The Role of Imaging Techniques to Define a Peri-Prosthetic Hip and Knee Joint Infection: Multidisciplinary Consensus Statements
Abstract
1. Introduction
2. Assessment Parameters of Peri-Prosthetic Joint According to PJI Definitions
3. Conventional Techniques for Diagnosis of PJI
4. Nuclear Medicine Techniques for Diagnosis of PJI
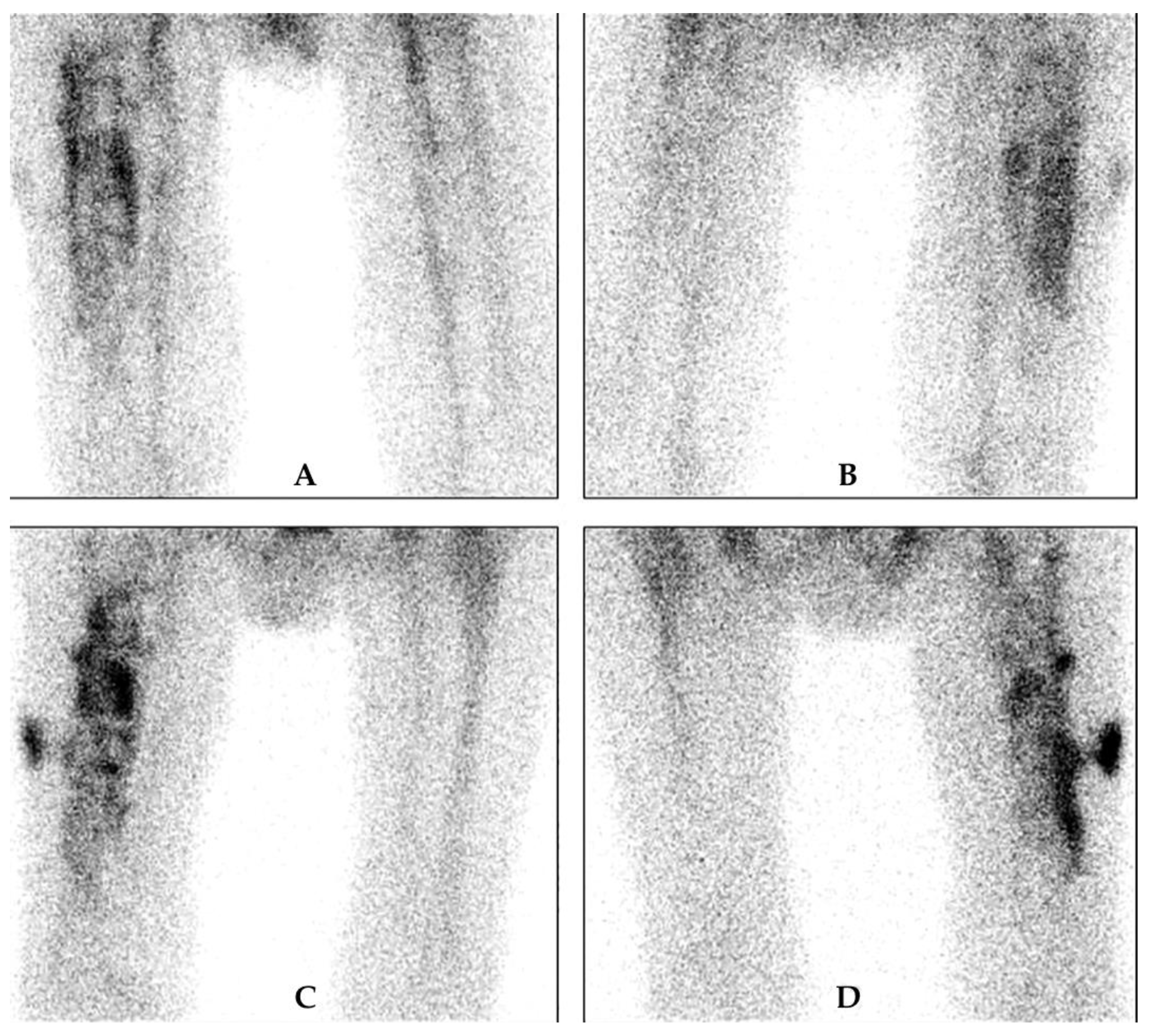
4.1. Bone Scintigraphy
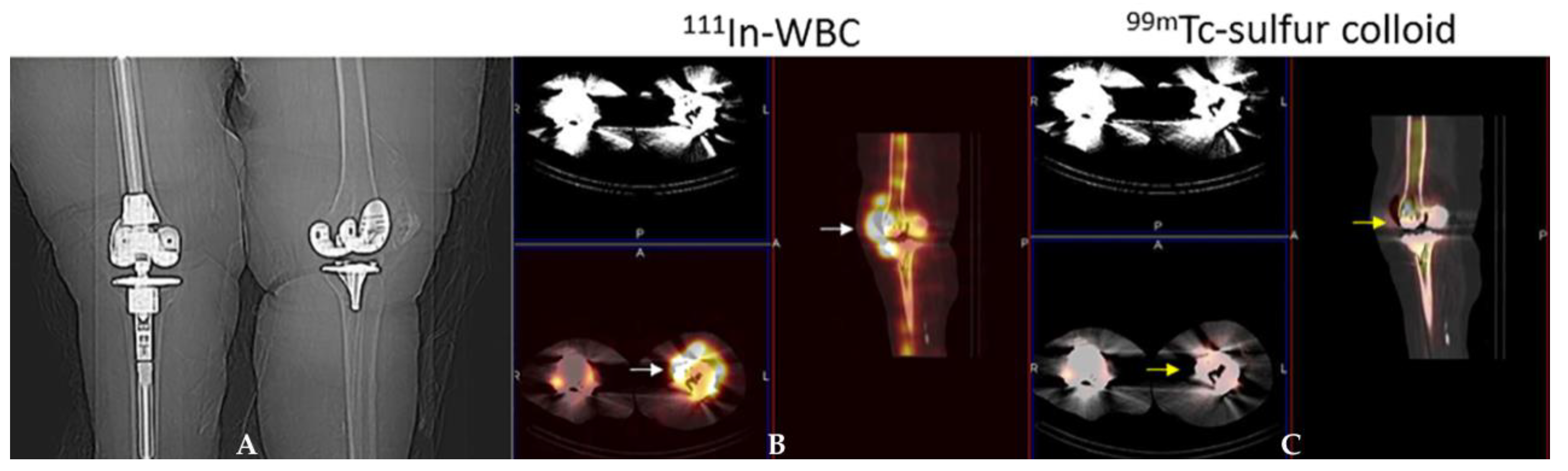
4.2. White Blood Cell Scintigraphy
4.3. Anti-Granulocyte Antibody Scintigraphy
4.4. Bone Marrow Scintigraphy
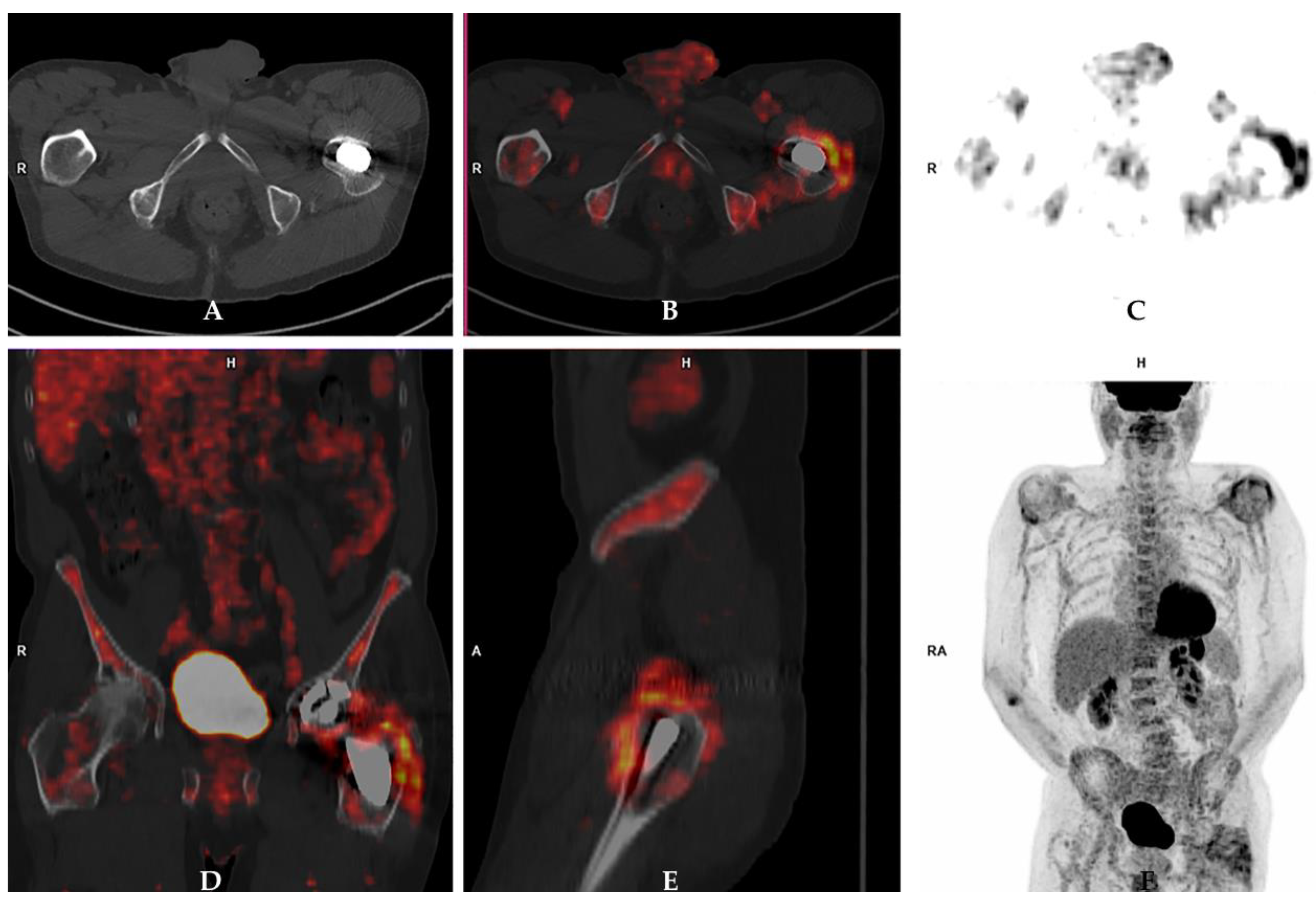
4.5. FDG PET/CT
4.6. Hybrid Imaging Techniques
5. Clinical Questions and Consensus Answers
5.1. What Is the Role of Conventional X-ray to Diagnose a PJI?
5.2. What Is the Role of Ultrasound to Diagnose a PJI?
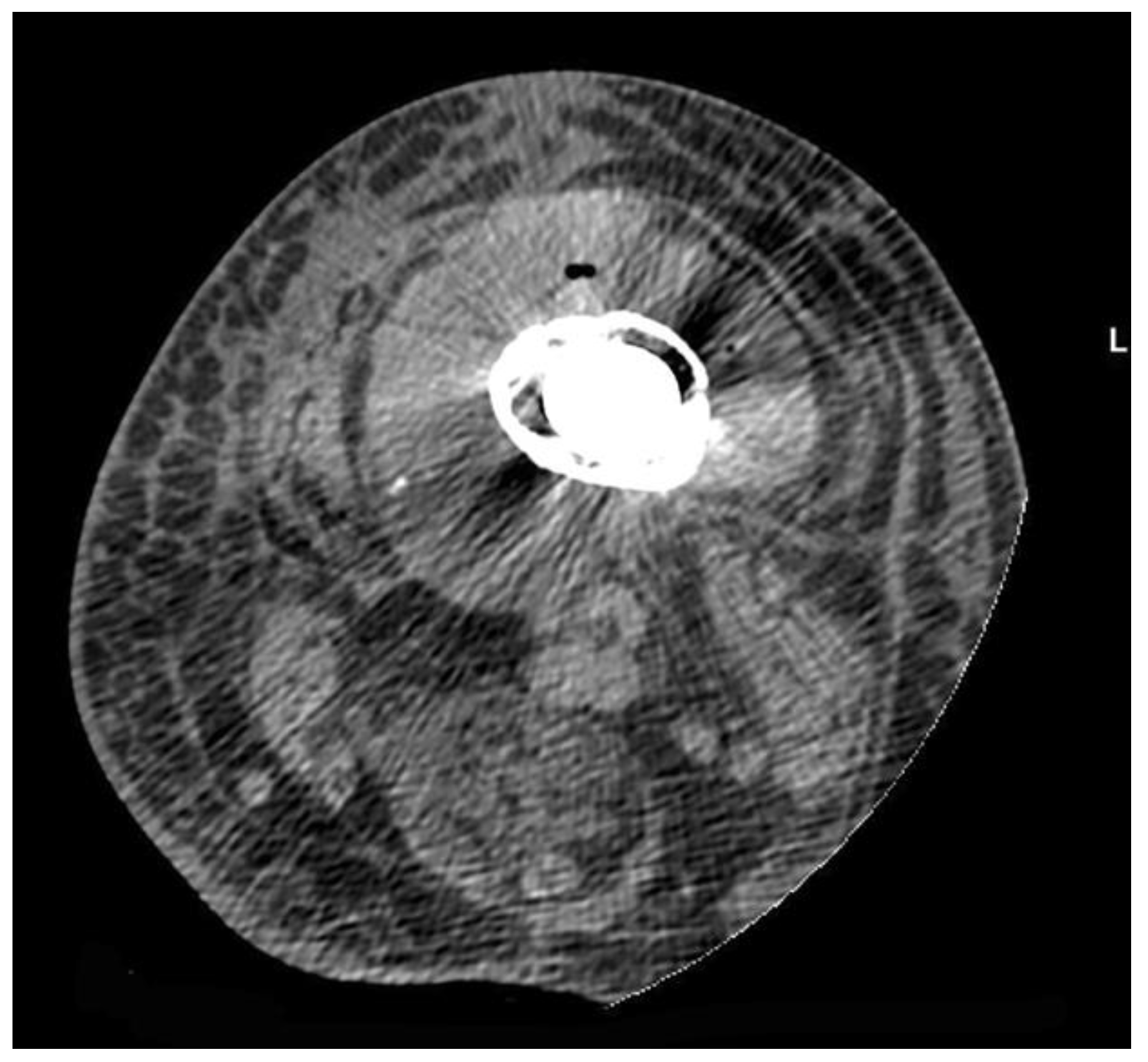
5.3. What Is the Role of CT to Diagnose a PJI?
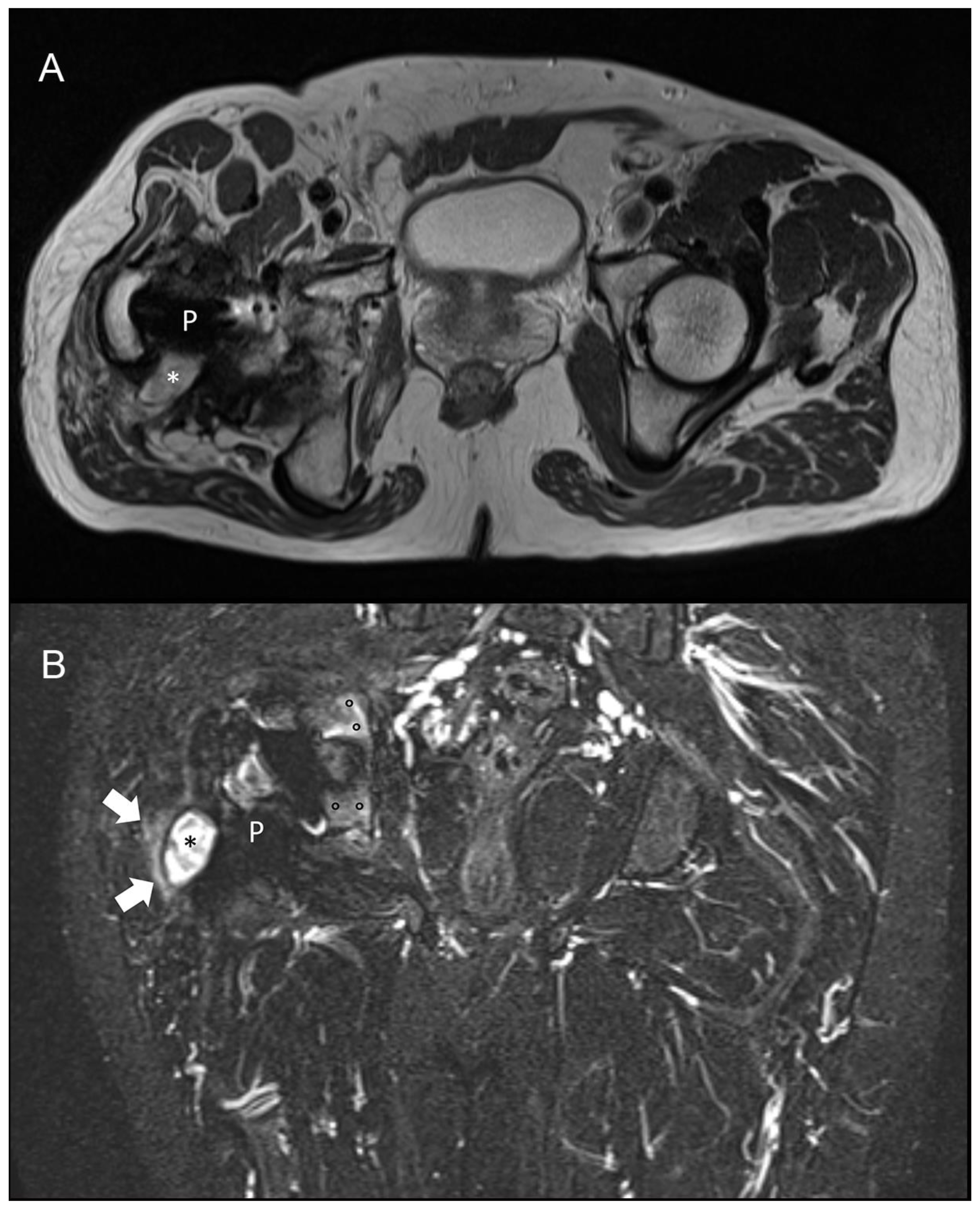
5.4. What Is the Role of MRI to Diagnose a PJI?
5.5. What Is the Role of Three-Phase Bone Scan to Diagnose a PJI (Is a Negative Scan Sufficient to Exclude a PJI)?
5.6. What Is the Minimum Time Window between the Date of Surgery and a Three-Phase Bone Scan to Diagnose a PJI?
5.7. What Is the Role of a WBC Scan to Diagnose a PJI (Is a Negative Scan Sufficient to Exclude a PJI)?
5.8. What Is the Role of [18F]-FDG-PET/CT to Diagnose a PJI (Is a Negative Scan Sufficient to Exclude a PJI)?
5.9. What Is the Spatial Resolution of Currently Available Imaging Techniques in Order to Describe the Extent of a PJI?
5.10. Can Clinicians Rely on a Scan to Decide to Maintain a Component of an Implant If Infection Is Ruled Out by Imaging Investigations?
5.11. Is There Any Evidence That Imaging Techniques May Have Different Accuracy or Thresholds to Diagnose High-Grade and Low-Grade Peri-Prosthetic Joint Infections?
5.12. Are There Any Studies Comparing Intra-Operative Histological Findings and/or Microbiological Examination with Imaging Investigations?
5.13. Is It Necessary to Stop Antibiotic Treatment before Performing a Scan to Diagnose a PJI?
5.14. What Are the Most Promising Technologies Currently under Investigation to Diagnose PJI and Other Implant-Related Infections?
5.15. Should Nuclear Medicine Imaging Techniques Be Included in the Definition of Peri-Prosthetic Joint Infection and, in Case of a Positive Answer, Which One Would You Recommend?
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Renz, N.; Yermak, K.; Perka, C.; Trampuz, A. Alpha Defensin Lateral Flow Test for Diagnosis of Periprosthetic Joint Infection: Not a Screening but a Confirmatory Test. J. Bone Jt. Surg. Am. 2018, 100, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Prieto, D.; Portillo, M.E.; Puig-Verdié, L.; Alier, A.; Martínez, S.; Sorlí, L.; Horcajada, J.P.; Monllau, J.C. C-reactive protein may misdiagnose prosthetic joint infections, particularly chronic and low-grade infections. Int. Orthop. 2017, 41, 1315–1319. [Google Scholar] [CrossRef] [PubMed]
- Romanò, C.L.; Romanò, D.; Morelli, I.; Drago, L. The Concept of Biofilm-Related Implant Malfunction and “Low-Grade Infection”. Adv. Exp. Med. Biol. 2017, 971, 1–13. [Google Scholar] [CrossRef]
- Baumbach, S.F.; Prall, W.C.; Scharpf, A.M.; Hererich, V.; Schmidt, M.; Suedkamp, N.P.; Stoehr, A.; Mayr, H.O. Significant increase of pathogen detection rate by dry arthroscopic biopsies at suspected low-grade infection following total knee arthroplasty: A prospective observational study. Arch. Orthop. Trauma Surg. 2018, 138, 1583–1590. [Google Scholar] [CrossRef] [PubMed]
- Morgenstern, C.; Cabric, S.; Perka, C.; Trampuz, A.; Renz, N. Synovial fluid multiplex PCR is superior to culture for detection of low-virulent pathogens causing periprosthetic joint infection. Diagn. Microbiol. Infect. Dis. 2018, 90, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Goswami, K.; Parvizi, J.; Maxwell Courtney, P. Current Recommendations for the Diagnosis of Acute and Chronic PJI for Hip and Knee-Cell Counts, Alpha-Defensin, Leukocyte Esterase, Next-generation Sequencing. Curr. Rev. Musculoskelet. Med. 2018, 11, 428–438. [Google Scholar] [CrossRef]
- Parvizi, J.; Zmistowski, B.; Berbari, E.F.; Bauer, T.W.; Springer, B.D.; Della Valle, C.J.; Garvin, K.L.; Mont, M.A.; Wongworawat, M.D.; Zalavras, C.G. New definition for periprosthetic joint infection: From the workgroup of the Musculoskeletal infection Society. Clin. Orthop. Relat. Res. 2011, 469, 2992e4. [Google Scholar] [CrossRef]
- Osmon, D.R.; Berbari, E.F.; Berendt, A.R.; Lew, D.; Zimmerli, W.; Steckelberg, J.M.; Rao, N.; Hanssen, A.; Wilson, W.R. Infectious Diseases Society of America. Diagnosis and management of prosthetic joint infection: Clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 2013, 56, e1–e25. [Google Scholar] [CrossRef]
- Parvizi, J.; Gehrke, T.; International Consensus Group on Periprosthetic Joint Infection. Definition of periprosthetic joint infection. J. Arthroplast. 2014, 29, 1331. [Google Scholar] [CrossRef]
- Parvizi, J.; Tan, T.L.; Goswami, K.; Higuera, C.; Della Valle, C.; Chen, A.F.; Shohat, N. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J. Arthroplast. 2018, 33, 1309–1314. [Google Scholar] [CrossRef]
- Parvizi, J.; Gehrke, T. Proceedings of the Second International Consensus Meeting on Musculoskeletal Infection; Hip and Knee Section Data Trace Publishing Company: Brooklandville, MD, USA, 2018; ISBN 978-1-57400-157-0. [Google Scholar]
- Romanò, C.L.; Khawashki, H.A.; Benzakour, T.; Bozhkova, S.; Del Sel, H.; Hafez, M.; Johari, A.; Lob, G.; Sharma, H.K.; Tsuchiya, H.; et al. The W.A.I.O.T. Definition of High-Grade and Low-Grade Peri-Prosthetic Joint Infection. J. Clin. Med. 2019, 8, 650. [Google Scholar] [CrossRef]
- Bozhkova, S.; Suardi, V.; Sharma, H.K.; Tsuchiya, H.; Del Sel, H.; Hafez, M.A.; Benzakour, T.; Drago, L.; Romanò, C.L. The, W.A.I.O.T. Definition of Peri-Prosthetic Joint Infection: A Multi-center, Retrospective Validation Study. J. Clin. Med. 2020, 9, 1965. [Google Scholar] [CrossRef]
- Signore, A.; Sconfienza, L.M.; Borens, O.; Glaudemans, A.W.J.M.; Cassar-Pullicino, V.; Trampuz, A.; Winkler, H.; Gheysens, O.; Vanhoenacker, F.M.H.M.; Petrosillo, N.; et al. Consensus document for the diagnosis of prosthetic joint infections: A joint paper by the EANM, EBJIS, and ESR (with ESCMID endorsement). Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 971–988. [Google Scholar] [CrossRef]
- Sessa, G.; Romanò, C.L. Linea guida SIOT diagnosi di infezione peri-protesica articolare ritardata o tardiva (tempo trascorso dall’intervento > 90 giorni). G. Ital. Ortop. Traumatol. 2019, 45, 187–213. [Google Scholar] [CrossRef]
- Sconfienza, L.M.; Signore, A.; Cassar-Pullicino, V.; Cataldo, M.A.; Gheysens, O.; Borens, O.; Trampuz, A.; Wörtler, K.; Petrosillo, N.; Winkler, H.; et al. Diagnosis of peripheral bone and prosthetic joint infections: Overview on the consensus documents by the EANM, EBJIS, and ESR (with ESCMID endorsement). Eur. Radiol. 2019, 29, 6425–6438. [Google Scholar] [CrossRef]
- Li, C.; Renz, N.; Trampuz, A. Management of Periprosthetic Joint Infection. Hip Pelvis. 2018, 30, 138–146. [Google Scholar] [CrossRef]
- Yoon, H.K.; Cho, S.H.; Lee, D.Y.; Kang, B.H.; Lee, S.H.; Moon, D.G.; Kim, D.H.; Nam, D.C.; Hwang, S.C. A Review of the Literature on Culture-Negative Periprosthetic Joint Infection: Epidemiology, Diagnosis and Treatment. Knee Surg. Relat. Res. 2017, 29, 155–164. [Google Scholar] [CrossRef]
- Drago, L.; Clerici, P.; Morelli, I.; Ashok, J.; Benzakour, T.; Bozhkova, S.; Alizadeh, C.; Del Sel, H.; Sharma, H.K.; Peel, T.; et al. The World Association against Infection in Orthopaedics and Trauma (WAIOT) procedures for Microbiological Sampling and Processing for Periprosthetic Joint Infections (PJIs) and other Implant-Related Infections. J. Clin. Med. 2019, 8, 933. [Google Scholar] [CrossRef]
- Boettner, F.; Koehler, G.; Wegner, A.; Schmidt-Braekling, T.; Gosheger, G.; Goetze, C. The Rule of Histology in the Diagnosis of Periprosthetic Infection: Specific Granulocyte Counting Methods and New Immunohistologic Staining Techniques may Increase the Diagnostic Value. Open Orthop. J. 2016, 10, 457–465. [Google Scholar] [CrossRef][Green Version]
- Klauser, A.S.; Tagliafico, A.; Allen, G.M.; Boutry, N.; Campbell, R.; Grainger, A.; Guerini, H.; McNally, E.; O’Connor, P.J. Clinical indications for musculoskeletal ultrasound: A Delphi-based consensus paper of the European Society of Musculoskeletal Radiology. Eur. Radiol. 2012, 22, 1140–1148. [Google Scholar] [CrossRef]
- Cyteval, C.; Hamm, V.; Sarrabère, M.P.; Lopez, F.M.; Maury, P.; Taourel, P. Painful infection at the site of hip prosthesis: CT imaging. Radiology 2002, 224, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Galley, J.; Sutter, R.; Stern, C.; Filli, L.; Rahm, S.; Pfirrmann, C.W.A. Diagnosis of Periprosthetic Hip Joint Infection Using MRI with Metal Artifact Reduction at 1.5 T. Radiology 2020, 12, 191901. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.H.; Lim, D.; Kim, E.; Kim, S.; Song, H.T.; Suh, J.S. Usefulness of slice encoding for metal artifact correction (SEMAC) for reducing metallic artifacts in 3-T MRI. Magn. Reson. Imaging 2013, 31, 703–706. [Google Scholar] [CrossRef]
- Li, A.E.; Sneag, D.; Greditzer, H.G., 4th; Johnson, C.C.; Miller, T.T.; Potter, H.G. Total Knee Arthroplasty: Diagnostic Accuracy of Patterns of Synovitis at MR Imaging. Radiology 2016, 27, 152828. [Google Scholar] [CrossRef]
- Plodkowski, A.J.; Hayter, C.L.; Miller, T.T.; Nguyen, J.T.; Potter, H.G. Lamellated hyperintense synovitis: Potential MR imaging sign of an infected knee arthroplasty. Radiology 2013, 266, 256–260. [Google Scholar] [CrossRef]
- Van den Wyngaert, T.; Strobel, K.; Kampen, W.U.; Kuwert, T.; van der Bruggen, W.; Mohan, H.K.; Gnanasegaran, G.; Delgado-Bolton, R.; Weber, W.A.; Beheshti, M.; et al. EANM Bone & Joint Committee and the Oncology Committee. The EANM practice guidelines for bone scintigraphy. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1723–1738. [Google Scholar] [CrossRef]
- De Vries, E.F.; Roca, M.; Jamar, F.; Israel, O.; Signore, A. Guidelines fort the labelling of leucocytes with (99m)Tc-HMPAO. Inflammation/Infection Taskgroup of the European Association of Nuclear Medicine. Eur. J. Nucl. Med. Mol. Imaging 2010, 37, 842–848. [Google Scholar] [CrossRef]
- Roca, M.; De Vries, E.F.J.; Jamar, F.; Israel, O.; Signore, A. Guidelines for the labelling of leucocytes with 111In-oxine. Eur. J. Nucl. Med. Mol. Imaging 2010, 37, 835–841. [Google Scholar] [CrossRef]
- Signore, A.; Jamar, F.; Israel, O.; Buscombe, J.; Martin-Comin, J.; Lazzeri, E. Clinical indications, image acquisition and data interpretation for white blood cells and anti-granulocyte monoclonal antibody scintigraphy: An EANM procedural guideline. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1816–1831. [Google Scholar] [CrossRef]
- Erba, P.A.; Glaudemans, A.W.; Veltman, N.C.; Sollini, M.; Pacilio, M.; Galli, F.; Dierckx, R.A.; Signore, A. Image acquisition and interpretation criteria for 99mTc-HMPAO-labelled white blood cell scintigraphy: Results of a multicentre study. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 615–623. [Google Scholar] [CrossRef]
- Gratz, S.; Reize, P.; Kemke, B.; Kampen, W.U.; Luster, M.; Höffken, H. Targeting osteomyelitis with complete [99mTc]besilesomab and fragmented [99mTc]sulesomab antibodies: Kinetic evaluations. Q. J. Nucl. Med. Mol. Imaging 2016, 60, 413–423. [Google Scholar] [PubMed]
- Jin, H.; Yuan, L.; Li, C.; Kan, Y.; Hao, R.; Yang, J. Diagnostic performance of FDG PET or PET/CT in prosthetic infection after arthroplasty: A meta-analysis. Q. J. Nucl. Med. Mol. Imaging 2014, 58, 85–93. [Google Scholar] [PubMed]
- Gemmel, F.; van den Wyngaert, H.; Love, C.; Welling, M.M.; Gemmel, P.; Palestro, C.J. Prosthetic joint infections: Radionuclide state-of-the-art imaging. Eur. J. Nucl. Med. Mol. Imaging 2012, 39, 892–909. [Google Scholar] [CrossRef] [PubMed]
- Reinartz, P. FDG-PET in patients with painful hip and knee arthroplasty: Technical breakthrough or just more of the same. Q. J. Nucl. Med. Mol. Imaging 2009, 53, 41–50. [Google Scholar]
- Chacko, T.K.; Zhuang, H.; Stevenson, K.; Moussavia, B.; Alavi, A. The importance of the location of fluorodeoxyglucose uptake in periprosthetic infection in painful hip prostheses. Nucl. Med. Commun. 2002, 23, 851–855. [Google Scholar] [CrossRef]
- Love, C.; Marwin, S.E.; Tomas, M.B.; Krauss, E.S.; Tronco, G.G.; Bhargava, K.K.; Nichols, K.J.; Palestro, C.J. Diagnosing infection in the failed joint replacement: A comparison of coincidence detection 18F-FDG and 111In-labeled leukocyte/99mTc-sulfur colloid marrow imaging. J. Nucl. Med. 2004, 45, 1864–1871. [Google Scholar]
- Familiari, D.; Glaudemans, A.W.; Vitale, V.; Prosperi, D.; Bagni, O.; Lenza, A.; Cavallini, M.; Scopinaro, F.; Signore, A. Can sequential 18F-FDG PET/CT replace WBC imaging in the diabetic foot? J. Nucl. Med. 2011, 52, 1012–1019. [Google Scholar] [CrossRef]
- Stumpe, K.D.; Nötzli, H.P.; Zanetti, M.; Kamel, E.M.; Hany, T.F.; Görres, G.W.; von Schulthess, G.K.; Hodler, J. FDG PET for differentiation of infection and aseptic loosening in total hip replacements: Comparison with conventional radiography and three-phase bone scintigraphy. Radiology 2004, 231, 333–341. [Google Scholar] [CrossRef]
- Wenter, V.; Müller, J.P.; Albert, N.L.; Lehner, S.; Fendler, W.P.; Bartenstein, P.; Cyran, C.C.; Friederichs, J.; Militz, M.; Hacker, M.; et al. The diagnostic value of [(18)F]FDG PET for the detection of chronic osteomyelitis and implant-associated infection. Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 749–761. [Google Scholar] [CrossRef]
- Treglia, G. Diagnostic Performance of (18)F-FDG PET/CT in Infectious and Inflammatory Diseases according to Published Meta-Analyses. Contrast Media Mol. Imaging 2019, 3018349. [Google Scholar] [CrossRef]
- Thang, S.P.; Tong, A.K.; Lam, W.W.; Ng, D.C. SPECT/CT in musculoskeletal infections. Semin. Musculoskelet. Radiol. 2014, 18, 194–202. [Google Scholar] [CrossRef]
- Tam, H.H.; Bhaludin, B.; Rahman, F.; Weller, A.; Ejindu, V.; Parthipun, A. SPECT-CT in total hip arthroplasty. Clin. Radiol. 2014, 69, 82–95. [Google Scholar] [CrossRef]
- Mariani, G.; Bruselli, L.; Kuwert, T.; Kim, E.E.; Flotats, A.; Israel, O.; Dondi, M.; Watanabe, N. A review on the clinical uses of SPECT/CT. Eur. J. Nucl Med. Mol. Imaging 2010, 37, 1959–1985. [Google Scholar] [CrossRef]
- Scharf, S. SPECT/CT imaging in general orthopedic practice. Semin. Nucl. Med. 2009, 39, 293–307. [Google Scholar] [CrossRef]
- van der Bruggen, W.; Bleeker-Rovers, C.P.; Boerman, O.C.; Gotthardt, M.; Oyen, W.J. PET and SPECT in osteomyelitis and prosthetic bone and joint infections: A systematic review. Semin. Nucl. Med. 2010, 40, 3–15. [Google Scholar] [CrossRef]
- Aliprandi, A.; Sconfienza, L.M.; Randelli, P.; Bandirali, M.; Tritella, S.; Di Leo, G.; Sardanelli, F. Magnetic resonance imaging of the knee after medial unicompartmental arthroplasty. Eur. J. Radiol. 2011, 80, e416–e421. [Google Scholar] [CrossRef]
- White, L.M.; Kim, J.K.; Mehta, M.; Merchant, N.; Schweitzer, M.E.; Morrison, W.B.; Hutchison, C.R.; Gross, A.E. Complications of total hiparthroplasty: MR imaging-initial experience. Radiology 2000, 215, 254–262. [Google Scholar] [CrossRef]
- Hayter, C.L.; Koff, M.F.; Shah, P.; Koch, K.M.; Miller, T.T.; Potter, H.G. MRI after arthroplasty: Comparison of MAVRIC and conventional fast spin-echo techniques. Am. J. Roentgenol. 2011, 197, W405–W411. [Google Scholar] [CrossRef]
- He, C.; Lu, Y.; Jiang, M.; Feng, J.; Wang, Y.; Liu, Z. Clinical value of optimized magnetic resonance imaging for evaluation of patients with painful hip arthroplasty. Chin. Med. J. 2014, 127, 3876–3880. [Google Scholar]
- Gille, J.; Ince, A.; González, O.; Katzer, A.; Loehr, J.F. Single-stage revision of peri-prosthetic infection following total elbow replacement. J. Bone Joint Surg. Br. 2006, 88, 1341–1346. [Google Scholar] [CrossRef][Green Version]
- Zajonz, D.; Wuthe, L.; Tiepolt, S.; Brandmeier, P.; Prietzel, T.; von Salis-Soglio, G.F.; Roth, A.; Josten, C.; Heyde, C.E.; Zajonz, M.G. Diagnostic Work-Up Strategy for Periprosthetic Joint Infections After Total Hip and Knee Arthroplasty: A 12-year Experience on 320 Consecutive Cases. Patient Saf. Surg. 2015, 16, 20. [Google Scholar] [CrossRef]
- Niccoli, G.; Mercurio, D.; Cortese, F. Bone scan in painful knee arthroplasty: Obsolete or actual examination? Acta Biomed. 2017, 88, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, H.; Chacko, T.K.; Hickeson, M.; Stevenson, K.; Feng, Q.; Ponzo, F.; Garino, J.P.; Alavi, A. Persistent non-specific FDG uptake on PET imaging following hip arthroplasty. Eur. J. Nucl. Med. 2002, 29, 1328–1333. [Google Scholar] [CrossRef] [PubMed]
- Palestro, C.J. Nuclear medicine and the failed joint replacement: Past, present, and future. World J. Radiol. 2014, 6, 446–458. [Google Scholar] [CrossRef] [PubMed]
- Auletta, S.; Riolo, D.; Varani, M.; Lauri, C.; Galli, F.; Signore, A. Labelling and clinical performance of human leukocytes with 99mTc-HMPAO using Leukokit® with gelofusine versus Leukokit® with HES as sedimentation agent. Contrast Media Mol. Imaging 2019, 4368342. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.O.; Na, S.J.; Oh, S.J.; Jung, B.S.; Lee, S.H.; Chang, J.S.; Bin, S., II; Ryu, J.S. Usefulness of Adding SPECT/CT to 99mTc-Hexamethylpropylene Amine Oxime (HMPAO)-labeled Leukocyte Imaging for Diagnosing Prosthetic Joint Infections. J. Comput. Assist. Tomogr. 2014, 38, 313–319. [Google Scholar] [CrossRef]
- El Espera, I.; Blondet, C.; Moullart, V.; Saïdi, L.; Havet, E.; Mertl, P.; Canarelli, B.; Schmit, J.-L.; Meyer, M.-E. The Usefulness of 99mTc Sulfur Colloid Bone Marrow Scintigraphy Combined With 111In Leucocyte Scintigraphy in Prosthetic Joint Infection. Nucl. Med. Commun. 2004, 25, 171–175. [Google Scholar] [CrossRef]
- Aksoy, S.Y.; Asa, S.; Ozhan, M.; Ocak, M.; Sager, M.S.; Erkan, M.E.; Halac, M.; Kabasakal, L.; Sönmezoglu, K.; Kanmaz, B. FDG and FDG-labelled leucocyte PET/CT in the imaging of prosthetic joint infection. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 556–564. [Google Scholar] [CrossRef]
- Teiler, J.; Ahl, M.; Åkerlund, B.; Wird, S.; Brismar, H.; Bjäreback, A.; Hedlund, H.; Holstensson, M.; Axelsson, R. Is 99mTc-HMPAO-leukocyte Imaging an Accurate Method in Evaluating Therapy Result in Prosthetic Joint Infection and Diagnosing Suspected Chronic Prosthetic Joint Infection? Q. J. Nucl. Med. Mol. Imaging 2020, 64, 85–95. [Google Scholar] [CrossRef]
- Kwee, T.C.; Kwee, R.M.; Alavi, A. FDG-PET for diagnosing prosthetic joint infection: Systematic review and metaanalysis. Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 2122–2132. [Google Scholar] [CrossRef]
- Basu, S.; Kwee, T.C.; Saboury, B.; Garino, J.P.; Nelson, C.N.; Zhuang, H.; Parsons, M.; Chen, W.; Kumar, R.; Salavati, A.; et al. FDG-PET for diagnosing infection in hip and knee prostheses: Prospective study in 221 prostheses and subgroup comparison with combined 111In-labeled leukocyte/99mTc- sulfur colloid bone marrow imaging in 88 prostheses. Clin. Nucl. Med. 2014, 39, 609–615. [Google Scholar] [CrossRef] [PubMed]
- Van Acker, F.; Nuyts, J.; Maes, A.; Vanquickenborne, B.; Stuyck, J.; Bellemans, J.; Vleugels, S.; Bormans, G.; Mortelmans, L. FDG-PET, 99mTc-HMPAO white blood cell SPET and bone scintigraphy in the evaluation of painful total knee arthroplasties. Eur. J. Nucl. Med. 2001, 28, 1496–1504. [Google Scholar] [CrossRef] [PubMed]
- Kiran, M.; Donnelly, T.D.; Armstrong, C.; Kapoor, B.; Kumar, G.; Peter, V. Diagnostic utility of fluorodeoxyglucose positron emission tomography in prosthetic joint infection based on MSIS criteria. Bone Jt. J. 2019, 101-B, 910–914. [Google Scholar] [CrossRef] [PubMed]
- Falstie-Jensen, T.; Lange, J.; Daugaard, H.; Vendelbo, M.H.; Sørensen, A.K.; Zerahn, B.; Ovesen, J.; Søballe, K.; Gormsen, L.C.; ROSA study-group. 18F FDG-PET/CT has poor diagnostic accuracy in diagnosing shoulder PJI. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2013–2022. [Google Scholar] [CrossRef] [PubMed]
- Falstie-Jensen, T.; Daugaard, H.; Søballe, K.; Ovesen, J.; Arveschoug, A.K.; Lange, J.; ROSA study group. Labeled white blood cell/bone marrow single-photon emission computed tomography with computed tomography fails in diagnosing chronic periprosthetic shoulder joint infection. J. Shoulder Elbow Surg. 2019, 28, 1040–1048. [Google Scholar] [CrossRef]
- Blanc, P.; Bonnet, E.; Giordano, G.; Monteil, J.; Salabert, A.-S.; Payou, P. The use of labelled leucocyte scintigraphy to evaluate chronic periprosthetic joint infections: A retrospective multicentre study on 168 patients. Eur. J. Clin. Microbiol. Infect. Dis. 2019, 38, 1625–1631. [Google Scholar] [CrossRef]
- Liberatore, M.; AL-Nahhas, A.; Rubello, D. White blood cell scan in the follow-up of infectious diseases: Is the withdrawal of antibiotic therapy necessary? Nucl. Med. Commun. 2007, 28, 151–153. [Google Scholar] [CrossRef]
- Govaert, G.A.M.; Bosch, P.; IJpma, F.F.A.; Glauche, J.; Jutte, P.C.; Lemans, J.V.C.; Wendt, K.W.; Reininga, I.H.F.; Glaudemans, A.W.J.M. High diagnostic accuracy of white blood cell scintigraphy for fracture related infections: Results of a large retrospective single-center study. Injury 2018, 49, 1085–1090. [Google Scholar] [CrossRef]
- Auletta, S.; Galli, F.; Lauri, C.; Martinelli, D.; Santino, I.; Signore, A. Imaging bacteria with radiolabelled quinolones, cephalosporins and siderophores for imaging infection: A systematic review. Clin. Transl. Imaging 2016, 4, 229–252. [Google Scholar] [CrossRef]
- Auletta, S.; Varani, M.; Horvat, R.; Galli, F.; Signore, A.; Hess, S. PET Radiopharmaceuticals for Specific Bacteria Imaging: A Systematic Review. J. Clin. Med. 2019, 8, 197. [Google Scholar] [CrossRef]
- Xing, D.; Ma, X.; Ma, J.; Wang, J.; Chen, Y.; Yang, Y. Use of Anti-Granulocyte Scintigraphy With 99mTc-labeled Monoclonal Antibodies for the Diagnosis of Periprosthetic Infection in Patients After Total Joint Arthroplasty: A Diagnostic Meta-Analysis. PLoS ONE 2013, 26, e69857. [Google Scholar] [CrossRef] [PubMed]
- Trevail, C.; Ravindranath-Reddy, P.; Sulkin, T.; Bartlett, G. An evaluation of the role of nuclear medicine imaging in the diagnosis of periprosthetic infections of the hip. Clin Radiol. 2016, 71, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, S.S.; Shaker, A.; Saffarini, M.; Chen, A.F.; Hirschmann, M.T.; Kohl, S. Accuracy of diagnostic tests for prosthetic joint infection: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 3064–3074. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Ledezma, C.; Lamberton, C.; Lichstein, P.; Parvizi, J. Diagnosis of Periprosthetic Joint Infection: The Role of Nuclear Medicine May Be Overestimated. J. Arthroplasty. 2015, 30, 1044–1049. [Google Scholar] [CrossRef]
- Sousa, R.; Massada, M.; Pereira, A.; Fontes, F.; Amorim, I.; Oliveira, A. Diagnostic Accuracy of Combined 99mTc-sulesomab and 99mTc-nanocolloid Bone Marrow Imaging in Detecting Prosthetic Joint Infection. Nucl. Med. Commun. 2011, 32, 834–839. [Google Scholar] [CrossRef]
- Gratz, S.; Reize, P.; Pfestroff, A.; Höffken, H. Intact Versus Fragmented 99mTc-monoclonal Antibody Imaging of Infection in Patients With Septically Loosened Total Knee Arthroplasty. J. Int. Med. Res. 2012, 40, 1335–1342. [Google Scholar] [CrossRef]
- Bhoil, A.; Caw, H.; Vinjamuri, S. Role of 18F-flurodeoxyglucose in orthopaedic implant-related infection: Review of literature and experience. Nucl. Med. Commun. 2019, 40, 875–887. [Google Scholar] [CrossRef]
- Zoccali, C.; Teori, G.; Salducca, N. The Role of FDG-PET in Distinguishing Between Septic and Aseptic Loosening in Hip Prosthesis: A Review of Literature. Int. Orthop. 2009, 33, 1–5. [Google Scholar] [CrossRef]
- Khalid, V.; Schønheyder, H.C.; Larsen, L.H.; Nielsen, P.T.; Kappel, A.; Thomsen, T.R.; Aleksyniene, R.; Lorenzen, J.; Ørsted, I.; Simonsen, O.; et al. Multidisciplinary Diagnostic Algorithm for Evaluation of Patients Presenting with a Prosthetic Problem in the Hip or Knee: A Prospective Study. Diagnostics 2020, 11, 98. [Google Scholar] [CrossRef]
- Savarino, L.; Tigani, D.; Baldini, N.; Bochicchio, V.; Giunti, A. Pre-operative diagnosis of infection in total knee arthroplasty: An algorithm. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 667–675. [Google Scholar] [CrossRef]
- Volpe, L.; Indelli, P.F.; Latella, L.; Poli, P.; Yakupoglu, J.; Marcucci, M. Periprosthetic joint infections: A clinical practice algorithm. Joints 2015, 13, 169–174. [Google Scholar] [CrossRef]
- Plate, A.; Weichselbaumer, V.; Schüpbach, R.; Fucentese, S.F.; Berli, M.; Hüllner, M.; Achermann, Y. Diagnostic Accuracy of 99 m Tc-antigranulocyte SPECT/CT in Patients With Osteomyelitis and Orthopaedic Device-Related Infections: A Retrospective Analysis. Int. J. Infect. Dis. 2020, 91, 79–86. [Google Scholar] [CrossRef] [PubMed]
- Graute, V.; Feist, M.; Lehner, S.; Haug, A.; Müller, P.E.; Bartenstein, P.; Hacker, M. Detection of Low-Grade Prosthetic Joint Infections Using 99mTc-antigranulocyte SPECT/CT: Initial Clinical Results. Eur. J. Nucl. Med. Mol. Imaging 2010, 37, 1751–1759. [Google Scholar] [CrossRef]
- Delank, K.-S.; Schmidt, M.; Michael, J.W.-P.; Dietlein, M.; Schicha, H.; Eysel, P. The Implications of 18F-FDG PET for the Diagnosis of Endoprosthetic Loosening and Infection in Hip and Knee Arthroplasty: Results from a Prospective, Blinded Study. BMC Musculoskelet Disord. 2006, 3, 7–20. [Google Scholar] [CrossRef]
- Stumpe, K.D.; Romero, J.; Ziegler, O.; Kamel, E.M.; von Schulthess, G.K.; Strobel, K.; Hodler, J. The value of FDG-PET in patients with painful total knee arthroplasty. Eur. J. Nucl. Med. Mol. Imaging 2006, 33, 1218–1225. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pill, S.G.; Parvizi, J.; Tang, P.H.; Garino, J.P.; Nelson, C.; Zhuang, H.; Alavi, A. Comparison of Fluorodeoxyglucose Positron Emission Tomography and (111)indium-white Blood Cell Imaging in the Diagnosis of Periprosthetic Infection of the Hip. J. Arthroplast. 2006, 21, 91–97. [Google Scholar] [CrossRef] [PubMed]
- Verberne, S.J.; Raijmakers, P.G.; Temmerman, O.P. The Accuracy of Imaging Techniques in the Assessment of Periprosthetic Hip Infection: A Systematic Review and Meta-Analysis. J. Bone Jt. Surg. Am. 2016, 5, 1638–1645. [Google Scholar] [CrossRef]
- Filippi, L.; Schillaci, O. Usefulness of Hybrid SPECT/CT in 99mTc-HMPAO-labeled Leukocyte Scintigraphy for Bone and Joint Infections. J. Nucl. Med. 2006, 47, 1908–1913. [Google Scholar]
| Definition Source | MSIS 2011 | IDSA 2013 | ICM 2013 | ICM 2018 | Proposed EBJIS 2018 |
|---|---|---|---|---|---|
| Scoring System | 1 of the 2 major criteria OR ≥4 of 6 minor criteria 1 | ≥1 positive criteria 2 | 1 of the 2 major criteria OR ≥3 of 5 minor criteria 3 | 1 of the 2 major criteria OR minor criteria scoring ≥6 infected 3–5 possibly infected (“consider further molecular diagnostics such as next-generation sequencing”) <3 not infected 4 | ≥1 positive criteria |
| Criteria | Major:
|
| Major:
| Major:
|
|
| No Infection | Contamination | BIM | LG-PJI | HG-PJI | |
|---|---|---|---|---|---|
| Clinical presentation | One or more condition(s), other than infection, can cause the symptoms or the reason for reoperation (e.g., wear debris, metallosis, recurrent dislocation or joint instability, fracture, malposition, neuropathic pain) | One or more of the following: otherwise “unexplained” pain, swelling, stiffness | Two or more of the following: pain, swelling, redness, warmth, functio laesa | ||
| (Number of positive rule IN tests)-(number of negative rule OUT tests) | <0 | <0 | <0 | ≥0 | ≥1 |
| Post-operatively confirmed if | Negative cultural examination | One pre- or intra-operative positive culture, with negative histology | Positive cultural examination (preferably with antibiofilm techniques) and/or positive histology | ||
| Rule OUT Tests (Sensitivity > 90%) EACH NEGATIVE TEST Scores − 1 (Positive Rule OUT Test Score 0) | |||||
| Serum | ESR (>30 mm/h) CRP (>10 mg/L) | ||||
| Synovial fluid | WBC (>1500/μL) LE (++) Alpha-defensin immunoassay (>5.2 mg/L) | ||||
| Imaging | 99mTc bone scan | ||||
| Rule IN Tests (Specificity > 90%) EACH POSITIVE TEST Scores + 1 (Negative Rule IN Test Score 0) | |||||
| Clinical examination | Purulence or draining sinus or exposed joint prosthesis | ||||
| Serum | IL-6 (>10 pg/mL) PC (>0.5 ng/mL) D-Dimer (>850 ng/mL) | ||||
| Synovial fluid | Cultural examination WBC (>3000/mL) LE (++) Alpha-defensin immunoassay (>5.2 mg/L) or lateral flow test | ||||
| Imaging | Radio-labelled leukocyte scintigraphy (if necessary, with combined bone marrow scintigraphy) | ||||
| Histology | Frozen section (5 neutrophils in at least 3 HPFs) | ||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romanò, C.L.; Petrosillo, N.; Argento, G.; Sconfienza, L.M.; Treglia, G.; Alavi, A.; Glaudemans, A.W.J.M.; Gheysens, O.; Maes, A.; Lauri, C.; et al. The Role of Imaging Techniques to Define a Peri-Prosthetic Hip and Knee Joint Infection: Multidisciplinary Consensus Statements. J. Clin. Med. 2020, 9, 2548. https://doi.org/10.3390/jcm9082548
Romanò CL, Petrosillo N, Argento G, Sconfienza LM, Treglia G, Alavi A, Glaudemans AWJM, Gheysens O, Maes A, Lauri C, et al. The Role of Imaging Techniques to Define a Peri-Prosthetic Hip and Knee Joint Infection: Multidisciplinary Consensus Statements. Journal of Clinical Medicine. 2020; 9(8):2548. https://doi.org/10.3390/jcm9082548
Chicago/Turabian StyleRomanò, Carlo Luca, Nicola Petrosillo, Giuseppe Argento, Luca Maria Sconfienza, Giorgio Treglia, Abass Alavi, Andor W.J.M. Glaudemans, Olivier Gheysens, Alex Maes, Chiara Lauri, and et al. 2020. "The Role of Imaging Techniques to Define a Peri-Prosthetic Hip and Knee Joint Infection: Multidisciplinary Consensus Statements" Journal of Clinical Medicine 9, no. 8: 2548. https://doi.org/10.3390/jcm9082548
APA StyleRomanò, C. L., Petrosillo, N., Argento, G., Sconfienza, L. M., Treglia, G., Alavi, A., Glaudemans, A. W. J. M., Gheysens, O., Maes, A., Lauri, C., Palestro, C. J., & Signore, A. (2020). The Role of Imaging Techniques to Define a Peri-Prosthetic Hip and Knee Joint Infection: Multidisciplinary Consensus Statements. Journal of Clinical Medicine, 9(8), 2548. https://doi.org/10.3390/jcm9082548











