visualisations. |
| Ethical | Equity | AI ensures healthcare access for IDPs. | Medium | High | Algorithms targeting vulnerable groups. |
| Regulatory | Global Standards | WHO compliance attracts investments. | Low | High | Certify AI systems. |
| Military | Health Monitoring | IoT for real-time monitoring in IDP camps | Medium | High | Deploy wearable devices |
| Scenario | Peak Infectious (% Change) | Peak Misinformation (% Change) | Peak Panic (% Change) |
|---|---|---|---|
| Baseline | 0.0 | 0.0 | 0.0 |
| High β | 28.3 | 0.0 | 0.0 |
| High βm | 5.2 | 22.7 | 18.9 |
| High βp | 12.6 | 0.0 | 15.4 |
| High δ | 20.8 | 0.0 | 0.0 |
| High κ | 15.1 | 0.0 | 0.0 |
| Scenario | Peak Infectious (% Change) | Peak Misinformation (% Change) | Peak Panic (% Change) |
|---|---|---|---|
| Baseline | 0.0 | 0.0 | 0.0 |
| High γm | −4.8 | −18.2 | −15.6 |
| High γp | −8.3 | 0.0 | −12.9 |
| Low κ | −10.7 | 0.0 | 0.0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bushuyev, S.; Bushuyeva, N.; Nekrasov, I.; Chumachenko, I. Successful Management of Public Health Projects Driven by AI in a BANI Environment. Computation 2025, 13, 160. https://doi.org/10.3390/computation13070160
Bushuyev S, Bushuyeva N, Nekrasov I, Chumachenko I. Successful Management of Public Health Projects Driven by AI in a BANI Environment. Computation. 2025; 13(7):160. https://doi.org/10.3390/computation13070160
Chicago/Turabian StyleBushuyev, Sergiy, Natalia Bushuyeva, Ivan Nekrasov, and Igor Chumachenko. 2025. "Successful Management of Public Health Projects Driven by AI in a BANI Environment" Computation 13, no. 7: 160. https://doi.org/10.3390/computation13070160
APA StyleBushuyev, S., Bushuyeva, N., Nekrasov, I., & Chumachenko, I. (2025). Successful Management of Public Health Projects Driven by AI in a BANI Environment. Computation, 13(7), 160. https://doi.org/10.3390/computation13070160






