Quality of Life Outcomes in Frontal Sinus Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Statistical Analysis
2.2. Statistical Software
3. Results
3.1. Symptom by Symptom Analysis—1–3 Months Postoperative Follow-Up
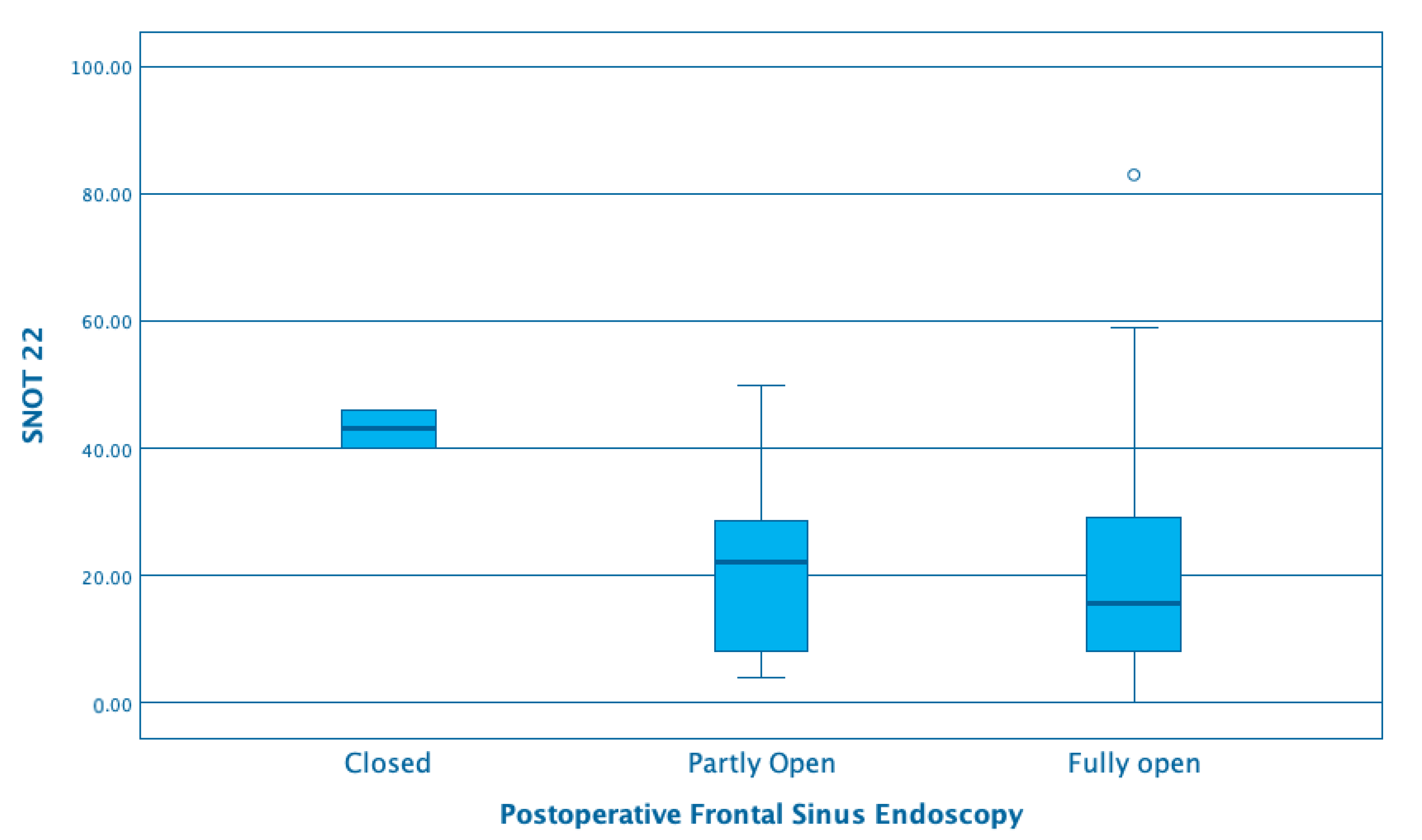
3.2. Endoscopic Examination of Frontal Sinus (Neo)-Ostium
4. Discussion
4.1. Endoscopic Sinus Surgery
4.2. Frontal Sinus Surgery
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Soler, Z.M.; Wittenberg, E.; Schlosser, R.J.; Mace, J.C.; Smith, T.L. Health state utility values in patients undergoing endoscopic sinus surgery. Laryngoscope 2011, 121, 2672–2678. [Google Scholar] [CrossRef] [PubMed]
- Fokkens, W.J.; Lund, V.J.; Mullol, J.; Bachert, C.; Alobid, I.; Baroody, F.; Cohen, N.; Cervin, A.; Douglas, R.; Gevaert, P.; et al. EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 2012, 50, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, C.; Rimmer, J.; Lund, V.J. Does time to endoscopic sinus surgery impact outcomes in Chronic Rhinosinusitis? Prospective findings from the National Comparative Audit of Surgery for Nasal Polyposis and Chronic Rhinosinusitis. Rhinol. J. 2015, 53. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, R.R.; Kingdom, T.; Hwang, P.H.; Smith, T.L.; Alt, J.A.; Baroody, F.M.; Batra, P.S.; Bernal-Sprekelsen, M.; Bhattacharyya, N.; Chandra, R.K.; et al. International Consensus Statement on Allergy and Rhinology: Rhinosinusitis. Int. Forum Allergy Rhinol. 2016, 6, S22–S209. [Google Scholar] [CrossRef]
- Draf, W. Endonasal micro-endoscopic frontal sinus surgery: The fulda concept. Oper. Tech. Otolaryngol. Neck Surg. 1991, 2, 234–240. [Google Scholar] [CrossRef]
- Weber, R.; Draf, W.; Keerl, R.; Behm, K.; Schick, B. Long-term results of endonasal frontal sinus surgery. HNO 1996, 44, 503–509. [Google Scholar] [CrossRef]
- Georgalas, C.; Hansen, F.; Videler, W.J.M.; Fokkens, W.J. Long terms results of Draf 3 procedure. Rhinology 2011, 49, 195–201. [Google Scholar] [CrossRef]
- Georgalas, C.; Fokkens, W. The Frontal Sinus. In Rhinology and Skull Base Surgery; Thieme Publications: Stuttgart, Germany, 2013. [Google Scholar]
- DeConde, A.S.; Smith, T.L. Outcomes After Frontal Sinus Surgery: An Evidence-Based Review. Otolaryngol. Clin. N. Am. 2016, 49, 1019–1033. [Google Scholar] [CrossRef]
- Piccirillo, J.F.; Haiduk, D.; Yonan, A.; Thawley, C. Psychometric and clinimetric validitiy of the 31-item rhinosinusitis outcome measure (RSOM-31). Am. J. Rhinol. Allergy 1995, 9, 297–306. [Google Scholar] [CrossRef]
- Hopkins, C.; Gillett, S.; Slack, R.; Lund, V.; Browne, J. Psychometric validity of the 22-item Sinonasal Outcome Test. Clin. Otolaryngol. 2009, 34, 447–454. [Google Scholar] [CrossRef]
- Lund, V.J.; Mackay, I.S. Staging in rhinosinusitus. Rhinol. J. 1993, 31, 183–184. [Google Scholar]
- Chiu, A. Frontal sinus surgery: Its evolution, present standard of care, and recommendations for current use. Ann. Otol. Rhinol. Laryngol. Suppl. 2006, 196, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Silverman, J.B.; Gray, S.T.; Busaba, N.Y. Role of Osteoplastic Frontal Sinus Obliteration in the Era of Endoscopic Sinus Surgery. Int. J. Otolaryngol. 2012, 2012, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Basu, S.; Georgalas, C.; Kumar, B.N.; Desai, S. Correlation between symptoms and radiological findings in patients with chronic rhinosinusitis: An evaluation study using the Sinonasal Assessment Questionnaire and Lund-Mackay grading system. Eur. Arch. Oto-Rhino-Laryngol. 2005, 262, 751–754. [Google Scholar] [CrossRef]
- Laababsi, R.; Bushra, A.; Elkrimi, Z.; Allouane, A.; Rouadi, S.; Abada, R.; Roubal, M.; Mahtar, M. Quality of life outcomes of patients with chronic rhinosinusitis after functional endoscopic sinus surgery, prospective cohort study. Ann. Med. Surg. 2019, 40, 9–13. [Google Scholar] [CrossRef]
- Hopkins, C.; Rudmik, L.; Lund, V.J. The predictive value of the preoperative Sinonasal outcome test-22 score in patients undergoing endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope 2015, 125, 1779–1784. [Google Scholar] [CrossRef]
- Zachary, M.S.; Rabun, J.; Le, P.; Rudmik, L.; Jose, L.M.; Shaun, A.N.; Rodney, J.S. Snot-22 Outcomes after Sinus Surgery: A Systematic Review and Meta-analysis. Laryngoscope 2018, 128, 581–592. [Google Scholar]
- Le, P.T.; Soler, Z.M.; Jones, R.; Mattos, J.L.; Nguyen, S.A.; Schlosser, R.J. Systematic Review and Meta-analysis of SNOT-22 Outcomes after Surgery for Chronic Rhinosinusitis with Nasal Polyposis. Otolaryngol. Neck Surg. 2018, 159, 414–423. [Google Scholar] [CrossRef]
- Beswick, D.M.; Mace, J.C.; Chowdhury, N.I.; Alt, J.A.; Hwang, P.H.; DeConde, A.S.; Smith, T.L. Comparison of surgical outcomes between patients with unilateral and bilateral chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2017, 7, 1162–1169. [Google Scholar] [CrossRef]
- Patel, V.S.; Choby, G.; Patel, Z.M.; Nayak, J.V.; Hwang, P.H.; Shih, L.-C. Equivalence in outcomes between Draf 2B vs Draf 3 frontal sinusotomy for refractory chronic frontal rhinosinusitis. Int. Forum Allergy Rhinol. 2017, 8, 25–31. [Google Scholar] [CrossRef]
- Jafari, A.; Tringale, K.R.; Panuganti, B.A.; Acevedo, J.R.; Pang, J.; DeConde, A.S. Short-Term Morbidity after the Endoscopic Modified Lothrop (Draf-III) Procedure Compared with Draf-IIa. Am. J. Rhinol. Allergy 2017, 31, 265–270. [Google Scholar] [CrossRef] [PubMed]
- DeConde, A.S.; Mace, J.C.; Alt, J.A.; Soler, Z.M.; Orlandi, R.R.; Smith, T.L. Investigation of change in cardinal symptoms of chronic rhinosinusitis after surgical or ongoing medical management. Int. Forum Allergy Rhinol. 2014, 5, 36–45. [Google Scholar] [CrossRef] [PubMed]
- Wong, E.; Do, T.Q.-P.; Harvey, R.J.; Orgain, C.A.; Sacks, R.; Kalish, L.H. Patient-reported olfaction improves following outside-in Draf III frontal sinus surgery for chronic rhinosinusitis. Laryngoscope 2018, 129, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Lal, D.; Rounds, A.; Divekar, R. Gender-Specific differences in chronic rhinosinusitis patients electing endoscopic sinus surgery. Int. Forum Allergy Rhinol. 2015, 6, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Lal, D.; Golisch, K.B.; Elwell, Z.A.; Divekar, R.; Rank, M.A.; Chang, Y.-H. Gender-specific analysis of outcomes from endoscopic sinus surgery for chronic rhinosinusitis. Int. Forum Allergy Rhinol. 2016, 6, 896–905. [Google Scholar] [CrossRef]

| Draf 2a (N = 21) | Draf 2b (N = 55) | Draf 3 (N = 23) | p | |
|---|---|---|---|---|
| Mean age/range | 43.8 (19–68) years | 47.5 (12–80) years | 43 (17–61) years | ns |
| Lund–Mckay CT Score: mean(SD) | 14.1 (5.1) | 14.6 (5.3) | 14.9 (5,8) | ns |
| Frontal sinus CT score: | 2.4 (1.3) | 2.3 (1.4) | 2.5 (1.2) | ns |
| Male/female ratio | 13/8 | 27/28 | 14/9 | ns |
| Revision surgery | 0 | 1 | 4 | ns |
| Local flap | 0 | 1 | 17 | p < 0.01 |
| Septoplasty and/or turbinoplasty | 4 | 7 | 0 | ns |
| Asthma | 0 | 0 | 1 | ns |
| AERD | 0 | 1 | 2 | ns |
| Operation | Mean | p-Value | |
|---|---|---|---|
| SNOT22 | Draf 2 | 45.63 | 0.023 |
| Draf 3 | 59.00 | ||
| Need to blow nose: | Draf 2 | 2.91 | 0.104 |
| Draf 3 | 3.63 | ||
| Sneezing: | Draf 2 | 1.58 | 0.081 |
| Draf 3 | 2.31 | ||
| Runny nose: | Draf 2 | 2.03 | 0.050 |
| Draf 3 | 2.94 | ||
| Nasal blockage: | Draf 2 | 3.56 | 0.996 |
| Draf 3 | 3.56 | ||
| Loss of smell/taste: | Draf 2 | 3.02 | 0.087 |
| Draf 3 | 3.94 | ||
| Cough: | Draf 2 | 1.42 | 0.572 |
| Draf 3 | 1.69 | ||
| Postnasal drip: | Draf 2 | 2.62 | 0.406 |
| Draf 3 | 3.00 | ||
| Thick nasal discharge: | Draf 2 | 2.68 | 0.029 |
| Draf 3 | 3.69 | ||
| Ear fullness: | Draf 2 | 1.61 | 0.273 |
| Draf 3 | 2.13 | ||
| Dizziness: | Draf 2 | 1.23 | 0.034 |
| Draf 3 | 2.13 | ||
| Ear pain: | Draf 2 | 0.85 | 0.791 |
| Draf 3 | 0.94 | ||
| Facial pain or pressure: | Draf 2 | 2.30 | 0.584 |
| Draf 3 | 2.56 | ||
| Difficulty falling asleep: | Draf 2 | 2.12 | 0.523 |
| Draf 3 | 2.44 | ||
| Wake up at night: | Draf 2 | 2.20 | 0.785 |
| Draf 3 | 2.06 | ||
| Lack of a good night’s sleep: | Draf 2 | 2.56 | 0.703 |
| Draf 3 | 2.75 | ||
| Wake up tired: | Draf 2 | 2.62 | 0.262 |
| Draf 3 | 3.13 | ||
| Fatigue: | Draf 2 | 2.52 | 0.273 |
| Draf 3 | 3.00 | ||
| Reduced productivity: | Draf 2 | 1.92 | 0.012 |
| Draf 3 | 3.13 | ||
| Reduced concentration: | Draf 2 | 1.74 | 0.004 |
| Draf 3 | 3.00 | ||
| Frustrated/restless/irritable: | Draf 2 | 2.11 | 0.008 |
| Draf 3 | 3.31 | ||
| Sadness: | Draf 2 | 1.17 | 0.012 |
| Draf 3 | 2.13 | ||
| Embarrassment: | Draf 2 | 0.83 | 0.056 |
| Draf 3 | 1.56 |
| Draf 2 | Draf 3 | |||||
|---|---|---|---|---|---|---|
| Mean Change | Standard Deviation | p Value | Mean Change | Standard Deviation | p Value | |
| SNOT22 | 22.87 | 20.9 | 0.000 | 37.00 | 25.73 | 0.000 |
| Need to blow nose | 1.47 | 1.78 | 0.000 | 2.27 | 1.94 | 0.000 |
| Sneezing | 0.45 | 1.66 | 0.048 | 1.53 | 1.30 | 0.000 |
| Runny nose | 1.24 | 1.66 | 0.000 | 2.47 | 1.95 | 0.000 |
| Nasal blockage | 1.89 | 1.84 | 0.000 | 2.33 | 1.63 | 0.000 |
| Loss of smell/taste | 1.29 | 2.20 | 0.000 | 0.87 | 2.20 | 0.149 |
| Cough | 0.69 | 1.39 | 0.001 | 0.93 | 1.53 | 0.034 |
| Postnasal drip | 1.02 | 1.75 | 0.000 | 1.47 | 1.84 | 0.008 |
| Thick nasal discharge | 0.94 | 1.99 | 0.001 | 1.87 | 1.72 | 0.001 |
| Ear fullness | 0.62 | 1.77 | 0.013 | 1.33 | 2.22 | 0.036 |
| Dizziness | 0.54 | 1.50 | 0.009 | 1.73 | 1.48 | 0.000 |
| Ear pain | 0.40 | 1.34 | 0.031 | 0.80 | 1.20 | 0.022 |
| Facial pain or pressure | 1.11 | 1.80 | 0.000 | 1.33 | 1.79 | 0.012 |
| Difficulty falling asleep | 1.45 | 1.58 | 0.000 | 1.67 | 1.98 | 0.006 |
| Wake up at night | 1.30 | 1.62 | 0.000 | 1.27 | 2.07 | 0.027 |
| Lack of a good night’s sleep | 1.37 | 1.47 | 0.000 | 1.33 | 1.92 | 0.041 |
| Wake up tired | 1.27 | 1.40 | 0.000 | 1.80 | 2.11 | 0.005 |
| Fatigue | 1.05 | 1.61 | 0.000 | 1.60 | 1.24 | 0.006 |
| Reduced productivity | 0.73 | 1.72 | 0.000 | 1.80 | 1.30 | 0.005 |
| Reduced concentration | 0.60 | 1.16 | 0.008 | 2.13 | 1.58 | 0.000 |
| Frustrated/restless/irritable | 1.00 | 1.02 | 0.000 | 2.53 | 1.61 | 0.000 |
| Sadness | 0.56 | 20.93 | 0.001 | 1.33 | 25.73 | 0.006 |
| Embarrassment | 0.38 | 1.78 | 0.008 | 1.20 | 1.94 | 0.012 |
| 1–3 Months | 3–6 Months | 6–12 Months | 12–24 Months | 24–48 Months | |
|---|---|---|---|---|---|
| Draf 2 | 22.7 (N = 55) | 20.9 (N = 37) | 25.5 (N = 18) | 29.5 (N = 9) | 31.0 (N = 2) |
| Draf 3 | 22 (N = 18) | 21.2 (N = 14) | 31.0 (N = 8) | 38.5 (N = 7) | 7.5 (N = 3) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Georgalas, C.; Detsis, M.; Geramas, I.; Terzakis, D.; Liodakis, A. Quality of Life Outcomes in Frontal Sinus Surgery. J. Clin. Med. 2020, 9, 2145. https://doi.org/10.3390/jcm9072145
Georgalas C, Detsis M, Geramas I, Terzakis D, Liodakis A. Quality of Life Outcomes in Frontal Sinus Surgery. Journal of Clinical Medicine. 2020; 9(7):2145. https://doi.org/10.3390/jcm9072145
Chicago/Turabian StyleGeorgalas, Christos, Marios Detsis, Ioannis Geramas, Dimitris Terzakis, and Andreas Liodakis. 2020. "Quality of Life Outcomes in Frontal Sinus Surgery" Journal of Clinical Medicine 9, no. 7: 2145. https://doi.org/10.3390/jcm9072145
APA StyleGeorgalas, C., Detsis, M., Geramas, I., Terzakis, D., & Liodakis, A. (2020). Quality of Life Outcomes in Frontal Sinus Surgery. Journal of Clinical Medicine, 9(7), 2145. https://doi.org/10.3390/jcm9072145






