Abstract
It is well-known that atmospheric pollution, first and foremost the particulate matter (PM), causes serious diseases in humans. China’s metropolises and Italy’s Po Valley have in fact achieved a concerning degree of notoriety thanks to runaway air pollution problems. The spread of viral respiratory diseases is facilitated in polluted environments, an example of which is the respiratory syncytial virus bronchiolitis. In this opinion paper, we consider the possible relationship between air pollution, primarily airborne PM10–2.5, and the spread of the novel coronavirus in Northern Italy. If it is true that the novel coronavirus remains active from some hours to several days on various surfaces, it is logical to postulate that the same can occur when it is adsorbed or absorbed by the atmospheric particulate matter, which may also help carry the virus into the human respiratory system. As the Earth presents us with a very high bill to pay, governments and other authorities need to take prompt action to counter excessive pollution levels, both in Italy and in other countries.
1. Air Quality in a Large Area of Northern Italy (the Po Valley) has been Severely Compromised for Decades
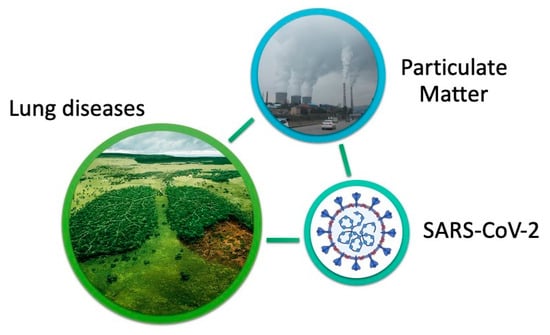
For many years, studies have been conducted into interactions between environmental pollution and the incidence of acute and chronic diseases. By way of example, in 1997, Cesare Cislaghi and Pier Luigi Nimis published an authoritative paper [1] on the striking correlation between lung cancer mortality in the “young” male population (<55 years) and the level of atmospheric pollution (Figure 1). Lichens are exceptional for biomonitoring air quality, and the paper met with considerable interest from the scientific world. This multi-year experimental investigation was carried out across the entire Italian region of Veneto (approximately 4 million inhabitants at the time of the experiment). Whilst this authoritative study managed to raise the alarm, administrators have since failed to take any real steps to limit the impact of air pollution (and environmental contamination in general).
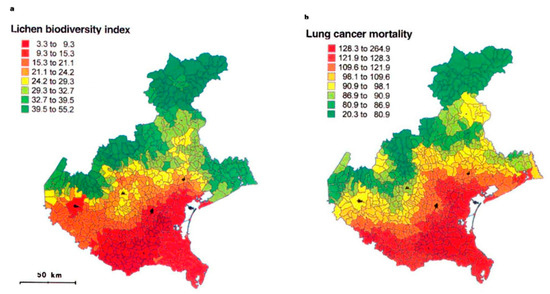
Figure 1.
(a) Lichen biodiversity index, calculated as the sum of frequencies of all epiphytic species in a sampling grid of 10 units; (b) lung cancer mortality in young male residents (expressed as observed/expected cases × 100), in the Italian region of Veneto. Scale intervals are based on percentiles of values distribution. Reprinted by permission from Springer Nature: Cislaghi and Nimis, “Lichens, air pollution and lung cancer”. ©Nature, 387:463–464, 1997.
A number of years later, in 2013, the Lyon-based International Agency for Research on Cancer (IARC—an agency that analyzes and classifies cancer-causing agents and substances on behalf of the World Health Organization) formally ranked the cocktail of combustions caused by traffic, heating, and industrial emissions in “group 1—definitely carcinogenic”. Accordingly, since 2013 the IARC, as the world’s leading cancer authority, has officially stated that particulates and various substances found in the atmosphere of our cities represent an unequivocally carcinogenic mixture for humans. Consider in this regard that particulate matter and tropospheric ozone have such negative effects on human health that, in many areas of the world, they surpass the total toxicity attributable to all the other airborne substances.
Given the above, a clarification should be made: areas particularly susceptible to pollution (especially to atmospheric pollution) include the vast urban and suburban districts/territories of Los Angeles, Mexico City, Central/Southern Asia, and the Chinese metropolises. Unfortunately, they also comprise the Po Valley in Northern Italy [2,3], formed by part of the regions of Piedmont, Lombardy, Emilia-Romagna, Veneto, and Friuli-Venezia Giulia. In actual fact, values of air pollution in the Po Valley exceed target limits to an almost chronic and sometimes alarming extent (see Figure 2 for a representative example). Due to the presence of the Alps (Central-Southern Europe’s highest mountains), which close the Italian peninsula to the northwest, overall reduced wind speed, average continental temperatures, high atmospheric humidity, and huge anthropic pressure, the Po Valley unfortunately has a series of characteristics that make it ideal for chronic persistence of pollutants, which are damaging for air, water, soil, and the organisms that populate them, including people.
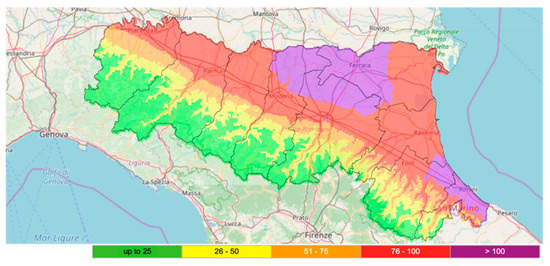
Figure 2.
Exemplifying map of the particulate matter (PM10) levels (expressed as µg m−3) reached in the Emilia-Romagna region, whose Northern/Western part is comprised in Italy’s Po Valley. Date: 16 January 2020, illustrating the recurrent situation on a number of many autumn/winter days. Printed by permission of the Environmental and Energy Protection Agency of Emilia-Romagna (ARPAE; http://www.arpae.it/, suite modelling “NINFA”), kindly acknowledged.
Thus, it is no coincidence that in the Po Valley, as indeed in Chinese metropolises, trends in certain contaminants are not decreasing over time; instead they are stationary, or even increasing. In relatively restricted, highly urbanized areas, the levels of pollutants often reach extreme peaks that damage the environment and pose a serious threat to human health. The damp climate, the absence of adequate ventilation, and in some cases the low temperatures are clearly all factors that combine to causing atmospheric stagnation, thus contributing towards air pollution.
2. Origin and Characteristics of Particulates
Particulates are microscopic solid or liquid particles temporarily suspended in the air. Aerosols, i.e., a combination of liquid droplets and solid particles, are also a form of particulate. The main natural and anthropogenic sources are volcano emissions, sand, rock erosion, forest fires, leaf litter, sewage manure spreading, pollens, lichen propagules, micrometeorites, quarries, mines, landfills, incinerators, cement plants, crumbled plaster, asphalt, motorized traffic, wear of brakes and tires, exhaust gases from aircraft engines, industrial fumes, domestic heating, foundries, steel mills, coal or heavy oil power plants, etc. Particulates also form abundantly in the atmosphere when low vapor pressure substances condensate, and/or following (photo)chemical reactions between gaseous primary pollutants, such as nitrogen and sulfur oxides, ozone, volatile organic compounds, and ammonia; all these are substances found in considerable amounts in densely-populated areas.
From a dimensional standpoint, particles that make up particulates are considered “coarse” if they have a diameter greater than 2.5 µm. Below this size, they are called “fine or thin” (<2.5 µm, up to 100 nm), “ultrafine” (up to 10 nm), or “nanoparticles” (up to 2 or very few nm). Refer to Figure 3 for a comparison between the average diameter of a human hair and some different airborne particles.
Figure 3.
Schematic dimensional comparison between some particles and the cross-section of a human hair (60 µm).
The amount of particulate matter in a certain volume of air is indicated by an index, called PM (which stands for “particulate matter”). The most common PM indices are PM10 and PM2.5, which indicate the total concentration of particles with a diameter of less than 10 and 2.5 µm, respectively. PM concentrations are currently expressed in µg m−3 of air. Unfortunately, there are still no official indices for ultrafine particles and nanoparticles. We can get an understanding of the “order of magnitude” if we bear in mind that the amount of particulate matter that can accumulate annually in a polluted area is in the order of hundreds of tons per 10,000 m2 (per hectare). See Figure 4 for a microscopic observation of the particulate matter deposited on a biological surface.
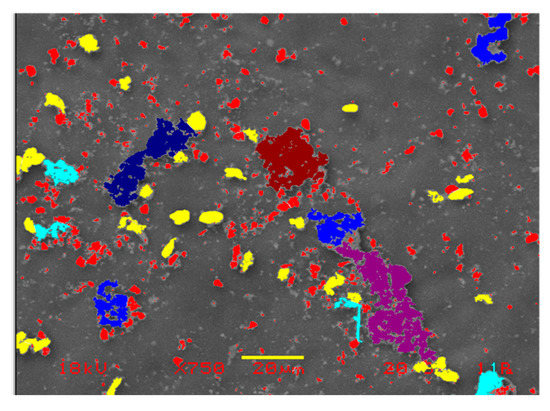
Figure 4.
Particulate matter deposition on a biological surface. Colors indicate the dimensional ranges of particles: red, ∅ < 1 µm; yellow, ∅ ~ 4 µm; light blue, ∅ ~ 8 µm; blue/dark blue, ∅ ~ 11.5 µm. Dimensional bar = 20 µm. Photo courtesy of Professor G. Lorenzini (University of Pisa, Italy), kindly acknowledged.
The World Health Organization has established that the maximum tolerable limits of PM10 and PM2.5 must not exceed an annual average of 20 and 10 µg m−3 of air, respectively; and 50 and 25 µg m−3 of air in 24 h, respectively. In the European Union and in Italy, the limits are as follows (Legislative Decree 155 of 13/8/2010 and EU Directive 2008/50/EC):
- PM10: 40 µg m−3 not to be exceeded as annual mean; and 50 µg µg m−3 not to be exceeded more than 35 times per year as daily mean.
- PM2.5: 25 µg m−3 not to be exceeded as annual mean, with the aim of not exceeding 20 µg m−3 as an annual mean starting from 1 January 2020.
3. Particulate Matter has Very Negative Effects on Environmental and Human Health
Given the above, based on current legislation, the overall situation in Italy (particularly in the Po Valley) is far from reassuring, because the legal limits are frequently exceeded, sometimes constantly in autumn/winter. The United Nations Environmental Program predicts that from 2020 the number of deaths in the world from air pollution could exceed 8 million (whilst in 2001 they numbered around 3 million). Unfortunately, little or nothing is known about fine, ultrafine, and nanoparticles, although they can in fact have a devastating impact on human health [4,5,6,7]. However, one thing is clear: fine, ultrafine, and nanoparticles are like gases, and tend to remain in suspension almost indefinitely. Simply put, a particle with a diameter half that of another, settles four times slower than the first. Indeed, the smaller the particles, the deeper they penetrate tissues and cells (even in our lungs), causing serious damage and/or carrying toxic substances, spores, viruses, bacteria [8,9,10,11,12,13], and in general anything that should not normally enter the body. One significant example is cadmium oxide (CdO), a constituent of particulate matter that has been associated with a 2.5-fold increase in the risk of chronic obstructive pulmonary disease [14].
In this regard, we should bear in mind one serious issue as regards indices coded by law for measuring the atmospheric particulate matter. For many years now, it has been a given that 1000 atmospheric particles of 1 µm (and, what is even more serious, one million particles from 100 nm) weigh as much as a single 10 µm particle [15]. However, as Dr. Stefano Montanari correctly points out, “the law makes no difference between a large particle and a million small particles. For science, however, the difference is immense. The absurd paradox is that we could breathe air that is “officially” clean (i.e., polluted below the law limits), but in fact composed of thousands of particles that have a potentially devastating impact on our lungs, our blood and our health” [15]. As a result, current legal limits are by no means a guarantee that the particulates have little impact on the environment or indeed on our bodies.
One notable feature of all particulates is that they can convey (and release) toxic molecules and/or microorganisms and/or spores and/or viral particles, etc. [8,9,10,11,12,13]. These components can be absorbed or adsorbed by the particulate particles, depending on whether they enter them (where they are potentially solubilized), or whether they bind to the external surface. Moreover, the particles can be broken, thus multiplying their polluting and carrying power. Particulate matter, especially fine/ultrafine/nanoparticles, can enter the bronchi and the lung alveoli (Figure 5) as well as the blood (both plasma and erythrocytes), the coronary arteries, the heart, the lymphatic system, and, ultimately, almost all organs, with serious or very serious consequences for health (e.g., carcinogenic and/or teratogenic effects). Last but not least, the smallest particles can enter the cell nucleus and target DNA, with devastating results [16].
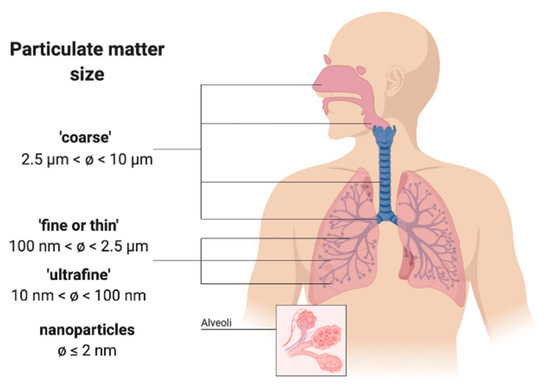
Figure 5.
The particulate matter of various sizes can penetrate the respiratory tract, in some cases up to the pulmonary alveoli.
As long ago as 1997–2001, official studies carried out by the Environmental Protection Agency of Italy’s Emilia-Romagna region (in the March–April 2020 “red zone”, due to the novel coronavirus spread) stated that “the qualitative and quantitative differences of the mutagenic effects found in samples of atmospheric particulate taken at different points of the network, as well as on the same site at different times, underline how urban atmospheric particulate matter is a complex mixture of mutagenic substances in continuous evolution, following changes in pressure factors and sources of pollutants, the influence of weather-climate conditions, place, seasonality, etc. The evidence of biological activity and the presence of ultrafine particles, above all PM2.5, poses an important risk factor for the health of citizens; it is therefore necessary to commit resources to primary prevention, particularly for long-term health effects, as a consequence of exposure to the finest particles”. The above was published in a report by Dr. Francesca Cassoni back in August 2002. What has changed in the intervening decades? Almost nothing, unfortunately.
4. Particulate Matter Causes Severe Diseases, but Drastic Measures to Reduce It have yet to be Taken
Taking all the above into account, we reach here the core of the whole issue: authoritative international publications have correlated atmospheric particulate matter with increased incidence of human diseases, including viral ones. In particular, lung diseases are significantly affected by the level of contamination in the atmosphere.
Italy’s Po Valley is doubtless one of the most polluted areas in the world [2,3]. Alarmingly, in this area, atmospheric particulate levels are comparable with those found in the Chinese metropolises, such as Wuhan (Central-Eastern China, over 6 million inhabitants). Of course, we are not presenting here a simplistic argument that deterioration of the environment is the only cause of the increase in viral diseases, in this case, of viruses associated with respiratory infections such as the novel coronavirus, but we are very inclined to believe that it is a significant contributing cause.
We examined authoritative scientific literature in the world’s leading databases. By way of example, this included an interesting publication entitled: “PM10 exposure is associated with increased hospitalizations for respiratory syncytial virus bronchiolitis among infants in Lombardy, Italy” [17]. This viral disease affecting children can become very severe and therefore require immediate hospitalization. The aforementioned scientists write that “exposure to environmental factors (e.g., air pollution) could influence the immune system and compromise its ability to limit the spread of infectious agents”, as is the case with the virus they studied. In addition, they add, “Exposure to air pollution is related to the worsening of respiratory diseases in adults and children”, along the same lines of the findings reported by Jo et al. [18] in relation to Korea (also badly affected by the novel coronavirus). Carugno and et al. [17] conclude that the concentration of PM10 in Lombardy, Italy, in the two weeks preceding hospitalization was strongly associated with an increased risk of hospitalization for the viral pathology they studied. This general conclusion is also supported by research carried out by various groups in Israel, Chile, Canada, Australia, and New Zealand, to name a few [19,20,21,22].
Another distinguished study carried out in China on over 36,000 children (city of Hangzhou, over 6 million inhabitants, Eastern China), reveals a positive correlation between infection with respiratory syncytial virus and atmospheric levels of PM2.5 and PM10 (almost systematically above the limits imposed by the World Health Organization); conversely, there is a negative correlation with temperature [23]. This means that higher temperatures have led to a decrease in the infection rate. Within the framework of the research, the most critical situation arose below 9 °C, while there was a marked improvement in health where temperatures were upwards of 20 °C. Essentially, similar results have been found by a number of studies conducted worldwide. In fact, dozens of experimental works published in international scientific journals have highlighted the close link between the level of air pollution and the incidence of respiratory diseases (including viral ones). They include Gordon et al., 2014; Liang et al., 2014; Walton et al., 2010; and Xu et al., 2013, to name a few [4,24,25,26].
In this regard, some scientists believe that the oxidative stress caused by air pollution, and in particular by particulate matter, may have negative effects on immune responses by interfering with the body’s antiviral defenses. Some studies actually support the theory that exposure to atmospheric pollutants can in fact (1) reduce the ability of macrophages to phagocytize pathogens, even viral ones; and (2) decrease the expression or activity of particular protective proteins against viral infections [10].
A large number of epidemiological studies conducted worldwide have found a clear link between air pollution levels and hospitalization for various diseases, particularly of a respiratory kind, as well as greater associated morbidity and mortality. Viral respiratory infections can be caused by over 200 different viruses, including rhinovirus, respiratory syncytial virus, influenza and parainfluenza virus, coronavirus, and adenovirus [27]. Unfortunately, regulations concerning microbial air contamination are lacking.
As regards the “novel coronavirus” (SARS-CoV-2), which causes the current COVID-19 disease (an acronym of COronaVIrus Disease), Conticini et al. (2020) [28] showed that atmospheric pollution can be considered a co-factor contributing to the extremely high level of lethality currently occurring in Northern Italy. Of course, it is not easy to discern between the rate of novel coronavirus spread in the population versus frequency of severe cases, as data in authoritative literature have been almost absent until now. However, Wu et al. (2020) [29] have demonstrated a large overlap between cause of death in COVID-19 patients and long-term exposure to PM2.5. In particular, these authors state that an increase of just 1 µg m−3 in PM2.5 is associated with a 15% increase in the COVID-19 death rate. In addition, correctly, they conclude, “The study results underscore the importance of continuing to enforce existing air pollution regulations to protect human health, both during and after the COVID-19 crisis”. In addition, Yao et al. (2020) [30] found in 49 Chinese cities (including Wuhan) that COVID-19 death rates in winter 2020 were higher where concentrations of PM2.5–10 were greater, possibly affecting the outcome for patients with mild to severe symptoms, and influencing the prognosis of COVID-19 patients. Also Martelletti and Martelletti (2020) [31] postulated a correlation between elevated concentrations of PM and the high spread and mortality rate of the novel coronavirus in Italy.
6. Conclusions
The Acting Secretary General of the European Public Health Alliance (EPHA) has declared: “The air may be clearing in Italy, but the damage has already been done to human health and people’s ability to fight off infection. Governments should have tackled chronic air pollution long ago, but have prioritised the economy over health. Science tells us that epidemics like COVID-19 will occur with increasing frequency. So, cleaning up the streets is a basic investment for a healthier future”. Indeed, administrators and governments must view potential interactions between exposure to pollutants (not only particulate matter, but also other solid, liquid, and gaseous contaminants) and the onset of pathologies (including those generated by respiratory viruses) as a tangible risk. The hypothesis that the novel coronavirus might exploit the “highways” made up of atmospheric particulates is a challenging point that, in our opinion, deserves further, immediate, and in-depth experimental investigations. It is to be hoped that steps will be taken promptly to clarify the dynamics involved in the current pandemic. However, above all, far-sighted measures are urgently needed to reduce air, water, and soil pollution drastically. The environment around us and our health demand it.
Author Contributions
Conceptualization, data curation, writing, and original draft preparation: L.S.d.T. (Luigi Sanità di Toppi), L.S.d.T. (Lorenzo Sanità di Toppi), and E.B. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cislaghi, C.; Nimis, P.L. Lichens, air pollution and lung cancer. Nature 1997, 387, 464. [Google Scholar] [CrossRef] [PubMed]
- European Environment Agency; European Topic Centre on Air Pollution and Climate Change Mitigation (ETC/ACM). Air Quality in Europe: 2017 Report; European Environment Agency: København, Denmark, 2017. [Google Scholar]
- Van Donkelaar, A.; Martin, R.V.; Brauer, M.; Kahn, R.; Levy, R.; Verduzco, C.; Villeneuve, P.J. Global Estimates of Ambient Fine Particulate Matter Concentrations from Satellite-Based Aerosol Optical Depth: Development and Application. Environ. Health Perspect. 2010, 118, 847–855. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.B.; Bruce, N.G.; Grigg, J.; Hibberd, P.L.; Kurmi, O.P.; Lam, K.H.; Mortimer, K.; Asante, K.P.; Balakrishnan, K.; Balmes, J.; et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2014, 2, 823–860. [Google Scholar] [CrossRef]
- Tellabati, A.; Fernandes, V.E.; Teichert, F.; Singh, R.; Rylance, J.; Gordon, S.; Andrew, P.W.; Grigg, J. Acute exposure of mice to high-dose ultrafine carbon black decreases susceptibility to pneumococcal pneumonia. Part. Fibre Toxicol. 2010, 7, 30. [Google Scholar] [CrossRef]
- Chen, R.; Hu, B.; Liu, Y.; Xu, J.; Yang, G.; Xu, D.; Chen, C. Beyond PM2.5: The role of ultrafine particles on adverse health effects of air pollution. Biochim. Biophys. Acta (BBA)-Gen. Subj. 2016, 1860, 2844–2855. [Google Scholar] [CrossRef]
- Stone, V.; Johnston, H.; Clift, M.J.D. Air Pollution, Ultrafine and Nanoparticle Toxicology: Cellular and Molecular Interactions. IEEE Trans. Nanobiosci. 2007, 6, 331–340. [Google Scholar] [CrossRef]
- Xia, T.; Korge, P.; Weiss, J.N.; Li, N.; Venkatesen, M.I.; Sioutas, C.; Nel, A. Quinones and Aromatic Chemical Compounds in Particulate Matter Induce Mitochondrial Dysfunction: Implications for Ultrafine Particle Toxicity. Environ. Health Perspect. 2004, 112, 1347–1358. [Google Scholar] [CrossRef]
- Asgharian, B.; Price, O.T. Deposition of Ultrafine (NANO) Particles in the Human Lung. Inhal. Toxicol. 2007, 19, 1045–1054. [Google Scholar] [CrossRef]
- Ciencewicki, J.; Jaspers, I. Air Pollution and Respiratory Viral Infection. Inhal. Toxicol. 2007, 19, 1135–1146. [Google Scholar] [CrossRef]
- Kreyling, W.G. Nanoparticles in the lung. Nat. Biotechnol. 2010, 28, 1275–1276. [Google Scholar] [CrossRef]
- Dumkova, J.; Vrlikova, L.; Vecera, Z.; Putnova, B.; Docekal, B.; Mikuska, P.; Fictum, P.; Hampl, A.; Buchtova, M. Inhaled Cadmium Oxide Nanoparticles: Their in Vivo Fate and Effect on Target Organs. IJMS 2016, 17, 874. [Google Scholar] [CrossRef]
- Onat, B.; Alver Şahin, Ü.; Sivri, N. The relationship between particle and culturable airborne bacteria concentrations in public transportation. Indoor Built Environ. 2017, 26, 1420–1428. [Google Scholar] [CrossRef]
- Rokadia, H.K.; Agarwal, S. Serum Heavy Metals and Obstructive Lung Disease: Results from the National Health and Nutrition Examination Survey. Chest 2013, 143, 388–397. [Google Scholar] [CrossRef] [PubMed]
- Montanari, S. L’insidia Delle Polveri Sottili e Delle Nanoparticelle; Macroedizioni: Cesena, Italy, 2007; ISBN 978-88-7507-849-2. [Google Scholar]
- Kim, K.-H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Carugno, M.; Dentali, F.; Mathieu, G.; Fontanella, A.; Mariani, J.; Bordini, L.; Milani, G.P.; Consonni, D.; Bonzini, M.; Bollati, V.; et al. PM10 exposure is associated with increased hospitalizations for respiratory syncytial virus bronchiolitis among infants in Lombardy, Italy. Environ. Res. 2018, 166, 452–457. [Google Scholar] [CrossRef] [PubMed]
- Jo, E.-J.; Lee, W.-S.; Jo, H.-Y.; Kim, C.-H.; Eom, J.-S.; Mok, J.-H.; Kim, M.-H.; Lee, K.; Kim, K.-U.; Lee, M.-K.; et al. Effects of particulate matter on respiratory disease and the impact of meteorological factors in Busan, Korea. Respir. Med. 2017, 124, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Yitshak-Sade, M.; Yudovitch, D.; Novack, V.; Tal, A.; Kloog, I.; Goldbart, A. Air Pollution and Hospitalization for Bronchiolitis among Young Children. Ann. ATS 2017, 14, 1796–1802. [Google Scholar] [CrossRef]
- Pino, P.; Walter, T.; Oyarzun, M.; Villegas, R.; Romieu, I. Fine Particulate Matter and Wheezing Illnesses in the First Year of Life. Epidemiology 2004, 15, 702–708. [Google Scholar] [CrossRef]
- Barnett, A.G.; Williams, G.M.; Schwartz, J.; Neller, A.H.; Best, T.L.; Petroeschevsky, A.L.; Simpson, R.W. Air Pollution and Child Respiratory Health: A Case-Crossover Study in Australia and New Zealand. Am. J. Respir. Crit. Care Med. 2005, 171, 1272–1278. [Google Scholar] [CrossRef]
- Lin, M.; Stieb, D.M.; Chen, Y. Coarse Particulate Matter and Hospitalization for Respiratory Infections in Children Younger Than 15 Years in Toronto: A Case-Crossover Analysis. Pediatrics 2005, 116, e235–e240. [Google Scholar] [CrossRef]
- Ye, Q.; Fu, J.; Mao, J.; Shang, S. Haze is a risk factor contributing to the rapid spread of respiratory syncytial virus in children. Environ. Sci. Pollut. Res. 2016, 23, 20178–20185. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Fang, L.; Pan, H.; Zhang, K.; Kan, H.; Brook, J.R.; Sun, Q. PM2.5 in Beijing—Temporal pattern and its association with influenza. Environ. Health 2014, 13, 102. [Google Scholar] [CrossRef] [PubMed]
- Walton, N.A.; Poynton, M.R.; Gesteland, P.H.; Maloney, C.; Staes, C.; Facelli, J.C. Predicting the start week of respiratory syncytial virus outbreaks using real time weather variables. BMC Med. Inform. Decis. Mak. 2010, 10, 68. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Hu, W.; Williams, G.; Clements, A.C.A.; Kan, H.; Tong, S. Air pollution, temperature and pediatric influenza in Brisbane, Australia. Environ. Int. 2013, 59, 384–388. [Google Scholar] [CrossRef]
- Dasaraju, P.V.; Liu, C. Infections of the Respiratory System. In Medical Microbiology; Baron, S., Ed.; University of Texas Medical Branch at Galveston: Galveston, TX, USA, 1996; ISBN 978-0-9631172-1-2. [Google Scholar]
- Conticini, E.; Frediani, B.; Caro, D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020, 114465. [Google Scholar] [CrossRef]
- Wu, X.; Nethery, R.C.; Sabath, B.M.; Braun, D.; Dominici, F. Exposure to Air Pollution and COVID-19 Mortality in the United States. medRxiv 2020. [Google Scholar] [CrossRef]
- Yao, Y.; Pan, J.; Wang, W.; Liu, Z.; Kan, H.; Meng, X.; Wang, W. Spatial Correlation of Particulate Matter Pollution and Death Rate of COVID-19. medRxiv 2020. [Google Scholar] [CrossRef]
- Martelletti, L.; Martelletti, P. Air Pollution and the Novel Covid-19 Disease: A Putative Disease Risk Factor. SN Compr. Clin. Med. 2020. [Google Scholar] [CrossRef]
- Sajadi, M.M.; Habibzadeh, P.; Vintzileos, A.; Shokouhi, S.; Miralles-Wilhelm, F.; Amoroso, A. Temperature, Humidity and Latitude Analysis to Predict Potential Spread and Seasonality for COVID-19. 2020. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3550308 (accessed on 28 April 2020). [CrossRef]
- Setti, L.; Passarini, F.; de Gennaro, G.; Di Gilio, A.; Palmisani, J.; Buono, P.; Fornari, G.; Perrone, M.G.; Piazzalunga, A.; Barbieri, P.; et al. Relazione Circa L’effetto Dell’inquinamento da Particolato Atmosferico e la Diffusione di Virus Nella Popolazione. Position Paper. 2020. Available online: file:///C:/Users/Utente/Desktop/coronavirus/position%20paper.pdf (accessed on 10 March 2020).
- Cui, Y.; Zhang, Z.-F.; Froines, J.; Zhao, J.; Wang, H.; Yu, S.-Z.; Detels, R. Air pollution and case fatality of SARS in the People’s Republic of China: An ecologic study. Environ. Health 2003, 2, 15. [Google Scholar] [CrossRef]
- Zhao, Y.; Richardson, B.; Takle, E.; Chai, L.; Schmitt, D.; Xin, H. Airborne transmission may have played a role in the spread of 2015 highly pathogenic avian influenza outbreaks in the United States. Sci. Rep. 2019, 9, 11755. [Google Scholar] [CrossRef]
- Reche, I.; D’Orta, G.; Mladenov, N.; Winget, D.M.; Suttle, C.A. Deposition rates of viruses and bacteria above the atmospheric boundary layer. ISME J. 2018, 12, 1154–1162. [Google Scholar] [CrossRef]
- Van Doremalen, N.; Bushmaker, T.; Morris, D.; Holbrook, M.; Gamble, A.; Williamson, B.; Tamin, A.; Harcourt, J.; Thornburg, N.; Gerber, S.; et al. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. N. Engl. J. Med. 2020, 382, 16. [Google Scholar] [CrossRef]
- Setti, L.; Passarini, F.; Gennaro, G.D.; Barbieri, P.; Perrone, M.G.; Borelli, M.; Palmisani, J.; Gilio, A.D.; Torboli, V.; Pallavicini, A.; et al. SARS-Cov-2 RNA Found on Particulate Matter of Bergamo in Northern Italy: First Preliminary Evidence. medRxiv 2020. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).