Abstract
Background: Brucella melitensis is recognized as one of the predominant zoonotic pathogens globally. Live-attenuated vaccine Rev 1 is currently the most effective vaccine for controlling B. melitensis in small ruminants. While Brucella inactivated, nanoparticle, and subunit vaccines are less effective and require multiple doses, live-attenuated vaccines are less expensive and more efficacious. Several drawbacks are associated with the administration of current attenuated B. melitensis vaccines, including interference with serological diagnostic tests, inducing abortion in pregnant animals, shedding in milk, and zoonotic infections in humans. In this systematic review, we summarize the current literature (1970–2022) on B. melitensis vaccines and review their advantages and disadvantages in order to support the rationale for a need for new or improved small ruminant brucellosis vaccines. Methods: A systematic search was carried out in Web of Science, CAB Abstracts, and PubMed. The original articles describing the B. melitensis vaccines were included. Review articles, articles not published in English, articles that did not offer full text, editorials, correspondences, case reports, case series, diagnostic tests, duplicate publications, and other Brucella vaccines (e.g., B. abortus and B. suis) were excluded. Results: Out of 3700 studies, we identified 18 articles that evaluated B. meltensis vaccines, including recombinant B. melitensis strains (16MΔhfq, 16MΔTcfSR, M5-90ΔmanB, LVM31, M5-90ΔvjbR, 16MΔmucR, ΔznuA, M5-90Δpgm, M5-90ΔwboA), live B. melitensis strain (Rev 1), nanoparticle vaccines (B. melitensis 16M, B. melitensis OMP 31, FliC protein—Mannosylated Chitosan Nanoparticles (FliC and FliC-MCN), B. melitensis and B. abortus combined, and B. melitensis 16M nanoparticles combined with oligopolysaccharide), subunit vaccines (outer membrane vesicles or outer membrane proteins), and a DNA vaccine based on B. melitensis outer membrane proteins (Omp25 and Omp31). The results from these studies revealed that these vaccines can induce humoral and cellular responses and reduce macrophage survival. However, most of these vaccines were evaluated only in murine models, which may not accurately reflect how they work in natural hosts. Conclusions: The high prevalence of B. melitensis in humans and animals remains an issue in many parts of the world. Human brucellosis can be prevented by controlling brucellosis in livestock using vaccination and test-and-removal strategies. Prospective vaccines have limitations, including interference with serodiagnostics after vaccination, virulence in humans and animals, the requirement of booster vaccinations, and insufficient efficacy in preventing infection or abortion. Moreover, most of these vaccines have been assessed in mice models, which have failed to predict immunogenicity or efficacy in natural hosts. Because of these limitations and the re-emergence of B. melitensis worldwide with a high incidence of human infection, our review suggests a need for additional research into the molecular pathology and immunological properties of B. melitensis infection and the identification of protective epitopes or genes that would allow for the development of improved vaccines for small ruminants.
1. Introduction
Because of the high number of human cases identified each year, Brucella melitensis is one of the most important zoonotic pathogens worldwide [1]. Three biovars of B. melitensis, 1, 2, and 3, are known but are not known to differ in virulence [2]. Goats and sheep are the most common natural hosts of B. melitensis. The most common route of transmission in natural hosts is most likely through oral or respiratory mucosa. The predilection of B. melitensis for colonization of trophoblasts in the placenta and fetal tissues leads to fetal stress or death and the induction of premature parturition (abortion) [1,2]. Although abortion is the primary clinical sign, it can be minimal in chronically infected herds. In addition to the shedding of high numbers of bacteria after abortion or birth of infected lambs or kids, some animals shed high levels of bacteria in the milk. Bacterial shed after parturition poses a risk for lateral transmission to other animals [2], whereas shedding in milk is a risk for vertical transmission. It is worth noting that contaminated milk can contribute to the human transmission of this infection. Failure to prevent exposure of uninfected animals to those shedding Brucella makes control of the disease difficult. Co-housing of ruminant species is a risk factor for brucellosis transmission [3]. Camels are highly susceptible to B. melitensis infection and play an important role in its epidemiology in some countries [4]. In other countries, endemic infection has been identified in Alpine ibex (Capra ibex) and chamois (Rupicapra rupicapra) and has occasionally led to brucellosis spillover into humans and domestic livestock [5].
Since the beginning of the 20th century, researchers have been searching for vaccines to prevent brucellosis in animals and humans [6]. Both live and inactive vaccines have been developed, but live-attenuated vaccines have been found to be better at inducing protective immunity against this intracellular pathogen [7]. Although a variety of killed vaccines have been developed, their success and acceptance have been limited, and none have induced the level of protection of live-attenuated vaccines. Historically, the first Brucella vaccine using killed Brucella was made in 1906 by Eyre who used it to vaccinate 51 soldiers [7]. Two killed vaccines that had more widespread use were B. melitensis H38 and B. abortus strain 45/20 with strain 45/20 utilized in cattle and sheep and H38 in cattle [8]. Due to their limitations in protective immunity as compared to the attenuated strains and their induction of persistent antibody titers, both are no longer utilized under field conditions.
The live vaccine B. melitensis Rev 1 (Rev 1) is currently utilized for the control of brucellosis in small ruminants. This strain was developed by Herzberg and Elberg in the mid-1950s and retains common characteristics of Brucella but is resistant to streptomycin and susceptible to penicillin G [9]. Subcutaneous or conjunctival immunization with Rev 1 confers protective immunity in small ruminants. However, Rev 1 vaccination stimulates an antibody response that reacts in serological tests, which cannot be differentiated from the humoral responses of infected animals. As B. melitensis can infect cattle, limited data have been reported that suggest that vaccination with Rev 1 has some efficacy in controlling infection with this Brucella species in cattle [10].
Due to the incubation period and potential latent infections, it is difficult to eradicate brucellosis by using serologic methods to detect and remove infected animals. The inclusion of vaccination programs to improve herd resistance is generally required to control the spread of the disease. To date, Rev 1 is the best available vaccine for the prevention of B. melitensis infection in small ruminants [9] and is typically administered to young animals (3–5 months old) at 0.5–2 × 109 colony-forming units (CFU) subcutaneously. Although a bacteremia occurs after vaccination, it has been reported that the vaccine strain is cleared in approximately 14 weeks in goats. Although a reduced dose of the Rev 1 vaccine (103–106 CFU) has been suggested for subcutaneous administration, it has been found to offer limited protection against disease and does not prevent abortions [11,12]. When administered to adult sheep or goats during pregnancy at 109 CFU, abortions and shedding of Rev 1 in milk are common [11,12]. This presents a challenge in endemic areas where mass vaccination is necessary for control and pregnant sheep and goats may need to be vaccinated despite the risk of adverse effects [13]. In addition to the disadvantages listed above, the strain is also virulent to humans, and zoonotic infections have occurred during vaccination from exposure to abortions or consumption of infected milk [14,15].
Administered subcutaneously, Rev 1 vaccine stimulates protective immunity against B. melitensis but can elicit long-lasting antibody responses that interfere with serological testing. In contrast, conjunctival administration of the vaccine confers immunity similar to the standard subcutaneous approaches but reduces the magnitude and persistence of serological responses. For this reason, conjunctival vaccination has been utilized in endemic areas, as it has less impact on serologic screening and facilitates control programs. When eradication is the ultimate goal of a control program, conjunctival vaccination of Rev 1 in adult animals is ideal for enhancing herd immunity and preventing B. melitensis infections. It has been hypothesized that Rev 1 vaccination may induce a high level of protective immunity for up to 4.5 years, which essentially is lifelong immunity for small ruminants in most production systems. This hypothesis that Rev 1 vaccination induces lifelong immunity has contributed to the belief that the vaccination of young stock is sufficient for adequate control of B. melitensis infection in small ruminants. However, this vaccination strategy is tenuous, and even developed countries have failed to control brucellosis in small ruminants with this approach. The failure of vaccination of young stock only could be due to (i) failure to obtain high vaccination coverage in a herd due to animal movement or introduction of unvaccinated animals; (ii) use of poor quality vaccines or products not maintained with appropriate cold chain conditions; and (iii) a possible decrease over time of protective immunity induced by vaccination. Therefore, vaccination of whole flocks is the only viable alternative to control B. melitensis infection in small ruminants under extensive control conditions characteristic of many developing countries [16].
To develop promising vaccines against brucellosis, it is critical to produce T helper 1 (Th1)-derived cytokines (interleukin-12, tumor necrosis factor α, interferon gamma γ) associated with cellular immunity and activation of macrophages, dendritic cells, and CD4+ and CD8+ T cells. T helper 2 (Th2) immune responses associated with humoral responses do not appear to have a major role in the clearance of infection [17]. A study has demonstrated that cytokines, such as IL-4 (Th2 cytokines) and IFN-γ (Th1 cytokines), stimulate different IgG subtypes (IgG1 and IgG2 antibodies, respectively) that may be indicative of differences in the immune response [17].
Although a few recombinant B. melitensis live-attenuated, subunit, DNA, and nanoparticle vaccines have been reported, none have progressed to commercial products. Moreover, many of these candidates induce adverse effects, can infect people, induce abortion in pregnant sheep and goats, and/or interfere with serological diagnostic tests. Thus, there continues to be a need for an improved B. melitensis vaccine and additional pathobiology, immunology, and molecular research is needed to facilitate the identification of protective epitopes and develop safer and more efficacious vaccine candidates. If a new or improved Brucella vaccine has been developed, addressing the previously mentioned limitations, public health officials can take necessary measures to implement and promote its use for controlling the infection. The purpose of this systematic review was to conduct a comprehensive search of the literature on available vaccines against B. melitensis and characterize their advantages and disadvantages in order to support the rationale for the need of a small ruminant brucellosis vaccine.
2. Materials and Methods
This study was conducted in accordance with the reporting items (PRISMA) statement for systematic reviews [18]. This systematic review has not been registered in PRISMA.
2.1. Search Strategy
A systematic search was carried out in Web of Science, CAB Abstracts, and PubMed for peer-reviewed articles addressing B. melitensis vaccines that may be effective to protect against infection of small ruminants.
A comprehensive search was conducted for the following terms in both the title and abstract fields:
“Brucella melitensis vaccines” OR “Brucella melitensis vaccines in sheep” OR “Brucella melitensis vaccines in goat” OR “Brucella melitensis vaccines in cattle” OR “Brucella melitensis vaccines in bovine” OR “Caprine brucellosis vaccines” OR “Ovine brucellosis vaccines” OR “Brucella melitensis vaccines in small ruminants” OR “Malta fever vaccines” OR “undulant fever vaccines” OR “O-antigen polysaccharide Brucella melitensis vaccines” OR “O-antigen polysaccharide vaccines and Brucella melitensis” OR “O-Linked Glycosylation System Brucella melitensis vaccines” OR “O-Linked Glycosylation System vaccines and Brucella melitensis”.
2.2. Study Selection
Research articles examining B. melitensis vaccines were included in this study. A date range of publication between 1970 and 2022 was specified and not limited by geographic location. Duplicate articles were removed, and Zotero (www.zotero.org) was used as the reference software. We performed reviews of the titles, abstracts, and full text. We excluded articles describing other Brucella vaccines (e.g., B. abortus and B. suis), review articles, those not published in English, those that did not offer full text, editorials, correspondences, case reports, case series, and diagnostic tests. Since this research was a systematic review of published articles, approval from an ethical review board was not required.
2.3. Screening and Data Extraction
The data were organized in Word for the extraction process. The data extraction terms included references, publication year, vaccine name, type of vaccine, advantages, and disadvantages. The findings were included in the results if the reported data indicated that B. melitensis vaccines were efficacious in protecting small ruminants from infection or abortion.
2.4. Quality Assessment
The quality assessment of the studies was performed using a critical appraisal checklist provided by the Joanna Briggs Institute (JBI) [19].
3. Results
Figure 1 displays an overview of the literature search and study selection methodology. A total of 18 publications met the search criteria and were included for analysis.
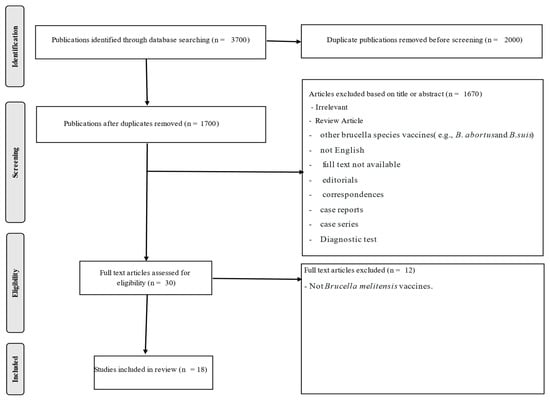
Figure 1.
Flow diagram of selection steps after search filtering procedures with Web of Science, CAB Abstracts, and PubMed.
3.1. Study Characteristics
The 18 studies described B. melitensis vaccines, including recombinant B. melitensis strains (16MΔhfq, 16MΔTcfSR, M5-90ΔmanB, LVM31, M5-90ΔvjbR, 16MΔmucR, ΔznuA, M5-90Δpgm, M5-90ΔwboA), live B. melitensis strains (Rev 1), nanoparticle vaccines (B. melitensis 16M, B. melitensis OMP 31, FliC protein—Mannosylated Chitosan Nanoparticles (FliC and FliC-MCN), B. melitensis and B. abortus combined, and B. melitensis 16M nanoparticles combined with oligopolysaccharide), subunit vaccines (outer membrane vesicles or outer membrane proteins), and DNA vaccines based on B. melitensis outer membrane proteins (Omp25 and Omp31). A summary of the vaccines described in these 18 studies to address the advantages and disadvantages is shown in Table 1.

Table 1.
Characteristics of the included studies.
3.2. Brucella melitensis Vaccines in Small Ruminants
Of the 18 included publications, nine contained information only relevant to recombinant vaccines, one to a live B. melitensis vaccine, five to nanoparticle vaccines, two to subunit vaccines, and one to a DNA vaccine. The recombinant B. melitensis 16M hfq (16MΔhfq) strain induced humoral and cellular responses in mice after intraperitoneal vaccination (ip) with increased expression of IgG1, IgG2a, IFN-γ, and IL-4. The recombinant strain did not differ from Rev 1 in the induction of cytokine responses, was cleared at approximately eight weeks post-vaccination (PV), and demonstrated protective immunity that was slightly less than Rev 1 vaccination after experimental challenge with B. melitensis 16M at eight weeks PV. [20]. Another study utilized a B. melitensis TcfSR promoter (16MΔTcfSR) recombinant strain in which one of the two-component regulatory systems that allow host cells to detect environmental changes and adapt to Brucella infection was mutated. The recombinant induced a high level of protective immunity when challenged approximately 1 week after vaccine strain clearance. Vaccination did not induce humoral responses that interfered with serodiagnostic tests [21]. The M5-90ΔwboA recombinant is a reduced virulence, attenuated vaccine that induces reduced inflammatory responses as compared to the parental strain. The reduced virulence and safety of this recombinant were based on the observation that splenomegaly did not occur in a murine host. When compared to the parental strain, comparable protection to the parental strain was observed in mice after experimental challenge approximately 1 week after vaccine strain clearance. Humoral responses in vaccinated sheep and mice allowed for vaccinates to be distinguished from infected animals [28]. Others have demonstrated that a DNA vaccine based on pcDNA3.1, encoding the ORF of B. melitensis Omp25 and Opm31 genes, may be a viable vaccine candidate due to induction of humoral (IgG) and cellular (Th1 cytokines IFN-ɣ and Th2 cytokines IL-10) in mice. The DNA vaccine construct elicited cellular and humoral responses to B. melitensis antigens after four inoculations at 1-week intervals [30]. Vaccination of mice with nanoparticle B. melitensis and B. abortus vaccines conferred less protection than Rev 1 vaccination when experimentally challenged 1 month after the last of three oral vaccinations. Protection was correlated with a mixed Th1-Th17 response [32]. In a different study, the authors demonstrated that a different nanoparticle vaccine (Omp31-loaded N-trimethyl chitosan nanoparticles) induced Th1–Th17 immune responses in mice after three dosages delivered orally or two dosages administered ip. Lower antibody titers were observed in mice orally immunized as compared to ip [34]. When experimentally challenged with B. melitensis strain 16M at 1 month after vaccination, oral vaccinates had greater protection than intraperitoneal vaccinates but less protection than Rev 1 vaccinates. A third nanoparticle vaccine (based on poly lactic-co-glycolic acid nanoparticles 50:50 and containing oligopolysaccharide antigens) induced humoral responses in mice that increased after each inoculation. Experimental challenge with B. melitensis 2 weeks after the third inoculation demonstrated reduced splenic infection when compared to the control mice [35].
Subunit vaccines offer the advantages of better safety profiles, induction of humoral responses [38], and faster production with reduced costs [39]. Candidate subunit vaccines identified in this search included OMVs vaccines in either Poly (I:C) or 327 CpG + Montanide ISA adjuvant formulations. Humoral responses increased after two vaccine dosages with adjuvanted vaccines demonstrating the greatest responses. Spleenocytes demonstrated greater cytokine responses (IFN-γ and IL-2) in vitro after stimulation with OMV antigens [36]. Another study that used a recombinant protein-based subunit vaccine (Omp10, Omp28, L7/L12 combinations) alone or with Taishan Pinus massoniana pollen polysaccharide adjuvants (TPPPS) demonstrated increased humoral responses after inoculation, but the responses were greater in mice inoculated with a live B. melitensis M5 vaccine. Serum IL-2, IL-4, and IFN-γ were increased in the vaccinated mice. After experimental challenge at 4 weeks after vaccination, the mice inoculated with subunit vaccines containing all antigens and adjuvant had reductions in splenic infection that were similar to but less than the reductions observed in the mice inoculated with the live vaccine [37].
Unfortunately, most B. melitensis candidate vaccines have only been evaluated in murine models in which disease pathogenesis can be markedly different from what occurs in ruminant hosts. Murine models are inbred as compared to outbred domestic livestock hosts. There are significant differences in ruminant immunologic responses from those of mice, including the observation that ruminants have a high percentage of circulating T cells expressing γδ markers. Lastly, infection in mice is generally quantified by the evaluation of hepatic and splenic colonization, whereas in ruminant hosts, infection is predominantly within lymphatic tissues. These differences emphasize the need for the evaluation of brucellosis vaccine candidates in the species of interest to address research needs. In addition, some studies in murine models administer experimental challenges prior to the immune system returning to a senescent state, and therefore, colonization data might be influenced by nonspecific immune activation.
4. Discussion
Annually, 2.1 million new human cases of brucellosis occur in different parts of the world [40]. Due to its potential to be used as a bioterrorism agent, communicability, pathogenic nature for humans, and clinical effects, Brucella has been designated by the Centers for Disease Control and Prevention as a category B agent that should be manipulated under biosafety level III conditions [41]. Human brucellosis can be prevented by controlling the incidence of brucellosis in livestock using vaccination and test-and-removal strategies [42]. Concern has been raised regarding use of brucellosis as a weapon of bioterrorism in the absence of an adequate human vaccine [41].
The development of a more efficacious and safe vaccine against B. melitensis has been a long-term challenge for scientists. Many current licensed brucellosis vaccines have limitations, including virulence in humans and pregnant animals and interference with serodiagnosis [43,44]. For example, Rev. 1, the most commonly used brucellosis vaccine in small ruminants, is a live-attenuated B. melitensis strain derived from a virulent B. melitensis isolate. The Rev 1 strain became dependent on streptomycin for its growth but lost this growth requirement during subculture while remaining streptomycin resistant [45]. Vaccination with Rev 1 stimulates protective immunity in sheep and goats against B. melitensis [9] and also protects rams from B. ovis. This vaccine is attenuated compared to the field strains but retains virulence characteristics in animal and human hosts [46]. The Rev 1 vaccine can induce dose-dependent abortions in pregnant sheep and goats [46,47,48] but is considered nonpathogenic [49] or low pathogenic in rams [50]. The strain is considered smooth, meaning it expresses the O-polysaccharide on its lipopolysaccharide. The O-polysaccharide is an immunodominant humoral antigen utilized in almost all brucellosis serological tests. Limited data suggest that Rev. 1 may be efficacious in protecting cattle against B. melitensis [51,52,53]. The live B. melitensis strain 2 is used in China to prevent Brucella infections in sheep, goats, cattle, and deer [54,55]. Studies reporting direct comparisons of Rev 1 and other vaccines for immunogenicity and protection against experimental challenge with B. melitensis in natural hosts are lacking. The few reports in the literature have failed to find vaccine candidates that have improved efficacy when compared to Rev 1 [56].
Brucella DNA-based vaccines are a type of subunit vaccine, and repeated administration can induce humoral and cellular immune responses [57]. DNA vaccines are plasmids that express genes encoding specific antigens. The most common genes include L7/L12, BLS, BCSP31, SOD Cu/Zn, Omp16, periplasmic immunogenic protein (P39), and BAB1-0278. Adjuvants are not commonly used in DNA vaccines [58]. The DNA vaccine encoding BAB 1-0278 confers protection in mice against B. abortus [59]. DNA vaccines containing BAB1 0273 or BAB1 0278 and SOD C induce immune responses in mice but are less protective. DNA vaccines encoding p39 or groEL and other DNA-based vaccine candidates require multiple booster vaccinations but offer only low levels of protection. Therefore, further research in this area is needed [60]. The expression of multiple antigens (Omp16 and L7/L12) in DNA vaccines and expression of cytokines (SOD, including IL-18 or IL-12) can be used to enhance the immune response and efficacy of Brucella DNA vaccines [58].
Brucellosis is considered an intracellular pathogen that survives within phagocytes and could be resistant to the bactericidal action of antimicrobial peptides [61]. Researchers reported that the subunit vaccines evaluated were safe and efficacious against brucellosis. These vaccines can be constituted using a recombinant, highly conserved protein that is expressed across the Brucella genus. However, the subunit vaccine does not replicate or mimic a natural Brucella infection. Thus, they induce lower protective immunity as compared with live-attenuated vaccines [38]. The main challenges for designing an effective subunit vaccine against brucellosis are poor antigenicity, instability, and short half-lives for recombinant subunit antigens [62]. Thus, adjuvants are essential to induce immune responses. Enhancing immunity depends on the type of antigen and adjuvant used in Brucella subunit vaccines. Freund’s adjuvant, Alum adjuvant, and aluminum hydroxide (the only adjuvant licensed for use in human vaccines) are considered to promote Th2 immune responses, while monophosphoryl lipid A and CpG are believed to generate Th1-type responses, which are considered the type of immunity required for protection against brucellosis.
This study’s limitations include the following: (1) scope of literature review: This study exclusively incorporated published papers pertaining to B. melitensis vaccines, potentially limiting the breadth of its findings, and (2) language bias: This systematic review includes only articles published in English, which may introduce bias.
When protecting against brucellosis, an ideal vaccine should (i) provide long-term protection against abortion and infection in the majority of animals with only one dose; (ii) prevent colonization and seroconversion with efficacy even when animals are exposed to virulent field strains; (iii) be safe for animals of all ages from young to adult; (iv) not shed the vaccine after inoculation; and (v) be able to differentiate between vaccinated animals and those that are infected [63].
While some scientists argue that the available diagnostic and intervention strategies for brucellosis control are diverse and adequate, the disease’s persistent high prevalence in some countries or regions demonstrates a need for additional disease management tools. Cost-effective strategies to combat and prevent the spread of brucellosis worldwide include the use of efficacious vaccines in livestock reservoirs.
Funding
This research received no external funding.
Institutional Review Board Statement
This project was approved by Colorado State University.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
Brian McCluskey is employed by Trace First Inc. All the authors have no conflict of interest.
References
- Welburn, S.C.; Beange, I.; Ducrotoy, M.J.; Okello, A.L. The Neglected Zoonoses—The Case for Integrated Control and Advocacy. Clin. Microbiol. Infect. 2015, 21, 433–443. [Google Scholar] [CrossRef] [PubMed]
- Godfroid, J.; DeBolle, X.; Roop, R.M.; O’Callaghan, D.; Tsolis, R.M.; Baldwin, C.; Santos, R.L.; McGiven, J.; Olsen, S.; Nymo, I.H.; et al. The quest for a true One Health perspective of brucellosis. Rev. Sci. Tech. 2014, 33, 521–538. [Google Scholar] [CrossRef] [PubMed]
- Muendo, E.N.; Mbatha, P.M.; Macharia, J.; Abdoel, T.H.; Janszen, P.V.; Pastoor, R.; Smits, H.L. Infection of cattle in Kenya with Brucella abortus biovar 3 and Brucella melitensis biovar 1 genotypes. Trop. Anim. Health Prod. 2012, 44, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Gwida, M.; El-Gohary, A.; Melzer, F.; Khan, I.; Rösler, U.; Neubauer, H. Brucellosis in camels. Res. Vet. Sci. 2012, 92, 351–355. [Google Scholar] [CrossRef]
- Mick, V.; Carrou, G.L.; Corde, Y.; Game, Y.; Jay, M.; Garin-Bastuji, B. Brucella melitensis in France: Persistence in wildlife and probable spillover from alpine ibex to domestic animals. PLoS ONE 2014, 9, e94168. [Google Scholar] [CrossRef]
- Nicoletti, P. Vaccination. In Animal Brucellosis; Nielsen, K., Duncan, J.R., Eds.; CRC Press: Boca Raton, FL, USA, 1990; pp. 284–299. [Google Scholar]
- Roux, J. Brucella vaccines in humans. In Brucellosis; Madkour, M.M., Ed.; Butterworths: London, UK, 1989; pp. 244–249. [Google Scholar]
- Plommet, M.; Renoux, G.; Philppon, A.; Lorentz, C.; Gestin, J. Experimental brucellosis, Comparison of vaccine efficacy B19 and H38 vaccine. Ann. Vet. Res. 1970, 1, 189–201. [Google Scholar]
- Elberg, S.S.; Faunce, K., Jr. Immunization against Brucella infection. VI. Immunity conferred on goats by a nondependent mutant from a streptomycin-dependent mutant strain of Brucella melitensis. J. Bacteriol. 1957, 73, 211–217. [Google Scholar] [CrossRef]
- Banai, M. Control of small ruminant brucellosis by use of Brucella melitensis Rev.1 vaccine: Laboratory aspects and field observations. Vet. Microbiol. 2002, 90, 497–519. [Google Scholar] [CrossRef]
- Alton, G.G. Vaccination of goats with reduced doses of Rev.1 Brucella melitensis vaccine. Res. Vet. Sci. 1970, 2, 54–59. [Google Scholar] [CrossRef]
- Blasco, J.M.; Molina-Flores, B. Control and eradication of Brucella melitensis infection in sheep and goats. Vet. Clin. N. Am. Food Anim. Pract. 2011, 27, 95–104. [Google Scholar] [CrossRef]
- Blasco, J.M. A review of the use of B. melitensis Rev.1 vaccine in adult sheep and goats. Prev. Vet. Med. 1997, 31, 275–283. [Google Scholar] [CrossRef]
- Vershilova, P. The use of live vaccine for vaccination of human beings against brucellosis in the USSR. Bull. World Health Organ. 1961, 24, 85. [Google Scholar]
- Pappas, G. The changing Brucella ecology: Novel reservoirs, new threats. Int. J. Antimicrob. Agents 2010, 36, S8–S11. [Google Scholar] [CrossRef] [PubMed]
- FAO/WHO/OIE. Round Table on the Use of Rev.1 Vaccine in Small Ruminants and Cattle; Garin-Bastuji, B., Benkirane, A., Eds.; CNEVA: Paris, France, 1995. [Google Scholar]
- Pasquevich, K.A.; Estein, S.M.; Samartino, C.G.; Zwerdling, A.; Coria, L.M.; Barrionuevo, P.; Fossati, C.; Giambartolomei, G.; Cassataro, J. Immunization with recombinant Brucella species outer membrane protein Omp16 or Omp19 in adjuvant induces specific CD4+ and CD8+ T cells as well as systemic and oral protection against Brucella abortus infection. Infect. Immun. 2009, 77, 436–445. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Institute, J. The Joanna Briggs Institute Critical Appraisal Tools for Use in JBI Systematic Reviews Checklist for Analytical Cross-Sectional Studies; The Joanna Briggs Institute: Adelaide, Australia, 2017. [Google Scholar]
- Zhang, J.; Guo, F.; Chen, C.; Li, Z.; Zhang, H.; Wang, Y.; Zhang, K.; Du, G.; Li, Y.; Wang, J.; et al. Brucella melitensis 16 M Δhfq attenuation confers protection against wild-type challenge in BALB/c mice. Microbiol. Immunol. 2013, 57, 502–510. [Google Scholar] [CrossRef]
- Li, Z.; Zhang, J.; Zhang, K.; Fu, Q.; Wang, Z.; Li, T.; Zhang, H.; Guo, F.; Chen, C. Brucella melitensis 16MΔTcfSR as a potential live vaccine allows for the differentiation between natural and vaccinated infection. Exp. Ther. Med. 2015, 10, 1182–1188. [Google Scholar] [CrossRef]
- Zhang, J.; Yin, S.; Yi, D.; Zhang, H.; Li, Z.; Guo, F.; Chen, C.; Fang, W.; Wang, J. The Brucella melitensis M5-90ΔmanB live vaccine candidate is safer than M5-90 and confers protection against wild-type challenge in BALB/c mice. Microb. Pathog. 2017, 112, 148–155. [Google Scholar] [CrossRef]
- Verdiguel-Fernández, L.; Oropeza-Navarro, R.; Ortiz, A.; Robles-Pesina, M.; Ramírez-Lezama, J.; Castañeda-Ramírez, A.; Verdugo-Rodríguez, A. Brucella melitensis omp31 mutant is attenuated and confers protection against virulent Brucella melitensis challenge in BALB/c mice. J. Microbiol. Biotechnol. 2020, 30, 497–504. [Google Scholar] [CrossRef]
- Li, Z.; Wang, S.; Zhang, H.; Xi, L.; Zhang, J.; Zhang, X.; Zhou, Q.; Yi, J.; Li, M.; Zhang, W.; et al. Development and evaluation of in murine model, of an improved live-vaccine candidate against brucellosis from to Brucella melitensis vjbR deletion mutant. Microb. Pathog. 2018, 124, 250–257. [Google Scholar] [CrossRef]
- Arenas-Gamboa, A.; Rice-Ficht, A.; Kahl-McDonagh, M.; Ficht, T. Protective efficacy and safety of Brucella melitensis 16MΔmucR against intraperitoneal and aerosol challenge in BALB/c mice. Infect. Immun. 2011, 79, 3653–3658. [Google Scholar] [CrossRef]
- Clapp, B.; Skyberg, J.A.; Yang, X.; Thornburg, T.; Walters, N.; Pascual, D.W. Protective live oral brucellosis vaccines stimulate Th1 and Th17 cell responses. Infect. Immun. 2011, 79, 4165–4174. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Li, T.; Zhang, J.; Li, Z.; Zhang, Y.; Wang, Z.; Feng, H.; Wang, Y.; Chen, C.; Zhang, H. The Brucella melitensis M5-90 phosphoglucomutase (PGM) mutant is attenuated and confers protection against wild-type challenge in BALB/c mice. World J. Microbiol. Biotechnol. 2016, 32, 58. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.-Q.; Shi, J.-X.; Fu, W.-D.; Zhang, Y.; Zhang, J.; Wang, Z.; Li, T.; Chen, C.; Guo, F.; Zhang, H. A Brucella melitensis M5-90 wboA deletion strain is attenuated and enhances vaccine efficacy. Mol. Immunol. 2015, 66, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Metwally, S.; Viljoen, G.; Idrissi, A. Veterinary Vaccines: Principles and Applications; John Wiley & Sons: Hoboken, NJ, USA, 2021; p. 298. [Google Scholar]
- Shojaei, M.; Tahmoorespur, M.; Soltani, M.; Sekhavati, M.H. Immunogenicity evaluation of plasmids encoding Brucella melitensis Omp25 and Omp31 antigens in BALB/c mice. Iran. J. Basic Med. Sci. 2018, 21, 957. [Google Scholar] [CrossRef]
- Karevan, G.; Ahmadi, K.; Taheri, R.A.; Fasihi-Ramandi, M. Immunogenicity of glycine nanoparticles containing a chimeric antigen as Brucella vaccine candidate. Clin. Exp. Vaccine Res. 2021, 10, 35. [Google Scholar] [CrossRef] [PubMed]
- Abkar, M.; Fasihi-Ramandi, M.; Kooshki, H.; Lotfi, A.S. Intraperitoneal immunization with Urease loaded N-trimethyl Chitosan nanoparticles elicits high protection against Brucella melitensis and Brucella abortus infections. Immunol. Lett. 2018, 199, 53–60. [Google Scholar] [CrossRef]
- Sadeghi, Z.; Fasihi-Ramandi, M.; Azizi, M.; Bouzari, S. Mannosylated chitosan nanoparticles loaded with FliC antigen as a novel vaccine candidate against Brucella melitensis and Brucella abortus infection. J. Biotechnol. 2020, 310, 89–96. [Google Scholar] [CrossRef]
- Abkar, M.; Fasihi-Ramandi, M.; Kooshki, H.; Lotfi, A.S. Oral immunization of mice with Omp31-loaded N-trimethyl chitosan nanoparticles induces high protection against Brucella melitensis infection. Int. J. Nanomed. 2017, 12, 8769. [Google Scholar] [CrossRef]
- Maleki, M.; Salouti, M.; Shafiee Ardestani, M.; Talebzadeh, A. Preparation of a nanovaccine against Brucella melitensis M16 based on PLGA nanoparticles and oligopolysaccharide antigen. Artif. Cells Nanomed. Biotechnol. 2019, 47, 4248–4256. [Google Scholar] [CrossRef]
- Golshani, M.; Amani, M.; Amirzadeh, F.; Nazeri, E.; Siadat, S.D.; Nejati-Moheimani, M.; Arsang, A.; Bouzari, S. Evaluation of Poly (I: C) and combination of CpG ODN plus Montanide ISA adjuvants to enhance the efficacy of outer membrane vesicles as an acellular vaccine against Brucella melitensis infection in mice. Int. Immunopharmacol. 2020, 84, 106573. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Wang, Q.; Wang, Y.; Xu, Y.; Peng, D.; Huang, H.; Hu, L.; Wei, K.; Zhu, R. Comparison of immune effects between Brucella recombinant Omp10-Omp28-L7/L1 proteins expressed in eukaryotic and prokaryotic systems. Front. Vet. Sci. 2020, 7, 576. [Google Scholar] [CrossRef] [PubMed]
- Ficht, T.A.; Kahl-McDonagh, M.M.; Arenas-Gamboa, A.M.; Rice-Ficht, A.C. Brucellosis: The case for live, attenuated vaccines. Vaccine 2009, 27, D40–D43. [Google Scholar] [CrossRef]
- Fu, S.; Xu, J.; Li, X.; Xie, Y.; Qiu, Y.; Du, X.; Yu, S.; Bai, Y.; Chen, Y.; Wang, T.; et al. Immunization of mice with recombinant protein CobB or AsnC confers protection against Brucella abortus infection. PLoS ONE 2012, 7, e29552. [Google Scholar] [CrossRef] [PubMed]
- Laine, C.G.; Johnson, V.E.; Scott, H.; Arenas-Gamboa, A.M. Global Estimate of Human Brucellosis Incidence. Emerg. Infect. Dis. 2023, 29, 1789–1797. [Google Scholar] [CrossRef]
- Franco, M.; Mulder, M.; Gilman, R.; Smits, H. Human brucellosis. Lancet Infect. Dis. 2007, 7, 775–786. [Google Scholar] [CrossRef]
- Jacob, J.M.; Curtiss, R. Characterization of Brucella abortus S19 as a challenge strain for use in a mouse model of brucellosis. Microbes Infect. 2021, 23, 104809. [Google Scholar] [CrossRef]
- Mantur, B.G.; Amarnath, S.K.; Shinde, R.S. Review of clinical and labora-tory features of human Brucellosis. Indian J. Med. Microbiol. 2007, 25, 188–202. [Google Scholar] [CrossRef]
- Shford, D.A.; di Pietra, J.; Lingappa, J.; Woods, C.; Noll, H.; Neville, B.; Weyant, R.; Bragg, S.L.; Spiegel, R.A.; Tappero, J.; et al. Adverse events in humans associated with accidentalexposure to the livestock brucellosis vaccine RB51. Vaccine 2004, 22, 3435–3439. [Google Scholar] [CrossRef]
- Schurig, G.G.; Sriranganathan, N.; Corbel, M.J. Brucellosisvaccines: Past, present and future. Vet. Microbiol. 2002, 90, 479–496. [Google Scholar] [CrossRef]
- Alton, G.G. Rev.1 and H38 Brucella melitensis vaccines. In Brucella Melitensis; Verger, J.M., Plommet, M., Eds.; Martinus Nijhoff: Dordrecht, The Netherlands, 1985; pp. 215–227. [Google Scholar]
- Alton, G.G.; Jones, L.M.; Pietz, D.E. Laboratory techniques in brucellosis. In World Health Organisation Technical Monograph; Series No. 55; WHO: Geneva, Switzerland, 1975. [Google Scholar]
- Blasco, J.M.; Marin, C.M.; Barberan, M.; Moriyon, I.; Diaz, R. Immunization with Brucella melitensis Rev.1 against Brucella ovis infection of rams. Vet. Microbiol. 1987, 14, 381–392. [Google Scholar] [CrossRef]
- Bardenstein, S.; Mandelboim, M.; Ficht, T.A.; Baum, M.; Banai, M. Identification of the Brucella melitensis vaccine strain Rev.1 in animals and humans in Israel by PCR analysis of the PstI site polymorphism of its omp2 gene. J. Clin. Microbiol. 2002, 40, 1475–1480. [Google Scholar] [CrossRef]
- Lantier, F.; Fensterbank, R. Kinetics of Rev.1 infection in sheep. In Brucella melitensis; Plommet, M., Verger, J.M., Eds.; Martinus Niijhoff: Dordrecht, The Netherlands, 1985; pp. 247–251. [Google Scholar]
- Van Drimmelen, C.; Horwell, F.D. Preliminary findings with the use of Brucella melitensis Rev.1 as a vaccine against brucellosis in cattle. Bull. Off. Int. Epiz. 1964, 62, 987. [Google Scholar]
- Horwell, F.D.; van Drimmelen, G.G. Brucella melitensis strain Rev.1 as a vaccine in cattle. S. Afr. Vet. Med. Assoc. 1971, 42, 233–235. [Google Scholar]
- Garcia-Carrillo, C. Comparison of Brucella melitensis Rev.1 and B. abortus strain 19 as a vaccine against brucellosis in cattle. Zentralbl. Veterinaermed. 1980, 27, 131–138. [Google Scholar] [CrossRef]
- Erasmus, J.A.; Bergh, E.C. Ovine brucellosis: Repeated vaccination with Rev.1 vaccine and the prevalence of the disease in the Winburg district. J. S. Afr. Vet. Assoc. 1985, 56, 205–208. [Google Scholar]
- Xie, X. Orally administrable brucellosis vaccine: Brucella suis strain 2 vaccine. Vaccine 1986, 4, 212–216. [Google Scholar]
- Lu, S.-L.; Zhang, J.-L. Brucellosis in China. In Brucellosis: Clinical and Laboratory Aspects; Young, E.J., Corbel, M.J., Eds.; CRC Press: Boca Raton, FL, USA, 1989; Chapter 13; pp. 173–180. [Google Scholar]
- Verger, J.M.; Grayon, M.; Zundel, E.; Lechopier, P.; Olivier-Bernardin, V. Comparison of the efficacy of Brucella suis strain 2 and Brucella melitensis Rev.1 live vaccines against a Brucella melitensis experimental infection in pregnant ewes. Vaccine 1995, 13, 7625115. [Google Scholar] [CrossRef] [PubMed]
- Gheibi, A.; Khanahmad, H.; Kashfi, K.; Sarmadi, M.; Khorramizadeh, M.R. Development of new generation of vaccines for Brucella abortus. Heliyon 2018, 4, e01079. [Google Scholar] [CrossRef] [PubMed]
- Hou, H.; Liu, X.; Peng, Q. The advances in brucellosis vaccines. Vaccine 2019, 37, 3981–3988. [Google Scholar] [CrossRef]
- Gomez, L.; Llanos, J.; Escalona, E.; Saez, D.; Alvarez, F.; Molina, R.; Flores, M.; Onate, A. Multivalent Fusion DNA Vaccine against Brucella abortus. BioMed Res. Int. 2017, 2017, 6535479. [Google Scholar] [CrossRef]
- Moreno, E.; Barquero-Calvo, E. The role of neutrophils in brucellosis. Microbiol. Mol. Biol. Rev. 2020, 84, e00048-e20. [Google Scholar] [CrossRef] [PubMed]
- Singha, H.; Mallick, A.I.; Jana, C.; Fatima, N.; Owais, M.; Chaudhuri, P. Co-immunization with interlukin-18 enhances the protective efficacy of liposomes encapsulated recombinant Cu–Zn superoxide dismutase protein against Brucella abortus. Vaccine 2011, 29, 4720–4727. [Google Scholar] [CrossRef] [PubMed]
- Olsen, S.C. Recent developments in livestock and wildlife brucellosis vaccination. Rev. Sci. Tech. 2013, 32, 207–217. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).