Abstract
This study aimed to evaluate the effect of the spiritual support intervention on spirituality and the clinical parameters of women who have undergone mastectomy. This is a pilot study of a randomized clinical trial. The spiritual support intervention was composed of meditation, guided imagery, music, and respiratory relaxation. The outcomes were: spirituality, blood pressure, heart rate, and oxygen saturation. A total of 27 patients were recruited for the study (intervention group, n = 13; control group, n = 14) (Clinical Trials: NCT 01866670/CAE: 00896312.0.0000.5393). The intervention helped patients with breast cancer to increase expression of their spirituality (p = 0.040) and it also decreased heart rate on the first (p = 0.038) and third day (p = 0.017). There was a difference in oxygen saturation on the second day in the control group (p = 0.039). Patients reported that their participation in the research was positive. This intervention had an effect on the sample of women who had undergone mastectomy.
1. Introduction
The World Health Organization (WHO) considers the spiritual dimension of healthcare to be relevant and represents a criterion for high-quality care to patients with chronic conditions such as cancer [].
Spirituality refers to connectedness, a sense of being human, transcendence, and meaning in life [,]. Regardless of the similarities between spirituality and religiosity, spirituality is considered to have a religious and non-religious dimension, related to finding meaning in life, while religiosity is related to specific beliefs, rituals, and values [].
Nurses should attend to patients as holistic beings, therefore the answers to life and illness related to spirituality may result in nursing diagnoses. For example, the nursing diagnosis of spiritual distress of NANDA International, Inc. (NANDA-I), that is listed since 1978, has been identified in people with chronic illness, and has been diagnosed in 42.2% of 45 hospitalized elderly patients with cancer [], women with breast cancer [], and patients undergoing chemotherapy []. Distinct interventions are recommended to cure, manage, or prevent this diagnosis, including spiritual support [].
Several interventions regarding the nursing care of patients in spiritual distress were found in a literature review []. The Elias et al. [] research was based on relaxing, guided imagery and spirituality, and was the foundation for this pilot study. This study used an intervention composed of those therapies, in a manner that could be standardized and controlled.
Meditation, relaxation, listening to music, and guided imagery are the interventions considered appropriate for spiritual support and are listed in the Nursing Interventions Classification []. In relation to the isolated effect of each intervention, a relationship has been found between loving-kindness meditation focused on the cardiac chakra and positive emotions, when developed by experienced facilitators over a long period of time []. Moreover, respiratory relaxation can reduce anxiety [], help to recover physical equilibrium, and influence the immune response []. Music can increase parasympathetic nervous system activity and provoke a drop in the heart rate (HR), blood pressure (BP) and, consequently, in cardiac output and oxygen saturation, particularly when chosen by the patient []. Guided imagery was associated with less fatigue and sleep problems, when carried out on pre- and postoperative patients [].
No studies were identified in the literature that combine these activities in randomized clinical trials. In this study, the intervention—spiritual support—consisted of relaxation, music, guided imagery and meditation, and the objective was to analyze the effect on clinical outcomes (heart rate, blood pressure, and oxygen saturation) and spirituality in mastectomized women.
2. Methods
A randomized controlled clinical trial was undertaken at the Teaching, Research, and Care Group for the Rehabilitation of women who have undergone mastectomy (REMA) at Ribeirão Preto College of Nursing of the University of São Paulo (EERP-USP). This centre works with breast cancer patients in rehabilitation. Participants were recruited based on the following inclusion criteria: breast cancer diagnosis; mastectomy in the last five years, and still continuing breast cancer treatment (surgical treatment, chemotherapy, or radiotherapy); aged over 18 years; no recorded history of psychiatric illnesses involving hallucinations; no reduced cognition, assessed by the mental state examination []; physical ability to perform activity, assessed using the Zubrod Scale []. The Zubrod scale is usually used to assess exercise capacity. It is a rating scale with the following grades: 0 (those who accomplish activities normally), 1 (symptoms of the disease, is able to walk while preserving daily activities), 2 (able to stay out of bed more than 50% of the time), 3 (remains in the bed more than 50% of the time and in need of intensive care), 4 (dependent patient, requiring active support treatment, end-of-life) [,]. A score lower than or equal to 3 was considered for this criterion, in order to reduce bias in the breathing exercise. All women attending the clinic were invited to participate in the study and scored lower than three. Patients receiving any complementary treatment were excluded from the study.
From the total population of women attending REMA, 136 women who underwent a mastectomy in the last five years were registered. All the women were invited to participate according to the inclusion criteria. For this pilot study a sample of 12 in each group was the target to test the feasibility of this intervention in a larger population. After analyzing the inclusion criteria, 27 women participated in the study: 14 were allocated to the control group and 13 to the experimental group (Figure 1). The randomization in two groups (experimental and control) was based on software of SPSS. Blinding was not possible as the intervention was behavioral. All participants had contact with the same researchers and the interventions were performed in the same environment. Each patient participated individually in this study. The short data collection period was chosen due to the nature of the intervention and the availability of the participants.
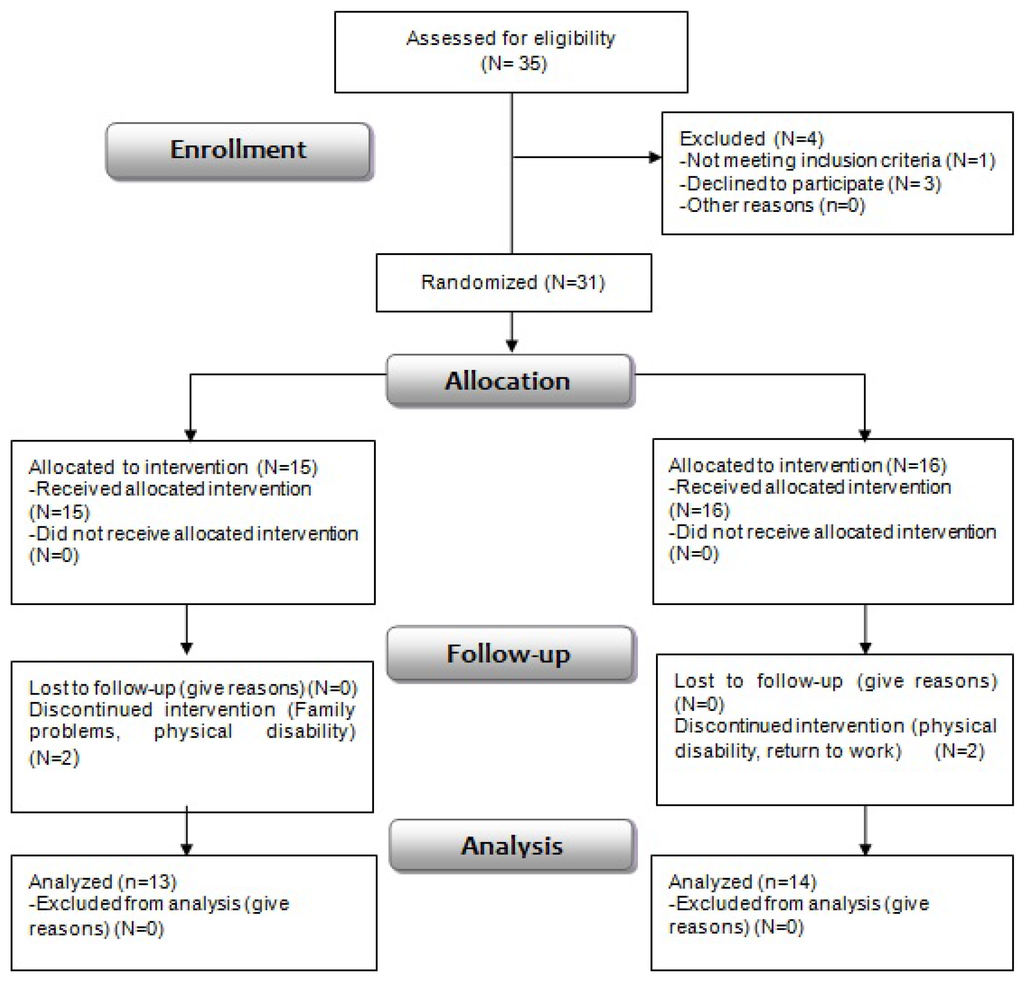
Figure 1.
CONSORT flow diagram of research participants’ allocation [].
In the experimental group, the spiritual support intervention consisted of respiratory relaxation, guided imagery, music, and meditation, in this sequence. Description of guided imagery: (1) Each patient was encouraged to visualize or feel her spiritual being according to her beliefs or preferences; (2) Encouraged to create love and inner light. The more love she felt, the more her heart would be lit up; (3) We encourage the patient to light the environment and connect with their spiritual being, connecting with the internal and external environment. The women were in mediation when focusing on the ambient light, remaining silent and only being focused on feeling love and the lighting.
Each participant in the control group only underwent respiratory relaxation. The intervention in the control group was based on Polit and Beck [], who consider the use of part of the experimental intervention as being relevant.
The sociodemographic variables were: age (years), education level (years of study), occupation, religion, and spiritual being the participant most identifies with or believes in.
The spirituality scores were assessed on the first and third days, using the Spirituality scale [] validated in Brazil []. The total score is obtained by adding up its five items []. If the score is higher than the median, spiritual wellbeing can be considered. The scale consists of two subscales (“Beliefs” and “Hope and optimism”). The score of each subscale was reached by adding up the items related to its dimension: the first two items make up the Beliefs subscale, and the final three items the Hope and Optimism subscale. The median of each item is 2.5. Values below the cut-off point indicate a low score, while higher values are considered a high score [,].
The spirituality scale (Pinto and Pais-Ribeiro) was validated in Brazilian cancer patients and it was chosen for this study because it was considered adequate in previous research []. The number of items was considered an advantage since they were being used in clinical settings.
The participant’s experience in the research was assessed by scoring their perception of how taking part in the research contributed to their spirituality, the extent to which they enjoyed participating in the research, and their opinion about the importance of spiritual care by nurses, on a scale of 0 to 10.
The clinical outcomes assessed over the three days (D1, D2 and D3) were: heart rate (HR), oxygen saturation (SatO2), systolic (SBP) and diastolic (DBP) blood pressure, measured with a multiparameter Bionet BM5® monitor.
The data were compiled in an Excel 8.0 worksheet and analyzed using SPSS. The significance was 5% (p < 0.05) for all tests. Wilcoxon’s test was used for dependent variables and Mann-Whitney’s test for independent variables, due to the number of participants. The continuing variables revealed the homogeneity of the research group, as verified by means of the Mann-Whitney test at the baseline of the study.
Institutional Review Board approval was sought from the Ribeirão Preto College of Nursing of University of São Paulo, CAE: 00896312.0.0000.5393. The study was also registered with Clinical Trials identification number: NCT 01866670. Consent was guaranteed by a free and informed consent form.
3. Results
Twenty-seven women participated in the study, randomized into a control group (n = 14) and experimental group (n = 13) (Table 1). Ages ranged between 35 and 77 years, with a mean age of 55.92 years (SD = 11.63) and median age of 53.50 years. The mean age in the control group was 54.69 years (SD = 12.54) and the median 52 years. The experimental group had higher mean age, of 57.15 years (SD = 11.02) and a median age of 58 years.

Table 1.
Demographic data.
Most participants had low education levels, as they indicated they had not finished basic education (48.14%) and had never been to school (11.11%). In relation to occupation, 29.62% were housewives and 18.51% retired. In both groups, the percentage of women who were housewives and who had a profession were the same (48.14%). Concerning religion, 66.66% were Catholic, 29.62% in the control group and 37.03% in the experimental group; 18.51% were Evangelical (14.81% of the control group) and 7.40% Spiritist (experimental group). In addition, one participant was a Jehovah Witness and another indicated no religion but that she was spiritual, both of these in the control group. When asked about the spiritual being they used to pray to or connect with, God prevailed (40.74%). Other references were Our Lady of Aparecida, Jesus, Jehovah, and Sacred Heart of Mary.
According to the Shapiro—Wilk test, the following were normally distributed: heart rate before and after the intervention of the first day (FC p = 0.36; p = 0.33); before and after the intervention of the third day (FC p = 0.27; p = 0.46); the systolic blood pressure after the first day of intervention (p = 0.12); the values of systolic and diastolic blood pressure before and after the second day of intervention (p = 0.16, p = 0.55; and p = 0.161, p = 0.33); and diastolic blood pressure values before the intervention of the third day (p = 0.65). All other variables were not normally distributed.
As regards the total spirituality score, a slight variation over the course of the study was identified in the participants. The total scores ranged between 14 and 20 (high levels), with means ranging between 17.64 and 18.77. The mean score of all participants on the spirituality scale at the baseline of the study was 18.11 (SD = 1.805; minimum 14 and maximum 20); at the end of the study, the mean was 18.19 (SD = 2.131; minimum 13 and maximum 20). No statistical intra- or inter-group differences were observed in the mean total coefficients on that scale (Table 2).

Table 2.
Spirituality Scores.
The coefficient on the Beliefs scale ranged between 4 and 8. At the baseline of the study, 77.77% (n = 21) awarded the highest score (8) on the Beliefs subscale, 14.81% (n = 4) scored 7 and 7.4% (n = 2) scored 6. The mean Beliefs score of all participants at the baseline of the study was 7.70 (SD = 0.609), while at the end of the study the mean was 7.67 (SD = 0.832). No difference was found in the mean scores before and after the intervention for both groups and between the control and experimental groups on the Beliefs subscale (Table 3).

Table 3.
Scores on the Beliefs subscale before and after the intervention.
The scores on the Hope and Optimism subscale, which assessed the existential aspect, ranged between 6 and 12. The mean score on the Hope and Optimism subscale at the baseline of the study was 10.41 (SD = 1.448) and, on the final day of the study, the mean score was 10.52 (SD = 1.784). When comparing the results between the control and experimental groups after the interventions, a difference was found (p = 0.040) (Table 4).

Table 4.
Scores on the Hope and Optimism subscale before and after the interventions.
As regards the patients’ assessment of the extent to which the research helped them in their spirituality, the data indicated a mean score of 9.04 (SD = 1.55; mean of CG = 9.07 and mean of EG = 9.0).
The patients stated, as regards their participation in the research, that they enjoyed the experience and the average score was 9.78 (SD = 0.609; mean of CG = 9.85, and of EG = 9.69). When considering the relevance of spirituality in nursing care, the participants considered it to be relevant (mean 9.70; SD = 0.609; CG mean = 9.78, and EG mean = 9.61).
Regarding the clinical variables, no statistical difference was found in the comparative assessment of the control group and the experimental group, except for heart rate (HR). The Wilcoxon test revealed a drop in the HR of the experimental group after spiritual support on D1 (p = 0.014) and D3 (p = 0.032). No differences were identified in the mean HR of the control group at any of the research phases (Table 5).

Table 5.
Heart Rate before and after the intervention over the three days.
In the Mann-Whitney test, a difference was identified on the first day after the intervention (p = 0.038), with a lower mean heart rate in the EG (82.54) than in the CG (84.00); and on the third day (p = 0.0017), with a heart rate of 75.77 in the EG and 85.00 in the CG. No differences were found in the other comparisons.
When combining data of the four participants who discontinued their participation in the study, two of the CG and two of the EG, the statistical difference in heart rate remained unchanged before and after the intervention (p = 0.001), with a mean before the intervention of 82.87 and after the intervention of 76.40. When comparing the groups using the Mann Whitney test, the statistical difference in heart rate after the intervention of the first day was maintained (p = 0.04). No statistical difference between the groups was found for the variables related to the Spirituality Scale on the first day.
4. Discussion
The age of the women who participated in the study was similar to other studies and compatible with the epidemiology of this illness [,].
As regards the participants’ education, higher levels have been found in the north of Brazil [], where 50% (n = 18) of the women with breast cancer had completed secondary education. The Brazilian Institute of Geography and Statistics (IBGE) has indicated that 22.77% of Brazilian women have completed 11 years of education [], closer to the findings in this study (33%).
The religion data are in line with the Brazilian reality. The 2010 population census showed increased diversity of religious entities in Brazil, with the number of Catholics as a majority and growing numbers of Evangelicals, Spiritists, and people without religion. 64.6% of Brazilians stated they were Catholic, 22.2% were Evangelical (60% charismatic, 18.5% mission, and 21.8% undetermined), and 2% Spiritist. The Catholic predominance was not related to gender [].
We gave participants the opportunity to choose the spiritual being they would mentally picture in the guided imagery, since in Brazilian culture the popular religions are intensely visual, mainly due to the history of subalternity and simplicity of the people [].
In terms of spirituality, women with breast cancer did not show spiritual suffering at the baseline of the study, contrary to the findings of the cited study [], showing a 42% prevalence in hospitalized women. This fact may be related to the participants’ physical and emotional condition, as they attended the activities of REMA on a weekly basis and had no severe limitations, contrary to that usually observed in hospitalized patients. Moreover, participating in the group activities may have influenced the patients’ general wellbeing and spiritual wellbeing. Both groups showed high scores when the interventions’ contribution to help them express their spirituality was assessed.
Nevertheless, when each item of the spirituality scale adopted in this study was individually assessed, the scores of the items of the Hope and Optimism subscale were noteworthy (existential domain). The low score on item 4—“I feel that my life has changed for the better”, is due to the fact these are patients being treated for breast cancer who have recently been diagnosed with a severe disease, are receiving the different treatments and are going through internal and social changes. The low scores on item 3—“I look to the future with hope”, are understandable since, owing to the severity of the disease, the treatment may not be effective and their future may be uncertain.
Two participants were in spiritual suffering at the end of the study, but as spiritual wellbeing can vary in the short term and as a result of countless factors, including aspects related to breast cancer, we considered that external events may have caused those variations. In terms of approval and satisfaction for having participated in the study, both participants attributed the maximum score.
As regards the relevance of nurses focusing more on spiritual aspects in patient care, the literature [] indicates the importance of including the spirituality domain in nursing care. Researchers [] have identified that at least 80% of cancer patients would like to participate in spiritual care activities. The difference of means (p = 0.04) in this study underlines the relevance of including spirituality in nursing care.
The literature [] indicates some possible intervening factors where oxygen saturation is concerned, related to comorbidities that can interfere with the supply of oxygen and removal of carbon dioxide gas, leading to reduced tissue blood flow, a reduced number of perfused capillary veins, a lower oxygen or carbon gas pressure gradient between capillaries and cells, deviation of the dissociation curve of oxyhemoglobin and hemoglobin concentration in the blood. Although these parameters were not the focus of this study, they may have interfered with the participants’ response, especially that of one participant with low oxygen saturation levels.
The heart rate in the experimental group dropped, which could indicate the activation of the parasympathetic nervous system. Nevertheless, no statistically provable alteration was observed in oxygen saturation and blood pressure levels. This may be related to participants’ insufficient cardiorespiratory synchronization, due to their low levels of experience with the technique or the short time span of the intervention [].
As regards blood pressure levels beyond normal parameters in 48.14% of the participants, similar data were found in other study [], in which an increase was observed in the mean SBP and DBP in age ranges similar to those of the present study’s participants. In a research study involving 380 elderly people [], 66.8% female with a mean age of 73.4 years (SD = 8.7 years), it was concluded that the mean SBP was 135mmHg (SD = 22.1) and DBP 78mmHg (SD = 11.2), ranging from 82 × 46 mmHg to 206 × 110 mmHg, and that almost half the participants (40.2%) had high blood pressure.
The non-reduction in mean BP after the interventions in both groups, both within and between the groups, may be associated with the non-impact of the intervention on that variable, considering its length and the number of times proposed. Nevertheless, another study concluded a similar effect by meditation on SBP, but without a reduction in DBP [].
Concerning the study limitations, some factors may have interfered with the data, including the small number of participants owing to patients’ availability to participate. More data related to comorbidities, including anemia, pulmonary problems, hypertension, and cancer and treatment-related conditions, is suggested for the purpose of future studies. In addition, physiological parameters were measured only once, instead of being confirmed and having the means analyzed. The length of the women’s participation in REMA was not calculated, nor was the length of contact with the research aids. The length of the intervention period, the type and length of treatment at the time of the intervention were also not considered, nor the use of a song the patients had selected.
The possible effect of relaxation on the results of both groups could not be analyzed, as each technique was not considered separately in the experimental group. Respiratory relaxation was common to all participants in both groups, and the effect was analyzed by oxygen saturation before and after the intervention.
This study did not aim to analyze the effect of each activity that composed the “spiritual support” intervention, but rather the intervention as a whole, considering the same sequence and duration of the intervention in all participants. Future studies may take into consideration the values between activities. Although this is a pilot study, the sample limited statistical data analysis.
5. Conclusions
When analyzing total scores on the spirituality scale and the Beliefs subscale, the mean score on the Hope and Optimism subscale increased for the experimental group’s participants, with a difference observed between the groups on the final day of the study.
Study researchers considered spiritual support as responsible for reducing the HR and improving the spirituality score (Hope and Optimism subscale). The women with breast cancer perceived their participation in the study as positive, as well as the extent to which the intervention helped them to express their spirituality. Additionally, they considered the inclusion of spirituality in nursing care as relevant.
The effect of spiritual support on the participants’ outcomes was considered satisfactory, and facilitated a connection with the expression of spirituality through the positive emotions obtained via meditation. Patients who participated in the relaxation, music, and guided imagery and meditation had higher scores on the Hope and Optimism subscale than the control group. On the other hand, the respiratory relaxation intervention in the CG did not provide the same spirituality outcomes as for patients of the EG.
The analysis of the effect of the spiritual support intervention on the physiological parameters of the participants who received that intervention concluded a reduction in the mean HR on days D1 and D3. No changes were found in mean blood pressure before and after the interventions and between the groups. The mean oxygen saturation on D2 in the control group had a statistical difference; the mean group performance changes when one patient with low SatO2 is excluded. No difference was found between the groups for this variable.
Acknowledgments
To the National Council for Scientific and Technological Development (CNPq) for financial support.
Author Contributions
Caroline Guilherme and Emilia Campos de Carvalho conceived and designed the RCT; Gabriela Roberta Ribeiro, Cristina Mara Zamarioli, Ana Railka de Souza Oliveira, and Ana Maria Almeida collected and analyzed the data and criticized the drafts; Caroline Guilherme and Sílvia Caldeira wrote the paper; Sílvia Caldeira and Emilia Campos de Carvalho reviewed the drafts and approved the final version.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| REMA | Research and Care Group for the Rehabilitation of Women who have undergone mastectomy |
| D1, D2, D3 | Day 1, Day 2, Day 3. |
| HR | Heart rate |
| SatO2 | Oxygen saturation |
| SBP | Systolic blood pressure |
| DBP | Diastolic blood pressure |
| CG | Control group |
| EG | Experimental group |
| SD | Standard Deviation |
References
- World Health Organization. National Cancer Control Programs: Policies Guidelines. Geneva: Health & Development Networks, 2002, p. 83. [Google Scholar]
- Harold Koenig. Handbook of Religion and Mental Health. Orlando: Elsevier, 1998. [Google Scholar]
- Elizabeth Weathers, Geraldine McCarthy, and Alice Coffey. “Concept Analysis of Spirituality: An evolutionary approach.” Nursing Forum. Available online: http://onlinelibrary.wiley.com/doi/10.1111/nuf.12128/epdf (accessed on 21 November 2015).
- Lynn Underwood-Gordon, David Jesse Peters, Polly Bijur, and Marcus J. Fuhrer. “Roles of Religiousness and spirituality in Medical Rehabilitation and the lives of persons with disabilities.” American Journal of Physical Medicine & Rehabilitation 76 (1997): 255–57. [Google Scholar] [CrossRef]
- Silvia Caldeira, Emilia Campos de Carvalho, and Margarida Vieira. “Entre o bem-estar spiritual e a angústia espiritual: Possíveis fatores relacionados a idosos com cancro.” Rev Latino-Am Enfermagem 22 (2015): 28–34. [Google Scholar] [CrossRef] [PubMed]
- Silvia Caldeira, Fiona Timmis, Emilia C. de Carvalho, and Margarida Vieria. “Nursing Diagnosis of ‘Spiritual Distress’ in Women with Breast Cancer.” In Cancer Nursing. Available online: http://www.ncbi.nlm.nih.gov/pubmed/26496518 (accessed on 21 November 2015).
- Silvia Caldeia, Fiona Timmins, Emilia Campos de Carvalho, and Margarida Vieira. “Clinical Validation of the Nursing Diagnosis Spiritual Distress in Cancer Patients Undergoing Chemotherapy.” International Journal of Nursing Knowledge. Available online: http://onlinelibrary.wiley.com/doi/10.1111/2047-3095.12105/epdf (accessed on 21 November 2015).
- Caroline Guilherme, and Emilia Campos de Carvalho. “Spiritual distress in cancer patients: Nursing interventions.” Journal of Nursing UFPE on Line 5 (2011): 290–94. [Google Scholar] [CrossRef]
- Ana Catarina Araújo Elias, Joel Sales Giglio, Cibele Andrucioli de Mattos Pimenta, and Linda Gentry El-Dash. “Therapeutical Intervention, Relaxation, Mental Images, and Spirituality (RIME) for Spiritual Pain in Terminal Patients. A Training Program.” The Scientific World Journal 6 (2006): 2158–69. [Google Scholar] [CrossRef] [PubMed]
- Gloria M. Bulechek, Howard K. Butcher, Joanne M. Dochterman, and Cheryl Wagner. Nursing Interventions Classification (NIC), 6th ed. Philadelphia: Elsevier, 2013. [Google Scholar]
- Chih-Hao Chang, and Pei-Chein Lo. “Effects of Long-Term Dharma-Chan Meditation on Cardiorespiratory Synchronization and Heart Rate Variability Behaviour.” Rejuvenation Research 16 (2013): 115–23. [Google Scholar] [CrossRef] [PubMed]
- Taís Cardoso Zeni, and Renata Brasil Araujo. “Deep breathing in the management of craving and anxiety symptoms of crack-cocaine-dependent patients.” Rev Psiquiatr Rio Gd Sul 31 (2009): 116–19. [Google Scholar] [CrossRef]
- Duck-Hee Kang, Traci McArdle, Na-Jin Park, Michael T. Weaver, Barbara Smith, and John Carpenter. “Dose effects of relaxation practice on immune responses in women newly diagnosed with breast cancer: An exploratory study.” Oncology Nursing Forum 38 (2011): E40–E52. [Google Scholar] [CrossRef] [PubMed]
- Douglas Vizzu Nobre, Hércules Ribeiro Leite, Marco Orsini, and Clynton Lourenço Corrêa. “Physiological Responses to music stimuli: Literature review.” Rev Neurocienc 20 (2012): 625–33. [Google Scholar]
- Bert Garssen, Martijn Boomsma, Eltica de Jager Meezenbroek, Terry Porsild, Johannes Berkhof, Monique Berbee, Adriaan Visser, Sybren Meijer, and Rob H. J. Beelen. “Stress management training for breast cancer surgery patients.” Psychooncology 22 (2013): 572–80. [Google Scholar] [CrossRef] [PubMed]
- Sonia M. D. Brucki, Ricardo Nitrini, Paulo Caramelli, Paulo H. F. Bertolucci, and Ivan H. Okamoto. “Suggestions for utilization of the mini-mental state examination in Brazil.” Arquivos de NeuroPsiquiatria 61 (2003): 777–81. [Google Scholar] [CrossRef]
- Instituto Nacional do Câncer. “Cancer palliative care in oncology symptom control.” Revista Brasileira de Cancerologia 48 (2002): 191–11. [Google Scholar]
- Martin M. Oken, Richard H. Creech, Douglass C. Tormey, John Horton, Thomas E. Davis, and Eleanor T. Mcfadden. “Toxicity and Response Criteria of The Eastern CooperativeOncology Group.” American Journal of Clinical Oncology 5 (1982): 649–55. [Google Scholar] [CrossRef] [PubMed]
- Brasil. Ministério da Saúde. “Instituto Nacional do Câncer. Cuidados Paliativos Oncológicos—Controle de Sintomas.” Revista Brasileira de Cancerologia 48 (2002): 243–56. [Google Scholar]
- Denise F. Polit, and Cheryl Tatano Beck. Essentials of Nursing Research: Apraising Evidence for Nursing Practice, 8th ed. Philadelphia: Wolter Kuwer Health/Lippincott Williams & Wilkins, 2013. [Google Scholar]
- Kenneth F. Schulz, Douglas G. Altman, and David Moher. “CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomized trials.” Annals of Internal Medicine 152 (2010): 726–32. [Google Scholar] [CrossRef] [PubMed]
- Cândida Pinto, and José Luís Pais-Ribeiro. “Development of a Scale for the Assessment of Spirituality in Health Settings.” Arquivos de Medicina 21 (2007): 47–53. [Google Scholar]
- Erika de Cássia Lopes Chaves, Emilia Campos de Carvalho, Rosana Aparecida Spadoti Dantas, Fábio de Souza Terra, Denis de Paula Nogueira, and Luiz de Souza. “Validation of Pinto and Pais-Ribeiro’s spirituality scale in patients with chronic renal insufficiency in hemodialysis.” Revista de Enfermagem UFPE On Line 4 (2010): 715–21. [Google Scholar] [CrossRef]
- Cândida Pinto, and José Luís Pais-Ribeiro. “Construção de uma escala de avaliação da espiritualidade em contextos de saúde.” Arquivos de Medicina 21 (2007): 47–53. [Google Scholar]
- Rodrigo Antonini Ribeiro, Maira Caleffi, and Carisi Anne Polanczyk. “Cost-effectiveness of na organized breast cancer screening program in Southern Brazil.” Cad Saúde Pública 29 (2013): 131–45. [Google Scholar] [CrossRef]
- Nathalia Santos da Penha, Daisy Esther Batista do Nascimento, Ana Cristina Costa Pantoja, Annie Elisandra Mesquita de Oliveira, Cristiane do Socorro Ferraz Maia, and Ana Carolina Soares Vieira. “Perfil sócio demográfico e possíveis fatores de risco em mulheres com câncer de mama: Um retrato da Amazônia.” Journal of Basic and Applied Pharmaceutical Sciences 34 (2013): 579–84. [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística. “Pesquisa Nacional de Amostra de Domicílios 2012.” 2012. Available online: http://ftp.ibge.gov.br/Trabalho_e_Rendimento/Pesquisa_Nacional_por_Amostra_de_Domicilios_anual/2012/tabelas_pdf/brasil_3_2.pdf (accessed on 2 August 2014). [Google Scholar]
- Instituto Brasileiro de Geografia e Estatística. “Comunicado Nacional de 2012 Sobre o Censo 2010.” 2012. Available online: http://censo2010.ibge.gov.br/noticias-censo?view=noticia&id=3&idnoticia=2170&busca=1&t=censo-2010-numero-catolicos-cai-aumenta-evangelicos-espiritas-sem-religiao (accessed on 2 August 2014). [Google Scholar]
- José de Souza Martins. “A imagem incomum: A fotografia dos atos de fé no Brasil.” Estudos Avançados 16 (2002): 223–60. [Google Scholar] [CrossRef]
- Rebecca L. Polzer Casarez, and Joan C. Engebretson. “Ethical issues of incorporating spiritual care into clinical practice.” Journal of Clinical Nursing 21 (2012): 2099–107. [Google Scholar] [CrossRef] [PubMed]
- Ana Cláudia Mesquita, Érika de Cássia Lopes Chaves, Carolina Costa Valcanti Avelino, Denismar Alves Nogueira, Raquel Gerhke Panzini, and Emilia Campos de Carvalho. “A utilização do enfrentamento religioso/espiritual por paciente com câncer em tratamento quimioterápico.” Revista Latino-Am Enfermagem 21 (2013): 539–45. [Google Scholar] [CrossRef]
- Alvaro Réa Neto. Monitorização em UTI. Rio de Janeiro: Revinter, 2004. [Google Scholar]
- Joaquim Guerra de Oliveira Neto, Dilma Aurélia de Carvalho, Guilherme Guarino de Moura Sá, Marilza Martins Monteiro, Katiuscia Danyla Carvalho Lima Lopes, and Markia do Carmo de Carvalho e Martins. “Pressão arterial e perfil socioeconômico de idosos atendidos na estratégia saúde da família de floriano-Piauí.” Revista de Saúde Pública de Santa Catarina 7 (2014): 17–28. [Google Scholar]
- Mathew J. Gregoski, Vernon A. Barnes, Martha S. Tingen, Gregory A. Harshfield, and Frank A. Treiber. “Breathing Awareness Meditation and Lifeskills Training Programs Influence Upon Ambulatory Blood Pressure and Sodium Excretion Among African American Adolescents.” Journal of Adolescent Health 48 (2011): 59–64. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).