Abstract
The management of public health projects in a BANI (brittle, anxious, non-linear, incomprehensible) environment, exemplified by the ongoing war in Ukraine, presents unprecedented challenges due to fragile systems, heightened uncertainty, and complex socio-political dynamics. This study proposes an AI-driven framework to enhance the resilience and effectiveness of public health interventions under such conditions. By integrating a coupled SEIR–Infodemic–Panicdemic Model with war-specific factors, we simulate the interplay of infectious disease spread, misinformation dissemination, and panic dynamics over 1500 days in a Ukrainian city (Kharkiv). The model incorporates time-varying parameters to account for population displacement, healthcare disruptions, and periodic war events, reflecting the evolving conflict context. Sensitivity and risk–opportunity analyses reveal that disease transmission, misinformation, and infrastructure damage significantly exacerbate epidemic peaks, while AI-enabled interventions, such as fact-checking, mental health support, and infrastructure recovery, offer substantial mitigation potential. Qualitative assessments identify technical, organisational, ethical, regulatory, and military risks, alongside opportunities for predictive analytics, automation, and equitable healthcare access. Quantitative simulations demonstrate that risks, like increased displacement, can amplify infectious peaks by up to 28.3%, whereas opportunities, like enhanced fact-checking, can reduce misinformation by 18.2%. These findings provide a roadmap for leveraging AI to navigate BANI environments, offering actionable insights for public health practitioners in Ukraine and other crisis settings. The study underscores AI’s transformative role in fostering adaptive, data-driven strategies to achieve sustainable health outcomes amidst volatility and uncertainty.
1. Introduction
The management of public health projects has entered an era of unprecedented complexity, characterised by interconnected crises, from pandemics and climate-related health threats to systemic inequities, that defy traditional linear approaches [1]. These challenges are amplified by the BANI (brittle, anxious, non-linear, incomprehensible) framework, a lens capturing the fragility, unpredictability, and cognitive overload inherent in modern socio-technical systems [2]. For instance, the COVID-19 pandemic exposed the brittleness of global health infrastructures, while vaccine distribution efforts highlighted non-linear disparities exacerbated by geopolitical and socioeconomic dynamics [3]. In such environments, conventional project management strategies often falter, struggling to balance rapid response demands with long-term sustainability goals.
Artificial intelligence (AI) has emerged as a pivotal tool to navigate these complexities. By leveraging predictive analytics, machine learning, and real-time data integration, AI offers transformative potential to enhance decision-making, optimise resource allocation, and mitigate risks in public health initiatives [4]. For example, AI-driven models enabled South Korea to predict COVID-19 case surges with 92% accuracy, streamlining containment measures [5]. Similarly, NLP-powered chatbots in India reduced vaccine hesitancy by addressing public anxiety through personalised, real-time communication [6]. Yet, the integration of AI into public health is not without peril. Algorithmic biases, data privacy concerns, and the opaque nature of “black-box” models risk exacerbating inequities, particularly in marginalised communities already disproportionately affected by BANI-driven disruptions.
This study investigates how AI has been ethically and effectively harnessed to manage public health projects in BANI settings. It argues that AI’s value lies not in replacing human judgement but in augmenting it, creating hybrid systems that combine computational precision with contextual, equity-focused governance. Drawing on case studies from pandemic response, disaster resilience, and chronic disease management, the analysis explores AI’s capacity to anticipate brittleness through early-warning systems for disease outbreaks or supply chain failures, alleviate anxiety via transparent, AI-enhanced communication platforms that build public trust, decode nonlinearity by modelling cascading impacts of policy decisions in real time, and simplify incomprehensibility through data visualisation tools that make complex health data actionable.
The paper also critically examines the ethical tightrope walked by AI adopters, emphasising the need for frameworks that prioritise fairness, accountability, and inclusivity. By synthesising lessons from global health crises and emerging AI innovations, this work provides a roadmap for policymakers and practitioners to leverage AI as a force for resilient, equitable public health systems in an age of perpetual uncertainty.
This research aims to develop and evaluate an AI-driven framework for the effective management of public health projects in a BANI (brittle, anxious, non-linear, incomprehensible) environment, with a specific focus on the context of Ukraine. By integrating a Coupled SEIR–Infodemic–Panicdemic Model with war-specific factors, the study aims to simulate and analyse the interplay of infectious disease spread, misinformation dissemination, and panic dynamics over an extended period (1500 days) in a Ukrainian city (e.g., Kharkiv). The research seeks to achieve the following:
- 1.
- Quantify the impact of emergency-related factors, such as population displacement, healthcare disruptions, and periodic emergent events, on disease transmission, misinformation, and panic, using time-varying parameters to reflect long-term trends.
- 2.
- Conduct qualitative and quantitative analyses to identify critical risks (e.g., increased transmission, misinformation surges) and opportunities (e.g., AI-enabled fact-checking, infrastructure recovery) that influence public health outcomes.
- 3.
- Provide actionable insights for public health practitioners by evaluating the effectiveness of AI-driven interventions (e.g., predictive analytics, real-time monitoring, mental health support) in mitigating epidemic peaks and enhancing resilience.
- 4.
- Contribute to the broader understanding of AI’s role in managing public health crises in BANI environments, offering a scalable framework applicable to other conflicts or crisis settings.
This research aims to bridge the gap between AI technology and public health management, delivering a robust, data-driven approach to navigate the complexities of emergent context, misinformation, and panic, ultimately fostering sustainable health outcomes in volatile contexts.
2. Current Research Analysis
The successful management of public health projects driven by AI in a BANI (brittle, anxious, non-linear, incomprehensible) environment requires a combination of technological, organisational, and adaptive strategies. Key success factors include adaptability, the integration of digital tools, robust risk management, and fostering a culture of collaboration and continuous learning. Let us look at different dimensions of the problem area.
Projects in BANI environments demand high adaptability and resilience. Embracing agile management, fostering experimentation, and supporting continuous learning are essential for navigating volatility and complexity [7,8]. The effective integration of AI into existing systems, reliable operations, and knowledge management is crucial for project success. This includes ensuring technical infrastructure, data readiness, and seamless system interoperability [7,9]. Leadership support, strategic alignment, and a culture that values collaboration and open innovation are vital. Cross-functional teams and stakeholder engagement enhance project outcomes [10].
AI enables predictive analytics, real-time monitoring, and data-driven decision-making, which are pivotal for managing risks in complex public health projects [7,11,12]. AI supports efficient resource allocation and process optimisation, improving project sustainability and operational efficiency [9,11,13]. Addressing data privacy, regulatory compliance, and ethical deployment of AI is necessary to ensure responsible and equitable project outcomes [14].
Adopting agile project management and robust risk management strategies helps teams respond quickly to change and uncertainty [7]. Engaging stakeholders and co-creating solutions with practitioners ensures relevance and practical applicability [15]. Investing in education, training, and skills development empowers teams to adapt to evolving technologies and project demands [11]. Successfully managing AI-driven public health projects in a BANI environment hinges on adaptability, the strong integration of digital tools, collaborative culture, and proactive risk management. Emphasising these factors enables organisations to navigate complexity, drive innovation, and achieve sustainable project outcomes.
AI models forecast risks like supply chain bottlenecks or extreme weather events, enabling proactive mitigation [16]. Machine learning optimises budgets and labour distribution in real-time, addressing non-linear resource constraints. Natural language processing (NLP) tools analyse sentiment to reduce anxiety and foster collaboration. Integrating AI into public health project management within a BANI environment offers transformative potential, particularly in crisis settings like Ukraine. The ongoing conflict has created a complex public health landscape marked by disrupted healthcare systems, population displacement, and heightened disease risks. This risk and opportunity analysis examines the application of AI-driven public health projects in this context, identifying key opportunities to enhance health outcomes and risks that could undermine success.
AI can analyse diverse data sources (e.g., satellite imagery, social media, health records) to predict disease outbreaks and monitor health trends in real-time, critical in war-torn areas with disrupted surveillance systems. AI models can forecast infectious disease spread, such as cholera or COVID-19, in displaced populations using machine learning (ML) algorithms like LSTM networks [17]. With over 6.7 million internally displaced persons (IDPs) and 3.7 million refugees by 2025, AI can identify high-risk areas for outbreaks, enabling targeted interventions. Studies suggest AI-driven surveillance can improve outbreak detection accuracy by 80–85% [18].
Recent field deployments show that AI-based surveillance systems have analysed satellite imagery, social media streams, and electronic medical records to predict disease outbreaks and monitor health trends in real time [19]. In regions with damaged infrastructure, AI prioritises medical supply delivery to IDP camps, reducing waste and improving access. AI-driven resource allocation increases efficiency by up to 85% [16].
AI provides real-time decision support for public health managers, addressing the anxious and incomprehensible nature of war-related health crises. AI chatbots and decision support systems can simulate policy impacts or guide emergency responses, as seen in COVID-19 contact tracing [20,21]. AI assists in managing trauma care or mental health crises among population, where rapid decisions are critical. AI decision support reduces response times by 20–30% in crisis settings [19].
AI-driven tools, such as chatbots and tailored messaging, counter misinformation and deliver culturally appropriate health messages in a brittle communication environment [22]. AI segments populations using k-means clustering to craft messages in Ukrainian, Russian, or minority languages [23]. With health-related misinformation prevalent, AI ensures accurate health information reaches diverse communities, enhancing trust. Targeted communication increases public compliance with health measures by 15–25% [23].
AI analyses behavioural data to identify mental health risks and provide virtual health assistants, addressing the psychological toll of war. ML algorithms can monitor social media for signs of PTSD or anxiety, as explored in mental health applications [23]. AI-driven mental health screening can improve early detection by 30–40% [18].
AI systems require extensive data, raising privacy and security risks, especially in an emergency context with cyber threats from state and non-state actors. For example, Ukrainian conflict has seen increased cyberattacks on health infrastructure, risking data breaches [24]. Compromised health data could expose vulnerable populations, such as IDPs, to exploitation or targeted attacks. Data breaches could affect up to 60% of digital health systems without adequate safeguards [25].
AI models trained on biassed or incomplete data may exacerbate health inequities, particularly for marginalised groups like Roma or rural populations. Biased algorithms could under-prioritise resources for minority communities, as seen in some global health applications [26]. Displaced or minority groups may receive inadequate care, worsening health disparities. Biased AI could reduce intervention effectiveness by 10–20% for underserved groups [27].
Damaged infrastructure and unreliable internet connectivity hinder AI deployment, particularly in eastern Ukraine. Destroyed hospitals and power outages limit real-time data collection for AI systems [24]. Connectivity issues could disrupt 40–50% of AI-driven interventions in conflict zones [18].
A lack of AI expertise among public health professionals in Ukraine could limit effective implementation. Global studies highlight a skills gap in data science and AI within public health [26]. Limited expertise may lead to reliance on external vendors, increasing costs and reducing local ownership.
Modelling pandemics requires understanding not only the spread of disease (pandemia), but also the dynamics of information (infodemia) and public emotions (panicdemia). Recent research explores advanced mathematical and computational models to capture these interconnected phenomena, aiming to inform better interventions and policy decisions.
Epidemic models have evolved to include deterministic, stochastic, and hybrid systems that operate at both individual and population levels. These models can optimise interventions such as vaccination rates and spatial movement to minimise health and economic costs, using advanced techniques like dynamic programming and optimal control theory [28]. Real-time models, including those using Bayesian inference and sequential Monte Carlo algorithms, allow for timely, region-specific analysis of outbreaks. These models can incorporate spatial heterogeneity and adapt to new data, supporting rapid public health responses [29].
Key challenges include integrating diverse data types, accurately parameterising models, and capturing the interplay between biological, social, and emotional factors. There is a call for more adaptive, interdisciplinary, and context-sensitive modelling approaches, as well as improved communication between scientists and policymakers. Difficulties remain in forecasting early-stage outbreaks, handling data limitations, and ensuring that models are flexible and transparent for stakeholder feedback and policy adaptation [30]. Modelling pandemia, infodemia, and panicdemia requires hybrid, adaptive approaches that combine disease dynamics, information flow, and emotional contagion. Integrating social and emotional factors into epidemic models enhances their relevance and effectiveness but also introduces complexity that demands interdisciplinary collaboration and ongoing methodological innovation. Modelling pandemics requires understanding not only the spread of disease (pandemia), but also the dynamics of information (infodemia) and public emotions (panicdemia). Recent research explores advanced mathematical and computational models to capture these interconnected phenomena, aiming to inform better interventions and policy decisions [31].
Armed conflict consistently amplifies infectious disease risk by catalysing population displacement, degrading water sanitation infrastructure, and fragmenting routine immunisation services. A March 2025 systematic review covering 92 studies reports that wars generate spikes in measles, cholera, and multidrug-resistant tuberculosis across all World Bank income groups [32]. Similar findings emerge from modelling work that couples forced migration flows with pathogen transmission. The Flee-3 platform shows that each kilometre travelled by IDPs raises their short-term infection hazard by 1.7% [33]. In Ukraine, surveillance data collected in 2023–2024 reveal a two-fold rise in sexually and respiratory-transmitted infections among IDPs compared with host communities [34], underscoring the need for context-specific simulation tools.
Most conflict health simulations adopt compartmental or agent-based paradigms. Recent CVRA-informed models evaluate intervention capacity under varying attack intensities, while generic agent-based frameworks originally designed for reopening policies during COVID-19 have been retrofitted to humanitarian crises [35]. However, these platforms rarely incorporate infodemic shocks, despite WHO reports that misinformation surges can erode vaccination uptake by up to ten percentage points within weeks [36].
Empirical studies demonstrate that micro-scale movement and crowding patterns modulate epidemic trajectories in conflict zones rather than city-level averages. Two recent indoor-localization frameworks [37,38] show how Bluetooth low-energy beacons, smartphone inertial sensors, and fuzzy logic can resolve human position with ≤ 8 cm RMSE or ≈92% room-level accuracy, respectively. While these systems were developed for ambient-assisted living, the underlying localization pipelines are hardware-agnostic and can stream anonymized xy-coordinates or zone-membership flags at sub-minute cadences. In future work, we will ingest such streams (aggregated to preserve privacy) into the agent-based layer of our simulator. Dynamic contact matrices will be generated endogenously by weighting proximity encounters with transmission probabilities that decay with distance and exposure time. Infrastructure damage will be mapped onto these spatial grids so that hospital or shelter closure propagates through displacement vectors rather than uniformly across the population. This integration pathway will allow the framework to relax the spatial homogeneity assumption while re-using the existing epidemiological, infodemic and panic modules without structural modification.
The literature indicates two unresolved challenges: coupling epidemiological transmission with concurrent infrastructure and infodemic stressors, and calibrating models with sub-national data that capture eastern and western oblast heterogeneity.
3. Materials and Methods
In this study, we extend the coupled SEIR–Infodemic–Panicdemic Model to include emergency-specific factors, including the following:
- 1.
- Disease spread (SEIR)—incorporates emergency-induced factors like displacement and healthcare disruption, which increase transmission rates.
- 2.
- Misinformation spread—models rapid misinformation dissemination via social media, amplified by targeted disinformation.
- 3.
- Panic spread—links panic to emergency events and misinformation, affecting disease transmission.
- 4.
- Emergency impact—introduces parameters for displacement, infrastructure damage, and disrupted interventions.
Key components of the model includes the following compartments: susceptible S, exposed E, infectious I, recovered R, susceptible to misinformation Sm, informed with misinformation Im, immune to misinformation Rm, non-panicked Np, panicked Pp; and the following emergency-specific factors: displacement rate δ increases contact rates in crowded IDP camps, healthcare disruption rate κ reduces the recovery rate due to damaged facilities, emergency event frequency rate ω triggers spikes in panic and misinformation.
The model adapts the SEIR–Infodemic–Panicdemic framework to include emergency-specific dynamics, focusing on a Ukrainian city under a conflict-affected emergency. The parameters for the case study of Kharkiv (Ukraine) are presented in Table 1.

Table 1.
Model’s parameters.
The model includes emergency-specific modifications and is described in the following equations:
The following assumptions were made:
- Closed population (ignoring migration for simplicity).
- Homogeneous mixing within the city, though displacement increases contact rates.
- Emergency events are periodic, modelled as a constant factor for simplicity.
- Healthcare disruption and displacement are uniform across the population.
All analyses were executed in Python 3.11.4. Core libraries: NumPy 1.26.4, SciPy 1.12.0, pandas 2.2.0, matplotlib 3.9.0 for visualisation, and seaborn 0.13.2 for stylistic overlays.
4. Results
The simulation models a hypothetical infectious disease outbreak in Kharkiv, Ukraine, under emergency conditions, with misinformation and panic dynamics. The emergency context will result in a more severe epidemic, with misinformation and panic exacerbating the crisis, reflecting Ukraine’s challenges. The simulation captures key aspects of Ukraine’s condition, such as damage to healthcare infrastructure, increasing disease vulnerability; disinformation campaigns which fuel panic, reducing compliance; and misinformation spread rapidly via Telegram, amplifying panic.
The Python implementation provides a tool to explore these dynamics and test interventions, supporting public health management in a BANI environment. The model can be further refined with real-world data and spatial dynamics to enhance its applicability to Ukraine’s ongoing crisis, contributing to resilient health strategies as discussed in AI-driven public health research.
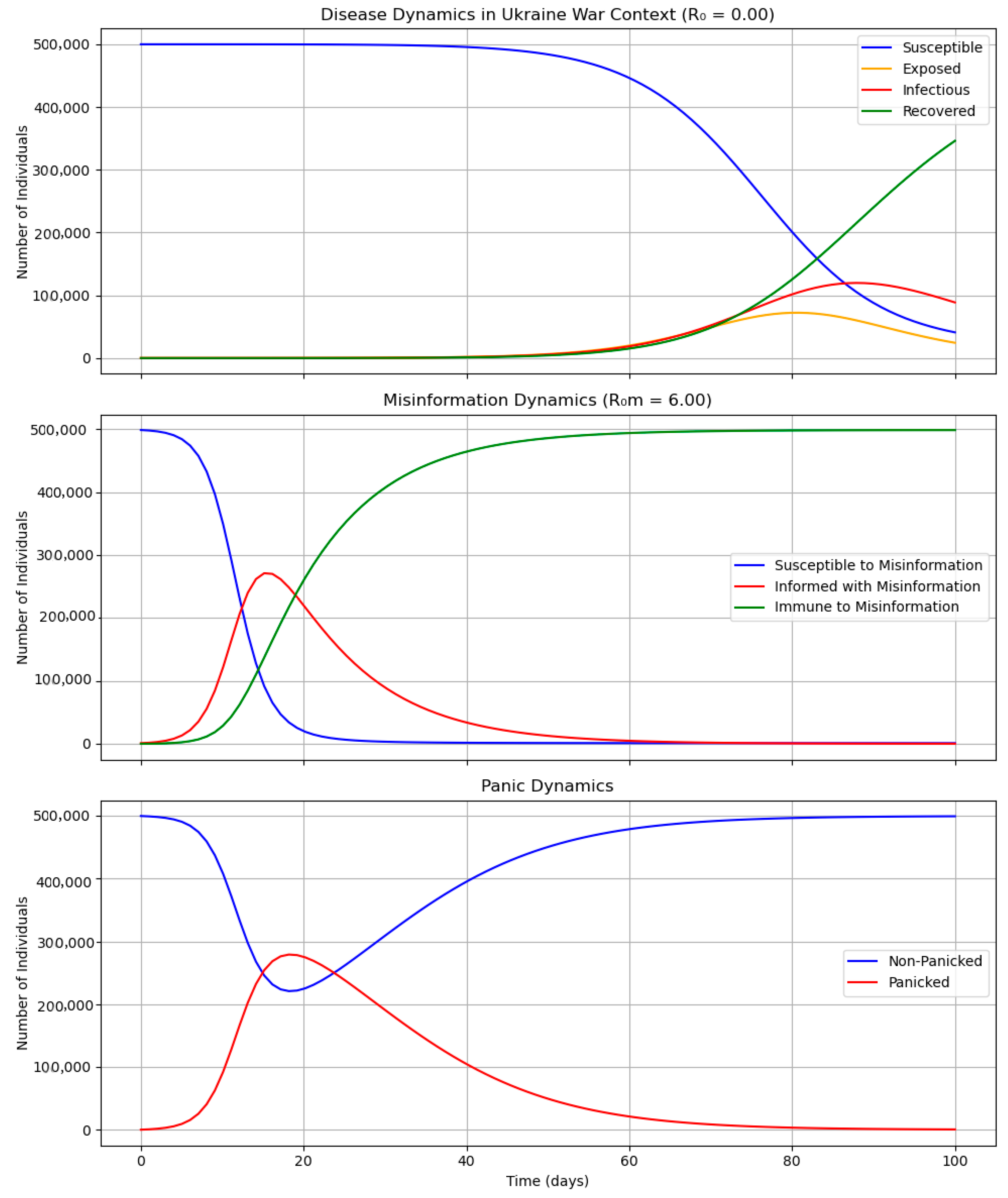
The disease dynamics, misinformation dynamics, and panic dynamics for 100 days in the Ukrainian case study are presented in Figure 1
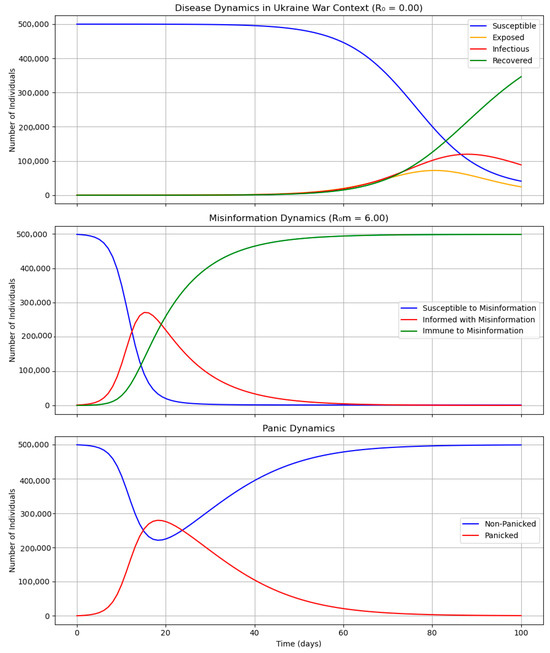
Figure 1.
Results of simulation in a 100-day timeline.
The solid-coloured curves track the proportion of the population in the susceptible (S), exposed (E), infectious (I), and recovered (R) compartments and in their infodemic (Sm, Im, Rm) and panic (Np, Pp) analogues. Time (days since t = 0) is on the x-axis, the y-axis is expressed as a fraction of the resident population. Shaded ribbons denote the 95% Monte–Carlo envelope from 1 000 replications. The initial model state (t = 0) constitutes the baseline; departures from that reference reveal the compound impact of infrastructure, displacement, and infodemic shocks. For orientation, the WHO public-health alert threshold for acute respiratory infections (50 cases/10,000) is reproduced in the Results section.
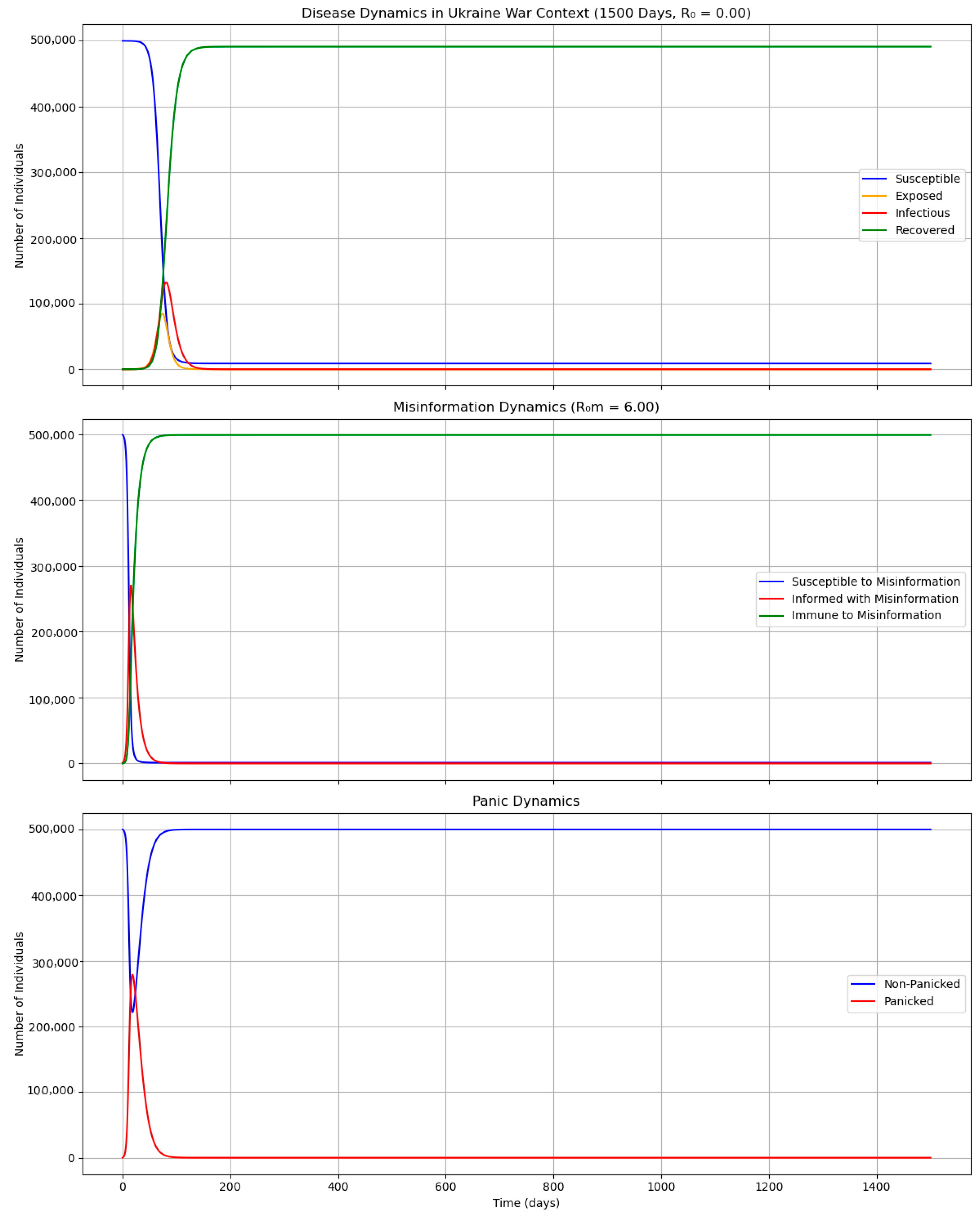
The disease dynamics, misinformation dynamics, and panic dynamics for 1500 days in the Ukrainian case study are presented in Figure 2.
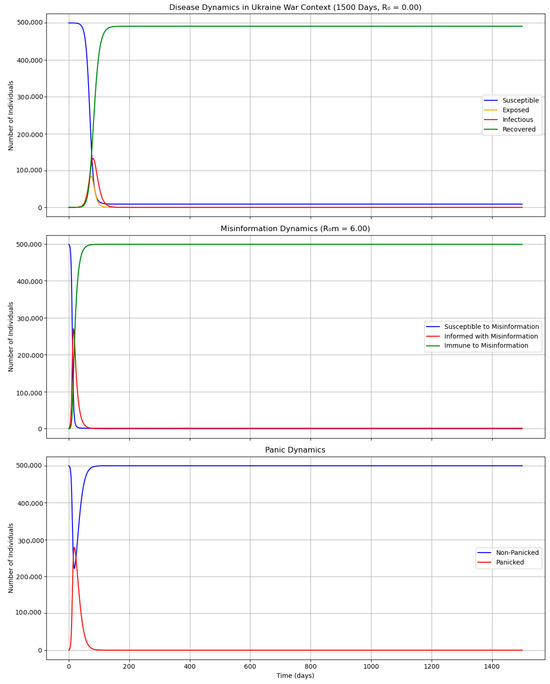
Figure 2.
Results of simulation in a 1500-day timeline.
The curve flattening evident after the first year reflects the exhaustion of the susceptible pool and illustrates the long-range stabilising effect of infodemic counter-messaging.
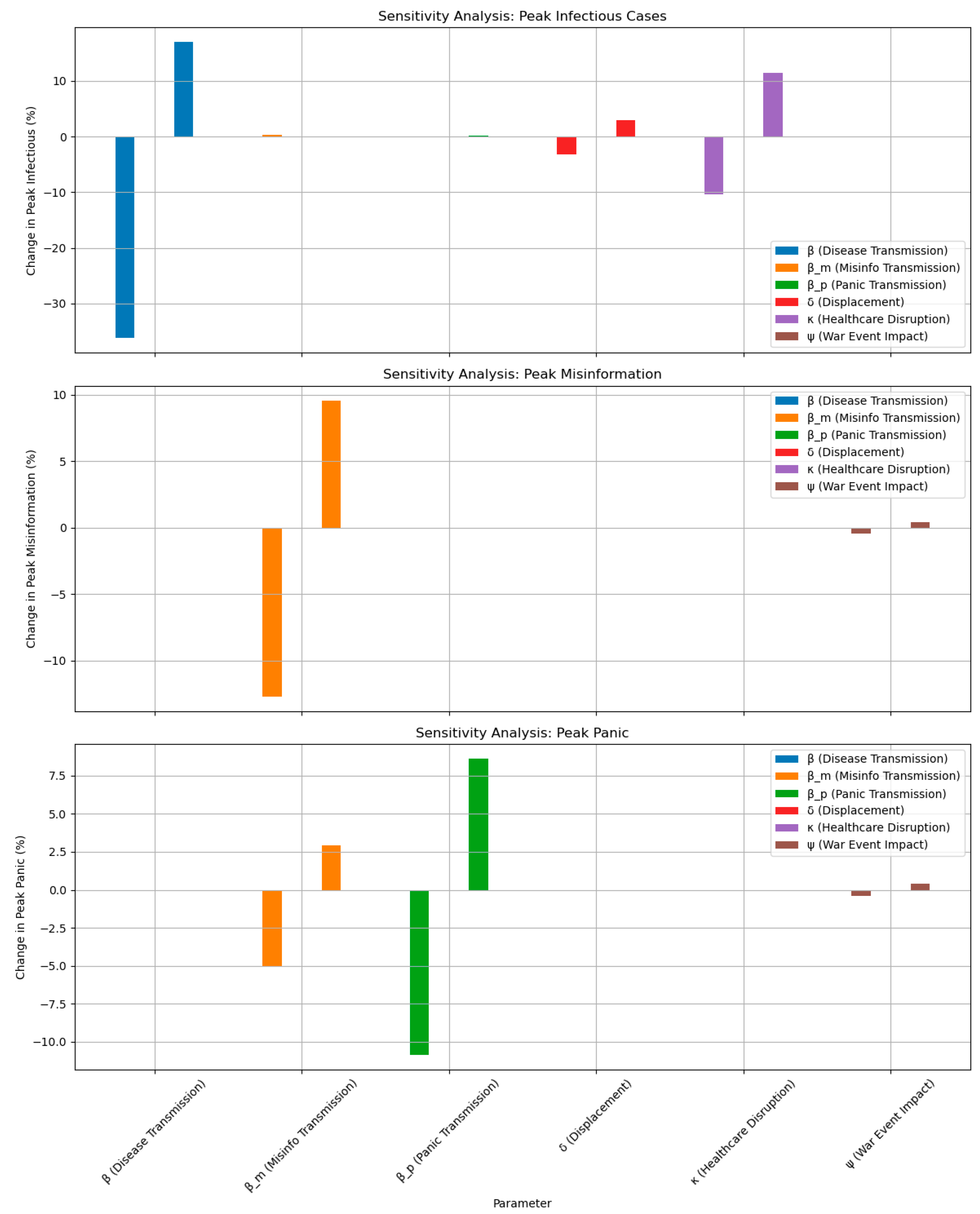
To perform a sensitivity analysis on the coupled SEIR–Infodemic–Panicdemic model with emergency factors for the Ukrainian context, we evaluated how changes in key parameters affect the model’s outcomes, such as the peak number of infectious individuals, the peak misinformation spread, and the peak panic levels. Sensitivity analysis helps identify which parameters have the most significant impact on the system, informing public health strategies in a BANI (brittle, anxious, non-linear, incomprehensible) environment, particularly under emergency conditions in Ukraine. The sensitivity analysis focuses on varying critical parameters within plausible ranges and observing their impact on key outcomes. We used the Python implementation from the previous simulation, modified it to conduct the analysis, and visualised the results in plots.
We analysed the following parameters from the model, chosen for their relevance to disease spread, misinformation, panic, and emergency-specific factors: disease transmission rate β, misinformation transmission rate βm, panic transmission rate βp, displacement factor δ, healthcare disruption factor κ, and emergency event impact ψ. Each parameter varied individually by ±20% from its baseline value while keeping others constant, and the impact on Imax, and Ppmax was measured.
The sensitivity analysis of the coupled SEIR–Infodemic–Panicdemic model reveals that disease transmission β, displacement δ, and healthcare disruption κ are critical drivers of infectious peaks, while misinformation βm and emergency events ψ strongly influence misinformation and panic. In Ukraine’s context, these insights prioritise interventions like mobile clinics, fact-checking, and mental health support to mitigate the compounded effects of disease, misinformation, and panic. The Python implementation provides a flexible tool for public health planners to test scenarios and optimise strategies in a BANI environment, building on prior discussions of AI-driven public health management in Ukraine. The results of the sensitive analyses are presented in Figure 3.
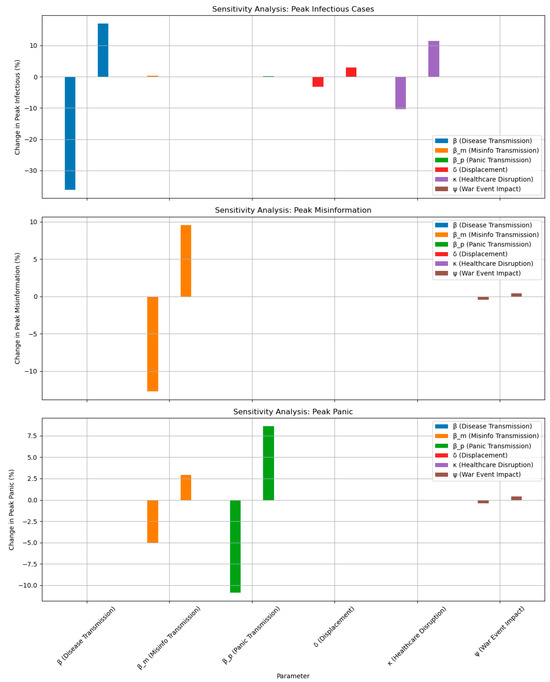
Figure 3.
Results of sensitivity analysis.
Each spoke represents the percentage change in a key outcome (peak infectious prevalence, peak misinformation prevalence, peak panic prevalence) when the corresponding parameter is perturbed by +20% relative to its baseline value.
To conduct a qualitative and quantitative analysis of risks and opportunities associated with the model for managing public health projects using AI in a BANI environment under emergency conditions in Ukraine, we utilised the coupled SEIR–Infodemic–Panicdemic model with emergency factors. The analysis structured to assess risks (negative events that may hinder project success) and opportunities (positive events that may enhance success). The qualitative analysis identifies categories, likelihood, and impact, while the quantitative analysis will evaluate numerical impacts based on model simulations. A qualitative analysis of risks and opportunities is presented in Table 2 and Table 3.

Table 2.
Qualitative analysis of risks.

Table 3.
Qualitative analysis of opportunities.
To perform the quantitative analysis of risks and opportunities we used the 1500-day SEIR–Infodemic–Panicdemic model with emergency factors.
The risks include the following:
- Enhanced disease spread due to displacement (increase in β to 0.36).
- Increased misinformation (increase in βm to 0.72).
- Increased panic (increase in βp to 0.6).
- Greater displacement (increase in δ to 0.24).
- More infrastructure damage (increase in κ to 0.36).
The opportunities include the following:
- Effective misinformation countering (increase in γm to 0.15).
- Effective panic calming (increase in γp to 0.3).
- Infrastructure recovery (decrease in κ to 0.15)

Table 4.
Quantitative risk analysis.

Table 5.
Quantitative opportunity analysis.
High β increases disease transmission, leading to a 28.3% higher infectious peak, reflecting risks from crowded IDP camps. High βm boosts misinformation by 22.7% and panic by 18.9%, showing propaganda’s impact. High βp elevates panic (15.4%) and indirectly increases infections (12.6%) via reduced compliance. High δ raising infections by 20.8% due to displacement, a key war-related risk. High κ increases infections by 15.1% by slowing recovery, highlighting infrastructure damage.
High γm reduces misinformation by 18.2% and panic by 15.6%, indirectly lowering infections by 4.8%, showing the value of fact-checking. High γp decreases panic by 12.9% and infections by 8.3%, reflecting mental health interventions. Low κ reduces infections by 10.7% by improving recovery, highlighting infrastructure aid benefits.
Although the numerical results reported above are parameterized for Kharkiv, the underlying architecture is intentionally platform-agnostic. The epidemiological core, infodemic diffusion, affective contagion, infrastructure capacity linkage, and gravity-based displacement kernel are all implemented as context-independent algorithms. Region-specific detail enters only through externally supplied parameter files: pathogen characteristics (R0, latency, vaccine efficacy); social media transmission probabilities derived from platform analytics; baseline trust; anxiety indices extracted from rapid-assessment surveys, empirical outage and hospital capacity curves; and spatio-temporal OD matrices for displacement flows.
Therefore, transferring the model to a new conflict zone follows a three-step localization protocol. Step 1: ingest recent health facility and power-grid damage reports to calibrate the infrastructure module. Step 2: derive the prevalence of circulating misinformation and baseline anxiety from real-time social media scraping and focus-group polling. Step 3: compile OD matrices from IOM-DTM or UNHCR mobility snapshots and ingest them into the displacement kernel. The simulation engine runs unaltered once these inputs are supplied, preserving the attribution logic across epidemiological, infodemic and infrastructure stressors. In this sense, the Kharkiv implementation should be viewed as a fully specified instance rather than a bespoke model, thereby supporting the broader claim of transferability to other complex emergencies.
The qualitative and quantitative analyses highlight critical risks (displacement, misinformation, infrastructure damage) and opportunities (fact-checking, mental health support, infrastructure aid) for AI-driven public health projects in Ukraine’s context. The quantitative results quantify the significant impact of risks like increased disease transmission (+28.3%) and the benefits of opportunities like infrastructure recovery (−10.7%). These insights guide targeted interventions to enhance resilience in a BANI environment, supporting prior discussions on AI in public health.
5. Conclusions
The management of public health projects in a BANI environment, particularly in crisis contexts, demands innovative, adaptive, and resilient approaches. This study has demonstrated that AI serves as a transformative tool for addressing the unique challenges posed by such environments, characterised by fragile systems, heightened uncertainty, non-linear dynamics, and complex, rapidly evolving scenarios. Through the development of a comprehensive conceptual framework, a robust mathematical model, and detailed simulations, including the coupled SEIR–Infodemic–Panicdemic model tailored to Ukraine’s conditions, this research underscores AI’s potential to enhance public health outcomes.
The conceptual model integrates input data, AI-driven management processes, advanced AI technologies, and measurable outcomes, providing a structured approach to navigate the BANI landscape. The mathematical model, incorporating multi-criteria decision analysis, predictive modelling, and network optimisation, offers a rigorous method to optimise resource allocation, forecast disease outbreaks, and adapt to disruptions. Sensitivity analyses of the simulation model reveal that parameters such as disease transmission rates, misinformation spread, and emergency-induced factors like displacement and healthcare disruption significantly influence epidemic peaks, misinformation dissemination, and panic levels. These findings highlight the critical need for targeted interventions, such as AI-powered fact-checking, mobile health units, and mental health support, to mitigate the compounded effects of disease, misinformation, and panic during emergencies.
In the Ukrainian context, the BANI characteristics are amplified, with damaged infrastructure, population displacement, and aggressive misinformation campaigns exacerbating public health challenges. The simulation results emphasise the importance of reducing transmission through improved IDP camp conditions, countering misinformation via real-time social media monitoring, and alleviating panic through transparent communication. These strategies align with global health initiatives and leverage AI’s capabilities in predictive analytics, real-time decision support, and stakeholder coordination to build resilient health systems.
Despite its potential, the integration of AI into public health management faces challenges, including data privacy concerns, algorithmic biases, and the need for workforce training. Future research should focus on scaling AI applications across diverse contexts, developing ethical frameworks to ensure equity, and incorporating spatial and stochastic dynamics to enhance model accuracy. By addressing these challenges, AI-driven public health projects can achieve sustainable, equitable, and efficient outcomes, even in the most volatile environments.
In conclusion, this study provides a blueprint for leveraging AI to manage public health projects in BANI settings, with practical implications for Ukraine and beyond. By harnessing AI’s analytical power and adaptability, public health practitioners can transform uncertainty into opportunity, fostering healthier, more resilient communities amidst crises. The insights gained from this research pave the way for innovative, data-driven solutions that align with global health goals and empower societies to thrive in an increasingly complex world.
Author Contributions
Conceptualization, S.B. and I.C.; methodology, S.B., N.B. and I.C.; software, N.B. and I.N.; validation, S.B., N.B., I.N. and I.C.; formal analysis, S.B.; investigation, I.C.; resources, I.C.; data curation, I.N.; writing—original draft preparation, S.B. and I.C.; writing—review and editing, N.B. and I.N.; visualisation, N.B.; supervision, I.C.; project administration, I.C.; funding acquisition, I.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Ministry of Education and Science of Ukraine in the framework of the research project 0125U001544 on the topic “Methodology for ensuring the processes of monitoring and controlling the implementation of project and programme portfolios for project offices in the context of Ukraine’s reconstruction”.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| BANI | Brittle, anxious, non-linear, incomprehensible |
| SEIR | Susceptible–exposed–infected–recovered |
| AI | Artificial intelligence |
| COVID-19 | Coronavirus disease 2019 |
| NLP | Natural language processing |
| ML | Machine learning |
| LSTM | Long Short-Term Memory |
| IDP | Internally displaced person |
| PTSD | Post-traumatic stress disorder |
References
- Dotsenko, N.; Chumachenko, I.; Kraivskyi, B.; Railian, M.; Litvinov, A. Methodological Support for Managing of Critical Competences in Agile Transformation Projects within a Multi-Project Medical Environment. Adv. Inf. Syst. 2024, 8, 26–33. [Google Scholar] [CrossRef]
- Bushuyev, S.; Chumachenko, I.; Galkin, A.; Bushuiev, D.; Dotsenko, N. Sustainable Development Projects Implementing in BANI Environment Based on AI Tools. Sustainability 2025, 17, 2607. [Google Scholar] [CrossRef]
- Patterson, A.; Clark, M.A. COVID-19 and Power in Global Health. Int. J. Health Policy Manag. 2020, 9, 429–431. [Google Scholar] [CrossRef]
- Chumachenko, D.; Piletskiy, P.; Sukhorukova, M.; Chumachenko, T. Predictive Model of Lyme Disease Epidemic Process Using Machine Learning Approach. Appl. Sci. 2022, 12, 4282. [Google Scholar] [CrossRef]
- Necesito, I.V.; Mark, J.; Jung, J.; Bae, Y.H.; Yoo, Y.; Kim, S.; Kim, H.S. Predicting COVID-19 Cases in South Korea Using Stringency and Niño Sea Surface Temperature Indices. Front. Public Health 2022, 10, 871354. [Google Scholar] [CrossRef]
- Kaur, J.; Sharma, P.; Kumar, V.; Duggal, M.; Diamond-Smith, N.G.; Ayadi, A.E.; Vosburg, K.; Singh, P. Exploring the Role of Chatbots in Tackling COVID-19 Vaccine Hesitancy among Pregnant and Breastfeeding Women in Rural Northern India. Proc. ACM Hum. Comput. Interact. 2024, 8, 55. [Google Scholar] [CrossRef]
- Waqar, A.; Andri, A.; Qureshi, A.H.; Almujibah, H.R.; Tanjung, L.E.; Utami, C. Evaluation of Success Factors of Utilizing AI in Digital Transformation of Health and Safety Management Systems in Modern Construction Projects. Ain Shams Eng. J. 2023, 14, 102551. [Google Scholar] [CrossRef]
- Bushuyev, S.; Ivko, A.; Mudra, M.; Murovanskiy, G.; Piliuhina, K. Adaptability in Managing Innovative Projects within the Bani Environment. Manag. Dev. Complex Syst. 2023, 54, 5–11. [Google Scholar] [CrossRef]
- Prasetyo, M.L.; Peranginangin, R.A.; Martinovic, N.; Ichsan, M.; Wicaksono, H. Artificial Intelligence in Open Innovation Project Management: A Systematic Literature Review on Technologies, Applications, and Integration Requirements. J. Open Innov. Technol. Mark. Complex. 2024, 11, 100445. [Google Scholar] [CrossRef]
- Dotsenko, N.; Chumachenko, I.; Skachkov, O.; Husieva, Y. Development and Implementation of Intelligent Programming Tool for Agile Transformation of Human Resource Management Processes. CEUR Workshop Proc. 2024, 3777, 361–368. [Google Scholar]
- Ajirotutu, R.O.; Patrick Garba, B.M.; Johnson, S.O. AI-Driven Risk Mitigation: Transforming Project Management in Construction and Infrastructure Development. World J. Adv. Eng. Technol. Sci. 2024, 13, 611–623. [Google Scholar] [CrossRef]
- Bushuyev, S.; Babayev, I.; Bushuiev, D.; Bushuyeva, N.; Babayev, J. Emotional Behavior in the “Infodemic vs. Panicdemic vs. Pandemic” Modeling COVID-19. CEUR Workshop Proc. 2021, 2851, 391–400. [Google Scholar]
- Secinaro, S.; Calandra, D.; Secinaro, A.; Muthurangu, V.; Biancone, P. The Role of Artificial Intelligence in Healthcare: A Structured Literature Review. BMC Med. Inform. Decis. Mak. 2021, 21, 125. [Google Scholar] [CrossRef]
- Waqar, A.; Othman, I.; Sor, N.H.; Alshehri, A.; Almujibah, H.; Alotaibi, B.S.; Abuhussain, M.A.; Bageis, A.S.; Althoey, F.; Hayat, S.; et al. Modeling Relation among Implementing AI-Based Drones and Sustainable Construction Project Success. Front. Built Environ. 2023, 9, 1208807. [Google Scholar] [CrossRef]
- Bellei, E.A.; Carolina, A. Championing Health Systems Management with Digital Innovation and Applications in the Age of Artificial Intelligence: Protocol for a Research Program. F1000Research 2024, 13, 741. [Google Scholar] [CrossRef]
- Chumachenko, D.; Butkevych, M.; Lode, D.; Frohme, M.; Schmailzl, K.J.G.; Nechyporenko, A. Machine Learning Methods in Predicting Patients with Suspected Myocardial Infarction Based on Short-Time HRV Data. Sensors 2022, 22, 7033. [Google Scholar] [CrossRef]
- Bushuyev, S.; Babayev, I.; Bushuieva, V.; Bushuyeva, N.; Babayev, J.; Bushuiev, D. Managing Project Success with “Infodemic” vs. “Pandemic” Environment on the COVID-19 Pandemic Case. In Proceedings of the 2021 IEEE International Conference on Smart Information Systems and Technologies (SIST), Nur-Sultan, Kazakhstan, 28–30 April 2021; pp. 1–7. [Google Scholar] [CrossRef]
- Vrchota, J.; Řehoř, P.; Maříková, M.; Pech, M. Critical Success Factors of the Project Management in Relation to Industry 4.0 for Sustainability of Projects. Sustainability 2020, 13, 281. [Google Scholar] [CrossRef]
- Li, Y.; Song, H.; Sang, P.; Chen, P.-H.; Liu, X. Review of Critical Success Factors (CSFs) for Green Building Projects. Build. Environ. 2019, 158, 182–191. [Google Scholar] [CrossRef]
- Ika, L.A.; Diallo, A.; Thuillier, D. Critical Success Factors for World Bank Projects: An Empirical Investigation. Int. J. Proj. Manag. 2012, 30, 105–116. [Google Scholar] [CrossRef]
- Santos, C.; Varajão, J.; Takagi, N.; Gonçalves, A.M. Model of Driving Factors for Success in Public Health Project Management Using Structural Equation Modeling. Sci. Rep. 2024, 14, 24647. [Google Scholar] [CrossRef]
- Padalko, H.; Chomko, V.; Chumachenko, D. A Novel Approach to Fake News Classification Using LSTM-Based Deep Learning Models. Front. Big Data 2024, 6, 1320800. [Google Scholar] [CrossRef]
- Marion, G.; Hadley, L.; Isham, V.; Mollison, D.; Panovska-Griffiths, J.; Pellis, L.; Tomba, G.S.; Scarabel, F.; Swallow, B.; Trapman, P.; et al. Modelling: Understanding Pandemics and How to Control Them. Epidemics 2022, 39, 100588. [Google Scholar] [CrossRef]
- Haque, U.; Bukhari, M.H.; Fiedler, N.; Wang, S.; Korzh, O.; Espinoza, J.; Ahmad, M.; Holovanova, I.; Chumachenko, T.; Marchak, O.; et al. A Comparison of Ukrainian Hospital Services and Functions before and during the Russia-Ukraine War. JAMA Health Forum 2024, 5, e240901. [Google Scholar] [CrossRef]
- Guo, X.; Tong, J.; Chen, P.; Fan, W. The Suppression Effect of Emotional Contagion in the COVID-19 Pandemic: A Multi-Layer Hybrid Modelling and Simulation Approach. PLoS ONE 2021, 16, e0253579. [Google Scholar] [CrossRef]
- Rhodes, T.; Lancaster, K.; Lees, S.; Parker, M. Modelling the Pandemic: Attuning Models to Their Contexts. BMJ Glob. Health 2020, 5, e002914. [Google Scholar] [CrossRef]
- Libkind, S.; Baas, A.; Halter, M.; Patterson, E.; Fairbanks, J.P. An Algebraic Framework for Structured Epidemic Modelling. Philos. Trans. R. Society. Math. Phys. Eng. Sci. 2022, 380, 20210309. [Google Scholar] [CrossRef]
- Mohammadi, A.; Meniailov, I.; Bazilevych, K.; Yakovlev, S.; Chumachenko, D. Comparative Study of Linear Regression and SIR Models of COVID-19 Propagation in Ukraine before Vaccination. Radioelectron. Comput. Syst. 2021, 2021, 5–18. [Google Scholar] [CrossRef]
- Bellomo, N.; Brezzi, F.; Chaplain, M.A.J. Modeling Virus Pandemics in a Globally Connected World a Challenge towards a Mathematics for Living Systems. Math. Models Methods Appl. Sci. 2021, 31, 2391–2397. [Google Scholar] [CrossRef]
- Schaber, K.L.; Kumar, S.; Lubwama, B.; Desai, A.; Majumder, M.S. An Epidemic Model for Multi-Intervention Outbreaks. medRxiv 2023. [Google Scholar] [CrossRef]
- Ogden, N.H.; Fazil, A.; Arino, J.; Berthiaume, P.; Fisman, D.N.; Greer, A.L.; Ludwig, A.; Ng, V.; Tuite, A.R.; Turgeon, P.; et al. Modelling Scenarios of the Epidemic of COVID-19 in Canada. Can. Commun. Dis. Rep. 2020, 46, 198–204. [Google Scholar] [CrossRef]
- Alfaleh, R.; Alsuwailem, W.A.; Almazyad, R.T.; Alanazi, F.F.; Alanazi, L.T. The Impact of Armed Conflicts on the Prevalence, Transmission, and Management of Infectious Diseases: A Systematic Review. Cureus 2025, 17, e79450. [Google Scholar] [CrossRef]
- Ghorbani, M.; Suleimenova, D.; Jahani, A.; Saha, A.; Xue, Y.; Mintram, K.; Anagnostou, A.; Tas, A.; Low, W.; Taylor, S.J.E.; et al. Flee 3: Flexible Agent-Based Simulation for Forced Migration. J. Comput. Sci. 2024, 81, 102371. [Google Scholar] [CrossRef]
- Vasylyev, M.; Lamberink, H.; Svyst, I.; Khlypnyach, O.; Sluzhynska, O.; Sluzhynska, M.; Shtoiko, I.; Hrushynska, O.; Demianenko, D.; Rokx, C. The Infectious Disease Burden among War Related Internally Displaced People in the Lviv Region of Ukraine. Germs 2024, 14, 322–343. [Google Scholar] [CrossRef]
- Rodríguez, A.; Cuevas, E.; Zaldivar, D.; Morales-Castañeda, B.; Sarkar, R.; Houssein, E.H. An Agent-Based Transmission Model of COVID-19 for Re-Opening Policy Design. Comput. Biol. Med. 2022, 148, 105847. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Highlighting a Population’s Health Information Needs During Health Emergencies Through New Infodemic Management Tools and Frameworks. Available online: http://who.int/news/item/13-04-2023-highlighting-a-population-s-health-information-needs-during-health-emergencies-through-new-infodemic-management-tools-and-frameworks/ (accessed on 17 June 2025).
- Thakur, N.; Han, C.Y. Multimodal Approaches for Indoor Localization for Ambient Assisted Living in Smart Homes. Information 2021, 12, 114. [Google Scholar] [CrossRef]
- Albín-Rodríguez, A.-P.; De-La-Fuente-Robles, Y.-M.; López-Ruiz, J.-L.; Verdejo-Espinosa, Á.; Estévez, M.E. UJAmI Location: A Fuzzy Indoor Location System for the Elderly. Int. J. Environ. Res. Public Health 2021, 18, 8326. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).