Abstract
Healthcare resource utilization peaks throughout the first year following acute myocardial infarction (AMI). Data linking the former and outcomes are sparse. We evaluated the associations between subsequent length of in-hospital stay (SLOS) and primary ambulatory visits (PAV) within the first year after AMI and long-term mortality. This retrospective analysis included patients who were discharged following an AMI. Study groups: low (0–1 days), intermediate (2–7) and high (≥8 days) SLOS; low (<10) and high (≥10 visits) PAV, throughout the first post-AMI year. All-cause mortality was set as the primary outcome. Overall, 8112 patients were included: 55.2%, 23.4% and 21.4% in low, intermediate and high SLOS groups respectively; 26.0% and 74.0% in low and high-PAV groups. Throughout the follow-up period (up to 18 years), 49.6% patients died. Multivariable analysis showed that an increased SLOS (Hazard ratio (HR) = 1.313 and HR = 1.714 for intermediate and high vs. low groups respectively) and a reduced number of PAV (HR = 1.24 for low vs. high groups) were independently associated with an increased risk for mortality (p < 0.001 for each). Long-term mortality following AMI is associated with high hospital and low primary ambulatory services utilization throughout the first-year post-discharge. Measures focusing on patients with increased SLOS and reduced PAV should be considered to improve patient outcomes.
1. Introduction
Throughout the past few decades, dramatic changes have been introduced to most aspects of acute myocardial infarction (AMI) management, resulting in significant improvement of patient outcomes [1,2,3,4,5]. However, AMI survivors continue to be at excessive risk of long-term morbidity and mortality as well as of increased healthcare resource utilization and economic burden, particularly in the first year following the index event [6,7,8,9]. Risk stratification of AMI survivors could improve long-term outcomes and target allocation of resources. Identification of risk factors for long-term outcomes after AMI have focused mainly on data available at the time of the initial hospitalization for AMI [10,11]. Wang et al. [12] recently showed that in-hospital admissions after AMI were associated with the risk of a subsequent AMI.
Data evaluating the associations between healthcare resource utilization following AMI and mortality are scant. The aim of the current study was to evaluate the association between length of stay of subsequent hospitalizations (SLOS) and the number of primary ambulatory clinic visits (PAV) during the first post-AMI year and long-term mortality.
2. Materials and Methods
2.1. Study Population
This retrospective observational study evaluated patients who were admitted with and survived an AMI from 1.1.2002 through 12.31.2012 to a tertiary medical center (Soroka University Medical Center) in Southern Israel. Patients were excluded due to the following criteria: (1) death during the index AMI admission or during the first year after discharge; (2) not citizens of the State of Israel, (3) insured by neither Maccabi Healthcare Services nor Clalit Health Services (the two largest health plans in Israel) and (4) recurrent hospitalizations for AMI during the study period (only the first AMI admission (index admission) was included).
The local ethics committees approved the study (Soroka University Medical Center, Maccabi Healthcare Services and Clalit Health Services, identifiers; SOR-0167-12, 28/2014, COM-0071-13, respectively), which was performed in accordance with the Helsinki declaration. Exemption from informed consent was granted and personal details of investigated patients remained confidential.
2.2. Data Sources and Classifications
We obtained the data from the electronic medical records of the Soroka University Medical Center, Maccabi Healthcare Services and Clalit Health Services. Mortality data were obtained from the Ministry of the Interior population registry. Individual patient-level data from the different databases were linked using the unique personal identification number, followed by coding into a study identification number prior to further data processing.
The baseline data included demographics and clinical characteristics of the index hospitalizations (comorbidities, type of AMI, work-up as well as interventions administered for the AMI), as previously reported for the Soroka Acute Myocardial Infarction (SAMI) project [10,13].
The diagnosis of AMI was based on the international Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes: ST-elevation AMI (STEMI) 410.0*–410.6* and Non-ST-elevation AMI (NSTEMI) 410.7*–410.9*. Grouping of diseases and interventions were based on ICD-9-CM discharge codes [10,13].
Adherence with the following guideline-recommended medical therapy was evaluated: Aspirin, Statins, Beta blockers, Angiotensin-converting enzyme (ACE) inhibitors or Angiotensin II receptor blockers (ARBs). The adherence was calculated as the rate of issued monthly prescriptions throughout the first year following hospital discharge. Patients with an adherence of 80% or more for all the evaluated medication groups were classified as adherent while the rest were classified as non-adherent [14,15,16]. Based on previous reports, a one-year adherence interval (as applied herein) reflects the adherence plateau, beyond which adherence leveled off [17,18].
2.3. Healthcare Services Utilization and the Study Groups
Data regarding hospitalizations and primary ambulatory services utilization during the first year after discharge were obtained from the databases of the two health plans [19,20]. All-cause subsequent hospitalizations and their length (SLOS) and number of PAV were quantified. The SLOS groups were defined as: low hospital utilization (0–1 days); intermediate utilization (2–7 days) and high utilization (>8 days). In addition, the number of PAV were divided into four equally sized groups (quartiles) followed by their merging into two groups according to the strength of the univariate association with the dependent variable. Thus, two groups of primary ambulatory healthcare services utilization were created in accordance with the number of PAV: <10 visits (low utilization) and ≥10 visits (high utilization).
2.4. Propensity Scores
We calculated propensity scores or predicted probabilities of the healthcare services utilization (SLOS and PAV) based on a set of relevant patient characteristics using a two-step procedure: (1) the parameters (SLOS and PAV) were modeled as the outcome variables in a general linear model included as predictor variables a selected covariates that were identified as key confounders and (2) predicted probabilities of SLOS and PAV (“propensity scores”) were used as covariates in the final regression model (propensity score adjustment).
A total of 34 covariates (including age, sex, nationality, cardiovascular risk factors, other comorbidities, type of AMI, type of treatment and compliance with the medications) were initially included in the propensity score model. Of those, 23 variables consisted of the propensity scores.
2.5. Follow-Up and Outcomes
Follow-up started from the second year (≥day 366 following the date of the discharge from the index hospitalization) and continued up to 18 years (or till 7.1.2020). The primary outcome was all-cause mortality.
2.6. Statistical Analysis
Statistical analysis was performed using IBM SPSS 26 (SPSS Inc., Chicago, IL, USA) Statistics software. Patient characteristics were presented as mean and standard deviation (SD) for continuous variables and numbers (n) and percent (%) for the categorical data. In addition, SLOS and PAV parameters were presented as median and inter-quartile range (IQR). The comparison of baseline characteristics between the study groups was performed using Chi-square test/Chi-square test for linear trend for categorial variables and Student’s t-test/analysis of variance (ANOVA) for linear trend for continuous variables for PAV and SLOS categories respectively. The comparison of outcomes between the study groups was performed using the survival approach. The univariate analysis compared the risk of mortality with the creation of survival functions (Kaplan–Meier) using the Log-rank test. In addition, we used Cox regression analysis to estimate the relative risk of long-term mortality for the study groups. Four models were built: the first and second models were the univariate models which included the variables of SLOS and PAV (a separate model for each). The third model included the variables of SLOS and PAV together. Finally, the forth model included these above variables and the investigated baseline characteristics which were statistically related to the outcome and the propensity scores. The results of the models were presented as the regression coefficients (B) and their standard errors (SE), hazard ratios (HR) and 95% Confidence intervals (CI) for HR. For each test, p < 0.05 was considered as statistically significant.
3. Results
3.1. Study Population and Groups
Overall, 8112 of 12,503 post-AMI patients were included in the current study. The reasons patients were excluded were as follows: death during the index AMI admission or during the first year after discharge (n = 1931), not citizens of the State of Israel (n = 414) and not insured by Maccabi Healthcare Services or Clalit Health Services (n = 2046). The mean SLOS was 5.98 (SD = 15.5) days, median 1 day (IQR: 0–6); 4068 (50.2%) of patients were admitted to hospital for one day or longer throughout the first year after the index hospitalization.
The mean SLOS of patients hospitalized for one day or more throughout the first post-AMI year was 11.9 (SD = 20.3) days, a median of 6 days (IQR: 3–13). There were 4474 (55.2%) patients included in the low hospital services utilization group; 1899 (23.4%) in the intermediate hospital services utilization group; and 1739 (21.4%) in the high hospital services utilization group.
A total of 7938 (97.9%) patients has at least one PAV throughout the first follow-up year, with a mean of 18.7 (SD = 12.2), a median of 17 (IQR: 10–25) visits. The distribution according to the number of PAV was as following: 2111 (26%) patients were included in the group of low ambulatory services utilization and the rest, consisting of 6001 (74%) patients, comprised the high ambulatory utilization group. A negative significant association between the SLOS and the number of PAV was found (p < 0.001).
Table 1 displays patient characteristics according to the groups of SLOS and the number of PAV throughout the first year following AMI. Greater SLOS was associated with increased patient age, while greater number of PAV was related to a mildly reduced age. Male patients had lower SLOS with no difference between the sexes in PAV. The minorities (Arabs) were characterized by lower PAV compared with Jews, with no significant differences in SLOS between these groups. Higher utilization of both services was associated with an increased prevalence of cardiovascular risk factors, except smoking and family history of cardiovascular diseases. Congestive heart failure as well as most non-cardiovascular comorbidities were also more prevalent among patients with greater SLOS and PAV. Presentation as STEMI tended to be more prevalent among patients with higher SLOS and PAV (borderline significance for the latter). In-hospital stay of 7 days or more at the index admission was associated with greater SLOS and PAV. Patients who underwent percutaneous coronary intervention (PCI) and those who underwent coronary artery bypass graft surgery (CABG) had reduced SLOS but greater PAV. Higher adherence to guideline-recommended medical therapy throughout the first year was observed in patients with lower SLOS and a greater number of PAV (p < 0.001 for each, see also Table S1).

Table 1.
Baseline characteristics and mortality data of the patients by the groups of length of stay of subsequent hospitalizations (SLOS) and number of primary ambulatory visits (PAV) throughout the first year following acute myocardial infarction (AMI).
Abbreviates: SLOS, Length of stay of subsequent hospitalizations; PAV, Primary ambulatory visits; SD, standard deviation; CIHD, Chronic ischemic heart disease; PVD, Peripheral vascular disease; IHD, Ischemic heart disease; COPD, Chronic obstructive pulmonary disease; AMI, Acute myocardial infarction; STEMI, ST segment elevation myocardial infarction; ICCU, Intensive cardiac care unit; LOS, Length of stay; PCI, Percutaneous coronary intervention; CABG, Coronary artery bypass surgery; LV, Left ventricular.
3.2. Follow-Up and Outcomes
The follow-up lasted from 366 up to 6575 days (18 years) post-hospital discharge with a median follow-up of 3334 days (9.1 years). During the follow-up period, 4021 (49.6%) patients died with a cumulative mortality of 0.63. Mortality data and survival curves according to healthcare services utilization are presented in Table 1 and Figure 1. Higher SLOS was significantly associated with increased mortality while the opposite association was found with PAV (p < 0.001 for each).
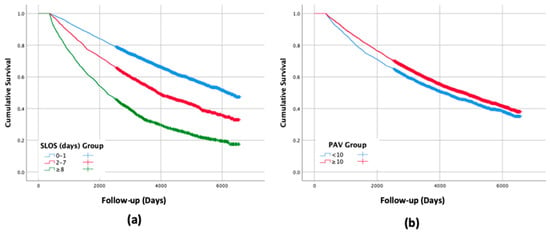
Figure 1.
Survival curves for long-term mortality by the groups of: (a) Length of stay of subsequent hospitalizations (SLOS); (b) Number of and primary ambulatory visits (PAV) throughout the first year following acute myocardial infarction (AMI) (p < 0.001 for each). Abbreviates: SLOS—Length of stay of subsequent hospitalizations, PAV—Primary ambulatory visits.
3.3. Univariate Analysis
The results of the univariate models (Table 2, models a and b) showed an increased risk of approximately 1.7 and 3.0 for long-term mortality in the groups of intermediate and the high hospital healthcare services utilization group respectively as compared with the group of low utilization. In contrast, high primary ambulatory services utilization was associated with approximately 1.2 decreased risk of mortality.

Table 2.
Relationships between length of stay of subsequent hospitalizations (SLOS) and number of and primary ambulatory visits (PAV) throughout the first year following acute myocardial infarction (AMI) and the risk of long-term all-cause mortality: (a) this model included only SLOS variables; (b) this model included only PAV variables; (c) this model included both SLOS and PAV variables; and (d) this model included both SLOS and PAV variables adjusted for the investigated baseline characteristics and propensity scores.
3.4. Multivariable Analysis
The results of the univariate analysis were consistent with the findings of the multivariable models before (Table 2, model c) and after (Table 2, model d) adjustment for potential confounders. The results of the multivariable models have shown that increased SLOS (HR ~ 1.3. and 1.7 for intermediate and high as compared with low SLOS group) and reduced number of PAV (HR ~ 1.2 for low as compared with high PAV group) were significantly associated with increased risk of mortality (p < 0.001 for each). Most of the investigated comorbidities (age, heart diseases, cardiovascular and non-cardiovascular risk factors) were associated with an increased risk of long-term mortality (except for “family history of ischemic heart disease” which had a negative association with the outcome). Additionally, invasive treatment of AMI (PCI and CABG) seems to be related with a lower risk of dying.
4. Discussion
In the current study, from a large Israeli hospital combined with ambulatory data, we evaluated the association between the extent of healthcare resource utilization during the first year following AMI and long-term survival. The main findings include a significant, independent, dose-response like association between the extent of hospital healthcare services utilization and long-term all-cause mortality. Furthermore, a significant reverse association was found between primary ambulatory services utilization throughout first year and long-term mortality.
Various studies have consistently shown that healthcare services utilization are highest throughout the first year following an AMI [7,8,9,21,22]. The association between hospital readmission following AMI and worse subsequent outcomes has been previously reported and is consistent with our findings regarding SLOS and outcomes [23,24,25]. However, our study adds to the current knowledge by (1) evaluating SLOS, though obviously associated with readmissions, focusing on the total time spent in the hospital rather than just the number of readmissions and (2) focusing on a long period of time (a year) following AMI and a relatively long follow-up period for the outcome.
Several potential mechanisms could explain our findings. It is plausible that increased SLOS, as previously reported for readmissions, results at least partially from increased co-morbidity as well as worse outcomes following the index AMI (i.e., reduced left ventricular function) [26,27]. Although we adjusted for many of these confounders, it is still possible that additional unaccounted confounders or an underappreciation of the severity of some of the existing confounders could explain our findings. An additional explanation for our findings could be the post-discharge management of these AMI patients. Better post-discharge management and better compliance are associated with improved patient outcomes [15,16,17,28,29,30,31].
We believe that our finding of a reverse association between ambulatory visits and mortality strongly supports the latter explanation since low (especially very low) numbers of such ambulatory visits probably represents, to some extent, undertreatment and reduced compliance. Furthermore, we have actually shown the latter associated in the current study: increased compliance with guideline-recommended medical therapy throughout the first year was associated with a higher number of primary care visits and reduced SLOS. Furthermore, the common reasons for subsequent hospitalizations throughout the first year following AMI (e.g., diabetes mellitus, anemia, heart failure, pneumonia, gastrointestinal hemorrhage, renal failure, and complications of an implant or graft) have been shown to be associated with increased risk of major cardiovascular events [12,32]. Moreover, hospitalizations themselves could actually be a risk factor for negative outcomes and mortality, mediated by an increased risk of infections, stress, inflammation and depression [12].
Interestingly, we found that male patients had lower SLOS compared with females, yet the PAVs were similar between the sexes. Is seems that the most plausible reason for these findings is the significant age difference between the sexes (with females approximately eight years older than male patients) as a strong positive association between age and SLOS (but not PAV) was observed. Nevertheless, sex-related disparities in other characteristics and in in-hospital and post-discharge management of AMI patients were previously described and could, at least partially, explain reduced hospital referral and admission (both self-referral and referral by caregivers [33,34].
Limitations
Several limitations of the current study should be mentioned. First, this is a single center (single country) retrospective observational study which shares the limitations of such a design and could have limited external validity. Second, we did not differentiate cardiovascular versus non-cardiovascular-related healthcare services utilization and causes of mortality. Third, we used administrative data which may be subject to recording bias. Fourth, private visits or even hospitalizations which were paid by patients out of their own pocket were not accounted for. Fifth, we did not evaluate the potential causality between SLOS and mortality. Sixth, evaluating long-term outcomes, we excluded patients who died throughout the first year, hence the observed associations are not applicable to this subgroup. Furthermore, the choice of one year for SLOS and PAV, although based on previous reports of peaks in healthcare services utilization, is somewhat arbitrary and might not necessarily represent the optimal predictive period following admission. Seventh, the current study did not include citizens from relatively small insurers (< 20%) and patients who were not Israeli citizens. Although this could be a potential source of bias, all insurers (plans) in Israel must by law accept citizens regardless of any preexisting conditions or health status and provide relatively similar coverage regarding the investigated services, hence this is unlikely to significantly bias our findings. Eighth, adherence rates were calculated based on computerized dispensing records which might not fully represent actual medication taking. However, using computerized records diminished the possibility of recall or self-reporting bias. Finally, we did not collect information regarding the rate of administration and adherence with dual anti-platelet therapy.
5. Conclusions and Clinical Implications
The current study demonstrated a potential, “dose-response like” association between SLOS throughout one-year following AMI and long-term all-cause mortality. Furthermore, a reverse association was found between the number of PAV throughout the first year and long-term mortality. The findings of this study suggest that clinicians should focus on patients with subsequent admissions and those with reduced primary care visits following AMI, in order to identify the patient-specific reasons for these negative prognostic factors, followed by custom-tailored interventions (e.g., increase PAVs and secondary prevention measures) to improve patient outcomes. Furthermore, our findings can assist decision makers and healthcare providers in long-term risk stratification of AMI survivors. Moreover, continuity of care and optimal transfer of medical information between the primary care facilities and hospitals are important to enable recognition of targets and interventions to improve long-term outcomes.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/9/8/2528/s1, Table S1: Adherence to the guideline-recommended medical therapy during the first year of the follow-up.
Author Contributions
Y.P., D.G., H.G., A.S. and J.E.A. contributed to the conception and design of the work. Y.P. contributed to the acquisition and analysis of data for the work, A.S. and H.G. contributed to data interpretation. A.S., Y.P. and H.G. drafted the manuscript. D.G. and J.E.A. critically revised the manuscript. All gave final approval and agreed to be accountable for all aspects of work ensuring integrity and accuracy. All authors have read and agreed to the published version of the manuscript.
Funding
The work was supported by research grants from Maccabi Institute for Health Services Research and The Israel National Institute for Health Policy Research.
Acknowledgments
We are indebted to Asaf Cohen, Maccabi Institute for Health Services Research for his assistance on data preparation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Peterson, E.D.; Shah, B.R.; Parsons, L.; Pollack, C.V., Jr.; French, W.J.; Canto, J.G.; Gibson, C.M.; Rogers, W.J.; NRMI Investigator. Trends in quality of care for patients with acute myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am. Heart J. 2008, 156, 1045–1055. [Google Scholar] [CrossRef] [PubMed]
- Braunwald, E.; Antman, E.M.; Beasley, J.W.; Califf, R.M.; Cheitlin, M.D.; Hochman, J.S.; Jones, R.H.; Kereiakes, D.; Kupersmith, J.; Levin, T.N.; et al. ACC/AHA 2002 guideline update for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction—Summary article: A report of the American College of Cardiology/American Heart Association task force on practice guidelines (Committee on the Management of Patients with Unstable Angina). J. Am. Coll. Cardiol. 2002, 40, 1366–1374. [Google Scholar] [CrossRef] [PubMed]
- Kushner, F.G.; Hand, M.; Smith, S.C., Jr.; King, S.B., III; Anderson, J.L.; Antman, E.M.; Bailey, S.R.; Bates, E.R.; Blankenship, J.C.; Casey, D.E., Jr.; et al. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update) a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2009, 54, 2205–2241. [Google Scholar] [CrossRef] [PubMed]
- Plakht, Y.; Gilutz, H.; Shiyovich, A. Temporal trends in acute myocardial infarction: What about survival of hospital survivors? Disparities between STEMI & NSTEMI remain. Soroka acute myocardial infarction II (SAMI-II) project. Int. J. Cardiol. 2016, 203, 1073–1081. [Google Scholar] [CrossRef] [PubMed]
- Plakht, Y.; Gilutz, H.; Shiyovich, A. Excess long-term mortality among hospital survivors of acute myocardial infarction. Soroka Acute Myocardial Infarction (SAMI) project. Public Health 2017, 143, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Yang, E.; Stokes, M.; Johansson, S.; Mellström, C.; Magnuson, E.; Cohen, D.J.; Hunt, P. Clinical and economic outcomes among elderly myocardial infarction survivors in the United States. Cardiovasc. Ther. 2016, 34, 450–459. [Google Scholar] [CrossRef]
- Janzon, M.; Henriksson, M.; Hasvold, P.; Hjelm, H.; Thuresson, M.; Jernberg, T. Long-term resource use patterns and healthcare costs after myocardial infarction in a clinical practice setting: Results from a contemporary nationwide registry study. Eur. Heart J. Qual. Care Clin. Outcomes 2016, 2, 291–298. [Google Scholar] [CrossRef]
- Etemad, L.R.; McCollam, P.L. Total first-year costs of acute coronary syndrome in a managed care setting. J. Manag. Care Spec. Pharm. 2005, 11, 300–306. [Google Scholar] [CrossRef]
- Zhao, Z.; Winget, M. Economic burden of illness of acute coronary syndromes: Medical and productivity costs. BMC Health Serv. Res. 2011, 11, 35. [Google Scholar] [CrossRef]
- Plakht, Y.; Shiyovich, A.; Weitzman, S.; Fraser, D.; Zahger, D.; Gilutz, H. A new risk score predicting 1- and 5-year mortality following acute myocardial infarction Soroka Acute Myocardial Infarction (SAMI) Project. Int. J. Cardiol. 2012, 154, 173–179. [Google Scholar] [CrossRef]
- Shore, S.; Jones, P.G.; Maddox, T.M.; Bradley, S.M.; Stolker, J.M.; Arnold, S.V.; Parashar, S.; Peterson, P.; Bhatt, D.L.; Spertus, J.; et al. Longitudinal persistence with secondary prevention therapies relative to patient risk after myocardial infarction. Heart 2015, 101, 800–807. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Leifheit, E.; Normand, S.L.T.; Krumholz, H.M. Association Between Subsequent Hospitalizations and Recurrent Acute Myocardial Infarction Within 1 Year After Acute Myocardial Infarction. J. Am. Heart Assoc. 2020, 9, e014907. [Google Scholar] [CrossRef] [PubMed]
- Shiyovich, A.; Bental, T.; Plakht, Y.; Vaknin-Assa, H.; Greenberg, G.; Lev, E.I.; Kornowski, R.; Assali, A. Prediction of mortality in hospital survivors of STEMI: External validation of a novel acute myocardial infarction prognostic score. Cardiovasc. Revasc. Med. 2019, 20, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Blaschke, T.F.; Osterberg, L.; Vrijens, B.; Urquhart, J. Adherence to medications: Insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu. Rev. Pharmacol. Toxicol. 2012, 52, 275–301. [Google Scholar] [CrossRef] [PubMed]
- Bansilal, S.; Castellano, J.M.; Garrido, E.; Wei, H.G.; Freeman, A.; Spettell, C.; Garcia-Alonso, F.; Lizano, I.; Arnold, R.J.; Rajda, J.; et al. Assessing the Impact of Medication Adherence on Long-Term Cardiovascular Outcomes. J. Am. Coll. Cardiol. 2016, 68, 789–801. [Google Scholar] [CrossRef]
- Valgimigli, M.; Garcia-Garcia, H.M.; Vrijens, B.; Vranckx, P.; McFadden, E.P.; Costa, F.; Pieper, K.; Vock, D.M.; Zhang, M.; Van Es, G.A.; et al. Standardized classification and framework for reporting, interpreting, and analysing medication non-adherence in cardiovascular clinical trials: A consensus report from the Non-adherence Academic Research Consortium (NARC). Eur. Heart J. 2019, 40, 2070–2085. [Google Scholar] [CrossRef]
- Hamood, H.; Hamood, R.; Green, M.S.; Almog, R. Determinants of adherence to evidence-based therapy after acute myocardial infarction. Eur. J. Prev. Cardiol. 2016, 23, 975–985. [Google Scholar] [CrossRef]
- Butler, J.; Arbogast, P.G.; BeLue, R.; Daugherty, J.; Jain, M.K.; Ray, W.A.; Griffin, M.R. Outpatient adherence to beta-blocker therapy after acute myocardial infarction. J. Am. Coll. Cardiol. 2002, 40, 1589–1595. [Google Scholar] [CrossRef][Green Version]
- Shiyovich, A.; Gilutz, H.; Arbelle, J.E.; Greenberg, D.; Plakht, Y. Temporal trends in healthcare resource utilization and costs following acute myocardial infarction. Isr. J. Health Policy Res. 2020, 9, 6. [Google Scholar] [CrossRef]
- Plakht, Y.; Gilutz, H.; Arbelle, J.E.; Greenberg, D.; Shiyovich, A. Healthcare-service utilization and direct costs throughout ten years following acute myocardial infarction: Soroka Acute Myocardial Infarction II (SAMI II) Project. Curr. Med. Res. Opin. 2019, 35, 1257–1263. [Google Scholar] [CrossRef]
- Menzin, J.; Korn, J.R.; Cohen, J.; Lobo, F.; Zhang, B.; Friedman, M.; Newmann, P.J. Relationship between glycemic control and diabetes-related hospital costs in patients with type 1 or type 2 diabetes mellitus. J. Manag. Care Pharm. 2010, 16, 264–275. [Google Scholar] [CrossRef] [PubMed]
- Kern, D.M.; Mellström, C.; Hunt, P.R.; Tunceli, O.; Wu, B.; Westergaard, M.; Hammar, N. Long-term cardiovascular risk and costs for myocardial infarction survivors in a US commercially insured population. Curr. Med. Res. Opin. 2016, 32, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Jepma, P.; Ter Riet, G.; van Rijn, M.; Latour, C.H.M.; Peters, R.J.G.; op Reimer, W.S.; Buurman, B.M. Readmission and mortality in patients >/=70 years with acute myocardial infarction or heart failure in the Netherlands: A retrospective cohort study of incidences and changes in risk factors over time. Neth. Heart J. 2019, 27, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Krumholz, H.M.; Lin, Z.; Keenan, P.S.; Chen, J.; Ross, J.S.; Drye, E.E.; Bernheim, S.M.; Wang, Y.; Bradley, E.H.; Han, L.F.; et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA 2013, 309, 587–593. [Google Scholar] [CrossRef]
- Dharmarajan, K.; Hsieh, A.F.; Lin, Z.; Bueno, H.; Ross, J.S.; Horwitz, L.I.; Barreto-Filho, J.A.; Kim, N.; Bernheim, S.M.; Suter, L.G.; et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA 2013, 309, 355–363. [Google Scholar] [CrossRef]
- Radovanovic, D.; Maurer, L.; Bertel, O.; Witassek, F.; Urban, P.; Stauffer, J.C.; Pedrazzini, G.; Erne, P. Treatment and outcomes of patients with recurrent myocardial infarction: A prospective observational cohort study. J. Cardiol. 2016, 68, 498–503. [Google Scholar] [CrossRef]
- Ahmedani, B.K.; Solberg, L.I.; Copeland, L.A.; Fang-Hollingsworth, Y.; Stewart, C.; Hu, J.; Nerenz, D.R.; Williams, L.K.; Cassidy-Bushrow, A.E.; Waxmonsky, J.; et al. Psychiatric comorbidity and 30-day readmissions after hospitalization for heart failure, AMI, and pneumonia. Psychiatr. Serv. 2015, 66, 134–140. [Google Scholar] [CrossRef]
- Rodriguez, F.; Cannon, C.P.; Steg, P.G.; Kumbhani, D.J.; Goto, S.; Smith, S.C.; Eagle, K.A.; Ohman, E.M.; Umez-Eronini, A.A.; Hoffman, E.; et al. Predictors of long-term adherence to evidence-based cardiovascular disease medications in outpatients with stable atherothrombotic disease: Findings from the REACH Registry. Clin. Cardiol. 2013, 36, 721–727. [Google Scholar] [CrossRef]
- Osterberg, L.; Blaschke, T. Adherence to medication. N. Engl. J. Med. 2005, 353, 487–497. [Google Scholar] [CrossRef]
- Ferdinand, K.C.; Senatore, F.F.; Clayton-Jeter, H.; Cryer, D.R.; Lewin, J.C.; Nasser, S.A.; Fiuzat, M.; Califf, R.M. Improving Medication Adherence in Cardiometabolic Disease: Practical and Regulatory Implications. J. Am. Coll. Cardiol. 2017, 69, 437–451. [Google Scholar] [CrossRef]
- Gilutz, H.; Steinberg, S.; Zahger, D.; Grotto, I. Secondary prevention after myocardial infarction: It takes two (physician and patient) to tango. Int. J. Cardiol. 2014, 172, e259–e260. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, J.; Zheng, X.; Jiang, Z.; Hu, S.; Wadhera, R.K.; Bai, X.; Lu, J.; Wang, Q.; Li, Y.; et al. Risk Factors Associated with Major Cardiovascular Events 1 Year After Acute Myocardial Infarction. JAMA Netw. Open 2018, 1, e181079. [Google Scholar] [CrossRef] [PubMed]
- Harel Gilutz, M.D.; Arbelle, J.E.; Shiyovich, A. Sex and Ethnic Disparities in Health-Related Outcomes Following Acute Myocardial Infarction in Israel. Isr. Med. Assoc. J. 2020, 22, 303–309. [Google Scholar]
- Roggeri, D.P.; Roggeri, A.; Rossi, E.; Cinconze, E.; De Rosa, M.; Maggioni, A.P.; The ARNO Cardiovascular Observatory. Direct healthcare costs and resource consumption after acute coronary syndrome: A real-life analysis of an Italian subpopulation. Eur. J. Prev. Cardiol. 2014, 21, 1090–1096. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).