Nutritional Vulnerability of Displaced Persons: A Study of Food Security and Access in Kumba Municipality, Cameroon
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Variables
2.2. Data Collection Tool and Procedures
2.3. Data Management and Analysis
2.4. Ethical Considerations
3. Results
3.1. Sociodemographic Characteristics of Adult Participants
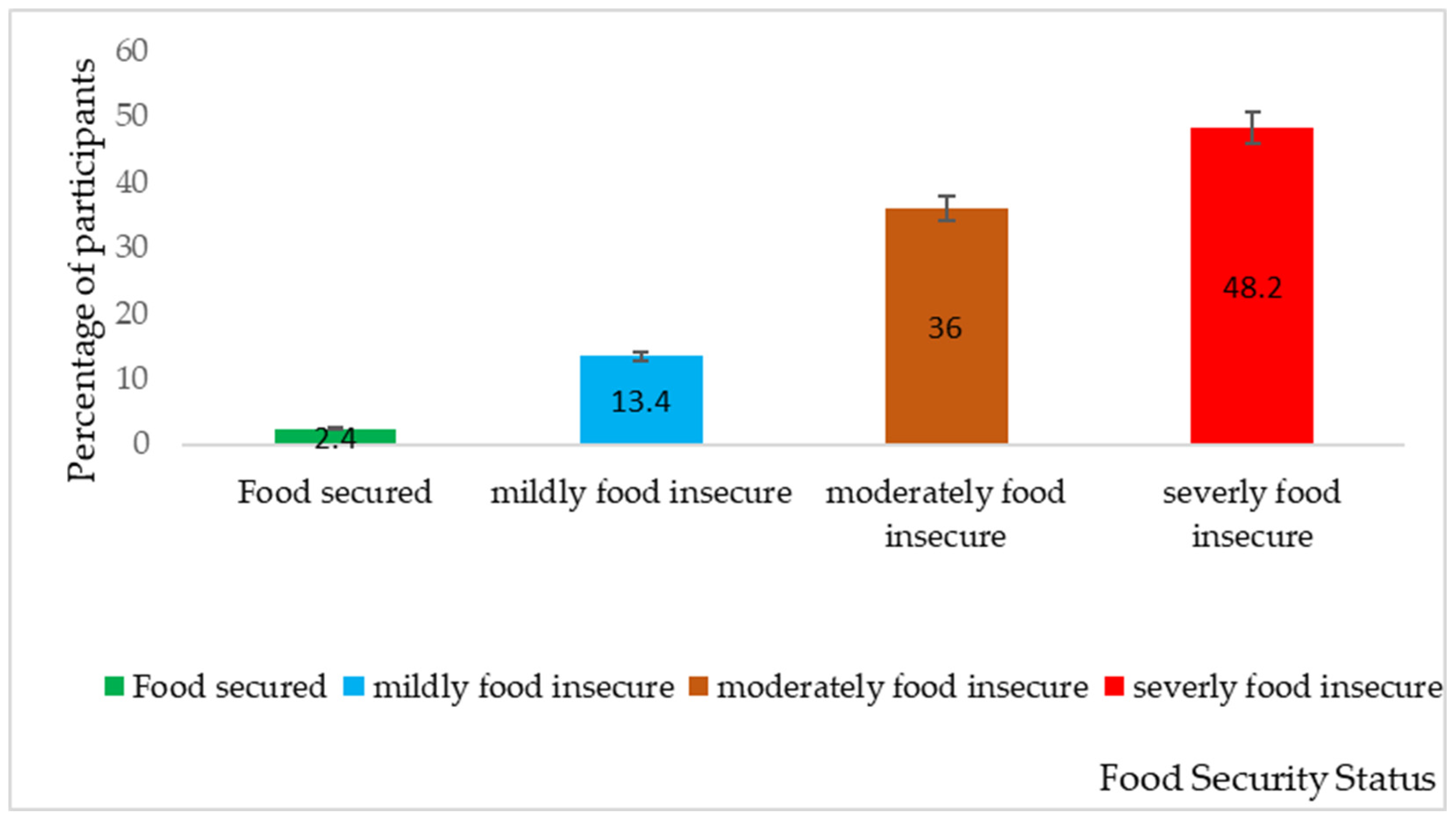
3.2. Household Food Insecurity
3.3. Coping Strategies Among IDPs
3.4. Household Dietary Diversity
3.5. Nutritional Status of IDP Adults
3.6. Nutritional Status of IDP Children
3.7. Nutritional Status and Food Insecurity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Barrett, C.B. Overcoming Global Food Security Challenges through Science and Solidarity. Am. J. Agric. Econ. 2021, 103, 422–447. [Google Scholar] [CrossRef]
- Mohamed, E.S.E. Environmental Change, Conflicts and Internal Displacement as Destabilizing Factors to Food Security in Sudan: Econometric Analysis. J. Intern. Displac. 2020, 10, 2–24. [Google Scholar]
- Prosekov, A.Y.; Ivanova, S.A. Food security: The challenge of the present. Geoforum 2018, 91, 73–77. [Google Scholar] [CrossRef]
- Wudil, A.H.; Usman, M.; Rosak-Szyrocka, J.; Pilař, L.; Boye, M. Reversing Years for Global Food Security: A Review of the Food Security Situation in Sub-Saharan Africa (SSA). Int. J. Environ. Res. Public Health 2022, 19, 14836. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.R.; Kleinert, W.L.; Sheppard, A.V.; Cantrell, K.A.; Freeman-Coppadge, D.J.; Tsoy, E.; Roberts, T.; Pearrow, M. The Relationship Between Food Security, Housing Stability, and School Performance Among College Students in an Urban University. J. Coll. Stud. Retent. Res. Theory Pract. 2015, 19, 284–299. [Google Scholar] [CrossRef]
- Gonzalez, C. World poverty and food insecurity. Penn State J. Law Int. Aff. 2014, 3, 56. [Google Scholar]
- Carril-Caccia, F.; Paniagua, J.; Suarez-Varela, M. Forced Migration and Food Crises; Banco de Espana: Madrid, Spain, 2022. [Google Scholar]
- Owoaje, E.; Uchendu, O.; Ajayi, T.; Cadmus, E. A review of the health problems of the internally displaced persons in Africa. Niger. Postgrad. Med. J. 2016, 23, 161. [Google Scholar] [CrossRef]
- Osman, A.A.; Abebe, G.K. Rural Displacement and Its Implications on Livelihoods and Food Insecurity: The Case of Inter-Riverine Communities in Somalia. Agriculture 2023, 13, 1444. [Google Scholar] [CrossRef]
- George, J.; Adelaja, A. Forced Displacement and Agriculture: Implications for Host Communities. Sustainability 2021, 13, 5728. [Google Scholar] [CrossRef]
- Tóth, G.; Zachár, J. Towards food justice—The global-economic material balance analysis of hunger, food security and waste. Agronomy 2021, 11, 1324. [Google Scholar] [CrossRef]
- Tambe, B.A.; Mabapa, N.S.; Mbhatsani, H.V.; Mandiwana, T.C.; Mushaphi, L.F.; Mohlala, M.; Mbhenyane, X.G. Household socio-economic determinants of food security in Limpopo Province of South Africa: A cross sectional survey. Agric. Food Secur. 2023, 12, 19. [Google Scholar] [CrossRef]
- Bhardwaj, R.L.; Parashar, A.; Parewa, H.P.; Vyas, L. An Alarming Decline in the Nutritional Quality of Foods: The Biggest Challenge for Future Generations’ Health. Foods 2024, 13, 877. [Google Scholar] [CrossRef] [PubMed]
- Knez, M.; Ranić, M.; Gurinović, M. Underutilized plants increase biodiversity, improve food and nutrition security, reduce malnutrition, and enhance human health and well-being. Let’s put them back on the plate! Nutr. Rev. 2024, 82, 1111–1124. [Google Scholar] [CrossRef]
- Tefera, M.L.; Carletti, A.; Altea, L.; Rizzu, M.; Migheli, Q.; Seddaiu, G. Land degradation and the upper hand of sustainable agricultural intensification in sub-Saharan Africa-A systematic review. J. Agric. Rural. Dev. Trop. Subtrop. 2024, 125, 63–83. [Google Scholar] [CrossRef]
- Johns, T.; Powell, B.; Maundu, P.; Eyzaguirre, P.B. Agricultural biodiversity as a link between traditional food systems and contemporary development, social integrity and ecological health. J. Sci. Food Agric. 2013, 93, 3433–3442. [Google Scholar] [CrossRef] [PubMed]
- Tambe, A.B.; Akeh, M.L.; Tendongfor, N.; Dhlamini, T.; Chipili, G.; Mbhenyane, X. The predictors of food security and dietary diversity among internally displaced persons’ children (6–59 months) in Bamenda health district, Cameroon. Confl. Health 2023, 17, 11. [Google Scholar] [CrossRef]
- Maxwell, D.; Caldwell, R.; Bell, B. The Coping Strategies Index Field Methods Manual, 2nd ed.; Cooperative for Assistance and Relief Everywhere, Inc.: Geneva, Switzerland, 2008. [Google Scholar]
- FANTA; FAO. Minimum Dietary Diversity for Women: A Guide for Measurement; FAO: Rome, Italy, 2016. [Google Scholar]
- Coates, J.; Swindale, A.; Bilinsky, P. Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide: Version 3; American Psychological Association: Washington, DC, USA, 2007. [Google Scholar]
- World Health Organization. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: Joint Statement by the World Health Organization and the United Nations Children’s Fund; World Health Organization Press: Geneva, Switzerland, 2009. [Google Scholar]
- World Health Organization. WHO Child Growth Standards: Length/height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Vu, K.; Vuong, N.D.T.; Vu-Thanh, T.A.; Nguyen, A.N. Income shock and food insecurity prediction Vietnam under the pandemic. World Dev. 2022, 153, 105838. [Google Scholar] [CrossRef]
- Swann, C.A. Household history, SNAP participation, and food insecurity. Food Policy 2017, 73, 1–9. [Google Scholar] [CrossRef]
- Olayemi, A.O. Effects of Family Size on Household Food Security in Osun State, Nigeria. Asian J. Agric. Rural. Dev. 2012, 2, 136–141. [Google Scholar]
- Singh, K.P.; Bhoopathy, S.V.; Worth, H.; Seale, H.; Richmond, R.L. Nutrition among men and household food security in an internally displaced persons camp in Kenya. Public Health Nutr. 2015, 19, 723–731. [Google Scholar] [CrossRef][Green Version]
- Huang, X.; King, C. Food insecurity transitions and housing hardships: Are immigrant families more vulnerable? J. Aff. 2018, 40, 1146–1160. [Google Scholar] [CrossRef]
- Gregory, C.A.; Coleman-Jensen, A. Food Insecurity, Chronic Disease, and Health Among Working-Age Adults; United States Department of Agriculture: Washington, DC, USA, 2017. [Google Scholar]
- Belayneh, M.; Loha, E.; Lindtjørn, B. Seasonal Variation of Household Food Insecurity and Household Dietary Diversity on Wasting and Stunting among Young Children in A Drought Prone Area in South Ethiopia: A Cohort Study. Ecol. Food Nutr. 2021, 60, 44–69. [Google Scholar] [CrossRef] [PubMed]
- Akerele, D.; Momoh, S.; Aromolaran, A.B.; Oguntona, C.R.B.; Shittu, A.M. Food insecurity and coping strategies in South-West Nigeria. Food Secur. 2013, 5, 407–414. [Google Scholar] [CrossRef]
- Debessa, A.A.; Tolossa, D.; Denu, B.; Debessa, A.A.; Tolossa, D.; Denu, B. Analysis of the Nexus between Coping Strategies and Resilience to Food Insecurity Shocks: The Case of Rural Households in Boricha Woreda, Sidama National Regional State, Ethiopia; IntechOpen: London, UK, 2022. [Google Scholar] [CrossRef]
- Sambo, T.A.; Oguttu, J.W.; Mbombo-Dweba, T.P. Analysis of the dietary diversity status of agricultural households in the Nkomazi Local Municipality, South Africa. Agric. Food Secur. 2022, 11, 46. [Google Scholar] [CrossRef]
- Gallegos, D.; Eivers, A.; Sondergeld, P.; Pattinson, C. Food insecurity and child development: A state-of-the-art review. Int. J. Environ. Res. Public Health. 2021, 18, 8990. [Google Scholar] [CrossRef]
- Reeder, N.; Tolar-Peterson, T.; Bailey, R.H.; Cheng, W.H.; Evans, M.W. Food Insecurity and Depression among US Adults: NHANES 2005–2016. Nutrients 2022, 14, 3081. [Google Scholar] [CrossRef]
- Farb, M.G.; Gokce, N. Visceral adiposopathy: A vascular perspective. Horm. Mol. Biol. Clin. Investig. 2015, 21, 125–136. [Google Scholar] [CrossRef]
- Nam, H.K.; Park, J.; Cho, S.I. Association between depression, anemia and physical activity using isotemporal substitution analysis. BMC Public Health 2023, 23, 2236. [Google Scholar] [CrossRef]
- Tian, J.; Fan, Y.; Wei, X.; Li, J.; Yang, Z.; Na, X.; Zhang, Y. Hospitalization of patients with nutritional anemia in the United States in 2020. Front. Public Health 2024, 12, 1333069. [Google Scholar] [CrossRef]
- Schramm, S.; Ocaka Kaducu, F.; Smedemark, S.A.; Ovuga, E.; Sodemann, M. Gender and age disparities in adult undernutrition in northern Uganda: High-risk groups not targeted by food aid programmes. Trop. Med. Int. Health 2016, 21, 807–817. [Google Scholar] [CrossRef]
- Carvajal-Aldaz, D.; Cucalon, G.; Ordonez, C. Food insecurity as a risk factor for obesity: A review. Front. Nutr. 2022, 9, 1012734. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, K.Y.; Dadi, A.F.; Ogbo, F.A.; Page, A.; Agho, K.E.; Akalu, T.Y.; Baraki, A.G.; Tesema, G.A.; Teshale, A.B.; Alamneh, T.S.; et al. Population-Modifiable Risk Factors Associated with Childhood Stunting in Sub-Saharan Africa. JAMA Netw. Open 2023, 6, e2338321. [Google Scholar] [CrossRef] [PubMed]
- Akombi, B.J.; Agho, K.E.; Hall, J.J.; Wali, N.; Renzaho, A.M.N.; Merom, D. Stunting, Wasting and Underweight in Sub-Saharan Africa: A Systematic Review. Int. J. Environ. Res. Public Health 2017, 14, 863. [Google Scholar] [CrossRef] [PubMed]
- Olwedo, M.; Mworozi, E.; Bachou, H. Factors associated with malnutrition among children in internally displaced person\’s camps, northern Uganda. Afr. Health Sci. 2008, 8, 244–252. [Google Scholar]
| Variable Category | Frequency | Percentage |
|---|---|---|
| Adult’s Sex | ||
| Female | 173 | 70.0 |
| Male | 74 | 30.0 |
| Adult’s Age (Years) | ||
| 18–34 | 123 | 49.8 |
| 35–54 | 107 | 43.3 |
| 55–70 | 17 | 6.9 |
| Child’s Sex | ||
| Female | 102 | 41.3 |
| Male | 145 | 58.7 |
| Child’s Age (Months) | ||
| 3–11 | 40 | 16.2 |
| 12–24 | 66 | 26.7 |
| 25–59 | 141 | 57.1 |
| Nationality | ||
| Cameroonian | 237 | 96.0 |
| Foreign nationals | 10 | 4.0 |
| Current Occupation | ||
| Businessperson | 21 | 8.5 |
| Farmer | 94 | 38.1 |
| Public/Civil Servant | 2 | 0.8 |
| Work in the Private Sector | 14 | 5.7 |
| Unemployed | 78 | 31.7 |
| Other Occupation | 38 | 15.2 |
| Occupation before displacement | ||
| Businessperson | 17 | 6.9 |
| Farmer | 130 | 52.6 |
| Public/Civil servant | 7 | 2.8 |
| Work in the Private Sector | 21 | 8.5 |
| Unemployed | 64 | 26 |
| Other Occupation | 8 | 3.2 |
| Monthly income | ||
| USD 30–60 | 94 | 38.1 |
| USD 61–100 | 116 | 47 |
| USD 101–200 | 34 | 13.8 |
| USD 201–300 | 3 | 1.2 |
| Money spent on food monthly | ||
| USD 20–60 | 213 | 86.2 |
| USD 60–100 | 25 | 10.1 |
| USD 101–620 | 9 | 3.6 |
| Level of education | ||
| FSLC | 81 | 32.8 |
| O-Level | 39 | 15.8 |
| A-Level | 12 | 4.9 |
| Bachelors | 16 | 6.5 |
| No Formal Education | 48 | 19.4 |
| Others | 51 | 20.6 |
| Marital status | ||
| Single | 78 | 31.6 |
| Married | 117 | 47.4 |
| Divorce | 1 | 0.4 |
| Widowed | 26 | 10.5 |
| Cohabitation | 25 | 10.1 |
| Number of household members | ||
| 2–4 persons | 76 | 30.8 |
| 5–7 persons | 144 | 58.3 |
| More than 7 persons | 27 | 10.9 |
| Duration of displacement | ||
| Less than 1 year | 58 | 23.5 |
| 1–4 years | 130 | 52.6 |
| 5–6 years | 59 | 23.9 |
| Consider food to be more accessible now | ||
| Yes | 17 | 6.9 |
| No | 230 | 93.1 |
| Coping Strategy | Frequency | Percentage |
|---|---|---|
| Dietary change | ||
| Rely on less preferred and less expensive foods | 241 | 97.5 |
| Consume less variety of food | 243 | 98.4 |
| Increase short-term household food availability | ||
| Borrow food from a friend or relative | 37 | 15.0 |
| Purchase food on credit | 140 | 56.7 |
| Depend on aid from outside the household | 119 | 48.2 |
| Gather wild food, hunt, or harvest immature crops | 48 | 19.4 |
| Consume seed stock held for next season | 77 | 31.2 |
| Decrease number of people | ||
| Send household members to beg | 22 | 8.9 |
| Send household members to eat elsewhere | 117 | 47.4 |
| Rationing strategy | ||
| Limit portion size at mealtimes | 219 | 88.7 |
| Restrict consumption by adults for small children to eat | 201 | 81.4 |
| Feed working members of HH at the expense of non-working members | 12 | 4.8 |
| Ration the money you have and buy prepared food | 182 | 73.7 |
| Spend an entire day without eating | 31 | 12.5 |
| Nutritional Status | Frequency | Percentage |
|---|---|---|
| Adult BMI | ||
| Underweight | 54 | 21.9 |
| Normal | 123 | 49.8 |
| Overweight | 59 | 23.9 |
| Obese | 11 | 4.5 |
| Total | 247 | 100 |
| Waist Circumference | ||
| Normal | 155 | 62.8 |
| Overweight | 53 | 21.5 |
| Obese | 39 | 15.8 |
| Total | 247 | 100 |
| Waist/Hip ratio | ||
| Low risk | 127 | 51.4 |
| Moderate | 56 | 22.7 |
| High risk | 64 | 25.9 |
| Total | 247 | 100 |
| Anemia | ||
| No | 185 | 74.9 |
| Yes | 62 | 25.1 |
| Total | 247 | 100 |
| Nutritional Status | Frequency | Percentage |
|---|---|---|
| Child’s MUAC | ||
| Severe acute malnutrition | 8 | 3.2 |
| Moderate acute malnutrition | 93 | 37.7 |
| Normal | 146 | 59.1 |
| Height-for-Age (Stunting) | ||
| Normal | 122 | 49.4 |
| Moderately stunted | 63 | 25.5 |
| Severely stunted | 62 | 25.1 |
| Weight-for-Age (Underweight) | ||
| Severely undernourished for age | 30 | 12.2 |
| Underweight for age | 63 | 25.5 |
| Normal | 151 | 61.1 |
| Possibly overweight | 3 | 1.2 |
| Weight-for-height (Wasting) | ||
| Severe acute malnutrition | 7 | 2.8 |
| Moderate acute malnutrition | 32 | 12.9 |
| Normal | 188 | 76.1 |
| Overweight | 13 | 5.3 |
| Obese | 7 | 2.8 |
| Socio-Demographic Characteristics | Total Number | Food Security | |||
|---|---|---|---|---|---|
| Food Secure | Food Insecure | Chi-Square | p-Value | ||
| n (%) | n (%) | ||||
| Sex | |||||
| Female | 173 | 4 (1.6) | 169 (68.4) | 0.033 | 0.855 |
| Male | 74 | 2 (0.8) | 72 (29.2) | ||
| Age (Years) | |||||
| 18–34 | 123 | 2 (0.8) | 121 (49.0) | 2.750 | 0.600 |
| 35–54 | 107 | 4 (1.6) | 103 (41.7) | ||
| 55–70 | 17 | 0 (0) | 17 (6.9) | ||
| Child’s Sex | |||||
| Female | 102 | 3 (1.2) | 99 (40.1) | 0.192 | 0.661 |
| Male | 145 | 3 (1.2) | 142 (57.5) | ||
| Child’s Age (Months) | |||||
| 3–11 | 40 | 1 (0.4) | 39 (15.8) | 0.332 | 0.847 |
| 12–24 | 66 | 1 (0.4) | 65 (26.3) | ||
| 25–29 | 141 | 4 (1.6) | 137 (55.5) | ||
| Nationality | |||||
| Cameroonian | 237 | 6 (2.4) | 231 (93.5) | 0.259 | 0.610 |
| Foreigner | 10 | 0 (0.0) | 10 (4.0) | ||
| Current Occupation | |||||
| Businessperson | 21 | 2 (0.8) | 19 (7.7) | 17.187 | <0.001 |
| Farmer | 94 | 0 (0.0) | 94 (38.1) | ||
| Public/Civil Servant | 2 | 0 (0.0) | 2 (0.8) | ||
| Work in the Private Sector | 14 | 2 (0.8) | 12 (4.9) | ||
| Unemployed | 64 | 0 (0.0) | 78 (31.7) | ||
| Other Occupation | 52 | 2 (0.8) | 36 (14.4) | ||
| Occupation before displacement | |||||
| Businessperson | 17 | 1 (0.4) | 16 (6.5) | 17.190 | 0.004 |
| Farmer | 130 | 0 (0.0) | 130 (52.6) | ||
| Public/Civil Servant | 7 | 0 (0.0) | 7 (2.8) | ||
| Work in the Private Sector | 21 | 4 (1.6) | 17 (6.9) | ||
| Unemployed | 64 | 1 (0.4) | 63 (25.5) | ||
| Other Occupation | 8 | 0 (0.0) | 8 (3.2) | ||
| Monthly Income (FCFA) | |||||
| 15,000–30,000 | 94 | 0 (0.0) | 94 (38.1) | 69.960 | <0.001 |
| 30,001–50,000 | 116 | 0 (0.0) | 116 (46.9) | ||
| 50,001–100,000 | 34 | 4 (1.6) | 30 (12.1) | ||
| 100.000+ | 3 | 2 (0.8) | 1 (0.4) | ||
| Money Spent on Food Monthly (FCFA) | |||||
| 10,000–30,000 | 213 | 0 (0.0) | 213 (86.2) | 112.737 | <0.001 |
| 30,001–50,000 | 24 | 1 (0.2) | 24 (9.7) | ||
| 50,001+ | 9 | 5 (2.0) | 4 (1.6) | ||
| Level of Education | |||||
| No Formal Education | 48 | 0 (0.0) | 48 (19.4) | 37.390 | <0.001 |
| FSLC | 80 | 1 (0.4) | 80 (3.2) | ||
| O-Level | 39 | 0 (0.0) | 39 (15.7) | ||
| A-Level | 12 | 0 (0.0) | 12 (4.9) | ||
| Bachelors | 16 | 4 (2.4) | 12 (4.9) | ||
| Others | 51 | 1 (0.4) | 50 (20.2) | ||
| Marital Status | |||||
| Single | 78 | 0 (0.0) | 78 (31.6) | 5.469 | 0.240 |
| Married | 117 | 3 (1.2) | 114 (46.1) | ||
| Divorce | 1 | 0 (0.0) | 1 (0.4) | ||
| Widowed | 26 | 1 (0.4) | 25 (10.1) | ||
| Cohabitation | 25 | 2 (0.8) | 23 (9.3) | ||
| Number of Household Members | |||||
| 2–4 persons | 76 | 2 (0.8) | 74 (29.9) | 0.271 | 0.870 |
| 5–7 persons | 144 | 3 (1.2) | 141 (57.1) | ||
| More than 7 persons | 27 | 1 (0.4) | 26 (10.5) | ||
| Duration of Displacement | |||||
| Less than 1 year | 58 | 1 (0.4) | 57 (23.1) | 2.692 | 0.260 |
| 1–4 years | 130 | 5 (2.0) | 125 (50.6) | ||
| 5–6 years | 59 | 0 (0.0) | 59 (23.9) | ||
| Consider food to be more available now | |||||
| Yes | 17 | 5 (2.0) | 12 (4.9) | 56.080 | <0.001 |
| No | 230 | 1 (0.4) | 229 (92.7) | ||
| Total | 247 | 6 (2.4) | 241 (97.6) | ||
| Nutritional Status | Total Number | Food Security | Chi-Square | p-Value | |
|---|---|---|---|---|---|
| Food Secure n (%) | Food Insecure n (%) | ||||
| BMI of caregivers | |||||
| Underweight | 54 | 0 (0.0) | 54 (21.9) | 20.635 | <0.001 |
| Normal | 123 | 0 (0.0) | 123 (49.8) | ||
| Overweight | 59 | 4 (1.6) | 55 (22.3) | ||
| Obese | 11 | 2 (0.8) | 9 (3.6) | ||
| Waist Circumference of caregivers | |||||
| Normal | 155 | 1 (0.4) | 154 (62.3) | 7.044 | 0.030 |
| Overweight | 38 | 2 (0.8) | 36 (20.6) | ||
| Obese | 54 | 3 (1.2) | 51 (14.6) | ||
| Waist/Hip ratio caregivers | |||||
| Low risk | 127 | 2 (0.8) | 125 (50.6) | 5.727 | 0.060 |
| Moderate | 56 | 0 (0.0) | 56 (22.7) | ||
| High risk | 64 | 4 (1.6) | 60 (24.3) | ||
| Anemia | |||||
| No | 185 | 6 (2.4) | 179 (72.5) | 2.061 | 0.150 |
| Yes | 62 | 0 (0.0) | 62 (25.1) | ||
| Child’s MUAC | |||||
| Severe acute malnutrition | 8 | 0 (0.0) | 8 (3.2) | 4.254 | 0.120 |
| Moderate acute malnutrition | 93 | 0 (0.0) | 93 (37.7) | ||
| Normal | 146 | 6 (2.4) | 140 (56.7) | ||
| Child’s HAZ | |||||
| Severely stunted | 62 | 0 (0.0) | 119 (25.1) | 3.088 | 0.214 |
| Moderately stunted | 63 | 3 (1.2) | 63 (24.3) | ||
| Normal | 122 | 3 (1.2) | 59 (28.5) | ||
| Child’s WHZ | |||||
| Severely Malnourished | 7 | 0 (0.0) | 7 (2.8) | 5.489 | 0.241 |
| Normal | 188 | 5 (2.0) | 215 (87.0) | ||
| Overweight | 13 | 0 (0.0) | 13 (5.3) | ||
| Obese | 7 | 1 (0.4) | 6 (2.4) | ||
| Child’s WAZ | |||||
| Severely undernourished | 30 | 2 (0.8) | 28 (11.3) | 15.327 | 0.002 |
| Underweight for age | 63 | 1 (0.4) | 62 (25.1) | ||
| Normal | 151 | 2 (0.8) | 149 (60.3) | ||
| Possible overweight | 3 | 1 (0.4) | 2 (0.8) | ||
| DDS food group | |||||
| Low dietary diversity (≤3) | 52 | 0 (0.0) | 52 (21.1) | 15.549 | <0.001 |
| Moderate dietary diversity (4–5) | 125 | 0 (0.0) | 125 (50.6) | ||
| High dietary diversity (≥6) | 68 | 6 (0.0) | 64 (25.9) | ||
| Variable | Std. Error | Standardized Coefficients | R2 | t | p-Value |
|---|---|---|---|---|---|
| Age of the caregivers (year) | 0.023 | 0.016 | 0.491 | 0.343 | 0.732 |
| Child age (months) | 0.016 | 0.011 | 0.237 | 0.813 | |
| Monthly salary of the caregivers | 0.000 | −0.303 | −3.906 | <0.001 | |
| Monthly average money spends on food | 0.000 | −0.443 | −5.640 | <0.001 | |
| Family size | 0.148 | −0.186 | 3.885 | <0.001 | |
| Duration of displacement (Years) | 0.013 | −0.051 | −1.083 | 0.280 | |
| CSI group | 0.041 | 0.382 | 0.348 | 6.993 | <0.001 |
| DDS Score 17 | 0.139 | −0.342 | −6.265 | <0.001 | |
| BMI | 0.170 | −0.293 | 0.146 | −2.385 | 0.400 |
| Waist Circumference | 0.844 | −1.281 | −0.843 | 0.417 | |
| HIP Circumference | 1.854 | 0.851 | 0.813 | 0.451 | |
| Waist/hip ratio | 80.480 | 0.548 | 0.754 | 0.673 | |
| MUAC | 0.151 | 0.040 | 0.422 | 0.540 | |
| Head Circumference | 0.080 | −0.040 | −0.614 | 0.868 | |
| MUAC child | 0.335 | −0.014 | −0.166 | 0.167 | |
| Childs BMI | 0.225 | −0.151 | −1.386 | 0.378 | |
| HAZ | 2.080 | 0.645 | 0.883 | 0.465 | |
| WHZ | 0.938 | 0.186 | 0.732 | 0.392 | |
| WAZ | 3.191 | −0.613 | −0.858 | 0.395 | |
| BAZ | 1.996 | 0.420 | 0.852 | 0.400 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Metuge, K.N.; Tambe, B.A.; Djikeng, F.T.; Achidi, A.U.; Chipili, G.; Mbhenyane, X.G. Nutritional Vulnerability of Displaced Persons: A Study of Food Security and Access in Kumba Municipality, Cameroon. Challenges 2025, 16, 7. https://doi.org/10.3390/challe16010007
Metuge KN, Tambe BA, Djikeng FT, Achidi AU, Chipili G, Mbhenyane XG. Nutritional Vulnerability of Displaced Persons: A Study of Food Security and Access in Kumba Municipality, Cameroon. Challenges. 2025; 16(1):7. https://doi.org/10.3390/challe16010007
Chicago/Turabian StyleMetuge, Kevin N., Betrand A. Tambe, Fabrice Tonfack Djikeng, Aduni Ufuan Achidi, Given Chipili, and Xikombiso G. Mbhenyane. 2025. "Nutritional Vulnerability of Displaced Persons: A Study of Food Security and Access in Kumba Municipality, Cameroon" Challenges 16, no. 1: 7. https://doi.org/10.3390/challe16010007
APA StyleMetuge, K. N., Tambe, B. A., Djikeng, F. T., Achidi, A. U., Chipili, G., & Mbhenyane, X. G. (2025). Nutritional Vulnerability of Displaced Persons: A Study of Food Security and Access in Kumba Municipality, Cameroon. Challenges, 16(1), 7. https://doi.org/10.3390/challe16010007





