Family Oncology Caregivers and Relational Health Literacy
Abstract
1. Introduction
Dr. Platon asked Connie to step into the hallway, leaving Ben alone in his ER patient room. Dr. Platon told Connie that Ben was dying, that any pursuit of treatment was futile, and that his liver had completely stopped functioning. Connie was dismayed. They had originally come to the hospital that morning to be cleared for gall bladder removal the following day.
2. Considering Current Definitions of Health Literacy
Connie was left to tell Ben about the change in surgical plans, and had to describe some version of what Dr. Platon told her. Ben became angry and insisted they leave the hospital. As they were walking down the hall, Dr. Platon intercepted them and spoke with both of them this time. He told Ben that he had some kind of cancer, and that he was referring them to a regional cancer center to be ‘diagnosed and staged’.
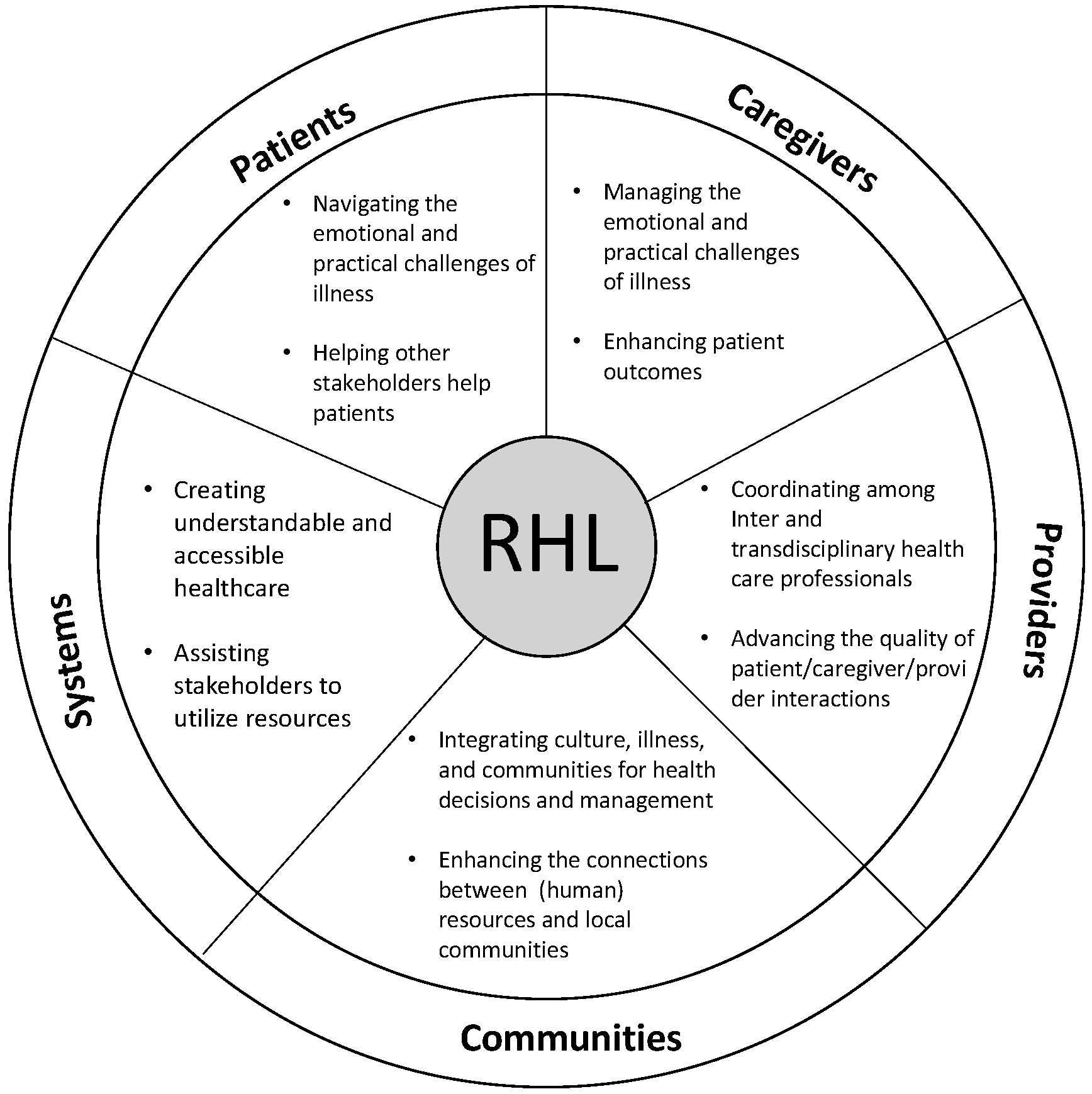
3. Conceptualizing Relational Health Literacy
Ben was diagnosed at the regional cancer center with adenocarcinoma of unknown primary site, an aggressive metastatic cancer. It was Stage IV. He had not eaten for 7 days and was struggling to drink. Unlike Dr. Platon, oncologists there did not offer suggestions about abandoning treatment, and instead referred him on to a comprehensive cancer center in southern Texas. This would mean a 10-hour grueling car ride.
3.1. Patients
Connie wanted Ben to live and to receive treatment. She had two disparate diagnoses and descriptions from providers about how Ben could navigate this illness, and was eager to act on the second version—treat and survive. Once in south Texas, Ben continued to worsen. He was too weak to sit in the clinic waiting room before his appointment, and Connie went alone instead with Ben’s records.
3.2. Caregivers
Connie met with Dr. Brown, a gastrointestinal oncologist. After a great deal of resistance, Dr. Brown acquiesced to Connie and ordered a round of chemotherapy for Ben. The infusion would start that evening if Connie could complete the payment for it before billing closed at 5 pm.
3.3. Providers
In a span of less than 10 days, Connie and Ben had entered a new universe of cancer and fear. The first chemo infusion ended early, as Ben became violently ill. He took to his bed at the hotel, and Connie waited for improvements or their next appointment, whichever might come first. They knew no one in South Texas, and they knew no one with cancer. Their hotel was far from a grocery store as it was located in downtown Houston, and Ben was too sick to be left alone.
3.4. Communities
Ben never got out of bed after his one and only chemotherapy treatment. Connie had completed the payment for $12,000.00 using their bank card. They were between health insurances and had no coverage. Both Connie and Ben were wealthy, and were in a unique position to pay outright for the single treatment. Despite their wealth, Ben and Connie were stuck in a hotel across from the hospital, and the only place to go for help was the ER. After three days of watching Ben writhe in pain, unable to take liquids or eat, Connie chartered a private plane home to Oklahoma. Once there, she initiated hospice care on her own, without the support of Dr. Platon, their local physician.
3.5. Systems
4. Conclusions and Recommendations
Author Contributions
Funding
Conflicts of Interest
References
- Laidsaar-Powell, R.; Butow, P.; Bu, S.; Charles, C.; Gafni, A.; Fisher, A.; Juraskova, I. Family involvement in cancer treatment decision-making: A qualitative study of patient, family, and clinician attitudes and experiences. Patient Educ. Couns. 2016, 99, 1146–1155. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Cho, J.; Roter, D.L.; Kim, S.Y.; Yang, H.K.; Park, K.; Kim, H.J.; Shin, H.Y.; Kwon, T.G.; Park, J.H. Attitudes toward Family Involvement in Cancer Treatment Decision Making: The Perspectives of Patients, Family Caregivers, and Their Oncologists. Psychooncology 2017, 26, 770–778. [Google Scholar] [CrossRef] [PubMed]
- Laidsaar-Powell, R.; Butow, P.; Boyle, F.; Juraskova, I. Managing challenging interactions with family caregivers in the cancer setting: Guidelines for clinicians (TRIO Guidelines-2). Patient Educ. Couns. 2018, 101, 983–994. [Google Scholar] [CrossRef] [PubMed]
- Gallup Healthways Wellbeing Survey More than One in Six American Workers Also Act as Caregivers. Available online: http://www.gallup.com/poll/148640/One-Six-American-Workers-Act-Caregivers.aspx (accessed on 2 April 2017).
- National Academies of Sciences Engineering and Medicine. Families Caring for an Aging America; National Academies Press: Washington, DC, USA, 2016. [Google Scholar]
- Sterling, M. What Family Caregivers Need from Health IT and the Healthcare System to be Effective Health Managers. Available online: http://www.connectedhealthresources.com/What_Family_Caregivers_Need_from_Health_IT_and_the_Healthcare_System_to_be_Effective_Health_Managers_Sterling_December_2014_v2.pdf (accessed on 2 April 2018).
- Smedley, B.D.; Stith, A.Y.; Nelson, A.R. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Available online: https://www.nap.edu/read/12875/chapter/1 (accessed on 1 March 2016).
- Gibson, J.; Snodgrass, J. The relationship of health literacy to the stress level of informal caregivers. Int. J. Literacies 2014, 20, 1–20. [Google Scholar] [CrossRef]
- Schulz, R.; Sherwood, P.R. Physical and mental health effects of family caregiving. Am. J. Nurs. 2008, 108, 23–27. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services, Office of Disease Prevention and Health. National Action Plan to Improve Health Literacy; U.S. Department of Health and Human Services: Washington, DC, USA, 2010.
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Health Literacy: A Prescription to End Confusion; National Academics: Washington, DC, USA, 2004. [Google Scholar]
- The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020: Phase I Report, Recommendations for the Framework and Format of Healthy People 2020. Available online: https://www.healthypeople.gov/sites/default/files/PhaseI_0.pdf (accessed on 18 August 2018).
- Center for Disease Control and Prevention. Learn about Health Literacy. Available online: https://www.cdc.gov/healthliteracy/learn/ (accessed on 2 April 2018).
- Haun, J.N.; Valerio, M.A.; McCormack, L.A.; Sørensen, K.; Paasche-Orlow, M.K. Health literacy measurement: An inventory and descriptive summary of 51 instruments. J. Health Commun. 2014, 19, 302–333. [Google Scholar] [CrossRef] [PubMed]
- Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association. Health literacy: Report of the council on scientific affairs. J. Am. Med. Assoc. 1999, 281, 552–557. [Google Scholar] [CrossRef]
- Cutilli, C.C.; Bennett, I.M. Understanding the health literacy of America results of the National Assessment of Adult Literacy. Orthop. Nurses 2009, 28, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Denning, P.; DiNenno, E. Communities in Crisis: Is There a Generalized HIV Pidemic in Lmpoverished Urban Areas of the United States? Available online: https://www.cdc.gov/hiv/group/poverty.html (accessed on 2 April 2018).
- Sorenson, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, B. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.; Wood, F.; Davies, M.; Edwards, A. ‘Distributed health literacy’: Longitudinal qualitative analysis of the roles of health literacy mediators and social networks of people living with a long-term health condition. Health Expect. 2015, 18, 1180–1193. [Google Scholar] [CrossRef] [PubMed]
- Batterham, R.W.; Hawkins, M.; Collins, P.A.; Buchbinder, R.; Osborne, R.H. Health literacy: Applying current concepts to improve health services and reduce health inequalities. Public Health 2016, 132, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Chou, W.S.; Gaysynsky, A.; Persoskie, A. Health literacy and communication in palliative care. In Textbook of Palliative Care Communication; Wittenberg, E., Ferrell, B.R., Goldsmith, J., Smith, T., Ragan, S.L., Glajchen, M., Handzo, G., Eds.; Oxford University Press: Oxford, UK, 2015; pp. 90–101. [Google Scholar]
- Young, A.J.; Stephens, E.; Goldsmith, J.V. Family caregiver communication in the ICU: Toward a relational view of health literacy. J. Fam. Commun. 2017, 17, 137–152. [Google Scholar] [CrossRef]
- Baker, D.W. The meaning and the measure of health literacy. J. Gen. Intern. Med. 2006, 21, 878–883. [Google Scholar] [CrossRef] [PubMed]
- Paasche-Orlow, M.K.; Wolf, M.S. The causal pathways linking health literacy to health outcomes. Am. J. Health Behav. 2007, 31, S19–S26. [Google Scholar] [CrossRef] [PubMed]
- Parnell, T.A. Health Literacy in Nursing: Providing Person-Centered Care; Springer Publishing Company: New York, NY, USA, 2015. [Google Scholar]
- Yuen, E.Y.N.; Dodson, S.; Batterham, R.; Knight, T.; Chirgwin, J.; Livingston, P. Development of a conceptual model of cancer caregiver health literacy. Eur. J. Cancer Care 2016, 25, 294–306. [Google Scholar] [CrossRef] [PubMed]
- National Alliance for Caregiving. From Insight to Advocacy: Addressing Family Caregiving as a National Public Health Issue; National Alliance for Caregiving: Bethesda, MD, USA, 2018. [Google Scholar]
- Chae, J.; Lee, C.J.; Jensen, J.D. Correlates of cancer information overload: Focusing on individual ability and motivation. Health Commun. 2016, 31, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Given, B.A.; Sherwood, P.; Given, C.W. Support for caregivers of cancer patients: Transition after active treatment. Cancer Epidemiol. Prev. Biomark. 2011, 20, 2015–2021. [Google Scholar] [CrossRef] [PubMed]
- Lau, D.T.; Berman, R.; Halpern, L.; Pickard, A.S.; Schrauf, R.; Witt, W. Exploring factors that influence informal caregiving in medication management for home hospice patients. J. Palliat. Med. 2010, 13, 1085–1090. [Google Scholar] [CrossRef] [PubMed]
- Mayahara, M. Pain medication management by hospice caregivers. J. Pain 2011, 12, P27. [Google Scholar] [CrossRef]
- Miaskowski, C.; Dodd, M.J.; West, C.; Paul, S.M.; Tripathy, D.; Koo, P.; Schumacher, K. Lack of adherence with the analgesic regimen: A significant barrier to effective cancer pain management. J. Clin. Oncol. 2001, 19, 4275–4279. [Google Scholar] [CrossRef] [PubMed]
- Wittenberg Lyles, E.; Goldsmith, J.; Ragan, S.; Sanchez-Reilly, S. Dying with Comfort: Family Illness Narratives and Early Palliative Care; Hampton Press: New York, NY, USA, 2010. [Google Scholar]
- Goldsmith, J.; Wittenberg Lyles, E.; Shaunfield, S.; Sanchez-Reilly, S. Unfolding case responses to a palliative appropriate patient: A reflective practice dilemma when the case does not fit the algorithm. Am. J. Hospice Palliat. Med. 2011, 26, 236–241. [Google Scholar]
- Fernandez, D.M.; Larson, J.L.; Zikmund-Fisher, B.J. Associations between health literacy and preventive health behaviors among older adults: Findings from the health and retirement study. BMC Public Health 2016, 16, 596. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.; Braun, K.L. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J. Health Commun. 2012, 17, 82–99. [Google Scholar] [CrossRef] [PubMed]
- Leung, A.Y.M.; Bo, A.; Hsiao, H.Y.; Wang, S.S.; Chi, I. Health literacy issues in the care of Chinese American immigrants with diabetes: A qualitative study. BMJ Open 2014, 4, e005294. [Google Scholar] [CrossRef] [PubMed]
- White, R.O.; Chakkalakal, R.J.; Presley, C.A.; Bian, A.; Schildcrout, J.S.; Wallston, K.A.; Barto, S.; Kripalani, S.; Rothman, R. Perceptions of provider communication among vulnerable patients with diabetes: Influences of medical mistrust and health literacy. J. Health Commun. 2016, 21, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Schinckus, L.; Dangoisse, F.; Van den Broucke, S.; Mikolajczak, M. When knowing is not enough: Emotional distress and depression reduce the positive effects of health literacy on diabetes self-management. Patient Educ. Couns. 2018, 101, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Rajah, R.; Ahmad Hassali, M.A.; Jou, L.C.; Murugiah, M.K. The perspective of healthcare providers and patients on health literacy: A systematic review of the quantitative and qualitative studies. Perspect. Public Health 2018, 138, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Schulz, P.J.; Nakamoto, K. Health literacy and patient empowerment in health communication: The importance of separating conjoined twins. Patient Educ. Couns. 2013, 90, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Street, R.L., Jr.; Makoul, G.; Arora, N.K.; Epstein, R.M. How does communication heal? Pathways linking clinician–patient communication to health outcomes. Patient Educ. Couns. 2009, 74, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Arnold, C.L.; Coran, J.J.; Hagen, M.G. Revisiting patient communication training: An updated needs assessment and the AGENDA model. Patient Educ. Couns. 2012, 88, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Ewing, G.; Ngwenya, N.; Benson, J.; Gilligan, D.; Bailey, S.; Seymour, J.; Farquhar, M. Sharing news of a lung cancer diagnosis with adult family members and friends: A qualitative study to inform a supportive intervention. Patient Educ. Couns. 2016, 99, 378–385. [Google Scholar] [CrossRef] [PubMed]
- Ferrell, B.; Wittenberg, E. A review of family caregiving intervention trials in oncology. CA A Cancer J. Clin. 2017, 67, 318–325. [Google Scholar] [CrossRef] [PubMed]
- Northouse, L.L.; Katapodi, M.C.; Song, L.; Zhang, L.; Mood, D.W. Interventions with family caregivers of cancer patients: Meta-analysis of randomized trials. CA A Cancer J. Clin. 2010, 60, 317–339. [Google Scholar] [CrossRef] [PubMed]
- Chi, N.C.; Demiris, G. The roles of telehealth tools in supporting family caregivers: Current evidence, opportunities, and limitations. J. Gerontol. Nurs. 2017, 43, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Dilger, D. The Emotional Health Literacy Block. Available online: https://www.kevinmd.com/blog/2013/11/emotional-health-literacy-block.html (accessed on 14 May 2018).
- Schumacher, K.L.; Plano Clark, V.L.; West, C.M.; Dodd, M.J.; Rabow, M.W.; Miaskowski, C. Pain medication management processes used by oncology outpatients and family caregivers part II: Home and lifestyle contexts. J. Pain Symptom Manag. 2014, 48, 784–796. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, B.S.; Miaskowski, C.; Given, B.; Schumacher, K. The cancer family caregiving experience: An updated and expanded conceptual model. Eur. J. Oncol. Nurs. 2012, 16, 387–398. [Google Scholar] [CrossRef] [PubMed]
- Roter, D.L.; Narayanan, S.; Smith, K.; Bullman, R.; Rausch, P.; Wolff, J.L.; Alexander, G.C. Family caregivers’ facilitation of daily adult prescription medication use. Patient Educ. Couns. 2018, 101, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Rodakowski, J.; Rocco, P.B.; Ortiz, M.; Folb, B.; Schulz, R.; Morton, S.C.; Leathers, S.C.; Hu, L.; James, A.E., 3rd. Caregiver integration during discharge planning for older adults to reduce resource use: A metaanalysis. J. Am. Geriat. Soc. 2017, 65, 1748–1755. [Google Scholar] [CrossRef] [PubMed]
- Robotin, M.C.; Porwal, M.; Hopwood, M.; Nguyen, D.; Sze, M.; Treloar, C.; George, J. Listening to the consumer voice: Developing multilingual cancer information resources for people affected by liver cancer. Health Expect. 2017, 20, 171–182. [Google Scholar] [CrossRef] [PubMed]
- Huntington, B.; Kuhn, N. Communication gaffes: A root cause of malpractice claims. Proc. (Bayl. Univ. Med. Cent.) 2003, 16, 157–161. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, T.A.; Atkinson, T.M.; Latella, L.E.; Rogers, M.; Morrissey, D.; DeRosa, A.P.; Parker, P.A. Promoting patient participation in healthcare interactions through communication skills training: A systematic review. Patient Educ. Couns. 2017, 100, 1247–1257. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.Y.; Vang, S. Barriers to cancer screening in Hmong Americans: The influence of health care accessibility, culture, and cancer literacy. J. Commun. Health 2010, 35, 302–314. [Google Scholar] [CrossRef] [PubMed]
- Fang, M.C.; Machtinger, E.L.; Wang, F.; Schillinger, D. Health literacy and anticoagulation-related outcomes among patients taking warfarin. JGIM 2006, 21, 841–846. [Google Scholar] [CrossRef] [PubMed]
- Molina, Y.; Hohl, S.D.; Ko, L.K.; Rodriguez, E.A.; Thompson, B.; Beresford, S.A. Understanding the patient-provider communication needs and experiences of Latina and non-Latina White women following an abnormal mammogram. J. Cancer Educ. 2014, 29, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Rikard, R.V.; Thompson, M.S.; McKinney, J.; Beauchamp, A. Examining health literacy disparities in the United States: A third look at the National Assessment of Adult Literacy (NAAL). BMC Public Health 2016, 16, 975. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention. Use of Social Networks to Identify Persons with Undiagnosed HIV Infection—Seven U.S. Cities, October 2003–September 2004. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5424a3.htm (accessed on 2 April 2018).
- Finn, S.; O’Fallon, L. The emergence of environmental health ltieracy—From its roots to its future potential. Environ. Health Perspect. 2017, 125, 495–501. [Google Scholar] [PubMed]
- Federal Drug Administration Federal Plain Language Guidelines. Available online: https://www.fda.gov/downloads/AboutFDA/PlainLanguage/UCM346279.pdf (accessed on 26 March 2018).
- Nouri, S.S.; Rudd, R.E. Health literacy in the “oral exchange”: An important element of patient-provider communication. Patient Educ. Couns. 2015, 98, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Kaphingst, K.A.; Kreuter, M.W.; Casey, C.; Leme, L.; Thompson, T.; Cheng, M.-R.; Jacobsen, H.; Sterling, R.; Oguntimein, J.; Filler, C. Health literacy INDEX: Development, reliability, and validity of a new tool for evaluating the health literacy demands of health information materials. J. Health Commun. 2012, 17, 203–221. [Google Scholar] [CrossRef] [PubMed]
- Mead, E.L.; Doorenbos, A.Z.; Javid, S.H.; Haozous, E.A.; Alvord, L.A.; Flum, D.R.; Morris, A.M. Shared decision-making for cancer care among racial and ethnic minorities: A systematic review. Am. J. Public Health 2013, 103, e15–e29. [Google Scholar] [CrossRef] [PubMed]
- Costas-Muniz, R.; Sen, R.; Leng, J.; Aragones, A.; Ramirez, J.; Gany, F. Cancer stage knowledge and desire for information: Mismatch in Latino cancer patients? J. Cancer Educ. 2013, 28, 458–465. [Google Scholar] [CrossRef] [PubMed]
- Campesino, M.; Saenz, D.S.; Choi, M.; Krouse, R.S. Perceived discrimination and ethnic identity among breast cancer survivors. Oncol. Nurs. Forum 2012, 39, E91–E100. [Google Scholar] [CrossRef] [PubMed]
- Youdelman, M.K. The medical tongue: U.S. laws and policies on language access. Health Aff. 2008, 27, 424–433. [Google Scholar] [CrossRef] [PubMed]
- Stabler, R. What we’ve got here is failure to communicate: The Plain Writing Act of 2010. J. Legis. 2013, 40, 280–323. [Google Scholar]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goldsmith, J.V.; Terui, S. Family Oncology Caregivers and Relational Health Literacy. Challenges 2018, 9, 35. https://doi.org/10.3390/challe9020035
Goldsmith JV, Terui S. Family Oncology Caregivers and Relational Health Literacy. Challenges. 2018; 9(2):35. https://doi.org/10.3390/challe9020035
Chicago/Turabian StyleGoldsmith, Joy V., and Sachiko Terui. 2018. "Family Oncology Caregivers and Relational Health Literacy" Challenges 9, no. 2: 35. https://doi.org/10.3390/challe9020035
APA StyleGoldsmith, J. V., & Terui, S. (2018). Family Oncology Caregivers and Relational Health Literacy. Challenges, 9(2), 35. https://doi.org/10.3390/challe9020035



