Urogynaecological Symptoms among Oncological Survivors and Impact of Oncological Treatment on Pelvic Floor Disorders and Lower Urinary Tract Symptoms. A Six-Month Follow-Up Study
Abstract
:1. Introduction
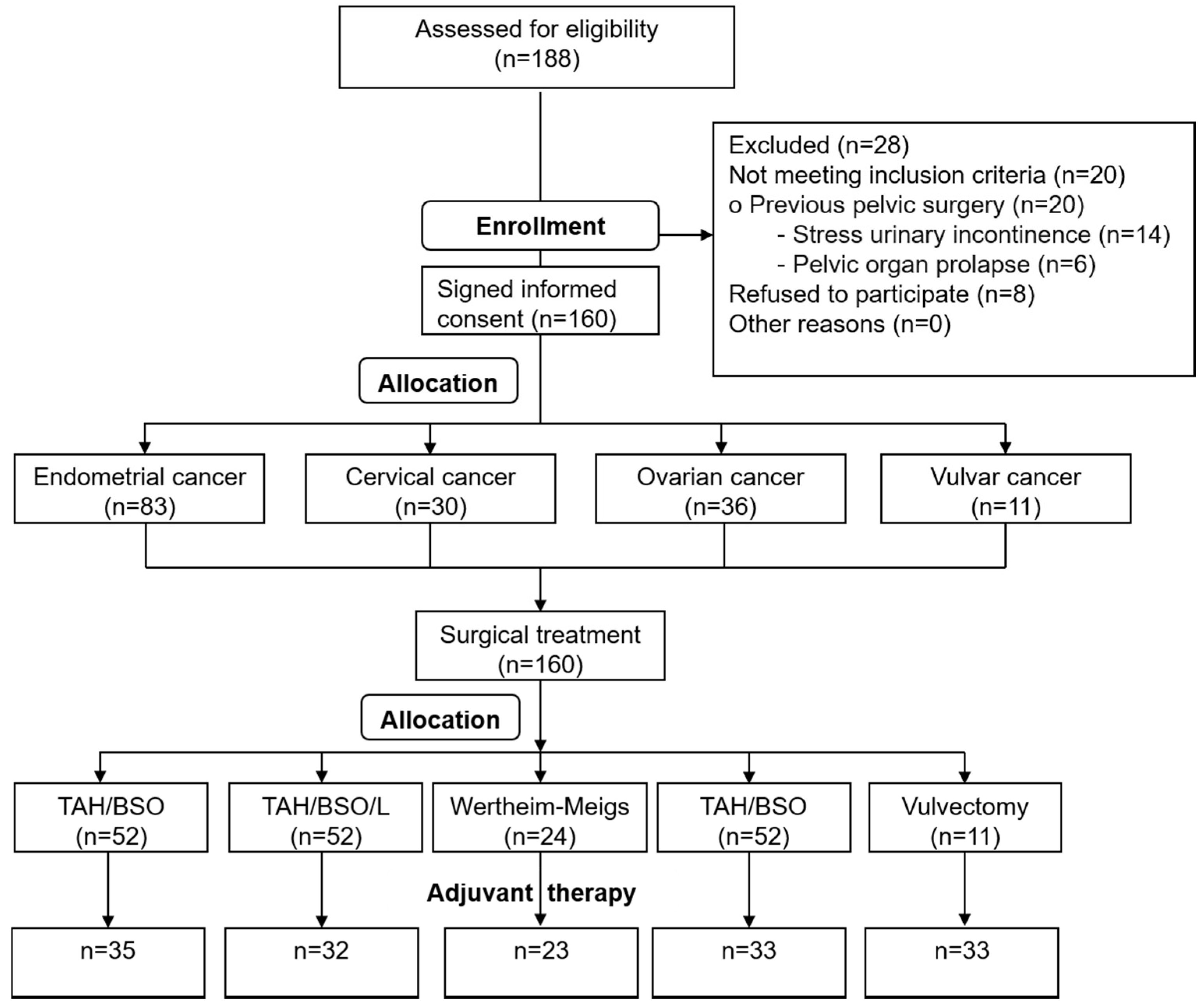
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Neron, M.; Bastide, S.; De Tayrac, R.; Masia, F.; Ferrer, C.; Labaki, M.; Boileau, L.; Letouzey, V.; Huberlant, S. Impact of gynecologic cancer on pelvic floor disorder symptoms and quality of life: An observational study. Sci. Rep. 2019, 9, 2250. [Google Scholar] [CrossRef] [Green Version]
- Hsieh, C.-I.; Lung, A.-L.; Chang, L.-I.; Sampselle, C.M.; Lin, C.-C.; Liao, Y.-M. Prevalence, associated factors, and relationship to quality of life of lower urinary tract symptoms: A cross-sectional, questionnaire survey of cancer patients. Int. J. Clin. Pract. 2013, 67, 566–575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Novackova, M.; Pastor, Z.; Chmel, R.; Brtnicky, T.; Chmel, R. Urinary tract morbidity after nerve-sparing radical hysterectomy in women with cervical cancer. Int. Urogynecol. J. 2019, 31, 981–987. [Google Scholar] [CrossRef] [PubMed]
- Coyne, K.S.; Wein, A.J.; Tubaro, A.; Sexton, C.C.; Thompson, C.L.; Kopp, Z.S.; Aiyer, L.P. The burden of lower urinary tract symptoms: Evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009, 103, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Didkowska, J.; Wojciechowska, U.; Zatoński, J. Prognozy Zachorowalności i Umieralności na Nowotwory Złośliwe w Polsce do 2025 Roku; Polska Unia Onkologii: Warsaw, Poland, 2013; Available online: http://www.puo.pl/publikacje/statystyki/prognozy-zachorowalnosci-i-umieralnosci-na-nowotwory-zlosliwe-w-polsce-do-2025-roku (accessed on 10 October 2013).
- Deimling, G.T.; Pappada, H.; Ye, M.; Nalepa, E.; Ciaralli, S.; Phelps, E.; Burant, C.J. Factors Affecting Perceptions of Disability and Self-Rated Health Among Older Adult, Long-Term Cancer Survivors. J. Aging Health 2017, 31, 667–684. [Google Scholar] [CrossRef] [PubMed]
- Ramaseshan, A.S.; Felton, J.; Roque, D.; Rao, G.; Shipper, A.G.; Sanses, T.V.D. Pelvic floor disorders in women with gynecologic malignancies: A systematic review. Int. Urogynecol. J. 2017, 29, 459–476. [Google Scholar] [CrossRef] [PubMed]
- Chiaffarino, F.; Parazzini, F.; Lavezzari, M.; Giambanco, V. Impact of urinary incontinence and overactive bladder on quality of life. Eur. Urol. 2003, 43, 535–538. [Google Scholar] [CrossRef]
- Irwin, D.E.; Milsom, I.; Kopp, Z.S.; Abrams, P. Symptom Bother and Health Care–Seeking Behavior among Individuals with Overactive Bladder. Eur. Urol. 2008, 53, 1029–1037. [Google Scholar] [CrossRef]
- Helfand, B.T.; Lee, J.Y.; Sharp, V.; Foster, H.; Naslund, M.; Williams, O.D.; McVary, K.T.; CAMUS Study Group. Associations between Improvements in Lower Urinary Tract Symptoms and Sleep Disturbance over Time in the CAMUS Trial. J. Urol. 2011, 185, 2223–2228. [Google Scholar] [CrossRef]
- Skorupska, K.; Miotła, P.; Kubik-Komar, A.; Skorupski, P.; Rechberger, T. Development and validation of the Polish version of the Urogenital Distress Inventory short form and the Incontinence Impact Questionnaire short form. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 215, 171–174. [Google Scholar] [CrossRef]
- Brazier, J.E.; Czoski-Murray, C.; Roberts, J.; Brown, M.; Symonds, T.; Kelleher, C. Estimation of a Preference-Based Index from a Condition-Specific Measure: The King’s Health Questionnaire. Med. Decis. Mak. 2008, 28, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Vij, M.; Srikrishna, S.; Robinson, D.; Cardozo, L. Quality assurance in quality of life assessment—Measuring the validity of the King’s Health Questionnaire. Int. Urogynecol. J. 2014, 25, 1133–1135. [Google Scholar] [CrossRef] [PubMed]
- Tylka, J. [SF-36 questionnaire—Final part of discussion]. Kardiol. Pol. 2010, 68, 985. [Google Scholar] [PubMed]
- Tamanini, J.T.; Dambros, M.; D’Ancona, C.A.; Palma, P.C.; Botega, N.J.; Rios, L.A.; Gomes, C.M.; Baracat, F.; Bezerra, C.A.; Netto, N.R., Jr. Concurrent validity, internal consistency and responsiveness of the portuguese version of the king’s health questionnaire (KHQ) in women after stress urinary incontinence surgery. Int. Braz. J. Urol. 2004, 30, 479–486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [Green Version]
- Wehrberger, C.; Madersbacher, S.; Jungwirth, S.; Fischer, P.; Tragl, K.-H. Lower urinary tract symptoms and urinary incontinence in a geriatric cohort—A population-based analysis. BJU Int. 2012, 110, 1516–1521. [Google Scholar] [CrossRef]
- Bosch, J.R.; Norton, P.; Jones, J.S. Should we screen for and treat lower urinary tract dysfunction after major pelvic surgery? ICI-RS 2011. Neurourol. Urodyn. 2012, 31, 327–329. [Google Scholar] [CrossRef]
- Brown, J.S.; Sawaya, G.; Thom, D.H.; Grady, D. Hysterectomy and urinary incontinence: A systematic review. Lancet 2000, 356, 535–539. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kim, S.K.; Kim, S.R.; Bai, S.W. The significance and factors related to bladder outlet obstruction in pelvic floor dysfunction in preoperative urodynamic studies: A retrospective cohort study. Obstet. Gynecol. Sci. 2014, 57, 59–65. [Google Scholar] [CrossRef] [Green Version]
- Donovan, K.A.; Boyington, A.R.; Judson, P.L.; Wyman, J.F. Bladder and bowel symptoms in cervical and endometrial cancer survivors. Psychooncology 2014, 23, 672–678. [Google Scholar] [CrossRef] [Green Version]
- Erekson, E.A.; Sung, V.W.; DiSilvestro, P.A.; Myers, D.L. Urinary symptoms and impact on quality of life in women after treatment for endometrial cancer. Int. Urogynecol. J. 2009, 20, 159–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krhut, J.; Gärtner, M.; Mokris, J.; Horcicka, L.; Svabik, K.; Zachoval, R.; Martan, A.; Zvara, P. Effect of severity of urinary incontinence on quality of life in women. Neurourol. Urodyn. 2018, 37, 1925–1930. [Google Scholar] [CrossRef] [PubMed]
- Yen, A.; Tian, Z.; Hrycushko, B.; Albuquerque, K. Risk factors for fistula formation after interstitial brachytherapy for locally advanced gynecological cancers involving vagina. J. Contemp. Brachytherapy 2018, 10, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Manchana, T.; Puangsricharoen, P.; Sirisabya, N.; Worasethsin, P.; Vasuratna, A.; Termrungruanglert, W.; Tresukosol, D. Comparison of Perioperative and Oncologic Outcomes with Laparotomy, and Laparoscopic or Robotic Surgery for Women with Endometrial Cancer. Asian Pac. J. Cancer Prev. 2015, 16, 5483–5488. [Google Scholar] [CrossRef] [Green Version]
- Farquhar, C.; Brown, P.M.; Furness, S. Cost effectiveness of pre-operative gonadotrophin releasing analogues for women with uterine fibroids undergoing hysterectomy or myomectomy. BJOG 2002, 109, 1273–1280. [Google Scholar] [CrossRef]
- Kim, H.S.; Kim, K.; Ryoo, S.B.; Seo, J.H.; Kim, S.Y.; Park, J.W.; Kim, M.A.; Hong, K.S.; Jeong, C.W.; Song, Y.S.; et al. Conventional versus nerve sparing radical surgery for cervical cancer: A meta-analysis. J. Gynecol. Oncol. 2015, 26, 100–110. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Wang, G.C.; Liu, Y.J.; Wang, Y.C.; Chen, X.B.; Luo, Y.L.; Li, D.; Xing, H.B.; Gao, C.Q. Surgical concept and techniques of recurrent cervical cancer patients accompanied with high risk of intestinal obstruction after radical radiotherapy. Zhonghua Zhong Liu Za Zhi 2020, 42, 61–64. [Google Scholar] [CrossRef]
- De Boer, S.M.; Nout, R.A.; Jürgenliemk-Schulz, I.M.; Jobsen, J.J.; Lutgens, L.C.; van der Steen-Banasik, E.M.; Mens, J.W.; Slot, A.; Stenfert-Kroese, M.C.; Oerlemans, S.; et al. Long-Term Impact of Endometrial Cancer Diagnosis and Treatment on Health-Related Quality of Life and Cancer Survivorship: Results From the Randomized PORTEC-2 Trial. Int. J. Radiat. Oncol. 2015, 93, 797–809. [Google Scholar] [CrossRef] [Green Version]
- Pisani, C.; Deantonio, L.; Surico, D.; Brambilla, M.; Galla, A.; Ferrara, E.; Masini, L.; Gambaro, G.; Surico, N.; Krengli, M. Quality of life in patients treated by adjuvant radiotherapy for endometrial and cervical cancers: Correlation with dose-volume parameters. Clin. Transl. Oncol. 2016, 18, 901–908. [Google Scholar] [CrossRef]
- White, A.J.; Reeve, B.B.; Chen, R.C.; Stover, A.M.; Irwin, D.E. Coexistence of urinary incontinence and major depressive disorder with health-related quality of life in older Americans with and without cancer. J. Cancer Surviv. 2014, 8, 497–507. [Google Scholar] [CrossRef] [Green Version]
- Balzarro, M.; Rubilotta, E.; Goss, C.; Costantini, E.; Artibani, W.; Sand, P. Counseling in urogynecology: A difficult task, or simply good surgeon-patient communication? Int. Urogynecol. J. 2018, 29, 943–948. [Google Scholar] [CrossRef] [PubMed]
| Age Groups | E | C | O | V |
|---|---|---|---|---|
| W1 | 14 | 10 | 15 | 2 |
| W2 | 27 | 8 | 6 | 2 |
| W3 | 18 | 8 | 9 | 2 |
| W4 | 24 | 4 | 6 | 5 |
| Total | 83 | 30 | 36 | 11 |
| FIGO | E | C | O | V | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| UI | POP | UI + POP | UI | POP | UI + POP | UI | POP | UI + POP | UI | POP | UI + POP | |||||
| I | 68 | 23 (33.8%) | 30 (44.1%) | 19 (27.9%) | 23 | 14 (60.9%) | 10 (43.5%) | 9 (39.1%) | 9 | 6 (66.7%) | 5 (55.6%) | 4 (44.4%) | 7 | 1 | - | - |
| II | 13 | 9 (69.2%) | 11 (84.6%) | 7 (53.8%) | 6 | 2 (33.3%) | 2 (33.3%) | 1 (16.7%) | 12 | 9 (75%) | 7 (58.3%) | 5 (41.7%) | 4 | - | - | - |
| III | 2 | 1 (50%) | - | 1 (50%) | 1 | - | - | - | 13 | 3 (23.1%) | 2 (15.4%) | 1 (7.7%) | 0 | - | - | - |
| IV | 0 | - | - | 0 | - | - | - | 2 | 1 (50%) | - | - | 0 | - | - | - | |
| Total | 83 | 33 (39.8%) | 41 (49.4%) | 27 (32.5%) | 30 | 16 (53.3%) | 12 (40%) | 10 (33.3%) | 36 | 19 (52.8%) | 14 (38.9%) | 10 (27.8%) | 11 | 1 | - | - |
| Type of Surgical Treatment | Radiation (n) | Chemoradiation (n) | Chemotherapy (n) | None (n) |
|---|---|---|---|---|
| TAH/BSO (n = 52) | 29 | 4 | 2 | 17 |
| TAH/BSO/L (n = 38) | 16 | 13 | 3 | 6 |
| Wertheim-Meigs hysterectomy (n = 24) | 1 | 18 | 4 | 1 |
| Debulking surgery (n = 35) | 6 | 4 | 23 | 2 |
| Vulvectomy (n = 11) | 6 | 3 | 0 | 2 |
| Before n (%) | At Follow-Up | ||||
|---|---|---|---|---|---|
| After n (%) | De Novo n (%) | Reduction of Symptoms n (%) | Resolution of Symptoms n (%) | ||
| Urinary incontinence (UI) | 69 (43.0%) | 78 (48.8%) | 25 (32.1%) | 5 (6.4%) | 16 (20.5%) |
| Concomitant POP | 40 (58.0%) | 49 (62.8%) | 14 (28.6%) | 2 (4%) | 5 (10.2%) |
| Pelvic organ prolapse (POP) | 67 (41.9%) | 65 (40.6%) | 10 (15.4%) | 2 (3.1%) | 12 (18.4%) |
| Concomitant UI | 44 (65.7%) | 32 (49.2%) | 6 (18.8%) | 1 (3.1%) | 18 (56.3%) |
| Questionnaire | n | Mean | SD | T | Z | p |
|---|---|---|---|---|---|---|
| UDI-6 before | 160 | 38.64 | 24.11 | 1689.00 | 4.69 | p < 0.05 |
| UDI-6 after | 51.04 | 28.47 | ||||
| II-Q7 before | 160 | 54.02 | 27.59 | 2373.00 | 6.93 | p < 0.05 |
| II-Q7 after | 76.79 | 36.62 |
| Questionnaire | UDI-6 | II-Q7 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | Before | After | ||||||||
| Surgery Type | n | Mean (±SD) | Mean (±SD) | T | Z | p | Mean (±SD) | Mean (±SD) | T | Z | p |
| TAH/BSO | 52 | 34.21 (22.83) | 47.67 (27.2) | 141 | 3.48 | p < 0.05 | 47.25 (18.28) | 71.15 (30.42) | 132.5 | 5.07 | p < 0.05 |
| TAH/BSO/lymphadenectomy | 38 | 41.23 (26.93) | 54.17 (26.88) | 75.5 | 2.73 | p < 0.05 | 59.4 (32.61) | 82.46 (39.36) | 180 | 2.76 | p < 0.05 |
| Wertheim-Meigs radical hysterectomy | 24 | 41.67 (23.79) | 50.17 (32.5) | 46 | 1.44 | p < 0.05 | 52.98 (29.4) | 79.56 (40.61) | 39 | 3.17 | p < 0.05 |
| Debulking surgery | 35 | 38.57 (23.45) | 53.93 (32.18) | 73.5 | 2.39 | p < 0.05 | 55.92 (31.47) | 80.68 (41.03) | 129 | 3.05 | p < 0.05 |
| Vulvectomy | 11 | 48.86 (22.75) | 48.86 (19.01) | 18 | 0 | p < 0.05 | 63.64 (25.4) | 65.37 (29.21) | 27 | 0.53 | p < 0.05 |
| Before | After | |||
|---|---|---|---|---|
| Domain | Mean (±SD) | Mean (±SD) | Z | p |
| GH | 41.87 (21.99) | 51.17 (28.17) | 2.13 | p < 0.05 |
| II | 35.41 (23.55) | 50.31 (34.75) | 3.96 | p < 0.05 |
| RL | 38.12 (26.12) | 51.15 (30.98) | 4.02 | p < 0.05 |
| PL | 36.45 (22.28) | 50.1 (28.75) | 10.93 | p < 0.05 |
| SL | 33.47 (2.9) | 48.21 (31.44) | 3.67 | p < 0.05 |
| PR | 28.33 (30.47) | 44.02 (41.22) | 3.55 | p < 0.05 |
| E | 30.76 (26.26) | 46.89 (35.37) | 10.60 | p < 0.05 |
| S/E | 53.77 (38.24) | 53.77 (38.24) | 4.06 | p < 0.05 |
| SM | 51.91 (31.06) | 57.94 (35.16) | 1.62 | p < 0.05 |
| Surgery Type | Domain | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| GH | II | RL | PL | SL | PR | E | S/E | SM | |
| TAH/BSO | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | ||||
| TAH/BSO/lymphadenectomy | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | ||
| Wertheim-Meigs radical hysterectomy | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | |||
| Debulking surgery | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | p < 0.05 | |||
| Vulvectomy | |||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ziętek-Strobl, A.; Futyma, K.; Kuna-Broniowska, I.; Wojtaś, M.; Rechberger, T. Urogynaecological Symptoms among Oncological Survivors and Impact of Oncological Treatment on Pelvic Floor Disorders and Lower Urinary Tract Symptoms. A Six-Month Follow-Up Study. J. Clin. Med. 2020, 9, 2804. https://doi.org/10.3390/jcm9092804
Ziętek-Strobl A, Futyma K, Kuna-Broniowska I, Wojtaś M, Rechberger T. Urogynaecological Symptoms among Oncological Survivors and Impact of Oncological Treatment on Pelvic Floor Disorders and Lower Urinary Tract Symptoms. A Six-Month Follow-Up Study. Journal of Clinical Medicine. 2020; 9(9):2804. https://doi.org/10.3390/jcm9092804
Chicago/Turabian StyleZiętek-Strobl, Alicja, Konrad Futyma, Izabela Kuna-Broniowska, Małgorzata Wojtaś, and Tomasz Rechberger. 2020. "Urogynaecological Symptoms among Oncological Survivors and Impact of Oncological Treatment on Pelvic Floor Disorders and Lower Urinary Tract Symptoms. A Six-Month Follow-Up Study" Journal of Clinical Medicine 9, no. 9: 2804. https://doi.org/10.3390/jcm9092804
APA StyleZiętek-Strobl, A., Futyma, K., Kuna-Broniowska, I., Wojtaś, M., & Rechberger, T. (2020). Urogynaecological Symptoms among Oncological Survivors and Impact of Oncological Treatment on Pelvic Floor Disorders and Lower Urinary Tract Symptoms. A Six-Month Follow-Up Study. Journal of Clinical Medicine, 9(9), 2804. https://doi.org/10.3390/jcm9092804





