Reference Intervals for Platelet Counts in the Elderly: Results from the Prospective SENIORLAB Study
Abstract
:1. Introduction
2. Materials and Methods
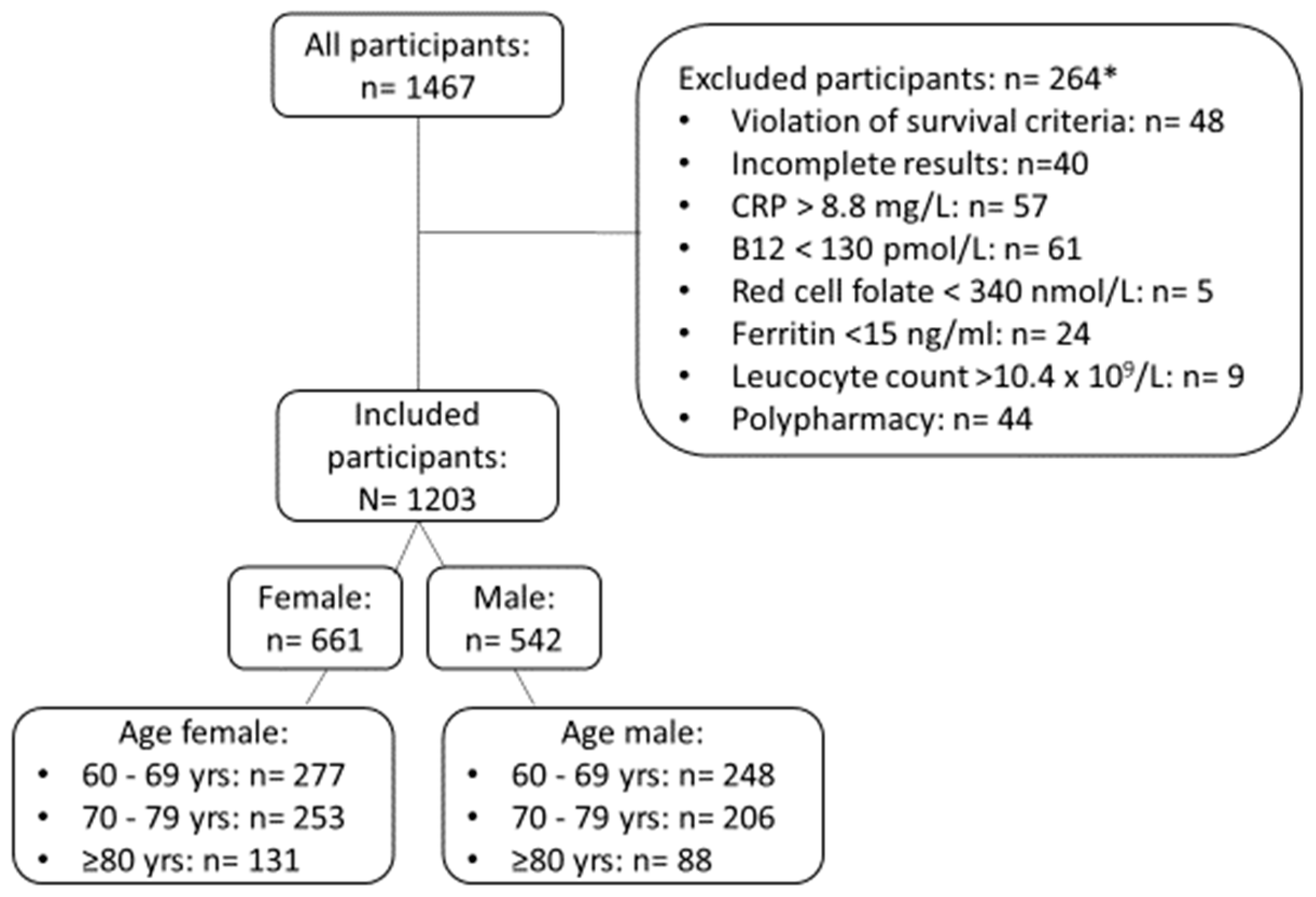
2.1. Study Participants and Patient Cohorts
2.2. Laboratory Methods
2.3. Statistical Methods
3. Results
3.1. Direct Evaluation of Reference Intervals
3.2. Validating the Reference Intervals with Indirect Methods
3.3. Impact of Novel Reference Intervals on Frequency of Abnormal Platelet Counts
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gremmel, T.; Frelinger, A.L., 3rd; Michelson, A.D. Platelet Physiology. Semin. Thromb. Hemost. 2016, 42, 191–204. [Google Scholar]
- Preston, R.J.S.; Lisman, T. Extrahemostatic Functions of Platelets and Coagulation Factors. Semin. Thromb. Hemost. 2018, 44, 89–90. [Google Scholar]
- Wille, K.; Sadjadian, P.; Griesshammer, M. Thrombocytosis and thrombocytopenia-background and clinical relevance. Dtsch. Med. Wochenschr. 2017, 142, 1732–1743. [Google Scholar]
- Smock, K.J.; Perkins, S.L. Thrombocytopenia: An update. Int. J. Lab. Hematol. 2014, 36, 269–278. [Google Scholar] [CrossRef]
- Appleby, N.; Angelov, D. Clinical and laboratory assessment of a patient with thrombocytosis. Br. J. Hosp. Med. 2017, 78, 558–564. [Google Scholar] [CrossRef]
- Harker, L.A. Platelet production. N. Engl. J. Med. 1970, 282, 492–494. [Google Scholar] [CrossRef]
- Reese, J.A.; Peck, J.D.; Deschamps, D.R.; McIntosh, J.J.; Knudtson, E.J.; Terrell, D.R.; Vesely, S.K.; George, J.N. Platelet Counts during Pregnancy. N. Engl. J. Med. 2018, 379, 32–43. [Google Scholar] [CrossRef]
- Ankus, E.; Price, S.J.; Ukoumunne, O.C.; Hamilton, W.; Bailey, S.E.R. Cancer incidence in patients with a high normal platelet count: A cohort study using primary care data. Fam. Pract. 2018, 35, 671–675. [Google Scholar] [CrossRef] [Green Version]
- Wallace, K.; Li, H.; Brazeal, J.G.; Lewin, D.N.; Sun, S.; Ba, A.; Paulos, C.M.; Rachidi, S.; Li, Z.; Alekseyenko, A.V. Platelet and hemoglobin count at diagnosis are associated with survival in African American and Caucasian patients with colorectal cancer. Cancer Epidemiol. 2020, 67, 101746. [Google Scholar] [CrossRef]
- Serefhanoglu, K.; Kaya, E.; Sevinc, A.; Aydogdu, I.; Kuku, I.; Ersoy, Y. Isolated thrombocytopenia: The presenting finding of typhoid fever. Clin. Lab. Haematol. 2003, 25, 63–65. [Google Scholar] [CrossRef]
- Bogaart, L.V.D.; Ranzani, A.; Oreni, L.; Giacomelli, A.; Corbellino, M.; Rusconi, S.; Galli, M.; Antinori, S.; Ridolfo, A.L. Overlooked cases of HIV infection: An Italian tale of missed diagnostic opportunities. Eur. J. Intern. Med. 2020, 73, 30–35. [Google Scholar] [CrossRef]
- Uhl, L.; Assmann, S.F.; Hamza, T.H.; Harrison, R.W.; Gernsheimer, T.; Slichter, S.J. Laboratory predictors of bleeding and the effect of platelet and RBC transfusions on bleeding outcomes in the PLADO trial. Blood 2017, 130, 1247–1258. [Google Scholar] [CrossRef] [Green Version]
- Neunert, C.; Lim, W.; Crowther, M.; Cohen, A.; Solberg, L.A. The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopenia. Blood 2011, 117, 4190–4207. [Google Scholar] [CrossRef] [Green Version]
- Neunert, C.; Terrell, D.R.; Arnold, D.M.; Buchanan, G.; Cines, D.B.; Cooper, N.; Cuker, A.; Despotovic, J.M.; George, J.N.; Grace, R.F.; et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019, 3, 3829–3866. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ittermann, T.; Feig, M.A.; Petersmann, A.; Radke, D.; Greinacher, A.; Völzke, H.; Thiele, T. Mean platelet volume is more important than age for defining reference intervals of platelet counts. PLoS ONE 2019, 14, e0213658. [Google Scholar] [CrossRef] [Green Version]
- Cheng, C.K.-W.; Chan, J.; Cembrowski, G.S.; Van Assendelft, O.W. Complete blood count reference interval diagrams derived from NHANES III: Stratification by age, sex, and race. Lab. Hematol. 2004, 10, 42–53. [Google Scholar] [CrossRef] [Green Version]
- Helmersson-Karlqvist, J.; Ridefelt, P.; Lind, L.; Larsson, A. Reference values for 34 frequently used laboratory tests in 80-year-old men and women. Maturitas 2016, 92, 97–101. [Google Scholar] [CrossRef]
- Park, S.H.; Park, C.-J.; Lee, B.-R.; Kim, M.-J.; Han, M.-Y.; Cho, Y.-U.; Jang, S. Establishment of Age- and Gender-Specific Reference Ranges for 36 Routine and 57 Cell Population Data Items in a New Automated Blood Cell Analyzer, Sysmex XN-2000. Ann. Lab. Med. 2016, 36, 244–249. [Google Scholar] [CrossRef]
- Troussard, X.; Vol, S.; Cornet, E.; Bardet, V.; Couaillac, J.-P.; Fossat, C.; Luce, J.-C.; Maldonado, E.; Siguret, V.; Tichet, J.; et al. Full blood count normal reference values for adults in France. J. Clin. Pathol. 2014, 67, 341–344. [Google Scholar] [CrossRef] [Green Version]
- Adeli, K.; Raizman, J.E.; Chen, Y.; Higgins, V.; Nieuwesteeg, M.; Abdelhaleem, M.; Wong, S.L.; Blais, D. Complex biological profile of hematologic markers across pediatric, adult, and geriatric ages: Establishment of robust pediatric and adult reference intervals on the basis of the Canadian Health Measures Survey. Clin. Chem. 2015, 61, 1075–1086. [Google Scholar] [CrossRef] [Green Version]
- Kratz, A.; Ferraro, M.; Sluss, P.M.; Lewandrowski, K.B. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Laboratory reference values. N. Engl. J. Med. 2004, 351, 1548–1563. [Google Scholar] [CrossRef] [PubMed]
- Baccini, V.; Genevieve, F.; Jacqmin, H.; Chatelain, B.; Girard, S.; Wuilleme, S.; Vedrenne, A.; Guiheneuf, E.; Toussaint-Hacquard, M.; Everaere, F.; et al. Platelet Counting: Ugly Traps and Good Advice. Proposals from the French-Speaking Cellular Hematology Group (GFHC). J. Clin. Med. 2020, 9, 908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janu, M.R.; Creasey, H.; Grayson, D.A.; Cullen, J.S.; Whyte, S.; Brooks, W.S.; Waite, L.M.; Broe, G.A. Laboratory results in the elderly: The Sydney Older Persons Study. Ann. Clin. Biochem. 2003, 40, 274–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jernigan, J.A.; Gudat, J.C.; Blake, J.L.; Bowen, L.; Lezotte, D.C. Reference values for blood findings in relatively fit elderly persons. J. Am. Geriatr. Soc. 1980, 28, 308–314. [Google Scholar] [CrossRef]
- Zaninetti, C.; Biino, G.; Noris, P.; Melazzini, F.; Civaschi, E.; Balduini, C.L. Personalized reference intervals for platelet count reduce the number of subjects with unexplained thrombocytopenia. Haematologica 2015, 100, e338–e340. [Google Scholar] [CrossRef]
- Sloan, A.W. The Normal Platelet Count in Man. J. Clin. Pathol. 1951, 4, 37–46. [Google Scholar] [CrossRef] [Green Version]
- Risch, M.; Nydegger, U.; Risch, L. SENIORLAB: A prospective observational study investigating laboratory parameters and their reference intervals in the elderly. Medicine 2017, 96, e5726. [Google Scholar] [CrossRef]
- CLSI. Defining, Establishing and Verifying Reference Intervals in the Clinical Laboratory; Approved Guideline; Third Edition CLSI Document EP28-A3c; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2008. [Google Scholar]
- WHO; WHO/UNICEF/UNU. Iron Deficiency Anaemia: Assessment, Prevention, and Control; WHO: Geneva, Switzerlan, 2001. [Google Scholar]
- Aparicio-Ugarriza, R.; Palacios, G.; Alder, M.; González-Gross, M. A review of the cut-off points for the diagnosis of vitamin B12 deficiency in the general population. Clin. Chem. Lab. Med. 2015, 53, 1149–1159. [Google Scholar] [CrossRef]
- de Benoist, B. Conclusions of a WHO Technical Consultation on folate and vitamin B12 deficiencies. Food Nutr. Bull. 2008, 29, S238–S244. [Google Scholar] [CrossRef]
- Arzideh, F.; Wosniok, W.; Haeckel, R. Reference limits of plasma and serum creatinine concentrations from intra-laboratory data bases of several German and Italian medical centres: Comparison between direct and indirect procedures. Clin. Chim. Acta 2010, 411, 215–221. [Google Scholar] [CrossRef]
- Nutritional Anaemias. Report of a WHO scientific group. World Health Organ. Tech. Rep. Ser. 1968, 405, 5–37. [Google Scholar]
- Risch, L.; Saely, C.H.; Neyer, U.; Hoefle, G.; Gouya, G.; Zerlauth, M.; Risch, G.M.; Risch, M.; Drexel, H. Prevalence of decreased glomerular filtration rate in patients seeking non-nephrological medical care—An evaluation using IDMS-traceable creatinine based MDRD as well as Mayo Clinic quadratic equation estimates. Clin. Chim. Acta 2007, 378, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Amt, für, Statistik. Statistisches Jahrbuch Liechtensteins 2017; Regierung des Fürstentum Liechenstein: Vaduz, Liechtenstein, 2017.
- Bossard, M.; Pumpol, K.; van der Lely, S.; Aeschbacher, S.; Schoen, T.; Krisai, P.; Lam, T.; Todd, J.; Estis, J.; Risch, M.; et al. Plasma endothelin-1 and cardiovascular risk among young and healthy adults. Atherosclerosis 2015, 239, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Altman, D.G. Construction of age-related reference centiles using absolute residuals. Stat. Med. 1993, 12, 917–924. [Google Scholar] [CrossRef] [PubMed]
- Arzideh, F.; Wosniok, W.; Gurr, E.; Hinsch, W.; Schumann, G.; Weinstock, N.; Haeckel, R. A plea for intra-laboratory reference limits. Part 2. A bimodal retrospective concept for determining reference limits from intra-laboratory databases demonstrated by catalytic activity concentrations of enzymes. Clin. Chem. Lab. Med. 2007, 45, 1043–1057. [Google Scholar] [CrossRef]
- Haeckel, R.; Wosniok, W.; Arzideh, F. A plea for intra-laboratory reference limits. Part 1. General considerations and concepts for determination. Clin. Chem. Lab. Med. 2007, 45, 1033–1042. [Google Scholar] [CrossRef]
- Haeckel, R.; Wosniok, W.; Arzideh, F. Proposed classification of various limit values (guide values) used in assisting the interpretation of quantitative laboratory test results. Clin. Chem. Lab. Med. 2009, 47, 494–497. [Google Scholar] [CrossRef]
- Arzideh, F.; Brandhorst, G.; Gurr, E.; Hinsch, W.; Hoff, T.; Roggenbuck, L.; Rothe, G.; Schumann, G.; Wolters, B.; Wosniok, W.; et al. An improved indirect approach for determining reference limits from intra-laboratory data bases exemplified by concentrations of electrolytes. J. Lab. Med. 2009, 33, 52–66. [Google Scholar]
- Zierk, J.; Arzideh, F.; Haeckel, R.; Rascher, W.; Rauh, M.; Metzler, M. Indirect determination of pediatric blood count reference intervals. Clin. Chem. Lab. Med. 2013, 51, 863–872. [Google Scholar] [CrossRef] [Green Version]
- Zierk, J.; Arzideh, F.; Rechenauer, T.; Haeckel, R.; Rascher, W.; Metzler, M.; Rauh, M. Age- and sex-specific dynamics in 22 hematologic and biochemical analytes from birth to adolescence. Clin. Chem. 2015, 61, 964–973. [Google Scholar] [CrossRef]
- Arzideh, F.; Wosniok, W.; Haeckel, R. Indirect reference intervals of plasma and serum thyrotropin (TSH) concentrations from intra-laboratory data bases from several German and Italian medical centres. Clin. Chem. Lab. Med. 2011, 49, 659–664. [Google Scholar] [CrossRef] [PubMed]
- Zierk, J.; Arzideh, F.; Haeckel, R.; Rauh, M.; Metzler, M.; Ganslandt, T.; Krause, S.W. Indirect determination of hematology reference intervals in adult patients on Beckman Coulter UniCell DxH 800 and Abbott CELL-DYN Sapphire devices. Clin. Chem. Lab. Med. 2019, 57, 730–739. [Google Scholar] [CrossRef] [PubMed]
- Zierk, J.; Hirschmann, J.; Toddenroth, D.; Arzideh, F.; Haeckel, R.; Bertram, A.; Cario, H.; Frühwald, M.C.; Groß, H.-J.; Groening, A.; et al. Next-generation reference intervals for pediatric hematology. Clin. Chem. Lab. Med. 2019, 57, 1595–1607. [Google Scholar] [CrossRef] [PubMed]
- Kaushansky, K.; Lichtman, M.A.; Prchal, J.T.; Levi, M.M.; Press, O.W.; Burns, L.J.; Caligiuri, M. Williams Hematology, 9th ed.; McGraw-Hill Education: New York, NY, USA, 2016. [Google Scholar]
- Nordin, G.; Martensson, A.; Swolin, B.; Sandberg, S.; Christensen, N.J.; Thorsteinsson, V.; Franzson, L.; Kairisto, V.; Savolainen, E. A multicentre study of reference intervals for haemoglobin, basic blood cell counts and erythrocyte indices in the adult population of the Nordic countries. Scand. J. Clin. Lab. Investig. 2004, 64, 385–398. [Google Scholar] [CrossRef] [PubMed]
- Biino, G.; Santimone, I.; Minelli, C.; Sorice, R.; Frongia, B.; Traglia, M.; Ulivi, S.; Di Castelnuovo, A.; Gögele, M.; Nutile, T.; et al. Age- and sex-related variations in platelet count in Italy: A proposal of reference ranges based on 40987 subjects’ data. PLoS ONE 2013, 8, e54289. [Google Scholar] [CrossRef] [Green Version]
- Giacomini, A.; Legovini, P.; Gessoni, G.; Antico, F.; Valverde, S.; Salvadego, M.; Manoni, F. Platelet count and parameters determined by the Bayer ADVIATM 120 in reference subjects and patients. Clin. Lab. Haematol. 2001, 23, 181–186. [Google Scholar] [CrossRef]
- Nah, E.-H.; Kim, S.; Cho, S.; Cho, H.-I. Complete Blood Count Reference Intervals and Patterns of Changes Across Pediatric, Adult, and Geriatric Ages in Korea. Ann. Lab. Med. 2018, 38, 503–511. [Google Scholar] [CrossRef]
- Walz, B.; Fierz, W. The concept of reference change values (RCV). Will it supersede reference intervals? Ther. Umsch. 2015, 72, 130–135. [Google Scholar] [CrossRef]
- Pineda-Tenor, D.; Laserna-Mendieta, E.J.; Timón-Zapata, J.; Rodelgo-Jiménez, L.; Ramos-Corral, R.; Recio-Montealegre, A.; Reus, M.G.-S. Biological variation and reference change values of common clinical chemistry and haematologic laboratory analytes in the elderly population. Clin. Chem. Lab. Med. 2013, 51, 851–862. [Google Scholar] [CrossRef]
- Petersen, P.H.; Fraser, C.G.; Sandberg, S.; Goldschmidt, H. The index of individuality is often a misinterpreted quantity characteristic. Clin. Chem. Lab. Med. 1999, 37, 655–661. [Google Scholar]
- Giles, C. The platelet count and mean platelet volume. Br. J. Haematol. 1981, 48, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Huber, K.R.; Mostafaie, N.; Stangl, G.; Worofka, B.; Kittl, E.; Hofmann, J.; Hejtman, M.; Michael, R.; Weissgram, S.; Leitha, T.; et al. Clinical chemistry reference values for 75-year-old apparently healthy persons. Clin. Chem. Lab. Med. 2006, 44, 1355–1360. [Google Scholar] [CrossRef] [PubMed]
- Tsang, C.W.; Lazarus, R.; Smith, W.; Mitchell, P.; Koutts, J.; Burnett, L. Hematological indices in an older population sample: Derivation of healthy reference values. Clin. Chem. 1998, 44, 96–101. [Google Scholar] [PubMed]
- Greer, J.P.; Arber, D.A.; Glader, B.E.; List, A.F.; Means, R.M.; Rodgers, G.M. Wintrobe’s Clinical Hematology, 14th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2019. [Google Scholar]
- Biino, G.; Balduini, C.L.; Casula, L.; Cavallo, P.; Vaccargiu, S.; Parracciani, D.; Serra, D.; Portas, L.; Murgia, F.; Pirastu, M. Analysis of 12,517 inhabitants of a Sardinian geographic isolate reveals that predispositions to thrombocytopenia and thrombocytosis are inherited traits. Haematologica 2011, 96, 96–101. [Google Scholar] [CrossRef]
- Daly, M.E. Determinants of platelet count in humans. Haematologica 2011, 96, 10–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaushansky, K. Determinants of platelet number and regulation of thrombopoiesis. Hematol. Am. Soc. Hematol. Educ. Program 2009, 2009, 147–152. [Google Scholar] [CrossRef] [Green Version]
- Izzi, B.; Bonaccio, M.; De Gaetano, G.; Cerletti, C. Learning by counting blood platelets in population studies: Survey and perspective a long way after Bizzozero. J. Thromb. Haemost. 2018, 16, 1711–1721. [Google Scholar] [CrossRef] [Green Version]
- Bain, B.J. Ethnic and sex differences in the total and differential white cell count and platelet count. J. Clin. Pathol. 1996, 49, 664–666. [Google Scholar] [CrossRef]
- Biino, G.; Gasparini, P.; D’Adamo, P.; Ciullo, M.; Nutile, T.; Toniolo, D.; Sala, C.; Minelli, C.; Gögele, M.; Balduini, C.L. Influence of age, sex and ethnicity on platelet count in five Italian geographic isolates: Mild thrombocytopenia may be physiological. Br. J. Haematol. 2012, 157, 384–387. [Google Scholar] [CrossRef]
- Santimone, I.; Di Castelnuovo, A.; De Curtis, A.; Spinelli, M.; Cugino, D.; Gianfagna, F.; Zito, F.; Donati, M.; Cerletti, C.; De Gaetano, G.; et al. White blood cell count, sex and age are major determinants of heterogeneity of platelet indices in an adult general population: Results from the MOLI-SANI project. Haematologica 2011, 96, 1180–1188. [Google Scholar] [CrossRef] [Green Version]
- Naugler, C.; Ma, I. More than half of abnormal results from laboratory tests ordered by family physicians could be false-positive. Can. Fam. Physician 2018, 64, 202–203. [Google Scholar] [PubMed]
- White, G.H. Trusting numbers: Uncertainty and the pathology laboratory. Med. J. Aust. 2002, 177, 153–155. [Google Scholar] [CrossRef] [PubMed]
- Jackson, B.R. The dangers of false-positive and false-negative test results: False-positive results as a function of pretest probability. Clin. Lab. Med. 2008, 28, 305–319. [Google Scholar] [CrossRef] [PubMed]
- Baltes, P.B.; Smith, J. New frontiers in the future of aging: From successful aging of the young old to the dilemmas of the fourth age. Gerontology 2003, 49, 123–135. [Google Scholar] [CrossRef]


| Characteristic | Females (n = 661) | Males (n = 542) |
|---|---|---|
| Age, years | 72 (66, 78) | 70 (65, 76) |
| Body mass index, kg/m2 | 24.5 (22.1, 27) | 25.4 (23.7, 28.1) |
| Systolic blood pressure, mmHg | 146 (130, 162) | 146 (132, 162) |
| Hemoglobin, g/dL | 137 (131, 142) | 149 (143, 156) |
| Leukocytes, ×109/L | 5.3 (4.5, 6.3) | 5.6 (4.8, 6.6) |
| Platelet count, ×109/L | 243 (211, 278) | 208 (182, 237) |
| Reticulocytes, ×106/L | 0.04 (0.03, 0.05) | 0.04 (0.04, 0.05) |
| eGFR (CKD-EPICreatinine), mL/min/1.73 m2 | 80 (69, 89) | 80 (70, 88) |
| ALAT, U/L | 17 (14, 21) | 21 (17, 27) |
| HbA1c, % | 5.8 (5.6, 6) | 5.8 (5.6, 6.1) |
| Ferritin, μg/L | 90 (59,131) | 159 (93,237) |
| Vitamin B12, pmol/L | 248 (198, 322) | 234 (192, 289) |
| Red blood cell folate, nmol/L | 950 (701, 1244) | 888 (702, 1159) |
| CRP, mg/L | 1.4 (0.7, 2.6) | 1.2 (0.7, 2.3) |
| Female Reference Interval | Male Reference Interval | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Group, y | Participants, N | Lower Limit | Upper Limit | Lower Limit 90% CI | Upper Limit 90% CI | Participants, N | Lower Limit | Upper Limit | Lower Limit 90% CI | Upper Limit 90% CI |
| 60–69 | 274 | 168 | 363 | 163 to 174 | 352 to 375 | 240 | 151 | 300 | 147 to 156 | 290 to 309 |
| 70–79 | 248 | 168 | 351 | 163 to 173 | 339 to 363 | 199 | 133 | 293 | 127 to 140 | 284 to 302 |
| ≥80 | 126 | 162 | 358 | 155 to 170 | 339 to 377 | 88 | 121 | 304 | 112 to 131 | 286 to 322 |
| Female Reference Interval | Male Reference Interval | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age Group | Patients, N | Lower Limit | Upper Limit | pU-LRL | pU-URL | Patients, N | Lower Limit | Upper Limit | pU-LRL | pU-URL |
| 60–69 | 13,721 | 163 | 368 | 152 to 173 | 348 to 389 | 10482 | 135 | 325 | 126 to 144 | 304 to 340 |
| 70–79 | 10,272 | 164 | 392 | 153 to 175 | 370 to 414 | 7419 | 128 | 325 | 119 to 137 | 306 to 344 |
| ≥80 | 6399 | 149 | 371 | 138 to 159 | 350 to 392 | 3394 | 112 | 330 | 104 to 121 | 310 to 351 |
| Sex | Age, y | N | Abnormal, N | Abnormal, % (95% CI) | Thrombocytopenia, N | Thromboyctopenia, % (95% CI) | Thrombocytosis, N | Thrombocytosis, % (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Female | 60–69 | 3840 | 774 | 20.2 (18.9, 21.59) | 141 | 557 | 14.5 (13.4, 15.7) | |
| 70–79 | 3687 | 796 | 21.6 (20.3, 22.9) | 201 | 5.5 (4.8, 6.2) | 595 | 16.1 (15, 17.4) | |
| ≥80 | 3672 | 1003 | 27.3 (25.9, 28.8) | 373 | 10.2 (9.2, 11.2) | 630 | 17.2 (16, 18.4) | |
| All | 11,199 | 2573 | 23 (22.2, 23.8) | 715 | 6.4 (5.9, 6.9) | 1782 | 15.9 (15.2, 16.6) | |
| Male | 60–69 | 4995 | 870 | 17.4 (16.4, 18.5) | 429 | 8.6 (7.8, 9.4) | 441 | 8.8 (8.1, 9.6) |
| 70–79 | 4039 | 825 | 20.4 (19.2, 21.7) | 489 | 12.1 (11.1, 13.1) | 336 | 8.3 (7.5, 9.2) | |
| ≥80 | 2567 | 780 | 30.4 (28.6, 32.2) | 547 | 21.3 (19.8, 22.9) | 233 | 9.1 (8, 10.3) | |
| All | 11,601 | 2475 | 21.3 (20.6, 22.1) | 1465 | 12.6 (12, 13.2) | 1010 | 8.7 (8.2, 9.2) |
| Sex | Age, y | N | Abnormal, N | Abnormal, % (95% CI) | Thrombocytopenia, N | Thromboyctopenia, % (95% CI) | Thrombocytosis, N | Thrombocytosis, % (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Female | 60–69 | 3840 | 787 | 20.5 (19.2, 21.8) | 251 | 6.5 (5.8, 7.4) | 536 | 14.0 (12.9, 15.1) |
| 70–79 | 3687 | 869 | 23.6 (22.2, 25) | 319 | 8.7 (7.8, 9.6) | 550 | 14.9 (13.8, 16.1) | |
| ≥80 | 3672 | 1,084 | 29.5 (28.1, 34) | 488 | 13.3 (12.2, 14.4) | 596 | 16.2 (15.1, 17.5) | |
| All | 11,199 | 2,740 | 24.5 (23.7, 25.3) | 1058 | 9.4 (8.9, 10) | 1682 | 15.0 (14.4, 15.7) | |
| Male | 60–69 | 4995 | 1,309 | 26.2 (25, 27.4) | 429 | 8.6 (7.8, 9.4) | 880 | 17.6 (16.6, 18.7) |
| 70–79 | 4039 | 971 | 24.0 (22.7, 25.4) | 295 | 7.3 (6.5, 8.1) | 676 | 16.7 (15.6, 17.2) | |
| ≥80 | 2567 | 696 | 27.1 (25.4, 28.9) | 276 | 10.8 (9.6, 12) | 420 | 16.4 (15, 17.8) | |
| All | 11,601 | 2976 | 25.7 (24.9, 26.5) | 1000 | 8.6 (8.1, 9.1) | 1976 | 17.0 (16.4, 17.7) |
| Authors | Year | Sex Stratification | Age Stratification | Age Range | Sex | N | Reference Group | LRL (90% CI) | URL (90% CI) | Ref. |
|---|---|---|---|---|---|---|---|---|---|---|
| Books and Standard References | ||||||||||
| Giles | 1981 | no | no | NA | Female/Male | NA | NA | 150 (NA) | 450 (NA) | [55] |
| Laurell | 1997 | no | no | NA | Female/Male | NA | NA | 125 (NA) | 340 (NA) | Cited in [48] |
| Kratz et al. | 2004 | no | no | NA | Female/Male | NA | NA | 150 (NA) | 350 (NA) | [21] |
| Williams 9th ed. | 2017 | no | no | NA | Female/Male | NA | NA | 175 (NA) | 450 (NA) | [47] |
| Wintrobes 14th ed. | 2019 | no | no | NA | Female/Male | NA | NA | 177 (NA) | 406 (NA) | [58] |
| Original Papers | ||||||||||
| Hermann et al. | 2020 | yes | yes | 60–99 | Female | 648 | Prospectively assembled cohort of subjectively healthy participants in Switzerland with exclusion of individuals with disease | 167 (164–170) | 355 (347, 362) | ** |
| 60–69 | Male | 240 | 151 (147–156) | 300 (290, 309) | ||||||
| 70–79 | Male | 199 | 133 (127–150) | 293 (284–302) | ||||||
| 80–94 | Male | 88 | 121 (112–131) | 304 (286–322) | ||||||
| Biino et al. * | 2013 | yes | yes | 15–64 | Female | 16,358 | Pooled analysis of 3 population-based studies in Italy with exclusion of individuals with disease | 156 (153–158) | 405 (401–410) | [49] |
| 65–100 | Female | 4835 | 140 (137–144) | 379 (372–390) | ||||||
| 15–64 | Male | 13,789 | 141 (140–144) | 362 (358–365) | ||||||
| 65–100 | Male | 4303 | 122 (119–126) | 350 (343–360) | ||||||
| Nah et al. | 2018 | yes | yes | 12–99 | Female | 196,419 | Checkups of individuals performed at 16 health promotion centers in 13 Korean cities with exclusion of individuals with disease | 159 (NA) | 367 (NA) | [51] |
| 60–75 | Male | NA | 140 (NA) | 367 (NA) | ||||||
| 76–99 | Male | NA | 126 (NA) | 367 (NA) | ||||||
| Giacomini et al. | 2001 | yes | yes | 45–65 | Female | 50 | Blood donors and healthy individuals presenting to laboratory for checkup in Italy | 156 (NA) | 351 (NA) | [50] |
| 45–65 | Male | 50 | 156 (NA) | 300 (NA) | ||||||
| 66–85 | Female/Male | 100 | 139 (NA) | 363 (NA) | ||||||
| Adeli et al. | 2015 | yes | no | 27–79 | Female | 1390 | Canadian Health Measures Survey (CHMS) with exclusion of sick participants | 153 (138–169) | 361 (348–375) | [20] |
| 27–79 | Male | 1490 | 152 (144–159) | 324 (315–333) | ||||||
| Troussard et al. | 2013 | yes | no | 55–69 | Female | 4739 | Periodic health assessment in 11 prevention and public health centers in western France, mainly Caucasian; exclusion of participants with disease | 187 (NA) | 420 (NA) | [19] |
| 60–64 | Male | 1747 | 191 (NA) | 393 (NA) | ||||||
| Park et al. | 2016 | yes | no | >60–? | Female | 40 | Healthy adults who received a general health examination in Korea | 135 (NA) | 326 (NA) | [18] |
| >60–? | Male | 51 | 125 (NA) | 347 (NA) | ||||||
| Helmersson-Karlqvist et al. | 2016 | yes | no | 80 | Female | 228 | Population-based study in Uppsala with exclusion of patients with diabetes mellitus and/or cardiovascular disease | 156 (136–175) | 426 (387–466) | [17] |
| 80 | Male | 181 | 116 (99–134) | 399 (306–493) | ||||||
| Nordin et al. | 2004 | yes | no | 18–91 | Female | 960 | Healthy laboratory staff from 102 medical laboratories in Scandinavia and their adult family members | 165 (159–173) | 387 (375–403) | [48] |
| 18–90 | Male | 866 | 145 (138–145) | 348 (334–358) | ||||||
| Tsang et al. | 1998 | yes | no | 49–97 | Female | 1837 | Population-based study in Sydney with exclusion of individuals with disease | 163 (NA) | 414 (NA) | [57] |
| 49–97 | Male | 1382 | 153 (NA) | 382 (NA) | ||||||
| Jernigan et al. | 1980 | No | no | 64–94 | Female/Male | 73 | Healthy participants at a periodic health exam | 140 (NA) | 440 (NA) | [24] |
| Janu et al. | 2003 | no | no | 75–100 | Female/Male | 338 | Community-dwelling cohort with random sampling in Sydney (including 38 nursing home residents) | 150 (NA) | 450 (NA) | [23] |
| Huber et al. | 2006 | no | no | 75 | Female/Male | 119 | Selection of apparently healthy individuals from a prospective population-based study in Vienna by exclusion of individuals with disease | 114 (84–144) | 452 (389–472) | [56] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hermann, W.; Risch, L.; Grebhardt, C.; Nydegger, U.E.; Sakem, B.; Imperiali, M.; Renz, H.; Risch, M. Reference Intervals for Platelet Counts in the Elderly: Results from the Prospective SENIORLAB Study. J. Clin. Med. 2020, 9, 2856. https://doi.org/10.3390/jcm9092856
Hermann W, Risch L, Grebhardt C, Nydegger UE, Sakem B, Imperiali M, Renz H, Risch M. Reference Intervals for Platelet Counts in the Elderly: Results from the Prospective SENIORLAB Study. Journal of Clinical Medicine. 2020; 9(9):2856. https://doi.org/10.3390/jcm9092856
Chicago/Turabian StyleHermann, Wolfgang, Lorenz Risch, Chris Grebhardt, Urs E. Nydegger, Benjamin Sakem, Mauro Imperiali, Harald Renz, and Martin Risch. 2020. "Reference Intervals for Platelet Counts in the Elderly: Results from the Prospective SENIORLAB Study" Journal of Clinical Medicine 9, no. 9: 2856. https://doi.org/10.3390/jcm9092856
APA StyleHermann, W., Risch, L., Grebhardt, C., Nydegger, U. E., Sakem, B., Imperiali, M., Renz, H., & Risch, M. (2020). Reference Intervals for Platelet Counts in the Elderly: Results from the Prospective SENIORLAB Study. Journal of Clinical Medicine, 9(9), 2856. https://doi.org/10.3390/jcm9092856







