Advancing Digital Workflows for Refractive Error Measurements
Abstract
1. Introduction
2. Experimental Section
2.1. Subjects
2.2. Experimental Procedures to Measure Refractive Errors Objectively and Subjectively
2.3. Assessment of Visual Acuity and Subjective Preference
2.4. Analysis and Statistics
3. Results
3.1. Agreement Between Subjective and Objective Refractions
3.2. Differences in Cylinder and Its Axis
3.3. Visual Acuity from Different Correction Methods
3.4. Subjective Preferences in Correction
3.5. Number of Decisions and Time for the Assessment of the Refraction
4. Discussion
4.1. Agreement and Percentage of Agreement Between Subjective and Objective Refractions
4.2. Differences in Cylinder and Its Axis
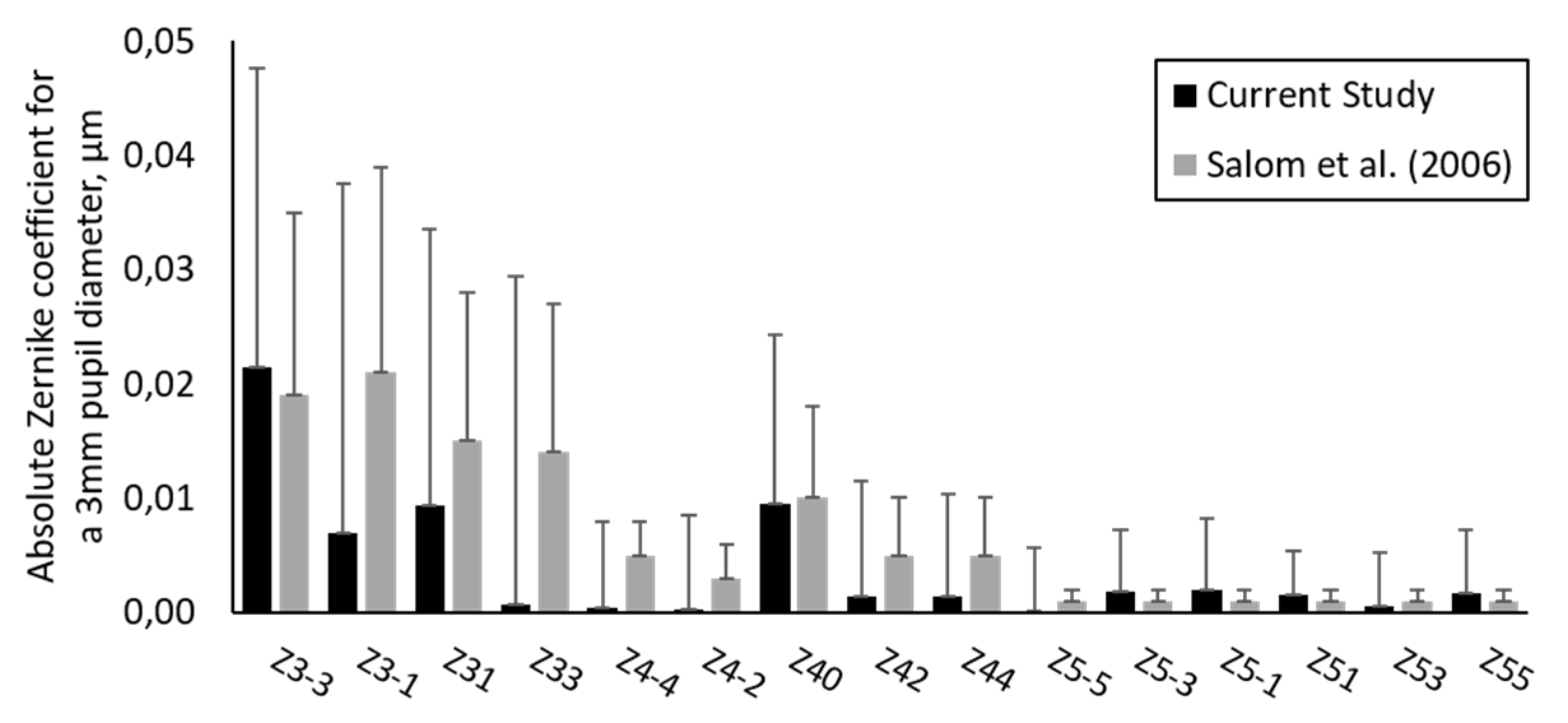
4.3. Impact of Higher Order Aberrations on Refraction Assessment
4.4. Visual Acuity with Each Correction
4.5. Subjective Preferences in Correction
4.6. Number of Decisions and Time for the Assessment of the Refraction
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Borish, I.M.; Benjamin, W.J. Borish’s Clinical Refraction, 2nd ed.; Benjamin, W.J., Ed.; Elsevier: Amsterdam, The Netherlands, 1998. [Google Scholar]
- Rosenfield, M.; Chiu, N.N. Repeatability of subjective and objective refraction. Optom. Vis. Sci. 1995, 72, 577–579. [Google Scholar] [CrossRef]
- Bullimore, M.A.; Fusaro, R.E.; Adams, C.W. The repeatability of automated and clinician refraction. Optom. Vis. Sci. 1998, 75, 617–622. [Google Scholar] [CrossRef]
- Goss, D.A.; Grosvenor, T. Reliability of refraction—A literature review. J. Am. Optom. Assoc. 1996, 67, 619–630. [Google Scholar]
- Raasch, T.W.; Schechtman, K.B.; Davis, L.J.; Zadnik, K. Repeatability of subjective refraction in myopic and keratoconic subjects: Results of vector analysis. Ophthalmic Physiol. Opt. 2001, 21, 376–383. [Google Scholar] [CrossRef]
- Zadnik, K.; Mutti, D.O.; Adams, A.J. The repeatability of measurement of the ocular components. Investig. Ophthalmol. Vis. Sci. 1992, 33, 2325–2333. [Google Scholar]
- Pesudovs, K.; Weisinger, H.S. A comparison of autorefractor performance. Optom. Vis. Sci. 2004, 81, 554–558. [Google Scholar] [CrossRef] [PubMed]
- Porter, J.; Guirao, A.; Cox, I.G.; Williams, D.R. Monochromatic aberrations of the human eye in a large population. J. Opt. Soc. Am. A 2001, 18, 1793. [Google Scholar] [CrossRef]
- Philip, K.; Sankaridurg, P.; Holden, B.; Ho, A.; Mitchell, P. Influence of higher order aberrations and retinal image quality in myopisation of emmetropic eyes. Vis. Res. 2014, 105, 233–243. [Google Scholar] [CrossRef] [PubMed]
- Salmon, T.O.; West, R.W.; Gasser, W.; Kenmore, T. Measurement of refractive errors in young myopes using the COAS Shack-Hartmann aberrometer. Optom. Vis. Sci. 2003, 80, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Nissman, S.A.; Tractenberg, R.E.; Saba, C.M.; Douglas, J.C.; Lustbader, J.M. Accuracy, repeatability, and clinical application of spherocylindrical automated refraction using time-based wavefront aberrometry measurements. Ophthalmology 2006, 113, 577.e1–2. [Google Scholar] [CrossRef]
- Ommani, A.; Hutchings, N.; Thapa, D.; Lakshminarayanan, V. Pupil Scaling for the Estimation of Aberrations in Natural Pupils. Optom. Vis. Sci. 2014, 91, 1175–1182. [Google Scholar] [CrossRef]
- Pesudovs, K.; Parker, K.E.; Cheng, H.; Applegate, R.A. The precision of wavefront refraction compared to subjective refraction and autorefraction. Optom. Vis. Sci. 2007, 84, 387–392. [Google Scholar] [CrossRef] [PubMed]
- Navarro, R. Objective refraction from aberrometry: Theory. J. Biomed. Opt. 2009, 14, 024021. [Google Scholar] [CrossRef] [PubMed]
- International Organization for Standardization. ISO 8596:2018—Ophthalmic Optics—Visual Acuity Testing—Standard and Clinical Optotypes and Their Presentation; International Organization for Standardization: Geneva, Switzerland, 2018. [Google Scholar]
- Mon-Williams, M.; Tresilian, J.R.; Strang, N.C.; Kochhar, P.; Wann, J.P. Improving vision: Neural compensation for optical defocus. Proc. Biol. Sci. 1998, 265, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. 1997, 74, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 327, 307–310. [Google Scholar] [CrossRef]
- Grein, H.-J.; Schmidt, O.; Ritsche, A. Reproducibility of subjective refraction measurement. Ophthalmologe 2014, 111, 1057–1064. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, H.; Pardhan, S.; Calver, R.I.; O’Leary, D.J. Unequal reduction in visual acuity with positive and negative defocusing lenses in myopes. Optom. Vis. Sci. 2004, 81, 14–17. [Google Scholar] [CrossRef]
- Leube, A.; Ohlendorf, A.; Wahl, S. The Influence of Induced Astigmatism on the Depth of Focus. Optom. Vis. Sci. 2016, 93, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
- Cleary, G.; Spalton, D.J.; Patel, P.M.; Lin, P.-F.; Marshall, J. Diagnostic accuracy and variability of autorefraction by the Tracey Visual Function Analyzer and the Shin-Nippon NVision-K 5001 in relation to subjective refraction. Ophthalmic Physiol. Opt. 2009, 29, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Allen, P.M.; Radhakrishnan, H.; O’Leary, D.J. Repeatability and validity of the PowerRefractor and the Nidek AR600-A in an adult population with healthy eyes. Optom. Vis. Sci. 2003, 80, 245–251. [Google Scholar] [CrossRef]
- Salmon, T.O.; van de Pol, C. Evaluation of a clinical aberrometer for lower-order accuracy and repeatability, higher-order repeatability, and instrument myopia. Optometry 2005, 76, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Lebow, K.A.; Campbell, C.E. A comparison of a traditional and wavefront autorefraction. Optom. Vis. Sci. 2014, 91, 1191–1198. [Google Scholar] [CrossRef] [PubMed]
- Teel, D.F.W.; Jacobs, R.J.; Copland, J.; Neal, D.R.; Thibos, L.N. Differences between Wavefront and Subjective Refraction for Infrared Light. Optom. Vis. Sci. 2014, 91, 1158–1166. [Google Scholar] [CrossRef] [PubMed]
- Atchison, D.A.; Smith, G. Chromatic dispersions of the ocular media of human eyes. J. Opt. Soc. Am. A 2005, 22, 29. [Google Scholar] [CrossRef]
- Guirao, A.; Williams, D.R. A method to predict refractive errors from wave aberration data. Optom. Vis. Sci. 2003, 80, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Wosik, J.; Patrzykont, M.; Pniewski, J. Comparison of refractive error measurements by three different models of autorefractors and subjective refraction in young adults. J. Opt. Soc. Am. 2019, 36, 1–6. [Google Scholar] [CrossRef]
- Jinabhai, A.; O’Donnell, C.; Radhakrishnan, H. A comparison between subjective refraction and aberrometry-derived refraction in keratoconus patients and control subjects. Cur. Eye Res. 2010, 35, 703–714. [Google Scholar] [CrossRef]
- Sabesan, R.; Jeong, T.M.; Carvalho, L.; Cox, I.G.; Williams, D.R.; Yoon, G. Vision improvement by correcting higher-order aberrations with customized soft contact lenses in keratoconic eyes. Opt. Lett. 2007, 32, 1000–1002. [Google Scholar] [CrossRef]
- Thibos, L.N.; Hong, X.; Bradley, A.; Applegate, R.A. Accuracy and precision of objective refraction from wavefront aberrations. J. Vis. 2004, 4, 9. [Google Scholar] [CrossRef]
- Salmon, T.O.; van de Pol, C. Normal-eye Zernike coefficients and root-mean-square wavefront errors. J. Cataract Refract. Surg. 2006, 32, 2064–2074. [Google Scholar] [CrossRef] [PubMed]



| Mean Difference, D | 95% Limit of Agreement, D | p | ||
|---|---|---|---|---|
| Wavefront Refraction vs. Autorefraction | S * | +0.36 | ±0.76 | < 0.001 |
| M’ | +0.36 | ±0.76 | < 0.001 | |
| J0° | Not assessed | |||
| J45^ | Not assessed | |||
| Standard Refraction vs. Autorefraction | S * | +0.27 | ±0.88 | < 0.001 |
| M’ | +0.35 | ±0.84 | < 0.001 | |
| J0° | −0.05 | ±0.35 | < 0.001 | |
| J45^ | +0.02 | ±0.27 | < 0.01 | |
| Standard Refraction vs. Wavefront Refraction | S * | 0.09 | ±0.65 | = 0.6 |
| M’ | +0.0 | ±0.65 | = 0.3 | |
| J0° | -0.05 | ±0.36 | < 0.001 | |
| J45^ | +0.02 | ±0.27 | < 0.01 | |
| Mean Difference in VA, logMAR | 95% Limit of Agreement, logMAR | p | |
|---|---|---|---|
| Wavefront Refraction vs. Autorefraction | −0.02 | ±0.07 | < 0.001 |
| Standard Refraction vs. Autorefraction | −0.03 | ±0.10 | < 0.001 |
| Standard Refraction vs. Wavefront Refraction | −0.01 | ±0.09 | = 0.02 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohlendorf, A.; Leube, A.; Wahl, S. Advancing Digital Workflows for Refractive Error Measurements. J. Clin. Med. 2020, 9, 2205. https://doi.org/10.3390/jcm9072205
Ohlendorf A, Leube A, Wahl S. Advancing Digital Workflows for Refractive Error Measurements. Journal of Clinical Medicine. 2020; 9(7):2205. https://doi.org/10.3390/jcm9072205
Chicago/Turabian StyleOhlendorf, Arne, Alexander Leube, and Siegfried Wahl. 2020. "Advancing Digital Workflows for Refractive Error Measurements" Journal of Clinical Medicine 9, no. 7: 2205. https://doi.org/10.3390/jcm9072205
APA StyleOhlendorf, A., Leube, A., & Wahl, S. (2020). Advancing Digital Workflows for Refractive Error Measurements. Journal of Clinical Medicine, 9(7), 2205. https://doi.org/10.3390/jcm9072205





